Abstract
OBJECTIVE.
To determine the association between contact precautions and depression or anxiety as well as feelings of anger, sadness, worry, happiness, or confusion.
DESIGN.
Prospective frequency-matched cohort study.
SETTING.
The University of Maryland Medical Center, a 662-bed tertiary care hospital in Baltimore, Maryland.
PARTICIPANTS.
A total of 1,876 medical and surgical patients over the age of 18 years were approached; 528 patients were enrolled from January through November 2010, and 296 patients, frequency matched by hospital unit, completed follow-up on hospital day 3.
RESULTS.
The primary outcome was Hospital Anxiety and Depression Scale (HADS) scores on hospital day 3, controlling for baseline HADS scores. Secondary moods were measured with visual analog mood scale diaries. Patients under contact precautions had baseline symptoms of depression 1.3 points higher (P< .01) and anxiety 0.8 points higher (P = .08) at hospital admission using HADS. Exposure to contact precautions was not associated with increased depression (P = .42) or anxiety (P = .25) on hospital day 3. On hospital day 3, patients under contact precautions were no more likely than unexposed patients to be angry (20% vs 20%; P = .99), sad (33% vs 38%; P = .45), worried (51% vs 46%; P = .41), happy (58% vs 67%; P = .14), or confused (23% vs 24%; P = .95).
CONCLUSIONS.
Patients under contact precautions have more symptoms of depression and anxiety at hospital admission but do not appear to be more likely to develop depression, anxiety, or negative moods while under contact precautions. The use of contact precautions should not be restricted by the belief that contact precautions will produce more depression or anxiety.
Multidrug-resistant (MDR) bacteria are a common cause of healthcare-associated infections and are associated with increased morbidity and mortality in hospitalized patients.1 The Centers for Disease Control and Prevention (CDC) guidelines and others recommend contact precautions (the use of gowns, gloves, and single rooms) to prevent the spread of MDR bacteria.2–4
Contact precautions change the way care is delivered.2,5,6 Multiple studies have observed that healthcare workers visit patients under contact precautions approximately half as frequently as other patients.7 Patients under contact precautions have longer hospital stays, worse quality of care, and a higher frequency of preventable adverse events.3,8 These consequences are of increasing importance given the growing number of patients placed under contact precautions as a result of state-level and federal Veterans Affairs screening mandates for methicillin-resistant Staphylococcus aureus.2,3,9–11
Current CDC contact precaution guidelines instruct healthcare workers to “counteract possible adverse effects” on patient anxiety, depression, and other mood disturbances.3 The studies that led to these recommendations have significant limitations, and more recent studies of depressive symptoms and their association with contact precautions report mixed results.6,7,12–14 Few studies have prospectively assessed whether contact precautions lead to more symptoms of depression or anxiety during hospitalization.15 In a cohort of 51 patients, those under contact precautions reported increased depression and anxiety after 1 week of hospitalization. The presumed psychological basis for contact precautions causing depression and anxiety was frustration, anger, worry, isolation, and stigmatization.7,16,17 These negative emotions have been described in qualitative studies but have rarely been quantified.7
Public perception of contact precautions is focused on unintended consequences, as reflected in recent editorials in the New York Times.18,19 Concern about possible unintended consequences of contact precautions has limited their application toward infection prevention. Some have even questioned whether the use of contact precautions is ethical.20
To assess the relationship between contact precautions and incident depression, anxiety, and mood changes, we conducted a prospective cohort study of hospitalized patients. Strengths of our study include a large sample size adequately powered to detect minimal clinical differences, frequency matching of exposed and unexposed patients by minimum length of stay and hospital unit, and prospective measurement of depression, anxiety, and moods after hospital admission.
METHODS
Study Sample
We conducted a longitudinal frequency-matched cohort study of patients admitted to general medical and surgical units at the University of Maryland Medical Center (UMMC), a 662-bed tertiary care teaching hospital in Baltimore, Maryland. In our hospital, contact precautions are used for MDR bacteria and Clostridium difficile and require the use of a disposable gown and gloves for all patient contact. Visitors are required to use contact precautions, and patients are housed in single or cohorted rooms. Patient education for MDR bacteria is provided. This study received institutional review board approval from the University of Maryland, Baltimore.
