Abstract
Background
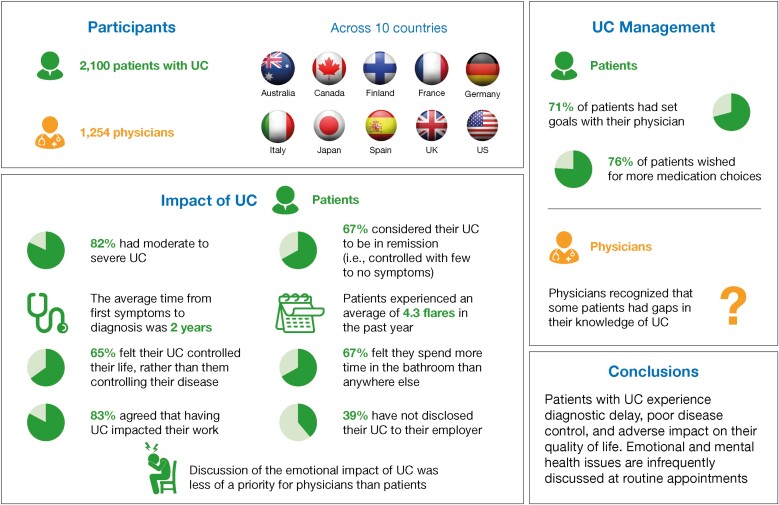
The Ulcerative Colitis (UC) Narrative is a global patient and physician survey aimed at identifying the impact of UC and comparing and contrasting perceptions of UC burden and management approaches.
Methods
Surveys of patients with UC (self-reported diagnosis; n = 2100) and physicians (n = 1254) were completed across 10 countries by The Harris Poll between August 2017 and February 2018. Questionnaires covered multiple aspects of UC, including diagnosis, treatment, and impact on patient quality of life, in addition to standard demographic information. Descriptive statistics are reported.
Results
The majority of patients (82%) had moderate to severe UC (based on medication history; those who had only ever taken 5-aminosalicylates were excluded); 67% described their UC as controlled with few to no symptoms. On average, patients experienced 4.3 flares (standard deviation, 7.4) in the past year. Diagnostic delay was on average 2.0 years (standard deviation, 5.4); 42% of patients waited ≥1 year. Most patients (65%) felt that UC controlled their life rather than them controlling their disease. Because of the fear of repercussions, many patients had not disclosed their UC to their employer. Discussion of the emotional impact of UC during routine appointments was less of a priority for physicians, compared with patients.
Conclusions
The data from this global survey highlight that patients with UC experience diagnostic delay, poor disease control, and adverse impact on their quality of life. Patients report UC to be a mentally exhausting condition; however, emotional and mental health issues are infrequently discussed at routine appointments.
Keywords: ulcerative colitis, patient survey, quality of life, inflammatory bowel disease
Graphical Abstract
Graphical Abstract.
INTRODUCTION
Ulcerative colitis (UC) is a chronic disabling inflammatory bowel disease (IBD) requiring lifelong medical follow-up and medical or surgical treatments.1 Because of the unpredictable disease course and frequent fluctuations in the severity of physical symptoms, patients with UC often experience a significant impact on their quality of life.2 To date, only a few studies have reported on the impact of UC on patients’ lives. A survey of patients with UC in Germany revealed a high psychosocial burden on patients.3 A more recent survey of patients with UC in Spain concluded that UC management requires a more patient-centered approach that includes psychological, emotional, and social aspects.4
Previous surveys of patients with UC and healthcare professionals (HCPs) identified differences between patients’ and HCPs’ perceptions of the impact of UC symptoms on patients’ lives. The results from these surveys showed that HCPs underestimated the effect of specific UC symptoms on patients,5 whereas many patients considered their symptoms and flares to be normal.2 A previous patient survey suggested medical management alone to be insufficient in allowing patients to live a “normal life”, with adaptation strategies and outside support influencing patient management of their UC.6 Management of UC should be governed by shared decision-making with well-informed patients;7 therefore, patient education on disease knowledge is paramount.8
The UC Narrative is composed of 2 related global surveys (1 patient-based and 1 physician-based) to engage patients with UC and physicians to characterize how the disease affects people living with UC. The survey explored several aspects of living with UC, including day-to-day disease impact, disease management, goal-setting, and communication. Here, we report patient and physician responses to survey questions relating to disease etiology and the impact of living with UC.
MATERIALS AND METHODS
Study Design and Populations
The UC Narrative is an initiative sponsored by Pfizer Inc and directed by a global advisory panel comprising of adults living with UC, leading gastroenterologists, IBD nurses, a psychologist, and representatives of identified IBD patient advocacy organizations from 10 countries: Australia, Canada, Finland, France, Germany, Italy, Japan, Spain, the United Kingdom, and the United States. The surveys were designed to assess multiple aspects of UC and its management, in addition to standard demographic information (Supplementary Table 1 in Supplementary Materials).
