Abstract
Objective
To compare the effects of arthroscopic debridement and repair in treating Ellman grade II bursal‐side partial‐thickness rotator cuff tears.
Methods
This is a single‐center, prospective, randomized controlled trial. From September 2017 to April 2019, 78 patients underwent arthroscopic debridement (35 patients) or repair (43 patients) due to Ellman grade II bursal‐side partial‐thickness rotator cuff tears. Twenty‐six men and 52 women were included in the study, with an average age of 56.31 years (range, 42 to 74 years). After the acromioplasty was formed, the debridement group only performed stump refreshing and surrounding soft tissue cleaning, while the repair group converted the partial tears into full‐thickness tears and then sutured them by single row or suture bridge technique. The visual analogue scale (VAS), Constant‐Murley shoulder (CMS), American Shoulder and Elbow Surgeons (ASES), and University of California, Los Angeles (UCLA) scores were used to evaluate clinical results preoperatively and at 6, 12, and 18 months postoperatively. Magnetic resonance imaging was used to assess the integrity of the rotator cuff, muscle atrophy, and fat infiltration.
Results
A total of 85 patients met the inclusion criteria and were randomly divided into the debridement group (41 patients) and the repair group (43 patients). During the 18‐month follow‐up period, a total of seven patients were lost to follow‐up. The functional scores of both groups were significantly improved: the VAS score decreased 5.06 and 4.63 in the debridement group (5.77 preoperative to 0.71 postoperative) and the repair group (5.49 to 0.86) (P < 0.05). Moreover, the CMS, ASES, UCLA scores increased 51.63, 58.24, 20.57 in debridement group (39.46 to 91.09, 34.14 to 92.38, 13.29 to 33.86), and increased 48.14, 60.53, 20.93 in repair group (43.63 to 91.77, 33.10 to 93.63, 12.58 to 33.51) (P < 0.05). No significant differences were found in functional scores between the two groups at 6, 12, and 18 months postoperatively (P > 0.05). The magnetic resonance imaging showed no re‐tears, and no difference was observed in the degree of muscle atrophy and fat infiltration between the two groups (P > 0.05). Except for four cases of shoulder stiffness, no other obvious surgery‐related complications were found.
Conclusion
For Ellman grade II bursal‐side partial‐thickness rotator cuff tears, both the debridement and repair groups achieved good results during 18‐month follow‐ups, with no difference between the two groups.
Keywords: Arthroscopic debridement, Arthroscopic repair, Bursal‐side tear, Partial‐thickness rotator cuff tear
For Ellman grade II bursal‐side partial‐thickness rotator cuff tears, both the arthroscopic debridement and the arthroscopic repair achieved good results during 18 months follow‐ups, and there was no difference between the two groups.
Introduction
Rotator cuff tear (RCT) is a common cause of shoulder pain, and its treatment options are based on the symptoms and types of tears. According to the injury site, RCTs can be classified as bursal‐side, articular‐side, or intratendinous. Ellman 1 classified the RCTs into three levels based on the percentage of tear thickness. Grade I: tear thickness <25%; grade II: tear thickness 25%–50%; grade III: tear thickness >50%. For the best treatment of RCTs, the patients' age, symptoms, dysfunction, tear size, tear position, cause, health status, etc. should be considered. Whether it is the bursal‐side or articular‐side, the surgical treatment is mainly evaluated according to the depth of the tear 2 . Most studies have shown that partial RCTs show very low self‐healing ability during natural progression. Yang et al. 3 conducted a biomechanical study and found that when the RCT thickness >50%, the stress on the remaining tendons would be significantly increased, and the possibility of tendon tearing on the cross‐section would be increased. They supported arthroscopic debridement when the tear thickness was less than 50% and arthroscopic repair when the tear was more than 50%. Arthroscopic repairs can achieve good therapeutic effects for patients with tear thickness greater than 50% 4 , 5 . However, treatment options are still controversial for patients with tear thickness less than 50%, especially those with tear thickness of 25%–50% (Ellman grade II) who have not responded to conservative treatment for more than 3 months 6 , 7 , 8 , 9 , 10 , 11 .
Strauss et al. 12 suggested that arthroscopic debridement could be effective for RCTs with tear thickness <50%. Park et al. 13 performed arthroscopic debridement on patients with tear thickness less than 50%. After a follow‐up of 2 years, 92% of the patients with bursal‐side tears reported that there was no pain in the shoulder joint either at rest or in motion, and the shoulder function was recovered. Other studies recommended that all RCTs with a tear thickness >25% could be treated with arthroscopic repair 14 , 15 . Arthroscopic repair may also be performed in some nonessential patients with the continuous improvement in surgical techniques and surgeons' proficiency. Further studies were needed to determine the treatment of Ellman grade II RCTs.
