Abstract
Objective
To assess the feasibility and results of tibial cortex transverse distraction (TCTD) followed by open correction with internal fixation (OCIF) for foot and ankle deformity with concurrent ulcers.
Methods
A retrospective analysis was conducted. Between 2010 and 2019, a two‐stage management of TCTD followed by OCIF was performed in 13 patients (13 feet). There were five males and eight females with a mean age of 33.8 ± 14.6 years. Ten patients had a right‐side lesion, and three patients had a left‐side lesion. The etiology of deformity included seven cases of congenital neurological disease, one case of Charcot–Marie–Tooth disease, one case of trauma sequelae, and three cases of myelomeningocele. Duration of disease, size of ulcers, surgical procedures, healing time, external fixation time, and complications of these patients were recorded. The Texas wound classification and National Pressure Ulcer Advisory Panel (NPUAP) classification were used for assessing the ulcers. The modified Dimeglio score of deformity and American Orthopeadic Foot and Ankle Society (AOFAS) ankle‐hindfoot score were applied to evaluate the status before treatment and the results at final follow‐up.
Results
The TCTD and wound debridement were performed in all patients, and an additional Ilizarov correction technique was added in two patients. All ulcers were healed in 3 months after first‐stage treatment. The median patient self‐report time of ulcer healing was 2.0 weeks (IQR, 1.8–3.3). The median external fixation time was 138.0 days (IQR, 134.5–141.5) days. After second‐stage operative correction, the patients were followed‐up for an average of 28.0 ± 2.9 months. At the final follow‐up, the modified Dimeglio score of deformity was decreased from 6.7 ± 2.1 to 1 (IQR, 0.0–1.0), and the mean AOFAS score was improved from 42.9 ± 19.1 to 82.6 ± 7.7. Before the treatment, there were eight patients with severe deformity, four patients with moderate deformity, and one patient with mild deformity. Postoperatively, seven patients were classified as mild deformity and six patients had a postural foot. The results of AOFAS ankle‐hindfoot score were defined as excellent in three patients, as good in five, and as fair in five. Complications include one case of mild displacement of the osteotomized cortex and one case of pin‐tract infection. No delayed union, nonunion, relapse of ulcers, or deformity were observed.
Conclusions
The two‐stage management of TCTD followed by OCIF could be considered as an alternative treatment for foot and ankle deformities combined with chronic ulcers.
Keywords: Foot and ankle deformity, Ilizarov, Open correction and internal fixation, Tibial cortex transverse distraction, Ulcer
We applied a two‐stage management of tibial cortex transverse distraction (TCTD) followed by open correction with internal fixation (OCIF) for foot and ankle deformities combined with chronic ulcers. This strategy could be considered as an alternative treatment for recalcitrant ulcers with deformity in foot and ankle, as complete healing of ulcers and excellent correction of deformity were achieved in this case series.

Introduction
Foot and ankle deformity with concurrent ulcer is one of the difficult clinical problems in foot and ankle surgery and its underlying etiology can be various. This complex problem is common in patients with neurologic foot or trauma sequelae. On the one hand, foot and ankle deformities caused by various diseases can result in abnormal foot pressure distribution 1 . This long‐term high pressure in some weight‐bearing areas of foot predisposes callosities, soft‐tissue damage, and even chronic ulcers 2 , 3 , 4 , 5 . On the other hand, ulcers or sinus tract could also occur in non‐weight‐bearing area in some patients with trauma sequelae (Fig. 1). Trauma could lead to foot and ankle deformities, infective ulcers or sinus tract, and insufficient blood perfusion at the same time. This kind of non‐healing ulcer was not caused by high pressure but resulted from the original injury.
Fig. 1.
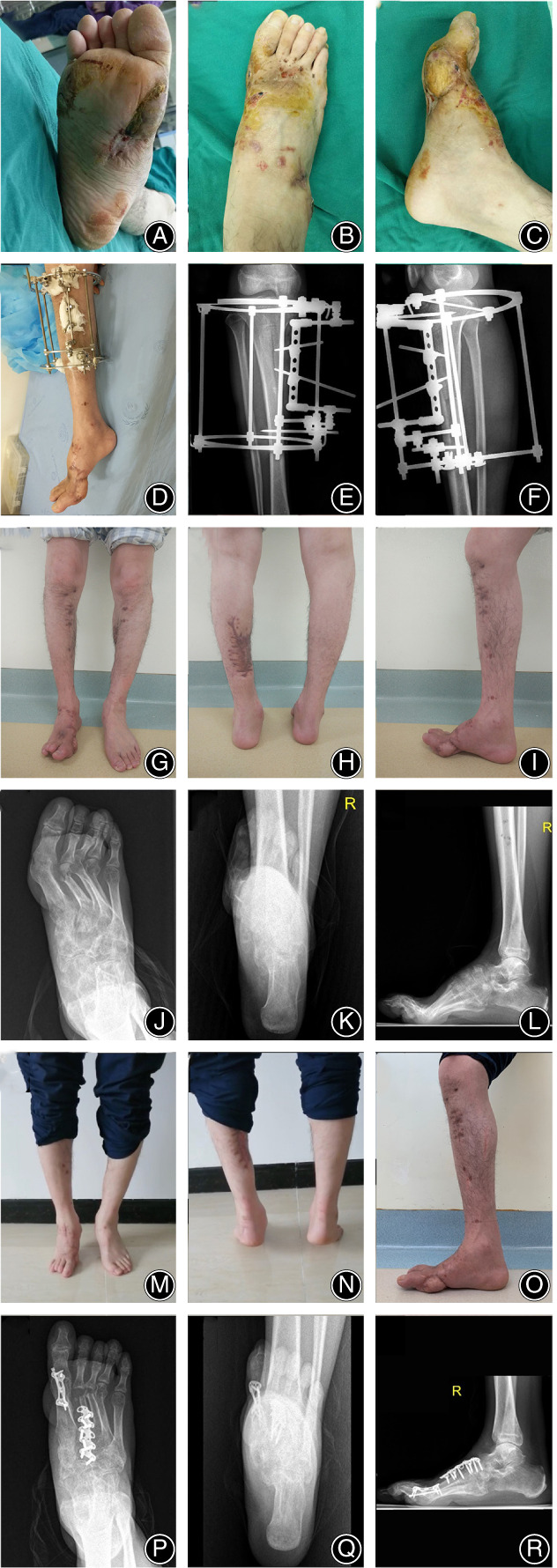
(A–C) Preoperative photographs show a foot deformity with a concurrent ulcer. (D–F) An Ilizarovtransverse distraction frame is used for tibial transverse distraction. (G–L) After the first‐stage treatment, theulcer has healed but the foot deformity needs to be corrected. (M) The anterior and (N) the posterior photographs of his standing on tiptoes and the lateral photograph of his foot appearance show excellent foot function and deformity correction after open correction with internalfixation. (P–R) Postoperative radiographs show satisfactorycorrection of the foot deformity.
