Abstract
Background
Although graduate medical education accrediting bodies recognize the importance of leadership for residents and encourage curricular development, it remains unclear which competencies are most important for early career physicians to possess.
Objective
To generate a prioritized list of essential postgraduate leadership competencies to inform best practices for future curricular development.
Methods
In 2019, we used a Delphi approach, which allows for generation of consensus, to survey internal medicine (IM) physicians in leadership roles with expertise in medical education and/or leadership programming within national professional societies. Panelists ranked a comprehensive list of established leadership competencies for health care professionals, across 3 established domains (character, emotional intelligence, and cognitive skills), on importance for categorical IM residents to perform by the end of residency. Respondents also identified number of content hours and pedagogical format best suited to teach each skill.
Results
Sixteen and 14 panelists participated in Delphi rounds 1 and 2, respectively (88% response rate). Most were female (71%) and senior (64% in practice > 15 years, 57% full professor). All practiced in academic environments and all US regions were represented. The final consensus list included 12 “essential” and 9 “very important” leadership skills across all 3 leadership domains. Emotional intelligence and character domains were equally represented in the consensus list despite being disproportionately underweighted initially. Panelists most frequently recommended content delivery via mentorship/coaching, work-based reflection, and interactive discussion.
Conclusions
This study's results suggest that postgraduate curricular interventions should emphasize emotional intelligence and character domains of leadership and prioritize coaching, discussion, and reflection for delivery.
Objectives
To create consensus around a prioritized list of leadership skills and competencies to guide curricular development for internal medicine (IM) residents.
Findings
The final consensus list included 12 “essential” and 9 “very important” leadership skills across all 3 established leadership domains (character, emotional intelligence, and cognitive skills). Emotional intelligence and character domains were equally represented despite being disproportionately underweighted initially.
Limitations
Given our Delphi panel was comprised of senior leaders in academic internal medicine, these findings may not be generalized to other populations (eg, levels of trainees, non-academic settings, specialties outside of IM) or speak to the perspectives of other members of the health care team.
Bottom Line
Postgraduate leadership curricular interventions should emphasize emotional intelligence and character domains of leadership, in addition to cognitive domains, and should prioritize coaching, discussion, and reflection as methods of delivery.
Introduction
Physicians lead complex, diverse teams in the domains of research, education, and patient care.1,2 Yet physician-leaders have been described as “accidental administrators,” often lacking training in skills necessary to be an effective leader.3–5 Given current challenges facing health care, the need for physicians to develop effective leadership skills is paramount.1,2,6,7
The call to action to increase formal and comprehensive leadership training for physicians and trainees is not new,1,2,8–10 and it has been the focus of several recent systematic reviews.11–13 Graduate medical education (GME) accrediting bodies have recognized the importance of leadership training for residents and have encouraged curricular development through published educational policy and guidance. The US Institute of Medicine report, Crossing the Quality Chasm: A New Health System for the 21st Century, emphasized the need to develop physician leaders across all levels.14 Subsequently, in 2013, the Association of American Medical Colleges added interprofessional collaboration and personal and professional development to its list of key competencies.15 Similarly, the Accreditation Council for Graduate Medical Education (ACGME) has listed leadership domains, including interpersonal communication, quality improvement, and systems-based practice, as milestones of residency education.16 Though trainees desire more leadership development during residency,17,18 few GME programs provide opportunities for leadership development, and published curricula are heterogenous in terms of content and delivery.12,13
Existing GME leadership development programs most commonly employ classroom-based didactics coupled with independent reading or discussion and reflection in the small group setting—neither of which provide opportunity for skills practice.11–13 Described curricula place a disproportionate level of focus on technical/conceptual knowledge and individual skill development, as opposed to other domains of effective leadership such as self-awareness, emotional intelligence, and organizational understanding.11–13 As stated by Sultan et al, the “competency-centric medical education culture” represents a likely driver of this skewed focus toward cognitive, skills-based leadership competencies.13 However, there have been increasing calls for a more comprehensive approach to leadership development—one that incorporates a deliberate focus on developing the (often neglected) leadership domains of emotional intelligence and character.19–21 The “character-competence entanglement” paradigm from Sturm et al describes the existence of a mutually reinforcing effect between character and competence that leads to extraordinary leadership performance.22
It remains unclear which domains and competencies are most important for early career physicians.11,23,24 Furthermore, published curricular interventions for trainees employ a variety of pedagogical methodologies.11–13 It is unknown if specific leadership skills or domains are best suited to a particular approach. We conducted a Delphi study with the primary aim of creating consensus around a prioritized list of leadership skills and competencies to guide curricular development for internal medicine (IM) residents.
