Abstract
Background:
The association of acculturation with health among immigrant populations is believed to be mediated, in part, by acculturation-related stress and stress biology.
Objectives:
To review and qualitatively synthesize empirical findings on the relationship of acculturation with stress-related inflammatory and endocrine biomarkers and composite allostatic load (AL) scores.
Methods:
A literature search was performed in the PubMed and PsycInfo databases. Article titles, abstracts or full-texts were screened and checked for match with the search criteria. Studies were eligible if they empirically tested the relationship between acculturation and inflammatory/endocrine stress biomarkers or composite AL scores, and were published in the English language.
Results:
Among the 41 articles identified as relevant and included in this review, the majority were published after 2010, included adult Hispanic U.S.-based populations, used cross-sectional study designs, operationalized acculturation as a unidimensional construct, and varied considerably in the selection of covariates in the analyses. Acculturation was significantly associated with stress biomarkers in 29 studies, but the direction of effects varied across studies. Specifically, acculturation, operationalized as a higher orientation towards the host culture, was associated with inflammatory biomarkers in 10 of 14 studies, with endocrine stress biomarkers in 12 of 20 studies, and with composite AL scores in 7 of 8 studies. Overall, language-based proxy measures of acculturation were related to higher levels of stress-related inflammatory and endocrine biomarkers and to lower levels of AL scores, whereas nativity-, generation status- and length of stay-based proxy measures of acculturation were related to higher levels of inflammatory biomarkers and AL score.
Discussion:
The majority of studies reported associations between measures of acculturation and stress biomarkers, however the directions of effects varied across studies. We suggest this heterogeneity may, in part, be a function of limitations imposed by cross-sectional research designs and unidimensional measures of acculturation measures, and we highlight the need for longitudinal studies and use of multidimensional measures of acculturation to better uncover the biobehavioral mechanisms and pathways linking acculturation with health outcomes.
Keywords: Acculturation, Stress biology, Inflammation, Endocrine, Allostatic load
1. Introduction
In a world that is “on the move”, with societies becoming superdiverse, health disparities in immigrant groups become more prevalent and constitute a current issue in health research and policies (The Lancet Public Health, 2018). The causes of these pronounced health disparities between the migrant and non-migrant population are not well understood. Although numerous pre-migration and transit factors (e.g., adverse living conditions in country of origin, war trauma) may contribute to a higher susceptibility for diseases, the prevailing observation is that health disparities often do not exist at the time of immigration to the host country, but develop over the course of stay in the host country (Cunningham et al., 2008). Thus, in order to understand the manifestation of health disparities, post-migration factors that may contribute to health decline in immigrants and their offspring need to be considered. Numerous studies now propose a pervasive role of acculturation, a construct that captures the sociocultural adaptation to the culture of the host country (Berry, 2006), in predicting a wide array of unfavorable health conditions (Lara et al., 2005). These health conditions mostly encompass non-communicable diseases or health risk factors and mental health problems that are known to manifest more likely under conditions of chronic, accumulated stress experiences. Alterations in the biological response to stress across different physiological systems (e.g., immune, endocrine) are a potential key pathway by which experiences during the acculturation process may become biologically embedded, thereby contributing to the manifestation of health disparities. The aim of this review article is to summarize the existing empirical studies that investigate the link between acculturation and immune or endocrine stress markers and allostatic load. Before presenting the results of our review, we will first provide a rationale for the proposed relationship between acculturation and alterations in biological systems related to stress.
1.1. The concept of acculturation
The concept of acculturation describes the extent of post-migration acquisition of the culture of the host country that may result in loss of heritage culture and social ties, while simultaneously negotiating conflicting aspects between both cultures (Sam, 2006). Culture here encompasses any cultural aspects, such as, for example, language use, dietary habits, beliefs, and others. Earlier approaches regarded acculturation as a unidimensional concept, i.e., individuals either orient themselves towards the heritage or the host culture (Liebkind, 2006). This approach is reflected in proxy measures of acculturation that are widely used in research, such as nativity, citizenship, length of stay, and host language use. This is based on the assumption that individuals born in the host country (so-called 2nd or 3rd generation migrants), have lived longer in the host country, and/or speak the main language of the host country better than they speak the heritage language, are more acculturated (Arends-Toth and Vijver, 2006). However, this approach neglects that individuals also can develop bicultural identities, which is why more recent theories conceptualize acculturation as a bidimensional construct. This means that individuals can position themselves concurrently on a continuum of high vs. low orientation towards the host and heritage culture, resulting in four different acculturation types or strategies: assimilation (i.e., high orientation towards the host culture, low orientation towards the heritage culture), segregation (i.e., low orientation towards the host culture, high orientation towards the heritage culture), integration (i.e., high orientation towards both the host and the heritage culture), and marginalization (i.e., low orientation towards both the host and the heritage culture) (Berry, 2006). Measuring acculturation in accordance with this typology requires adequate assessment, for example, by providing separate subscales to measure host and heritage cultural orientation independently, along the cultural domains language use and preference, media use, cultural or ethnic identity of self, family and friends, and others (e.g., ARSMA scale (Cuellar et al., 1995)). Thus, the different conceptualizations of acculturation are reflected in a variety of measures that are commonly used which will be addressed in the present review.
1.2. A conceptual framework on the link between acculturation and health
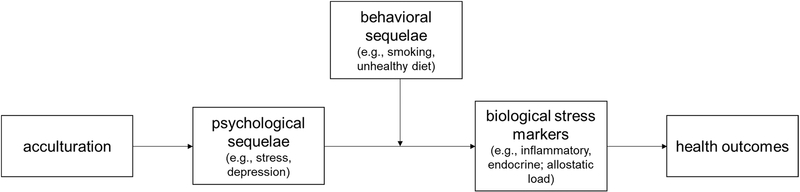
It is a common epidemiologic finding that immigrants are often as healthy or even healthier than the host population upon arrival, and that this advantage diminishes over length of stay in the target country and even across generations (Cunningham et al., 2008). Thus, in recent years, research has focused on the role of acculturation for health, and has elucidated relationships between acculturation and for example higher body mass index (BMI) (Chen et al., 2012; Ruiz et al., 2007), hypertension (Divney et al., 2019), diabetes (Anderson et al., 2016), cardiovascular diseases (Commodore-Mensah et al., 2018), poorer overall physical health (Riosmena et al., 2013), depression (Castillo et al., 2015), and poorer birth outcomes (Lara et al., 2005). The onset and progression of many of these non-communicable diseases is associated with chronic stress exposure (Vanitallie, 2002). At the same time, psychological sequelae of acculturation, including chronic stress experience, have been described and are discussed as key mediators in the link between acculturation and health decline (Finch and Vega, 2003). In the context of acculturation, psychological stress experience may result from discrimination experiences, loss of social ties and social support, negotiation between conflicting aspects of heritage and host culture, or identity conflicts (Berry et al., 1987; Fox et al., 2017a). The effects of acculturation on health via stress experience can be also amplified by behavioral factors (Lara et al., 2005). We propose a conceptual framework which states that acculturation is linked to health via stress experience, and that this link can be moderated by behavioral factors (including unfavorable health behaviors like smoking, substance and alcohol abuse, diet and lack of physical activity, see Fig. 1). Alternatively, both psychological and behavioral alterations could be mediators linking acculturation and health (Fox et al., 2015). However, since the focus of the current review is on acculturation’s effects on stress biology, we center the framework around the mediating role of stress and highlight the role of behavioral changes as important moderating factors that need to be addressed in this context. Alternative biological pathways that result from behavioral changes (e.g., related to nutrition or substance use) are beyond the scope of the current review.
Fig. 1.
Pathways linking acculturation and health.
1.2.1. Acculturation and biological stress response
Based on the consideration that physiological alterations underlie disease risk, the link between acculturation and health-related biological markers is of interest in this context, and given the rationale that acculturation may impair health via chronic stress experience, the role of stress biology is particularly relevant. Our conceptual framework postulates that the sequelae of acculturation become biologically embedded via alterations in stress-related biological systems, thereby increasing the vulnerability to develop mental or physical disorders (Fox et al., 2017a). The above-mentioned stress experiences in the context of acculturation may induce a physiological stress response if they are evaluated as threats through hippocampal, amygdaloid, and prefrontal activation (Herman et al., 2005; McEwen, 2007). This, in turn, will initiate the sympathetic-adrenal-medullary (SAM) axis release of catecholamines and the hypothalamic-pituitary-adrenal (HPA) axis secretion of glucocorticoids. The activation of the SAM can also prompt an acute inflammatory response (Prather et al., 2009; Steptoe et al., 2007) by inducing up-regulation of the transcription factor NF-κB, a key regulator of inflammation, in circulating immune cells (Bierhaus et al., 2003). While adaptive acutely, chronic over-activation of SAM- and HPA-axis products induce a downstream effect on interconnected biological systems (neuroendocrine, immune, metabolic, and cardiovascular) (McEwen, 1998b, 1998a). Prolonged or persistent activation of these systems through chronic stress exposure leads to their dysregulation, contributing to “allostatic load” that represents the cumulative “wear and tear” experienced over time. A large body of evidence shows that chronic stress exposure is associated with a reduced sensitivity of the glucocorticoid receptor (GR), which mediates the HPA axis negative feedback. Because of the increased resistance of the GR that expands to immune cells, the anti-inflammatory properties of cortisol are also reduced, resulting in higher inflammation levels particularly after acute stress exposure (Cohen et al., 2012).
The effects of stress experience on physiological alterations can be moderated by the adverse or beneficial effects of health behaviors, such as dietary practices, sleep quality, physical activity and alcohol, smoking or drug use alterations that are also believed to be a consequence of acculturation (Lara et al., 2005). Such behavioral adjustments are often an attempt to buffer stress experience, but if they are maladaptive, they do not represent effective coping mechanisms and may ultimately increase disease susceptibility (Rodriquez et al., 2017). For example, smoking is related to higher cortisol secretion (Cohen et al., 2019), and unhealthy diet and sedentary behavior may result in overweight which is associated with higher pro-inflammatory status (Visser et al., 1999).
Finally, chronic alterations in stress-responsive biological systems may enhance the susceptibility to adverse health outcomes. Research indicates strong associations between stress biological markers and numerous medical risk factors, non-communicable diseases and mental disorders (Djuric et al., 2008), including those that often show high prevalence in immigrant groups as a function of acculturation (Lara et al., 2005; Rosenthal, 2018).
1.2.2. Objectives
It has been proposed that the strong link between acculturation and health decline in different immigrant groups emerges via alterations in biological pathways related to stress regulation. Until now, several studies have investigated the relationship between acculturation and biological stress markers, but to our knowledge, these studies have not yet been systematically reviewed and summarized. The aim of our review was thus to identify and synthesize existing empirical studies that investigate the relationship between acculturation and biological stress markers. We focus here on inflammatory and endocrine stress markers and allostatic load because these are robust antecedents and/or correlates of the health disparities that are often found in immigrant groups. We expected that acculturation levels will be positively related to levels of inflammatory and endocrine markers and allostatic load scores. Given the considerable heterogeneity in stress biomarkers, especially the endocrine markers, we specify hypotheses in greater detail (below) in the Results section. Another aim is to outline and discuss methodological challenges in the research on acculturation and stress biological markers, focusing on study designs and conceptualization of acculturation.
The questions that guided our review were the following:
What are the characteristics of the studies in terms of study design (e.g., cross-sectional, longitudinal), study samples (e.g., ethnicity, age groups), conceptualization of acculturation (i.e., unidimensional vs. bidimensional measures) and selection of covariates in the analyses?
Is acculturation linked to stress biomarkers across different studies in the expected directions?
Does the link between acculturation and stress biomarkers vary as a function of study design, sample, acculturation measure, or outcome measure?
2. Methods
This systematic review mostly follows the guidelines of the “Preferred Reporting Items for Systematic and Meta-analysis protocol for scoping reviews” (PRISMA-ScR) (Tricco et al., 2018).
2.1. Data sources and searches
The search strategy targeted studies that assessed the relationship of acculturation with immune markers, endocrine markers, and allostatic load (AL) scores. Articles were searched in the databases PubMed and PsycInfo that were published until November 30th, 2020 when the literature search was conducted. Search terms included “acculturation” combined with terms related to immune and endocrine stress markers and allostatic load scores: “inflammation”, “inflammatory marker”, ”inflammatory state”, “cytokines”, “c-reactive protein”, “CRP”, “interleukin”, “IL-1β”, “IL-2”, “IL-4”, “IL-6”, “IL-8”, “IL-10”, “e-selectin”, “fibrinogen”, “TNF-α“, “alpha-amylase”, “cortisol”, “corticotropin-releasing hormone”, “CRH”, “ACTH”, “hypothalamic pituitary adrenal axis”, “hpa-axis”, “endocrine system”, “adrenaline”, “epinephrine”, “nor-adrenaline”, “nor-epinephrine”, “catecholamines”, “stress biology”, “biological stress response”, and “allostatic load”.
