Abstract
Purpose
To evaluate the safety and efficacy of hip arthroscopy immediately following gunshot wound (GSW) to the hip.
Methods
Patients who received hip arthroscopy for GSWs from 2006 to 2020 by 2 surgeons at a level I trauma center were identified by Current Procedural Terminology codes. Inclusion criteria were those patients who suffered a GSW to the hip, received hip arthroscopy for treatment, and had a minimum follow-up of 2 months. The exclusion criteria were any patients younger than 18 years of age. Medical records were reviewed for patient demographics, surgical details, clinical outcomes, and complications.
Results
A total of 50 hip arthroscopy cases were identified by Current Procedural Terminology codes. Of the 50 cases identified, 8 patients met the inclusion criteria. All 8 patients were male, African-American, and the mean age was 31 years (range, 19-54 years) with mean follow-up of 14 months. Five of 8 cases were noted to have poor visualization with arthroscopy. Common reasons for poor visualization were difficult access to the bullet fragments, morbid obesity, hematoma formation, and pre-existing arthritis. Of these 5 cases, 2 were converted to open procedures to retrieve the remaining bullet fragments. One patient developed abdominal compartment syndrome, most likely due to increased pulse pressure over a prolonged operative period and involvement of the acetabular fovea. Emergent exploratory laparotomy and abdominal compartment fluid release were performed, and the patient had an otherwise unremarkable hospital course.
Conclusions
There are risks with the use of arthroscopic methods to remove GSW fragments, which may be greater than elective hip arthroscopy. Certain factors, such as the surgeon’s arthroscopic experience, locations of bullets fragments, visual quality, length of procedure, and concomitant acetabular fractures, must be considered before proceeding with arthroscopy.
Level of Evidence
Therapeutic case series.
Gunshot wounds (GSWs) to the hip are uncommon, typically causing articular damage and shrapnel retained within the joint. If not removed, these fragments subject the patient to an increased risk of arthritis secondary to third-body wear, chondrotoxicity from metal particles, and mechanical pain.1 Open arthrotomy for shrapnel removal has been the procedure of choice for many years, but in 1998 arthroscopic extraction of bullet fragments was first introduced as an alternative for patients with GSWs to the hip.2
Since then, arthroscopy has become an attractive alternative because it minimizes muscle and soft-tissue dissection and may decrease operative time and speed postoperative recovery. Also, there may be a reduced risk of vascular injury and consequently osteonecrosis of the femoral head since hip dislocation is not warranted in most cases.3 Despite the impressive evolution of arthroscopic techniques and experience throughout the years, there is still limited literature on indications, success rate, and complications in individuals who suffer from GSWs to the hip. The methods by which main outcomes were measured were modeled after previous studies that looked at bullet fragment removal in patients using surgical hip-dislocation methods.3 The purpose of this study is to evaluate the safety and efficacy of hip arthroscopy immediately following GSW to the hip. We hypothesized that there would be risks associated with arthroscopy for GSW to the hip; however, the success of the surgeries at removing fragments would be appreciable.
Methods
Two attending surgeons (B.M. and J.E.) performed hip arthroscopy at our institution. Hip arthroscopies performed by these physicians for loose bodies at the level 1 trauma center from 2006 to 2020 were obtained. These surgeries were performed at a Level l urban academic trauma center in the Midwest. Current Procedural Terminology codes (2980, 29861, 29862, 29863, 29916) were used to distinguish hip arthroscopy cases. The inclusion criteria consisted of patients who suffered a GSW to the hip and had arthroscopy performed with a minimum follow-up of 6 months. The GSWs from the 8 patients had various degrees of intra-articular fragments with signs of bullet components imbedded into the acetabulum. The study excluded patients younger than 18 years of age. Electronic medical records were reviewed to determine whether any complications developed either during the inpatient stay or as an outpatient, and the efficacy of the procedures were determined by the type of complications noted. The outcomes of the procedures also were noted to determine the efficacy of the procedure (i.e., whether any pain or functional impairments occurred postoperatively).
Hip arthroscopy was performed with the patient in the supine position under general anesthesia and with the extremity in traction on a fracture table. Traction was applied to the effected hip joint of the patient. The hip joint was entered by making anterior, anterolateral, and posterolateral portals.
