Abstract
Background
Increasing evidence suggests that structural stigma (e.g. discriminatory laws, policies and population attitudes) can give rise to minority stress reactions (i.e. rejection sensitivity, internalized homophobia and identity concealment) to compromise sexual minorities’ mental health. Yet, many sexual minorities encounter divergent structural stigma climates over the life course, with potential implications for their experience of minority stress reactions and mental health. We take advantage of sexual minority male migrants’ lifecourse-varying exposures to structural stigma contexts to examine this possibility.
Methods
A sample of 247 sexual minority men who had migrated from 71 countries to the low-structural-stigma context of Sweden completed a survey regarding migration experiences, minority stress reactions and mental health. This survey was linked to objective indices of structural stigma present in these men’s countries of origin, diverse in terms of structural stigma.
Results
Country-of-origin structural stigma was significantly associated with poor mental health and this association was mediated by rejection sensitivity and internalized homophobia, but only among those who arrived to Sweden at an older age and more recently.
Conclusions
Prolonged exposure to high levels of structural stigma can give rise to stressful cognitive, affective and behavioural coping patterns to jeopardize sexual minority men’s mental health; yet, these consequences of structural stigma may wane with increased duration of exposure to more supportive structural contexts.
Introduction
Sexual minorities across global contexts experience disproportionate rates of mental health problems compared with their heterosexual peers.1 Structural stigma includes discriminatory cultural norms (e.g. expectations that couples consist of opposite-gender members only), population attitudes (e.g. normative opinions that homosexuality is sinful) and societal laws and institutional policies (e.g. death penalty for homosexuality) that serve to keep sexual minorities out of reach of power and equal treatment. Given its role in diminishing life opportunities for stigmatized populations, structural stigma has been argued to be a key driver of sexual minorities’ poorer mental health.2–5 Perhaps the most convincing evidence that structural stigma might negatively impact sexual minorities’ mental health derives from natural experiments.5,6 While such studies provide initial support for structural stigma as a cause of sexual minorities’ poorer mental health, diverse methodologies are needed to further establish a causal impact of structural stigma on sexual minorities’ mental health.7
One methodological approach for strengthening causal inference for the role of structural stigma on sexual minorities’ mental health seeks to identify the mechanisms through which this association might operate. Structurally stigmatizing environments surrounding sexual minorities have been theorized to induce stigma-related minority stress reactions, such as stress related to the anticipation of being rejected because of one’s sexual orientation, the internalization of negative societal attitudes and concealing one’s sexual orientation, that could help explain how structural stigma compromises sexual minorities’ mental health.7–9 In fact, recent studies have found evidence that sexual orientation concealment mediates the association between structural stigma and sexual minority men’s mental health,3 providing initial support for such mechanistic pathways. Whether other pathways operate similarly to mediate the association between structural stigma and mental health remains largely unknown.
Still, yet another approach for strengthening causal inference would be to examine whether duration of structural stigma exposure affects mental health outcomes and hypothesized mechanisms. This approach would be particularly important given that few existing studies have examined the reversibility of the effect of structural stigma once exposure to it has been reduced or eliminated—a criterion required to establish causality.10 Therefore, examining the associations between structural stigma exposure, mental health and minority stress reactions as a function of length of exposure to structurally stigmatizing contexts would help strengthen causal inference regarding the role of structural stigma on sexual minorities’ mental health. Specifically, longer exposure to structural stigma may lead to poorer mental health for sexual minorities by instilling stressful, yet potentially adaptive, cognitive, affective and behavioural coping patterns the longer one lives under such conditions. Conversely, among sexual minorities who may have moved from a high-structural-stigma environment to a more supportive context, these negative effects might wane over time. Hence, sexual minorities who have moved from one structural stigma environment to another, spending varying amount of time in each, provide a unique opportunity to examine this possibility.