During a 10-month period, study personnel received a daily list of all adults admitted within the past 24 hours to all general medical and surgical services. Patients under contact precautions were approached for enrollment in the study within 36 hours of admission. After providing informed consent, patients were administered a 36-item questionnaire containing baseline demographic information, medical and psychiatric history, the Hospital Anxiety and Depression Scale (HADS), and visual analog mood scales (VAMS).
On the third hospital day, each patient still in the hospital underwent a follow-up interview that assessed HADS and VAMS. After a contact precaution patient completed day 3, a newly admitted patient (within 36 hours of admission) not under contact precautions was recruited from the same hospital unit as a control. If the newly admitted non–contact precaution patient did not stay until day 3 or was placed under contact precautions, another non–contact precaution patient was recruited from the same hospital unit until 1 non–contact precaution patient completed the same follow-up interview on day 3. Patients under contact precautions who remained inpatients for 3 days were frequency matched by hospital unit to patients who remained inpatients for 3 days who were not under contact precautions, to ensure each group had similar levels of care and other unmeasured variables. Patients remaining hospitalized beyond day 3 were reapproached weekly to obtain HADS and VAMS.
Power Calculation
This study was powered to detect a clinically important difference in symptoms of depression or anxiety on hospital day 3. A minimal important difference in HADS was determined to be a change of 1.5 points on either scale in a clinical trial of patients with chronic obstructive pulmonary disorder.21 This represented answering “often” instead of “sometimes” for 1 or 2 questions relating to mood (see “Discussion” for examples). With 80% power and α = .05, we needed 113 patients in each group to detect an average difference of 1.5 (after exposure to contact precautions) on either the depression or the anxiety subscale of HADS.
Outcomes
The primary outcome was score on the depression and anxiety subscales of HADS, a 14-item scale designed to limit the interference of somatic problems in the detection of symptoms of anxiety and depression in hospital inpatients.22 At enrollment patients were asked to report symptoms over the past week, and on hospital day 3 they were asked to rate their symptoms since hospital admission.23 Each HADS subscale score (7 items for depression and 7 for anxiety) ranges from 0 to 21. A score of 0–7 on either measure indicates no depression or anxiety, and a score of 8 or higher on either scale represents possible or probable cases of depression or anxiety disorder.22 HADS has been found to be reliable and valid in hospital inpatients. Depression and anxiety subscales were chosen a priori to distinguish effects of contact precautions. A 1.5 difference on each subscale is the minimum clinically important difference between groups.21,22
VAMS were used to measure anger, happiness, sadness, confusion, and worry. Each 100-mm scale had a drawing of a face with an emotionally appropriate expression on the left end of the scale and a neutral face on the other end of the scale.24 The name of each mood was written under each face. Patients were asked to make a vertical mark representing where their current mood fell on the 100-mm scale. We measured distance from the mood of interest, with 0 mm representing the maximum expression of that mood and 100 mm representing neutral. To analyze change in VAMS scores at 2 time points in a format that could be represented visually, for each VAMS, if patients scored below 50, they were considered to exhibit that mood.25,26 Change in VAMS score from hospital day 1 to day 3 was also analyzed. VAMS have been used in many patient populations—including emergency department patients, patients with insomnia, and patients at risk for carrying genetic disease—and in random clinical trials.25,26,33,34
Other Measurements
Demographic variables, psychiatric history, and smoking status were obtained during baseline interview. Data on Charlson Comorbidity Index, hospital length of stay, and intensive care unit transfer were obtained from the UMMC central data repository. The UMMC central data repository is a relational database that contains patients’ administrative, pharmacy, and laboratory data and is maintained by the University of Maryland Information Technology Group. These data have been used in previous epidemiological studies.27–30
Analysis
Differences in baseline characteristics between patients under contact precautions and those not under contact precautions were compared using χ2 tests for dichotomous variables and t tests or nonparametric tests for continuous variables. We also assessed the association between variables and presence of possible depression or anxiety on HADS using χ2 tests.