2.2. Eligibility criteria and study selection
The goal was to select empirical articles that test the relationship between acculturation and immune/inflammatory or endocrine stress markers and AL scores. The selection criteria were: (a) empirically testing the relationship between acculturation – either assessed with proxy measures, index scores, or validated scales – and immune/inflammatory stress markers, endocrine stress markers, or AL scores, and (b) study published in English language. Studies were considered as eligible independent of study design, publication year, participants’ age group, ethnicity, or country of residence. Studies were excluded if they 1) did not include analyses on the relationship between acculturation and immune/inflammatory or endocrine stress markers or AL score, 2) were review articles, dissertations, conceptual papers, abstracts only etc., or 3) samples comprised indigenous groups as the focus is here primarily on groups that underwent between-nation migration.
2.3. Data extraction and quality assessment
One author (LS) conducted the search of articles, removed duplicates and screened titles and abstracts of the articles followed by a full-text review to check inclusion criteria. Each item and extracted data was double checked by the same person. If questions arose regarding eligibility of a study, this was discussed with the other coauthors. From each of the selected articles we extracted the study design, sample characteristics (sample size, participants’ stage of life, country of origin, country of residence, gender), acculturation measures, stress biomarkers, covariates in the analyses, and the finding on the relationship between acculturation and stress biomarkers.
3. Results
The search was conducted in PubMed and PsycInfo, yielding 653 matches (see Fig. 1). After removal of 222 duplicates, 431 entries remained. 390 articles were excluded, of which 360 were removed after initial screening of descriptors (i.e., title, abstract, key words) and another 30 articles were removed after full-text screening. 41 articles were identified that met the search criteria.
3.1. Characteristics of included studies
Table 1 presents descriptive statistics of the selected articles. It should be noted that many studies included several acculturation measures and/or different stress biomarkers, which is why they reported more relationships that partly differ in their direction. Table 1 therefore presents the number of studies per category and how many of the studies reported at least one significant relationship between acculturation and stress biomarker. In addition, the table shows how many analyses within the various studies reported a positive, negative, or no association. The number of analyses is thus greater than the number of studies. Table 2 provides detailed information for each of the selected articles.
Table 1.
Descriptive characteristics of included articles (N = 41).
| Immune | Endocrine | AL | |
|---|---|---|---|
|
| |||
| Total N | 24,159 | 4786 | 27,433 |
| Number of studies | 14 [10; 13↑, 2↓, 19←] | 20 [12; 7↑, 9↓, 34←] | 8 [7; 12↑, 5↓, 7←] |
| Stress biomarker | |||
| Pro-inflammatory markers | |||
| CRP | 11 [7; 8↑, 1↓, 10←] | – | – |
| IL-6 | 3 [1; 1↑, 0↓, 4←] | – | – |
| sTNFR2 | 1 [1; 0↑, 1↓, 1←] | – | – |
| Anti-inflammatory markers | |||
| IL-10 | 1 [0; 0↑, 0↓, 3←] | – | – |
| IL-1RA | 2 [2; 4↑, 0↓, 0←] | – | – |
| Epinephrine | 2 [1; 1↑, 0↓, 4←] | ||
| Norepinephrine | 2 [1; 1↑, 0↓, 4←] | ||
| CRH | – | 1 [1; 1↑, 0↓, 0←] | – |
| Estriol-progesterone ratio | – | 1 [1; 1↑, 0↓, 0←] | – |
| Parathyroid hormone | – | 1 [0; 0↑, 0↓, 1←] | – |
| Cortisol | 15 [9; 3↑, 9↓, 25←] | ||
| from blood | – | 1 [1; 0↑, 1↓, 0←] | – |
| from hair | 1 [0; 0↑, 0↓, 3←] | ||
| salivary, single or averaged | – | 3 [1; 0↑, 1↓, 8←] | – |
| salivary, CAR | – | 4 [4; 2↑, 4↓, 2←] | – |
| salivary, diurnal slope | – | 2 [1; 0↑, 1↓, 4←] | – |
| salivary, diurnal AUC | – | 3 [1; 1↑, 1↓, 2←] | – |
| salivary, reactivity during TSST | – | 3 [1; 0↑, 1↓, 6←] | – |
| AL immune, endocrine, cardiovascular, metabolic | – | – | 3 [2; 3↑, 1↓, 5←] |
| AL immune, cardiovascular, metabolic | – | – | 4 [4; 9↑, 3↓, 2←] |
| AL endocrine, cardiovascular, metabolic | – | – | 1 [1; 0↑, 1↓, 0←] |
| Acculturation measure | |||
| Host cultural orientation | |||
| Proxy measures | |||
| Language | 4 [3; 3↑, 0↓, 2←] | 5 [4; 2↑, 2↓, 2←] | 7 [3; 0↑; 3↓, 4←] |
| Age at arrival | 1 [0; 0↑, 0↓, 1←] | 0 | 3 [2; 2↑, 0↓, 1←] |
| Nativity / generation status | 2 [1; 1↑, 0↓, 3←] | 5 [0; 0↑, 0↓, 6←] | 4 [4; 4↑, 0↓, 0←] |
| Length of stay in host country | 8 [6; 6↑, 1↓, 4←] | 2 [1; 1↑, 0↓, 1←] | 4 [4; 4↑, 0↓, 0←] |
| Host lifestyle identification | 0 | 1 [0; 0↑, 0↓, 2←] | 0 |
| Scores | |||
| Index score or latent variable of proxies | 2 [1; 1↑, 0↓, 1←] | 1 [1; 1↑, 0↓, 0←] | 0 |
| Host diet | 2 [1; 1↑, 0↓, 2←] | 0 | 0 |
| Individualistic/independent self-construal | 0 | 2 [1; 1↑, 1↓, 1←] | 0 |
| Host cultural orientation scorea | 1 [1; 0↑, 1↓, 1←] | 3 [0; 0↑, 0↓, 5←] | 0 |
| Heritage cultural orientation | |||
| Proxy measures | |||
| Length of stay in heritage country | 0 | 1 [0; 0↑, 0↓, 1←] | 0 |
| Heritage lifestyle identification | 0 | 1 [0; 0↑, 0↑, 2←] | 0 |
| Scores | |||
| Heritage cultural orientation scoreb | 0 | 2 [0; 0↑, 0↓, 4←] | 0 |
| Heritage diet | 2 [0; 0↑, 0↓, 3←] | 0 | 0 |
| Collectivistic/interdependent self-construal | 0 | 2 [1; 1↑, 0↓, 1←] | 0 |
| Composite acculturation score (unidimensional)c | 1 [1; 1↑, 0↓, 0←] | 5 [3; 1↑, 3↓, 5←] | 0 |
| Interaction host X heritage cultural (bidimensional) | 0 | 2 [2; 2↑, 0↓, 0←] | 0 |
| Measure not specified | 0 | 1 [0; 0↑, 0↓, 1←] | 0 |
| Publication year | |||
| <2006 | 0 | 1 [1; 2↑, 0↓, 4←] | 0 |
| 2006–2010 | 2 [2; 2↑, 0↓, 1←] | 2 [2; 1↑, 1↓, 0←] | 1 [1; 3↑, 0↓, 3←] |
| 2011–2015 | 4 [3; 5↑, 2↓, 9←] | 8 [6; 2↑, 5↓, 12←] | 4 [3; 2↑, 2↓, 3←] |
| 2016–2020 | 8 [5; 6↑, 0↓, 9←] | 9 [3; 2↑, 3↓, 18←] | 3 [3; 7↑, 3↓, 1←] |
| Study design | |||
| Cross-sectional | 12 [9; 12↑, 2↓, 15←] | 16 [10; 7↑, 7↓, 25←] | 8 [7; 12↑, 5↓, 7←] |
| Laboratory stress paradigm | 0 | 3 [1; 0↑, 1↓, 6←] | 0 |
| Prospective | 1 [1; 1↑, 0↓, 0←] | 1 [1; 0↑, 1↓, 3←] | 0 |
| Randomized trial | 1 [0; 0↑, 0↓, 4←] | 0 | 0 |
| Ethnicity | |||
| Hispanics/Latinos | 11 [7; 10↑, 0↓, 17←] | 12 [9; 2↑, 7↓, 18←] | 7 [6; 10↑, 5↓, 7←] |
| Asian | 2 [2; 2↑, 2↓, 2←] | 5 [2; 4↑, 1↓, 13←] | 0 |
| Blacks | 0 | 0 | 1 [1; 2↑, 0↓, 0←] |
| Other | 1 [1; 1↑, 0↓, 0←] | 3 [1; 1↑, 1↓, 3←] | 0 |
| Country of residence | |||
| US | 13 [9; 12↑, 2↓, 19←] | 19 [12; 7↑, 9↓, 33←] | 8 [7; 12↑, 5↓, 7←] |
| Canada | 1 [1; 1↑, 0↓, 0←] | 0 | 0 |
| Australia | 0 | 1 [0, 0↑, 0↓, 1←] | 0 |
| Age group | |||
| Childhood | 1 [0; 0↑, 0↓, 1←] | 1 [1; 0↑, 1↓, 0←] | 0 |
| Adolescence | 0 | 4 [2; 0↑, 2↓, 5←] | 0 |
| Adulthood | 10 [7; 8↑, 2↓, 12←] | 11 [5; 5↑, 4↓, 26←] | 8 [7; 12↑, 5↓, 7←] |
| Pregnancy | 3 [3; 5↑, 0↓, 6←] | 4 [4; 2↑, 2↓, 3←] | 0 |
| Nativity | |||
| Foreign- or native-born | 7 [5; 8↑, 0↓, 12←] | 16 [8; 4↑, 6↓, 30←] | 6 [5; 10↑, 4↓, 6←] |
| Foreign-born | 5 [4; 4↑, 2↓, 5←] | 2 [2; 3↑, 1↓, 4←] | 1 [1; 2↑, 0↓, 1←) |
| Native-born | 1 [1; 1↑, 0↓, 1←] | 0 | 0 |
| Unclear | 1 [0; 0↑, 0↓, 1←] | 2 [2; 0↑, 2↓, 0←] | 1 [1; 0↑, 1↓, 0←] |
| Sex | |||
| Women and men | 8 [6; 7↑, 0↓, 7←] | 12 [7; 3↑, 7↓, 16←] | 8 [7; 12↑, 5↓, 7←] |
| Women only | 6 [4; 6↑, 2↓, 12←] | 7 [5; 4↑, 2↓, 17←] | 0 |
| Men only | 0 | 1 [0; 0↑, 0↓, 1←] | 0 |
| Covariates | |||
| Socioeconomic factors (education, income, etc.) | 6 [5; 6↑, 0↓, 5←] | 5 [3; 1↑, 3↓, 8←] | 5 [4; 10↑, 3↓, 6←] |
| Demographic and biophysical factors (age, sex, BMI, etc.) | 12 [9; 10↑, 2↓, 12←] | 11 [7; 1↑, 7↓, 16←] | 5 [4; 10↑, 3↓, 6←] |
| Medical conditions (medication, diseases, etc.) | 3 [3; 3↑, 0↓, 2←] | 4 [2; 1↑, 1↓, 8←] | 0 |
| Psychological conditions (stress, depression, etc.) | 4 [4; 4↑, 2↓, 1←] | 10 [7; 4↑, 5↓, 13←] | 2 [1; 2↑, 3↓, 2←] |
| Behavioral factors (diet, physical activity, smoking, etc.) | 3 [2; 2↑, 0↓, 6←] | 4 [2; 1↑, 2↓, 8←] | 4 [3; 7↑, 3↓, 5←] |
| Other | 4 [2; 2↑, 0↓, 5←] | 5 [4; 3↑, 4↓, 3←] | 0 |
| Unadjusted | 2 [1; 3↑, 0↓, 7←] | 6 [2; 2↑, 1↓, 17←] | 3 [3; 2↑, 2↓, 1←] |
Note. Read as: Number of studies per category [number of studies showing at least one significant association between acculturation and stress biomarker; number of analyses showing a positive association ↑, number of analyses showing a negative association ↑, number of analyses showing no association ←]. The sum of the numbers next to the arrows equals the total number of analyses in this category. Acculturation measures that were included in single studies but not presented here are social acculturation, ethnic identity, interaction with mainstream society, importance of preserving Mexican culture, site of residence, environmental mastery, Mexican American Cultural Values Scale.
(ARSMA-II, BARSMA–II, VIA, GEQ-A
ARSMA-II, BARSMA–II, VIA
ARSMA, ARSMA-II, SL-ASIA, SASH.
The table refers to the study by Cedillo et al. (2020) in both the immune and AL score section.
Table 2.