The current study aims to explore the association between structural stigma exposure, minority stress reactions and mental health, as a function of length of exposure to structural stigma among self-identified sexual minority men who have changed structural stigma environments. We hypothesized that: (i) higher levels of country-of-origin structural stigma will be associated with increased risk of poor mental health; (ii) this association will be mediated by minority stress reactions (i.e. sexual orientation-related rejection sensitivity, internalized homophobia and sexual orientation concealment); (iii) this association will be stronger among migrant sexual minority men who experienced longer exposure to their country-of-origin structural stigma (i.e. arrived at an older age to Sweden; more recently arrived to Sweden) and (iv) the indirect effects linking country-of-origin structural stigma and poor mental health through minority stress reactions will be stronger among those who experienced longer exposure to their country-of-origin structural stigma.
Methods
Participants
Between October 2017 and March 2018, 2615 individuals responded to an online survey on determinants of sexual minority men’s mental health in Sweden. Participants were recruited through advertisements on dating apps and social media (e.g. Qruiser.com). Of the 481 men who reported having been born outside of Sweden, 247 (51%) completed our study variables, were currently living in Sweden, self-identified as non-heterosexual and were therefore included in the current study. In comparison, among the 1817 men who reported having been born in Sweden, 1107 (61%) met these criteria.
Measures
Country-of-origin structural stigma
Structural stigma in participants’ country of origin was based on a country-level index of population attitudes and the presence of discriminatory laws and policies. Specifically, data on population attitudes towards sexual minorities in each country were derived from the Global Acceptance Index 2014–2017 across 174 countries.11 Data on discriminatory laws and unequal policies were derived from a report by the International Lesbian, Gay, Bisexual, Trans and Intersex Association on the global criminalization and the human rights situation of sexual minorities in 201612 and scored based on precedent.13 The attitudinal and legal measures were highly significantly correlated (r=0.77, P<0.001). Thus, a composite score of country-of-origin structural stigma was created by centring the measures’ averaged z-scores around the reference score for Sweden; while positive scores represented a change coming from a higher-structural-stigma country than Sweden, negative scores represented a change from a lower-structural-stigma country. Although participants were originally exposed to structural stigma specific to the time period of residing in their countries of origin, attitudinal data show that the relative rank ordering of structural stigma climates has been relatively stable over a total of 30 and 40 years across 174 countries and all US states, respectively.4,11 Therefore, the score is likely to represent the relative difference in structural stigma climates between country of origin and Sweden, regardless of year of migration to Sweden.
Years living in Sweden
Participants reported the number of years they have been living in Sweden.
Age of arrival to Sweden
Participants’ age of arrival to Sweden was calculated from the participants’ current age subtracted by the self-reported number of years they have been living in Sweden.
Mental health problems
Mental health problems were measured with the Brief Symptom Inventory-18 scale.14–16 With this scale, participants were asked to rate 18 items regarding depression, anxiety and somatization symptoms in terms of how distressed or bothered they were by these experiences over the past seven days. Response alternatives ranged from 0 = not at all to 4 = extremely (α=0.94).
Rejection sensitivity
Sexual orientation-related rejection sensitivity was measured as replies to 14 vignettes describing hypothetical rejection situations.17 Participants were asked to rate both how concerned or anxious they would be when exposed to each event and how likely it would be that this event would happen to them because of their sexual orientation on scales from 1 = very unconcerned or very unlikely to 6 = very concerned or very likely, respectively. The anxiety and likelihood scores for each item were summed to derive a total score (α=0.92).
Internalized homophobia
Internalized homophobia was measured with a nine-item scale regarding the way participants felt about being gay or bisexual.18 Participants were asked about the frequency of nine different thoughts and feelings in the past year, including the wish to ‘stop being attracted to men’ and the feeling that ‘being gay or bisexual was a personal shortcoming’, on a four-point scale from 1 = never to 4 = often, combined into a total sum score (α=0.91).
Sexual orientation concealment
Sexual orientation concealment was assessed as the degree of outness to five categories of individuals: ‘family’, ‘gay, lesbian and bisexual friends’, ‘straight friends’, ‘co-workers’, and ‘healthcare providers’.19 Response options were ‘out to none’, ‘out to some’, ‘out to most’, and ‘out to all’. As the data were highly skewed, sexual orientation concealment was dichotomously coded to capture either being out to any person across the different social groups (0 = not concealing) or out to none within any of the groups (1 = concealing).