A detailed description of the UC Narrative Survey, including the patient and physician populations, has been reported by Rubin et al.9 In brief, eligible patients (aged ≥18 years) were those with a confirmed endoscopic diagnosis of UC who had not had a colectomy, but had visited a gastroenterologist/internist in the past 12 months and had ever taken prescription medication for their UC (see Supplementary Materials 1, 2). Eligible physicians saw ≥10 patients with UC per month (≥5 in Japan), with at least 10% of their patients currently taking a biologic for UC (see Supplementary Materials 1, 3).
Analyses of Patient and Physician Surveys
The methodology for the analysis of patient and physician survey responses is described in Rubin et al9 and is summarized in Supplementary Materials 1.
Patient-Reported Outcomes
In the patient survey, patients self-reported remission and flares. Remission was defined as UC being controlled with few to no symptoms, and a flare was defined as a period with a dramatic increase in symptoms compared with those typically experienced. These definitions were included in the survey questions (refer to Supplementary Materials 2).
Ethical Considerations
In the United States, the research method and survey questionnaire were reviewed and received independent review board approval (Western Institutional Review Board PRO number 20171627). The surveys were noninterventional, were not intended to provide clinical data for treatment decisions, and were not conducted as a clinical trial for any endpoints; ethics approval was therefore not required. Both patients and physicians provided their consent before completing the questionnaire and received remuneration (on behalf of the investigators by the sponsor [Pfizer Inc]) for their participation in the survey.
RESULTS
Survey Respondents
Across 10 countries, 2100 patients with UC responded to the patient survey and 1254 physicians responded to the physician survey (Table 1 and Supplementary Table 2 in Supplementary Materials). Patient disease characteristics and demographics, and physician demographics, are presented in Table 1. Globally, 67% of patients self-reported being in remission, although a higher proportion of patients from Finland (77%) and Japan (75%) reported remission compared with the other 8 countries.
TABLE 1.
Patient and Physician Demographics and Characteristics
| Patient Respondents (n = 2100) | Physician Respondents (n = 1254) | |
|---|---|---|
| Country of residence, n (%) | ||
| Australia | 57 (3) | 34 (3) |
| Canada | 90 (4) | 54 (4) |
| Finland | 15 (1) | 9 (1) |
| France | 164 (8) | 98 (8) |
| Germany | 214 (10) | 128 (10) |
| Italy | 164 (8) | 98 (8) |
| Japan | 336 (16) | 200 (16) |
| Spain | 126 (6) | 75 (6) |
| United Kingdom | 162 (8) | 96 (8) |
| United States | 773 (37) | 462 (37) |
| Male, n (%) | 1111 (53) | 1066 (85) |
| Mean age, y (SD) | 40.8 (12.4) | 47.6 (10.0) |
| Age (y) when experienced first symptoms, n (%) | ||
| 0-17 | 303 (14) | NA |
| 18-24 | 444 (21) | NA |
| 25-29 | 339 (16) | NA |
| 30-39 | 558 (27) | NA |
| 40-49 | 293 (14) | NA |
| ≥50 | 164 (8) | NA |
| Age (y) when diagnosed with UC, n (%) | ||
| 0-17 | 179 (9) | NA |
| 18-24 | 408 (19) | NA |
| 25-29 | 372 (18) | NA |
| 30-39 | 627 (30) | NA |
| 40-49 | 323 (15) | NA |
| ≥50 | 191 (9) | NA |
| Moderate to severe UC, n (%)* | 1731 (82) | NA |
| Mean time since diagnosis, y (SD) | 8.8 (9.2) | NA |
| Current overall health, n (%) | ||
| Good/excellent | 778 (37) | NA |
| Fair | 1010 (48) | NA |
| Poor | 311 (15) | NA |
| Self-reported remission,† n (%) | 1415 (67) | NA |
| Primary medical specialty, n (%) | ||
| Gastroenterology | NA | 994 (79) |
| Gastroenterology internist | NA | 162 (13) |
| Internist with gastroenterology focus | NA | 71 (6) |
| Gastroenterology surgery | NA | 27 (2) |
| Mean time in specialty practice, y (SD) | NA | 16.4 (8.4) |
*Patients with mild UC comprised ≤20% of the total patient respondents.
†Remission was defined as disease being controlled with few to no symptoms.
Course of UC
Patients typically experienced initial symptoms at a mean age of 30.0 years (standard deviation [SD], 12.7; median, 29) and were diagnosed with UC at a mean age of 32.0 years (SD, 12.2; median, 30; Table 1). The mean duration between UC symptom onset and UC diagnosis was 2.0 years (SD, 5.4); 42% of patients waited ≥1 year for diagnosis, and 11% of patients had waited ≥5 years.
Patients reported receiving their diagnosis of UC a mean of 8.8 years (SD, 9.2) earlier. A high proportion (87%) of patients reported having experienced a flare in the past year, with an average of 4.3 flares (SD, 7.4) experienced. The mean number of flares that patients reported in the past year was greater in Australia (6.5; SD, 11.6), Germany (6.2; SD, 9.1), France (5.9; SD, 9.4), Spain (5.7; SD, 9.3), and Canada (5.2; SD, 6.9), compared with the United States (4.2; SD, 8.0), Italy (3.3; SD, 3.1), Finland (3.1; SD, 3.2), the UK (2.6; SD, 3.1), and Japan (2.5; SD, 4.1). The mean number of flares for those who considered themselves to be in remission was 3.4 (SD, 6.0), compared with 6.2 (SD, 9.6) for patients who did not consider their UC to be in remission.
