Abstract
Aims
The aim of this study was to investigate whether on-demand removal (ODR) is noninferior to routine removal (RR) of syndesmotic screws regarding functional outcome.
Methods
Adult patients (aged above 17 years) with traumatic syndesmotic injury, surgically treated within 14 days of trauma using one or two syndesmotic screws, were eligible (n = 490) for inclusion in this randomized controlled noninferiority trial. A total of 197 patients were randomized for either ODR (retaining the syndesmotic screw unless there were complaints warranting removal) or RR (screw removed at eight to 12 weeks after syndesmotic fixation), of whom 152 completed the study. The primary outcome was functional outcome at 12 months after screw placement, measured by the Olerud-Molander Ankle Score (OMAS).
Results
There were 152 patients included in final analysis (RR = 73; ODR = 79). Of these, 59.2% were male (n = 90), and the mean age was 46.9 years (SD 14.6). Median OMAS at 12 months after syndesmotic fixation was 85 (interquartile range (IQR) 60 to 95) for RR and 80 (IQR 65 to 100) for ODR. The noninferiority test indicated that the observed effect size was significantly within the equivalent bounds of -10 and 10 scale points (p < 0.001) for both the intention-to-treat and per-protocol, meaning that ODR was not inferior to RR. There were significantly more complications in the RR group (12/73) than in the ODR group (1/79) (p = 0.007).
Conclusion
ODR of the syndesmotic screw is not inferior to routine removal when it comes to functional outcome. Combined with the high complication rate of screw removal, this offers a strong argument to adopt on demand removal as standard practice of care after syndesmotic screw fixation.
Cite this article: Bone Joint J 2021;103-B(11):1709–1716.
Keywords: Syndesmotic screw, Syndesmotic injury, Implant removal, Functional outcome, Functional outcome scores, syndesmotic screws, multicentre randomized controlled trial, syndesmotic injuries, trauma, Olerud-Molander Ankle Score, surgical site infections (SSIs), randomized controlled trial, revision surgery, Mann-Whitney U test
Introduction
Syndesmotic injuries are present in approximately 15% to 20% of surgically treated ankle fractures.1,2 The most common surgical treatment of syndesmotic injuries is syndesmotic screw fixation, which is traditionally removed after eight to 12 weeks, as it is thought to hamper ankle function and cause pain when in place during weight bearing.3-5 It has also been argued that removing this screw is necessary to achieve final anatomical reduction.6 Other studies found that syndesmotic screw removal does not result in improvement of functional outcome or range of motion (ROM).7-11 In case of a broken or loosened screw, restrictions of natural movement of the distal tibiofibular syndesmosis would no longer be present.8,10,11
Syndesmotic screw removal is a procedure that rarely takes more than an hour. Prophylactic antibiotics are therefore not routinely used. Nevertheless, infectious complications are not uncommon, with surgical site infection (SSI) rates of up to 9%.11-14 With the relatively high complication rate of screw removal in mind, it could be beneficial to retain them or to remove them only if the patient experienced difficulties.
We therefore aimed to investigate the effect of on-demand removal (ODR) of the syndesmotic screw on functional outcome. The hypothesis was that functional outcome at 12 months after syndesmotic fixation is comparable in patients between ODR and routine removal (RR).
Methods
The ROutine vs on DEmand removal Of the syndesmotic screw (RODEO) trial was a pragmatic international multicentre randomized controlled trial, comparing ODR and RR of the syndesmotic screw. The study was registered at ClinicalTrials.gov (NCT02896998) and the study protocol was published.15 The trial was conducted in 17 European centres, of which 14 were teaching hospitals and three were academic, level 1 trauma centres.