Covariates
Since age has been linked to improved mental health,20 we controlled for it in analyses to ensure that the association between age of arrival to, or years living in, Sweden and mental health was not a function of increased age or the passage of time. Country-of-origin income inequality was used as a covariate to control for the strong association between living standard equality and population mental health21,22 and was measured using the Gini-index for each country, derived from the World Bank.23
Data analysis
To test the study hypotheses, we employed regression models in Mplus (version 8) using maximum likelihood with robust standard error estimates. We considered using multilevel modelling with participants clustered within country of origin, but as participants were not sampled within their country of origin or recruited based on their migration background, the participants were arguably not nested within their countries of origin by design. Other reasons to not employ multilevel modelling included the interclass correlation coefficient of poor mental health (range in ICC: 0.123–0.161), the high number of clusters (k = 71) and low mean cluster size (M = 3.48), resulting in a low design effect (range in deff: 1.30–1.39).24–26
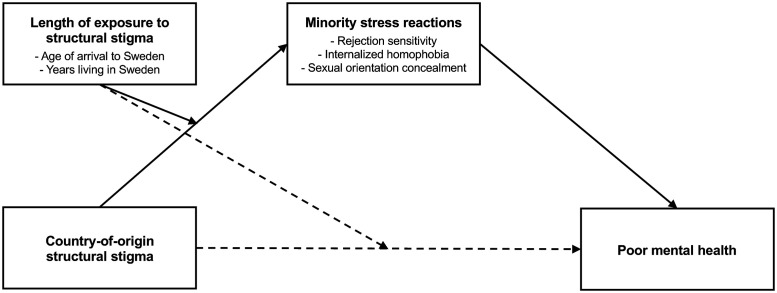
After examining whether descriptive statistics differed by country-of-origin structural stigma, we tested, in a stepwise approach,27 the mediation of poor mental health by country-of-origin structural stigma through three minority stress reaction mediators: rejection sensitivity, internalized homophobia and sexual orientation concealment. We then examined whether both age of arrival to Sweden and number of years living in Sweden moderated the associations of country-of-origin structural stigma with poor mental health and the proposed mediators. Finally, we tested moderated mediation models. We separately examined both age of arrival to and years living in Sweden as moderators of the association between country-of-origin structural stigma and each mediator (figure 1). To examine if indirect effects varied as a function of age of arrival to and years living in Sweden, conditional indirect effects were fixed at low and high values of both moderators: around the 15th (i.e. at 3 years) and the 85th percentile (i.e. at 30 years) of their respective distributions. All models and preparatory tests were adjusted for country-of-origin income inequality. In all analyses, a significance level of α=0.05 was used.
Figure 1.
Moderated mediation model whereby the association between structural stigma and poor mental health is mediated by rejection sensitivity, internalized homophobia and sexual orientation concealment, as moderated by length of exposure to structural stigma
Results
Sample demographic characteristics are presented in table 1 according to dichotomized country-of-origin structural stigma. Sexual minority men who had migrated from countries with higher-than-mean levels of structural stigma (n = 57) were younger and moved to Sweden at a younger age, compared with those who had migrated from countries with lower-than-mean structural stigma (n = 190).
Table 1.