Multivariate linear regression models were fit to examine the independent relationship between exposure to contact precautions and depression and the relationship between exposure to contact precautions and anxiety. Aside from including our main predictor variable, contact precautions, we chose a priori to include the following biologically important variables: age, sex, Charlson Comorbidity Index, history of depression or anxiety (depression in the depression model, anxiety in the anxiety model), and baseline HADS subscale score. Models were fit by including all variables that were significantly related to contact precautions, depression, or anxiety (α = .05) in the bivariable analyses. In the multivariate model, variables not significantly associated with the outcome were removed from the model, then reinserted in the order of expected effect on the coefficient for contact precautions. If the factor changed the regression coefficient for contact precautions by more than 20%, it was left in the final model.
RESULTS
Between January 11, 2010, and November 17, 2010, 1,876 patients were approached, and 528 patients agreed to participate and completed the HADS measure within 36 hours of admission to UMMC. Of these, 296 provided follow-up information on day 3 (Figure 1). Most patients who were lost to follow-up were discharged before their third day in the hospital (n = 209 [40%]); only 3% withdrew between day 1 and day 3 (n = 16). Reasons for loss to follow-up included inability to complete HADS on day 3 (weak or deceased; n = 6) or transfer to a psychiatry unit (n = 1). Table 1 compares characteristics of patients who were approached but declined to enroll and patients who enrolled and provided day 1 data.
FIGURE 1.

Flowchart demonstrating enrollment and inclusion of patients in the final matched cohort.
TABLE 1.
Comparison between Patients in Final Study Sample and Patients Who Did Not Enroll in the Study
| Variable | Approached but not enrolled (n = 1,876) | Approached and enrolled on day 1 (n = 528) | P |
|---|---|---|---|
| Mean age, years | 54.4 | 52.7 | .04 |
| Female sex, % | 48.3 | 47.1 | .64 |
| Mean length of stay, days | 4.5 | 5.1 | .07 |
| Inpatient mortality, % | 1.1 | 0.6 | .57 |
| Admitted to an intensive care unit during stay, % | 7.0 | 6.4 | .69 |
Frequency matching by medical unit of admission for patients with 3 days of hospitalization reduced many of the baseline differences seen between contact precaution patients and non–contact precaution patients (Table 2). Unadjusted analyses showed that mean HADS depression scores on day 1 were significantly higher in patients under contact precautions (6.0 vs 4.7; P< .01). There was a non–statistically significant trend toward higher HADS anxiety scores on day 1 (7.5 vs 6.7; P = .08). Unadjusted analysis of the 298 frequency-matched patients revealed that those under contact precautions continued to have higher unadjusted mean depression (6.1 vs 4.9; P ≤ .01) and anxiety (7.2 vs 6.1; P = .03) on hospital day 3. On hospital day 7, 28 patients remained under contact precautions, and 27 remained not under contact precautions. The group under contact precautions had higher mean day 7 HADS depression scores (6.3 vs 5.0; P = .18) than patients not under contact precautions as well as higher mean HADS anxiety scores (7.5 vs 5.6; P = .12; Figures 2, 3).
TABLE 2.
Demographic and Baseline Information on All Enrolled Patients and Those Who Were Frequency Matched by Staying in the Same Unit until Hospital Day 3
| Entire population (all patients enrolled on day 1) |
Frequency-matched population (patients who provided day 3 follow-up) |
|||||
|---|---|---|---|---|---|---|
| CP (n = 238) | Non-CP (n = 290) | P | CP (n =148) | Non-CP (n =148) | P | |
| Age, mean (SD), years | 52.4 (13.4) | 52.9 (14.8) | .69 | 52.0 (13.9) | 52.3 (14.6) | .18 |