Living With UC
Globally, the majority of patients with moderate to severe disease (84%) reported UC to be mentally exhausting; even patients with milder UC (75%) or patients who self-reported being in remission (82%) agreed. Most patients (65%) felt that UC controlled their life rather than them controlling their UC, although patient opinion varied by country, with 69% of patients in France and Germany feeling that UC controlled their life, compared with 57% of patients in Finland. Approximately two-thirds of patients (67%) felt that they spent more time in the bathroom than anywhere else; compared with all the other countries surveyed, fewer patients (61%) in Finland felt that they spent more time in the bathroom than anywhere else. A similar proportion of patients (62%) who considered themselves to be in remission felt that they spent more time in the bathroom than anywhere else.
Patients reported visiting the bathroom (for any reason, including to pass stool, air, blood, or mucus) a mean of 3.5 times (SD, 2.9) on their best day and 9.8 times (SD, 7.4) on their worst day. Corresponding values for patients who self-reported remission were 3.3 (2.8) and 8.9 times (6.9), respectively. The majority of physicians (67%) thought that more than half of their patients with UC believed that bathroom urgency was part of living with UC, and 62% of physicians agreed that more than half of their patients believed that spending significant time in the bathroom was part of living with UC.
Overall, the majority (83%) of patients agreed that having UC impacted their work, with 74% of employed patients reporting work absence because of their UC and missing a mean of 8.1 working days (SD, 16.7) in the past 12 months because of their UC symptoms. Most patients (81%) who considered themselves to be in remission also agreed that having UC had impacted their work and reported missing a mean of 7.3 working days (SD, 16.6) because of UC symptoms. Most patients (74%) considered their employer to be very understanding of their condition, and 58% felt comfortable discussing their health in the workplace. However, 39% of patients had not told their employer about their UC diagnosis because of a fear of repercussions. Approximately two-thirds of patients (63%) reported UC to have had a negative effect on their confidence at work (Supplementary Fig. 1 in Supplementary Materials). The proportion of patients agreeing that UC impacted their work was greatest in Australia (74%) and Japan (74%), compared with patients in Spain (56%; Supplementary Fig. 1 in Supplementary Materials). More than one-third of patients (37%) reported that UC had influenced their decisions regarding family (including deciding not to have children, to have any more children, postponing having children, deciding to adopt, stopping treatment to start a family, or postponing/ending/avoiding romantic relationships).
Emotional Impacts of UC
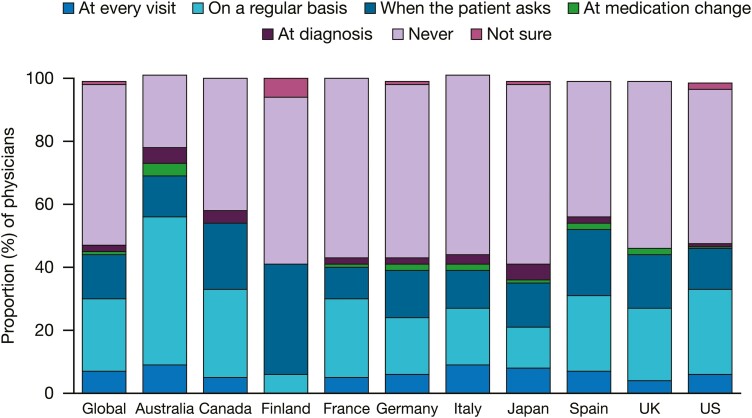
In total, 21% and 15% of patients self-reported receiving a diagnosis of anxiety or depression, respectively, although this finding varied by country. Only 2% of patients in Japan reported ever receiving a diagnosis of anxiety, compared with 30% of patients in Italy, and 9% of patients in Japan reported receiving a diagnosis of depression, compared with 22% of patients in Canada and Finland. Of all survey respondents, few (7%) patients reported currently seeing a psychiatrist, psychologist, or therapist as part of their UC management. Globally, the majority (71%) of patients were very/somewhat satisfied with the discussions they had with their physician relating to the mental and emotional health impacts of UC. Discussing the emotional impact of UC during routine appointments was less of a priority for physicians compared with patients. Overall, 7% of physicians considered it as one of their top 3 priorities vs 13% of patients. The greatest discordance between patients (20%) and physicians (6%) on this topic was in Germany. In Finland, although only 9 physicians responded to this question, none discussed the emotional impact of UC with their patients during routine appointments.
Globally, approximately half (52%) of patients felt comfortable discussing emotional concerns with their physician; however, comfort did vary between countries, with only 40% of patients in France feeling comfortable discussing emotional concerns with their physician, compared with 61% of patients in the UK. Overall, only 23% of physicians regularly discussed the impact of UC on mental and emotional health with patients, and approximately half (51%) never discussed this topic (Fig. 1). Compared with all the other countries, a greater proportion (47%) of physicians in Australia reported regularly discussing the impact of UC on patients’ mental and emotional health (Fig. 1).
FIGURE 1.
When physicians typically discuss the impact of UC on patients’ mental/emotional health. Because of rounding, the sum of all categories does not equal 100%.