Results
A total of 50 hip arthroscopy procedures were identified. Eight of these patients met the inclusion criteria. All patients were male, African-American, and the mean age was 31 years. Two patients were lost to follow-up (Table 1: Patients 1-2), whereas the mean follow-up period for the remaining patients (Table 1: Patients 3-8) was 57 weeks (∼14 months) with a range of 2 months to 5 years. Five of the 7 cases were noted to have poor visualization with arthroscopy (Table 1: Patients 1-4, 7). Reasons for poor visualization were difficult access to the bullet fragments, morbid obesity, hematoma formation, and pre-existing arthritis. Of these 5 cases, 2 were converted to open procedures (Table 1: Patients 2, 4) to retrieve the remaining bullet fragments. In 2 other cases, the decision was made against an open procedure (Table 1: Patient 1, 3), since the location and the amount of debris suggested minimal clinical significance. The other case with poor visualization (Table 1: Patient 7) developed abdominal compartment syndrome immediately after arthroscopy.
Table 1.
List of Patients Who Suffered Gunshot Wounds to the Hip
| Patients | Diagnosis | Operation | Complications | Blood Loss, mL | Surgical Time, min |
|---|---|---|---|---|---|
| Patient 1∗ | Left hip gunshot wound | Left hip arthroscopy with bullet removal and chondroplasty | Nothing acute but no follow-up | 5 | 178 |
| Patient 2∗,† | Left hip gunshot wound | Left hip diagnostic arthroscopy | Nothing acute but no follow-up | 50 | 129 |
| Patient 3∗ | Right hip gunshot wound | Right hip diagnostic arthroscopy | Hip pain | 10 | 17 |
| Patient 4∗,† | Right hip gunshot wound, right femoral head/acetabular fractures | Right hip arthroscopy with loose body removal | Post-traumatic arthritis | 600 | 248 |
| Patient 5 | Right hip gunshot wound, right femoral head/acetabular fractures | EUA, right hip arthroscopy with loose body removal and chondroplasty | Post-traumatic arthritis | 5 | 59 |
| Patient 6 | Left hip gunshot wound, left femoral head/acetabular fractures | Left hip arthroscopy with loose body removal | None | 10 | 69 |
| Patient 7∗ | Left hip gunshot wound, Left acetabular fracture | EUA, left hip arthroscopy with loose body removal | Abdominal compartment syndrome | 10 | 103 |
| Patient 8 | Left hip gunshot wound | Left hip arthroscopy with loose body removal | None | 10 | 71 |
EUA, examination under anesthesia.
Case was reported to have poor visualization with arthroscopy.
Case was converted to an open approach, generally due to poor visualization.
Two cases were converted to open procedures since bullet fragments could not be visualized with arthroscopy but could with fluoroscopy. In 1 case (Table 1: Patient 2), the modified Gibson posterior surgical approach was used (in between gluteus maximus and medius) and the bullet fragments were successfully removed. The patient did not suffer acute complications but was lost to follow-up. A Kocher–Langerback posterior approach was used in the other case (Table 1: Patient 4), and the bullet fragments were successfully removed with no acute complications. The decision to not convert the other 3 cases that had poor visualization (Table 1: Patients 1, 3, 7) was primarily due to the observed risks of converting to an open procedure versus the opportunity to remove all bullet fragments.
Two patients developed radiographic and clinical signs of post-traumatic arthritis. In one procedure, the Kocher–Langerback (Table 1: Patient 4), the open posterior approach was used to remove the remaining bullet debris. The patient had no complaints at 1 month following the procedure but complained of right hip pain 5 years later during a visit with a primary care physician. Radiographs at that time demonstrated post-traumatic arthritis. Another patient (Table 1: Patient 5) complained of continued hip pain 3 months postoperatively, and radiographs at that time also demonstrated the development of post-traumatic arthritis. Of note, these 2 patients did present with combined acetabular and femoral head fractures.