However, no matter what causes foot and ankle deformity with concurrent ulcers, the management for this disease is challenging. Unfortunately, as far as we know, only one study has focused on the management of this complex condition 4 . In their study, Kliushin et al. applied an Ilizarov corrective frame for management of neurologic deformity of ankle and foot with concurrent osteomyelitis in a total of 77 patients 4 . Their management was divided into three phases including: (i) debridement and stabilization (approximately 3–4 weeks); (ii) active osteosynthesis (approximately 2–4 weeks); and (iii) consolidation (approximately 2–4 months). Even though ulcer healing and eradication of infection could be obtained and a stable plantigrade foot could be achieved, the lengthy duration of external fixation caused serious inconvenience to the patients and limited their quality of life as acknowledged by the authors themselves 4 . The application of open correction with internal fixation (OCIF) could obtain immediate correction and thus avoid prolonged external fixation but is restricted by the existence of infected ulcers. When OCIF is selected, the management of infected ulcers is an important and priority step in achieving an ulcer‐free plantigrade foot in these patients.
In the complex situation of foot and ankle deformity with concurrent ulcers, although these ulcers were not caused by diabetes or ischemic disease, in the wound still existed microcirculation disorder, local tissue ischemia, and chronic inflammation. Thus, their treatment should also follow the following principles: controlling infection, modulating inflammation, promoting angiogenesis, and consequently facilitating wound healing 5 , 6 , 7 , 8 , 9 . Conventional treatments for chronic ulcers include debridement, infection control, mechanical off‐loading, and wound care therapies 10 , 11 . For some patients, however, the long process of treatment makes it difficult to adhere the treatment, or the chronic ulcers still fail to heal despite treatment, requiring advanced methods are for adequate wound healing 12 , 13 .
Tibial cortex transverse distraction (TCTD), a novel technique based on the “tension‐stress principle” proposed by Ilizarov 14 , 15 , has been shown as an effective treatment for chronic ulcers resulting from diabetes mellitus, thromboangiitis obliterans, and chronic ischemic diseases 16 , 17 , 18 . It also has been demonstrated that TCTD has the advantages of facilitating the healing of recalcitrant non‐diabetic ulcers and shortening the healing time compared with conventional surgical methods 19 . The oretically, based on the potential mechanisms (promote angiogenesis, control infection, and improve wound healing) of TCTD, this technique could also be used for the management of foot and ankle deformities with concurrent ulcers which share common characteristics with diabetic or ischemic ulcers: chronic inflammation and impaired microcirculation. The longstanding pathological conditions of chronic ulcers in these patients might be corrected by TCTD based on the Ilizarov tension‐stress principle. TCTD may also reduce the healing time and increase the success rate for ulcers compared with traditional method and OCIF could provide precise correction and avoid the inconvenience of prolonged external fixation time compared with external fixation. To our best knowledge, however, the application of tibial cortex transverse distraction in foot and ankle deformity with concurrent ulcers has not been previously reported.
Consequently, we hypothesized that: (i) first‐stage treatment using TCTD would be an effective method to facilitate healing of chronic pressure ulcers caused by foot and ankle deformities; (ii) second‐stage treatment of OCIF could provide effective correction for foot and ankle deformities with less recurrence risk of infection and deformity; and (iii) two‐stage management of TCTD followed by OCIF could be considered as an alternative method for foot and ankle deformity with concurrent ulcers. To prove these hypotheses, a retrospective study was performed to evaluate the outcomes of the two‐stage treatment, TCTD followed by OCIF, in a consecutive series of 13 patients. The aims of the present study were: (i) to evaluate the clinical outcomes of TCTD followed by OCIF in this specific series of patients; (ii) to provide our initial experience using TCTD for promoting ulcer healing in patients who suffered from foot and ankle deformity with concurrent ulcers; and (iii) to analyze the advantages and disadvantages of TCTD followed by OCIF for management of foot and ankle deformity combined with chronic ulcers.
Materials and Methods
Inclusion and Exclusion Criteria
A retrospective review of collected data between 2010 and 2019 from our department database was conducted under the ethical approval by the Research Ethics Committee of our Hospital.
The inclusion criteria followed the PICOS principle: (i) patients diagnosed with foot and ankle deformity with non‐healing or recurrent ulcers; (ii) patients treated with TCTD followed by OCIF; (iii) preoperative and postoperative comparisons were made with measures including the American Orthopeadic Foot and Ankle Society (AOFAS) ankle hindfoot score and the modified Dimeglio score; (iv) postoperative AOFAS ankle hindfoot score and modified Dimeglio score are significantly improved compared to preoperatively; and (v) the study design was a retrospective study. Eighteen patients (18 feet) met the inclusion criteria in initial screening (Fig. 2A–F).
Fig. 2.