Participants
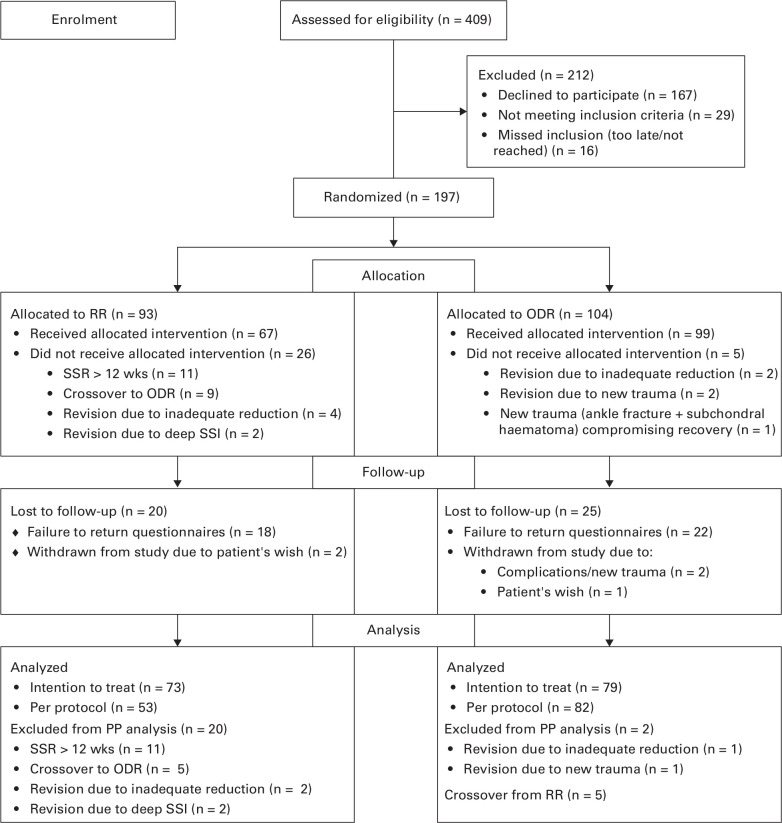
All adult patients (aged above 17 years) with traumatic syndesmotic injury, surgically treated within two weeks of trauma using one or two syndesmotic screws, were eligible for inclusion. Both unstable ankle fractures with syndesmotic disruption and isolated syndesmotic injuries were included. Exclusion criteria were: an Injury Severity Score > 15,16 insufficient physical condition (to allow for potential screw removal), concomitant injury of the ipsi- or contralateral side or other medical conditions hampering rehabilitation, and insufficient comprehension of English, Dutch, Finnish, or Swedish language (Figure 1).
Fig. 1.
CONSORT flow diagram of included patients. ODR; on-demand removal; PP, per protocol; RR, routine removal; SSI, surgical site infection; SSR, syndesmotic screw removal.
Out of 197 patients randomized between January 2017 and April 2019, 45 did not have complete primary outcome data, leaving 152 (73 patients in RR and 79 patients in ODR group) for inclusion in final analysis. Of all included patients, 59.2% were male (n = 90) and the mean age was 46.9 years (standard deviation (SD) 14.6). The number of patients in the < 60 years group was 120 (RR 59, ODR 61) and 32 (RR 14, ODR 18) in the ≥ 60 years group. Baseline characteristics were similar between randomization groups (Table I), as well as between included patients and those lost to follow-up (Supplementary Table i). The per-protocol groups consisted of 53 and 82 patients for RR and ODR, respectively.
Table I.
Baseline patient and surgical characteristics.
| Variable | RR (n = 73) | ODR (n = 79) |
|---|---|---|
| Male, n (%) | 47 (64) | 43 (54) |
| Mean age, yrs (SD) | 45.3 (15) | 48.3 (14) |
| Age, yrs, n (%) | ||
| < 60 | 59 (81) | 61 (77) |
| ≥ 60 | 14 (19) | 18 (23) |
| Mean weight, kg (SD) | 85 (14) | 88 (18) |
| Missing, n | 0 | 2 |
| Mean BMI, kg/m2 (SD) | 27 (4) | 29 (6) |
| Missing, n | 4 | 2 |
| Nicotine use, n (%) | 17 (25) | 18 (24) |
| Missing, n | 6 | 4 |
| Alcohol abuse, n (%) ‡ | 6 (9) | 8 (11) |
| Missing, n | 5 | 4 |
| Illegal drug use, n (%) | 8 (12) | 1 (1) |
| Missing, n | 4 | 4 |
| Diabetes mellitus, n (%) | 3 (4) | 4 (5) |
| Type 1 | 1 | 0 |
| Type 2 | 2 | 4 |
| COPD, n (%) | 0 | 3 (3.8) |
| PAD, n (%) | 0 | 1 (1.3) |
| Injury, n (%) | ||
| Weber B | 17 (24) | 18 (23) |
| Weber C | 41 (57) | 39 (49) |
| Maisonneuve | 11 (15) | 22 (28) |
| Isolated syndesmosis | 2 (3) | 0 |
| Other | 1 (1) | 0 |
| Missing | 1 | |
| ASA classification, n (%) | ||
| I | 38 (53) | 28 (36) |
| II | 33 (46) | 41 (53) |
| III | 1 (1) | 8 (10) |
| Missing | 1 | 2 |
| Mean surgery duration, mins (SD) | 65 (38) | 63 (36) |
| Missing, n | 7 | 8 |
| Tourniquet use, n (%) | 21 (40) | 18 (29) |
| Missing, n | 21 | 17 |
| Screws, n (%)§ | ||
| 1 | 50 (69) | 51 (65) |
| 2 | 22 (31) | 28 (35) |
| Screw diameter, mm, n (%) | ||
| 3.0 | 3 (4) | 1 (1) |
| 3.5 | 64 (89) | 74 (94) |
| 4.0 | 1 (1) | 1 (1) |
| 4.5 | 4 (6) | 3 (4) |
| Missing | 1 | |
| Cortices, n (%) | ||
| 3 | 57 (79) | 62 (78) |
| 4 | 15 (21) | 17 (22) |
| Missing | 1 | |
| Mean level, mm (SD) * | 24 (7) | 23 (9) |
| Missing, n | 4 | 3 |
| Mean time in cast after surgery, wks (SD) | 5 (2) | 5 (2) |
| Missing, n | 9 | 9 |
| Complication of fixation, n (%) | 16 (22) | 12 (15.2) |
| Missing, n | 1 | |
| Mean wks to full weightbearing (SD) | 5 (2) | 5 (2) |
| Missing, n | 2 | 1 |
Measured from tibial plafond to most distal syndesmotic screw.