The main cause of RCTs is tendon degeneration, but some scholars also believe that bursal‐side partial‐thickness RCTs (BPTRCTs) are caused by subacromial impingeme 16 , 17 . For Ellman grade II BPTRCTs, arthroscopic debridement with acromioplasty may be good enough to achieve clinical satisfaction. In a previous study 18 , the therapeutic effects of arthroscopic debridement and repair for Ellman grade II BPTRCTs were retrospectively compared, concluding that arthroscopic debridement was equivalent to arthroscopic repair at the 2‐year follow‐up. The effect of arthroscopic debridement was even better than that of arthroscopic repair 6 months after the surgery. However, for the debridement group, the previous retrospective study inevitably excluded a subset of patients whose joint debridement surgery failed and who then underwent repair, so that the efficacy might be overestimated. A prospective study was necessary to minimize bias.
Therefore, in this study, we followed up patients who underwent arthroscopic debridement or repair for RCTs. The purpose of this prospective, randomized controlled trial was to: (i) evaluate the clinical and radiographic results of arthroscopic debridement and repair in the early and middle stages; (ii) evaluate the incidence of rotator cuff retears and other complications in two operations; and (iii) provide the basis of treatment choice for surgeons. It was hypothesized that no differences existed in prognosis between arthroscopic debridement and repair.
Methods
Participants
The study included eligible patients with Ellman grade II BPTRCTs. The inclusion criteria were as follows: (i) Ellman grade II BPTRCTs confirmed by preoperative magnetic resonance imaging (MRI) and intraoperative arthroscopic exploration; (ii) failure of conservative treatment for more than 3 months; (iii) patients that agreed to receive arthroscopic debridement or repair; and (iv) complete follow‐up data. The exclusion criteria were as follows: (i) previous surgery of the shoulder; (ii) articular‐side or intratendinous RCTs; (iii) combined articular‐side partial‐thickness rotator cuff tears (APTRCTs) and BPTRCTs, or full‐thickness RCTs; (iv) accompanying shoulder lesions that needed to be addressed, such as biceps tendon disorders and labral tears; (v) presence of other diseases that affected shoulder function; and (vi) contraindication to arthroscopic surgery or anesthesia. Before the study, written informed consent was obtained from all participants.
Study Design and Setting
A single‐center, prospective, double‐blinded, randomized controlled trial was conducted to compare arthroscopic debridement (debridement group) and arthroscopic repair (repair group) for Ellman grade II BPTRCTs. Patients were recruited from September 2017 to April 2019. The study was approved by the Medical Ethics Committee of Affiliated Hospital of Qingdao University (QYFYWZLL26071) and was registered at clinicaltrials.gov (NCT04710966). It was also conducted and reported following the Consolidated Standards of Reporting Trials statement.
Sample Size
The sample size calculation was based on data from previous studies 10 , 19 , where the difference in the Constant‐Murley Shoulder (CMS) score between patients with arthroscopic repair and arthroscopic debridement was 8.81 points (93.90 vs 85.09) with standard deviations of 5.4 and 21. Accepting an α risk of 0.05 and a β risk of 0.2 in a bilateral contrast, the minimum sample size required for each group was 35. To compensate for an estimated 15% loss to follow‐up, at least 82 patients were to be included.
Randomization and Blinding
Before initiating the trial, an investigator who was not involved in the study generated a computer‐generated randomization list (block length 10, ratio 1:1). The investigator arranged the random numbers of each block in sequence and ascending order, and then marked the first five random numbers as the debridement group and the last five as the repair group. Thus, for every block of 10 participants, five would be allocated to each arm of the trial. Allocation concealment was achieved using opaque, sealed, sequentially numbered envelopes containing details of group assignment. The baseline data was recorded by the recruiter who was not involved in surgical operation and postoperative evaluation, and then the eligible participants received an envelope in order. Arthroscopic debridement or arthroscopic repair was performed by the same‐group senior orthopedic surgeons according to the assignment information in the envelope. Only the outcome assessors and data analysts remained blinded throughout the study period.