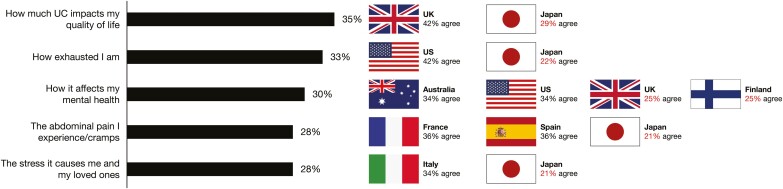
Three in 10 patients (30%) wished that their physicians better understood the effect of UC on their mental health, whereas 40% of patients (and 44% of physicians) considered managing the psychological impact of UC to be important in managing UC.
Expectations of UC Management
Approximately 7 in 10 patients surveyed (71%) had set goals with their physician for managing their UC. Overall, the top 5 concerns that patients wished physicians better understood were “how much UC impacts on my quality of life” (35%), “how exhausted I am” (33%), “how it affects my mental health” (30%), “the abdominal pain I experience/cramps” (28%), and “the stress it causes me and my loved ones” (28%; Fig. 2). Patient responses differed by country, with fewer patients (29%) in Japan wishing that their physician better understood how much UC impacts on their quality of life, compared with 42% of patients in the UK (Fig. 2). Most physicians (62%) agreed that more than half of their patients with UC had accepted that having UC meant that they had to settle for a reduced quality of life. Approximately half (54%) of physicians considered more than half of their patients with UC to believe that pain and cramping were just part of living with UC.
FIGURE 2.
The top 5 aspects that patients wished physicians better understood about the impact of UC on their quality of life. Countries with the highest and lowest proportions of respondents who agreed with each statement are shown. For countries with the highest proportion of respondents, the percentage is shown in black; for countries with the lowest proportion of respondents, the percentage is shown in red.
Globally, patients and physicians generally agreed that the ability to perform daily activities and the ability to control pain were among the most important aspects of UC management for patients (Table 2).
TABLE 2.
The Most Important Aspects of UC Management
| Patients, % (overall ranking) | Physicians, % (overall ranking) | |
|---|---|---|
| Ability to conduct daily activities | 59 (1) | 77 (1) |
| Reducing the risk of cancer | 57 (2) | 50 (7) |
| Avoiding toileting accidents/needing to prepare | 55 (3) | 54 (6) |
| Ability to control pain | 53 (4) | 61 (4) |
| Avoiding colectomy | 52 (5) | 70 (2) |
| Avoiding hospitalization | 52 (5) | 70 (2) |
| Reducing fatigue | 49 (7) | 44 (10) |
| Ability to eat anything without symptoms | 45 (8) | 45 (9) |
| Ability to travel | 44 (9) | 49 (8) |
| Minimizing/avoiding adverse effects from medication | 44 (9) | 57 (5) |
Patient and physician responses were derived from independent questionnaires and therefore no formal statistical analysis was performed. Ranking shown for patients and physicians of the top 10 aspects selected by patients.
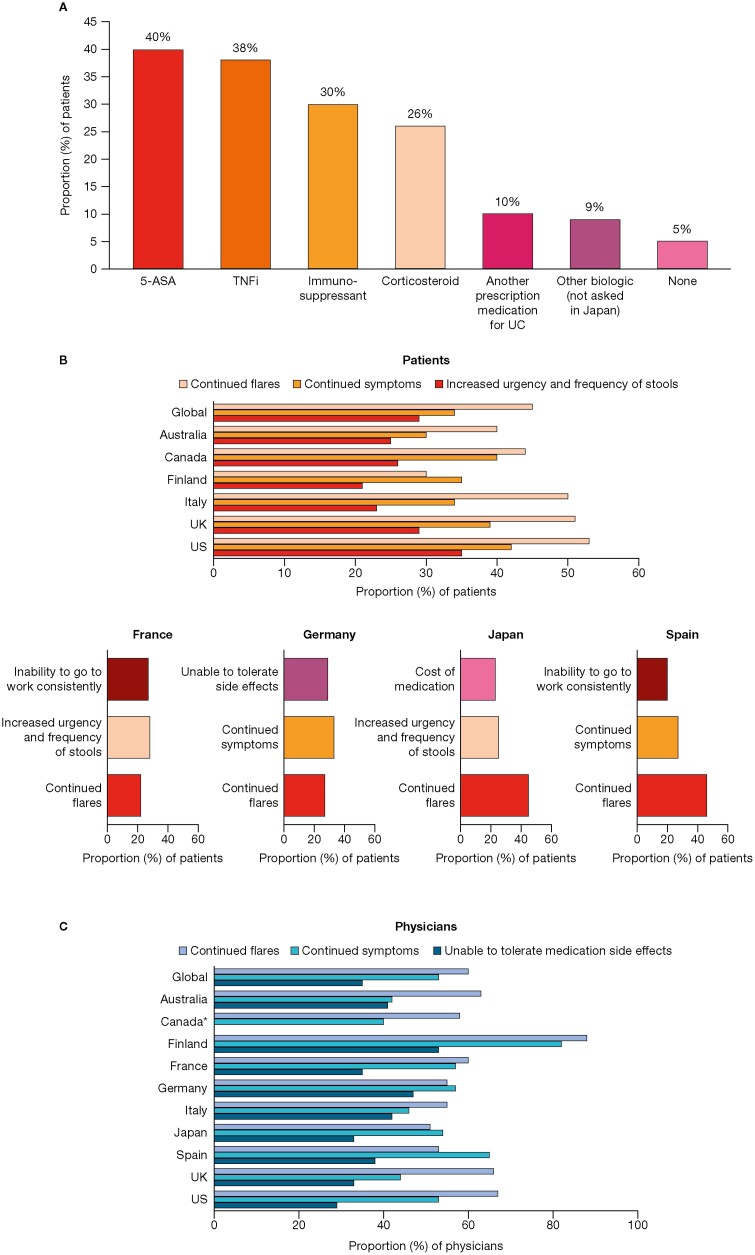
UC Medication