Three patients complained of postoperative hip pain. Two patients had radiographic films confirming post-traumatic arthritis (Table 1: Patients 4, 5). In another case (Table 1: Patient 3), during arthroscopy, poor visualization was noted secondary to morbid obesity and pre-existing significant arthritis. It was determined to not perform open removal, since the bullet fragments were not impinging on the joint and the patient suffered a recent myocardial infarction and consequently was a poor candidate for a prolonged procedure with increased blood loss. The patient did well initially and had no acute complications postoperatively. During a 3-month orthopaedic follow-up, the patient had no complaints and it was then determined that he could follow-up as needed. However, during a general surgery follow-up 2 months later, the patient complained of increasing hip pain. An orthopaedic referral was made, but the patient did not follow-up.
The most serious complication occurred in 1 individual (Table 1: Patient 7) immediately after arthroscopy. Poor visualization was noted secondary to blood and severe acetabular wall comminution, and the decision was made to increase the fluid pulse pressure. Of note, the major bullet fragment had penetrated the fovea centralis and left the acetabulum comminuted. Due to the high degree of comminution at the fovea, the increase in fluid pulse pressure caused an increase in the peritoneal cavity. After taking down the drapes, the patient was noted to have a significantly larger abdomen (Fig 1), and general surgery was urgently consulted for abdominal compartment syndrome. General surgery performed an exploratory laparotomy with intra-pelvic extravasation of arthroscopic fluid and blood. The patient did not experience any other postoperative complications and had an unremarkable hospital and outpatient course without further complications.
Fig 1.
Patient 7 immediately after drapes were removed, showing significant abdominal distention from fluid extravasation. General surgery was immediately consulted.
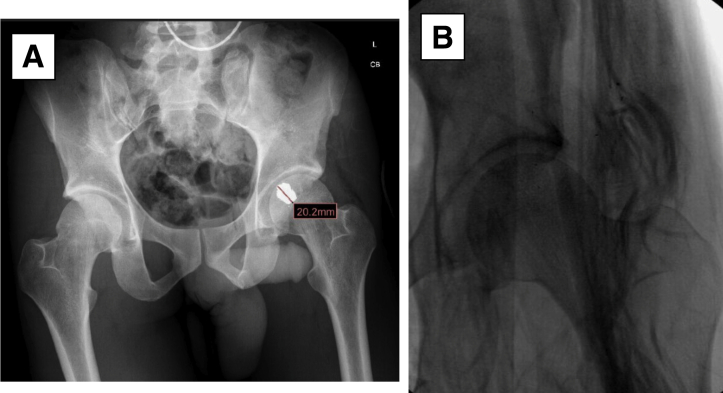
Of note, in 6 of 8 cases we were able to remove a majority if not all of the bullet fragments in the joint space. In 5 of the 8 cases, we were able to successfully remove all foreign debris, which was confirmed through intra- and/or postoperative plain films. Figure 2A shows an arthroscopic image of Patient 8 before the removal of any fragments. Bullet fragments can be noted on in the synovial space of the hip. Figure 2B shows an arthroscopic image of the same patient after the removal of all of the bullet fragments along with the fragment itself outside of the patient’s joint. The difference in bullet fragments postdebridement can be appreciated. Further confirmation of the removal of all the bullet fragments can be seen in the plain films taken postoperatively compared with the films taken preoperatively (Fig 3 A and B).
Fig 2.
Patient 8: Arthroscopic images taken intraoperatively as well as the bone fragment that was extracted. (A) Primary bullet fragment embedded in the articular surface of the. acetabulum. (B) Bone defect after bullet fragment was removed. (C) Major bullet fragment removed from the joint space.
Fig 3.
Pelvic radiograph imaging of Patient 8. (A) Preoperative imaging of patient’s pelvis with bullet fragment dimensions shown. (B) Postoperative imaging of the hip joint showing. complete removal of the bullet fragment.
Discussion
This study showed that there are risks for complications associated with arthroscopy following a GSW that have not been previously reported for this injury. Bullet fragments in the hip joint present a significant problem, as they increase the risk of chondrotoxity from metal breakdown, synovitis, deep-tissue infection, and traumatic arthritis.4 The bullet typically must be removed and the joint thoroughly irrigated. There are advantages to arthroscopy over open arthrotomy, which include visualization of the hip joint without the need to dislocate the femoral head, minimal soft-tissue disruption, typically shorter operative times, faster recovery, and theoretically decreasing the risk of avascular necrosis and stiffness.3,5 These advantages have made hip arthroscopy a popular alternative for orthopaedic surgeons when managing patients with GSWs to the hip.
