Abstract
This paper analyses the health policy response to the COVID-19 pandemic in the four Visegrad countries – Czechia, Hungary, Poland, and Slovakia – in spring and summer 2020. The four countries implemented harsh transmission prevention measures at the beginning of the pandemic and managed to effectively avoid the first wave of infections during spring. Likewise, all four relaxed most of these measures during the summer and experienced uncontrolled growth of cases since September 2020. Along the way, there has been an erosion of public support for the government measures. This was mainly due to economic considerations taking precedent but also likely due to diminished trust in the government. All four countries have been overly reliant on their relatively high bed capacity, which they managed to further increase at the cost of elective treatments, but this could not always be supported with sufficient health workforce capacity. Finally, none of the four countries developed effective find, test, trace, isolate and support systems over the summer despite having relaxed most of the transmission protection measures since late spring. This left the countries ill-prepared for the rise in the number of COVID-19 infections they have been experiencing since autumn 2020.
1. Introduction
The Visegrad Group (V4) was formed in 1991 by the heads of the Czechoslovak Republic, now Czechia and Slovakia, Hungary and Poland. The formation of the Group was motivated by the common desire to eliminate the remnants of communism and to successfully accomplish social transformation and join in the European integration process [7]. It was supported by the geographic proximity of the signatory countries but also by their shared history and cultural and political similarities. The intensity of the cooperation, governed by means of rotating presidencies and frequent meetings at presidential and ministerial levels, decreased since the early years, and the European Union (EU) became the main platform for cooperation amongst the four countries.
All four countries started the transformation with highly centralized, Semashko-style health care systems inherited from the communist era and swiftly adopted or reintroduced social health insurance in the first half of 1990s. Common legacies from the Semashko era that are discernible to this day include excess capacity in the inpatient care sector (Table 1 ), inequitable regional distribution and/or low quality of care, with which the four countries have grappled with varying success. These problems have been aggravated by the emigration of the health workforce, especially after the EU accession in 2004.
Table 1.
Selected demographic, socioeconomic and health sector indicators, 2019 or latest available year.
| Czechia | Hungary | Poland | Slovakia | EU | |
|---|---|---|---|---|---|
| Demographic factors | |||||
| Population (million) | 10.6 | 9.8 | 38 | 5.4 | 512 |
| Share of population over age 65 (%) | 18.8 | 18.7 | 16.5 | 15.0 | 19.4 |
| Life expectancy | 79.1 | 76.0 | 77.8 | 77.3 | 80.9 |
| Socioeconomic factors | |||||
| GDP per capita (EUR PPP) | 26,900 | 20,300 | 20,900 | 22,900 | 30,000 |
| Relative poverty rate (%) | 9.1 | 13.4 | 15.0 | 12.4 | 16.9 |
| Unemployment rate | 2.9 | 4.2 | 4.9 | 8.1 | 7.6 |
| Health resources | |||||
| Health spending as a share of GDP (%) | 7.1 | 7.4 | 6.5 | 7.1 | 9.9 |
| OOP spending as a share of total health spending (%) | 15 | 30 | 23 | 18 | 16 |
| Hospital beds per 1000 people | 6.9 | 7.0 | 6.6 | 5.8 | 5.1 |
| Practicing doctors per 1000 people | 3.7 | 3.2 | 2.4 | 3.5 | 3.6 |
| Practicing nurses per 1000 people | 8.1 | 6.4 | 5.1 | 5.7 | 8.4 |
With increasing incomes, health spending has also increased in all four countries, both as a share of GDP and in per capita terms. However, this trend was interrupted by the global financial crisis of 2008, especially in Hungary, which had previously also experienced a fiscal crisis in the early 2000s. Despite the increases, health spending remains lower than the EU average in all four countries.
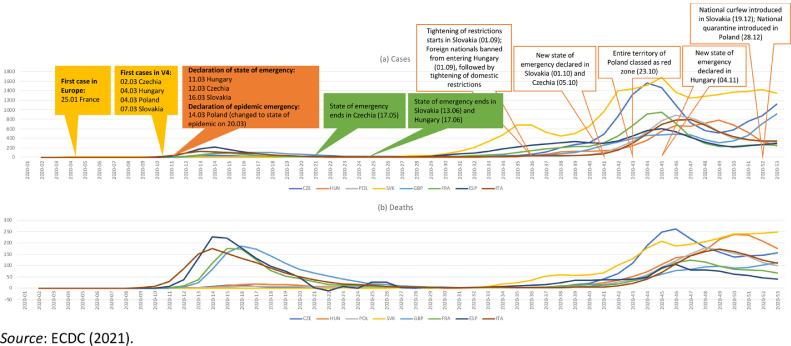
The novel coronavirus reached the V4 countries in early March 2020, over a month after the first recorded case of COVID-19 in Europe (Fig. 1 ). By that time, transmission was exponentially accelerating in several countries in Western Europe, with the number of new cases in Italy already surpassing 700 per day [3]. When the first cases appeared within their national borders, the Visegrad countries acted quickly and decisively, implementing severe restrictions to limit transmission and effectively putting their entire populations under ‘lockdown’. Likely thanks to these protective measures, relatively few cases and deaths were recorded in the V4 countries during spring 2020: by the end of April, 22 COVID-19 deaths were recorded in Slovakia, 227 in Czechia, 312 in Hungary and 624 in Poland (the most populous country in the V4 group) [3]. Given the favourable epidemiological situation and increasingly negative public sentiment against the restrictions, the harsh measures were largely relaxed since late spring and few protective measures were in place over the summer. Hospital capacity that was freed up for treating potential COVID-19 patients was reduced and provision of care was reoriented towards non-COVID-19 patients. At the same time, governments were reluctant to introduce measures even in the face of a rising number of cases. This left the V4 countries ill-prepared for the autumn 2020, when the number of cases rose sharply, quickly surpassing the peak numbers from spring by multiple times.
Fig. 1.
14-day notification rate of new COVID-19 cases and deaths per 100,000 people in the Visegrad and selected other countries, 2020. Source: Authors based on COVID-19 HSRM and ECDC [3].
The aim of this article is to analyse the evolution of the policy responses to COVID-19 in the Visegrad countries between March and August 2020 in a comparative manner, distil similarities and offer lessons for policy makers. As appropriate, comments on key developments up until the end of 2020 are also included.