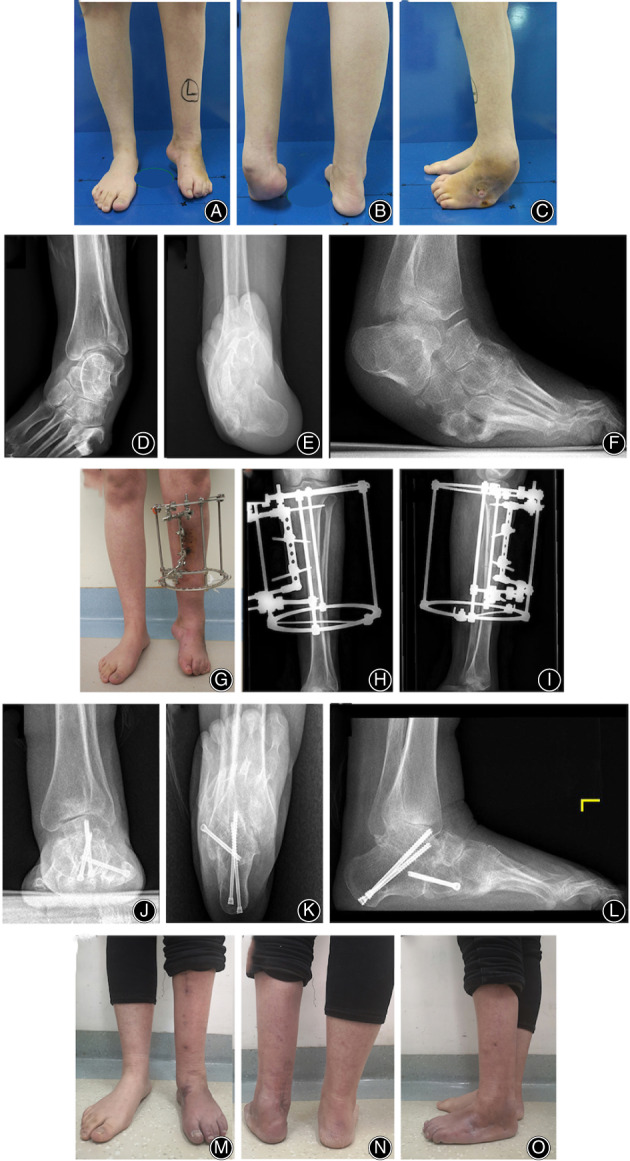
Clinical and radiographical photographs of a 30‐year‐old female patient who has an equinocavovarus foot with a concurrent chronic ulcer not responding to multiple debridements. (A–F) Preoperative photographs show an equinocavovarus foot with a concurrent ulcer. (G–I) Tibial transverse distraction is performed with an Ilizarov transverse distraction frame. (J–O) After ulcer healing and removal of Ilizarov frame, the patient undergoes open correction and internal fixation.
Exclusion criteria were patients with: (i) Charcot arthropathy (one patient); (ii) peripheral vascular dysfunction (two patients); (iii) diabetes mellitus (two patients, one of the two patients has been excluded due to Charcot arthropathy resulted from diabetes); and (iv) follow‐up of <24 months (one patient). Thus, five patients were excluded according to the exclusion criteria.
Based on the inclusion and exclusion criteria, the final analysis included the data of 13 patients (13 feet). The details of the patients are shown in Table 1. All patients were treated by TCTD followed by OCIF because they had not responded to previous treatments for a minimum of 3 months. Previous treatments included non‐operation management (including wound care, off‐loading, etc.), debridement only, skin grafting and flap transplantation.
TABLE 1.
Descriptive characteristics of patients
| Case | Age (years) | Gender | Side | Etiology | Duration of deformity (years) | Type of deformity | Duration of ulcer (years) | Site of ulcer | Size of ulcer (cm2) | Texas wound classification | NPUAP classification |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 54 | Female | Right | Congenital neurological diseases | 50 | Equinocavovarus | 4 | Forefoot | 6.8 | 2D | III |
| 2 | 46 | Female | right | Charcot–Marie–Tooth Disease | 30 | Equinocavovarus | 6 | Forefoot | 9.0 | 3D | IV |
| 3 | 41 | Female | Right | Poliomyelitis | 37 | Equinocavovarus | 2 | Forefoot | 3.6 | 3D | IV |
| 4 | 38 | Male | Right | Trauma sequelae | 2 | Equinocavovarus | 1 | Forefoot | 0.8 | 3D | IV |
| 5 | 25 | Female | right | Myelomeningocele | 13 | Equinocavovarus | 1 | Hindfoot | 100.0 | 3D | IV |
| 6 | 18 | Male | Left | Congenital neurological diseases | 18 | Equinocavovarus | 3 | Midfoot | 6.2 | 3B | IV |
| 7 | 16 | Female | Right | Congenital neurological diseases | 16 | Equinovarus | 1 | Forefoot | 9.0 | 3B | IV |
| 8 | 30 | Male | Right | Myelomeningocele | 20 | Equinocavovarus | 4 | Forefoot | 0.8 | 2D | III |
| 9 | 48 | Female | Right | Congenital neurological diseases | 48 | Equinocavovarus | 2 | Midfoot | 1.0 | 2D | III |
| 10 | 30 | Female | Left | Congenital neurological diseases | 30 | Equinovarus | 2 | Midfoot | 0.8 | 3B | IV |
| 11 | 14 | Male | Right | Congenital neurological diseases | 14 | Equinocavovarus | 2 | Midfoot | 2.6 | 2D | III |
| 12 | 23 | Female | Right | Myelomeningocele | 14 | Equinocavovarus | 1 | Forefoot | 4.0 | 3D | IV |
| 13 | 57 | Male | Left | Congenital neurological diseases | 50 | Equinocavovarus | 2 | Midfoot | 1.0 | 2C | III |
Management
First Stage
Preoperatively, plain radiography, computed tomography (CT) scans, magnetic resonance imaging (MRI), color Doppler sonography (CDS) of peripheral blood vessels, routine blood examination, erythrocyte sedimentation rate (ESR) and serum level of C‐reactive protein (CRP), and bacterial culture of wound were performed to determine a reasonable operation plan. Empirical antibiotics were administered as early as possible. All procedures were performed under general anesthesia in the supine position by a senior surgeon.
Proximal tibial corticotomy was first performed with the infected ulcers covered by sterile dressing. An 8 cm longitudinal incision was made on the anteromedial of lower leg to expose the tibial. The tibial periosteum was exposed but not removed from the cortex. After the rough location of corticotomy on the medial cortex of tibia was determined, a cortical window with a size of 1.5 × 10 cm was osteotomized by carefully drilling multiple holes in ipsilateral cortex with the help of a special guide. During this process, cool normal saline was used to prevent thermal injury and all surrounding tissues including the periosteum should be protected as much as possible. After drilling, two distraction pins (diameter: 3.5 mm; distance between the two pins: 3 cm; the angle between the two pins: 5°–10°) were inserted through unilateral cortex for postoperative distraction of osteotomized cortex. Then, to install a special Ilizarov frame which consists of: (i) two tibial rings (attached with one wire and one half pin on each ring or two half pins on each ring) for fixation; and (ii) a combined unit for transverse distraction (Fig. 2G,I). The two rings were connected longitudinally with four rods with 20 cm between the two rings. The two distraction pins were screwed onto the straight metal piece using blots, and then the whole distraction unit (including the two distraction pins and the metal piece) was attached to the frame using rods and screws which allow the distraction movement postoperatively. For tibial corticotomy, an osteotome could be useful to connect all the holes so as to separate the cortex from the tibial shaft. For patients with severe deformity, limited soft‐tissue releases were performed to address tissue contracture and an additional Ilizarov frame was simultaneously installed at this time to gradually correct soft tissue. The surgical incisions were irrigated before closing. Sterile gauze was used to cover and dress the wound, which would prevent contamination of the corticotomy wound by debridement. Then, thorough debridement was performed at the site of ulcers to remove all unhealthy, infected, and devitalized tissue. Different samples of tissues were collected and sent for bacterial culture and histopathologic examination.