Empirical studies on acculturation and stress biomarkers.
| # | Author, year | Study design | Sample | Measure of acculturation | Outcome | Covariates | Result |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Immune/inflammatory markers | |||||||
| 1 | (Ablow Measelle et al., 2019) | Cross-sectional | N = 129 adults From Mexico Living in the U.S. Foreign-born Women and men |
Unidimensional: Length of stay Age at arrival Language acculturation Site of residence |
CRP from blood | Income, age, BMI, income-to-poverty ratio X English language orientation | ← ← ← Language orientation, length of stay and site of residence were not related to CRP. ← Age at arrival positively correlated with CRP but was not a significant predictor in regression models. In men, but not women, greater English language orientation in conjunction with higher income were related to higher CRP levels. |
| 2 | (Fang et al., 2014) | Cross-sectional | N = 407 adults From China Living in the U.S. Foreign-born Women |
Unidimensional: Length of stay GEQ-A |
CRP, sTNFR2 from blood | Age, BMI, positive life events, negative life events, acculturative stress | ↑ ↓ Longer length of stay was related to significantly higher CRP concentrations and to lower concentrations of sTNFR2. ↓ ← Higher GEQ-A scores were related to significantly lower concentrations of CRP, but were unrelated to sTNFR2. |
| 3 | (Gouin and MacNeil, 2019) | Cross-sectional | N = 58 adults From different countries Living in Canada Foreign-born Women and men |
Unidimensional: Length of stay |
CRP from blood | Education, age, sex, BMI, geographical region of origin, attachment anxiety, attachment avoidance, relationship satisfaction, attachment anxiety X length of stay, attachment avoidance X length of stay, relationship satisfaction X length of stay | ↑ Longer length of stay was related to significantly higher CRP concentrations. The interaction between length of stay and attachment anxiety was significantly positive. |
| 4 | (Kannan et al., 2013) | Cross-sectional | N = 143 children Puerto Rican Living in the U.S. Nativity not reported Boys and girls |
Unidimensional: Maternal place of birth (∼generation status) |
CRP from blood | Child’s gender, day care attendance | ← Maternal place of birth was unrelated to children’s levels of CRP. |
| 5 | (Lommel et al., 2019) | Cross-sectional | N = 592 adults From Mexico Living in the U.S. Foreign-born Women and men |
Unidimensional: Index of proxy measures (proportion of life residing in the U.S., language acculturation) |
CRP from blood | Age, gender, self-rated health, depressive symptoms | ↑ Higher acculturation index was related to significantly higher CRP concentrations. |
| 6 | (Pierce et al., 2007) | Cross-sectional | N = 496 adults From Japan Living in the U.S. Native-born (2nd and 3rd generation) Women and men |
Unidimensional: Dietary acculturation |
CRP from blood | Age, sex, oral contraceptive use, diabetes, hypertension, history of myocardial infarction or coronary artery disease, hormone replacement therapy, food factor scores, smoking | ↑ The Western food factor score was related to higher CRP concentrations in 3rd, but not in 2nd generation individuals. ← The Japanese food factor was not associated with CRP. |
| 7 | (Rodriguez et al., 2012) | Cross-sectional | N = 11,858 adults Hispanics Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: Length of stay Language acculturation |
CRP from blood | Education, insurance, age, gender, BMI, cholesterol, hypertension, diabetes mellitus, statin use, smoking, usual place of care | ← Length of stay was unrelated to CRP. ↑ Language acculturation was associated with higher CRP levels. |
| 8 | (Rosenberg et al., 2017) | Cross-sectional | N = 1002 adults From Mexico Living in the U.S. Foreign- or native-born Women |
Unidimensional: Index of proxy measures (nativity, length of stay, language acculturation) |
CRP from blood | Unadjusted | ← The acculturation index was not related to the probability to have CRP concentrations > 3.0 mg/L. |
| 9 | (Ruiz et al., 2007) | Cross-sectional | N = 206 pregnant women Hispanics Living in the U.S. Foreign- or native-born |
Unidimensional: Length of stay |
IL-1RA from blood | Pre-pregnancy BMI, depressive symptoms | ↑ Longer time in U.S. was associated with higher IL-1RA concentrations. |
| 10 | (Santiago-Torres et al., 2016) | Randomized trial of dietary intervention | N = 53 adults From Mexico Living in the U.S. Foreign- or native-born Women |
Unidimensional: random assignment to a Mexican vs. US diet for 24 days |
CRP, IL-6 from blood | Age, BMI, diet sequence, feeding period, baseline and washout biomarker concentrations | ← ← ← ← US and Mexican diet were not associated with concentrations of CRP and IL-6. |
| 11 | (Scholaske et al., 2018) | Prospective | N = 75 pregnant women From Mexico Living in the U.S. Foreign- or native-born |
Unidimensional: ARSMA | IL-6 from blood | Income, pregnancy BMI, obstetric risks, gestational week at assessment | ↑ Higher ARSMA score was related to higher IL-6 concentrations across pregnancy. |
| 12 | (Steffen et al., 2016) | Cross-sectional | N = 310 adults From Mexico Living in the U.S. Foreign-born Women and men |
Unidimensional: Length of stay |
CRP from blood | Financial strain, sex, BMI, length of stay X financial strain | ↑ Longer stay in the US was related to higher CRP levels. This relationship remained significant after controlling for sex, but became insignificant when controlling for BMI. There was no interaction effect of acculturation and financial strain in predicting CRP. |
| 13 | (Wommack et al., 2013) | Cross-sectional | N = 470 pregnant women Hispanics Living in the U.S. Foreign- or native-born |
Unidimensional: Nativity Length of stay Language acculturation |
IL-1RA (anti-inflammatory), IL-10 (anti-inflammatory), IL-6 from blood | Unadjusted | ↑ ↑ ↑ Longer length of stay in US, high English proficiency and being born in U.S. were related to higher likelihood to have IL-1RA concentrations above median. ← ← ← ← ← ← Acculturation measures were unrelated to IL-6 and IL-10 concentrations. |
| Endocrine markers | |||||||
| 14 | (Brown and James, 2000) | Cross-sectional | N = 31 adults from the Philippines Living in the U.S. Foreign-born Women |
Unidimensional: Length of stay Filipino and American lifestyle identification |
Urinary catecholamines (epinephrine, norepinephrine) in different settings | Unadjusted | ↑ ↑ Longer stay in the U.S. significantly positively correlated with norepinephrine levels at work and home, but not during sleep, and with epinephrine levels at work, but not at home and during sleep. ← ← ← ← Filipino and American lifestyle identification did not correlate with epinephrine and norepinephrine at work, home and during sleep. |
| 15 | (Burt et al., 2018) | Cross-sectional | N = 316 adults (students) From Asia Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: Nativity individualistic and collectivistic self-construal |
Salivary cortisol (CAR) | Feeling happy/excited at waking on second day of saliva collection (in 1st generation females), time of first saliva collection on first day of measurements (in 2nd generation males) | ← CAR did not significantly differ between 1st and 2nd generation (unadjusted). ↓ ↑ Higher individualistic self-construal was related to attenuated CAR in 1st generation men and women and to higher CAR in 2nd generation men, but not in women. ↑ Higher collectivistic self-construal was related to higher CAR in 1st generation, but not in 2nd generation. |
| 16 | (D’Anna et al., 2012) | Prospective | N = 55 pregnant women From Mexico Living in the U.S. Foreign- or native-born |
Unidimensional: SASH (composite score) |
Salivary cortisol (diurnal slope at different pre- and postpartum time points) | Maternal age | ↓ ← ← ← A higher SASH score (i.e., a higher orientation towards the American than Mexican culture) was associated with a flatter diurnal cortisol slope in late pregnancy, but not in early or mid pregnancy or during the postpartum period. |
| 17 | (Gonzales et al., 2018) | Experimental | N = 264 adolescents From Mexico Living in the U.S. Nativity not reported Girls and boys |
Bidimensional: BARSMA-II (Anglo and Mexican Orientation Scales) |
Salivary cortisol reactivity during Trier Social Stress Test (TSST) | Sex | ↓ A high orientation towards the American culture combined with a low orientation towards Mexican culture was associated with the flattest cortisol reactivity to the TSST with lower peak. (↑) Biculturalism (i.e., interaction term between host and heritage cultural orientation) was associated with a steeper increase in cortisol reactivity and higher cortisol peak during the TSST. |
| 18 | (Jimenez et al., 2012) | Cross-sectional | N = 301 adults From Mexico Living in the U.S. Foreign- or native-born Women |
Unidimensional: Nativity Language acculturation |
Urinary catecholamines (epinephrine, norepinephrine) | SES (composite of education and income), SES X nativity, SES X language, BMI, menopausal status, medications for thyroid disorders, depressive symptoms, physical activity, smoking, sleep quality | ← ← ← ← Language preference and nativity were not associated with epinephrine and norepinephrine. There was a significant interaction between language and SES, indicating that high language acculturation in conjunction with high SES predicted higher epinephrine and nor-epinephrine. |
| 19 | (Mangold et al., 2012) | Cross-sectional | N = 59 adults From Mexico Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: ARSMA-II (composite score) Generation status |
Salivary cortisol (CAR) | Age, gender, neuroticism, clinical depression, childhood trauma, sampling time, ARSMA X neuroticism, ARSMA X neuroticism X time | ↓ Participants with higher ARSMA scores had an attenuated CAR. ← Generation status was not significantly associated with CAR. There was a significant interaction between acculturation and neuroticism and between acculturation, neuroticism and time. Participants with a great Anglo orientation in conjunction with high neuroticism levels had an attenuated CAR, while participants with a great Mexican orientation and low neuroticism had a healthy robust CAR. |
| 20 | (Mangold et al., 2010) | Cross-sectional | N = 59 adults From Mexico Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: ARSMA-II (composite score) |
Salivary cortisol (CAR) | Age, gender, early trauma exposure, sampling time, ARSMA X trauma exposure, ARSMA X trauma exposure X time | ↓ Participants with higher ARSMA scores had an attenuated CAR. Participants with low ARSMA score and low trauma exposure had a healthy robust CAR, whereas a high ARSMA score in conjunction with trauma exposure was associated to an attenuated CAR. |
| 21 | (Mendoza et al., 2017) | Cross-sectional | N = 71 children Hispanics Living in the U.S. Nativity not reported Girls and boys |
Unidimensional: Language acculturation |
Salivary cortisol (averaged across collection time points) | Poverty level, economic hardship, age, sex, immigration stress, economic hardship X immigration stress, acculturation X economic hardship | ↓ Higher acculturation was marginally significantly related to lower cortisol levels. There was a significant interaction between acculturation and economic hardship, indicating that low economic hardship in conjunction with low acculturation levels was related to higher cortisol concentrations. |
| 22 | (Nabipour et al., 2011) | Cross-sectional | N = 1705 adults From different countries Living in Australia Foreign- or native-born Men |
Unidimensional: Nativity |
Parathyroid hormone from blood | Unadjusted | ← There was no difference in parathyroid hormone levels between Australian-born and foreign-born participants. |
| 23 | (Nicholson et al., 2013) | Cross-sectional | N = 137 adults From the former Soviet Union Living in the U.S. Foreign-born Women and men |
Unidimensional: Language acculturation Environmental mastery |
Salivary cortisol (diurnal AUC) | Education, employment status, age, smoking, length of stay | ↑ Language mastery predicted higher AUC in women, but not in men. ↓ Environmental mastery predicted lower AUC in men, but not in women. |
| 24 | (Qu et al., 2020) | Cross-sectional | N = 95 adolescents and one biological parent From China Living in the U.S. Foreign- or native-born Girls and boys |
Unidimensional: ARSMA-II adapted for Chinese Americans (composite score) |
Salivary cortisol (diurnal AUC) | Family income, child sex, child birthplace, study week, ARSMA X school problems | ← Adolescents’ and parents’ ARSMA score was not significantly related to adolescents’ daily cortisol AUC (unadjusted). The significant interaction between adolescents’ ARSMA score and school problems indicated that adolescents had higher cortisol AUC on days when they experienced more school problems when they were more oriented towards the Chinese than adolescents that were more oriented towards the US culture. |
| 25 | (Ruiz et al., 2006) | Cross-sectional | N = 106 pregnant women Hispanic Living in the U.S. Foreign- or native-born |
Unidimensional: Language acculturation |
CRH from blood | Gestational age at birth, biobehavioral risk, perceived stress (path model) | ↑ English acculturation was related to higher CRH concentrations at 22–25 weeks of gestation via perceived stress in a path model. |
| 26 | (Ruiz et al., 2012) | Cross-sectional | N = 470 pregnant women Hispanics Living in the U.S. Foreign- or native-born |
Unidimensional: Latent variable of generation status, length of stay, language acculturation |
Estriol, progesterone from blood | History of preterm birth, preterm birth, depressive symptoms, depressive symptoms X EP-ratio, preeclampsia (structural equation model) | ↑ In structural equation model, acculturation as a latent variable (generation status, length of stay, English proficiency) predicted significantly higher estriol-to-progesterone ratio. |
| 27 | (Ruiz et al., 2013) | Cross-sectional | N = 470 pregnant women From Mexico Living in the U.S. Foreign- or native-born |
Bidimensional: Language acculturation |
Cortisol from blood | Unadjusted | ↓ Participants with high English proficiency had significantly lower mean cortisol concentrations compared to participants with high Spanish proficiency and than participants who scored in the bilingual category. (↑) Vice versa, bilingual participants had higher cortisol concentrations than participants with high English proficiency. They also had lower cortisol concentrations than participants with high Spanish proficiency, but this difference was not tested for significance. |
| 28 | (Torres et al., 2018) | Cross-sectional | N = 18 adults Hispanics Living in the U.S. Foreign- or native-born Women |
Unidimensional: BARSMA–II (Anglo and Mexican Orientation Scales) |
Salivary cortisol (waking, 30 min post-waking, bedtime) | Unadjusted | ← ← ← ← ← ← Host and heritage cultural orientation scores did not significantly correlate with cortisol at waking, 30 min post-waking, and bedtime. |
| 29 | (Wang and Lau, 2018) | Experimental | N = 133 adults Euro Americans, Asian Americans Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: VIA (host and heritage culturation orientation scores) Independent and interdependent self-construal |