Sample demographic characteristics and experiences of minority stress reactions and poor mental health, by country-of-origin structural stigma climate
| Total (n = 247) | Country-of-origin structural stigma |
P value | ||
|---|---|---|---|---|
| Higher than mean (n = 57) | Mean or lower than mean (n = 190) | |||
| Age, M (SD) | 34.6 (11.2) | 30.7 (7.4) | 36.8 (13.0) | 0.001* |
| Sexual orientation | 0.163** | |||
| Gay, % (n) | 73.3 (181) | 70.2 (40) | 74.2 (141) | |
| Bisexual, but mostly gay, % (n) | 15.0 (37) | 19.3 (11) | 13.7 (26) | |
| Bisexual, equally gay and heterosexual, % (n) | 4.0 (10) | 1.8 (1) | 4.7 (9) | |
| Bisexual, but mostly heterosexual, % (n) | 3.2 (8) | 1.8 (1) | 3.7 (7) | |
| Pansexual, % (n) | 1.6 (4) | 1.8 (1) | 1.6 (3) | |
| Queer, % (n) | 2.0 (5) | 1.8 (1) | 2.1 (4) | |
| Uncertain or don’t know, % (n) | 0.8 (2) | 3.5 (2) | 0.0 (0) | |
| Education | 0.406** | |||
| Attended higher education, % (n) | 69.2 (171) | 73.7 (42) | 67.9 (129) | |
| Employment | 0.951** | |||
| Unemployed, % (n) | 3.6 (9) | 3.5 (2) | 3.7 (7) | |
| Personal income | 0.852** | |||
| Above the country mean, % (n) | 35.8 (87) | 36.8 (21) | 35.5 (66) | |
| Age of arrival to Sweden, M (SD) | 19.0 (11.6) | 16.4 (10.6) | 20.0 (12.1) | 0.045* |
| Years living in Sweden, M (SD) | 16.2 (14.0) | 14.1 (12.5) | 16.8 (14.5) | 0.203* |
| Rejection sensitivity, M (SD) | 166.0 (110.3) | 211.1 (123.6) | 153.1 (103.0) | 0.001* |
| Internalized homophobia, M (SD) | 15.1 (7.0) | 18.6 (7.8) | 14.0 (6.3) | <0.001* |
| Sexual orientation concealment, % (n) | 37.3 (82) | 57.1 (28) | 31.6 (54) | 0.001** |
| Poor mental health, M (SD) | 17.4 (14.6) | 23.3 (15.7) | 15.7 (13.1) | <0.001* |
P values based on a Student’s t-test.
P values based on a chi-square test.
Mediation of the association between structural stigma and poor mental health by minority stress reactions
As an initial step, greater country-of-origin structural stigma was significantly associated with poorer mental health (b = 1.799, P=0.005); this association remained significant while further adjusting for age of arrival to Sweden (b = 1.353, P=0.036) or the number of years living in Sweden (b = 1.927, P=0.003). Higher levels of country-of-origin structural stigma were significantly associated with increased rejection sensitivity (b = 18.925, P=0.001), internalized homophobia (b = 1.115, P=0.001) and sexual orientation concealment (b = 0.054, P=0.010); these associations remained significant while further adjusting for age of arrival to and years living in Sweden. While further adjusting for country-of-origin structural stigma, to test covariance regardless of the independent variable, and age of arrival to and years living in Sweden, both rejection sensitivity (b = 0.037, P<0.001) and internalized homophobia (b = 0.689, P<0.001) were significantly associated with poor mental health. We found no significant direct association between sexual orientation concealment and poor mental health (P=0.058).
In mediation models, greater country-of-origin structural stigma was indirectly associated with poor mental health through increased rejection sensitivity (b = 0.681, P=0.005; 41% of the total effect, b = 1.647, P=0.033) and internalized homophobia (b = 0.677, P=0.011; 44% of the total effect, b = 1.526, P=0.017), when further adjusting for age of arrival to and years living in Sweden. We found no remaining significant direct effects of country-of-origin structural stigma on poor mental health in the context of these mediators (P=0.127 and P=0.214, respectively). We found no significant indirect effect through sexual orientation concealment (P=0.194).