2. Methods
This analysis builds on the methodology and content compiled in the COVID-19 Health System Response Monitor (HSRM), where information on how health systems in the WHO European Region have been responding to the COVID-19 outbreak has been systematically collected since March 2020 (see www.covid19healthsystem.org). It is a joint initiative by the European Observatory on Health Systems and Policies, the WHO Regional Office for Europe and the European Commission.
The HSRM content is structured broadly around the standard health system functions [27], capturing information on policy responses related to governance, resource generation, financing, and service delivery. In addition, the HSRM also includes policy responses that aim specifically to prevent transmission of the virus and other non-health system measures. The information is collected and regularly updated by way of an evolving set of questions that serve as prompts for the country health policy experts contributing to the platform. By following a structured questionnaire and having a team of Observatory staff editing the responses, information is collected in a way that enables broad comparisons across countries.
The identification of key policy insights from country experiences followed a deliberative process that included extensive review of the HSRM materials and structured discussions amongst article co-authors, Observatory editors, and other experts. Where relevant, other country material, key documents and literature are used to inform the paper.
The analysis focuses on the following three topics, which are the main areas of similarities in the COVID-19 response amongst the four countries:
-
•
Governance, which relates to the planning of the pandemic response, including the role of scientific advice, and the steering of the health system to ensure its continued functioning. Information is predominantly drawn from Section 5 in the HSRM profiles of the four countries.
-
•
Transmission prevention (Section 1 in the HSRM profiles), which includes measures put in place to test and identify cases and trace contacts.
-
•
Physical infrastructure and workforce capacity (Section 2 in the HSRM profiles), which describes pre-existing availability of physical and human resources as well as measures in place to surge them during the initial stages of the pandemic.
3. Results
With a few notable exceptions, the comparative analysis of the four countries has identified six main areas of similarities in the COVID-19 responses of the V4 countries. These findings relate to (1) the centralization of governance, (2) the role of scientific advice, (3) the prevention of the transmission with movement restrictions, (4) the scaling up of capacities, (5) the shortage of human resources, and (6) the shortcomings of the Find, Test, Trace, Isolate and Support (FTTIS) systems. The related findings are described in detail in the following sections.
Governance of the COVID-19 response has been highly centralized
Compared to many countries in western Europe, the Visegrad countries were very quick to react once the first cases of COVID-19 were detected within their national borders. The responses started with the declarations of the states of emergency, which gave the governments extraordinary powers to fight the pandemic. This took place on the 11th of March in Hungary, on the 12th of March in Czechia and on the 16th of March in Slovakia – almost immediately after the first cases of COVID- 19 were reported in these countries and soon after severe movement restrictions were introduced in affected areas in Italy (9th of March) (Fig. 1). The states of emergency were recalled after about two months in Czechia and a month later in Slovakia and Hungary.
Unlike the other three countries, Poland refrained from declaring a state of emergency, but instead opted for introducing a state of ‘epidemic emergency’ on the 14th of March, followed by the declaration of the ‘state of epidemic’ on the 20th of March. Ever since, there has been a heated debate on whether the government should have declared a state of emergency instead (no such debates occurred in Czechia, Hungary, and Slovakia, although there were some discussions about the duration of the implemented emergency measures). Imposition of a state of emergency would have introduced ready-made legal solutions provided for in the Constitution and existing legal acts to introduce severe but precisely delineated restrictions of civil rights as well as special powers to fight the pandemic. These special powers include, amongst others, the ability to use of the police and army to supress unrest; suspend the heads of the local self-government and replace them with special commissioners if they do not perform their duties; isolate individuals who threaten the ‘public order’, and censor public media. Under the current ‘state of epidemic’, this is done via enacting special resolutions and provisions – an approach that risks violating the Constitution and other laws. There are three key reasons why the government may have found this solution to be preferable. Declaration of a state of epidemic instead of a state of emergency meant that: (1) presidential elections, scheduled on the 10th of May, could go ahead as planned; (2) the government was not obligated to compensate the citizens for any economic losses caused by the introduced restrictions; and (3) the government was not obligated to coordinate the response with the local self-government, with the municipalities, counties and voivodeships effectively managing the response in their local areas [25]. Unlike the state of emergency, the duration of a state of epidemic is not limited in time and it has remained in place since its introduction at the end of March.
Czechia, Hungary, and Slovakia had pre-existing national response plans for pandemic influenza, but they had little applicability to the new coronavirus (and in some cases were also outdated), they were either outright abandoned (Czechia), very loosely followed (Slovakia) or substantially overhauled to reflect the specificities of COVID-19 (Hungary). Poland's response followed the 2008 Infectious Diseases Act, which determines the functioning of public authorities during an infectious disease outbreak. A dedicated COVID-19 response strategy was released in September 2020 [16].
In all four countries, COVID-19 response was led by the central government, with involvement of the relevant ministries, including the ministry responsible for health. The response was coordinated through the offices of the Prime Minister with the support of dedicated crisis management bodies (Table 2 ). These were intersectoral and included representatives of key ministries and national agencies. When the epidemiological situation improved, these bodies were either dismantled or reduced their level of activity. For example, in Czechia, the Central Crises Staff was deactivated in early summer when the threat of COVID-19 appeared to be under control and reactivated in late September 2020; and the COVID-19 Central Management team was initially established as an advisory body to the government but then became an advisory body to the Ministry of Health in early summer (2020).
Table 2.