Of which two combined with nonunion and one with bad reduction.
More than two units per day.
Data missing for one patient in the RR group.
ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease; ODR, on-demand removal; PAF, peripheral artery disease; RR, routine removal; SD, standard deviation.
Interventions
Patients randomized for RR were scheduled for screw removal routinely at eight to 12 weeks after definitive syndesmotic fixation according to protocol.15 If the screws were already broken at that time, surgeons were advised not to remove them unless they caused complaints. The exact timing of removal (within a window of eight to 12 weeks) and postoperative treatment regimen was left to the judgement of the treating surgeon and the hospital protocol. Patients were seen at the outpatient clinic by their treating surgeon and the coordinating investigator (MFB or FS) at three, six, and 12 months after syndesmotic fixation. During each of these visits, ROM was measured, and the patients filled out functional outcome questionnaires. Additionally, at three-month follow-up, wound inspection and radiological imaging (Mortise view) were performed. Patients randomized for ODR were seen according to the same follow-up schedule. ODR was defined as retaining the screw unless there were complaints warranting removal (e.g. localized pain, screw backing out causing skin irritation, infection). Patients (or surgeon) could opt for removal at any time, but were usually advised to wait, at least until fracture healing allowed for any additional implants to be removed (if necessary), in order to combine these procedures in case of clinically relevant hardware complaints. Time of removal and whether or not additional material was removed was recorded for all patients.
Objectives
The objective of this pragmatic RCT was to investigate the functional outcome of ODR compared to RR of the syndesmotic screw, placed in acute syndesmotic injuries. The hypothesis was that ODR would result in a noninferior functional outcome when compared to RR.
Outcomes
The primary outcome was functional outcome at 12 months after syndesmotic fixation, as measured by the Olerud-Molander Ankle Score (OMAS),17 a patient-reported outcome measure with a final score of 0 to 100, with 100 indicating full function. The OMAS was also filled out at three and six months after fixation. One could argue that older individuals are less likely to be hampered by the suggested limited ROM that occurs when the screw is left in place. To evaluate the difference in effect of screw removal on young, active patients and the older population, a subgroup analysis was performed on the OMAS using age groups (< 60 and ≥ 60 years). Secondary outcomes were: functional outcome using the American Orthopaedic Foot and Ankle Hindfoot Score (AOFAS);18 pain, using a ten-point visual analogue scale (VAS); active ROM, reported as the difference in absolute number of degrees (flexion + extension) between the injured and the healthy side; and complications. Wound healing problems, such as wound dehiscence or surgical site infections (SSIs) according to Centers for Disease Control criteria19 and recurrent diastasis (diagnosed based on complaints and radiological imaging), were specifically enquired after during follow-up visits. Other complications (e.g. deep vein thrombosis, malreduction, nonunion) were reported to the coordinating researcher at the time they occurred. All charts were screened at least 12 months after inclusion of the final patient in order not to miss any unreported complications or revision procedures.
All mentioned outcomes were measured at three, six, and 12 months after syndesmotic fixation. Furthermore, baseline patient, fracture, and surgical characteristics were collected, as well as the immobilization and weightbearing policy. Status of the screw was documented as the last date it was reported to be intact and the first date it was found to be broken, using radiological imaging and surgical documentation.
Sample size
The sample size calculation was based on a noninferiority design, using the OMAS at 12 months as primary outcome measure. With a one-sided significance level (α) of 0.025, 90% power (ß), SD of 19 points, and a noninferiority limit of ten points on the OMAS, 152 subjects were required to prove noninferiority. In order to conduct a subgroup analysis based on age with the same power, lower SDs, and incorporating a loss-to-follow-up rate of 10%, a total of 196 would have to be included.15
Randomization
Patients were randomized 1:1 to either RR or ODR, using variable blocks of four, six, and eight, stratified per institute and by age category. Randomization was performed centrally by the coordinating investigator, who then notified the patient and treating (orthopaedic) surgeon. The randomization sequence was generated by a dedicated computer randomization software program (Castor EDC)20 ensuring allocation concealment. Considering the nature of the intervention, blinding of patient, surgeon, or outcome assessor was not possible.