Overall, 95% of patients self-reported currently taking prescription medication for their UC, which included biologics (44%), 5-aminosalicylates (40%), immunosuppressants (30%), corticosteroids (26%), and other prescription medication for UC (10%) (Fig. 3A). Of patients currently taking corticosteroids, the majority (76%) were afraid to stop because of fears of experiencing an immediate UC flare. Almost all patients (95%) who were currently taking corticosteroids said they had experienced a flare within the past 12 months. Most patients (84%) who were prescribed medication for their UC responded that they were very/somewhat satisfied with their current medication, which was in agreement with physicians’ mean estimation of 74% of patients being very/somewhat satisfied with their current medication.
FIGURE 3.
Patients currently taking prescription medication for their UC (A) and the top 3 indicators for considering changing medication according to (B) patients and (C) physicians. “Cost of medication” was not asked in France. Patients (A) could select all prescription medications they were currently taking for their UC. Patients (B) and physicians (C) could select up to 3 reasons why they would consider changing medication; selected responses shown. *Increased urgency and frequency of stools was ranked 3rd (40%) by Canadian physicians. 5-ASA, 5-aminosalicylates; TNFi, tumor necrosis factor inhibitor.
Among patients who were satisfied with their current medication, the top 3 reasons were less frequent flares (54%), less abdominal pain (47%), and less urgency to go to the bathroom (47%). Of patients currently taking biologics, 42% were not happy with this medication. More patients in Australia were not happy with biologics (66%) compared with all the other countries (<55%).
In total, 76% of patients wished that they had more medication choices to treat their UC. Assuming equal effectiveness between medications, 58% of patients preferred orally administered medication. Approximately three-quarters of patients (74%) wished that they knew more about all the available UC medications at initial diagnosis. Compared with patients from all the other countries surveyed, a greater proportion of patients in France (86%), Spain (85%), and Italy (84%) wished that they had knowledge about all the available UC medications at initial diagnosis. Globally, 54% of patients wished that their gastroenterologists had discussed all the available treatment options with them earlier so that they had a better idea of their choices. Compared with all the other countries surveyed, a greater proportion of patients (74%) in Italy expressed a desire for discussion of all treatment options earlier. Approximately three-quarters of physicians (74%) wished that they had more time to discuss all available treatment options with their patients earlier.
Overall, the top 2 indicators for considering changing medications were similar for patients and physicians: continued flares (45% of patients; 60% of physicians) and continued symptoms (34% of patients; 53% of physicians). Globally, there was greater variance among patients regarding the top 3 indicators for considering medication changes (Fig. 3B), whereas physicians generally agreed on the top 3 indicators (Fig. 3C). For example, in Japan, the cost of medication/changes in affordability was selected by 23% of patients, whereas the proportion of patients who selected this option in other countries ranged from 3% to 16%, with a global mean of 12% (Fig. 3B).