Salivary cortisol reactivity during TSST | Unadjusted | ← ← ← ← Host and heritage cultural orientation scores and independent and interdependent self-construal were not significantly correlated with cortisol reactivity during TSST in Euro or Asian Americans. |
| 30 | (Wu et al., 2019) | Cross-sectional | N = 166 adults Asian Living in the U.S. Foreign- or native born Women and men |
Unidimensional: Length of stay in host and heritage country SL-Asia (composite score) |
Hair cortisol | Age, BMI, perceived stress, perceived racism, weight stigma, weight stigma X acculturation | ← ← Longer stay in the U.S. and in Asia were each related to lower levels of cortisol, but this relationship became insignificant after removing n = 6 outliers from the sample. ← SL-Asia score was unrelated to cortisol levels. |
| 31 | (Yim et al., 2019) | Experimental | N = 127 adults Different ethnicities Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: Nativity ARSMA-II (Anglo Orientation Subscale) |
Salivary cortisol reactivity during TSST | Unadjusted | ← ← Cortisol reactivity during TSST did not differ between foreign- and native-born Latinos and did not correlate with the Anglo Orientation Subscale in the overall sample or in subgroups (foreign-born, native-born, Latino, non-Latino). |
| 32 | (Zeiders et al., 2012) | Cross-sectional | N = 100 adolescents From Mexico Living in the U.S. Foreign- or native-born Girls and boys |
Unidimensional: Mexican American Cultural Values Scale |
Salivary cortisol (CAR, AUC, waking, bedtime) | Family income, gender, oral contraceptives, life stressors, depression symptoms, daily stress level, discrimination, physical activity, caffeine use, daily wake time, daily hours of sleep | ↓ ← ← ← Higher acculturation was marginally significantly related to a blunted CAR, and was unrelated to cortisol AUC, waking and bedtime cortisol levels. |
| 33 | (Zeiders et al., 2018) | Cross-sectional | N = 103 adolescents From Mexico Living in the U.S. Foreign- or native-born Girls and boys |
Not stated | Salivary cortisol (diurnal slopes) | Gender, medication level, ethnic-racial identity components (exploration, resolution, affirmation), life stressors, ethnic-racial discrimination, physical activity, caffeine use, daily hours of sleep | ← Acculturation was not related to cortisol diurnal slopes. |
| Allostatic load scores | |||||||
| 34 | (Arevalo et al., 2014) | Cross-sectional | N = 984 adults From Puerto Rico Living in the U.S. Foreign- or native-born Women and Men |
Unidimensional: Age at arrival Language acculturation |
Immune (CRP), endocrine (DHEA-S, cortisol, epinephrine, norepinephrine), cardiovascular (SBP, DBP), metabolic (TC, HDL-C, HbA1c, WC) | Education, age, sex, 2-year trajectories of stressful life events, stressful life events X age at arrival, smoking, alcohol use, baseline allostatic load | ← ← Language proficiency and age at arrival were not associated with AL. Moderate stressful life events in conjunction with 6–11 years at arrival predicted higher AL compared to low stress and 5 years of age at arrival. |
| 35 | (Cedillo et al., 2020) | Cross-sectional | N = 8360 adults Hispanics Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: Nativity Length of stay Age at arrival Language acculturation |
Immune (CRP), cardiovascular (SBP, DBP, 60-s pulse), metabolic (TC, HDL-C, creatinine clearance, serum albumin) | Education, income, marital status, age, sex, - Education, income, sex |
↑ Allostatic load was higher in U.S.-born compared to foreign-born Hispanics (unadjusted). ↑ ↑ ← In foreign-born Hispanics, length of residence and age at arrival, but not language use, were associated with higher allostatic load index after adjustment for covariates. These relationships were more pronounced for men compared to women in an unadjusted ANOVA. - ↑ ↑ Longer stay in the U.S. was significantly and language use marginally significantly related to higher CRP concentrations. |
| 36 | (Doamekpor and Dinwiddie, 2020) | Cross-sectional | N = 2897 adults Blacks Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: Nativity Length of stay |
Immune (CRP), cardiovascular (SBP, DBP, 60-s pulse), metabolic (TC, HDL-C, creatinine clearance, serum albumin) | Education, income, marital status, age, gender, smoking | ↑ U.S.-born Blacks had higher allostatic load than foreign-born Blacks. ↑ Among foreign-born Blacks, longer time in the U.S. was related to higher AL score. |
| 37 | (Mattei et al., 2011) | Cross-sectional | N = 1117 adults From Puerto-Rico Living in the U.S. Nativity not reported Women and men |
Unidimensional: Language acculturation |
Endocrine (DHEA-S, cortisol, epinephrine, norepinephrine), cardiovascular (SBP, DBP), metabolic (TC, HDL-C, HbA1c, WC) | Unadjusted | ↓ Higher acculturation was related to significantly lower AL score. |
| 38 | (McClure et al., 2015) | Cross-sectional | N = 126 adults From Mexico Living in the U.S. Foreign-born Women and men |
Unidimensional: Length of stay Age at arrival Language acculturation |
Immune (CRP), cardiovascular (SBP, DBP), metabolic (TC, fasting glucose, WC) | Unadjusted | ↑ In women, but not in men, longer stay in the U.S. was related to significantly higher AL score. ↑ Older age at arrival was related to significantly higher AL score in women and men. ← English language orientation was not related to AL score. |
| 39 | (Niño and Hearne, 2020) | Cross-sectional | N = 11,841 adults Hispanics Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: Generation status Language acculturation Social acculturation Ethnic identity |
Immune (CRP, white blood count), cardiovascular (SBP, resting heart rate, lung function), metabolic (HDL-C, LDL-C, triglycerides, fasting glucose, HbA1c, HOMA index of insulin resistance, BMI, WHR, urine microalbumin, creatinine) | education, income, employment status, relationship status, insurance, age, age2, depressive symptoms, physical activity, generation status X language acculturation, generation status X social acculturation, generation status X ethnic identity | ↑ US-born participants had higher AL scores than 1st generation immigrants, and this difference was significant for Dominican women, Puerto Rican women and men, and marginally significant for Central/South American and Cuban men and Mexican women. ↓ Language acculturation was related so significantly lower AL score in Central/South American men and Puerto Rican women. ↓ Social acculturation was linked to significantly lower AL score in Dominican men and Cuban women. ↓↑ Ethnic identity was related to significantly lower AL score in Dominican men, and to higher AL score in Central/South American men. |
| 40 | (Peek et al., 2010) | Cross-sectional | N = 733 adults From Mexico / Hispanics Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: Nativity Length of stay Language acculturation Childhood and adulthood interaction with mainstream culture Importance of preserving Mexican culture |
Immune (CRP, IL-6, IL-10, TNF-α), endocrine (cortisol), cardiovascular (SBP, DBP), metabolic (HDL-C, TC to HDL-C ratio, triglycerides, HbA1c, BMI) | Education, income, insurance, age, physical activity, smoking | ↑ Being born in the U.S. was related to significantly higher AL score categories. ↑ Longer stay in the U.S. (>10 years) had a stronger association with a higher AL score than shorter stay in the U.S. (<=10 years). ↑ Foreign-born Mexicans who had lived in the US for more than 10 years had higher risk for higher AL categories than foreign-born Mexicans that lived in the US for 10 years or less. ← ← ← Interaction with mainstream society both as an adult and as a child, the importance of preserving Mexican culture, and English-language use were unrelated with AL score. |
| 41 | (Todorova et al., 2013) | Cross-sectional | N = 1375 adults From Puerto Rico Living in the U.S. Foreign- or native-born Women and men |
Unidimensional: Language acculturation |
Immune (CRP), endocrine (DHEA-S, cortisol, EPI, NOREPI), cardiovascular (SBP, DBP), metabolic (TC, HDL-C, HbA1c, WC) | Unadjusted | ↓ There was a marginally significant negative correlation between acculturation and AL score. |
Note. If not stated otherwise, immune markers represent pro-inflammatory markers. Language acculturation refers to a variety of different acculturation measures that capture aspects of language use, such as English language use in different settings, language proficiency, language preference, and others.
As shown in Table 1, articles were published from 2006 onwards, and the vast majority of the articles was published after 2010. The articles comprised a total of 56,378 participants (these were not always unique subjects as some articles used data from same studies, e.g., NHANES, Boston Puerto Rican Health study, however, these will be not disentangled here). The majority of the studies included adult samples, while only 2 studies included children (Kannan et al., 2013; Mendoza et al., 2017) and 4 adolescents (Gonzales et al., 2018; Qu et al., 2020; Zeiders et al., 2018, 2012). Except for two studies, all other studies were conducted in the U.S. Most studies included Hispanic samples, while only few studies included Asian or other focus groups. Most of the studies included both foreign- and native-born people, whereas only few studies included either foreign-born or US-/native-born participants.
The vast majority of the studies applied cross-sectional designs. 3 studies applied a laboratory stress paradigm, the Trier Stress Test (TSST) (Gonzales et al., 2018; Wang and Lau, 2018; Yim et al., 2019). Two studies investigated the prospective relationship between acculturation and stress biomarkers during pregnancy (D’Anna et al., 2012; Scholaske et al., 2018). Another study was a randomized control study that investigated the effects of Mexican vs. US diet on stress (which can be regarded as a behavioral sequelae of acculturation) on stress biomarkers (Santiago-Torres et al., 2016).
The selection of covariates in statistical analyses differed between studies with immune, endocrine, and AL as the outcome: Most analyses with immune markers were adjusted for demographic and biophysical factors (e.g., age, sex, BMI), whereas analyses with endocrine markers as the outcome were often adjusted for psychological conditions (e.g., stress, depression) in addition to demographic and biophysical factors (e.g., age, sex), and studies with AL as the outcome controlled for demographic and biophysical factors (e.g., age, sex) and socioeconomic factors (e.g., education, income). Some of these covariates include factors that are components of our framework (e.g., stress experience) and therefore could provide evidence on whether the associations are fully mediated by these factors.
We did not evaluate further strategies that were applied to control for the potential effects of other factors such as inclusion/exclusion criteria for study participation or analyses, selection of covariates via correlational pattern (i.e., include variable as covariate of significantly correlated with the outcome), separate analyses for different groups, or sensitivity analyses as this is beyond the scope of our article.
3.2. Acculturation measures used in the included studies
There was a high level of heterogeneity between the studies regarding how acculturation was assessed. The most often used acculturation measures were language acculturation (n = 15 studies), length of stay in the host country (n = 13 studies) and nativity / generation status (n = 10 studies). Thus, most studies used proxy measures that represent a unidimensional conceptualization of acculturation.
A total of 11 studies used validated scales (e.g., Acculturation Rating Scale for Mexican Americans, Vancouver Acculturation Index), especially in the studies with endocrine markers (D’Anna et al., 2012; Fang et al., 2014; Gonzales et al., 2018; Mangold et al., 2012, 2010; Qu et al., 2020; Scholaske et al., 2018; Torres et al., 2018; Wang and Lau, 2018; Wu et al., 2019; Yim et al., 2019) (see Table 1). These provided separate scores for heritage and host cultural orientations that can be used separately or as a composite score, indicating a unidimensional conceptualization of acculturation. A bidimensional conceptualization that reflects the different acculturation strategies in accordance with Berry’s acculturation model is operationalized for example by an interaction term between host and heritage cultural orientation in the analyses (Nguyen and Benet-Martínez, 2007). Only two of the reviewed studies reflected a bidimensional conceptualization of the acculturation construct. One study used an interaction term between the host and heritage cultural orientation as proposed by Berry et al. (Gonzales et al., 2018). Another study used a language scale as a bidimensional measure, categorizing participants in three groups representing high English proficiency, low English proficiency, and bilingualism (Ruiz et al., 2013). All other studies used a composite score of the two scores or used them as predictors in separate analyses. One study did not report how the acculturation score was created (Zeiders et al., 2018).
3.3. Association between acculturation and stress biomarkers
Table 1 gives an overview of the studies organized by the different sections (i.e., studies with immune, endocrine, and AL scores). It includes information on study (i.e., publication year, study design, covariates, acculturation measure, stress biomarkers used in the studies) and sample characteristics (i.e., ethnicity, country of residence, age group, nativity, gender). In addition, the number of studies for which each characteristic applies is indicated, as is the number of studies among those that reported a significant association between acculturation and a stress biomarker. In addition, the table presents the number of analyses within the studies that reported a positive, negative or null association.
Most of the studies included endocrine markers (n = 20), while 14 studies included immune/inflammatory markers, and 9 included an AL score as the outcome. One study on the relationship between acculturation and AL scores in addition also presented separate analyses on the pro-inflammatory marker CRP (Cedillo et al., 2020) and is therefore included in both the AL and the immune/inflammatory section. In several studies, multiple acculturation measures and stress biomarkers were used, and inconsistent relationships between different acculturation measures with the same biomarkers, or between the same acculturation measure and different biomarkers, were reported. For example, one study reported that longer length of stay was related to higher concentrations of CRP and to lower concentrations of sTNFR2, while acculturation as measured by the GEQ-A was related to lower concentrations of CRP but was unrelated to sTNFR2 (Fang et al., 2014). Yet another study found that higher acculturation was related to a blunted CAR, but was unrelated to cortisol AUC, waking and bedtime cortisol levels (Zeiders et al., 2012).