However, hip arthroscopy may not be familiar to as many surgeons as standard open techniques.3 Complications of hip arthroscopy include iatrogenic articular injury, pudendal nerve injuries, typically if traction exceeds 2 hours and if there is inadequate padding of the perineal region, and the potential for abdominal compartment syndrome, seen with intra-articular fluid extravasation. However, hip arthroscopy offers a minimally invasive surgery while having the ability to diagnose and treat acute and chronic pathologies of the hip.6
Due to the uniqueness of this injury, there is not extensive literature pertaining to arthroscopy following GSWs to the hip. Of 14 publications found specific to this topic, 9 were case studies that focused on a single patient,1, 2, 3, 4, 5,7, 8, 9, 10 whereas 1 study included 4 patients and another study compiled 4 patients from 5 different studies.6,11 To the best of our knowledge, despite the small series reported in this study, it is the largest series reported to date at a single institution. The consensus in the limited literature, including a recent systematic review, is that hip arthroscopy may provide an efficient way to remove bullet fragments while limiting complications.12 This study was able to report outcomes of several arthroscopically managed GSWs from a single hospital facility for the first time. Previous studies have not been able to analyze the outcomes of arthroscopic surgeries for the treatment of GSWs with as many patients from a single institution.
Overall complications of hip arthroscopy have been estimated to be ∼1% to 13%.13 The most common complications are traction injuries or peripheral nerve injuries, such as peroneal, sciatic, femoral nerve injuries, lateral femoral cutaneous nerve transection, and pressure wounds to the sacrum.14 These injuries can be seen with longer operative times (>2 hours) as well as with inexperienced surgeons.1 These common complications reported in the literature were not seen in our series.
In this series, complications were seen in 4 patients (57%) postoperatively. Three patients complained of hip pain, 2 of whom had radiographic evidence of post-traumatic arthritis. This was not a complication unique to this study. Cory and Ruch5 published a case report in which the patient presenting with a GSW and consequently a significantly comminuted femoral head fracture was treated with arthroscopy. One year postoperatively, radiographic images were significant for joint space narrowing and subchondral sclerosis. Interestingly, the 2 patients in our study who developed post-traumatic arthritis also presented with intra-articular fractures. In another study, a patient who received hip arthroscopy after a GSW presented 2 years postoperatively with significant hip pain secondary to chondral damage, which ultimately needed surgical dislocation and open debridement.4 With this in mind, even though arthroscopy theoretically limits the risk of chondral damage and arthritis, there is still a moderate risk of these complications due to significant soft-tissue damage and intra-articular fractures from the initial trauma.
Another interesting finding in our study was that 5 of the 7 arthroscopic procedures (71%) were noted to yield poor visualization of the bullet fragments. The inadequate visualization was secondary to multiple factors, such as morbid obesity, pre-existing arthritis, significant hematoma formation, and difficulty accessing the location. Two arthroscopic procedures were converted to open procedures due to the inability to access the remaining bullet fragments in the hip joint (Table 1: Patients 2 and 4). In one procedure, consideration was given to convert to open, but the patient’s medical condition was poor and the surgeon felt the risks outweighed the benefits. In 1 case (Table 1: Patient 2) the bullet fragments were deep, sitting just off of the posterior wall of the acetabulum and in the other case (Table 1: Patient 4), the bullet fragment was deep and located in the inferior hip joint. Lee et al.11 had 1 of 4 patients require conversion to open arthrotomy because the bullet’s location prevented safe arthroscopic extraction without further damage to the bone. Given the findings in this paper in conjunction with other studies, it is important for the surgeon attempting arthroscopy to be comfortable converting to an open approach, and the open approach might be favored over hip arthroscopy if preoperative imaging suggests the fragment may be difficult to visualize or reach. Cases involving significant soft-tissue injury requiring debridement and large osteochondral fragments should also be considered to be treated with open arthrotomy rather than an arthroscopic procedure.8