Overview of the national governance of COVID-19 response, spring and summer 2020
| Czechia | Hungary | Poland | Slovakia |
|---|---|---|---|
| Head of country emergency response | |||
| Prime Minister | Prime Minister | Prime Minister | Prime Minister |
| Authority for country emergency response | |||
| • Central Crises Staff led by the Minister of Interior (over the summer the response was led by the Governmental Committee for Health Risks) | • Operative Corps led by Minister of Interior and Minister of Human Capacities | • Government Crisis Management Team led by the Prime Minister | • Central Crisis Management Group led by Minister of Interior (in practice by the Prime Minister) |
| Head of health system response | |||
| Minister of Health | Minister of Human Capacities | Minister of Health | Minister of Health |
| Authority for health system emergency response | |||
| COVID-19 Central Management Team | COVID-19 Management Team at the Ministry of Human Capacities | Crisis Management Team at the Ministry of Health | Internal Crisis Management Group at the Ministry of Health |
| Representatives of authority for health system emergency response | |||
| • Ministries/ government: | • Ministry: | • Ministries/ government: | • Ministries/ government: |
| o Ministry of Health | • State Secretary for Health, State Secretary for Social Affairs | o Ministry of Defence | o All ministries |
| o Chief Public Health Officer | • Undersecretaries of State of the State Secretariat for Health | Ministry of the Interior | o Communication and crisis officers of ministries of health and interior affairs |
| o Ministry of Defence | • National agencies: | o Ministry of Foreign Affairs | o Self-governing regions |
| o Ministry of Interior | • National Chief Medical Officer / National Public Health Centre | o Special Forces Coordinator | • Experts: |
| o Government IT Commissioner | • National Healthcare Service Centre | • National agencies: | o Chief public health officer |
| o Regions’ Association | • Providers: | o National Institute of Public Health | o Representatives of health insurance companies |
| • National agencies: | • National Emergency Ambulance Service | o State Sanitary Inspectorate | o Chief expert for infectious diseases |
| o General Health Insurance Fund | • Directors of selected* hospitals | o Chief expert for epidemiology | |
| • Other: | Experts: | o Head of Slovak academy of science | |
| o Army | • Anaesthesiologist, artificial ventilation expert | ||
| o Police | |||
| o Fire service | |||
| COVID-19 scientific advisors | |||
| • Chief Public Health Officer | • National Chief Medical Officer and other experts of the National Public Health Center | • Team for COVID-19 strategic response planning at the Ministry of Health (est. in July), incl. representatives of the National Institute of Public Health, State Sanitary Inspectorate, Chief Statistical Office, national health technology assessment agency (AOTMiT), E-Health Centre | • Expert group chosen by the Prime Minister, incl. top experts on epidemiology, virology, infectiology and related areas |
| • Institute for Health Information and Statistics (subordinated to the Ministry of Health) | • Head of the Infectious Diseases Department of Southern Pest Centre Hospital | • Team for COVID-19 monitoring and forecasting (est. in September) | |
| • Ministry of Health's Laboratory Expert Committee (advising on testing matters) | • University researchers | ||
| • Economic team of the Central Crises Staff (advising on economic matters) | |||
| Pre-existing pandemic emergency legislation or plans | |||
| • 2011 Czech pandemic plan (mainly focusing on influenza) | • 2009 National pandemic response plan for pandemic influenza | • 2008 Infectious Diseases Act | • 2005 National pandemic plan for pandemic influenza |
Notes: * The National Korányi Institute of Tuberculosis and Pulmonology and the Southern Pest Centre Hospital, which were the two primary COVID-19 hospitals, treating all COVID-19 patients during the first wave.
Source: Authors based on COVID-19 HSRM.
The role of scientific advice in decision-making varied across the four countries but in all four its importance has diminished from late spring
The national responses to the COVID-19 pandemic were underpinned by scientific advice in all four countries (Table 2). However, the various advisory bodies that were established to guide the response planning mainly involved representatives of different state authorities, with independent scientists playing a relatively minor role, particularly in Czechia and Poland, at least initially. At a minimum, scientific advice involved the chief public health or medical officers, as in the case of Czechia, where no independent scientific experts were involved in spring 2020. Similarly, Poland only included national agencies. None of the V4 countries documented involvement of non-governmental stakeholders, such as community representatives, in the response planning.
Hungary and Slovakia had relatively greater involvement of independent scientific experts at the start of the response. In Hungary, experts from various areas, including epidemiology, virology, infectiology, mathematics, data analysis and modelling, were actively involved in supporting the government during the first wave in spring 2020, including planning and later relaxing the restrictions. In Slovakia, an expert group comprising top experts in epidemiology, virology, infectiology and related areas, was established at the beginning of the pandemic to provide advice to the Prime Minister and the Internal Crisis Management Group at the Ministry of Health. Their work mainly focused on how to ease the restrictions introduced in early March (see Table A1 in the Online Appendix).
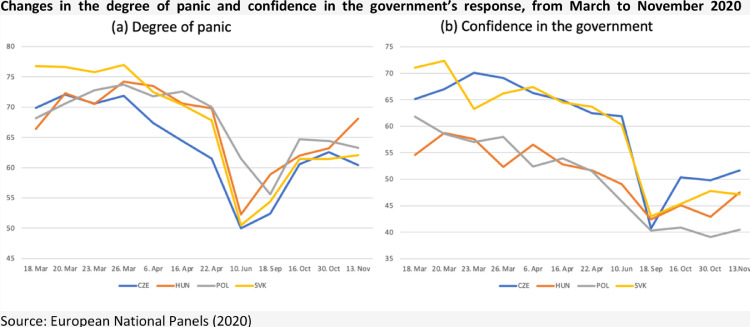
In all four countries, the influence of independent scientific experts diminished by late summer, with their advice often overridden by other, mainly economic and political considerations. With few COVID-19 deaths and low infection rates (Fig. 1) and drastically worsening GDP forecasts [18], [19], [20], public support for the restrictions had fallen (Fig. 2 ). Although the unemployment rates did not rise dramatically, the four governments were anxious to protect their economies and avoid further restrictions [2].
Fig. 2.
Changes in the public attitude towards the pandemic and implemented measures in the Visegrad countries, March to November 2020. Initial COVID-19 responses involved drastic restrictions of movement into and within the countries, but these were largely relaxed, and few protective measures were maintained over the summer [5].
Further, the relatively good epidemiological situation (see for example [14]) made the population optimistic or even complacent that the pandemic was under control. The ‘end of the pandemic’ mass dinner held on Prague's Charles Bridge on June 30, 2020, epitomizes this feeling, where thousands shared food and drink that they had brought [2]. In Poland, the (false) sense of optimism was fuelled by top politicians rallying the population and especially older people – the key electoral base of the incumbent president - to vote in the presidential election in July. Public stance towards the restrictions was likely further affected by the instances of high-level public officials breaking the restrictions, e.g., not wearing face coverings in public places or breaking visitation bans in the hospitals, and cases of flagrant corruption publicised by the national press. Governments in Poland and Hungary appear to also have used the COVID-19 crisis to push controversial legislation and strengthen their grip on power [15]. In Poland, the parliament moved forward a controversial act restricting abortion, which has led to large public protests. It has also continued with its efforts to assert further control over the judicial system. In Hungary, at the end of March the parliament passed a bill that allowed imprisonment for publishing false or distorted facts. Although the parliament rescinded these powers in June, there are still concerns that the government now holds greater power than before the crisis.