3.3.1. Acculturation and immune/inflammatory markers
14 studies included analyses on acculturation and inflammation markers (see Table 1). The most often used markers were the pro-inflammatory markers CRP (n = 11) (Ablow Measelle et al., 2019; Cedillo et al., 2020; Fang et al., 2014; Gouin and MacNeil, 2019; Kannan et al., 2013; Lommel et al., 2019; Pierce et al., 2007; Rodriguez et al., 2012; Rosenberg et al., 2017; Santiago-Torres et al., 2016; Steffen et al., 2016), whereas other markers such as IL-6 (n = 3) (Santiago-Torres et al., 2016; Scholaske et al., 2018; Wommack et al., 2013), sTNFR2 (n = 1) (Fang et al., 2014), and anti-inflammatory markers IL-1RA (n = 2) (Ruiz et al., 2007; Wommack et al., 2013) and IL-10 (n = 1) (Wommack et al., 2013), were less common. In each of the studies concentrations of inflammatory markers were analyzed in blood samples.
Under conditions of chronic stress, concentrations of pro-inflammatory markers (e.g., CRP, IL-6) increase, and this provokes an enhanced release of anti-inflammatory markers (e.g., IL-1RA, IL-10) in order to counter-regulate a pro-inflammatory state (Ouyang et al., 2011). Previous studies suggest that chronic stress is related to alterations in the balance between pro- and anti-inflammatory markers (Coussons-Read et al., 2007; Gouin et al., 2012) which is why we hypothesized that acculturation would be related to higher levels of pro- and anti-inflammatory markers.
In line with our expectation, 10 out of 14 studies reported at least one significant association between an acculturation measure and concentrations of inflammatory markers across 15 out of 34 analyses, specifically to higher (n = 7 studies / 8 analyses) (Cedillo et al., 2020; Fang et al., 2014; Gouin and MacNeil, 2019; Lommel et al., 2019; Pierce et al., 2007; Rodriguez et al., 2012; Steffen et al., 2016) and lower (n = 1) CRP (Fang et al., 2014), higher IL-1RA (n = 2 studies / 4 analyses) (Ruiz et al., 2007; Wommack et al., 2013), higher IL-6 (n = 1) (Scholaske et al., 2018), and lower sTNFR2 (n = 1) (Fang et al., 2014) concentrations.
A total of 8 studies also indicated no relationship between acculturation and immune markers across 18 analyses, including CRP (n = 6 studies / 10 analyses) (Ablow Measelle et al., 2019; Kannan et al., 2013; Pierce et al., 2007; Rodriguez et al., 2012; Rosenberg et al., 2017; Santiago-Torres et al., 2016), IL-6 (n = 2 studies / 4 analyses) (Santiago-Torres et al., 2016; Wommack et al., 2013), sTNFR2 (n = 1 study / 1 analysis) (Fang et al., 2014), and IL-10 (n = 1 study / 3 analyses) (Wommack et al., 2013). With regard to adjustment for psychological states and conditions, 4 of the 10 studies that reported a significant relationship between acculturation and inflammatory markers were adjusted for psychological factors (Fang et al., 2014; Gouin et al., 2012; Gouin and MacNeil, 2019; Lommel et al., 2019; Ruiz et al., 2007), while none of the studies that did not find a relationship were adjusted for this.
Table 1 presents the number of studies indicating associations between acculturation and stress biomarkers per category. Most studies reported at least one positive relationship between acculturation and immune markers. Study characteristics were rather homogenous between the studies. Thus, it is not possible to infer the extent to which the association between acculturation and immune markers varied as a function of factors such as year of publication, study design, and sample characteristics. As a large proportion of the studies indicated a positive relationship between acculturation and inflammatory markers, this relationship might be generalizable to cross-sectional studies that relate unidimensional measures of acculturation, especially length of stay, to CRP levels in samples of Hispanic adult foreign- or native-born men and women. Language-related measures and length of stay in the host country were most often used as acculturation measures in these studies and were related to higher levels of inflammatory markers in most of the studies.
3.3.2. Acculturation and endocrine markers
20 studies investigated the link between acculturation and different endocrine markers (see Table 1). The vast majority of studies with endocrine markers as the outcome focused on different cortisol measures (n = 15): cortisol concentrations assessed in blood (n = 1 study) (Ruiz et al., 2013) or hair (n = 1 study) (Wu et al., 2019), salivary cortisol levels at single or averaged across different measurement time points across the day (n = 3 studies) (Mendoza et al., 2017; Torres et al., 2018; Zeiders et al., 2012), the salivary cortisol awakening response (CAR, n = 4 studies) (Burt et al., 2018; Mangold et al., 2012, 2010; Zeiders et al., 2012), the salivary cortisol diurnal slope (n = 2) (D’Anna et al., 2012; Zeiders et al., 2018), salivary cortisol diurnal output (diurnal area under the curve (AUC, n = 3 studies) (Nicholson et al., 2013; Qu et al., 2020; Zeiders et al., 2012), and salivary cortisol reactivity during the Trier Social Stress Tests (TSST, n = 3 studies) (Gonzales et al., 2018; Wang and Lau, 2018; Yim et al., 2019). Only a small number of studies included other endocrine markers such as urinary catecholamines epinephrine and norepinephrine (n = 2 studies) (Brown and James, 2000; Jimenez et al., 2012), CRH from blood in pregnant women (n = 1 study) (Ruiz et al., 2006), estriol-progesterone ratio from blood (n = 1 study) (Ruiz et al., 2012), and parathyroid hormone from blood (n = 1 study) (Nabipour et al., 2011).
Chronic stress contributes to dysregulation of the hypothalamic-pituitary-adrenal axis as reflected in higher baseline concentrations of specific hormones (e.g., CRH, cortisol, epinephrine). In addition, it affects the diurnal rhythm of cortisol release. After awakening, cortisol levels increase and reach their peak at around 30 min later, also referred to as the cortisol awakening response (CAR). In individuals who experience chronic stress, alterations were found in the CAR (Kuras et al., 2017), and cortisol diurnal slope, i.e., the decline in cortisol levels from morning to night (Adam et al., 2015, 2017) which may reflect impairments in the negative feedback regulation of the HPA axis. In studies that apply laboratory paradigms to induce stress, e.g., the Trier Stress Test (TSST), cortisol concentrations are assessed before, during and after a laboratory stressor in order to assess the cortisol reactivity. While the stressor triggers an increase of cortisol levels in healthy individuals, participants with chronic stress experience often show an altered response (Metz et al., 2020). Thus, the expectation is that acculturation is related to concentrations of baseline endocrine markers, the CAR, the cortisol diurnal slope and overall cortisol output across the day (AUC) and cortisol reactivity during experimental stress paradigms.
Estriol and progesterone are assumed to play an important role in parturition (Goodwin, 1999; Kamel, 2010). Estriol concentrations increase and progesterone levels decrease in the month before delivery, resulting in a higher estriol-progesterone ratio (Smith et al., 2009). It has been proposed that a higher estriol-progesterone ratio may mediate the link between acculturation and preterm birth risk (Ruiz et al., 2012). Parathyroid hormone is the primary regulator of calcium homeostasis in the blood (Culhane et al., 2018). Elevations in parathyroid hormone are believed to play a key role in mediating the link between enhanced stress levels and poorer bone health (Ng and Chin, 2021). We therefore expected that acculturation would be related to the estriol-progesterone ratio and concentrations of parathyroid hormones.
In line with our expectation that acculturation is related to altered concentrations of endocrine markers, in 12 out of 20 studies, acculturation was related to concentrations or measures of endocrine markers across 16 out of 50 analyses, specifically, to higher concentrations of catecholamines (n = 1 study/2 analyses) (Brown and James, 2000), higher concentrations of CRH in pregnant women (n = 1 study / 1 analysis) (Ruiz et al., 2006), and a higher estriol-progesterone ratio (n = 1 study / 1 analysis) in pregnant women (Ruiz et al., 2012). Regarding cortisol measures, acculturation was related to lower cortisol concentrations in blood samples (n = 1 study / 1 analysis) (Ruiz et al., 2013), lower (n = 1 study / 1 analysis) single or averaged across different measurements salivary cortisol values (Mendoza et al., 2017), to an elevated (n = 1 study / 2 analyses) (Burt et al., 2018) or attenuated (n = 4 studies / 4 analyses) (Burt et al., 2018; Mangold et al., 2012, 2010; Zeiders et al., 2012) CAR, a flatter cortisol diurnal slope (n = 1 study / 1 analysis) (D’Anna et al., 2012), to a higher (n = 1 study/1 analysis) and lower cortisol diurnal AUC (n = 1 study / 1 analysis) (Nicholson et al., 2013), and to decreased (n = 1 study / 1 analysis) cortisol reactivity during a laboratory stress paradigm (Gonzales et al., 2018).
A total of 13 studies also reported no relationship between acculturation and endocrine markers across 34 out of 50 analyses, including catecholamines (n = 2 studies/8 analyses) (Brown and James, 2000; Jimenez et al., 2012), parathyroid hormone (n = 1 study/1 analysis) (Nabipour et al., 2011), hair cortisol (n = 1 study/3 analyses) (Wu et al., 2019), salivary cortisol at different sampling times across the day (n = 2 studies / 8 analyses) (Torres et al., 2018; Zeiders et al., 2012), CAR (n = 2 studies/2 analyses) (Burt et al., 2018; Mangold et al., 2012), cortisol diurnal slope (n = 2 studies / 4 analyses) (D’Anna et al., 2012; Zeiders et al., 2018), cortisol diurnal AUC (n = 2 studies/2 analyses) (Qu et al., 2020; Zeiders et al., 2012), and cortisol reactivity during the TSST (n = 2 studies / 6 analyses) (Wang and Lau, 2018; Yim et al., 2019). 7 of the 12 studies that showed a relationship (Burt et al., 2018; Mangold et al., 2012, 2010; Mendoza et al., 2017; Ruiz et al., 2006, 2012; Zeiders et al., 2012) and 6 of the 13 studies that showed no relationship (Burt et al., 2018; Jimenez et al., 2012; Mangold et al., 2012; Wu et al., 2019; Zeiders et al., 2018, 2012) were adjusted for psychological conditions.
There was little variation in the study characteristics between studies that included endocrine measures as the outcome (see Table 1). That is, most of the evidence derives from cross-sectional studies published since 2011 with foreign- or native-born adult Hispanic women and men in the U.S. There is larger variance in the stress biomarkers especially regarding the different measures of cortisol that were significantly associated with acculturation in almost two thirds of the studies. Acculturation measures were related to lower CAR in the 4 studies that investigated this relationship. However, the number of studies that used these markers is small and therefore does not allow for a systematic analysis.
There is heterogeneity in the acculturation measures that were used in the studies with endocrine markers as outcomes. Language acculturation (n = 5 studies) and nativity (n = 5 studies) were the most often used proxy measure of acculturation. While language acculturation was significantly associated with endocrine markers in most studies, nativity was not related to endocrine markers in any of the studies. Only 2 studies applied a bidimensional measures and found that a high orientation towards both host and heritage culture (i.e., an interaction term between host and heritage cultural orientation of the BARSMA-II) was related to a steeper increase in cortisol reactivity and higher cortisol peak during the TSST, while a high orientation towards the host culture in conjunction with a low orientation towards heritage culture was associated with the flattest cortisol reactivity to the TSST (Gonzales et al., 2018). In the other study it was shown that participants with high English proficiency had significantly lower mean cortisol concentrations compared to participants with high Spanish proficiency and compared to bilingual participants (Ruiz et al., 2013).
3.3.3. Acculturation and AL scores
8 studies tested the relationship between acculturation and allostatic (AL) load scores (see Table 1). These studies differed in the selection of physiological systems, as they comprised markers of the immune (e.g., CRP, IL-6), endocrine (e.g., cortisol, DHEA-S), cardiovascular (e.g., systolic and diastolic blood pressure, heart rate), and/or metabolic system (e.g., total and HDL cholesterol, glucose), and in the number of biological markers included in the score, ranging from 6 to 15. AL scores included either markers of the immune, endocrine, cardiovascular, and metabolic system (n = 3 studies) (Arevalo et al., 2014; Peek et al., 2010; Todorova et al., 2013), of the immune, cardiovascular and metabolic system (n = 4 studies) (Cedillo et al., 2020; Doamekpor and Dinwiddie, 2020; McClure et al., 2015; Niño and Hearne, 2020), or of the endocrine, cardiovascular and metabolic system (n = 1 study) (Mattei et al., 2011). That is, cardiovascular and metabolic markers were included in all of the AL scores. Chronic stress was found to be related to altered levels of AL in previous studies (Juster et al., 2010), thus we expected that acculturation would be associated with AL scores.
7 out of 8 studies showed a significant relationship between acculturation and AL scores across 17 out of 24 studies, specifically, to a higher (n = 1 study / 3 analyses) (Peek et al., 2010) and lower (n = 1 study / 1 analysis) (Todorova et al., 2013) AL score that comprised immune, endocrine, cardiovascular and metabolic markers, to a higher (n = 4 studies / 9 analyses) (Cedillo et al., 2020; Doamekpor and Dinwiddie, 2020; McClure et al., 2015; Niño and Hearne, 2020) and lower (n = 1 study / 3 analyses) (Niño and Hearne, 2020) AL score that comprised immune, cardiovascular and metabolic markers, and to a lower AL score that included endocrine, cardiovascular and metabolic markers (n = 1 study / 1 analysis) (Mattei et al., 2011). In one study (2 analyses), acculturation was unrelated to an AL score that comprised immune, endocrine, cardiovascular and metabolic markers (Arevalo et al., 2014), and in the studies by Cedillo (Cedillo et al., 2020) and Peek (Peek et al., 2010), further acculturation measures were unrelated to the AL score (6 analyses). 1 of the 7 studies that showed a relationship (Niño and Hearne, 2020)and the study that did not show a relationship (Arevalo et al., 2014) were adjusted for psychological conditions.