Methods
The Delphi approach generates consensus from a panel of experts, is used to close gaps when empiric data is lacking,25–27 and works best with high-level concepts.28
Participants
We utilized a purposive sampling strategy to assemble a geographically diverse group of panelists with expertise in leadership and GME who represented clinical practice, research, education, administration, and quality improvement domains of leadership in keeping with the established Delphi practice.29 We were particularly interested in physician leaders within an academic environment who could speak to pedagogical considerations for content delivery. As such, in 2019, we recruited IM physicians in leadership roles with training and expertise in medical education and/or leadership programming within national professional societies (eg, Alliance for Academic Internal Medicine, Society of General Internal Medicine). We sought individuals who met at least one of the following inclusion criteria: (1) has presented on leadership topic at the national level; (2) has served in a GME leadership capacity with a designated leadership title within their institution; and/or (3) has served in a leadership capacity with a designated leadership title on a national GME committee within the aforementioned professional societies.
We emailed 44 potential panelists an invitation to participate in the study, which was conducted via a custom online Delphi survey system. There is no consensus on what constitutes an appropriate sample size of a Delphi study; studies with 6 panelists have been published, and a sample size of 12 or more is deemed reasonable.26,30 Given that a 70% response rate between rounds is needed to maintain study rigor,25 we sought to enroll 15 panelists in round 1 with at least 12 completing round 2. No incentive was offered.
Survey Method
Two authors (S.M., J.C.) with advanced training in medical education, national experience in teaching leadership development, and GME program leadership (J.C.) developed this survey (provided as online supplementary data). We identified a preliminary list of leadership skills to be included in this study through review of published literature regarding competencies for health care professions.11,24,31–35 We employed a framework that uses 3 established leadership development domains (character, emotional intelligence, and cognitive skills) to classify leadership skills, as described in a recent systematic review of leadership curricula in postgraduate medical education.13 This holistic perspective defines leaders (eg, those who inspire, engage, influence, empower) as demonstrating expertise across a variety of intellectual and affective competencies. This definition is also echoed in the broader business literature.21 Skills included were vetted by local experts with experience in leadership development and education to establish content validity. Five local, general IM, core residency faculty with expertise in leadership piloted the survey to establish response process validity. We employed 2 rounds of survey administration for all panelists.
Our initial contact included a standardized definition of physician leadership adapted from the American Medical Association: “consistent use by a physician of the leadership knowledge, skills, and expertise necessary to identify, engage, and elicit from each team member the unique set of contributions needed to help patients achieve their care goals.”36 During round 1, panelists ranked 28 leadership skills on importance (1 = not important, 2 = of little importance, 3 = somewhat important, 4 = very important, 5 = essential) for categorical IM residents to achieve competence by the second half of residency and apply during the first 3 to 5 years post-residency. For each skill, we also asked panelists to identify the number of content hours required for training and the ideal pedagogical method. We categorized pedagogical approaches as outlined in a recent systematic review13 of leadership development programs in GME. These included experiential, mentorship/coaching, work-based, theoretical learning, interactive discussion, reflection, and project-based. Round 1 also included a demographic questionnaire and an open-ended question to identify additional important topics.
We calculated median importance scores with IQRs from pooled, de-identified data. Consensus was defined a priori. Any skill ranked by > 70% of panelists as a Likert 4 or 5 (very important or essential) met automatic inclusion criteria. Any skill ranked by > 70% of panelists as a Likert 1 or 2 (not important or of little importance) met automatic exclusion, in accordance with typical definitions of consensus.26 Any skill not meeting these criteria was sent to round 2 for re-ranking.
During round 2, panelists reviewed their answers from round 1 along with pooled median importance scores with IQRs as well as descriptive pooled data regarding number of content hours and pedagogical methods. We then allowed panelists to adjust their responses after reviewing group distribution; however, we made it clear that they were not required to do so if their thoughts had not changed. Round 2 also included any new skills identified from free text responses in round 1. During round 2, respondents were also asked to identify up to 5 topics they felt to be critical to teach IM residents. The final list of consensus topics included all of those ranked as a Likert 4 or 5 by > 70% of panelists. We considered skills with a pooled median importance rating of > 4 as “essential” and those with a pooled median importance rating = 4 as “very important.”