Statistical analysis
Descriptive methods were used to assess distribution of data and homogeneity of treatment groups. The primary outcome was analyzed according to the intention-to-treat as well as the per-protocol principle, noninferiority only being declared if both analyses proved noninferiority of ODR compared to RR. In per-protocol analysis, crossovers were analyzed in the group they crossed over to and patients not treated according to the protocol of either group were excluded, as were patients in whom syndesmotic fixation was revised (due to a new trauma or complication). The primary outcome was presented as median and interquartile range (IQR) and tested for noninferiority using a one-sided two one-sided test (TOST) equivalence test based on the independent-samples t-test21 with an α of 0.025, equal variances assumed, and equivalent bounds of -10 and 10 scale points. Secondary outcomes were analyzed using either a independent-samples t-test or Mann-Whitney U test for continuous data, according to distribution, and a chi-squared test for categorical data. Possible predictors of functional outcome were identified using a univariable linear regression, subsequently adding all variables with a significant or near-significant relationship with the 12-month OMAS (p < 0.2) to multivariable linear regression in order to identify independent predictors of functional outcome. All analyses were performed using SPSS v. 26.0 (IBM, USA).
Results
In the RR group, screw removal was performed in 67 of 73 cases (five crossovers, one revision surgery) at a mean of 11 weeks (SD 2.4) after syndesmotic fixation. Patients having their screw routinely removed after more than 12 weeks (usually due to planning reasons) were excluded from the per-protocol analysis, but included in the intention-to-treat. In nine cases, the screw was already broken at the time of removal. The number of removals within 12 months in the ODR group was 18 (23%) at a mean of 33 weeks (SD 10.1) after syndesmotic fixation. Reasons for removal were pain (n = 7), limited ROM (n = 4), stiffness (n = 2), revision surgery where new syndesmotic fixation was indicated (n = 2), skin reaction to implants (n = 1), screw backing out (n = 1), or patient’s wish not otherwise described (n = 1). None of the five patients who crossed over from RR to ODR had their screw removed.
Of the 61 ODR patients who retained their screw, 19 broke within 12 months (13 after > 12 weeks). Out of the 18 ODR patients who underwent screw removal, the screw was already broken in ten cases. In addition, two out of the five crossovers broke their screw.
Primary outcome
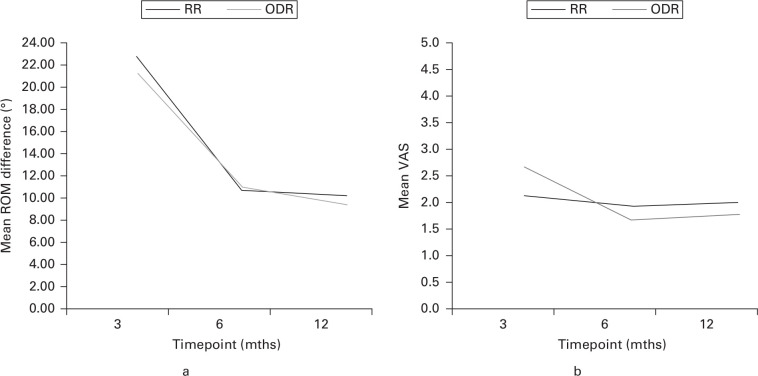
The median OMAS at 12 months after syndesmotic fixation was 85 (IQR 60 to 95) for the RR group and 80 (IQR 65 to 100) for the ODR group (Figure 2). The noninferiority test indicated that for the intention-to-treat analysis the observed effect size was significantly within the equivalent bounds (t-statistic = -3.56 (n = 150); p < 0.001, TOST equivalence test), meaning ODR was not inferior to RR. In the per-protocol groups the median OMAS was 85 (IQR 62.5 to 95) for RR and 82.5 for ODR (IQR 65 to 96.3) at 12 months, which was also noninferior (t-statistic = -3.14 (n = 133); p = 0.001, TOST equivalence test).
Fig. 2.
Olerud-Molander Ankle Score (OMAS) at each timepoint for intention to treat groups. Boxplot depicting minimum, maximum, interquartile range, and median of the OMAS for randomized groups at different timepoints. ODR, on-demand removal; RR, routine removal.