Overall, the V4 governments appeared to be reluctant to re-impose any restrictions, even if these were favoured by the scientific experts, including when infection rates started increasing at the end of the summer. For example, the Czech Prime Minister blocked the Health Minister's plan to reintroduce facemasks indoors from the 1st of September, ascribing the decision to ‘high societal demand’ for no restrictions and ‘low infectiousness of the virus at that time’ [6]. Proximity to the regional councils’ elections, scheduled for 2nd −3rd October 2020, may have played a role in that decision [2]. A similar situation occurred in Slovakia in early October, when the Prime Minister explicitly rejected expert recommendations and increased the number of guests allowed at weddings [28].
Declarations of the states of emergency (and the state of ‘epidemic emergency’ in Poland) enabled the V4 countries to introduce measures to prevent transmission of the novel coronavirus to and within their countries that severely affected civil liberties of their citizens. Measures introduced in the four countries were broadly similar. An overview of the measures introduced in Slovakia is presented in Table A1 in the Online Appendix.
The V4 countries were amongst the first countries in Europe to close their national borders. The Czech government limited cross-border travels starting on the 16th of March, with general border closures implemented on the 31st of March. Czech citizens were not allowed to leave the country and foreigners were not allowed to enter, except for permanent residents and holders of temporary residence permits. Everyone entering the country had to quarantine for 14 days after entry. Similar border restrictions were introduced in Hungary (with the first limitations introduced already on the 11th of March), Poland and Slovakia.
Czechia and Slovakia were the only countries in Europe that made masque-wearing mandatory from the start of the pandemic, introducing this obligation within a few weeks since the first cases were recorded. This policy was thought to be a major factor in the early success in controlling the virus in both countries. The obligation to use face coverings was also introduced in Poland and Hungary but only about a month later. Further measures to limit community transmission included physical distancing requirements, restrictions on public gatherings, closures of educational facilities (Czechia was amongst the countries in Europe where schools were shut the longest in 2020) and non-essential businesses as well as curfews and other limitations of the free movement of people. In combination, these measures amounted to what was termed as ‘national lockdowns’ and were associated with significant reduction in contacts.
Most of the restrictions were relaxed before the start of the summer. This usually happened in several stages. In Czechia, for example, a 5-stage plan to relax restrictions was announced on the 14th of April and stage 1 commenced on the 20th of April. However, a new version of the plan was released three days later, on the 23rd of April, to ease restrictions more quickly. This was likely motivated by the improved epidemiological situation but probably also due to the Prague City Court's annulment, at the end of April, of restrictive measures implemented in response to the pandemic (although this order was later overturned by the Supreme Administrative Court in early 2021), and further lawsuits questioning the legality of measures taken by the government. Easing of restrictions was also sped up in Slovakia, with final restrictions eased by the beginning of July (Table A1 in the Online Appendix). In Poland and Hungary, where staged easing plans were also implemented, final stages of easing restrictions started in early to mid-May.
In all four countries, few protective measures remained in effect over the summer. In Czechia, the mandatory requirement on wearing face masks was withdrawn in June, with some exceptions. Other restrictions, such as on physical distancing, were relaxed too and mass gatherings of up to 1000 people (or even more in certain conditions) were allowed throughout the summer. In Slovakia, where the use of face coverings was also mandated early into the pandemic, this obligation was retained in indoor places during the summer, but it was abolished outdoors. In Hungary and Poland individuals were required to continue wearing face masks in shops and on public transport and maintain safe physical distance during the summer. However, other restrictions, such as on public gatherings and travel restrictions, have been relaxed and business and social life largely resumed in summer 2020.
Measures were taken to ensure adequate hospital capacity to treat COVID-19 patients, but this capacity was underutilized in the spring and was reduced over the summer
Alongside measures to prevent transmission of the virus, the V4 countries took steps to ensure sufficient treatment capacity for prospective COVID-19 patients. For many years seen as a source of inefficiency, the relatively high number of hospital beds in the V4 countries (see Table 1) became an asset during the pandemic and initial efforts to ensure sufficient treatment capacity centred around hospital care.
In all four countries, additional bed capacity for treating COVID-19 patients was secured in spring 2020 by suspending all elective care. No further measures to increase capacity were introduced in Czechia, where the Ministry of Health estimated that the health system could absorb up to 30,000 confirmed COVID-19 cases. This was based on the Ministry of Health's assumption that 10% of confirmed cases (i.e., 3000 people) would require hospitalization. While a contingency plan for repurposing standard hospital beds as ICU beds was prepared, it was not implemented in spring 2020 due to very low case numbers (see Fig. 1). In Slovakia, simulation models produced by the Institute of Health Policies at the Health Ministry at the end of March forecasted that between 1800 and 2200 beds would be needed for COVID-19 patients, out of which approximately 600 would require ventilation. The models’ worst-case scenarios predicted that these capacities would be filled around the end of May but since the epidemiological situation remained good, no further measures besides procuring additional ventilators (see below) were taken to increase hospital capacity.
More preparations were undertaken in Poland and Hungary to secure bed capacity for COVID-19 patients in spring 2020. In Poland, measures included designating hospital departments or entire hospitals for sole use by COVID-19 patients. A total of 22 hospitals, at least one in each voivodeship, were transformed into such single-infection hospitals, securing a total of 10,000 beds. Other measures included repurposing of existing facilities, e.g., hospital wards were fitted with physical barriers and otherwise adapted to keep patients apart and a percentage (the target was 10% of the total) of mechanical ventilation were designated beds for treatment of COVID-19 patients.