| Female sex | 44.3 (105) | 52.0 (151) | .08 | 41.9 (62) | 49.3 (73) | .20 |
| Education (some college) | 36.6 (87) | 49.1 (142) | <.01 | 37.8 (56) | 57.8 (85) | <.01 |
| Married or living with partner | 36.7 (87) | 43.5 (126) | .11 | 38.5 (57) | 50.0 (74) | .05 |
| Homeowner | 44.3 (105) | 57.4 (166) | <.01 | 48.0 (71) | 62.2 (92) | .01 |
| Psychiatric history | ||||||
| History of depression | 40.3 (96) | 30.9 (89) | .09 | 31.8 (47) | 27.0 (40) | .37 |
| History of anxiety | 31.5 (71) | 24.7 (75) | .08 | 31.0 (46) | 26.4 (39) | .36 |
| History of schizophrenia | 2.1 (5) | 2.8 (8) | .61 | 1.4 (2) | 2.7 (4) | .68 |
| History of bipolar disorder | 8.4 (20) | 6.3 (18) | .34 | 7.4 (11) | 3.4 (5) | .12 |
| History of substance abuse | 28.2 (67) | 14.6 (42) | <.01 | 25.7 (38) | 10.1 (15) | <.01 |
| Previous psychiatric admission | 18.9 (45) | 11.5 (33) | .02 | 16.2 (24) | 7.5 (11) | .02 |
| Current smoker | 33.2 (79) | 25.3 (73) | .05 | 30.4 (45) | 18.9 (28) | .02 |
| Charlson Comorbidity Index, median (IQR) | 1.0 (3.0) | 1.0 (2.0) | .07 | 1.0 (3.0) | 1.0 (2.0) | .18 |
| Admission to an intensive care unit during hospitalization | 5.0 (12) | 6.6 (21) | .46 | 5.4 (8) | 9.8 (14) | .18 |
| Length of hospital stay, mean (SD), days | 3.8 (4.9) | 3.0 (3.4) | <.01 | 5.5 (4.3) | 4.7 (3.8) | .16 |
| HADS score on day 1, mean (SD) | ||||||
| Depression subscale | 6.2 (3.9) | 4.6 (3.9) | <.01 | 6.0 (3.7) | 4.7 (4.1) | <.01 |
| Anxiety subscale | 7.5 (4.1) | 6.8 (4.4) | .07 | 7.5 (3.8) | 6.7 (4.4) | .08 |
note. Data are % (no.), unless otherwise indicated. Within each group, those under contact precautions (CP) are compared with those not under CP. Missing demographic variables were present, but less than 2% of each variable was missing in the frequency-matched sample. HADS, Hospital Anxiety and Depression Scale; IQR, interquartile range; SD, standard deviation.
FIGURE 2.

Mean unadjusted Hospital Anxiety and Depression Scale depression subscale scores on hospital days 1, 3, and 7. Vertical lines represent 95% confidence intervals around the mean.
FIGURE 3.

Mean unadjusted Hospital Anxiety and Depression Scale anxiety subscale scores on hospital days 1, 3, and 7. Vertical lines represent 95% confidence intervals around the mean.
Adjusted models showed no significant difference in HADS anxiety or depression scores on day 3 related to use of contact precautions after adjustment for baseline HADS anxiety or depression scores and other relevant variables (Table 3). Aside from a priori variables, the only confounder for both depression and anxiety was previous psychiatric inpatient stay. Education was an important confounder between contact precautions and depression but not anxiety. Depression or anxiety score on day 1 best predicted symptoms of depression and anxiety on day 3.
TABLE 3.
Linear Regression Models for Association between Contact Precautions and Depression (Model 1) or Anxiety (Model 2) on Hospital Day 3, Adjusting for Baseline Symptoms of Depression or Anxiety and Other Possible Confounding Factors
| Depression (n = 296) |
Anxiety (n = 296) |
|||
|---|---|---|---|---|
| Adjusted difference (SE) | P | Adjusted difference (SE) | P | |
| Contact precautions | 0.22 (0.36) | .54 | 0.33 (0.34) | .34 |
| Female sex | −0.50 (0.36) | .17 | −0.34 (0.33) | .31 |
| Age, per year | −0.005 (0.01) | .69 | 0.02 (0.01) | .17 |
| Charlson Comorbidity Index, per point | 0.002 (0.09) | .98 | −0.03 (0.09) | .77 |
| Baseline HADS depression or anxiety scorea | 0.74 (0.05) | <.01 | 0.70 (0.44) | <.01 |
| History of depression or anxietyb | 0.74 (0.42) | .18 | 0.71 (0.42) | .09 |
| History of inpatient psychiatry admissionc | 0.65 (0.58) | .26 | 1.13 (0.57) | .05 |
| Some college education or greaterd | 0.80 (0.42) | .05 | −0.18 (0.34) | .61 |
note. Age, sex, and comorbidities were included a priori in each model.
