Abstract
Background
In ulcerative colitis, a pouchitis is the most common long-term adverse effect after proctocolectomy and ileal pouch-anal anastomosis. Approximately 5% of patients develop chronic antibiotic-dependent or antibiotic-refractory pouchitis without any effective treatment. The aim of this trial was to investigate the efficacy and safety of fecal microbiota transplantation in the treatment of chronic pouchitis.
Methods
This was a single-center, double-blinded, parallel group trial comparing donor fecal microbiota transplantation with placebo (autologous transplant) in chronic pouchitis. Twenty-six patients were recruited at the Helsinki University Hospital between December 2017 and August 2018 and were randomly allocated a 1:1 ratio to either donor fecal microbiota transplantation or placebo. The protocol included 2 transplantations into the pouch on weeks 0 and 4, and patients were followed up for 52 weeks.
Results
Nine patients in the intervention group and 8 patients in the placebo group relapsed during the 52-week follow-up, and the relapse-free survival did not differ between the groups (P = 0.183, log-rank; hazard ratio, 1.90 [95% confidence interval, 0.73-4.98; P = 0.190]). In the subgroup analysis of patients using continuous antibiotics before the study, the relapse-free survival was shorter in the intervention group (P = 0.004, log-rank; hazard ratio, 13.08 [95% confidence interval, 1.47-116.60; P = 0.021]). No major adverse effects were reported.
Conclusions
The fecal microbiota transplantation treatment regime used in our study was not effective in the treatment of chronic pouchitis. The safety profile of fecal microbiota transplantation was good.
ClinicalTrials.gov identifier
Keywords: chronic pouchitis, fecal microbiota transplantation, ulcerative colitis
INTRODUCTION
Despite more effective medical treatment in recent years, a substantial proportion of patients with ulcerative colitis (UC) still need surgery. Approximately 20% to 30% of patients with UC undergo surgery at some point during their disease course.1 For the majority of those patients, restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the operation of choice. The most prevalent long-term adverse effect after IPAA for UC is pouchitis. It seems that pouchitis is not an isolated disease entity but is rather a disease spectrum ranging from acute antibiotic-responsive pouchitis to antibiotic-refractory chronic pouchitis. Up to 50% of patients with UC develop at least 1 episode of pouchitis at 10-year follow-up, and up to 80% develop pouchitis at 30-year follow-up.2 In approximately 5% of those patients, pouchitis becomes chronic.3
The etiology remains unclear. There is clinical evidence implicating that pouch microbiota plays an important role in the pathogenesis of pouchitis. Fecal stasis because of altered bowel anatomy and an increased microbial load in the pouch mucosa results in colon-like mucosa, ie, colonic metaplasia, of the ileal pouch, which in turn creates an environment susceptible to inflammation.4 In addition, colonic metaplasia induces a dysbiosis of the pouch toward colon-like microbiota.5 In patients operated on for familiar adenomatous polyposis, pouchitis is far less likely,6 suggesting that genetic factors may also have a role in its pathogenesis.
Increased stool frequency, bloody stools, urgency, incontinence, and abdominal pain characterize the condition. Initial acute episodes typically respond to antibiotic therapy such as ciprofloxacin or metronidazole, but some patients become dependent on antibiotics or develop refractory disease. Currently, there is no established effective treatment for chronic antibiotic-dependent or antibiotic-refractory pouchitis. In fact, chronic pouchitis is one cause for excision of the pouch and permanent ileostomy; approximately 11% of pouch excisions are caused by chronic pouchitis.7 Different treatments for chronic pouchitis have been tested including immunomodulatory treatments used in UC, but long-term remission is seldom achieved.8-10 Probiotics, especially products containing many strains, such as VSL#3, have been effective in some studies.11 It is worth noting that there are only a few randomized trials evaluating the treatment methods for chronic pouchitis.
It has been shown that fecal microbiota transplantation (FMT) through colonoscopy is an effective treatment for recurrent Clostridioides difficile infection,12,13 which is currently the only clinical indication of FMT with sufficient evidence of benefit.14,15 Research has also investigated FMT in other disorders with increasing intensity.16,17 The results of FMT in the treatment of inflammatory bowel diseases are inconsistent, but some studies have shown FMT to have efficacy over placebo.18
The aim of our study was to investigate the long-term efficacy and safety of FMT in the treatment of chronic pouchitis in a randomized, double-blinded, placebo-controlled trial with a follow-up of 52 weeks.