Much more was done in Hungary (see Figure A1 in the Online Appendix), where the Minister for Human Capacities ordered hospitals to vacate 60% of the total bed capacity (39,500 beds) by the 15th of April. This was later revised by an official announcement, published on the government's COVID-19 website on the 15th of April, requiring that 50% of the total hospital bed capacity (i.e., 32,900 beds) be freed up for COVID-19 patients by the 19th of April [17]. If needed, this share was meant to increase back to 60%. The estimates were based on the epidemic modelling produced by an expert team at the Ministry of Human Capacities, which, drawing on data from the most affected parts of the USA and Italy, predicted 3.4 million infections by May 2020 as the best-case scenario. In contrast, experts from the Ministry of Innovation and Technology predicted 200–300 thousand cases by October 2020, assuming a 50% reduction of physical contacts [17] and in fact physical contacts have fallen by over 60% thanks to the national lockdown. As a preparation for the acceleration of the infection rate, hospitals were required to report data on key human and other resources and secure bed capacity for COVID-19 patients by relocating existing patients. However, some hospital directors did not agree that the epidemiological situation justified securing such large numbers of beds for COVID-19 patients and did not comply with the preparatory measures. This led to directors of two hospitals, the Fejér County Hospital and the National Institute of Medical Rehabilitation, being removed from their posts in mid-April by the Minister for Human Capacities [1], [11]. As the epidemiological situation improved in late spring 2020, most measures aimed at securing hospital capacity were rolled back and providers started focusing on reducing the backlog of elective care. In Czechia, this was explicitly encouraged through financial incentives.
The availability of equipment, such as personal protective equipment (PPE) and ventilators, was initially limited but stocks were built up quickly, mainly by centralized procurement from abroad. However, in some cases this lacked transparency and several high-profile cases of corruption were brought to the light by the press in Poland [9], [10], [13] and Slovakia [12], likely contributing to the deterioration of public trust in the state response (see Fig. 2). Material stocks were also built up by home production (e.g., hand sanitizers in Czechia) and banning exports of needed equipment (e.g., of ventilators in Poland), or potential drugs (e.g., hydroxychloroquine in Hungary; [26]). Populations were also encouraged to make their own face coverings and public response to this call was very positive in general, especially in Czechia and Slovakia where masque-wearing was mandatory from the start of the pandemic but the governments in these countries did not provide masks to the population and instead relied on the initiative of ordinary citizens to make them. In Poland, private companies provided material support by, amongst others, donating cleaning and disinfectant products to hospitals or providing free courier services to help deliver supplies of PPE.
To support home production of needed equipment and materials, the approval process for development, production and licensing of new drugs, medical devices and aids associated with treating the COVID-19 infection was accelerated. In Czechia, this benefited the development and production of facial respirators using nanotechnologies and a new type of emergency lung ventilator designed for COVID-19 patients with respiratory failures. New types of ventilators, especially designed for COVID-19 patients, as well as for parallel ventilation of up to 50 patients, were also developed in Hungary with funding from the government. The first prototypes were ready by end of March 2020, and after the clinical trials, the production has started from the end of May. In Slovakia, the existing national producer of ventilators increased its production allowing the government to secure a sufficient stock. While the medicines approval processes have not been accelerated in Slovakia, the Slovak medicines agency prioritised all applications related to the treatment of COVID-19.
Strategies to increase hospital capacity were supported by measures to secure human resources
Efforts to increase capacity of hospital beds had to be supported by ensuring sufficient numbers of medical staff, which has been especially challenging due to the already existing shortages and, in Poland and Hungary, by the removal of health professionals over the age of 65 from direct patient care. During the early stage of the pandemic, measures to maintain the capacity of the existing professional workforce included asking health professionals to work extra hours; cancelling leaves of absence; suspending limitations on night shifts and on-call duties; prohibition of leaving the country; and automatically extending the operating licences of practicing health professionals. In Poland, health workers were also redeployed to work in other settings, e.g., in infectious diseases departments or in other settings where help was needed. In Poland and Hungary, older workers were moved from face-to-face consultations to answer helplines or provide teleconsultations. In all four countries, health workers involved in the COVID-19 response received some form of support, usually financial (e.g., bonuses) but also material (e.g., free childcare, free public transportation, free hotel accommodation) and psychological (e.g., via dedicated helplines).
To increase capacity, volunteering amongst final year medical and nursing students was encouraged in all four countries. Final year students in Poland were allowed to perform support roles, such as conducting epidemiological interviews. Poland has also simplified procedures to allow non-practicing nurses and midwives to return to work. Czechia has allowed physicians from outside the EU to practice without having passed the Czech specialization exam during the duration of the state of emergency in spring 2020. In October 2020, Czechia mandated medical students to work in the emergency response, if the epidemiological situation in the regions required this – it was the only country in Europe where contribution of medical students was not voluntary. These measures were not always enough. In Hungary, for example, excess ventilators had to be sold as there was not enough medical staff to operate them.
Not enough has been done to ensure adequate Find, Test, Trace, Isolate and Support systems ahead of the autumn wave
None of the four countries developed adequate Find, Test, Trace, Isolate and Support (FTTIS) systems over the summer to prepare for the expected surges in infection rates in the last quarter of the year. Already in the spring and summer 2020, notable weaknesses could be observed in sample collection and contact tracing. But these were not addressed, likely because there was no real need for it thanks to the favourable epidemiological situation, and other elements of the FTTIS systems were not developed either.
In Hungary and Slovakia, national emergency ambulance services were tasked with taking samples from suspected COVID-19 cases. In Czechia, sample collection was largely done in testing pods on the premises of hospitals and private laboratories, many with a drive-through option. By the end of June 2020, there were 87 sample collection points. Further, mobile teams (including army teams) were used to collect samples from people in quarantine, but their role decreased as the epidemiological situation improved since late spring. Drive-through testing points were also used in Poland and 180 such points were set up by the end of March throughout the country, with the total rising to 465 in early November 2020. In addition, first military drive-through points have been opened since early May. Furthermore, county sanitary stations used special ambulances (so-called ‘swab buses’) to collect samples from people in quarantine. Progressively, similar sample collection centres have been developed in Slovakia. From mid-October until the end of November, mass testing of the population was carried out in Slovakia in an attempt to prevent a second national lockdown (see Figure A2 in the Online Appendix). In Hungary, limited capacity was developed until late October, when the National Emergency Ambulance Service was tasked with training graduate medical and dental students who would staff the 200 newly created testing locations.
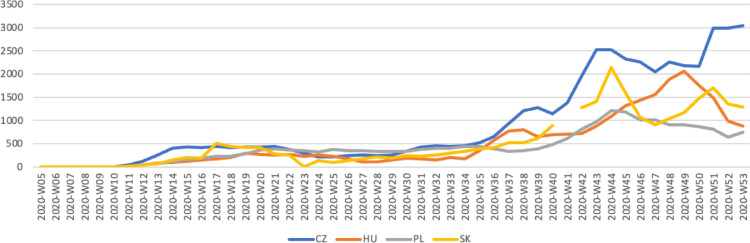
Laboratory testing capacity was adapted relatively quickly to the increasing demand, partly thanks to using private sector capacity. In Czechia, and Slovakia, prices of PCR tests were regulated and set relatively high, motivating private laboratories to increase their capacity. In contrast, the centrally regulated prices were set relatively low in Hungary and some private laboratories stopped providing diagnostics for PCR tests. As a result of these efforts, testing rates increased in all four countries since the summer (Fig. 3 ).