Statistical Methods
As this was a Delphi survey, results are largely descriptive in nature. Medians and IQRs were computed for Likert-type responses, and frequencies and percentages were calculated for nominal variables. To compare methods for delivering leadership curricula, we computed and tested all pairwise differences in proportions between each of the 8 methodology options using Wald tests and assuming a multinomial distribution. Bonferroni-adjusted P values were computed, as we performed 28 pairwise comparisons. A familywise type I error rate of 0.05 was assumed.
This study was deemed to be exempt by our local institutional review board.
Results
Sixteen panelists completed round 1 (of 44, 36% response rate); 14 (of 16, 88% response rate) completed round 2. Table 1 shows demographics of the 14 panelists who completed demographic items. Panelists held a variety of high-level university, hospital, and national professional organization leadership roles (Table 1).
Table 1.
Demographic Characteristics of Delphi Panelist Respondents
| Survey Responses | Panelist Respondents (n = 14), n (%) |
| Gender identification | |
| Male | 4 (29) |
| Female | 10 (71) |
| Clinical practice | |
| 6–10 years | 3 (21) |
| 11–15 years | 2 (14) |
| > 15 years | 9 (64) |
| Rank | |
| Assistant | 1 (7) |
| Associate | 5 (36) |
| Full | 8 (57) |
| Practice environment | |
| Urban academic | 10 (71) |
| Suburban academic | 4 (29) |
| Work environment | |
| Inpatient | 3 (21) |
| Mix inpatient/outpatient | 7 (50) |
| Nonclinical | 1 (7) |
| US region | |
| Northeast | 3 (21) |
| Mid-Atlantic | 3 (21) |
| Midwest | 2 (14) |
| West | 2 (14) |
| South | 4 (29) |
| University and hospital leadership roles | |
| Chair of medicine | 1 (7) |
| Vice chair of education | 5 (36) |
| Department chair | 1 (7) |
| Program director | 5 (36) |
| Associate program director | 4 (29) |
| Associate dean | 3 (21) |
| Chief of medicine | 1 (7) |
| Division chief | 1 (7) |
| Section chief | 1 (7) |
| Associate section chief | 1 (7) |
| GME chair of patient safety and quality improvement | 1 (7) |
Abbreviation: GME, graduate medical education.
Survey Method
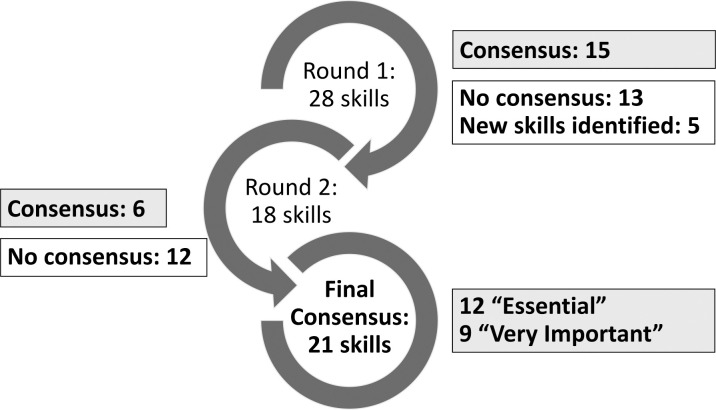
Of 28 leadership skills presented in round 1, 15 met automatic inclusion criteria, 0 met automatic exclusion criteria, and 13 did not generate consensus. Panelists generated 5 additional skills via free text response. Thus, round 2 was comprised of 18 skills, 13 without consensus from round 1 plus 5 additional skills (Figure). Of 18 skills included in round 2, 6 met automatic inclusion criteria, 0 met automatic exclusion criteria, and 12 did not generate consensus. Thus, our final consensus list included 12 “essential” and 9 “very important,” across all 3 leadership domains (6 character, 7 emotional intelligence, 8 cognitive skills; Table 2). Five of these skills were identified by > 30% of panelists as critical for residents to be taught (Table 3). Skills not meeting consensus for inclusion fell across the following domains: 1 character, 1 emotional intelligence, and 10 cognitive skills (Table 4).