Baseline depression score was added to the depression model and baseline anxiety score was added to the anxiety model.
History of depression was added to the depression model only and history of anxiety was added to the anxiety model only.
Two patients were excluded because of failure to provide a history of psychiatric admission.
One patient did not provide education history.
VAMS showed no significant differences between the 2 groups. At hospital admission, more than half the patients in each group reported being happy (58% under contact precautions, 67% not under contact precautions; P = .14), and about half reported being worried (46% under contact precautions, 51% not under contact precautions; P = .41). Less than half reported feeling sad (38% under contact precautions, 33% not under contact precautions; P = .46), angry (20% under contact precautions, 20% not under contact precautions; P = .99), or confused (23% under contact precautions, 24% not under contact precautions; P = .95). There were no significant differences in anger, confusion, worry, happiness, or sadness at baseline related to contact precautions. Logistic regression showed no significant changes in VAMS scores from baseline to hospital day 3. On day 3, the percentage of people reporting each mood remained similar to that on day 1, with no significant differences related to use of contact precautions (Figure 4). Exact numbers for each VAMS mood can be found in Table 4.
FIGURE 4.
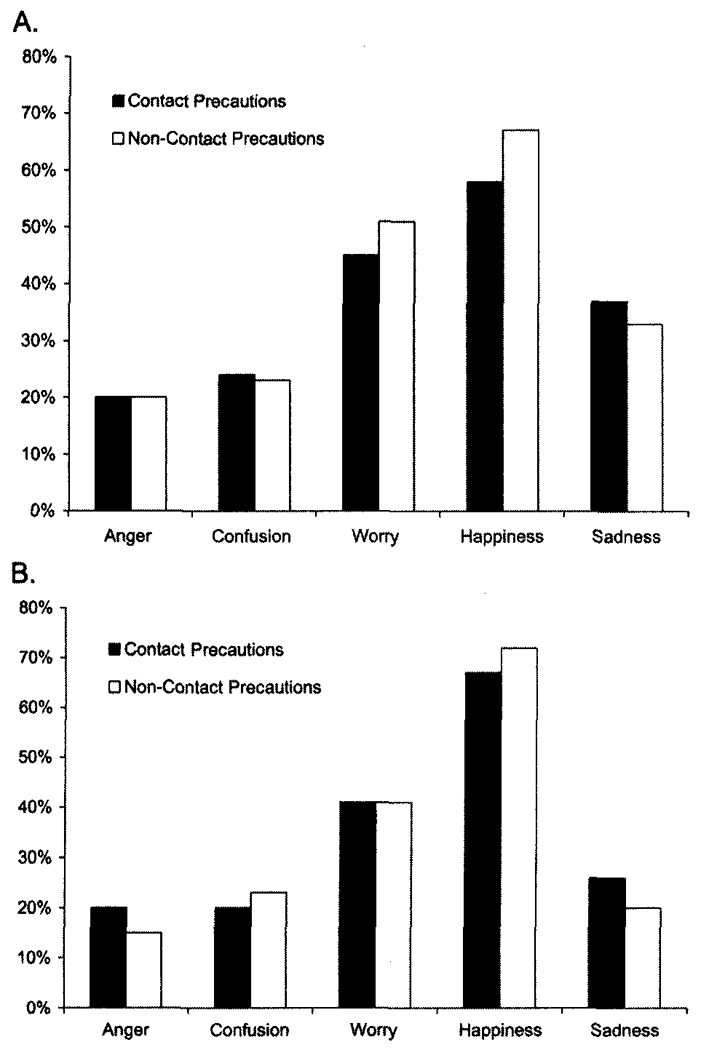
Frequency that patients identified themselves as angry, confused, worried, happy, or sad on visual analog mood scales at the time of hospital admission (A) and on hospital day 3 (B).
TABLE 4.