Regarding the question as to how different study characteristics may have contributed to differences in the reported results (especially regarding the direction of the relationship), it has to be noted that there was even less variance in study designs among the AL studies compared to the immune/inflammatory and endocrine studies in terms of selection of stress biomarkers (all included cardiovascular and metabolic markers in the AL score, and most included immune/inflammatory and/or endocrine markers), study design (all were cross-sectional), and sample characteristics (mostly Hispanic adult foreign- or native-born men and women) (see Table 1). Therefore, we cannot draw any conclusions on how these factors may explain the relationship between acculturation and AL scores. At the same time, although there was little variance between the studies in the choice of acculturation measures (mostly unidimensional proxy measures), a pattern emerged: use of language of the host country was related to lower AL scores, while nativity/generation status, length of stay and age at arrival were mostly related to higher AL scores throughout the studies.
4. Discussion
4.1. Summary of findings
In addressing our initial questions that guided our review we come to the following conclusions: First of all, most of the evidence on the relationship between acculturation and stress biomarkers originates from cross-sectional studies with mostly adult, Hispanic women and men living in the U.S. In these studies, mostly unidimensional measures of acculturation, especially proxy measures, were applied and analyses were adjusted for biophysical factors (immune/inflammatory), biophysical factors and psychological conditions (endocrine), or socioeconomic factors (AL). These studies often use the same set of biomarkers (i.e., CRP as an inflammatory marker, cortisol as an endocrine marker, and AL scores comprising immune/inflammatory, endocrine, cardiovascular, and metabolic markers).
Second, in 29 of the 41 studies reviewed, acculturation was significantly related to biological stress markers, with some inconsistency within studies reporting different results depending on acculturation measures, biological outcomes, groups (e.g., by ethnicity, gender, nativity), or covariates used in the analyses. Generally, the summation of the observed results substantiates the direction of our proposed hypotheses, in that acculturation in terms of a higher orientation towards the host culture is positively associated with levels of pro- and anti-inflammatory markers and higher allostatic load scores, whereas the direction of findings is more heterogenous in the case of endocrine markers.
Third, while there was little variation regarding study design, sample and outcome measures, some consistent patterns of results could be identified with respect to acculturation measures and biological stress markers. Overall, the different acculturation measures tended to be positively related to biological stress markers. Regarding the most often used acculturation measures, language acculturation was related to higher inflammatory and endocrine markers (and to lower AL scores), and nativity/generation status and length of stay were related to higher inflammatory markers and AL score.
A limitation of our systematic review is that only one author conducted the literature review and selected the articles. This represents a deviation from PRISMA guidelines. Nevertheless, this author double-checked each item regarding its eligibility based on the search criteria and double-checked the data that was extracted from each study.
4.2. Methodological challenges
This review focused on the relationship between acculturation and inflammatory and endocrine stress markers and AL scores across different studies. While most studies reported significant associations between acculturation and stress biomarkers, results are inconsistent, which may be due to methodological weaknesses regarding four aspects: a) the use of acculturation measures that do not reflect appropriate and timely conceptualization and operationalization of acculturation as reflected in bidimensional measures, b) cross-sectional study designs that do not allow insight into the stability of the effects of acculturation on stress biology over time, c) assessment of circulating stress biomarkers that provide only limited information about the dysregulation of physiological systems compared to the assessment of stress biomarkers under acute stress/ challenge conditions, and d) neglect of important covariates or the selection of covariates that may be on the causal pathways in the framework on how acculturation is linked to stress biology (e.g., stress experience, BMI, health behaviors). In the following, we will discuss these challenges and provide recommendations for future research.
4.3. Acculturation measures
Most of the studies reviewed here used unidimensional measures of acculturation, mostly proxy measures. While it has been noted that integration (i.e., orientation towards both the heritage and host culture) is an acculturation strategy related to best health outcomes (Yoon et al., 2013), this assumption has been only studied and shown with a comprehensive acculturation measure in one of the reviewed articles here where an interaction term between host and heritage cultural orientation was used as a predictor for cortisol concentrations during a laboratory stress paradigm (Gonzales et al., 2018). Their finding is in line with the assumption that the acculturation strategy integration is related to more favorable outcomes, while assimilation will be related to poorest outcomes. The exclusive use of unidimensional measures disregards and undermines the protective role of integration (Fox et al., 2017b). This may also explain why measures of host cultural orientation were related to both favorable and unfavorable outcomes (e.g., language acculturation was related to higher immune markers, but also to lower AL scores), raising the question as to what would be the relationship when moderated by heritage cultural orientation.
Of note, it seemed that proxy measures were relatively more often associated with stress biomarkers than were the measures using scores of validated acculturation scales. This is of particular interest since validated scales are believed to overcome the shortcomings of proxy measures, and it raises the question of whether validated scales appropriately conceptualize and operationalize the acculturation construct. It is often the case that validated scales capture different aspects of acculturation (such as language use or preference, media use, ethnic identity, or ethnic identity of peers) than proxy measures. They often do not capture aspects of acculturation that may be particularly relevant for health (e.g., stress, behaviors) along a bidimensional conceptualization of acculturation. We therefore propose that future studies should include such aspects in their measure of acculturation and go beyond the use of unidimensional proxy measures or indices by use of validated multidimensional acculturation scales with host and heritage cultural orientation subscales, and to account for the moderating role of contextual factors by implementing interaction terms with these factors in their analyses.
Some studies showed that acculturation was related to stress biomarkers in interaction with psychological (e.g., neuroticism, stress, trauma) or socioeconomic factors (e.g., SES, financial strain, income, income-to-poverty ratio), and in some of these studies the main effect of acculturation was not significant after adjusting for these factors. It has been argued elsewhere that studies should test interaction effects with contextual factors, such as neighborhood ethno-cultural composition, discrimination, discrepancy between heritage and host cultures, and individual and group attitudes towards assimilation as these are believed to be moderators on the effects of acculturation on health (Fox et al., 2017a). Thus, analyses strategies should be applied in future studies that determine the nature of the combined effect of acculturation, SES and psychological factors, to contrast overlapping (i.e., acculturation SES, and psychological state are redundant), additive (i.e., each measure provides independent prediction), and multiplicative (i.e., the impact of acculturation on stress biology is a function of SES and psychological state) effects.
4.4. Longitudinal studies
Most of the studies reviewed here applied cross-sectional study designs which means that acculturation measures were related to concurrent stress biomarker concentrations assessed at a single measurement time point. It has been proposed that the relationship between acculturation and physiological dysregulation results from long-term processes (Cunningham et al., 2008), and that the effects of acculturation are also forwarded to the offspring generation (Fox et al., 2015). In line with this assumption is the observation that in several cross-sectional studies reviewed here, longer length of stay and being born in the host country were related to higher concentrations of stress biomarkers. However, this approach may not sufficiently control for age, inheritance, or cohort effects as already mentioned (Fox et al., 2017b). At the same time, acculturation is operationalized as a state rather than a process in cross-sectional studies. We posit that there is a need for longitudinal study designs in order to address three questions. First, it needs to be studied if and how stress experience in the context of acculturation accumulates over time and thereby leads to physiological dysregulation or biological embedding. Second, it should be studied if and how intra-individual variability in acculturation levels (i.e., acquisition or abandonment of different acculturation strategies over time) contribute to physiological dysregulation over time. These can be likewise addressed by longitudinal studies as proposed above, where analyses target to quantify the effect of variability. Another more time-efficient, low cost possibility to address this question is to design acculturation instruments that simultaneously capture acculturation levels at several different time points in life (Fox et al., 2017b). Although retrospective response bias may reduce test quality, this can be an important first step in studying acculturation and its effect on physiology as a process.
Third, how health disparities are transmitted to the offspring generation is of high relevance for future studies. It is a common observation that offspring of immigrants often develop health disparities from the earliest ages that correlate with maternal acculturation levels (Fox et al., 2015, 2018). Many of these health disparities may originate during the fetal stage of life (Gluckman and Hanson, 2004). Thus, maternal-placental-fetal stress biology is proposed to be a key mediating pathway for this intergenerational transmission in the way that the excretion of stress biomarkers serve as signals of maternal states (e.g., psychological sequelae of acculturation) the developing fetus responds to (Fox et al., 2015, 2018). In order to test these relationships, prospective cohort studies constitute an adequate study design where mother-child-dyads participated in a longitudinal study beginning from pregnancy on with follow-up measurements until childhood (Euser et al., 2009). Some of the studies reviewed here included prospective cohort studies, albeit they included only measurements during pregnancy and did not follow-up on stress biomarkers in the newborn.
4.5. Stress biomarkers
In general, the use of biological markers as indicators of health are regarded as more reliable and objective measures and compared to self-reports that are often biased by subjective characteristics and cultural orientation (Fox et al., 2017b). Stress biomarkers are antecedents of unfavorable health outcomes that can already indicate health risks before health disparities manifest. Most of the studies reviewed here used one-time circulating biomarkers that were assessed as indicators of physiological dysregulation. However, measuring biological markers in response to acute stress exposure is believed to more reliably capture physiological dysregulation in stress-related biological systems (Epel et al., 2018). In the studies reviewed here, only three studies assessed stress biomarkers (i.e., cortisol) during a laboratory stress paradigm, the TSST. These showed mixed results regarding the relationship between acculturation and cortisol reactivity. Nevertheless, since so far only very few studies applying a laboratory stress paradigm exist in this context, we recommend that future studies should apply laboratory stress paradigms to more robustly relate acculturation levels to the reactivity of different physiological systems.
An alternative approach to examining circulating inflammatory markers is to stimulate the blood samples with a mitogen and quantify the cytokine response to this challenge ex vivo (Groote et al., 1992). For example, studies that investigate the relationship between depression and inflammation yielded more meaningful results using this approach (Majd et al., 2018). Furthermore, the pro-inflammatory state may be better depicted by pro- and anti-inflammatory ratios rather than using pro- and anti-inflammatory markers as separate outcomes (Lazarides et al., 2019).
In addition, we suggest future studies go beyond markers of immune, endocrine, metabolic and cardiovascular system and include stress biomarkers related to cellular senescence (e.g., telomere length), oxidative stress exposure (e.g., lipid hydroperoxides) and mitochondrial function.
We found that all studies that examined the relationship of nativity/generation status (n = 4) and length of stay (n = 4) with AL scores reported positive associations. This may be also due to the inclusion of cardiovascular and metabolic parameters in these AL scores. This raises the question whether this more comprehensive measure (compared to, e.g., using concentrations of single cytokines as the outcome) potentially is better at capturing a wider range of experiences and exposures related to acculturation.
4.6. Covariates
According to the proposed framework, psychological stress mediates the link between acculturation and stress biology, and its effects may be amplified by unhealthy behaviors. In addition, it has been suggested that socioeconomic status may confound or moderate the effects of acculturation on stress biomarkers (Fitzgerald, 2010). In due consideration of these relationships and in order to determine independent associations between acculturation on stress biomarkers, many of the reviewed studies thus included socioeconomic, biophysical, psychological and behavioral variables such as education, BMI, depression, or smoking status as covariates in their analyses. In most studies, because acculturation was significantly associated with stress biomarkers after adjustment for these variables, it is possible that a) acculturation, psychological and behavioral factors interpedently contribute to variation in stress biomarkers; b) the proposed pathway(s) only partly mediate the link between acculturation and stress biomarkers, or c) the covariates did not reflect the most important aspects of the specific pathways (e.g., models are adjusted for behavioral factors such as smoking, but diet could be more crucial). There were only few studies that directly investigated mediating pathways, such as Ruiz et al. (2006) who showed in a path model that English language-related acculturation was related to higher CRH concentrations at 22–25 weeks of gestation via perceived stress.
Given the relevance of theoretically and empirically derived frameworks, studies should also discuss in more detail what the pattern of results means in terms of (non)significant effects of predictors and covariates for the assumed cause-effect relationships. We recommend that future studies should go beyond considering these factors as confounders and examine their role as potential mediators or moderators (effect modifiers) in greater detail. Specifically, we recommend further investigation of the behavioral and psychological mediational pathways by which acculturation may contribute to alterations in stress biomarkers, and whether these relationships may be moderated by socioeconomic status or race/ethnicity. Appropriate statistical analysis methods in this context constitute mediation analyses using linear regression models or path models.
4.7. Generalizability
The goal of this article is to provide a comprehensive overview of the existing studies that have investigated the relationship between acculturation and stress biomarkers. We found that there is considerable heterogeneity regarding methodological aspects and study samples. Most of the studies reviewed here were conducted among Hispanic populations living in the US. A few additional studies involved Asians, Blacks, or immigrants from other countries living in the U.S., Canada, or Australia. These groups may differ systematically in terms of their general health status and health risks (e.g., behavioral health risk profiles), cultural aspects, acculturation levels, integration in host societies, perceived discrimination, socioeconomic status, language proficiency and use, reasons for immigration, and other aspects that may contribute to perceived stress levels and concentrations of stress biomarkers. We therefore recommend more studies in the future should be conducted in other ethnic groups and countries other than the U.S. This will then allow a systematic analysis of potential differences or similarities in observed associations across immigrant groups.