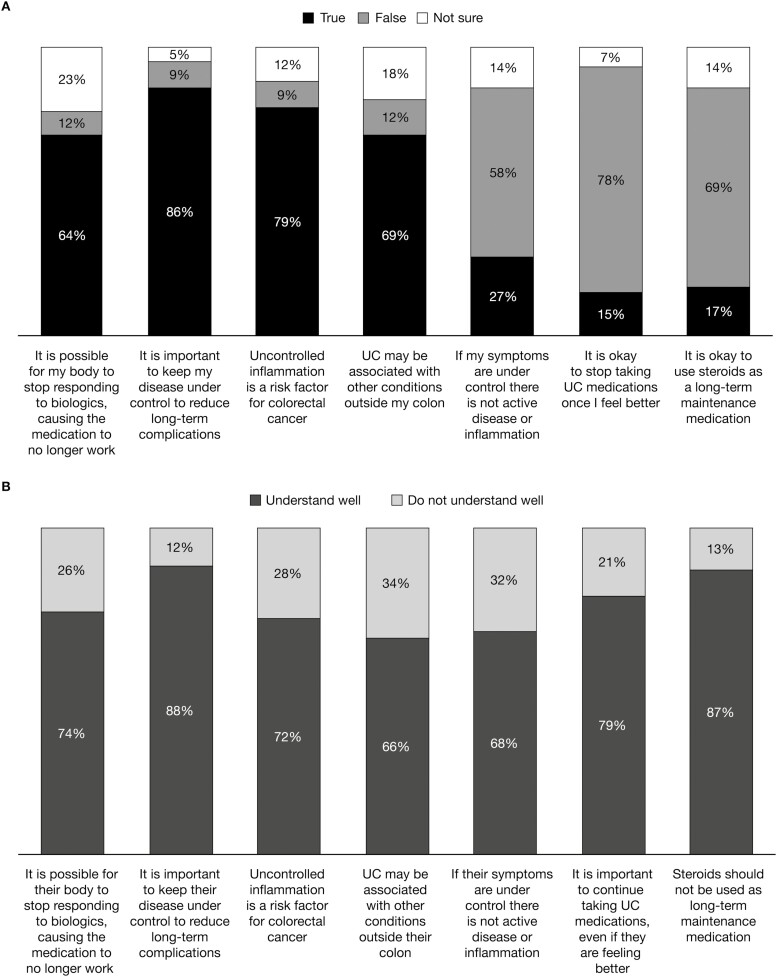
Disease Awareness and Knowledge
Only 25% of patients correctly responded to all 7 true/false questions relating to disease knowledge. When asked if uncontrolled inflammation was a risk factor for colorectal cancer, 9% of patients believed this to be false and 12% were not sure (Fig. 4A). More than one-quarter of patients (27%) incorrectly believed that if symptoms were controlled then their disease was not active and 14% were unsure. Nearly one-third of patients (30%; 18% unsure and 12% false) were not aware that UC may be associated with conditions outside of the colon.
FIGURE 4.
Patients’ understanding of UC from (A) patients’ perspective and (B) physicians’ perspective. Patient and physician responses are presented in separate images because of the slight difference in the phrasing of questions and to maintain alignment with the surveys.
Physicians’ responses to questions regarding their opinion of their patients’ moderate to severe UC understanding recognized their patients’ knowledge gaps (Fig. 4B). Overall, 87% of physicians believed that their patients with moderate to severe UC understood that steroids should not be used as long-term maintenance medication, compared with 69% of patients who responded to this question correctly.
DISCUSSION
Here, we present the results from 2 complementary global UC surveys—1 patient-based and 1 physician-based—that represent the largest pool of data of its kind. The survey populations were independent of each other, with no direct link between patient and physician responses, yet they allowed for the identification of differences in the perspectives of patients with UC and physicians who manage and treat patients with UC. Similarly, the global application of this survey also allowed for the identification of differences in the views and attitudes of patients and physicians across and between countries. Note that differences in healthcare systems between countries exist and, therefore, differences are apparent regarding the costs of healthcare and who is responsible for these costs.10, 11 These differences may affect the ability of physicians to prescribe a particular treatment, or a higher cost to patients may prevent them from taking a medication if they cannot afford it, thus affecting patient and physician perceptions of UC. Our survey also highlighted differences between countries with regard to the physical and emotional impact of UC. For example, the lower proportion of patients reporting receiving a diagnosis of anxiety or depression in Japan vs the global mean may reflect cultural differences, as patients in Asian countries may be less likely to voice concerns to their physician.8
Consistent with previous studies,12, 13 patients reported a delay between UC symptom onset and diagnosis with 42% of patients reporting more than 1 year between first symptoms and diagnosis. Delay in the diagnosis of UC has the potential to not only cause frustration and anxiety in the patient, but can also to adversely affect the patient-physician relationship.8 The consequences of delayed diagnosis include delayed initiation of UC therapy, potentially leading to complications, including a higher risk of UC-related intestinal surgery.14
The high proportion of patients reporting treatment satisfaction was also consistent with previous surveys of patients with UC.2, 15, 16 However, many expressed a desire for greater medication choices and only 37% regarded their overall health to be excellent/good, suggesting that patients may have low expectations of treatment for their condition, and patients are settling for their current medication, and more options are needed to improve patients’ health. The results also suggest that from both patient and physician perspectives, more time is needed for UC management discussions.
The responses to this survey show that patients and physicians both consider quality of life and the ability to control pain to be central to UC management. A previous patient survey conducted in Spain reported the treatment attribute most valued by patients to be continuous symptom control and normalization of their quality of life.16 Here, the top 3 patient responses selected for medication satisfaction included less frequent flares, less abdominal pain, and less urgency to go to the bathroom.
These findings reiterate the results from previous studies illustrating the negative impact of UC even in patients who consider themselves to be in remission.17 The family life impact of UC reported in this survey is corroborated by other study findings, including an Australian study in which many women were concerned about passing the disease to their offspring, had concerns regarding infertility, and considered not having children.18 Our survey results also confirm that UC has a detrimental impact on patients’ professional lives, with many reporting absence from work because of UC, along with negative effects on their confidence in the workplace, findings which are in agreement with previous reports of 63.7% to 75% of patients reporting work absences because of their UC.13,17,19 Of note is that patients in Europe and Japan said they had missed work because of worry about the symptoms of UC rather than experiencing actual UC symptoms.13, 19
Depression and anxiety are common in patients with IBD, both of which can adversely affect patients’ quality of life.20, 21 In agreement with previous findings,2, 4, 22 both patients and physicians reported infrequently discussing emotional and mental health issues during routine appointments, suggesting that mental health concerns are not addressed despite most patients reporting UC to be a mentally exhausting condition.