Fig. 3.
COVID-19 testing rate by week, 2020. Notes: Testing rate = tests done per 100,000 population. The fall in the testing rate from around week 43 can be explained by a variety of factors, including the fall in infection rates after the autumn peak and testing policy (for example, in Poland, lower testing rates may be due to the policy of testing only symptomatic cases). Other reasons could include the introduction of mass antigen testing in Slovakia (see Figure A2 in the Online Appendix), which is not reported in these figures, or lower rates of self-reporting in Czechia to avoid quarantine. Source: ECDC [3].
Contact tracing capacity in the V4 countries was deemed adequate in the spring and was not further developed over the summer. Czechia entered the new school year with capacity to trace contacts limited to 400 new cases per day, while the daily number of cases was already twice as high by the end of the first week of September 2020 (see Figure A3 in the Online Appendix). The situation was similar in Slovakia, where the regional public health authority in Bratislava declared reaching capacity limits for contact tracing already back in August. Most of the remaining regional public health authorities in Slovakia soon also reached their capacity limits and the Minister of Health promised to significantly increase the budget for contact tracing. However, not much could be achieved to surge the capacity before the second wave of infections hit Slovakia at the end of October (see Fig. 1). In Poland, contact tracing capacity was deemed adequate in spring 2020, and was not increased over the summer. Contact tracing was mainly done using telephone interviews, with data gathered by the sanitary authorities, but capacity was limited. Use of contact tracing apps was minimal, with only about 2% of the population having downloaded the contact tracing app (STOP COVID) by autumn 2020. A higher uptake was noted in Czechia and Slovakia, where it came close to a fifth of the population and no contact tracing apps were used in Hungary.
Persons who came in contact with a confirmed case have been required to quarantine and show a negative COVID-19 test before being released in all four countries. People could quarantine in their homes or, if this was not possible, in specially designated facilities – these were free of charge in all four countries. In Slovakia, Roma communities were considered a high-risk group and, in some cases, entire settlements were forced into quarantine in place of personal isolation measures. In Poland, people in quarantine have been mandated to download the official quarantine app (‘Kwarantanna domowa’ or Home quarantine) through which they could upload photos confirming their whereabouts. Compliance with the quarantine rules was monitored by the police and breaches could result in high monetary fines. Similar apps have been used in Hungary and Slovakia but on a voluntary basis and only for a brief period of time in Slovakia. In all four countries, people covered by statutory social insurance who were required to quarantine could claim sick leave benefits for the duration of the quarantine and little other formal support was available. Further support, such as help with shopping, has been organised by volunteering groups and local communities.
4. Discussion
This article attempts to analyse health policy responses to the COVID-19 pandemic in Czechia, Hungary, Poland, and Slovakia.
The first wave of the pandemic - from early March to August 2020 - hit the Visegrad countries relatively less hard than many other European countries. This is likely because the infection reached these countries relatively late and gave governments the opportunity to observe what was happening in other countries in Europe. When the first cases of the coronavirus were recorded within their national borders the V4 governments reacted quickly, implementing strict national lockdowns and measures to prevent community transmission. The declarations of the states of emergency have likely sparked a sense of threat but also of solidarity amongst the citizens, contributing to the high public acceptance of these measures and motivating the populations to contribute, for example, by sewing face coverings at home or by providing other forms of volunteering work.
The lockdown measures masked the insufficiencies and the unpreparedness of the V4 health systems to tackle a health crisis of such unprecedented scale. But the implemented measures were highly effective in halting the spread of the virus and the V4 countries received international recognition as success stories of the first wave. This resulted in a false sense of security during the summer period and was manifested in diminished public confidence in the strict government response. In some countries, such as Poland and Czechia, this sentiment was purposefully reinforced by the government to build up support for the ruling politicians ahead of the elections and reassure the electorate that it was safe to vote. Highly publicised cases of high-level officials openly flaunting restrictions (Czechia) and cases of flagrant corruption (Poland) have likely contributed to the falling trust in the government response over the summer and early autumn 2020.
All the above, alongside the devastating economic consequences of the national lockdowns and the general fatigue after enduring the various restrictions, may partly explain why little was done when first signals of the worsening of the epidemiological situation started appearing at the end of the summer 2020. Even when the V4 countries started approaching similar number of cases as Italy during the first wave, the governments appeared hesitant to reintroduce any of the previous restrictions. When they finally started to act, the number of cases was already high and difficult to contain.
While the V4 countries intensively increased their hospital capacities in October 2020, adding more beds and buying large quantities of ventilators, this was not always supported by securing enough qualified health workers to operate them. The prevailing shortages of human resources have been a longstanding problem in all four countries, but they were not properly factored in the pandemic responses that in spring focused on increasing hospital capacity and then, in absence of effective FTTIS systems, allowed a virtually uncontrolled spread of the virus since the end of the summer, putting physical and especially human resources under huge strain.
This necessitated radical measures such as introduction of new restrictions and even new lockdowns that the governments had previously vowed to avoid. In Czechia, restrictions were gradually tightened in October 2020, starting with the declaration of a new state of emergency on the 5th of October. On the 24th of October, the entire territory of Poland was designated as a ‘red zone’, which essentially means a second lockdown (albeit with fewer restrictions than before). And in Slovakia, the Prime Minister resorted to compulsory mass testing of the entire population in an attempt to avoid a national lockdown, but a national curfew was nevertheless introduced in December. Stricter measures have also been introduced in Hungary, with a new state of emergency declared on the 4th of November.
As could be seen from the comparison of the COVID-19 responses of the V4 countries, management of a pandemic response is immensely complex, yet it involves standard political decision-making processes, where the technical and political feasibility as well as immediate and longer-term implications of various interventions must be considered. While public health experts may have felt disregarded by the governments not heeding their advice, this does not necessary mean that their data and projections were not taken into consideration; it may be that other public priorities took precedent. This was observed in early autumn 2020, when all V4 countries were reluctant to introduce movement limitations – this may have been motivated by concerns over the economy or the societal harm caused by the restrictions, or by other political considerations.