We recommend that future studies could also examine the association between acculturation and stress biomarkers using meta-analyses that focus only on one group of outcome measures at a time (i.e., immune, endocrine, or allostatic).
4.8. Conclusion and outlook
Current research shows a close relationship between acculturation and health decline in different immigrant / ethnic minority groups across different countries of origin and receiving countries. A number of studies now indicate that immune and endocrine stress response might be among the biological pathways that mediate this relationship. However, to date, this evidence is mostly restricted to cross-sectional studies that applied unidimensional measures of acculturation in samples of adult Hispanics in the U.S. Yet little is known about the relationship between acculturation and stress biology from a longitudinal or prospective perspective and in due respect of timely operationalization of the acculturation concept. Addressing these methodological challenges is thus a vital task for future studies.
Footnotes
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
References
- Ablow Measelle E, McClure HH, Snodgrass JJ, Martinez CR, Jiménez R, Isiordia L, 2019. Climbing the ladder of decline: income and acculturation associated with chronic inflammation among Mexican immigrants. Am. J. Hum. Biol.: Off. J. Hum. Biol. Counc 31 (4), 23271. 10.1002/ajhb.23271. [DOI] [PubMed] [Google Scholar]
- Adam EK, Heissel JA, Zeiders KH, Richeson JA, Ross EC, Ehrlich KB, Eccles JS, 2015. Developmental histories of perceived racial discrimination and diurnal cortisol profiles in adulthood: a 20-year prospective study. Psychoneuroendocrinology 62, 279–291. 10.1016/j.psyneuen.2015.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam EK, Quinn ME, Tavernier R, McQuillan MT, Dahlke KA, Gilbert KE, 2017. Diurnal cortisol slopes and mental and physical health outcomes: a systematic review and meta-analysis. Psychoneuroendocrinology 83, 25–41. 10.1016/j.psyneuen.2017.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson C, Zhao H, Daniel CR, Hromi-Fiedler A, Dong Q, Gbito A, Wu X, Chow W-H, 2016. Acculturation and diabetes risk in the Mexican American Mano a Mano cohort. Am. J. Public Health 106 (3), 547–549. 10.2105/AJPH.2015.303008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arends-Toth J, Vijver FJR van de, 2006. Assessment of psychological acculturation. In: Berry JW, Sam DL (Eds.), The Cambridge Handbook of Acculturation Psychology. Cambridge University Press, Cambridge, pp. 142–160. [Google Scholar]
- Arevalo SP, Tucker KL, Falcon LM, 2014. Life events trajectories, allostatic load, and the moderating role of age at arrival from Puerto Rico to the US mainland. Soc. Sci. Med 120, 301–310. 10.1016/j.socscimed.2014.09.040.Life. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry JW, 2006. Contexts of acculturation. In: Berry JW, Sam DL (Eds.), The Cambridge Handbook of Acculturation Psychology. Cambridge University Press, Cambridge, pp. 27–42. [Google Scholar]
- Berry JW, Kim U, Minde T, Mok D, 1987. Comparative studies of acculturative stress. Int. Migr. Rev 21 (3), 491–511. [Google Scholar]
- Bierhaus A, Wolf J, Andrassy M, Rohleder N, Humpert PM, Petrov D, Nawroth PP, 2003. A mechanism converting psychosocial stress into mononuclear cell activation. PNAS 100 (4), 1920–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DE, James GD, 2000. Physiological stress responses in Filipino-American Immigrant Nurses: the effects of residence time, life-style, and job strain. Psychosom. Med 62, 394–400. [DOI] [PubMed] [Google Scholar]
- Burt KB, Obradovic J, Leu J, 2018. Self-construal, family context, and the cortisol awakening response in first- and second-generation Asian American college students. Emerg. Adulthood 6 (2), 104–117. 10.1177/2167696817706039. [DOI] [Google Scholar]
- Castillo LG, Navarro RL, Walker JEOY, Schwartz SJ, Zamboanga BL, Krauss Whitbourne S, Caraway SJ, 2015. Gender matters: the influence of acculturation and acculturative stress on Latino college student depressive symptomatology. J. Lat. /o Psychol 3 (1), 40–55. 10.1037/lat0000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cedillo YE, Bertrand B, Baker E, Cherrington AL, Beasley TM, Fernández JR, 2020. Assimilation, acculturation, and allostatic load in U. S.- and Foreign-Born Hispanics. J. Immigr. Minor. Health 23 (1), 35–44. 10.1007/s10903-020-01012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Juon H-S, Sunmin L, 2012. Acculturation and BMI among Chinese, Korean and Vietnamese Adults. J. Community Health 37, 539–546. 10.1007/s10900-011-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A, Colodner R, Masalha R, Haimov I, 2019. The relationship between tobacco smoking, cortisol secretion, and sleep continuity. Subst. Use Misuse 54 (10), 1705–1714. 10.1080/10826084.2019.1608250. [DOI] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, Turner RB, 2012. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. PNAS 109 (16), 5995–5999. 10.1073/pnas.1118355109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commodore-Mensah Y, Nwakaego U, Cooper LA, Agyemang C, Dennison Himmelfarb C, 2018. The association between acculturation and cardiovascular disease risk in Ghanaian and Nigerian-born African immigrants in the United States: the Afro-Cardiac Study. J. Immigr. Minor. Health 20, 1137–1146. 10.1007/s10903-017-0644-y. [DOI] [PubMed] [Google Scholar]
- Coussons-Read ME, Okun ML, Nettles CD, 2007. Psychosocial stress increases inflammatory markers and alters cytokine production across pregnancy. Brain, Behav. Immun 21 (3), 343–350. 10.1016/j.bbi.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Cuellar I, Arnold B, Maldonado R, 1995. Acculturation rating scale for Mexican Americans-II: a revision of the original ARSMA-Scale. Hisp. J. Behav. Sci 17 (3), 275–304. [Google Scholar]
- Culhane KJ, Belina ME, Sims JN, Cai Y, Liu Y, Wang PSP, Yan ECY, 2018. Parathyroid hormone senses extracellular calcium to modulate endocrine signaling upon binding to the family B GPCR Parathyroid Hormone 1 Receptor. ACS Chem. Biol 13 (8), 2347–2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham SA, Ruben JD, Venkat Narayan KM, 2008. Health of foreign-born people in the United States: a review. Health Place 14 (4), 623–635. 10.1016/J.HEALTHPLACE.2007.12.002. [DOI] [PubMed] [Google Scholar]
- D’Anna KL, Hoffman MC, Zerbe GO, Coussons-Read M, Ross RG, Laudenslager ML, 2012. Acculturation, maternal cortisol and birth outcomes in women of Mexican descent. Psychosom. Med 74 (3), 296–304. 10.1097/PSY.0b013e318244fbde. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Groote D, Zangerle PF, Gevaert Y, Fassotte MF, Beguin Y, Noizat-Pirenne F, Pirenne J, Gathy R, Lopez M, Dehart I, 1992. Direct stimulation of cytokines (IL-1 beta, TNF-alpha, IL-6, IL-2, IFN-gamma and GM-CSF) in whole blood. I. Comparison with isolated PBMC stimulation . Cytokine 4 (3), 239–248. [DOI] [PubMed] [Google Scholar]
- Divney AA, Echeverria SE, Thorpe LE, Trinh-Shevrin C, Islam NS, 2019. Hypertension prevalence jointly influenced by acculturation and gender in US immigrant groups. Am. J. Hypertens 32 (1), 104–111. 10.1093/ajh/hpy130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djuric Z, Bird CE, Furumoto-Dawson A, Rauscher GH, Ruffin IV MT, Stowe RP, Masi CM, 2008. Biomarkers of psychological stress in health disparities research. Open Biomark. J 1, 7–19. 10.2174/1875318300801010007.Biomarkers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doamekpor LA, Dinwiddie GY, 2020. Allostatic load in foreign-born and US-born blacks: evidence from the 2001 – 2010 National Health and Nutrition Examination Survey. Am. J. Public Health 105 (3), 591–597. 10.2105/AJPH.2014.302285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel ES, Crosswell AD, Mayer SE, Prather AA, George M, Puterman E, Mendes WB, 2018. More than a feeling: a unified view of stress measurement for population science. Front. Neuroendocr 49, 146–169. 10.1016/j.yfrne.2018.03.001.More. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euser AM, Zoccali C, Jager KJ, Dekker FW, 2009. Cohort studies: prospective versus retrospective. Nephron Clin. Pract 113 (3), 214–217. 10.1159/000235241. [DOI] [PubMed] [Google Scholar]
- Fang CY, Ross EA, Pathak HB, Godwin AK, Tseng M, 2014. Acculturative stress and inflammation among Chinese immigrant women. Psychosom. Med 76 (5), 320–326. 10.1097/PSY.0000000000000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch BK, Vega WA, 2003. Acculturation stress, social support, and self-rated health among latinos in California. J. Immigr. Health 5 (3), 109–117. 10.1023/A:1023987717921. [DOI] [PubMed] [Google Scholar]
- Fitzgerald N, 2010. Acculturation, socioeconomic status, and health among Hispanics. Napa Bull. 34 (1), 28–46. 10.1111/j.1556-4797.2010.01050.x. [DOI] [Google Scholar]
- Fox M, Entringer S, Buss C, DeHaene J, Wadhwa PD, 2015. Intergenerational transmission of the effects of acculturation on health in Hispanic Americans: a fetal programming perspective. Am. J. Public Health 105, S409–S423. 10.2105/AJPH.2015.302571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox M, Thayer Z, Wadhwa PD, 2017a. Acculturation and health: the moderating role of socio-cultural context. Am. Anthr 119 (3), 405–421. 10.1111/aman.12867.Acculturation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox M, Thayer Z, Wadhwa PD, 2017b. Assessment of acculturation in minority health research. Soc. Sci. Med. 176, 123–132. 10.1016/j.socscimed.2017.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox M, Thayer ZM, Ramos IF, 2018. Prenatal and postnatal mother-to-child transmission of acculturation’s health effects in Hispanic Americans. J. Women’s Health 27 (8), 1054–1063. 10.1089/jwh.2017.6526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluckman PD, Hanson M. a, 2004. Living with the past: evolution, development, and patterns of disease. Science 305 (5691), 1733–1736. 10.1126/science.1095292. [DOI] [PubMed] [Google Scholar]
- Gonzales NA, Johnson M, Shirtcliff EA, Eskenazi B, Deardorff J, 2018. The role of bicultural adaptation, familism, and family conflict in Mexican American adolescents’ cortisol reactivity. Dev. Psychopathol 30 (5), 1571–1587. 10.1017/S0954579418001116.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin TM, 1999. A role for estriol in human labor, term and preterm. Am. J. Obstet. Gynecol 180 (1), S208–S213. [DOI] [PubMed] [Google Scholar]
- Gouin JP, MacNeil S, 2019. Attachment style and changes in systemic inflammation following migration to a new country among international students. Attach. Hum. Dev 21 (1), 38–56. 10.1080/14616734.2018.1541515. [DOI] [PubMed] [Google Scholar]
- Gouin JP, Glaser R, Malarkey WB, Beversdorf D, Kiecolt-Glaser J, 2012. Chronic stress, daily stressors, and circulating inflammatory markers. Health Psychol 31 (2), 264–268. 10.1037/a0025536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman JP, Ostrander MM, Mueller NK, Figueiredo H, 2005. Limbic system mechanisms of stress regulation: hypothalamo-pituitary-adrenocortical axis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 29, 1201–1213. 10.1016/j.pnpbp.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Jimenez JA, Shivpuri S, de Los Monteros KE, Matthews KA, Mills PJ, Gallo LC, 2012. Associations between socioeconomic status and catecholamine levels vary by acculturation status in Mexican-American women. Ann. Behav. Med 44 (1), 129–135. 10.1007/s12160-012-9365-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster RP, McEwen BS, Lupien SJ, 2010. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev 35 (1), 2–16. 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Kamel RM, 2010. The onset of human parturition. Arch. Gynecol. Obstet 281, 975–982. 10.1007/s00404-010-1365-9. [DOI] [PubMed] [Google Scholar]
- Kannan S, Acosta LM, Acevedo-Garcia D, Divjan A, Bracero LA, Perzanowski MS, Chew GL, 2013. Sociocultural characteristics, obesity and inflammatory biomarkers in Puerto Rican toddlers born in New York City. Pediatr. Allergy Immunol 24 (5), 487–492. 10.1111/pai.12084. [DOI] [PubMed] [Google Scholar]
- Kuras YI, Assaf N, Thoma MV, Gianferante D, Hanlin L, Chen X, Rohleder N, 2017. Blunted diurnal cortisol activity in healthy adults with childhood adversity. Front. Hum. Neurosci 11 (574), 1–8. 10.3389/fnhum.2017.00574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Hayes Bautista DE, 2005. Acculturation and Latino health in the united states: a review of the literature and its sociopolitical context. Annu. Rev. Public Health 26, 367–397. 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarides C, Epel ES, Lin J, Blackburn EH, Voelkle MC, Buss C, Entringer S, 2019. Maternal pro-inflammatory state during pregnancy and newborn leukocyte telomere length: a prospective investigation. Brain Behav. Immun 80, 419–426. 10.1016/J.BBI.2019.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebkind K, 2006. Ethnic identity and acculturation. In: Sam DL, Berry JW (Eds.), The Cambridge Handbook of Acculturation Psychology. Cambridge University Press, Cambridge, pp. 78–96. [Google Scholar]