Postoperatively, patients were treated with sensitive antibiotic and antithrombotic prophylaxis. Sensitive antibiotics were selected according to the result of bacterial culture. As shown in Fig. 3, after a latency period of 5 days, transverse distraction was performed at a rate of 0.25 mm every 6 h. Outward distraction was applied for 21 days, then inward distraction was applied for another 21 days to reposition the osteotomized cortex to its original position. The process of distraction was monitored by regular plain radiography. The distraction frame was usually removed 12 weeks after total distraction when bone healing was obtained. In patients with severe deformity, the process of gradual correction was simultaneously conducted with the process of transverse distraction. In other words, the two processes were independently performed and did not disrupt each other. The corrective frame was removed when rough correction was achieved. Patients were discharged 7 days after surgery when they learned to manage the Ilizarov frame. Mechanical unloading was maintained at the site of ulcers. Routine wound care was performed in an outpatient clinic, and no more additional technique was applied.
Fig. 3.
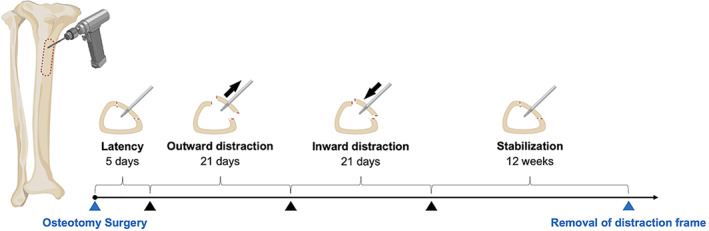
Schematic drawing of the management for tibial cortex transverse distraction (TCTD). Outward distraction was applied for 21 days, then inward distraction was applied for another 21 days to reposition the osteotomized cortex to its original position. The process of distraction was monitored by regular plain radiography. The distraction frame was usually removed 12 weeks after total distraction when bone healing was obtained.
Second Stage
After the ulcers healing with three consecutive normal results ESR and CRP, patients were readmitted for second‐stage corrective surgery. Weight‐bearing plain radiography, full‐length lower extremity radiographs, CT scans, and electromyogram (EMG) of lower limbs were performed before operation. An individualized open surgery was performed to correct the corresponding deformities(Fig. 2J–P). The procedures of each patient are shown in Table 2.
TABLE 2.
Outcomes of patients
| Case | Follow‐up (months) | Pre‐op deformity | Pre‐op AOFAS | First‐stage treatment | EFT (days) | Ulcer healing time*(weeks) | Ulcer healing < 3 months | Second‐stage treatment | Post‐op deformity | Post‐op AOFAS | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 27 | 9 | 34 | TCTD, WD | 142 | 2.0 | Yes | Midfoot osteotomy, proximal 1st metatarsal osteotomy, interphalangeal fusion | 0 | 70 | None |
| 2 | 27 | 7 | 26 | TCTD, WD | 49 | 2.5 | Yes | Proximal 1st metatarsal osteotomy, calcaneal osteotomy | 1 | 72 | Mild displacement of the osteotomized cortex |
| 3 | 25 | 6 | 65 | TCTD, WD | 139 | 2.0 | Yes | Midfoot osteotomy, limb lengthening | 0 | 97 | Pin‐tract infection |
| 4 | 24 | 4 | 54 | TCTD, WD | 136 | 1.5 | Yes | Midfoot osteotomy, 1st MTP fusion, 2nd, and 3rd MTP resection arthroplasty | 0 | 89 | None |
| 5 | 31 | 9 | 30 | TCTD, WD, ICT | 165 | 7.0 | Yes | Ankle fusion | 1 | 80 | None |
| 6 | 26 | 9 | 52 | TCTD, WD | 138 | 3.5 | Yes | Midfoot osteotomy, calcaneal osteotomy | 1 | 90 | None |
| 7 | 31 | 5 | 37 | TCTD, WD | 130 | 4.0 | Yes | Ankle fusion, limb lengthening | 0 | 78 | None |
| 8 | 25 | 3 | 58 | TCTD, WD | 141 | 1.5 | Yes | 1st‐5th metatarsal osteotomy | 0 | 87 | None |
| 9 | 31 | 7 | 14 | TCTD, WD | 136 | 1.5 | Yes | Subtalar arthrodesis, calcaneocuboid arthrodesis, talonavicular arthrodesis | 0 | 78 | None |
| 10 | 33 | 7 | 34 | TCTD, WD | 138 | 2.0 | Yes | Subtalar arthrodesis, calcaneocuboid arthrodesis, talonavicular arthrodesis | 1 | 84 | None |
| 11 | 29 | 9 | 53 | TCTD, WD, ICT | 173 | 2.0 | Yes | Midfoot osteotomy | 1 | 80 | None |
| 12 | 29 | 4 | 80 | TCTD, WD | 133 | 3.0 | Yes | Proximal 1st and 5th metatarsal osteotomy, calcaneal osteotomy | 1 | 90 | None |
| 13 | 26 | 8 | 21 | TCTD, WD | 141 | 2.0 | Yes | Subtalar arthrodesis, calcaneocuboid arthrodesis, talonavicular arthrodesis, Proximal 1st metatarsal osteotomy | 1 | 79 | None |
EFT, external fixation time; ICT, Ilizarov correction technique; MTP, metatarsophalangeal; Post‐op, postoperative; Pre‐op, preoperative; TCTD, tibial cortex transverse distraction; WD, wound debridement.
Patients self‐report time of ulcer healing.