Figure.
Overview of Outcomes, by Delphi Round, of Postgraduate Leadership Competencies for Internal Medicine Residents
Table 2.
“Essential” and “Very Important” Leadership Skills for Medical Residentsa
| Skill | Domain | N | Median (IQR) |
| Essential | |||
| The resident communicates effectively with individuals, across a spectrum of age, gender, ability, and social, cultural, religious, and ethnic backgrounds | Cognitive skills | 16 | 5.0 (5.0, 5.0) |
| The resident solicits and acts upon feedback from a variety of sources | Character | 16 | 5.0 (5.0, 5.0) |
| The resident treats mistakes as learning opportunities | Character | 16 | 5.0 (4.0, 5.0) |
| The resident can articulate one's own individual strengths and limitations | Emotional intelligence | 16 | 5.0 (4.0, 5.0) |
| The resident can articulate one's own personal and professional goals | Emotional intelligence | 16 | 5.0 (4.0, 5.0) |
| The resident has a clear sense of their role, responsibilities, and purpose within the team | Emotional intelligence | 16 | 5.0 (4.0, 5.0) |
| The resident values, respects, and promotes equality and diversity | Character | 16 | 5.0 (4.0, 5.0) |
| The resident takes appropriate action if ethics and values are compromised | Character | 16 | 5.0 (4.0, 5.0) |
| The resident delegates tasks to appropriate team members | Cognitive skills | 16 | 5.0 (4.0, 5.0) |
| The resident provides effective feedback to team members regarding performance | Cognitive skills | 16 | 5.0 (4.0, 5.0) |
| The resident actively seeks opportunities for personal learning and professional development | Emotional intelligence | 16 | 4.5 (4.0, 5.0) |
| The resident demonstrates self-awareness (eg, can identify when leadership skills are not working)b | Emotional intelligence | 14 | 4.5 (4.0, 5.0) |
| Very Important | |||
| The resident fosters collaboration (eg, actively seeks contributions, expertise, and views of others to build and sustain relationships) | Character | 16 | 4.0 (4.0, 5.0) |
| The resident can articulate individual values and principles, understanding how these may differ from those of others | Character | 14 | 4.0 (4.0, 5.0) |
| The resident appreciates that strong clinical leadership can provide opportunities to improve patient care | Cognitive skills | 16 | 4.0 (4.0, 5.0) |
| The resident plans workload and activities to fulfill work requirements and commitments, without compromising their own health (ie, maintains work-life balance) | Cognitive skills | 16 | 4.0 (4.0, 5.0) |
| The resident recognizes others' contributions and efforts, celebrating individual and team victories | Emotional intelligence | 14 | 4.0 (4.0, 5.0) |
| The resident employs effective conflict resolution strategies | Cognitive skills | 14 | 4.0 (4.0, 5.0) |
| The resident appreciates population, public, and social determinants of healthb | Cognitive skills | 14 | 4.0 (4.0, 5.0) |
| The resident adapts leadership style to a given situation | Emotional intelligence | 16 | 4.0 (3.5, 5.0) |
| The resident can define leadership | Cognitive skills | 14 | 4.0 (3.0, 4.0) |
Results from 2019 Delphi survey of panelists with expertise in leadership and in graduate medical education.
Skills generated by participants from round 1 free text responses.
Table 3.
Top 5 Critical Leadership Skills for Medical Residentsa
| Rank | Skill | Domain |
| 1 | The resident fosters collaboration (eg, actively seeks contributions, expertise, and views of others to build and sustain relationships) | Character |
| 2 | The resident communicates effectively with individuals, across a spectrum of age, gender, ability, and social, cultural, religious, and ethnic backgrounds | Cognitive skills |
| 3 | The resident treats mistakes as learning opportunities | Character |
| 4 | The resident can articulate one's own individual strengths and limitations | Emotional intelligence |
| 5 | The resident solicits and acts upon feedback from a variety of sources | Character |
Results from 2019 Delphi survey of panelists with expertise in leadership and in graduate medical education.
Table 4.