Moderation by age of arrival to, and years living in, Sweden of the indirect association between structural stigma and poor mental health through minority stress reactions
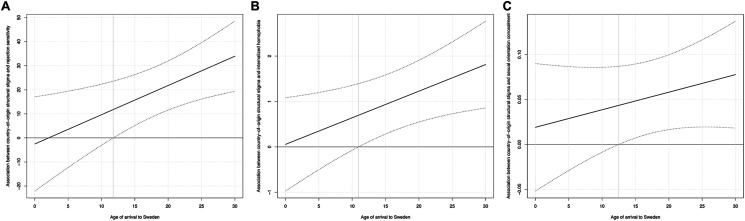
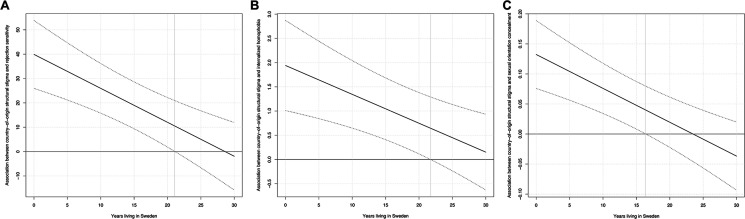
As an initial step, we found no significant moderation by age of arrival to Sweden of the association between country-of-origin structural stigma and poor mental health, when further adjusting for years living in Sweden (P=0.316). We also found no significant moderation by years living in Sweden of the association between country-of-origin structural stigma and poor mental health, when further adjusting for age of arrival to Sweden (P=0.093). While further adjusting for years living in Sweden, age of arrival to Sweden significantly moderated the associations between country-of-origin structural stigma and both rejection sensitivity (b = 1.215, P=0.009) and internalized homophobia (b = 0.059, P=0.022), such that the positive associations between country-of-origin structural stigma and both rejection sensitivity and internalized homophobia became stronger with increased age of arrival to Sweden (significant after the age of 12 and 11, respectively; figure 2a–c). However, we found no such significant moderation effect by age of arrival to Sweden of the association between country-of-origin structural stigma and the likelihood of sexual orientation concealment (P=0.260). While further adjusting for age of arrival to Sweden, we found significant moderation effects by years living in Sweden of the association between country-of-origin structural stigma and increased rejection sensitivity (b=−1.395, P<0.001), internalized homophobia (b=−0.060, P=0.002) and sexual orientation concealment (b=−0.006, P<0.001), such that the positive associations between country-of-origin structural stigma and rejection sensitivity, internalized homophobia and sexual orientation concealment became weaker with the increased number of years living Sweden (non-significant after 22, 22 and 17 years, respectively; figure 3a–c).
Figure 2.
Confidence bands of the associations between country-of-origin structural stigma and minority stress reactions [i.e. (a) rejection sensitivity, (b) internalized homophobia and (c) sexual orientation concealment] as a function of age of arrival to Sweden. Figures depict the 95% confidence band of the association, which is statistically significant for values of age of arrival to Sweden that do not include zero.
Figure 3.
Confidence bands of the associations between country-of-origin structural stigma and minority stress reactions [i.e. (a) rejection sensitivity, (b) internalized homophobia and (c) sexual orientation concealment] as a function of years living in Sweden. Figures depict the 95% confidence band of the association, which is statistically significant for values of years living in Sweden that do not include zero.
In moderated mediation models, we found a significant indirect association between country-of-origin structural stigma and poor mental health through rejection sensitivity, which included both age of arrival to and years living in Sweden as moderators of the pathway between country-of-origin structural stigma and rejection sensitivity. This indirect effect was conditional on the combination of older age of arrival to Sweden (i.e. 30 years) and fewer years living in Sweden (i.e. 3 years), b = 1.363, P=0.003. Conditional indirect effects for other fixed-moderator-value combinations were non-significant: arrived at a younger age to Sweden (i.e. 3 years) while living in Sweden for longer (i.e. 30 years) (P=0.680) or arrived at an older age to Sweden (i.e. 30 years) while living in Sweden for longer (i.e. 30 years) (P=0.847). In the context of these indirect effects, we found no remaining direct effect of country-of-origin structural stigma on poor mental health (P=0.145). Furthermore, we found a significant indirect association between country-of-origin structural stigma and poor mental health through internalized homophobia, which included both age of arrival to and years living in Sweden as moderators of the pathway between country-of-origin structural stigma and internalized homophobia. This indirect effect was conditional on the combination of older age of arrival to Sweden (i.e. 30 years) and fewer years living in Sweden (i.e. 3 years), b = 1.118, P=0.006. Conditional indirect effects for other fixed-moderator-value combinations were non-significant: arrived at a younger age to Sweden (i.e. 3 years) while living in Sweden for longer (i.e. 30 years) (P=0.930) or arrived at an older age to Sweden (i.e. 30 years) while living in Sweden for longer (i.e. 30 years) (P=0.615). In the context of these indirect effects, we found no remaining direct effect of country-of-origin structural stigma on poor mental health (P=0.204). We did not find significant conditional indirect effects in a similar moderated mediation model with sexual orientation concealment as the mediator.