Secondary outcomes
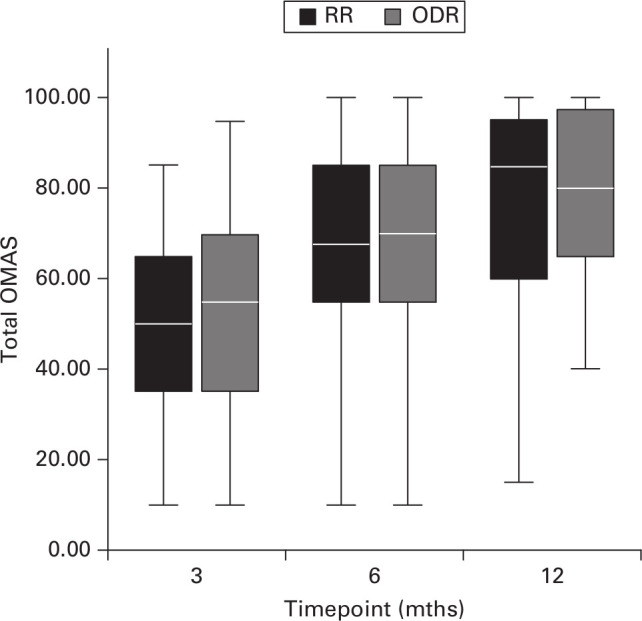
OMAS scores at three and six months after syndesmotic fixation were comparable between randomization groups, as illustrated in Figure 2. Functional outcome as measured by the AOFAS hindfoot score also did not differ between RR and ODR at any timepoint. At three months, median scores were 77 (IQR 61.3 to 82) and 78 (IQR 67 to 86) for RR and ODR, respectively (p = 0.138, Mann-Whitney U test), for six months this was 81 (IQR 71.8 to 88) and 85 (IQR 75 to 90) (p = 0.103, Mann-Whitney U test), and for 12 months 87 (IQR 84 to 98) and 85 (IQR 80 to 100) (p = 0.787, Mann-Whitney U test). When zooming in on the sub-scores of the AOFAS, the sub-score “function” was marginally higher for the ODR group at three and six months compared to the RR group (Supplementary Figure a). Neither ROM nor the VAS pain scores differed significantly at any timepoint (Figure 3).
Fig. 3.
a) Mean range of motion (ROM) difference (flexion + extension) between healthy and injured ankles. b) Mean visual analogue scale (VAS). ODR, on-demand removal; RR, routine removal.
Complications
There were significantly more complications in the RR group (12/73) than in the ODR group (1/79) (p = 0.007, chi-squared test). The 12 complications in the RR group comprised: wound dehiscence (n = 5), superficial SSI (n = 2), deep SSI (n = 2), diastasis after removal (n = 1), synovitis (n = 1), and increase in stiffness after removal (n = 1). Four of 12 patients had a complication of the syndesmotic fixation as well; two deep infections (one resulting in a flare-up after removal, one in diastasis after removal), one superficial SSI (wound dehiscence after removal), and a synovitis (persisting after removal). In addition, within the lost-to-follow-up group, three complications occurred consisting of one deep SSI, one superficial SSI, and one diastasis. In the ODR group, there was only one complication: a superficial SSI after removal of all implants, seven months after syndesmotic fixation. In the crossover patients, no complications arose. In one lost-to-follow-up patient, who would have crossed over to ODR, the retained screw started to back out 14 months after placement, ultimately resulting in a fistula, after which the screw was removed.
Predictors of functional outcome
Possible predictors for functional outcome, as identified in univariate linear regression, were age, sex, alcohol abuse, illegal drugs abuse, previous fracture, American Society of Anesthesiologists classification,22 type of fracture, duration of fixation surgery, diameter of screw, cast treatment (after syndesmotic fixation), status of screw (broken/intact/removed), complication of syndesmotic fixation surgery, complication of RR/ODR, and revision surgery. In multivariable analysis, female sex, longer duration of primary surgery, complication of fixation, and complication of RR/ODR remained independent predictors of outcome with a negative impact on 12-month OMAS (Supplementary Table ii).
Subgroup analysis
OMAS score at 12 months was noninferior between ODR and RR in patients aged < 60 years (p = 0.001, Mann-Whitney U test), with median of 85 (IQR 65 to 95) in the RR group and 85 (IQR 62.5 to 100) in the ODR groups. For patients aged ≥ 60 years, the median OMAS was 77.5 (IQR 55 to 96.3) in the RR group and 80 (IQR 63.8 to 92.5) in the ODR group, which was also noninferior (p = 0.041, TOST equivalence test).
Discussion
In this multicentre, randomized controlled trial, we found that ODR of the syndesmotic screw was noninferior to RR with regard to functional outcome. Additionally, no differences were identified in pain or ROM at any given timepoint between the two groups.
Functional outcome scores found in this trial were comparable to previous literature. Two systematic reviews have appeared discussing differences in functional outcome after removing or retaining the syndesmotic screw.23,24 Both concluded that RR is not indicated. However, this conclusion was based on low-quality and mostly retrospective studies. The one RCT that was included in both reviews found an OMAS of 82.4 in the group retaining the screw and 86.7 in the screw removal group (p = 0.367).11 In the other RCT by Høiness and Strømsøe,25 the RR group received one quadcortical screw and the ODR group two tricortical screws.25 They found significantly better outcomes of the ODR group at three months, but no statistically significant difference in mean OMAS after 12 months with 88.8 points for ODR and 83.3 for RR.25
Significantly more complications occurred in the RR group, mostly consisting of wound healing disorders. Previous studies have shown that the incidence of SSIs after syndesmotic screw removal was around 4%. We found SSI rates of 5%, and if patients without primary outcome were included this was even higher (8.2%). In addition, wound dehiscence was quite common (5/73).