Postoperatively, the foot and ankle were immobilized in a night splint. Patient‐specific exercises was performed under professional supervision. Full weight‐bearing was usually allowed when signs of bone healing present on the plain radiography. Routine follow‐up examinations were performed 1, 3, 6, 12 months postoperatively.
Assessments
General Information
The demographic and clinical data, including gender, age, side of lesion, etiology, duration of disease, size of ulcers, surgical procedures, healing time, external fixation time, and complications of these patients were recorded.
Ulcers Classification
Preoperatively, both Texas wound classification and NPUAP classification were applied to assess the chronic ulcers in this study due to the lack of dedicated evaluation of the ulcers combined with foot and ankle deformity. Texas wound classification system is one of the most common method for assessing diabetic foot lesion 20 . This classification mainly includes three sections: ulcers depth, wound infection and presence of ischemia. In this system, grading is done based on depth of the lesion, and stages are classified on presence of ischemia, wound bioburden or combination of both excluding neuropathy. In the previous study reported by Nie et al. 19 , the Texas wound classification system was also successfully used for evaluation the non‐diabetic ulcers. The National Pressure Ulcer Advisory Panel (NPUAP) classification is one of the most widely recognized systems for categorizing pressure ulcers 8 . This classification categorizes pressure ulcer from stage I to IV based on depth.
Modified Dimeglio Score
The Dimeglio scoring system is a classic evaluation for congenital club foot 21 . Lee et al. 22 modified the original classification of Dimegilo et al. 21 , and they used this modified scoring system for evaluation of foot deformity in adult patients. The modified Dimeglio score based on the measurement of five parameters: (i) equinus deformity in the sagittal plane; (ii) varus deformity in the frontal plane; (iii) derotation deformity of the calcaneopedal block in the horizontal plane; (iv) adduction deformity of the forefoot relative to the hindfoot in the horizontal plane; and (v) cavus deformity of the forefoot relative to the hindfoot in the sagittal plane. The total scores range from 10 to 0 points and is allocated to four grades: severe (7–10); moderate (4–6); mild (1–3); and postural (0).
American Orthopeadic Foot and Ankle Society Ankle‐Hindfoot Score
The American Orthopeadic Foot and Ankle Society (AOFAS) ankle‐hindfoot score 23 is a most commonly assessment for evaluating the functional status of patients with ankle or hindfoot disease. This evaluation system mainly includes nine aspects: pain, function, maximum walking distance, walking surfaces, gait abnormality, sagittal motion (plantarflexion plus dorsiflexion), hindfoot motion (inversion plus eversion), ankle‐hindfoot stability (anteroposterior, varus–valgus), and alignment. The AOFAS scores is categorized as excellent (90–100), good (80–89), fair (65–79), and poor (less than 65) in this study.
Statistical Analysis
SPSS statistical software package version 24.0 (IBM Inc., New York, USA) was used for statistical analysis. The Kolmogorov–Smirnov test was used to test the normality of data. Normally distributed continuous variables were presented as mean with standard deviation and non‐normally distributed data were presented as median with interquartile range (IQR). The Student's t‐test was used to compare the normally distributed data(preoperative and postoperative AOFAS ankle‐hindfoot scores). The Wilcoxon's signed‐rank test was conducted to compare the non‐normally distributed data (preoperative and postoperative modified Dimeglio scores of deformities). Statistical significance was set at P < 0.05.
Results
General Information
There were five males and eight females with a mean age of 33.8 ± 14.6 years (Table 1). Ten patients had a right‐side lesion, and three patients had a left‐side lesion. The etiology of deformity included seven cases of congenital neurological disease, one case of Charcot–Marie–Tooth disease, one case of trauma sequelae, and three cases of myelomeningocele. The mean duration of deformity was 26.3 ± 15.9 years. The types of deformity included equinocavovarus in 11 patients and equinovarus in two patients. The median duration of ulcers was 2.0 years (IQR, 1.0–3.5). The ulcers were located at forefoot in seven patients, at midfoot in five patients, and at hindfoot in one patient. The median size of ulcers was 3.6 cm2 (IQR, 0.9–7.9).
During the first‐stage surgery, the tibial transverse distraction technique and wound debridement were performed in all patients, and an additional Ilizarov correction technique was added in two patients (Fig. 4). Allulcers were healed in 3 months after first‐stage treatment. The median patient self‐report time of ulcer healing was 2.0 weeks (IQR, 1.8–3.3; Table 2). As the healing process occurred at home, the exact time of ulcers healing was not clear. The median external fixation time was 138.0 days (IQR, 134.5–141.5).
Fig. 4.
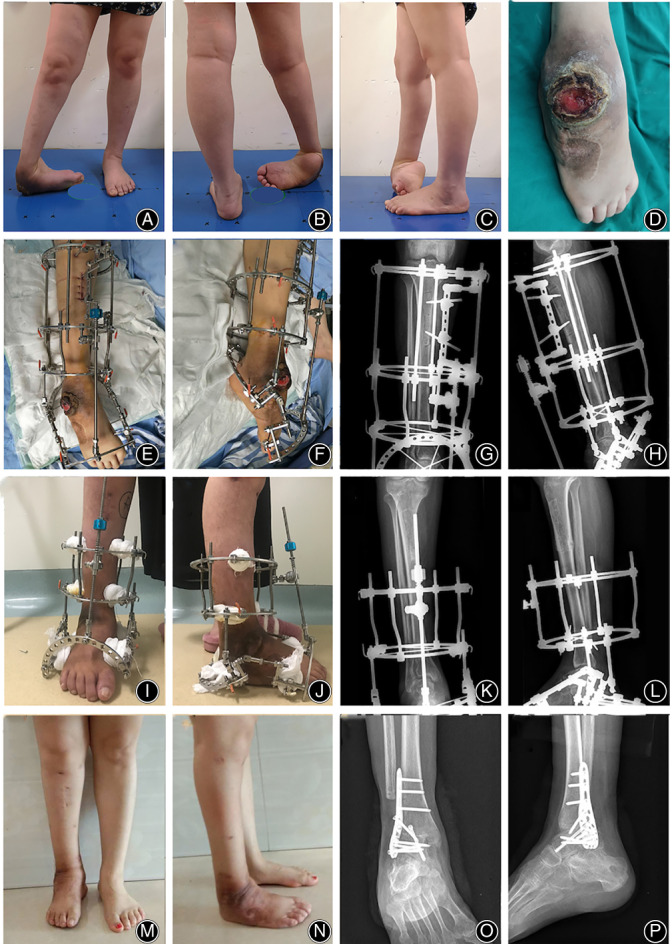
Clinical and radiographical photographs of a 25‐year‐old female patient who has a seriousequinocavovarus foot and a large ulcer. (A–D) Preoperative photographs show complex deformity of the right foot with a large concurrent ulcer. (E–H) An Ilizarov frame consisted by a part for transverse distraction and a part for deformity correction is installed. (I–L) After tibial cortex transverse distraction, the part for transverse distraction is removed and the part for deformity correction is maintained. (M–P) After ulcer healing and removal of external fixator, open correction and internal fixation is performed to obtain maximum correction.