Discussion
Taking advantage of a unique sample of sexual minority men who were born in 71 countries diverse in structural stigma and now living in Sweden, this study helps to strengthen causal inference in understanding the role of structural stigma on sexual minority men’s mental health. Specifically, this study finds that structural stigma in sexual minority male migrants’ countries of origin continues to be associated with their mental health even upon migrating to another structural stigma context. Those who moved from higher-structural-stigma countries reported worse mental health, greater rejection sensitivity and greater internalized homophobia and were more likely to conceal their sexual orientation than those who moved from lower-structural-stigma countries. This study does not find evidence that the association between country-of-origin structural stigma and mental health depends on age of arrival to and number of years living in Sweden. Yet, this study finds that the association between country-of-origin structural stigma and poor mental health was mediated by rejection sensitivity and internalized homophobia (but not by sexual orientation concealment) and that these indirect effects were stronger for those who had moved to Sweden at an older age and more recently.
Combined with the fact that psychosocial mechanisms and poor mental health are unlikely to cause structural stigma, the present findings further facilitate causal inference into the detrimental role of structural stigma on sexual minorities’ mental health in two notable ways. First, this study is among the few to examine potential mechanisms to explain how structural stigma might jeopardize sexual minority mental health and it represents the first known identification of rejection sensitivity and internalized homophobia as such mechanistic factors. Indeed, while minority stress theory hypothesizes that distal stressors such as structural stigma might ‘get under the skin’ to harm sexual minority mental health through these factors,7–9 no previous research has found support for this possibility. The one mechanism linking structural stigma to reduced sexual minority mental health that has been previously identified—sexual orientation concealment3—was unexpectedly not found to play such a role in the present study. This divergence from previous studies could potentially be explained by how sexual minorities may employ concealment to navigate their stigmatizing environments. While country-of-origin structural stigma was associated with concealment, concealment was in turn not associated with poorer mental health. In fact, a recent meta-analysis of sexual orientation concealment and poor mental health finds only a small association between the two,28 raising that possibility that concealment is often an adaptive protection against poor mental health for sexual minorities.4,29–31
Second, by examining these mechanisms as functions of duration of structural stigma exposure, this study was able to observe dose-response relationships and to model the reversibility of structural stigma effects: two requirements for causal inference in epidemiology.10 Specifically, our results show that the positive associations between structural stigma and both rejection sensitivity and internalized homophobia, as well as the mediating indirect effects of these minority stress reactions on the association between structural stigma and poor mental health, were only present among those sexual minority men who migrated to Sweden both at an older age and more recently. Among those who migrated at a younger age or among those who had lived in Sweden for a longer period, there was no link between country-of-origin stigma and these minority stress reactions. These results suggest that longer exposure to structural stigma might instill in sexual minority men certain stressful cognitive, affective and behavioural coping patterns, such as rejection sensitivity and internalized homophobia, to drive poor mental health. Conversely, our findings suggest that with longer exposure to more supportive structural climates, these mentally taxing coping patterns might wane, with benefits for mental health.
Study results must be interpreted in light of several limitations. First, our sample is not representative of all sexual minority male migrants or even those living in Sweden given the non-probabilistic sampling used in this study. Second, data missingness among sexual minority male migrants was considerable but no information was available regarding reasons for non-response. Third, we used age of arrival to Sweden as a proxy for duration of direct exposure to country-of-origin structural stigma, assuming participants migrated directly to Sweden from their country of birth. This precludes examination of indirect routes to Sweden, including through multiple diverse structural contexts. Fourth, although survey questions regarding migration history enabled us to estimate the temporal effects of structural stigma exposure, the cross-sectional nature of our data does not allow for direct causal conclusions. Finally, we did not assess other intersecting experiences of stigma, such as structural racism and xenophobia, which are known to affect sexual minority migrants to and within Europe.32–34 In fact, previous research has found that length of time since migration is associated with other health-risk behaviours among migrants, including HIV risk behaviour and substance use, perhaps as a function of exposure to structural racism or xenophobia upon arrival.35,36 Future studies should extend our findings by using an intersectional structural stigma approach.34
Conclusion
Taking advantage of a unique sample of sexual minority male migrants to Sweden from 71 countries, this study demonstrates that country-of-origin structural stigma might generate rejection sensitivity and internalized homophobia, which in turn, mediate the association between country-of-origin structural stigma and mental health as a function of length of time exposed to country-of-origin structural stigma. While our findings suggest that prolonged exposure to higher levels of structural stigma may induce cognitive, affective and behavioural coping patterns with potential negative consequences for mental health, we find that these stressful reactions may, in turn, wane over time upon exposure to more supportive structural environments. Taking advantage of the diverse life-course structural contexts encountered by sexual minority male migrants to Sweden, this study further facilitates causal inference when interpreting associations between structural stigma and sexual minority mental health.