Following a diagnosis of UC, patient education is of paramount importance in enabling patients to understand their condition, become informed about the medication options available, and provide the basis for an open and honest patient-physician relationship.8 However, in this survey it was shown that more education about the risks of UC and therapeutic options is needed.
Although this survey is the first global study to provide important data on patients’ most common worries and fears with UC, and on the diagnostic delay in UC, there are several limitations, which are detailed in Rubin et al.9 In brief, limitations include the reliance on accurate and honest recall and reporting by both patients and physicians. In addition, patients were recruited based on self-reported diagnosis of UC, and disease severity was established from medication history (patient-reported) with no clinical disease activity assessment. Furthermore, patients completed the survey online; patient participation was therefore limited to those with internet access and to those who had registered as members of the online panels from which patients were recruited. Finally, with some physician surveys completed by telephone, there was potential for interviewer technique/recording to impact upon the results. However, despite these limitations, a strength of this study is that through the representative weighting of results, the data presented here may reflect the populations surveyed.
CONCLUSIONS
The results of these surveys show a delay in the diagnosis of patients with UC, and despite patients reporting their UC to be in remission many are still experiencing flares and have poor general health, indicating a significant burden of disease and acceptance of negative disease symptoms even when in remission. Effective shared decision-making relies upon patients being educated and aware of treatment options to enable them to achieve a better quality of life. These survey results indicate a need for patient and physician education to improve understanding of the impact of UC and greater inclusion of discussions on the emotional and mental health impacts of UC during routine appointments. These results clearly show the major impact that UC has on a patient’s life and daily activities, and potential areas for further investigation into the relationship between patients with UC and HCPs involved in managing their UC.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the patients and physicians who were involved in the UC Narrative Survey. Study design was contributed by The Harris Poll and the UC Narrative Survey Panel; study support was contributed by GCI Health and The Harris Poll; statistical analysis was contributed by JCC and The Harris Poll. Medical writing support, under the guidance of the authors, was provided by Helen Findlow, PhD, CMC Connect, McCann Health Medical Communications and was funded by Pfizer Inc, New York, NY in accordance with Good Publication Practice (GPP3) guidelines (Battisti WP, Wager E, Baltzer L, et al. Ann Intern Med. 2015;163:461–464).
Author contributions: Manuscript drafting, critical revision, and final approval: all authors.
Supported by: The UC Narrative Surveys were sponsored by Pfizer Inc.
Presented at: Parts of the data in this manuscript were previously presented at the Crohn’s and Colitis Congress (2019) February 7–9, 2019, Las Vegas, Nevada.
Conflicts of interest: Marla C. Dubinsky has received financial support for research from AbbVie, Janssen, Pfizer Inc, and Prometheus Laboratories; and consultancy fees from AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Genentech, Janssen, Pfizer Inc, Prometheus Laboratories, Salix Pharmaceuticals, Shire, Takeda, and UCB. Kenji Watanabe has received financial support for research from AbbVie Japan, EA Pharma, JIMRO, Kyorin Pharmaceutical, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, and Zeria Pharmaceutical; consultancy fees from AbbVie Japan, EA Pharma, Janssen Pharmaceutical, JIMRO, Kissei Pharmaceutical, Kyorin Pharmaceutical, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, Olympus Corporation Takeda, Pfizer Japan, and Zeria Pharmaceutical; and lecture fees from AbbVie Japan, Astellas, Covidien Japan, EA Pharma, Janssen Pharmaceutical, JIMRO, Kissei Pharmaceutical, Kyorin Pharmaceutical, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, Nippon Kayaku, Pfizer Japan, Olympus Corporation, and Zeria Pharmaceutical. Pauliina Molander has received speaker fees and travel support from AbbVie, Ferring Pharmaceuticals, Janssen-Cilag, MSD, and Tillotts Pharma; and consulting fees from AbbVie, Janssen-Cilag, MSD, Orion Pharma, Pfizer Inc, Tillotts Pharma, and Takeda. Laurent Peyrin-Biroulet has received honoraria from AbbVie, Allergan, Alma, Amgen Biogen, Arena, Boehringer Ingelheim, Celgene, Celltrion, Enterome, Ferring Pharmaceuticals, Genentech, Gilead Sciences, Hikma, Index Pharmaceuticals, Janssen, MSD, Nestlé, Pfizer Inc, Pharmacosmos, Roche, Samsung Bioepis, Sandoz, Sterna, Takeda, and Tillotts; has received grants from AbbVie, MSD, and Takeda; and is a stockholder of CTMA. Michele Rubin has been an advisory board member for Pfizer Inc for this study. Gil Y. Melmed has acted as a consultant for AbbVie, Boehringer Ingelheim, Celgene, Genentech, Janssen, Medtronic, Pfizer Inc, Takeda, and UCB; and received support for research from Pfizer Inc and Prometheus Labs. Kathy Steinberg is an employee of The Harris Poll. Susan Connor has received speaker fees, educational and/or research support from, and/or been an advisory board member for, AbbVie, Aspen, Celgene, Celltrion, Ferring Pharmaceuticals, Gilead Sciences, Janssen, MSD, Novartis, Pfizer Inc, Shire, Takeda, and Vifor. J. Jasper Deuring, John Woolcott, and Joseph C. Cappelleri are employees and stockholders of Pfizer Inc.