We found that only 23% of patients (n = 18) randomized for ODR had their screw removed (within 12 months), in the scenario where patients were told that their screw could be removed at any time. If the results of this trial are implemented in guidelines, counselling of patients has the potential to further decrease the removal rate. As the results of this trial show, by not routinely removing screws, many removal procedures and therefore complications can be avoided.
As for the subgroup analysis on age, ODR was not inferior to RR. This, combined with the larger difference in median OMAS scores (in favour of ODR) for patients aged 60 years or over, might suggest that in this age group it may be even more beneficial to retain the syndesmotic screw. This finding is also supported by the fact that the higher the age and the comorbidities that come with it, the larger the risk of complications of every surgery. However, these results need to be interpreted with care as the group size, as calculated by the power calculation, was not reached and we are therefore unable to draw definitive conclusions regarding this hypothesis.
Our study has several limitations. First of all, since this was a pragmatic trial without instructions for fixation and no postoperative CT scans, the quality of tibiofibular reduction could not be guaranteed or evaluated sufficiently. The pragmatic design of this trial (different local protocols, surgeons, and surgical characteristics) may also be a potential weakness, since it induces heterogeneity. Second, a significant amount of patients who were eligible declined participation because of the randomization aspect, causing a potential selection bias. Moreover, the loss to follow-up rate (22.8%) was higher than predicted, thereby decreasing the power of the study. Most patients resumed their daily lives between three and six months after fixation, and were therefore less motivated to come back to the hospital and/or fill out the questionnaires at 12 months. Although baseline criteria of lost-to-follow-up patients were acquired, uncollected characteristics such as environment and social class may very well differ and influence the outcome, causing a selection bias.26 However, no significant differences were found in baseline criteria between patients lost to follow-up and included patients, and loss to follow-up was equally distributed over randomization groups. Moreover, a post-hoc power analysis showed that in order to achieve 80% power, 70 patients per group would be sufficient, which was achieved in all groups except from the subgroup of patients > 60 years. Another limitation is that the quality of the syndesmotic reduction was not routinely evaluated. Malreduction is common and can occur in over 16% of surgically treated patients with syndesmotic injury.27-29 A CT scan during surgery or postoperatively was not performed as this was not a standard procedure in the participating hospitals.
In line with the previous limitation, radiological imaging at the 12-month timepoint was only acquired in a minority of patients, which leaves us uncertain about the status of the screws (broken/intact) at that time. To compare outcome between removed, broken, and intact screws, we have excluded patients with no confirmed status of the screw, leading to smaller groups and conclusions based on incomplete data.
The short-term follow-up might be considered another limitation of the study. We chose the end point of one year because, as Egol et al1 showed, patients score at pre-injury levels of functional outcome at that time, and are believed to have reached their maximum functional recovery capacity.
Finally, although we found a very low rate of complications in the ODR group, 12-month follow-up might not be sufficient for this outcome. It is important to keep in mind that there might be long-term complications of retaining the syndesmotic screw that we have not encountered in this trial. Future studies should focus on the long-term consequences of retaining the syndesmotic screw and identifying uncontested indications for removal.
In this study, ODR of the syndesmotic screw was noninferior to RR in terms of functional outcome, supporting our hypothesis. Combined with the high complication rate of screw removal, this offers a strong argument to adopt ODR as standard practice of care after syndesmotic screw fixation.
Take home message
- Many complications including surgical site infections may be avoided without compromising functional outcome when syndesmotic screws are solely removed on demand.
- Novel, more expensive techniques for the fixation of syndesmotic injury no longer have an advantage when it comes to the argument of avoiding implant removal.
Author contributions
F. R. K. Sanders: Project administration, Supervision, Formal analysis, Writing – original draft, Writing – review & editing.
M. F. Birnie: Project administration, Supervision, Formal analysis, Writing – original draft, Writing – review & editing.
S. A. Dingemans: Conceptualization, Methodology, Project administration, Supervision, Formal analysis, Writing – review & editing.