During the second‐stage surgery, individualized OCIF was performed including midfoot osteotomy performed in five patients, metatarsal osteotomy performed in five patients, interphalangeal fusion in one, calcaneal osteotomy in three, limb lengthening in two, MTP fusion and resection arthroplasty in one, ankle fusion in two, and triple arthrodesis (subtalar arthrodesis, calcaneocuboid arthrodesis, talonavicular arthrodesis) in three (Table 2). After second‐stage surgical correction, the patients were followed‐up for a mean of 28.0 ± 2.9 months.
During the whole period of treatment and follow‐up, all complications were recorded. The mild displacement of the osteotomized cortex was observed in one patient who removed her external frame too early. One patient experienced pin‐tract infection without loosening, and she was successfully treated with pin‐tract care and oral antibiotics. Among all patients, no delayed union, nonunion, relapse of ulcers, or deformity were observed during the follow‐up period.
Ulcers Classification
Before the management, according to the Texas wound classification, one patient was classified as 2C, four patients were classified as 2D, three patients were classified as 3B, and five patients were classified as 3D. Based on the NPUAP classification, there were five patients with stage III and eight patients with stage IV ulcers (Table 1).
Modified Dimeglio Score
The modified Dimeglio scoring system was applied to assess the mean values of preoperative and postoperative deformities of these patients. Preoperatively, there were eight patients with severe deformity, four patients with moderate deformity, and one patient with mild deformity. At the final follow‐up, the modified Dimeglio score of deformity was decreased from 6.7 ± 2.1 to 1 (IQR, 0.0–1.0), and significant difference existed between them (Z = −3.190, P = 0.001; Fig. 5A). Postoperatively, seven patients were classified as mild deformity and six patients had a postural foot (Table 2).
Fig. 5.
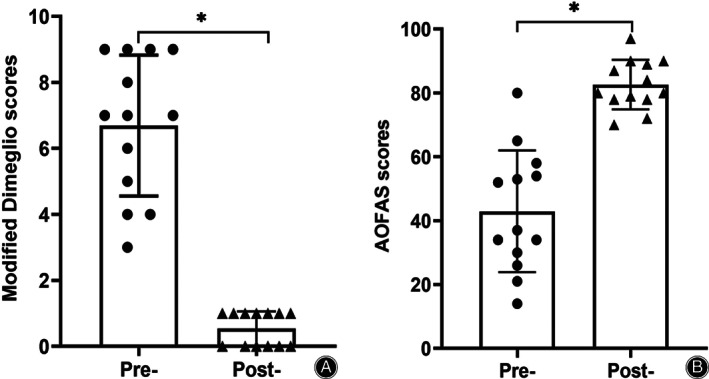
(A) Preoperative and postoperative modifiedDimeglio scores. (B) Preoperative and postoperative AOFAS scores. Pre‐: preoperative; Post‐: postoperative; * P < 0.05.
American Orthopedic Foot and Ankle Society Ankle‐Hindfoot Score
At the final follow‐up, the mean AOFAS score was improved from 42.9 ± 19.1 to 82.6 ± 7.7, and significant difference existed between them (t = 6.956, P < 0.001; Fig. 5B). According to the definition, the results of AOFAS ankle‐hindfoot score were defined as excellent in three patients, as good in five patients, and as fair in five patients (Table 2).
Discussion
Summary of the Major Results of the Study
The treatment objectives of foot and ankle deformities combined with chronic ulcers are infection eradication, ulcers healing, and obtaining a plantigrade and functional foot. In the present study, we adopted a two‐stage therapeutic strategy that includes the first‐stage treatment focusing on infection eradication and ulcer healing and the second‐stage treatment aiming to correct deformity and prevent relapse of ulcers or deformity. Our results supported that TCTD could be considered as an alternative method for the chronic ulcers accompanied by foot and ankle deformities, as complete healing of ulcers and excellent correction of deformity were achieved in all patients without severe complications at the final follow‐up. Our results also suggested that tibial cortex transverse distraction could be a potential therapy to treat the chronic ulcers of foot in patients with non‐diabetes and non‐ischemic diseases, such as pressure ulcers. Our finding is expected to provide some empirical support for expanding the indications of the TCTD.
Methods for Promoting Ulcers Healing
To enhance ulcer healing, various methods have been reported in previous studies, including surgical debridement, artificial skin substitute, flap reconstruction, negative pressure device, growth factors therapy, and even cell therapy 7 , 24 , 25 . However, these treatments might be ineffective or needed very long duration in some patients 7 , 26 . Thus, advanced techniques are necessary for better treatment of these recalcitrant ulcers. In this study, we employed TCTD as a primary method in the first‐stage treatment for promoting ulcer healing in patients who had failed to respond to their previous treatments. As we know, the Ilizarov technique is revolutionizing the therapy of deformity correction, bone reconstruction, infection control, and vascular regeneration. Originated from the principle of Ilizarov, TCTD is a novel technique for treatment of foot ulcers 16 , 27 . In a recent study, Chen and colleagues successfully employed optimized proximal TCTD to treat severe and recalcitrant diabetic foot ulcers in 136 patients and achieved ulcer healing in 96% of the patients 16 . The effective role of TCTD has been also demonstrated in recalcitrant non‐diabetic leg ulcers 19 . The potential mechanisms of TCTD are considered as follows, inducing neovascularization and consequently increasing blood perfusion, improving tissue healing, promoting anti‐infection and so on 19 . Based on the outstanding work in these previous studies, we proposed that TCTD could also promote the complete healing of chronic ulcers in the patients with foot and ankle deformity with ulcers.