Exact Numbers from Visual Analog Mood Scales for Each Emotion Recorded on Hospital Days 1 and 3 (Represented in a Binary Yes/No Fashion) and Change from Day 1 to Day 3 (in Absolute Scale from 0 to 100 mm), Comparing Those under Contact Precautions (CP) with Those Not under CP
| % of people reporting each emotion on day 1 | P | % of people reporting each emotion on day 3 | P | Change in emotion from day 1 to day 3, mm | P | |
|---|---|---|---|---|---|---|
| Anger | .99 | .34 | .10 | |||
| CP | 20.2 | 20.0 | ↑ 3.4 | |||
| Non-CP | 20.2 | 15.3 | ↓2.8 | |||
| Worry | .40 | .99 | .07 | |||
| CP | 46.0 | 40.5 | ↓ 2.8 | |||
| Non-CP | 51.2 | 40.5 | ↓ 9.2 | |||
| Sadness | .45 | .29 | .55 | |||
| CP | 37.9 | 26.5 | ↓ 4.3 | |||
| Non-CP | 33.3 | 20.7 | ↓ 6.4 | |||
| Confusion | .95 | .59 | .21 | |||
| CP | 23.4 | 20.0 | ↑ 3.5 | |||
| Non-CP | 23.7 | 22.9 | ↓ 0.8 | |||
| Happiness | .14 | .40 | .48 | |||
| CP | 58.1 | 66.9 | ↑ 5.5 | |||
| Non-CP | 67.2 | 71.9 | ↑ 3.0 |
DISCUSSION
We found that patients under contact precautions had more symptoms of depression and anxiety at hospital admission. However, over 3 days of exposure to contact precautions, we observed no increase in symptoms of depression or anxiety. Furthermore, we found no significant changes in anger, worry, happiness, sadness, or confusion related to contact precautions.
Contact precautions are applied to patients known to have MDR bacteria. In general, these patients are older and sicker and have greater exposure to health care.6–8 These factors are also associated with depression, anxiety, and other adverse outcomes, independent of contact precautions.7 To adjust for baseline patient status, we measured symptoms of anxiety, depression, and mood states at hospital admission and also matched for patients remaining in the hospital at least 3 days.
Patients under contact precautions had slightly more symptoms of depression and anxiety at hospital admission. The observed difference in HADS depression score of 4.6 versus 6.2 on day 1 (n = 528) is of borderline clinical relevance and represents the difference between answering “often” instead of “sometimes” for 1 or 2 questions, such as enjoying a good book or losing interest in one’s appearance.21 The observed baseline difference in HADS anxiety score of 6.7 versus 7.5 on day 1 (n = 528) is minimally different and not statistically significant.21 Our unadjusted findings are consistent with previous work finding a higher prevalence of depressive symptoms in patients under contact precautions.14,17,31
To assess whether contact precautions were associated with incident depression or anxiety, our study monitored patients longitudinally during their hospital stay using strict criteria for matching patients who stayed at least 3 days in the hospital. Frequency matching reduced baseline differences between patients under and not under contact precautions, as shown in Table 2. The only previous study to examine incident depression and anxiety in patients longitudinally in the hospital included only 51 patients with follow-up data and suffered from other methodological concerns, including not enrolling all patients at the time of admission and not adjusting for longer stay or more frequent psychiatric diagnoses in patients under contact precautions. In contrast to this limited study, our study found that inpatient exposure to contact precautions was not associated with increased symptoms of depression or anxiety.
Emotions theorized to underlie greater depression and anxiety in patients under contact precautions include sadness, pleasure, anger, worry, and a feeling of stigmatization.7,32 These emotions have rarely been studied quantitatively in patients under contact precautions.31 We used VAMS, a standardized approach to measure patient-reported mood states, to assess patient confusion, worry, anger, happiness, and sadness. We found no differences in happiness, sadness, or confusion on hospital day 3. The nonsignificant differences in anger and worry we observed over the course of hospitalization were likely clinically insignificant, as they were less than 10% different on VAMS, the standard for clinical relevance.33,34 Although previous studies have posited that patients under contact precautions experience more confusion, anger, stigma, worry, and sadness, our study is the first in which these emotions have been carefully assessed as a factor of contact precautions.7,32 A lack of association between contact precautions and changes in emotions is in agreement with the lack of observed differences in depression and anxiety, as these emotions are thought to be mechanisms for depression and anxiety.