MATERIALS AND METHODS
Study Design
We conducted a single-center, double-blinded, parallel group trial comparing FMT from a healthy donor with autologous FMT as the placebo treatment in maintenance therapy in patients with chronic pouchitis. Patients were randomly allocated in a 1:1 ratio to either FMT or placebo. The institutional review board and ethics committee of Helsinki University Hospital approved the study. The trial is registered with ClinicalTrials.gov (NCT03378921).
Participants
Patients were recruited at the Helsinki University Hospital between December 2017 and August 2018. Inclusion criteria were previous IPAA surgery for UC, endoscopically and histologically diagnosed pouchitis within 6 months before FMT, and frequent or continuous use of antibiotics because of the chronic pouchitis. We defined chronic pouchitis as having a duration of symptoms longer than 4 weeks. Frequent use of antibiotics was defined as a need for antibiotic treatment more than once within 1 year before recruitment to the study. Exclusion criteria were age < 18 years or > 75 years, use of immunosuppressive or immunomodulatory medication, and pregnancy. One of the exclusion criteria was also a suspicion or established diagnosis of Crohn disease. However, no patient had to be excluded because of this criterion. All patients provided written informed consent.
Interventions
The study protocol included 2 fecal transplants on weeks 0 and 4, first through flexible endoscopy and second via transanal catheter. If the patient was on antibiotics, then the antibiotic treatment was discontinued at least 36 hours before the first FMT. Patients were allowed to continue probiotics during the trial. All patients were instructed to take loperamide 2 mg half an hour before each procedure to keep the transplant in the J pouch for as long as possible.
After the patients gave consent, they were invited to pouchoscopy for the first FMT. Bowel preparation was not done before the procedure. All patients brought their own fresh fecal sample with them. In addition, all patients were asked to fill in the health-related quality of life 15D form (https://www.15d-instrument.net/15d/). An experienced endoscopist performed the pouchoscopy and took biopsy specimens from the J pouch and from the afferent limb. Meanwhile, a microbiologist prepared the fecal transplant (the donor’s frozen stool or the patient’s own fresh stool) in another room according to the allocated group. The preparation of fecal transplant from fresh or frozen stool was done according to the method described previously.19 Next, 170 mL of prepared fecal transplant containing 30 g of fecal material was infused into the afferent limb through the flexible endoscopy. Patients allocated to the FMT group had the transplant prepared from donor fecal material and freeze-stored at –80°C, and patients allocated to the placebo group had the transplant prepared from their own fresh stool. After the procedure, patients were instructed to postpone defecation as long as possible.
The donor of fecal material was a healthy woman aged 52 years with normal body weight (body mass index < 25), had not received antibiotics or probiotics within 6 months, and did not have any intestinal symptoms. The donor was screened according to the protocol described by Mattila et al12 and updated later in the international guidelines prepared by the European FMT Working Group.14 The donor’s fecal material had been previously used successfully in patients with recurrent C. difficile infection. We selected only 1 donor to minimize confounding factors.
Four weeks after the first fecal transplant, all patients were invited to a clinical visit and were instructed to bring their own fresh fecal sample with them. If a patient had relapsed before the second fecal transplant and had restarted antibiotics, he or she was instructed to discontinue the antibiotic treatment 36 hours before the second transplantation. The transplant was installed into the J pouch trough catheter (Torbot Medena Catheter 30Fz) according to the allocated group. As with the first FMT, the transplant was prepared by the same microbiologist in another room while the treating physician discussed the procedure with the patient.
Follow-up in both groups included a telephone interview 12 and 26 weeks after the first FMT and a clinical visit with pouchoscopy 52 weeks after the first FMT. In addition, patients were instructed to immediately report any adverse effect, gastrointestinal symptoms, or use of antibiotics for any indication. The clinical portion of the Pouchitis Disease Activity Index (PDAI)20 was assessed at 4, 12, and 26 weeks, and a total PDAI score was calculated at baseline and at 52 weeks when endoscopic and histologic data were also available. A pathologist examined all biopsy specimens of the pouch and afferent limb. Fecal samples for calprotectin measurement and later microbiota analysis were collected before the first FMT and at 4, 12, 26, and 52 weeks after the first FMT.