- Lommel LL, Thompson L, Chen JL, Waters C, Carrico A, 2019. Acculturation, inflammation, and self-rated health in Mexican American immigrants. J. Immigr. Minor. Health 21 (5), 1052–1060. 10.1007/s10903-018-0805-7. [DOI] [PubMed] [Google Scholar]
- Majd M, Graham-Engeland JE, Smyth JM, Sliwinski MJ, Lipton RB, Katz MJ, Engeland CG, 2018. Distinct inflammatory response patterns are evident among men and women with higher depressive symptoms. Physiol. Behav 184, 108–115. 10.1016/j.physbeh.2017.11.009.Distinct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangold D, Wand G, Javors M, Mintz J, 2010. Acculturation, childhood trauma and the cortisol awakening response in Mexican American adults. Horm. Behav 58 (4), 637–646. 10.1016/j.yhbeh.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangold D, Mintz J, Javors M, Marino E, 2012. Neuroticism, acculturation and the cortisol awakening response in Mexican American adults. Horm. Behav 61 (1), 23–30. 10.1016/j.yhbeh.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattei J, Noel SE, Tucker KL, 2011. A meat, processed meat, and french fries dietary pattern is associated with high allostatic load in Puerto Rican older adults. J. Am. Diet. Assoc 111 (10), 1498–1506. 10.1016/j.jada.2011.07.006.A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure HH, Snodgrass JJ, Martinez CR Jr., Squires EC, Jiménez RA, Isiordia LE, Small J, 2015. Stress, place, and allostatic load among Mexican immigrant farmworkers in Oregon. J. Immigr. Minor. Health 17, 1518–1525. 10.1007/s10903-014-0066-z. [DOI] [PubMed] [Google Scholar]
- McEwen BS, 1998a. Protective and damaging effects of stress mediators. N. Engl. J. Med. 338 (3), 171–179. 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McEwen BS, 1998b. Stress, adaptation, and disease: allostasis and allostatic load. Ann. N. Y. Acad. Sci. 840 (1), 33–44. 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS, 2007. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol. Rev 87, 873–904. 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- Mendoza MM, Dmitrieva J, Perreira KM, Hurwich-Reiss E, Watamura SE, 2017. The effects of economic and sociocultural stressors on the well-being of children of Latino immigrants living in poverty. Cult. Divers Ethn. Minor Psychol 23 (1), 15–26. 10.1037/cdp0000111.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metz S, Duesenberg M, Hellmann-Regen J, Wolf OT, Roepke S, Otte C, Wingenfeld K, 2020. Blunted salivary cortisol response to psychosocial stress in women with posttraumatic stress disorder. J. Psychiatr. Res 130, 112–119. 10.1016/j.jpsychires.2020.07.014. [DOI] [PubMed] [Google Scholar]
- Nabipour I, Cumming R, Handelsman DJ, Litchfield M, Naganathan V, Waite L, Seibel MJ, 2011. Socioeconomic status and bone health in community-dwelling older men: the CHAMP Study. Osteoporos. Int 22, 1343–1353. 10.1007/s00198-010-1332-0. [DOI] [PubMed] [Google Scholar]
- Ng J-S, Chin K-Y, 2021. Potential mechanisms linking psychological stress to bone health. Int. J. Med. Sci 18 (3), 604–614. 10.7150/ijms.50680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen A-MD, Benet-Martínez V, 2007. Biculturalism unpacked: components, measurement, individual differences, and outcomes. Soc. Personal. Psychol. Compass 1 (1), 101–114. 10.1111/j.1751-9004.2007.00029.x. [DOI] [Google Scholar]
- Nicholson LM, Miller AM, Schwertz D, Sorokin O, 2013. Gender differences in acculturation, stress, and salivary cortisol response among former soviet immigrants. J. Immigr. Minor. Health 15, 540–552. 10.1007/s10903-012-9752-x. [DOI] [PubMed] [Google Scholar]
- Niño MD, Hearne BN, 2020. Dimensions of acculturation and biological dysregulation among Latina/os: the role of ethnic background, gender, and immigrant generation. Ethn. Health 1–17. 10.1080/13557858.2020.1821175. [DOI] [PubMed] [Google Scholar]
- Ouyang W, Rutz S, Crellin NK, Valdez PA, Hymowitz SG, 2011. Regulation and functions of the IL-10 family of cytokines in inflammation and disease. Annu Rev. Immunol. 29, 71–109. [DOI] [PubMed] [Google Scholar]
- Peek MK, Cutchin MP, Salinas JJ, Sheffield KM, Eschbach K, Stowe RP, Goodwin JS, 2010. Allostatic load among non-Hispanic Whites, non-Hispanic Blacks, and people of Mexican origin: effects of Ethnicity, Nativity, and Acculturation. Am. J. Public Health 100 (5), 940–946. 10.2105/AJPH.2007.129312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce BL, Austin MA, Crane PK, Retzlaff BM, Fish B, Hutter CM, Fujimoto WY, 2007. Measuring dietary acculturation in Japanese Americans with the use of confirmatory factor analysis of food-frequency data. Am. J. Clin. Nutr 86 (2), 496–503. 10.1093/ajcn/86.2.496. [DOI] [PubMed] [Google Scholar]
- Prather AA, Carroll JE, Fury JM, McDade KK, Ross D, Marsland AL, 2009. Gender differences in stimulated cytokine production following acute psychological stress. Brain Behav. Immun 23 (5), 622–628. 10.1016/j.bbi.2008.11.004.Gender. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Y, Yang B, Telzer EH, 2020. The cost of academic focus: daily school problems and biopsychological adjustment in Chinese American families. J. Youth Adolesc 49, 1631–1644. 10.1007/s10964-020-01255-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riosmena F, Wong R, Palloni A, 2013. Migration selection, protection, and acculturation in health: a binational perspective on older adults. Demography 50 (3), 1039–1064. 10.1007/s13524-012-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez F, Peralta CA, Green AR, López L, 2012. Comparison of C-reactive protein levels in less versus more acculturated Hispanic adults in the United States (from the National Health and Nutrition Examination Survey 1999–2008). Am. J. Cardiol 109 (5), 665–669. 10.1016/j.amjcard.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriquez EJ, Gregorich SE, Livaudais-Toman J, Pérez-Stable EJ, 2017. Coping With chronic stress by unhealthy behaviors: a re- evaluation among older adults by race/ethnicity. J. Aging Health 29 (5), 805–825. 10.1177/0898264316645548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg N, Daviglus ML, DeVon HA, Park CG, Eldeirawi K, 2017. The association between parity and inflammation among Mexican-American women of reproductive age varies by acculturation level: results of the National Health and Nutrition Examination Survey (1999–2006). Women’s. Health Issues 27 (4), 485–492. 10.1016/j.physbeh.2017.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal T, 2018. Immigration and acculturation: impact on health and well-being of immigrants. Curr. Hypertens. Rep. 20, 70. 10.1007/s11906-018-0872-0. [DOI] [PubMed] [Google Scholar]
- Ruiz RJ, Dolbier CL, Fleschler R, 2006. The relationships among acculturation, biobehavioral risk, stress, corticotropin-releasing hormone, and poor birth outcomes in Hispanic women. Ethn. Dis 16 (4), 926–932. [PubMed] [Google Scholar]
- Ruiz RJ, Stowe RP, Goluszko E, Clark MC, Tan A, 2007. The relationships among acculturation, body mass index, depression, and interleukin 1-receptor antagonist in Hispanic pregnant women. Ethn. Dis 17, 338–343. [PubMed] [Google Scholar]
- Ruiz RJ, Marti CN, Pickler R, Murphey C, Wommack J, Brown CEL, 2012. Acculturation, depressive symptoms, estriol, progesterone, and preterm birth in Hispanic women. Arch. Women’s Ment. Health 15 (1), 57–67. 10.1007/s00737-012-0258-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz RJ, Pickler RH, Marti CN, Jallo N, 2013. Family cohesion, acculturation, maternal cortisol, and preterm birth in Mexican-American women. Int. J. Women’s Health 5, 243–252. 10.2147/IJWH.S42268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sam DL, 2006. Acculturation: conceptual background and core components. In: Sam DL, Berry JW (Eds.), The Cambridge Handbook of Acculturation Psychology. Cambridge University Press, Cambridge, pp. 11–26. [Google Scholar]
- Santiago-Torres M, Kratz M, Lampe JW, Tapsoba JDD, Breymeyer KL, Levy L, Neuhouser ML, 2016. Metabolic responses to a traditional Mexican diet compared with a commonly consumed US diet in women of Mexican descent: a randomized crossover feeding trial. Am. J. Clin. Nutr 103 (2), 366–374. 10.3945/ajcn.115.119016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholaske L, Buss C, Wadhwa PD, Entringer S, 2018. Acculturation and interleukin (IL)-6 concentrations across pregnancy among Mexican-American women. Brain Behav. Immun 73, 731–735. 10.1016/J.BBI.2018.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R, Smith JI, Shen X, Engel PJ, Bowman ME, McGrath SA, Smith DW, 2009. Patterns of plasma corticotropin-releasing hormone, progesterone, estradiol, and estriol change and the onset of human labor. Endocr. Care 94 (6), 2066–2074. 10.1210/jc.2008-2257. [DOI] [PubMed] [Google Scholar]
- Steffen PR, Walker J, Meredith R, Anderson C, 2016. The effects of job instability and financial strain on c-reactive protein in a sample of Mexican immigrants. Ethn. Dis 26 (1), 37–44. 10.18865/ed.26.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Hamer M, Chida Y, 2007. The effects of acute psychological stress on circulating inflammatory factors in humans: a review and meta-analysis. Brain, Behav. Immun 21, 901–912. 10.1016/j.bbi.2007.03.011. [DOI] [PubMed] [Google Scholar]
- The Lancet Public Health, 2018. No public health without migrant health. Lancet Public Health 3 (6), 259. 10.1016/S2468-2667(18)30101-4. [DOI] [PubMed] [Google Scholar]
- Todorova ILG, Tucker KL, Jimenez MP, Lincoln AK, Arevalo S, Falcón LM, 2013. Determinants of self-rated health and the role of acculturation: implications for health inequalities. Ethn. Health 18 (6), 563–585. 10.1080/13557858.2013.771147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres L, Mata-Greve F, Harkins AL, 2018. A preliminary investigation of acculturative stress and diurnal cortisol among latina women. J. Lat. /o Psychol 6 (2), 149–158. [Google Scholar]
- Tricco AC, Lillie E, Zarin W, Brien KKO, Colquhoun H, Levac D, Straus SE, 2018. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med 169 (7), 467–473. 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Vanitallie TB, 2002. Stress: a risk factor for serious illness. Metabolism 51 (6), S40–S45. 10.1053/meta.2002.33191. [DOI] [PubMed] [Google Scholar]
- Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB, 1999. Elevated C-reactive protein levels in overweight and obese adults. JAMA 282 (22), 2131–2135. [DOI] [PubMed] [Google Scholar]
- Wang S, Lau AS, 2018. Ethnicity moderates the benefits of perceived support and emotional expressivity on stress reactivity for asian americans and euro americans. Cult. Divers. Ethn. Minor. Psychol 24 (3), 363–373. 10.1037/cdp0000197. [DOI] [PubMed] [Google Scholar]
- Wommack JC, Ruiz RJ, Marti CN, Stowe RP, Brown CEL, Murphey C, 2013. Interleukin-10 predicts preterm birth in acculturated Hispanics. Biol. Res. Nurs 15 (1), 78–85. 10.1177/1099800411416225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Berry DC, Schwartz TA, 2019. Weight stigma and acculturation in relation to hair cortisol among Asian Americans with overweight and obesity: a cross-sectional study. Health Psychol. Open 1–13. 10.1177/2055102919829275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim IS, Corona K, Garcia ER, Acevedo AM, Campos B, 2019. Perceived stress and cortisol reactivity among immigrants to the United States: the importance of bicultural identity integration. Psychoneuroendocrinology 107, 201–207. 10.1016/j.psyneuen.2019.05.021. [DOI] [PubMed] [Google Scholar]
- Yoon E, Chang C-T, Kim A, S. C, Cleary SE, Hansen M, Gomes AM, 2013. A meta-analysis of acculturation/enculturation and mental health. J. Couns. Psychol. 60 (1), 15–30. 10.1037/a0030652. [DOI] [PubMed] [Google Scholar]
- Zeiders KH, Doane LD, Roosa MW, 2012. Perceived discrimination and diurnal cortisol: examining relations among Mexican American adolescents. Horm. Behav 61 (4), 541–548. 10.1016/j.yhbeh.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiders KH, Causadias JM, White RMB, 2018. The health correlates of culture: examining the association between ethnic-racial identity and diurnal cortisol slopes. J. Adolesc. Health 62 (3), 349–351. 10.1016/j.jadohealth.2017.09.020. [DOI] [PubMed] [Google Scholar]