This study has limitations, including the following: (1) it was conducted at a single center; (2) baseline measurement of depression and anxiety was made after admission to the hospital and not in the emergency department or the community (although the HADS used at baseline asked patients to rate their symptoms “over the past week”); (3) patients under contact precautions were all known in our system to have a MDR organism at the time of admission; (4) few scales have been developed to track changes in symptoms of depression and anxiety over short time periods, although previous authors have used HADS in a similar fashion;23 (5) most patients were discharged from the hospital before 1 week, so our conclusions may not apply to the long-term effect of contact precautions (but average hospital stay in many hospitals is 3 days); and (6) HADS was administered by an investigator using gowns and gloves if a patient was under contact precautions, which could modify responses.
In summary, in a large, frequency-matched prospective study, we found that hospitalized patients under contact precautions had slightly more symptoms of depression at baseline but did not develop increased symptoms of depression or anxiety while under contact precautions. Moods thought to be affected by contact precautions did not differ. Strengths of this study include a prospective design, a large sample size allowing detection of small differences, frequency matching by length of stay and hospital unit, and use of a validated depression and anxiety scale designed for hospital use.
Contact precautions have been associated with worse outcomes. Our study provides evidence that while contact precautions are associated with depression and anxiety, depression and anxiety do not worsen with exposure to contact precautions. Use of contact precautions should not be restricted by the belief that contact precautions will produce more depression or anxiety, although patients placed under contact precautions may benefit from mental health assessment because of increased depression and anxiety at baseline.
Financial support.
This work was supported by grants 1 K08 HS18111-01 AHRQ to D.J.M., VA HSRD IIR 04-123-2 to E.N.P., and 1 K24 5K24A1079040-02 NIH to A.D.H.
Footnotes
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the conflicts that the editors consider relevant to this article are disclosed here.
REFERENCES
- 1.Klevens RM, Edwards JR, Richards CL Jr, et al. Estimating health care–associated infections and deaths in U.S. hospitals, 2002. Public Health Rep 2007;122:160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muto CA, Jernigan JA, Ostrowsky BE, et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and Enterococcus. Infect Control Hosp Epidemiol 2003;24:362–386. [DOI] [PubMed] [Google Scholar]
- 3.Siegel JD, Rhinehart E, Jackson M, Chiarello L; Health Care Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control 2007; 35:S65–S164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calfee DP, Salgado CD, Classen D, et al. Strategies to prevent transmission of methicillin-resistant Staphylococcus aureus in acute care hospitals. Infect Control Hosp Epidemiol 2008;29(suppl 1):S62–S80. [DOI] [PubMed] [Google Scholar]
- 5.Abad C, Fearday A, Safdar N. Adverse effects of isolation in hospitalised patients: a systematic review. J Hosp Infect 2010;76:97–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Safdar N, Maki DG. The commonality of risk factors for nosocomial colonization and infection with antimicrobial-resistant Staphylococcus aureus, Enterococcus, gram-negative bacilli, Clostridium difficile, and Candida. Ann Intern Med 2002;136:834–844. [DOI] [PubMed] [Google Scholar]
- 7.Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: a review of the literature. Am J Infect Control 2009;37:85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA 2003;290:1899–1905. [DOI] [PubMed] [Google Scholar]
- 9.Illinois general assembly bill HB0378. [Google Scholar]
- 10.Kussman MJ. Veterans Health Administration directive 2007-002.
- 11.Weber SG, Huang SS, Oriola S, et al. Legislative mandates for use of active surveillance cultures to screen for methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci: position statement from the joint SHEA and APIC task force. Am J Infect Control 2007;35:73–85. [DOI] [PubMed] [Google Scholar]
- 12.Day HR, Perencevich EN, Harris AD, et al. Do contact precautions cause depression? a two-year study at a tertiary care medical centre. J Hosp Infect 2011;79:103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wassenberg M, Severs D, Bonten M. Psychological impact of short-term isolation measures in hospitalised patients. J Hosp Infect 2010;75:124–127. [DOI] [PubMed] [Google Scholar]
- 14.Day HR, Morgan DJ, Himelhoch S, Young A, Perencevich EN. Association between depression and contact precautions in veterans at hospital admission. Am J Infect Control 2011;39:163–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Catalano G, Houston SH, Catalano MC, et al. Anxiety and depression in hospitalized patients in resistant organism isolation. South Med J 2003;96:141–145. [DOI] [PubMed] [Google Scholar]
- 16.Hansen MS, Fink P, Frydenberg M, de Jonge P, Huyse FJ. Complexity of care and mental illness in medical inpatients. Gen Hosp Psychiatry 2001;23:319–325. [DOI] [PubMed] [Google Scholar]
- 17.Kennedy P, Hamilton LR. Psychological impact of the management of methicillin-resistant Staphylococcus aureus (MRSA) in patients with spinal cord injury. Spinal Cord 1997;35:617–619. [DOI] [PubMed] [Google Scholar]
- 18.Zuger A, Isolation, an ancient and lonely practice, endures. New York Times. August 30, 2010. http://www.nytimes.com/2010/08/31/health/31essay.html?_r=0. Accessed January 9, 2013.
