18F-GP1 is a novel radiotracer that binds to the platelet glycoprotein IIb/IIIa receptor and can image in vivo venous and arterial thrombi, including deep vein thrombosis and pulmonary thromboemboli (1–3). We performed 18F-GP1 positron emission tomography–computed tomography in six patients recovering from coronavirus disease (COVID-19) with concomitant pulmonary embolism (median age 56 [interquartile range, 53–60] years, one female, five requiring supplemental oxygen, no intensive care admissions) and undertook 18F-GP1 autoradiography of postmortem lung tissue in three patients who had died from COVID-19 (4).
All patients demonstrated increased pulmonary 18F-GP1 uptake at a median of 69 (interquartile range, 56–98) days after index presentation despite ongoing therapeutic oral anticoagulation. Focal intravascular uptake in persistent pulmonary embolism (Figure 1A) was seen, as described previously (1). However, we also noted parenchymal uptake in regions of consolidation (Figure 1B) as well as systemic uptake in an occluded saphenous vein coronary artery bypass graft and left ventricular thrombus, which was subsequently confirmed on echocardiography (Figure 1C). 18F-GP1 autoradiography also demonstrated focal and specific uptake colocalizing to intravascular thrombus in patients with confirmed diffuse alveolar damage (Figure 1D).
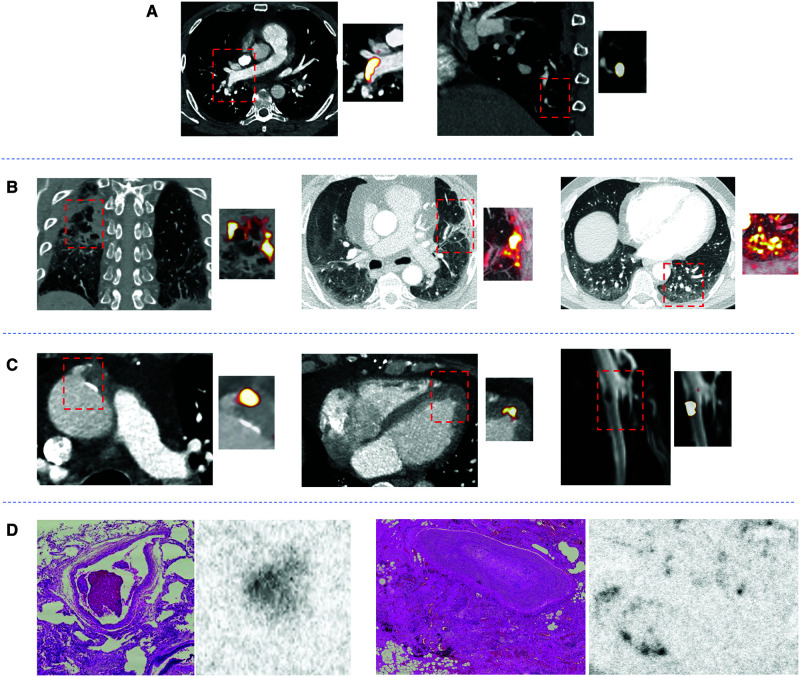
Figure 1.
(A) The left shows segmental pulmonary embolus with associated 18F-GP1 uptake, and the right shows focal 18F-GP1 uptake without computed tomography pulmonary angiogram evidence of subsegmental thrombus. (B) Three examples of parenchymal 18F-GP1 uptake associated with consolidation (left), healing peripheral infarction (middle), and nodular uptake in ground-glass changes with an associated dilated pulmonary artery but no evidence of pulmonary embolism at this site on computed tomography pulmonary angiogram (right). (C) Incidental systemic intravascular thrombosis and associated 18F-GP1 uptake at the site of an occluded saphenous vein coronary artery bypass graft (left), apical left ventricular thrombus (middle), and left common femoral vein deep vein thrombosis (right). (D) Hematoxylin and eosin–stained sections of postmortem pulmonary tissue with corresponding 18F-GP1 autoradiography in two patients who died of coronavirus disease (COVID-19). Diffuse alveolar damage and microvascular thrombosis was seen on histopathology. 18F-GP1 colocalizes to intravascular thrombus (left, center-left) but not to more organized thrombus of older duration (center-right, right). There is also 18F-GP1 signal in smoking-related anthracotic pigment.
Protracted systemic and pulmonary thrombosis may be a feature of COVID-19 that can persist despite systemic therapeutic anticoagulation. 18F-GP1 is able to detect pulmonary and systemic arterial thrombosis and has potential applications across a broad range of pathologies.
Footnotes
Supported by the British Heart Foundation (RG/16/10/32375, RE/18/5/34216, and PG/19/40/34422).
Author Contributions: R.B., J.P.M.A., M.C.W., E.J.R.v.B, M.R.D., and D.E.N. designed the study. R.B., J.P.M.A., M.C.W., E.J.R.v.B, C.L., G.M., T.C., N.K., A.W.S., M.G.M., A.A.S.T., K.D., D.A.D., C.D.L., M.R.D., and D.E.N. contributed to data acquisition and analysis or interpretation. R.B. drafted the work. All authors revised the final version and approved it for publication. R.B. is responsible for data integrity.
Originally Published in Press as DOI: 10.1164/rccm.202011-4182IM on August 10, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Kim C, Lee JS, Han Y, Chae SY, Jin S, Sung C, et al. Glycoprotein IIb/IIIa receptor imaging with (18)F-GP1 positron emission tomography for acute venous thromboembolism: an open-label, non-randomized, first-in-human phase 1 study. J Nucl Med. 2018;60:244–249. doi: 10.2967/jnumed.118.212084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chae SY, Kwon TW, Jin S, Kwon SU, Sung C, Oh SJ, et al. A phase 1, first-in-human study of 18F-GP1 positron emission tomography for imaging acute arterial thrombosis. EJNMMI Res. 2019;9:3. doi: 10.1186/s13550-018-0471-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lohrke J, Siebeneicher H, Berger M, Reinhardt M, Berndt M, Mueller A, et al. (18)F-GP1, a novel PET tracer designed for high-sensitivity, low-background detection of thrombi. J Nucl Med. 2017;58:1094–1099. doi: 10.2967/jnumed.116.188896. [DOI] [PubMed] [Google Scholar]
- 4. Dorward DA, Russell CD, Um IH, Elshani M, Armstrong SD, Penrice-Randal R, et al. Tissue-Specific Immunopathology in Fatal COVID-19. Am J Respir Crit Care Med. 2021;203:192–201. doi: 10.1164/rccm.202008-3265OC. [DOI] [PMC free article] [PubMed] [Google Scholar]