Funding
The current study was financially supported by grants from the Swedish Research Council [grant number 2016-01707] and the Swedish National Research School for Healthcare Sciences [grant number 2015-0133]. The funding agencies were not involved in study design, data collection, analyses, data interpretation or the reporting of the study.
Conflicts of interest: None declared.
Key points
This study advances understanding of structural stigma’s association with mental health by taking advantage of the divergent structural stigma climates experienced by sexual minority male migrants.
The study specifically finds that structural stigma is associated with rejection sensitivity, internalized homophobia and poor mental health as a function of sexual minority men’s length of exposure to structural stigma in their countries of origin.
Findings suggest that improving structural climates for sexual minorities may be an effective means to reduce the mental toll of minority stress.
References
- 1. Plöderl M, Tremblay P.. Mental health of sexual minorities. A systematic review. Int Rev Psychiatry 2015;27:367–85. [DOI] [PubMed] [Google Scholar]
- 2. Pachankis JE, Hatzenbuehler ML, Starks TJ.. The influence of structural stigma and rejection sensitivity on young sexual minority men's daily tobacco and alcohol use. Soc Sci Med 2014;103:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pachankis JE, Bränström R.. Hidden from happiness: structural stigma, sexual orientation concealment, and life satisfaction across 28 countries. J Consult Clin Psychol 2018;86:403–15. [DOI] [PubMed] [Google Scholar]
- 4. Van der Star A, Pachankis JE, Bränström R.. Country-level structural stigma, school-based and adulthood victimization, and life satisfaction among sexual minority adults: a life course approach. J Youth Adolesc 2020;50:189–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hatzenbuehler ML, Bränström R, Pachankis JE.. Societal-level explanations for reductions in sexual orientation mental health disparities: results from a ten-year, population-based study in Sweden. Stigma Health 2018;3:16–26. [Google Scholar]
- 6. Raifman J, Moscoe E, Austin SB, McConnell M.. Difference-in-differences analysis of the association between state same-sex marriage policies and adolescent suicide attempts. JAMA Pediatr 2017;171:350–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hatzenbuehler ML. Structural stigma: research evidence and implications for psychological science. Am Psychol 2016;71:742–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hatzenbuehler ML, Pachankis JE.. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: research evidence and clinical implications. Pediatr Clin North Am 2016;63:985–97. [DOI] [PubMed] [Google Scholar]
- 9. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Sex Orientat Gend Divers 2013;1:3–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bradford Hill A. The environment and disease: association or causation? J Roy Soc Med 1965;58:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Flores A. Social Acceptance of LGBT People in 174 Countries, 1981 to 2017. Los Angeles, CA: The Williams Institute; 2019. [Google Scholar]
- 12. Carroll A. State-Sponsored Homophobia 2016: A World Survey of Sexual Orientation Laws: Criminalisation, Protection and Recognition. Geneva: International Lesbian, Gay, Bisexual, Trans and Intersex Association; 2016. [Google Scholar]
- 13. Pachankis JE, Bränström R.. How many sexual minorities are hidden? Projecting the size of the global closet with implications for policy and public health. PLoS One 2019;14:e0218084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Derogatis LR, Melisaratos N.. The Brief Symptom Inventory: an introductory report. Psychol Med 1983;13:595–605. [PubMed] [Google Scholar]
- 15. Derogatis LR. Brief Symptom Inventory (BSI)-18: Administration, Scoring and Procedures Manual. Minneapolis, MN: NCS Pearson; 2001. [Google Scholar]