Leadership Skills Not Identified as Important for Postgraduate Medical Residentsa
| Skill | Domain |
| The resident can describe the characteristics, behaviors, and practices of various leadership styles | Cognitive skills |
| The resident takes into account the needs and work patterns of others | Emotional intelligence |
| The resident can facilitate/run an effective meeting | Cognitive skills |
| The resident coaches, mentors, or sponsors team members when appropriate | Cognitive skills |
| The resident understands work culture (eg, political, social, technical, economic, and organizational factors) | Character |
| The resident demonstrates effective change management skills (eg, creates shared vision, identifies stakeholders, engages leadership) | Cognitive skills |
| The resident understands the economics of medicine (eg, budgeting, fiscal planning, resource management, compensation) | Cognitive skills |
| The resident demonstrates effective project management (eg, project definition, risk management, obtains performance data, monitors outcomes) | Cognitive skills |
| The resident employs effective negotiation strategies | Cognitive skills |
| The resident understands appropriate use of social media, both by and for leadershipb | Cognitive skills |
| The resident understands the structures and processes of health care deliveryb | Cognitive skills |
| The resident understands principles of health system improvement (eg, principles/processes/tools, data, measurement)b | Cognitive skills |
Results from 2019 Delphi survey of panelists with expertise in leadership and in graduate medical education.
Skills generated by participants from round 1 free text responses.
Content Delivery
All panelists agreed that GME programs should include dedicated curricular time for leadership development for IM residents. Highest-ranked methods for delivering leadership curricula were “mentorship/coaching,” “work-based reflection,” and “interactive discussion,” which were chosen 27.4%, 27.7%, and 22.4% of the time, respectively. Pairwise comparisons in percentages between these top 3 formats and all other formats were significant with adjusted P values < .001. “Lecture” was the lowest-ranked format for content delivery. While experts generally recommended between 2 and 5 content hours per skill (range 0 to > 5 hours; median 2–3 hours; IQR 205 hours), they had varying recommendations regarding total number of content hours dedicated to leadership development (4–8 hours: 33%; 9–12 hours: 20%; > 12 hours: 40%).
Discussion
This study describes results of a rigorous Delphi survey of national experts to generate consensus on essential leadership competencies for IM residents. In addition to the prioritized list it generated, our study lends insight into optimal curricular methods to provide this education. These findings, including those that address feasibility and implementation, can help to inform best practices for future GME leadership curriculum development.
Interestingly, nearly two-thirds of skills identified in the final consensus list (13 of 21) and 80% (4 of 5) of skills identified as “critical” fell within character and emotional intelligence domains. Nearly all skills (10 of 12) excluded from the final list were categorized within the cognitive skills domain. Though the majority of published leadership development curricula focus on cognitive skills-based leadership competencies,13 our findings add to a growing body of evidence suggesting that leadership development programs should take a more comprehensive approach and include a strong focus on building character and developing emotional intelligence.19,20,22,37 Further, this work indicates that these more affective domains are perceived by experienced leaders to be equally as important for early career leaders and, in fact, might be more foundational than cognitive skills focused on by more executive-level leadership development programs.38 It is notable that, although identified as the most critical skill, collaboration was not identified as “essential” for IM residents by our participants. The inclusion of collaboration as one of the Association of American Medical Colleges' core competencies and its direct relation to the ACGME systems-based practice competency substantiates its critical designation.15,16
To date, few specialty-specific evaluations of specific leadership competencies for teaching leadership to residents have been undertaken. While it is possible that competencies may vary across specialty, a review of existing publications support the generalizability of our findings. More specifically, critical skills identified in this study, including collaboration, communication, and feedback, are identified as key competencies within surgical, emergency, and critical care settings.35,39,40 Similarly, character, emotional, and relational domains of leadership are emphasized both in the aforementioned settings39–41 and within pharmacy32 and nursing42 domains. Based on reviews of existing literature,39,40,43 one area in which leadership competencies for surgical specialties may diverge from our population of IM residents may be the need to incorporate additional cognitive-based skills such as group process, followership, emergent decision-making, and stress management, although these skills are also very important in procedure-based IM subspecialties.