M. P. J. van den Bekerom: Conceptualization, Methodology, Writing – review & editing.
M. Parkkinen: Writing – review & editing.
R. N. van Veen: Writing – review & editing.
J. C. Goslings: Conceptualization, Methodology, Formal analysis, Writing – review & editing.
T. Schepers: Conceptualization, Methodology, Formal analysis, Writing – review & editing.
Funding statement
This trial, including the open access fee, was funded by ZonMw, a non-profit Dutch Government Institution, with project number 843002705. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The RODEO collaborator group: Susan van Dieren, PhD, Epidemiologist, Trauma Unit, Department of Surgery, Amsterdam UMC, University of Amsterdam, Amsterdam; Frank W. Bloemers, MD, PhD, Trauma Surgeon, Department of Trauma Surgery, Amsterdam UMC, Amsterdam; Bart A. van Dijkman, MD, Trauma and General Surgeon, Department of Trauma Surgery, Spaarne Gasthuis, Haarlem; Elvira R. Flikweert, MD, Trauma and General Surgeon, Department of Trauma Surgery, Deventer Ziekenhuis, Deventer; Frank Garssen, MD, Trauma and General Surgeon, Department of Trauma Surgery, Ziekenhuis Amstelland, Amstelveen; Daniel Haverkamp, MD, Orthopaedic Surgeon, Department of Orthopaedic Surgery, Slotervaartziekenhuis, Amsterdam; Jochem Hoogendoorn, MD, PhD, Trauma and General Surgeon, Department of Trauma Surgery, MC Haaglanden, the Hague; Pieter Joosse, MD PhD, Trauma Surgeon, Department of Trauma Surgery, Noordwest Ziekenhuisgroep, Alkmaar; Ewan D. Ritchie, MD, Trauma Surgeon, Department of Trauma Surgery, Alrijne Ziekenhuis, Leiderdorp; Gert R. Roukema, MD, Trauma and General Surgeon, and Niels W L Schep, MD PhD, Trauma and General Surgeon, Department of Trauma Surgery, Maasstad Ziekenhuis, Rotterdam; Nico L Sosef, MD PhD, Trauma and General Surgeon, Jefrey Vermeulen, MD PhD, Trauma and General Surgeon, Steven van der Werff, MD, Resident not in training, Department of Trauma Surgery, Spaarne Gasthuis, Hoofddorp; Bas Twigt, MD PhD, Trauma Surgeon, Department of Trauma Surgery, BovenIJ ziekenhuis, Amsterdam; Alexander H. van der Veen, MD PhD, Trauma Surgeon, Department of Trauma Surgery, Catharina Ziekenhuis, Eindhoven; Jasper Winkelhagen, MD, Trauma Surgeon, Department of Trauma Surgery, Westfries Gasthuis, Hoorn; Babette C. van der Zwaard, PhD Research Scientist, Research and education, Jeroen Bosch Ziekenhuis, 's-Hertogenbosch, the Netherlands.
Ethical review statement
This trial (NL58539.018.16) was approved on the 6th of September, 2016 by the Medical Ethical Review Committee (METC) of the Academic Medical Centre, with local reference number "2016_197".
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Trial registration number
The study was registered at ClinicalTrials.gov (NCT02896998).
Supplementary material
Baseline criteria of included patients versus those who were lost to follow-up, and the predictors of functional outcome with their confidence intervals and statistical significance.
This article was primary edited by M. Hossain.
Contributor Information
Fay R. K. Sanders, Email: f.r.sanders@amc.nl.
Merel F. Birnie, Email: m.f.birnie@amsterdamumc.nl.
Siem A. Dingemans, Email: s.a.dingemans@amc.nl.
Michel P. J. van den Bekerom, Email: M.P.J.vandenBekerom@olvg.nl.
Markus Parkkinen, Email: medipark@me.com.
Ruben N. van Veen, Email: r.n.vanveen@olvg.nl.
J. Carel Goslings, Email: j.c.Goslings@amc.nl.
Tim Schepers, Email: t.schepers@amsterdamumc.nl.