TCTD Followed by OCIF for Foot and Ankle Deformities with Concurrent Ulcers
The choice of TCTD was determined by the following reasons. First, the pathological process of pressure ulcers is very complicated. For pressure ulcers, the local ischemia results from prolonged pressure, and when the pressure is relieved, the ischemia–reperfusion injury can occur 6 . Both ischemia and reperfusion could cause cell damage, increased inflammation, and impaired microcirculation, and consequently cause ulcers development 6 . And bacterial infection of the wound makes wound healing to be further delayed. These make the treatment more complicated. Appropriate offloading of the ulcers is certainly needed but may be insufficient for ulcer healing 6 . This is also the reason why conventional treatments are ineffective or need prolonged management for recalcitrant ulcers in some patients. As highlighted in the inclusion criteria, all the patients in this study had not responded to previous treatments (including wound care, off‐loading alone, debridement only, skin grafting and flap transplantation) for a minimum of 3 months and they were unwilling to undergo a longer treatment. Advanced techniques may be required to improve microcirculation, control infection, and promote wound healing. Second, despite that some pressure ulcers may heal themselves when avoiding abnormal pressure by long‐term off‐loading, the ulcers in non‐weight‐bearing areas (non‐pressure ulcers), as shown in Fig. 1, cannot. Specifically, in patients with foot and ankle deformity combined with concurrent ulcers resulted from a trauma, the ulcers were not caused by pressure, and traditional managements including off‐loading, wound care, and even multiple debridements might fail due to recalcitrant infections and insufficient blood supply. Therefore, in addition to the clearance of infection, it is also necessary to stimulate and increase neovascularization. Third, we must admit that ulcer healing and improving blood supply could be simultaneously obtained by an Ilizarov corrective frame, but the foot and ankle deformity may not always be serious and thus some patients do not need the prolonged gradual correction.
When deformity correction was completed but ulcers were unhealed in some patients with mild or moderate deformities, the Ilizarov corrective frame could only provide the role of a non‐weight‐bearing device. The distraction angiogenesis effects or the law of stress‐tension of the Ilizarov technique is unable to be fully functional in these cases. In contrast, the TCTD may play a more effective and sustained role in promoting ulcer healing at this time. Thus, we cautiously believe that TCTD in the first‐stage treatment is likely to make it possible to maximize the treatment efficacy of recalcitrant ulcers and minimize the risk of infection and/or relapse for patients with mild or moderate deformities and serious concurrent ulcers. When the ulcers healed, open operation with internal fixation as the second‐stage treatment could correct various deformities as optimal as possible and provide the patients with relief during the treatment period without need of long‐term external fixation. Conversely, for serious deformities combined with ulcers, the Ilizarov corrective technique could provide good deformity correction without shortening the foot and simultaneously promoting ulcer healing. Further studies are needed to compare TCTD and Ithe lizarov corrective technique.
Compare with the results of Kliushin et al. (mean, 179.9 days; range, 128–413 days), the duration of external fixation (median, 138.0 days; IQR, 134.5–141.5) in the present study was significantly shorter. Regrettably, in this study, we did not apply the improved technique as reported by Chen et al. 16 , which minimized the size of corticotomy window to 1.5 cm × 5.0 cm and shortened the time of distraction and fixation to 60 days 16 . Further, Li et al. 28 recently reported a more optimal surgical method and management of TCTD, including a same corticotomy of 1.5 × 5.0 cm and the shorter external fixation of 42 days, which shows comparable effectiveness and greater benefits. Although this more optimal management was not used in our study, it is not difficult to see that TCTD followed by OCIF may be very suitable for the treatment of foot and ankle deformities with concurrent ulcers. If the minimally invasive tibial cortex transverse transport described by Li et al. 28 is applied as the first‐stage treatment, OCIF could be performed immediately after the removal of fixator (approximately 6 weeks if the ulcers healed) without waiting for the union of tibial osteotomy site, since the patients will be instructed to remain non‐weight‐bearing after OCIF. This hypothetical management based on our findings may, theoretically, further reduce the external fixation time and the whole treatment duration. However, this hypothesis cannot be totally confirmed by this study due to the rapid development and improvement of TCTD.
Limitations of the Study
Our study is not without its limitations. First, as a retrospective study with a relatively small number of patients, the potential selection bias and confounding bias was inevitable. Second, as mentioned above, due to the lack of a control group, we could not compare our two‐stage management with the single‐stage management applied by Kliushin et al. 4 . As the problem of infected ulcers could be simultaneously solved during the gradual correction by the Ilizarov method, further work is needed to investigate whether TCTD has more advantages in promoting ulcer healing in patients with recalcitrant ulcers combined with foot and ankle deformities. Third, the surgical trauma caused by tibial corticotomy, and the tedious process of transverse distraction cannot be neglected. Fourth, due to the lack of appropriate wound classification for assessing the ulcers combined with foot and ankle deformity resulting from non‐diabetic and non‐ischemic diseases, we applied the Texas wound classification system and the pressure ulcers classification in this study 8 , 20 . More suitable evaluation system should be used in future studies. Fifth, we did not record the exact time of ulcers healing, as it occurred at home. Only the patient self‐report time of ulcers healing was recorded. Moreover, considering the medical cost for the patients, we also did not perform a CT angiography image or CDS after distraction to assess the change of peripheral blood vessels. However, the results of previous studies have established a role for tibial cortex transverse distraction technique in improving blood flow of lower limb 16 , 17 , 18 . The angiogenesis induced by TCTD was also confirmed in animal experiments 29 . Therefore, we believed that the results of our study could also confirm the effectiveness of TCTD as an alternative method for the treatment of chronic ulcers resulted from foot and ankle deformities.
Conclusions
In conclusion, our results demonstrated that the two‐stage management, including the first‐stage treatment based on TCTD and the second‐stage treatment of OCIF, could be considered as an alternative therapeutic strategy for foot and ankle deformities combined with chronic ulcers. However, prospective controlled studies with large sample sizes are needed to provide further evidence.
Consent for Publication
Each author confirms that this manuscript has not been published elsewhere and is not under consideration by another journal. All authors have approved the manuscript and agree with submission to Orthopaedic Surgery.
Ethics Approval
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Consent to Participate
All patients included in this study agree to participate in this study.
Acknowledgments
We thank Longmei Zhao PhD, Xiuzhen Zhang PhD and Yuting Song MD from West China Hospital of Sichuan University, for the drawing and their support during this research.