Outcomes
The primary outcome was remission defined as a PDAI score <7 and no need for antibiotic treatment of pouchitis during the 52-week follow-up. The secondary objective was to evaluate changes in the gut microbiota. Unfortunately, the recent lockdown measurements because of the COVID-19 pandemic restricted our laboratory activities for research and delayed the microbiota analysis significantly. Analysis of the gut microbiota has now begun, and the secondary outcomes will be reported later when the results become available.
Sample Size
Most of the previous FMT studies on pouchitis (case series) used single FMT with varying results. The only study using multiple FMTs suggested a remission rate of 80% (4 of 5 patients).21 In our study, we wanted to compare whether FMT is superior to placebo. The sample size (n = 26) was calculated according to the estimation that the remission rate in the FMT group would be 80% and 25% in the placebo group during the follow-up of 1 year. This difference of 55% was considered to be clinically meaningful. The significance level was selected to be 5%, and the power was set to 90%.
Randomization and Masking
The study nurse used block randomization with a varying block size (6 or 10). She informed the microbiologist about the allocated group by telephone and had no further role in this study. The recruiters, treating doctors, data collector, and patients were unaware of the randomization during the 52-week study period. Blinding was removed after all data were collected.
Statistical Analysis
In the analysis of baseline characteristics, we compared categorical variables using the χ 2 test or the Fisher exact test. Continuous variables were presented as mean and SD or median and range and were compared using the Mann-Whitney U test. Follow-up started on the date of the first FMT. We used the Kaplan-Meier method for the survival curves and the log-rank test to compare relapse-free survival between the groups. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using Cox regression analysis. We analyzed the follow-up data using pairwise comparisons. Each timepoint was compared separately to baseline. We calculated the difference between each timepoint and baseline and compared the groups using the Mann-Whitney U test or the linear-by-linear association test. We considered P values <0.05 to be statistically significant and used a 2-tailed test. Missing data, if any, are stated within the tables. We used SPSS Statistics 25 software (IBM Corporation, Armonk, NY) for the statistical analyses. No changes in the study protocol occurred after the trial started.
RESULTS
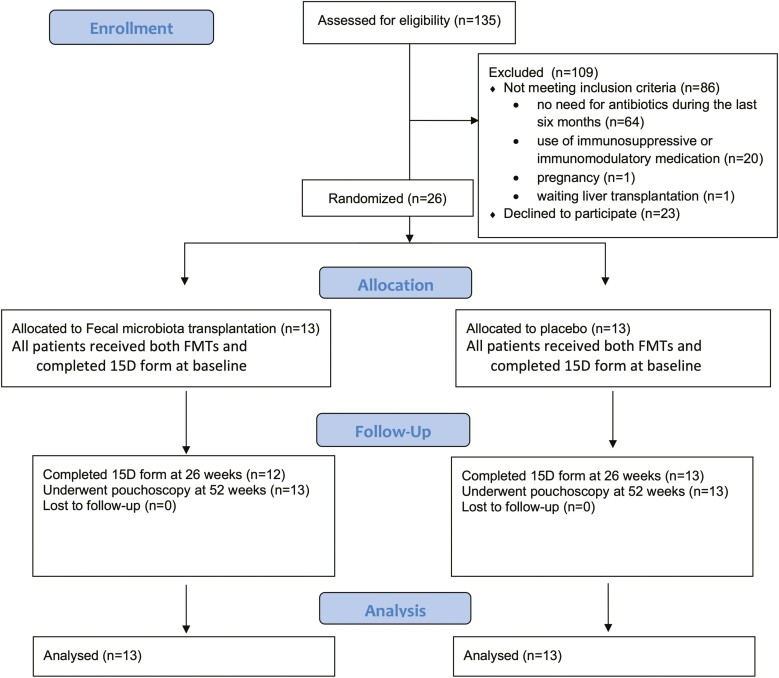
In total, 135 patients were assessed for eligibility at Helsinki University Hospital (Fig. 1). Of those, 86 patients met an exclusion criterion and 23 declined to participate. The remaining 26 patients were enrolled and randomly allocated to the treatment (donor FMT or placebo). All randomized patients received their allocated treatment and were followed for 52 weeks.