Most recommended pedagogical methods involved small group teaching or direct observation and debrief through coaching and reflection. Didactic formats were rarely recommended for content delivery, suggesting that formal curricular time and space, a commonly cited barrier in GME, may not impede the development of programming in this content area. Our results, which address feasibility, allow GME programs to tailor work-based leadership programming to meet individual needs and curricular space. These findings are congruent with prior work examining best practices for leadership training and indicate curricula that employ multiple work-based pedagogical approaches and experiential learning are most effective and favored by learners.11,12,32,44
Unlike many of the leadership skills within the cognitive skills domain, which lend themselves well to competency-based medical education, no clear standards exist to evaluate the competency of medical trainees regarding emotional intelligence and character. GME needs validated character and emotional intelligence assessment tools applicable to our population of learners and may look to the larger business literature to adapt tools to our learners.45,46
Limitations of our Delphi study include that our results are reflective of the opinions of our expert panel, as is inherent in Delphi methodology. Our panel was made up of senior leaders in academic IM—their opinions may not be generalized to other populations (eg, levels of trainees, non-academic settings, specialties outside of IM) or speak to the perspectives of other members of the health care team. Further, we did not specifically collect data on the types of teams that our panelists had direct experience in leading, or if panelists had pursued formal leadership training or degrees. Panelists who participated have all accrued significant academic credentials and/or formal administrative titles. However, it cannot be assumed that panelists' experience directly translates to either expertise in the management of multidisciplinary teams, specifically, or to expertise in the most appropriate pedagogical method to teach each leadership skill.
Next steps in the continuation of this work might be to vet this consensus list of essential leadership skills with other key stakeholders (eg, recent graduates across a variety of academic and non-academic settings, patients, other members of the health care team) to corroborate or refute content.12,13 Finally, the total number of curricular hours required to teach all leadership skills that were deemed essential may exceed the total number of curricular hours most programs have available to dedicate to leadership development, unless leadership development curricula are embedded within the program's existing structure and framework. A key component for how GME programs should structure their leadership curricula should be based on a local needs assessment and available curricular space.
Conclusions
In summary, prior work has demonstrated the importance of creating targeted leadership skills development programs for IM residents, and our results describe a list of skills deemed most important by national experts. These results suggest that GME leadership curricular interventions should emphasize emotional intelligence and character domains of leadership, in addition to cognitive domains, and should prioritize coaching, discussion, and reflection as methods of delivery.
Supplementary Material
Acknowledgments
The authors would like to thank Ethan Lennox, MA, Division of General Internal Medicine, University of Pittsburgh School of Medicine, and Linda Quinn, Systems Analyst, Center for Research on Health Care Data Center, Department of Medicine, University of Pittsburgh School of Medicine.
Footnotes
Funding: The authors received a faculty development grant from the Division of General Internal Medicine, University of Pittsburgh School of Medicine to support this work.
Conflict of interest: The authors declare they have no competing interests.
This work was previously presented at the Annual Meeting of the Society of General Internal Medicine, Birmingham, AL, May 6–9, 2020.
References
- 1.Stoller JK. Developing physician-leaders: a call to action. J Gen Intern Med. 2009;24(7):876–878. doi: 10.1007/s11606-009-1007-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blumenthal DM, Bernard K, Bohnen J, Bohmer R. Addressing the leadership gap in medicine: residents' need for systematic leadership training. Acad Med. 2012;87(4):513–522. doi: 10.1097/ACM.0b013e31824a0c47. [DOI] [PubMed] [Google Scholar]
- 3.Ackerly D, Sangvai D, Udayakumar K, et al. Training the next generation of physician-executives: an innovative residency pathway in management and leadership. Acad Med. 2011;86(5):575–579. doi: 10.1097/ACM.0b013e318212e51b. [DOI] [PubMed] [Google Scholar]
- 4.McKimm J, Swanwick T. Leadership development for clinicians: what are we trying to achieve? Clin Teach. 2011;8(3):181–185. doi: 10.1111/j.1743-498X.2011.00473.x. [DOI] [PubMed] [Google Scholar]