Further, introduction of a national lockdown is not the only way to keep the pandemic at bay, as shown by the examples of some Asia-Pacific countries [8]. There is a wide array of public health measures, including the implementation of FTTIS systems, that require less technical capacity to implement (compared to, for example, scaling up ICU units), yet are effective at halting transmission and have a lesser impact on the socio-economic activity. These could have been maintained over the summer and could have likely slowed down the surge in infections from September onwards. To what extent the cultural and political differences between countries in Europe and Asia-Pacific limit the feasibility of this “best-of-both-worlds” approach remains an open question. What is clear, however, is that the summer period represents a lost opportunity, especially with regards to strengthening the FTTIS systems, where the success of the first wave has largely been wasted by all V4 countries.
This is reflected in the COVID-19 statistics. In 2020, COVID-19 deaths officially accounted for 4.3% of all deaths in Slovakia, 6% in Poland, 7% in Hungary, and 9.2% in Czechia – the latter being more than 50% higher than across the EU as a whole [3], [4]. However, the broader indicator of excess mortality suggests that the direct and indirect death toll related to COVID-19 may be substantially higher. For example, in the excess mortality recorded in Poland and Slovakia between early March and end of 2020 was more than double the reported COVID-19 deaths. In Czechia excess mortality was 50% higher and in Hungary one third higher than registered COVID-19 deaths.
5. Conclusion
A long-sighted approach is needed to ensure success
The number of cases and deaths recorded in the four Visegrad countries during the 2020 spring wave of infections was very low. This was ascribed to quick and decisive actions taken by their governments, who did not hesitate to impose national lockdowns by closing the borders and restricting free movement of people within days from recording the first cases of COVID-19. But once the spread of the virus was supressed, little was done to prevent further surges in infections – borders reopened and internal movement restrictions were lifted, with few protective measures remaining in place and no effective FTTIS systems developed to minimise new infections over the summer 2020. Few preparations were made for the upcoming autumn period, despite no effective COVID-19 vaccine yet available, pupils and students returning to schools and universities, vacationers returning from abroad, and many countries in Europe experiencing high infection rates.
The role of scientific experts in the response planning diminished over time in all four countries. The key reason behind this was politics, although in some countries scientific capacity was also reduced by unavailability of reliable data. Concerns about large falls in national GDPs after the first wave may be the reason why the V4 governments avoided or were reluctant to implement strict measures during the onset of the second wave of the pandemic – after all, their popularity was largely based on strong GDP growth. However, the lack of preparation in the summer period and the reluctance to introduce even the economically unharmful measures early on proved to be a serious lapse in judgement, for which the four countries had to pay a high price. In countries such as Czechia and Poland, the governments further downplayed the risks of the virus in order to be seen as successful ahead of the elections. Pursuing controversial legislation in the midst of the pandemic was also a dangerous development in some countries. In Poland, this led to mass protests, which posed a health risk to people attending them.
The response should play to the countries’ strengths, but the weaknesses should not be ignored
All four countries started the pandemic with major structural weaknesses in their health systems. The relatively high numbers of hospital beds in all V4 countries, which for many years has been seen as a source of inefficiency, became an asset during the pandemic and efforts to ensure sufficient treatment capacity during the first wave played to this newly found strength and centred around hospital care. This seems to have worked initially but the health systems were not severely tested in spring, as the infection rates remained low and the hospital capacity prepared for treating prospective COVID-19 patients remained largely unused. The surge in infection rates in autumn has put a huge strain on the treatment capacity. While hospital capacity could be surged again, the same could not be done with human resources needed to operate the extra beds. While the relative shortages of doctors and nurses – another longstanding weakness of the V4 health systems – did not constitute a major problem in spring, they have proved to be a bottleneck in the COVID-19 response since the end of the summer. Creating surge capacity of infrastructure is thus not sufficient on its own and requires simultaneous workforce planning as well as focusing on measures that are not constrained by technical capacity limitations, such as maintaining the obligation to wear face coverings.
Declaration of Competing Interest
We declare no competing interests.
Funding
Lucie Bryndova's work on this article was supported by grant SVV 260 596.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.healthpol.2021.10.009.
Appendix B. Supplementary materials
References
- 1.Blikk.hu Emmi: az utasítások be nem tartása a betegek ellátását, életét veszélyezteti. [Failure to follow instructions engenders care and life of patients] Blikk.hu. Retrieved December 3, 2020. 2020 https://www.blikk.hu/aktualis/belfold/emmi-a-betegek-ellatasat-es-eletet-veszelyezteti-az-utasitasok-be-nem-tartasa/mcfkp6q from. [Google Scholar]
- 2.Balkaninsight.com Central Europe: From Pandemic Exemplar to Pariah. BIRN. Retrieved. 2020 https://balkaninsight.com/2020/10/15/central-europe-from-pandemic-exemplar-to-pariah December 3, 2020, from. [Google Scholar]
- 3.ECDC Data on 14-day notification rate of new COVID-19 cases and deaths. (2020a). ECDC. 2021 https://www.ecdc.europa.eu/en/publications-data/data-national-14-day-notification-rate-covid-19 Retrieved December 3, 2020, from. [Google Scholar]
- 4.EC . 2021. Eurostat [online database]. luxembourg: european commission.http://ec.europa.eu/eurostat/data/database Retrieved on July 20, 2021 from. [Google Scholar]
- 5.Europan National Panels (2020). National Pandemic Alarm. Representative survey monitoring public opinion, emotions and experience with novelty Corona virus spread in five Central European countries. Retrieved December 3, 2020, from https://www.nationalpandemicalarm.eu/en/2020-03-18?index=impact.