FIGURE 1.
Patient flow diagram.
Patient baseline characteristics were similar between the groups (Table 1). Five patients in the FMT group and 7 patients in the placebo group were using antibiotics continuously for chronic pouchitis at the time of study enrollment, and 8 patients in the FMT group and 6 patients in the placebo group were using repeated courses of antibiotics for chronic pouchitis when necessary. Patients were allowed to continue using probiotics during the study, and 5 patients in the FMT group and 6 patients in the placebo group decided to do so. All of these patients used probiotics comprising four strains of lactobacilli, three strains of bifidobacteria, and one strain of Streptococcus thermophilus.(VSL#3).
TABLE 1.
Baseline Characteristics
| FMT (n = 13) | Placebo (n = 13) | P | |
|---|---|---|---|
| Male sex | 7 (53.8%) | 8 (61.5%) | 0.691 |
| Mean age, y ± SD | 42.7 ± 10.2 | 45.5 ± 11.7 | 0.614 |
| Median y from IPAA surgery | 9.8 (1.6-21.9) | 8.3 (3.0-26.6) | 0.918 |
| Antibiotic use at time of study enrollment | 0.431 | ||
| Continuous use | 5 | 7 | |
| Repeated | 8 | 6 | |
| Probiotics | 5 | 6 | 0.691 |
Patients tolerated the FMT treatments well. In the FMT group, 3 patients reported an adverse effect within 1 week after FMT, including fever, abdominal pain, and fecal urgency. One of the patients in the FMT group lost a few kilograms because of nausea. All of these symptoms were self-limited. In the placebo group, 1 patient reported fever. Patients reported no major adverse effects.
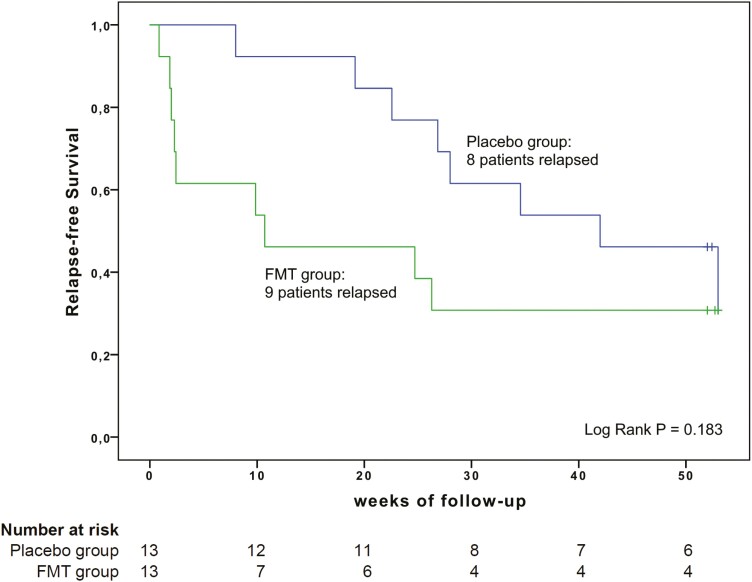
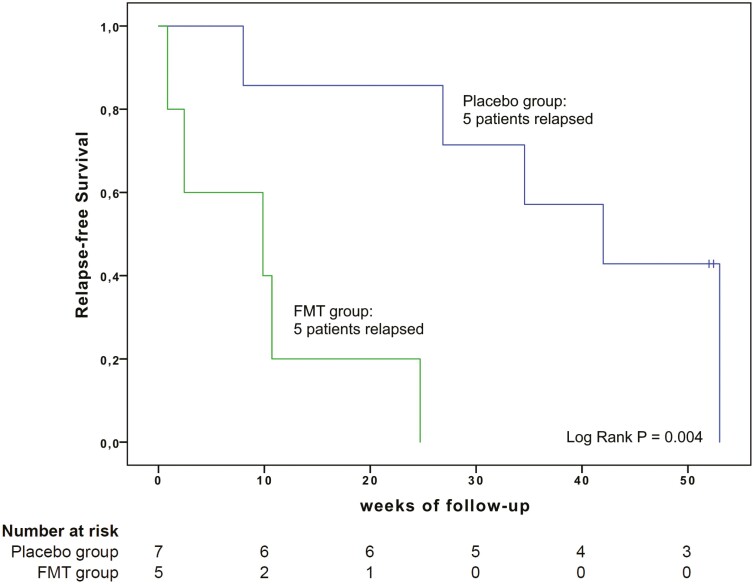
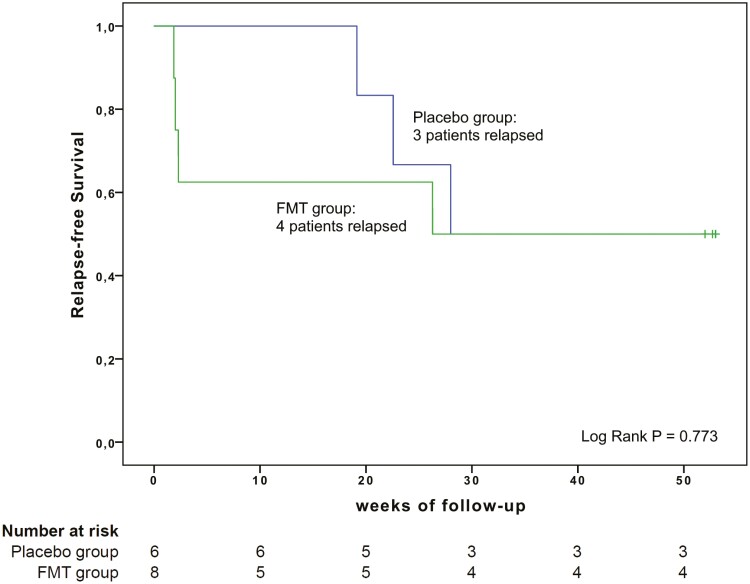
Overall, 9 patients in the FMT group and 8 patients in the placebo group relapsed during the 52-week follow-up (log-rank P = 0.183; Fig. 2). The difference was not significant. However, 5 patients in the FMT group relapsed even before the second fecal transplant, whereas in the placebo group no one relapsed during the first 4 weeks. Cox regression analysis showed a significantly increased hazard for relapse in the FMT group in patients using continuous antibiotics before the study