- 5.Arroliga AC, Huber C, Myers JD, Dieckert JP, Wesson D. Leadership in health care for the 21st century: challenges and opportunities. Am J Med. 2014;127(3):246–249. doi: 10.1016/j.amjmed.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Bohmer R. Designing Care: Aligning the Nature and Management of Health Care. Boston MA Harvard Business Press. 2009;22–23:173–174. [Google Scholar]
- 7.Lee T. Turning doctors into leaders. Harv Bus Rev. 20102021 https://hbr.org/2010/04/turning-doctors-into-leaders Accessed June 21. [PubMed]
- 8.Stoller JK. Commentary: recommendations and remaining questions for health care leadership training programs. Acad Med. 2013;88(1):12–15. doi: 10.1097/ACM.0b013e318276bff1. [DOI] [PubMed] [Google Scholar]
- 9.Detsy AS. How to be a good academic leader. J Gen Intern Med. 2010;26(1):88–90. doi: 10.1007/s11606-010-1486-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alpert JS. Leadership in academic medicine. Am J Med. 2010;123(12):1071–1072. doi: 10.1016/j.amjmed.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Frich JC, Brewster AL, Cherlin EJ, Bradley EH. Leadership development programs for physicians: a systematic review. J Gen Intern Med. 2015;30(5):656–674. doi: 10.1007/s11606-014-3141-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadowski B, Cantrell S, Barelski A, O'Malley PG, Hartzell JD. Leadership training in graduate medical education: a systematic review. J Grad Med Educ. 2018;10(2):134–148. doi: 10.4300/JGME-D-17-00194.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sultan N, Torti J, Haddara W, Inayat A, Inayat H, Lingard L. Leadership development in postgraduate medical education: a systematic review of the literature. Acad Med. 2019;94(3):440–449. doi: 10.1097/ACM.0000000000002503. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine (US), Committee on Quality of Health Care in America. Crossing the Quality Chasm A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 15.Englander R, Cameron T, Ballard AJ, Dodge J, Bull J, Aschenbrener CA. Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Acad Med. 2013;88(8):1088–1094. doi: 10.1097/ACM.0b013e31829a3b2b. [DOI] [PubMed] [Google Scholar]
- 16.The Accreditation Council for Graduate Medical Education. Common Program Requirements. 2021 https://www.acgme.org/what-we-do/accreditation/common-program-requirements/ Accessed June 21.
- 17.Mittwede PN. On leadership and service during medical training. Acad Med. 2015;90(4):399. doi: 10.1097/ACM.0000000000000667. [DOI] [PubMed] [Google Scholar]
- 18.Brouns JW, Berkenbosch L, Ploemen-Suijker FD, Heyligers I, Busari JO. Medical residents' perceptions of the need for management education in the postgraduate curriculum: a preliminary study. Int J Med Educ. 2010;1:76–82. doi: 10.5116/ijme.4cd8.43f1. [DOI] [Google Scholar]
- 19.Branch WT., Jr Supporting the moral development of medical students. J Gen Intern Med. 2000;15(7):503–508. doi: 10.1046/j.1525-1497.2000.06298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bryan CS, Babelay AM. Building character: a model for reflective practice. Acad Med. 2009;84(9):1283–1288. doi: 10.1097/ACM.0b013e3181b6a79c. [DOI] [PubMed] [Google Scholar]
- 21.Goleman D. What makes a leader? Harv Bus Rev. 19982021 https://hbr.org/2004/01/what-makes-a-leader Accessed June 21. [PubMed]
- 22.Sturm RE, Dusya V, Crossan M. The entanglement of leader character and leader competence and its impact on performance. Leadersh Q. 2017;28(3):349–366. doi: 10.1016/j.leaqua.2016.11.007. [DOI] [Google Scholar]
- 23.Warren OJ, Carnall R. Medical leadership: why it's important, what is required, and how we develop it. Postgrad Med J. 2011;87(1023):27–32. doi: 10.1136/pgmj.2009.093807. [DOI] [PubMed] [Google Scholar]
- 24.Sonnino RE. Health care leadership development and training: progress and pitfalls. J Healthc Leadersh. 2016;12:19–29. doi: 10.2147/JHL.S68068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keeney S, Hasson F, McKenna HP. The Delphi technique in nursing and health research. Hoboken, NJ: Wiley-Blackwell; 2010. [Google Scholar]
- 26.Humphrey-Murto S, Varpio L, Gonsalves C, Wood TJ. Using consensus group methods such as Delphi and Nominal Group in medical education research. Med Teach. 2017;39(1):14–19. doi: 10.1080/0142159X.2017.1245856. [DOI] [PubMed] [Google Scholar]
- 27.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311(7001):376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsu CC, Sanford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12(10) doi: 10.7275/PDZ9-TH90. [DOI] [Google Scholar]
- 29.Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? J Adv Nurs. 1997;26(3):623–630. doi: 10.1046/j.1365-2648.1997.t01-25-00999.x. [DOI] [PubMed] [Google Scholar]
- 30.Murphy MK, Black NA, Lamping DL, et al. Consensus development methods and their use in clinical guideline development. Health Technol Assess. 1998;2(3):i–iv. 1–88. [PubMed] [Google Scholar]
- 31.Dath D, Chan MK, CanMEDS Abbott C. 2015 From Manager to Leader. 2021 www.royalcollege.ca/rcsite/documents/cbd/canmeds-2015-manager-to-leader-e.pdf Accessed June 21.