The most significant finding in our study was the unfortunate complication of abdominal compartment syndrome that occurred in 1 patient (Table 1: Patient 7, Fig 1). In a cohort study of 15 expert hip arthroscopists, it was determined that fluid extravasation occurs approximately ∼0.1% with iliopsoas tenotomy and capsulotomy being known risk factors.13 Despite its rarity, this complication is of grave importance, as it has been previously reported and can even lead to cardiac arrest secondary to inferior vena cava compression.15
In the case of abdominal compartment syndrome, it was noted that visualization was poor due to the amount of blood in the joint along with severe comminution of the acetabular wall. At that time, fluid pulse pressure was increased to gain better visualization. Increased pump pressure is most likely a contributing factor to fluid extravasation as well.13 In one study, the pump pressure was set to 20 mm Hg to limit abdominal compartment syndrome, whereas in another study, the pump pressure was set to 40 to 60 mm Hg without complications.6 Mullis and Dahners14 performed hip arthroscopies with a pump pressure of 60 mm Hg in conjunction with hypotensive anesthesia (systolic blood pressure <100 mm Hg) with excellent visualization following hip dislocations. Extravasation of fluid into the gluteal compartment was frequently noted in that study, but it did not lead to any serious complications. The pump pressure in our case with abdominal syndrome was also set at 60 mm Hg. With this in mind, surgeons should be particular aware of the possible sequela of fluid extravasation and play close attention to the pulse pressure and time, as bullet tracts may allow communication between the abdomen, pelvis, and hip joint, especially if there is an associated acetabulum fracture.6 More so, surgeons should take extreme precautions when dealing with cases that involve the acetabular fovea due to the increased risk of fluid extravasation into the abdominal compartment. Poor visualization in cases that involve the fovea should have increased caution with the amount of fluid pulse pressure being introduced to the joint space to decrease the risk of abdominal compartment syndrome and other postoperative complications.
There are other measures that can be taken to limit abdominal compartment syndrome. In one study, frequent examination by palpation of the gluteal compartment was performed to check for clinical signs of compartment syndrome. Gravity also was used to control the rate of inflow and outflow of fluid throughout that procedure and was thought to limit extravasation.11 Also, limiting the operative time can decrease the possibility of extravasation of arthroscopic fluid, which is intuitive since the longer fluid is pumped in a joint the greater risk of extravasation. For instance, in a case report from Bartlett et al.,15 the patient did not develop cardiovascular arrest secondary to abdominal compartment syndrome until after 2 hours into the arthroscopy. Frequent compartment checks, careful control of fluid net flow, and minimizing operative time are useful strategies to limit complications with hip arthroscopy.
Compared with other surgical techniques to remove intra-articular bullet fragments in the hip, such as surgical hip dislocation, arthroscopic studies had lower amounts of blood loss (87 mL compared with 255 mL).2 Also, surgical time was on average 110 minutes long, which is a substantial decrease in the average amount of time other surgical techniques require for removal of bullet fragments. Niroopan16 commented on the overall success rates and complications with arthroscopic procedures in hip trauma. The study showed an overall major complication rate (i.e., pulmonary embolism and abdominal compartment) of 1.4%, compared with our study that has a major complication rate of 12.5%. Although this study showed a greater rate of major complications compared with previous studies, factors such as surgeon training in arthroscopic procedures could have impacted this finding. Previous studies also considered other traumas, which could skew the fact that bullet traumas are may be more functionally exacerbating.
Limitations
This study has potential limitations. The small sample size does not allow for statistical analysis on the data retrieved, which makes data interpretation difficult. The lack of statistical analysis also decreases the clinical impact of the study. However, the cases that were analyzed in this study have valuable information and implications on the future of arthroscopic procedures. Another limitation of the study was the amount of fallout from patients in the study with regards to follow-up, which may skew some of the predicted outcomes from the procedure.