when compared with the placebo group (P = 0.021; HR, 13.08; 95% CI, 1.47-116.60), but no difference was observed in the patients using repeated courses of antibiotics when necessary (P = 0.774; HR, 1.25; 95% CI, 0.28-5.60) (Table 2). The Kaplan-Meier results were consistent with the results from the Cox regression analysis (Figs. 3 and 4). Despite this finding, the patients in the FMT group reported an improved quality of life after 26 weeks of follow-up when compared with the placebo group (P = 0.036). We found no other significant differences regarding the follow-up data. Detailed information on the follow-up data can be found in Supplementary Table 1.
FIGURE 2.
Kaplan-Meier curve for relapse-free survival in placebo group and FMT group.
TABLE 2.
Primary Outcome
| 95% CI | ||||||
|---|---|---|---|---|---|---|
| Relapse-Free Survival Time (wks) (range minimum-maximum) | FMT (n = 13) | Placebo (n = 13) | HR | Lower | Upper | P |
| All patients | 10.7 (0.9-53.0) | 42.0 (8.0-53.0) | 1.902 | 0.727 | 4.977 | 0.190 |
| Patients with continuous use of antibiotics | 9.9 (0.9-24.7) | 42.0 (8.0-53.0) | 13.076 | 1.466 | 116.599 | 0.021 |
| Patients with repeated courses of antibiotics | 39.1 (1.9-53.0) | 40.0 (19.1-53.0) | 1.246 | 0.278 | 5.592 | 0.774 |
Cox regression analysis for relapse-free survival time.
FIGURE 3.
Relapse-free survival in patients using continuous antibiotics for chronic pouchitis before the trial.
FIGURE 4.
Relapse-free survival in patients using repeated courses of antibiotics for chronic pouchitis when necessary before the trial.
DISCUSSION
This study represents the first completed randomized controlled trial of FMT for the treatment of chronic pouchitis. We found that FMT does not seem to be effective treatment for chronic pouchitis with the used treatment protocol. Patients in the FMT group relapsed even earlier than patients in the placebo group. Interestingly, patients in the FMT group were more satisfied with their quality of life after 26 weeks of follow-up. The short- and long-term safety of FMT was good. Only minor adverse effects were observed within the adjacent days after FMT.