REFERENCES
- 1. Ungaro R, Mehandru S, Allen PB, et al. Ulcerative colitis. Lancet. 2017;389:1756–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: results of the European Federation of Crohn’s and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis. 2007;1:10–20. [DOI] [PubMed] [Google Scholar]
- 3. Bokemeyer B, Hardt J, Hüppe D, et al. Clinical status, psychosocial impairments, medical treatment and health care costs for patients with inflammatory bowel disease (IBD) in Germany: an online IBD registry. J Crohns Colitis. 2013;7:355–368. [DOI] [PubMed] [Google Scholar]
- 4. López-Sanromán A, Carpio D, Calvet X, et al. Perceived emotional and psychological impact of ulcerative colitis on outpatients in Spain: UC-LIFE survey. Dig Dis Sci. 2017;62:207–216. [DOI] [PubMed] [Google Scholar]
- 5. Schreiber S, Panés J, Louis E, et al. Perception gaps between patients with ulcerative colitis and healthcare professionals: an online survey. BMC Gastroenterol. 2012;12:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McMullan C, Pinkney TD, Jones LL, et al. Adapting to ulcerative colitis to try to live a “normal” life: a qualitative study of patients’ experiences in the Midlands region of England. BMJ Open. 2017;7:e017544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rubin DT, Krugliak Cleveland N. Using a treat-to-target management strategy to improve the doctor-patient relationship in inflammatory bowel disease. Am J Gastroenterol. 2015;110:1252–1256. [DOI] [PubMed] [Google Scholar]
- 8. Chew D, Zhiqin W, Ibrahim N, et al. Optimizing the multidimensional aspects of the patient-physician relationship in the management of inflammatory bowel disease. Intest Res. 2018;16:509–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rubin DT, Hart A, Panaccione R, et al. Ulcerative Colitis Narrative global survey findings: communication gaps and agreements between patients and physicians. Inflamm Bowel Dis. 2021;27:1096–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wei SC. Differences in the public medical insurance systems for inflammatory bowel disease treatment in Asian countries. Intest Res. 2016;14:218–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cohen RD, Yu AP, Wu EQ, et al. Systematic review: the costs of ulcerative colitis in Western countries. Aliment Pharmacol Ther. 2010;31:693–707. [DOI] [PubMed] [Google Scholar]
- 12. Nóbrega VG, Silva INN, Brito BS, et al. The onset of clinical manifestations in inflammatory bowel disease patients. Arq Gastroenterol. 2018;55:290–295. [DOI] [PubMed] [Google Scholar]
- 13. Lönnfors S, Vermeire S, Greco M, et al. IBD and health-related quality of life—discovering the true impact. J Crohns Colitis. 2014;8:1281–1286. [DOI] [PubMed] [Google Scholar]
- 14. Lee DW, Koo JS, Choe JW, et al. Diagnostic delay in inflammatory bowel disease increases the risk of intestinal surgery. World J Gastroenterol. 2017;23:6474–6481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gray JR, Leung E, Scales J. Treatment of ulcerative colitis from the patient’s perspective: a survey of preferences and satisfaction with therapy. Aliment Pharmacol Ther. 2009;29:1114–1120. [DOI] [PubMed] [Google Scholar]
- 16. Carpio D, López-Sanromán A, Calvet X, et al. Perception of disease burden and treatment satisfaction in patients with ulcerative colitis from outpatient clinics in Spain: UC-LIFE survey. Eur J Gastroenterol Hepatol. 2016;28:1056–1064. [DOI] [PubMed] [Google Scholar]
- 17. Calvet X, Argüelles-Arias F, López-Sanromán A, et al. Patients’ perceptions of the impact of ulcerative colitis on social and professional life: results from the UC-LIFE survey of outpatient clinics in Spain. Patient Prefer Adherence. 2018;12:1815–1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Selinger CP, Eaden J, Selby W, et al. Inflammatory bowel disease and pregnancy: lack of knowledge is associated with negative views. J Crohns Colitis. 2013;7:e206–e213. [DOI] [PubMed] [Google Scholar]
- 19. Ueno F, Nakayama Y, Hagiwara E, et al. Impact of inflammatory bowel disease on Japanese patients’ quality of life: results of a patient questionnaire survey. J Gastroenterol. 2017;52:555–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mikocka-Walus A, Knowles SR, Keefer L, et al. Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm Bowel Dis. 2016;22:752–762. [DOI] [PubMed] [Google Scholar]
- 21. Bannaga AS, Selinger CP. Inflammatory bowel disease and anxiety: links, risks, and challenges faced. Clin Exp Gastroenterol. 2015;8:111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rubin DT, Dubinsky MC, Martino S, et al. Communication between physicians and patients with ulcerative colitis: reflections and insights from a qualitative study of in-office patient-physician visits. Inflamm Bowel Dis. 2017;23:494–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.