- 19.Chen PW. Losing touch with the patient. New York Times. October 21, 2010. http://www.nytimes.com/2010/10/21/health/views/21chen.html. Accessed January 9, 2013.
- 20.Diekema DJ, Edmond MB. Look before you leap: active surveillance for multidrug-resistant organisms. Clin Infect Dis 2007; 44:1101–1107. [DOI] [PubMed] [Google Scholar]
- 21.Puhan MA, Frey M, Buchi S, Schunemann HJ. The minimal important difference of the Hospital Anxiety and Depression Scale in patients with chronic obstructive pulmonary disease. Health Qual Life Outcomes 2008;6:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361–370. [DOI] [PubMed] [Google Scholar]
- 23.Gustad LT, Chaboyer W, Wallis M. ICU patient’s transfer anxiety: a prospective cohort study. Aust Crit Care 2008;21:181–189. [DOI] [PubMed] [Google Scholar]
- 24.Crichton N Information point: visual analogue scale (VAS). J Clin Nurs 2001;10:706. [Google Scholar]
- 25.McConkie-Rosell A, Spiridigliozzi GA, Sullivan JA, Dawson DV, Lachiewicz AM. Longitudinal study of the carrier testing process for fragile X syndrome: perceptions and coping. Am J Med Genet 2001;98:37–45. [PubMed] [Google Scholar]
- 26.Moore A, Moore O, McQuay H, Gavaghan D. Deriving dichotomous outcome measures from continuous data in randomised controlled trials of analgesics: use of pain intensity and visual analogue scales. Pain 1997;69:311–315. [DOI] [PubMed] [Google Scholar]
- 27.McGregor JC, Perencevich EN, Furuno JP, et al. Comorbidity risk-adjustment measures were developed and validated for studies of antibiotic-resistant infections. J Clin Epidemiol 2006; 59:1266–1273. [DOI] [PubMed] [Google Scholar]
- 28.Osih RB, McGregor JC, Rich SE, et al. Impact of empiric antibiotic therapy on outcomes in patients with Pseudomonas aeruginosa bacteremia. Antimicrob Agents Chemother 2007;51(3):839–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schweizer ML, Furuno JP, Harris AD, et al. Empiric antibiotic therapy for Staphylococcus aureus bacteremia may not reduce in-hospital mortality: a retrospective cohort study. PloS ONE 2010;5(7):e11432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Furuno JP, Harris AD, Wright MO, et al. Value of performing active surveillance cultures on intensive care unit discharge for detection of methicillin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol 2007;28:666–670. [DOI] [PubMed] [Google Scholar]
- 31.Tarzi S, Kennedy P, Stone S, Evans M. Methicillin-resistant Staphylococcus aureus: psychological impact of hospitalization and isolation in an older adult population. J Hosp Infect 2001; 49(4):250–254. [DOI] [PubMed] [Google Scholar]
- 32.Knowles HE. The experience of infectious patients in isolation. Nurs Times 1993;89(30):53–56. [PubMed] [Google Scholar]
- 33.Zisapel N, Nir T. Determination of the minimal clinically significant difference on a patient visual analog sleep quality scale. J Sleep Res 2003;12(4):291–298. [DOI] [PubMed] [Google Scholar]
- 34.Singer AJ, Thode H. Determination of the minimal clinically significant difference on a patient visual analog satisfaction scale. Acad Emerg Med 1998;5(10):1007–1011. [DOI] [PubMed] [Google Scholar]