Herfarth et al22 performed a placebo-controlled double-blinded trial consisting of a single FMT via pouchoscopy followed by daily oral FMT for 2 weeks in patients with chronic pouchitis. Their study was stopped after enrolling 6 patients because of the low clinical remission rate and poor engraftment of the donor’s microbiota. One patient achieved clinical remission, and the donor’s microbiota seemed to colonize only in this patient. In a recent pilot study, Kousgaard et al23 observed a higher rate of the donor’s microbiota engraftment in 6 out of 9 patients. In their study, patients were treated by FMT enemas for 14 continuous days and followed up for 6 months. Three patients remained in remission. It thus seems that engraftment of donor microbiota is achieved better with multiple, frequent transplantations to the pouch. In our study, patients received 2 FMTs with a 4-week interval, and the first FMT was inserted into the afferent limb to lengthen the time of the FMT in the pouch before defecation. However, 5 patients in the treatment group relapsed even before the second FMT, whereas none in the placebo group relapsed between the first and the second FMT. It is possible that newly introduced microbes from the donor induced an inflammatory response in these patients, but the associated microbial changes remain to be assessed.
It is noteworthy that in this trial we did not preselect the donor based on microbiota characteristics, which may have had an impact on the clinical outcome. In a study by Moayyedi et al24 on FMT for active UC, the favorable outcome in 7 out of 9 patients was linked to a single donor, a so-called super-donor. However, the superiority of some donors over others in specific indications remains elusive and is difficult to determine prospectively. With current knowledge, we are not able to predict which donors could be optimal for pouchitis or any other specific indication. In our future studies we will analyze FMT-induced microbial changes in this cohort and correlate microbial composition to disease activity in time in individual patients. The assessment of microbiota engraftment from the donor and the identification of bacterial species associated with remission may help researchers select optimal donors for future studies. Optimally, it could be possible to identify a subgroup of patients who could benefit from FMT or another form of bacteriotherapy.
Overall, there are only a few studies about FMT in the treatment of chronic pouchitis, and more research is needed. In addition to the previously mentioned studies, there have been 3 prospective uncontrolled cohort studies and 3 case reports, reporting on 37 patients in total. One of the cohort studies used a single FMT infusion via nasogastric tube with 25% (2/8) of patients achieving clinical response, but no patient achieved clinical remission.25 Another cohort study of 18 patients used single FMT via pouchoscopy. The authors did not find any difference in PDAI scores, but there was improvement in bowel movement frequency and a trend to improvement in abdominal pain after 4 weeks of FMT.26 In the third cohort study, multiple FMT infusions were administered into the jejunum during esophagogastroduodenoscopy, 4 out of 5 patients achieved clinical remission, and the fifth patient achieved clinical response.21 All 3 case reports used single FMT via pouchoscopy with mixed results. Fang et al27 reported a resolution of symptoms of 1 patient at the 3-month follow-up, but another single-patient case report did not find any response.28 In the third case report, 1 of 3 patients achieved clinical response at 8 weeks after FMT, but no one achieved clinical remission.29 Overall, it seems that only a fraction of patients with pouchitis could benefit from FMT with the treatment protocols used thus far.
Future studies should investigate microbial dynamics, their association with clinical symptoms, and the possibilities of modulating pouch microbiota by FMT or other means. Our future analyses will increase knowledge about FMT-induced microbial changes in pouchitis and will show whether long-term alterations in pouch microbiota were achieved in any of the patients. If not, then the next step is to consider alternative ways to alter the pouch microbiota to increase its anti-inflammatory properties. Our donor was a healthy adult whose fecal material had been used successfully to treat patients with recurrent C. difficile infection but who may not have been an optimal donor for patients with pouchitis. It could be that FMT from a preselected super-donor with a specific gut microbiota composition would result in better treatment outcomes of chronic pouchitis in the future. Furthermore, the optimal number of FMT infusions and the time interval between them needs to be determined. In our unit, we do not use bowel preparation before pouchoscopy, and we chose to omit bowel preparation in this study as well. This decision may have had an impact on the colonization of the donor’s microbiota and FMT efficacy. Only 2 of the previously reported FMT studies for pouchitis used bowel preparation.26,29
This trial has some limitations. First, the study was powered to detect the superiority of FMT. We did the power calculation according to those few studies available at the time of initiation of the trial protocol. It now seems that the remission rate may be poorer than expected, which may cause a type 2 error. Second, we included patients with continuous use of antibiotics for chronic pouchitis and patients with frequent use of antibiotics for chronic pouchitis. Microbiota colonization may be different in these groups, which could have influenced the results of this study. However, there was a similar distribution of these patients between our study groups. Finally, patients tended to prolong the initiation of antibiotic therapy longer than they would normally because of the ongoing trial. Thus, the relapse-free survival time may actually be shorter in both groups.