- 32.Janke KK, Traynor AP, Boyle CP. Competencies for student leadership development in doctor of pharmacy curricula to assist curriculum committees and leadership instructors. Am J Pharm Educ. 2013;77(10):222. doi: 10.5688/ajpe7710222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Webb AMB, Tsipis NE, McClellan TR, et al. A first step toward understanding best practices in leadership training in undergraduate medical education: a systematic review. Acad Med. 2014;89(11):1563–1570. doi: 10.1097/ACM.0000000000000502. [DOI] [PubMed] [Google Scholar]
- 34.Valani R, Sriharan A, Scolnik D. Integrating CanMEDS competencies into global health electives: an innovative elective program. CJEM. 2011;13(1):34–39. doi: 10.2310/8000.2011.100206. [DOI] [PubMed] [Google Scholar]
- 35.Thoma B, Poitras J, Penciner R, et al. Administration and leadership competencies: establishment of a national consensus for emergency medicine. CJEM. 2015;17(2):107–114. doi: 10.2310/8000.2013.131270. [DOI] [PubMed] [Google Scholar]
- 36.American Medical Association. Physician-led Team Based Care (2015) 2021 https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/about-ama/councils/Council%20Reports/council-on-medical-service/issue-brief-physician-led-team-based-care.pdf Accessed June 21.
- 37.Fernández-Aráoz C. Great People Decisions Why They Matter So Much Why They are So Hard and How You Can Master Them. Hoboken, NJ: John Wiley & Sons Inc; 2007. [Google Scholar]
- 38.Morahan PS, Gleason KA, Richman RC, Dannels S, McDade SA. Advancing women faculty to senior leadership in U.S. academic health centers: fifteen years of history in the making. J Women High Educ. 2012;3(1):137–162. [Google Scholar]
- 39.Brewster DJ, Butt WW, Gordon LJ, Rees CE. Leadership in intensive care: a review. Anaesth Intensive Care. 2020;48(4):266–276. doi: 10.1177/0310057X20937319. [DOI] [PubMed] [Google Scholar]
- 40.Tan YX, Jalal AHB, Ngai V, et al. What are the non-technical skills required by junior doctors in the NHS to manage medical emergencies? A scoping review. 2021] doi: 10.1136/postgradmedj-2020-139285. [published online ahead of print February 4. Postgrad Med J doi: [DOI] [PubMed]
- 41.Green ML, Winkler M, Mink R, et al. Defining leadership competencies for pediatric critical care fellows: results of a national needs assessment. Med Teach. 2017;39(5):486–493. doi: 10.1080/0142159X.2017.1297527. [DOI] [PubMed] [Google Scholar]
- 42.Heinen M, van Oostveen C, Peters J. An integrative review of leadership competencies and attributes in advanced nursing practice. J Adv Nurs. 2019;75(11):2378–2392. doi: 10.1111/jan.14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Watters DA, Smith K, Tobin S, Beasley SW. Follow the leader: followership and its relevance for surgeons. ANZ J Surg. 2019;89(5):589–593. doi: 10.1111/ans.14912. [DOI] [PubMed] [Google Scholar]
- 44.Fraser TN, Blumenthal DM, Bernard K, et al. Assessment of leadership training needs of internal medicine residents at the Massachusetts General Hospital. Proc (Bayl Univ Med Cent) 2015;28(3):317–320. doi: 10.1080/08998280.2015.11929260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Crossan MM, Byrne A, Seijts GH, Reno M, Monzani L, Gandz J. Toward a framework of leader character in organizations. J Manage Stud. 2017;54(7):986–1018. doi: 10.1111/joms.12254. [DOI] [Google Scholar]
- 46.Crossan M, Seijts G, Gandz J. Developing Leadership Character. New York, NY: Routledge; 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.