References
- 1.Egol KA, Pahk B, Walsh M, Tejwani NC, Davidovitch RI, Koval KJ. Outcome after unstable ankle fracture: effect of syndesmotic stabilization. J Orthop Trauma. 2010;24(1):7–11. [DOI] [PubMed] [Google Scholar]
- 2.van den Bekerom MPJ, Lamme B, Hogervorst M, Bolhuis HW. Which ankle fractures require syndesmotic stabilization? J Foot Ankle Surg. 2007;46(6):456–463. [DOI] [PubMed] [Google Scholar]
- 3.Schepers T, van Zuuren WJ, Vogels LMM, van Lieshout EM. The management of acute distal tibio-fibular syndesmotic injuries: results of a nationwide survey. Injury Netherlands. 2012;43(10):1718–1723. [DOI] [PubMed] [Google Scholar]
- 4.Bell DP, Wong MK. Syndesmotic screw fixation in Weber C ankle injuries--should the screw be removed before weight bearing. Injury Netherlands. 2006;37(9):891–898. [DOI] [PubMed] [Google Scholar]
- 5.Miller AN, Paul O, Boraiah S, Parker RJ, Helfet DL, Lorich DG. Functional outcomes after syndesmotic screw fixation and removal. J Orthop Trauma. 2010;24(1):12–16. [DOI] [PubMed] [Google Scholar]
- 6.Amouzadeh Omrani F, Kazemian G, Salimi S. Evaluation of syndesmosis reduction after removal syndesmosis screw in ankle fracture with syndesmosis injury. Adv Biomed Res. 2019;8:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briceno J, Wusu T, Kaiser P, et al. . Effect of syndesmotic implant removal on dorsiflexion. Foot Ankle Int. 2019;40(5):499–505. [DOI] [PubMed] [Google Scholar]
- 8.Manjoo A, Sanders DW, Tieszer C, MacLeod MD. Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma United States. 2010;24(1):2–6. [DOI] [PubMed] [Google Scholar]
- 9.Pogliacomi F, Artoni C, Riccoboni S, Calderazzi F, Vaienti E, Ceccarelli F. The management of syndesmotic screw in ankle fractures. Acta Biomed. 2019;90(1):146–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaftandziev I, Spasov M, Trpeski S, Zafirova-Ivanovska B, Bakota B. Fate of the syndesmotic screw: search for a prudent solution. Injury Netherlands. 2015;46(Suppl 6):S125-9. [DOI] [PubMed] [Google Scholar]
- 11.Boyle MJ, Gao R, Frampton CMA, Coleman B. Removal of the syndesmotic screw after the surgical treatment of a fracture of the ankle in adult patients does not affect one-year outcomes: A randomised controlled trial. Bone Joint J. 2014;96-B(12):1699–1705. [DOI] [PubMed] [Google Scholar]
- 12.Andersen MR, Frihagen F, Madsen JE, Figved W. High complication rate after syndesmotic screw removal. Injury. 2015;46(11):2283–2287. [DOI] [PubMed] [Google Scholar]
- 13.Juarez-Jimenez HG, Garibay-Cervantes A, Rosas-Medina JA, Salas-Morales GA, Rodriguez-Reyes EJ. Prevalence of complications related to the removal of the syndesmotic screw. Acta Ortop Mex. 2018;32(2):76–81. [PubMed] [Google Scholar]
- 14.Schepers T, Van LE, de VM, der EM. Complications of syndesmotic screw removal. Foot Ankle Int. 2011;32(11):1040–1044. [DOI] [PubMed] [Google Scholar]
- 15.Dingemans SA, Birnie MFN, Sanders FRK, Van Den bekerom MPJ, Backes M, Van Beeck E. Routine versus on demand removal of the syndesmotic screw; A protocol for an international randomised controlled trial (RODEO-trial). BMC Musculoskelet Disord. 2018;19(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker SP, O’Neill B, Haddon W, Long WB. The Injury Severity Score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 17.Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103(3):190–194. [DOI] [PubMed] [Google Scholar]
- 18.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7). [DOI] [PubMed] [Google Scholar]
- 19.Berríos-Torres SI, Umscheid C, Bratzler D, et al. . Centers for Disease Control and Prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784–791. [DOI] [PubMed] [Google Scholar]
- 20. No authors listed . Castor Electronic Data Capture. 2021. https://castoredc.com (date last accessed 27 September 2021).
- 21.Lakens D. TOST equivalence testing. OSF. 2016. osf.io/q253c (date last accessed 27 September 2021).
- 22.Saklad M. Grading of patients for surgical procedures. Anesthesiol. 1941;2(5):281–284. [Google Scholar]
- 23.Dingemans SA, Rammelt S, White TO, Goslings JC, Schepers T. Should syndesmotic screws be removed after surgical fixation of unstable ankle fractures? a systematic review. Bone Joint J. 2016;98-B(11):1497–1504. [DOI] [PubMed] [Google Scholar]
- 24.Walley KC, Hofmann KJ, Velasco BT, Kwon JY. Removal of hardware after syndesmotic screw fixation: A systematic literature review. Foot Ankle Spec. 2017;10(3):252–257. [DOI] [PubMed] [Google Scholar]
- 25.Høiness P, Strømsøe K. Tricortical versus quadricortical syndesmosis fixation in ankle fractures: a prospective, randomized study comparing two methods of syndesmosis fixation. J Orthop Trauma. 2004;18(6):331–337. [DOI] [PubMed] [Google Scholar]
- 26.Murnaghan ML, Buckley RE. Lost but not forgotten: patients lost to follow-up in a trauma database. Can J Surg. 2002;45(3):191–195. [PMC free article] [PubMed] [Google Scholar]
- 27.Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma United States. 2005;19(2):102–108. [DOI] [PubMed] [Google Scholar]
- 28.Franke J, von Recum J, Suda AJ, Grützner PA, Wendl K. Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. J Bone Jt Surg - Ser A. 2012;94(15):1386–1390. [DOI] [PubMed] [Google Scholar]
- 29.Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012;26(7):439–443. [DOI] [PubMed] [Google Scholar]