Conclusions
There are risks with the use of arthroscopic methods to remove GSW fragments, which may be greater than elective hip arthroscopy. Certain factors, such as the surgeon’s arthroscopic experience, locations of bullets fragments, visual quality, length of procedure, and concomitant acetabular fractures, must be considered before proceeding with arthroscopy.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Kaya I., Ugras A.A., Saglam N., Sungur I., Cetinus E. Bullet in hip joint. Eurasian J Med. 2013;45:141–142. doi: 10.5152/eajm.2013.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teloken M.A., Schmietd I., Tomlinson D.P. Hip arthroscopy: A unique inferomedial approach to bullet removal. Arthroscopy. 2002;18:1–3. doi: 10.1053/jars.2002.32232. [DOI] [PubMed] [Google Scholar]
- 3.Al-Asiri J., Wong I. Arthroscopic bullet removal from the acetabulum (hip joint) J Surg Tech Case Rep. 2012;4:121–125. doi: 10.4103/2006-8808.110260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Çatma M.F., Ünlü S., Ersan Ö., Öztürk A. Treatment of the bullet, traversing femoral neck, lodged in hip joint: Initial arthroscopic removal and subsequent cartilage repair. J Orthop Case Rep. 2016;6:13–16. doi: 10.13107/jocr.2250-0685.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cory J.W., Ruch D.S. Arthroscopic removal of a 44 caliber bullet from the hip. Arthroscopy. 1998;14:624–626. doi: 10.1016/s0749-8063(98)70061-1. [DOI] [PubMed] [Google Scholar]
- 6.Howse E.A., Rogers J.P., Stone A.V., Mannava S., Allston J., Stubbs A.J. Arthroscopic bullet removal from the central and peripheral compartments of the hip joint. Arthrosc Tech. 2016;5:e217–e221. doi: 10.1016/j.eats.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singleton S.B., Joshi A., Schwartz M.A., Collinge C.A. Arthroscopic bullet removal from the acetabulum. Arthroscopy. 2005;21:360–364. doi: 10.1016/j.arthro.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Meyer N.J., Thiel B., Ninomiya J.T. Retrieval of an intact, intraarticular bullet by hip arthroscopy using the lateral approach. J Orthop Trauma. 2002;16:51–53. doi: 10.1097/00005131-200201000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Goldman A., Minkoff J., Price A., Krinick R. A posterior arthroscopic approach to bullet extraction from the hip. J Orthop Trauma. 1987;27:1294–1300. doi: 10.1097/00005373-198711000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Williams M., Hutcheson R., Miller A. A new technique for removal of intraarticular bullet fragments from the femoral head. Bull Hosp Joint Dis. 1997;56:107–110. [PubMed] [Google Scholar]
- 11.Lee G.H., Virkus W.W., Kapotas J.S. Arthroscopically assisted minimally invasive intraarticular bullet extraction: Technique, indications, and results. J Trauma. 2008;64:512–516. doi: 10.1097/TA.0b013e31814699ee. [DOI] [PubMed] [Google Scholar]
- 12.Tisnovsky I., Katz S.D., Pincay J.I., et al. Management of gunshot wound-related hip injuries: A systematic review of the current literature. J Orthop. 2021;23:100–106. doi: 10.1016/j.jor.2020.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kocher M.S., Frank J.S., Nasreddine A.Y., et al. Intra-abdominal fluid extravasation during hip arthroscopy: A survey of the MAHORN group. Arthroscopy. 2012;28:1654–1660. doi: 10.1016/j.arthro.2012.04.151. [DOI] [PubMed] [Google Scholar]
- 14.Mullis B., Dahners L.E. Hip arthroscopy to remove loose bodies after traumatic dislocation. J Orthop Trauma. 2006;20:22–26. doi: 10.1097/01.bot.0000188038.66582.ed. [DOI] [PubMed] [Google Scholar]
- 15.Bartlett C.S., DiFelice G.S., Buly R.L., et al. Cardiac arrest as a result of intraabdominal extravasation of fluid during arthroscopic removal of a loose body from the hip joint of a patient with an acetabular fracture. J Orthop Trauma. 1998;12:294–299. doi: 10.1097/00005131-199805000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Niroopan G., de Sa D., MacDonald A., Burrow S., Larson C.M., Ayeni O.R. Hip arthroscopy in trauma: a systematic review of indications, efficacy, and complications. Arthroscopy. 2016;32:692–703. doi: 10.1016/j.arthro.2015.12.029. e1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.