This trial has several strengths. First, it is double-blinded, and there were no incidences of ineffective blinding. Second, we had a long follow-up of 1 year, and no patient was lost to follow-up.
CONCLUSIONS
Our clinical results suggest that FMT is not effective in the treatment of chronic pouchitis with the treatment protocol that was used in this study. We found that FMT was well tolerated and did not cause any major adverse effects. Further microbial analyses are warranted to associate specific taxa with pouchitis remission and relapse to understand how pouch microbiota could be modulated for sustained remission.
Supplementary Material
Supported by: This work was supported by State Research Funding (grant number TYH2019204), the Mary and Georg C Ehrnroth Foundation, and the Academy of Finland (grant number 323156). The research was independent of the research funding sources.
REFERENCES
- 1. Biondi A, Zoccali M, Costa S, et al. . Surgical treatment of ulcerative colitis in the biologic therapy era. World J Gastroenterol. 2012;18:1861–1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lightner AL, Mathis KL, Dozois EJ, et al. . Results at up to 30 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Inflamm Bowel Dis. 2017;23:781–790. [DOI] [PubMed] [Google Scholar]
- 3. Keränen U, Luukkonen P, Järvinen H. Functional results after restorative proctocolectomy complicated by pouchitis. Dis Colon Rectum. 1997;40:764–769. [DOI] [PubMed] [Google Scholar]
- 4. de Silva HJ, Millard PR, Soper N, et al. . Effects of the faecal stream and stasis on the ileal pouch mucosa. Gut. 1991;32:1166–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kohyama A, Ogawa H, Funayama Y, et al. . Bacterial population moves toward a colon-like community in the pouch after total proctocolectomy. Surgery. 2009;145:435–447. [DOI] [PubMed] [Google Scholar]
- 6. Lovegrove RE, Tilney HS, Heriot AG, et al. . A comparison of adverse events and functional outcomes after restorative proctocolectomy for familial adenomatous polyposis and ulcerative colitis. Dis Colon Rectum. 2006;49:1293–1306. [DOI] [PubMed] [Google Scholar]
- 7. Tulchinsky H, Hawley PR, Nicholls J. Long-term failure after restorative proctocolectomy for ulcerative colitis. Ann Surg. 2003;238:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kelly OB, Rosenberg M, Tyler AD, et al. . Infliximab to treat refractory inflammation after pelvic pouch surgery for ulcerative colitis. J Crohns Colitis. 2016;10:410–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barreiro-de Acosta M, García-Bosch O, Gordillo J, et al. . Efficacy of adalimumab rescue therapy in patients with chronic refractory pouchitis previously treated with infliximab: a case series. Eur J Gastroenterol Hepatol. 2012;24:756–758. [DOI] [PubMed] [Google Scholar]
- 10. Bär F, Kühbacher T, Dietrich NA, et al. ; German IBD Study Group . Vedolizumab in the treatment of chronic, antibiotic-dependent or refractory pouchitis. Aliment Pharmacol Ther. 2018;47:581–587. [DOI] [PubMed] [Google Scholar]
- 11. Gionchetti P, Rizzello F, Helwig U, et al. . Prophylaxis of pouchitis onset with probiotic therapy: a double-blind, placebo-controlled trial. Gastroenterology. 2003;124:1202–1209. [DOI] [PubMed] [Google Scholar]
- 12. Mattila E, Uusitalo-Seppälä R, Wuorela M, et al. . Fecal transplantation, through colonoscopy, is effective therapy for recurrent Clostridium difficile infection. Gastroenterology. 2012;142:490–496. [DOI] [PubMed] [Google Scholar]
- 13. Hvas CL, Dahl Jørgensen SM, Jørgensen SP, et al. . Fecal microbiota transplantation is superior to fidaxomicin for treatment of recurrent Clostridium difficile infection. Gastroenterology. 2019;156:1324–1332.e3. [DOI] [PubMed] [Google Scholar]