- 6.Hospodářské noviny Roušky ano, roušky ne. Vojtěch po výtkách Babiše zrušil jejich nošení ve školách, obchodech i restauracích. Hospodářské Noviny. [Masks, no masks. After rebuking Babiš, Vojtěch cancels wearing of masks in schools, shops and restaurants.] Retrieved December 3, 2020. 2020 https://archiv.ihned.cz/c1-66805450-rousky-ano-rousky-ne-vojtech-po-vytkach-babise-zrusil-jejich-noseni-ve-skolach-obchodech-i-restauracich from. [Google Scholar]
- 7.Visegrad Group History of the Visegrad Group. Visegrad Group. 2020 http://www.visegradgroup.eu/history/history-of-the-visegrad Retrieved December 3, 2020, from. [Google Scholar]
- 8.Han E., et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. The Lancet. 2020;396(10261):1525–1534. doi: 10.1016/S0140-6736(20)32007-9. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20 32007-9/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polityka.pl Afery Szumowskiego. Za dużo tego, by zamieść pod dywan. [The Szumowski skandal. Too much to sweep under the rug] Polityka.pl. Retrieved. 2020 https://www.polityka.pl/tygodnikpolityka/kraj/1959028,1,afery-szumowskiego-za-duzo-tego-by-zamiesc-pod-dywan.read December 3, 2020, from. [Google Scholar]
- 10.Wyborcza.pl OKO.press: Minister Szumowski i interesy z oszustem. [Minister Szumowski and doing business with a fraudster] Wyborcza.pl. Retrieved. 2020 https://wyborcza.pl/7,75398,25959008,oko-press-minister-szumowski-i-interesy-z-oszustem.html?disableRedirects=true December 3, 2020, from. [Google Scholar]
- 11.Index.hu . Index.hu.; 2020. Kirúgott kórházigazgató: egy ilyen hiba bárhol előfordul. [Hospital director fired: such mistakes occur everywhere]https://index.hu/belfold/2020/04/11/kirugott_korhazigazgato_egy_ilyen_hiba_barhol_elofordul November 4. Retrieved December 3, 2020, from. [Google Scholar]
- 12.Sme.sk Kováč P., Sopóci P. SME Domov; 2020. NAKA zasahuje u bývalého šéfa hmotných rezerv kičuru aj u jeho otca. [NAKA intervenes with the former head of material reserves, kičuru, and his father]https://domov.sme.sk/c/22387859/naka-zasahuje-u-kajetana-kicuru.html April 21. Retrieved December 3, 2020, from. [Google Scholar]
- 13.Gazetaprawna.pl Bezkarność urzędnicza w rękach Trybunału Konstytucyjnego [Officials’ impunity in the hands of the Constitutional Tribunal] GazetaPrawna.pl. 2020 https://prawo.gazetaprawna.pl/artykuly/1493820,bezkarnosc-urzednicza-ustawa-trybunal-konstytucyjny.html Retrieved December 3,2020, from. [Google Scholar]
- 14.Merkely B., Szabó A.J., Kosztin A., et al. Novel coronavirus epidemic in the Hungarian population, a cross-sectional nationwide survey to support the exit policy in Hungary. GeroScience. 2020;42:1063–1074. doi: 10.1007/s11357-020-00226-9. (2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meyer B. 2020. Pandemic populism: an analysis of populist leaders’ responses to covid-19. tony blair institute for global change.https://institute.global/policy/pandemic-populism-analysis-populist-leaders-responses-covid-19 August 17. Retrieved December 3, 2020, from. [Google Scholar]
- 16.Ministry of Health of the Republic of Poland . [Strategy to combat the COVID-19 pandemic. Version 3.0. Autumn 2020.]; 2020. Strategia walki z pandemią COVID-19. wersja 3.0. jesień 2020.https://www.gov.pl/web/zdrowie/strategia-walki-z-pandemia-covid19 Retrieved December 3, 2020, from. [Google Scholar]
- 17.Nepszava.hu Októberre várják a halálozások felfutását [The death toll is expected to rise in October] Nepszava.hu. 2020 https://nepszava.hu/3093247_oktoberre-varjak-a-halalozasok-felfutasat Retrieved December 3, 2020, from. [Google Scholar]
- 18.OECD . 2019. Economic outlook no 106.https://stats.oecd.org/Index.aspx?DataSetCode=EO106_INTERNET November 2019. [Google Scholar]
- 19.OECD . 2020. Economic outlook no 107 - June 2020 – single-hit scenario. [Google Scholar]; https://stats.oecd.org/Index.aspx?DataSetCode=EO107_INTERNET_1
- 20.OECD . 2020. Economic outlook no 108.https://stats.oecd.org/Index.aspx?DataSetCode=EO December 2020. [Google Scholar]
- 21.OECD/European Observatory on Health Systems and Policies . OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels; 2019. Czechia: country health profile 2019, state of health in the eu. [Google Scholar]
- 22.OECD/European Observatory on Health Systems and Policies . OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels; 2019. Hungary: country health profile 2019, state of health in the eu. [Google Scholar]
- 23.OECD/European Observatory on Health Systems and Policies . OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels; 2019. Poland: country health profile 2019, state of health in the eu. [Google Scholar]
- 24.OECD/European Observatory on Health Systems and Policies . OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels; 2019. Slovakia: country health profile 2019, state of health in the eu. [Google Scholar]
- 25.Oko.press . OKO.press; 2020. Co będzie, gdy pis ogłosi stan nadzwyczajny? prawa dla obywateli albo dyktatura. wyjaśniamy różnice.https://oko.press/co-bedzie-gdy-pis-oglosi-stan-nadzwyczajny April 4. Retrieved December 3, 2020, from. [Google Scholar]
- 26.Portfolio.hu Koronavírus: van egy anyag, ami hatékonynak tűnik a betegség kezelésében [Coronavirus: is a substance that appears to be effective in treating the disease] Portfolio.hu. 2020 https://www.portfolio.hu/gazdasag/20200327/koronavirus-van-egy-anyag-ami-hatekonynak-tunik-a-betegseg-kezeleseben-422404 Retrieved December 3, 2020, from. [Google Scholar]
- 27.Rechel B., Maresso A., van Ginneken E. (2019) Health Systems in Transition. Template for authors. Copenhagen: World Health Organization (acting as the host for, and secretariat of, the European Observatory on Health Systems and Policies).
- 28.Tvnovinky.sk . Tvnovinky.sk.; 2020. Matovič: svadby budú do 100 ľudí, ale za prísnych podmienok a vysokých pokút za ich nedodržanie. [Matovič: weddings will be up to 100 people, but under strict conditions and heavy fines for not following them.]https://www.tvnoviny.sk/koronavirus/2007493_matovic-svadby-budu-do-100-ludi-ale-za-prisnych-podmienok-a-vysokych-pokut-za-ich-nedodrzanie September 16. Retrieved December 3, 2020, from. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.