- 16. Meijer RR, De Vries RM, Van Bruggen V.. An evaluation of the Brief Symptom Inventory–18 using item response theory: which items are most strongly related to psychological distress? Psychol Assess 2011;23:193–202. [DOI] [PubMed] [Google Scholar]
- 17. Pachankis JE, Goldfried MR, Ramrattan ME.. Extension of the rejection sensitivity construct to the interpersonal functioning of gay men. J Consult Clin Psychol 2008;76:306–17. [DOI] [PubMed] [Google Scholar]
- 18. Martin JL, L. Summary of D.. Measures: Mental Health Effects of AIDS on at-Risk Homosexual Men. New York, NY: Columbia University, Mailman School of Public Health; 1992. [Google Scholar]
- 19. Meyer IH, Rossano L, Ellis JM, Bradford J.. A brief telephone interview to identify lesbian and bisexual women in random digit dialing sampling. J Sex Res 2002;39:139–44. [DOI] [PubMed] [Google Scholar]
- 20. Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med 2000;30:11–22. [DOI] [PubMed] [Google Scholar]
- 21. Layte R. The association between income inequality and mental health: testing status anxiety, social capital, and neo-materialist explanations. Eur Sociol Rev 2012;28:498–511. [Google Scholar]
- 22. Wilkinson RG. Unhealthy Societies: The Afflictions of Inequality. London: Routledge; 1996. [Google Scholar]
- 23.World Bank. International Comparison Program Database: GINI Index. Washington, DC: World Bank; 2020. [Google Scholar]
- 24. Muthén BO, Satorra A.. Complex sample data in structural equation modeling. Sociol Methodol 1995;25:267–316. [Google Scholar]
- 25. Lai MHC, Kwok O-M.. Examining the rule of thumb of not using multilevel modeling: the “design effect smaller than two” rule. J Exp Educ 2015;83:423–38. [Google Scholar]
- 26. Bliese PD. Group size, ICC values, and group-level correlations: a simulation. Organ Res Methods 1998;1:355–73. [Google Scholar]
- 27. Baron R, Kenny D.. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–82. [DOI] [PubMed] [Google Scholar]
- 28. Pachankis JE, Mahon C, Jackson SD, et al. Sexual orientation concealment and mental health: a meta-analytic review. Psychol Bull 2020;146:831–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pachankis JE. The psychological implications of concealing a stigma: a cognitive-affective-behavioral model. Psychol Bull 2007;133:328–45. [DOI] [PubMed] [Google Scholar]
- 30. Pachankis JE, Cochran SD, Mays VM.. The mental health of sexual minority adults in and out of the closet: a population-based study. J Consult Clin Psychol 2015;83:890–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Van der Star A, Pachankis JE, Bränström R.. Sexual orientation openness and depression symptoms: a population-based study. Psychol Sex Orientat Gen Divers 2019;6:369–81. [Google Scholar]
- 32. Sältenberg H. Queer migrants in Sweden: subjectivities and spatiotemporal multiplicities. Diss., Lund University, Linköping, 2016. [Google Scholar]
- 33. Terzoglou F. Out of the closet, into the lagom (?): perceptions and feelings of inclusion, exclusion, and belonging among queer migrants in Sweden. Diss., Linköping University, Linköping, 2020. [Google Scholar]
- 34. Pachankis JE, Hatzenbuehler ML, Berg RC, et al. Anti-LGBT and anti-immigrant structural stigma: an intersectional analysis of sexual minority men’s HIV risk when migrating to or within Europe. J Acquir Immune Defic Syndr 2017;76:356–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Egan JE, Frye V, Kurtz SP, et al. Migration, neighborhoods, and networks: approaches to understanding how urban environmental conditions affect syndemic adverse health outcomes among gay, bisexual and other men who have sex with men. AIDS Behav 2011;15:35–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gelpí-Acosta C, Pouget ER, Reilly KH, et al. Time since migration and HIV risk behaviors among Puerto Ricans who inject drugs in New York City. Subst Use Misuse 2016;51:870–81. 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]