- 14. Cammarota G, Ianiro G, Tilg H, et al. ; European FMT Working Group . European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017;66:569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cammarota G, Ianiro G, Kelly CR, et al. . International consensus conference on stool banking for faecal microbiota transplantation in clinical practice. Gut. 2019;68:2111–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lahtinen P, Jalanka J, Hartikainen A, et al. . Randomised clinical trial: faecal microbiota transplantation versus autologous placebo administered via colonoscopy in irritable bowel syndrome. Aliment Pharmacol Ther. 2020;51:1321–1331. [DOI] [PubMed] [Google Scholar]
- 17. Halkjær SI, Christensen AH, Lo BZS, et al. . Faecal microbiota transplantation alters gut microbiota in patients with irritable bowel syndrome: results from a randomised, double-blind placebo-controlled study. Gut. 2018;67:2107–2115. [DOI] [PubMed] [Google Scholar]
- 18. Oka A, Sartor RB. Microbial-based and microbial-targeted therapies for inflammatory bowel diseases. Dig Dis Sci. 2020;65:757–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Satokari R, Mattila E, Kainulainen V, et al. . Simple faecal preparation and efficacy of frozen inoculum in faecal microbiota transplantation for recurrent Clostridium difficile infection—an observational cohort study. Aliment Pharmacol Ther. 2015;41:46–53. [DOI] [PubMed] [Google Scholar]
- 20. Sandborn WJ, Tremaine WJ, Batts KP, et al. . Pouchitis after ileal pouch-anal anastomosis: a Pouchitis Disease Activity Index. Mayo Clin Proc. 1994;69:409–415. [DOI] [PubMed] [Google Scholar]
- 21. Stallmach A, Lange K, Buening J, et al. . Fecal microbiota transfer in patients with chronic antibiotic-refractory pouchitis. Am J Gastroenterol. 2016;111:441–443. [DOI] [PubMed] [Google Scholar]
- 22. Herfarth H, Barnes EL, Long MD, et al. . Combined endoscopic and oral fecal microbiota transplantation in patients with antibiotic-dependent pouchitis: low clinical efficacy due to low donor microbial engraftment. Inflamm Intest Dis. 2019;4:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kousgaard SJ, Michaelsen TY, Nielsen HL, et al. . Clinical results and microbiota changes after faecal microbiota transplantation for chronic pouchitis: a pilot study. Scand J Gastroenterol. 2020;55:421–429. [DOI] [PubMed] [Google Scholar]
- 24. Moayyedi P, Surette MG, Kim PT, et al. . Fecal microbiota transplantation induces remission in patients with active ulcerative colitis in a randomized controlled trial. Gastroenterology. 2015;149:102–109.e6. [DOI] [PubMed] [Google Scholar]
- 25. Landy J, Walker AW, Li JV, et al. . Variable alterations of the microbiota, without metabolic or immunological change, following faecal microbiota transplantation in patients with chronic pouchitis. Sci Rep. 2015;5:12955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Selvig D, Piceno Y, Terdiman J, et al. . Fecal microbiota transplantation in pouchitis: clinical, endoscopic, histologic, and microbiota results from a pilot study. Dig Dis Sci. 2020;65:1099–1106. [DOI] [PubMed] [Google Scholar]
- 27. Fang S, Kraft CS, Dhere T, et al. . Successful treatment of chronic pouchitis utilizing fecal microbiota transplantation (FMT): a case report. Int J Colorectal Dis. 2016;31:1093–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schmid M, Frick JS, Malek N, et al. . Successful treatment of pouchitis with vedolizumab, but not fecal microbiota transfer (FMT), after proctocolectomy in ulcerative colitis. Int J Colorectal Dis. 2017;32:597–598. [DOI] [PubMed] [Google Scholar]
- 29. Nishida A, Imaeda H, Inatomi O, et al. . The efficacy of fecal microbiota transplantation for patients with chronic pouchitis: a case series. Clin Case Rep. 2019;7:782–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.