Disclosure: The authors declare that they have no conflict of interest. Ethical approval for all procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
References
- 1. Xu C, Wei J, Yan YB, et al. Pedobarographic analysis following Ponseti treatment for unilateral neglected congenital clubfoot. Sci Rep, 2018, 8: 6270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barreto JG, Salgado CG. Clinic‐epidemiological evaluation of ulcers in patients with leprosy sequelae and the effect of low level laser therapy on wound healing: a randomized clinical trial. BMC Infect Dis, 2010, 10: 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Capobianco CM, Ramanujam CL, Zgonis T. Charcot foot reconstruction with combined internal and external fixation: case report. J Orthop Surg Res, 2010, 5: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kliushin NM, Sudnitsyn AS, Subramanyam KN, George J. Management of neurologic deformity of the ankle and foot with concurrent osteomyelitis with the Ilizarov method. Foot Ankle Int, 2018, 39: 226–235. [DOI] [PubMed] [Google Scholar]
- 5. Urso B, Ghias M, John A, Khachemoune A. Neuropathic ulcers: a focused review. Int J Dermatol, 2020. 10.1111/ijd.15362 [DOI] [PubMed] [Google Scholar]
- 6. Mustoe T. Understanding chronic wounds: a unifying hypothesis on their pathogenesis and implications for therapy. Am J Surg, 2004, 187: 65S–70S. [DOI] [PubMed] [Google Scholar]
- 7. Xiao S, Liu Z, Yao Y, Wei ZR, Wang D, Deng C. Diabetic human adipose‐derived stem cells accelerate pressure ulcer healing by inducing angiogenesis and neurogenesis. Stem Cells Dev, 2019, 28: 319–328. [DOI] [PubMed] [Google Scholar]
- 8. Jaul E. Assessment and management of pressure ulcers in the elderly: current strategies. Drugs Aging, 2010, 27: 311–325. [DOI] [PubMed] [Google Scholar]
- 9. Morton LM, Phillips TJ. Wound healing and treating wounds: differential diagnosis and evaluation of chronic wounds. J Am Acad Dermatol, 2016, 74: 589–605 quiz 605‐606. [DOI] [PubMed] [Google Scholar]
- 10. Barnes LA, Marshall CD, Leavitt T, et al. Mechanical forces in cutaneous wound healing: emerging therapies to minimize scar formation. Adv Wound Care (New Rochelle), 2018, 7: 47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Saif AB, Jabbar S, Akhtar MS, Mushtaq A, Tariq M. Effects of topical vancomycin dressing on methicillin‐resistant Staphylococcus aureus (MRSA) positive diabetic foot ulcers. Pak J Med Sci, 2019, 35: 1099–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bus SA, van Deursen RW, Armstrong DG, Lewis JE, Caravaggi CF, Cavanagh PR. Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: a systematic review. Diabetes Metab Res Rev, 2016, 32: 99–118. [DOI] [PubMed] [Google Scholar]
- 13. Crews RT, Candela J. Decreasing an offloading device's size and offsetting its imposed limb‐length discrepancy lead to improved comfort and gait. Diabetes Care, 2018, 41: 1400–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ilizarov GA. The tension‐stress effect on the genesis and growth of tissues. Part I. the influence of stability of fixation and soft‐tissue preservation. Clin Orthop Relat Res, 1989, 238: 249–281. [PubMed] [Google Scholar]
- 15. Ilizarov GA. The tension‐stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res, 1989, 239: 263–285. [PubMed] [Google Scholar]
- 16. Chen Y, Kuang X, Zhou J, et al. Proximal Tibial cortex transverse distraction facilitating healing and limb salvage in severe and recalcitrant diabetic foot ulcers. Clin Orthop Relat Res, 2020, 478: 836–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zuo Q, Gao F, Song H, Zhou J. Application of Ilizarov transverse tibial bone transport and microcirculation reconstruction in the treatment of chronic ischemic diseases in lower limbs. Exp Ther Med, 2018, 16: 1355–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kulkarni S, Kulkarni G, Shyam AK, Kulkarni M, Kulkarni R, Kulkarni V. Management of thromboangiitis obliterans using distraction osteogenesis: a retrospective study. Indian J Orthop, 2011, 45: 459–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nie X, Kuang X, Liu G, et al. Tibial cortex transverse transport facilitating healing in patients with recalcitrant non‐diabetic leg ulcers. J Orthop Translat, 2021, 27: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care, 1998, 21: 855–859. [DOI] [PubMed] [Google Scholar]
- 21. Diméglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B, 1995, 4: 129–136. [DOI] [PubMed] [Google Scholar]
- 22. Lee DY, Choi IH, Yoo WJ, Lee SJ, Cho TJ. Application of the Ilizarov technique to the correction of neurologic equinocavovarus foot deformity. Clin Orthop Relat Res, 2011, 469: 860–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle‐hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int, 1994, 15: 349–353. [DOI] [PubMed] [Google Scholar]
- 24. Cushing CA, Phillips LG. Evidence‐based medicine: pressure sores. Plast Reconstr Surg, 2013, 132: 1720–1732. [DOI] [PubMed] [Google Scholar]
- 25. Clemens MW, Broyles JM, Le PN, Attinger CE. Innovation and management of diabetic foot wounds. Surg Technol Int, 2010, 20: 61–71. [PubMed] [Google Scholar]
- 26. Cavanagh PR, Lipsky BA, Bradbury AW, Botek G. Treatment for diabetic foot ulcers. Lancet, 2005, 366: 1725–1735. [DOI] [PubMed] [Google Scholar]
- 27. Baumhauer JF. CORR insights®: proximal Tibial cortex transverse distraction facilitating healing and limb salvage in severe and recalcitrant diabetic foot ulcers. Clin Orthop Relat Res, 2020, 478: 852–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen L, Zheng J, Li G, et al. Pathogenesis and clinical management of obesity‐related knee osteoarthritis: impact of mechanical loading. J Orthop Translat, 2020, 24: 66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Matsuyama J, Ohnishi I, Kageyama T, Oshida H, Suwabe T, Nakamura K. Osteogenesis and angiogenesis in regenerating bone during transverse distraction: quantitative evaluation using a canine model. Clin Orthop Relat Res, 2005, 433: 243–250. [DOI] [PubMed] [Google Scholar]