Surgical Procedures
Anesthesia and Position
Surgeries were performed by the same team of sports medicine surgeons under general anesthesia. The patients were placed in a lateral decubitus position, and a shoulder retractor (Spider 2 traction system; Smith & Nephew, Andover, MA, USA) was used to maintain arm flexion at 20° and abduction at 30°. Surgeries were performed by the same team of sports medicine surgeons under general anesthesia. The patients were placed in a lateral decubitus position, and a shoulder retractor was used to maintain arm flexion at 20° and abduction at 30°.
Approach and Exposure
The posterior portal (2 cm below and 1–2 cm medial to the posterolateral corner of acromion) was established routinely, and the anterolateral and anterior portals were established successively via the outside‐in technique.
Arthroscopic Exploration
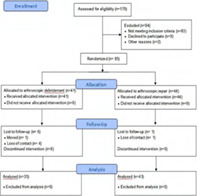
After inserting the arthroscope, a simple cleaning was performed after exploring the glenohumeral joint space. Next, the subacromial space was checked, and acromioplasty was performed according to the wear degree of the coracoacromial ligament on the side of the acromion (Fig. 1A). The surface of the rotator cuff was exposed after removing the subacromial hyperplastic tissue and subacromial bursa (Fig. 1B). A calibrated probe was used to measure the length and thickness of the tear after the degenerated tendons and soft tissues on the tear surface were completely removed, so as to confirm that the rotator cuff tear was classified as Ellman II (Fig. 1C). Patients with a tear thickness of less than 25% or greater than 50% were excluded from this study.
Fig. 1.
Intraoperative images. (A) Acromioplasty. (B) Clean inflammatory synovial tissues. (C) Probe the rotator cuff and evaluate the tear. (D) Stump refreshing. (E) Implantation of anchor. (F) Suture the tendon.
Arthroscopic Debridement and Arthroscopic Repair
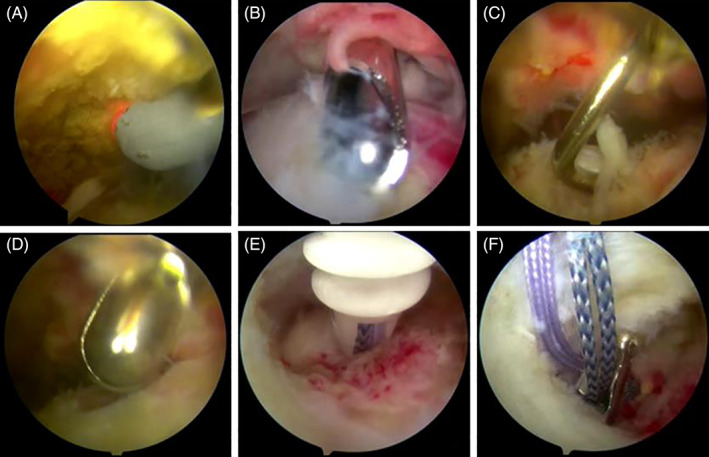
The patients were treated with arthroscopic debridement or repair based on the preoperative allocation. A schematic diagram of the operating procedure was shown in Fig. 2. For the debridement group, only stump refreshing and the surrounding soft tissue cleaning were performed (Figs 1D and 2B). For the repair group, partial tears were converted into full‐thickness tears and then sutured (Fig. 1E,F). The tendon was fixed with a single‐row suture (Fig. 2C) or the suture bridge technique (Fig. 2D). Before suturing, the tendon stump and the scar adhesion tissue were cleaned until fresh tissues appeared. The soft tissue and periosteum on the surface of the greater tuberosity and ground rough surface at the edges of the cartilage were removed to prepare the bone bed to promote healing of the reattached cuff.
Fig. 2.
Schematic diagram of operating procedure. (A) BPTRCT (red arrow) with subacromial impingement (red circle). (B) Arthroscopic debridement: acromioplasty, stump refreshing, and surrounding soft tissue cleaning. (C) Single‐row suture: a row of anchors was located on the outside of the footprint area. (D) Suture bridge technique: an internal row of anchors was embedded at the edge of the cartilage and a lateral row of anchors was placed outside the healing area of the greater tuberosity. For the lateral row, after knotting, the internal anchor sutures were fixed with a lateral row anchor using the suture bridge technique.
Postoperative Rehabilitation
The affected arm was fixed for 3 weeks with a 15° abductor sling and a neural‐rotator brace for patients undergoing arthroscopic debridement. Pendulum activity and passive range‐of‐motion (ROM) activity were initiated on day 1, and self‐help passive and active ROM exercises were encouraged after 3 weeks. The elastic band was used for active strength training 4–10 weeks after the surgery. Almost fully active ROM was allowed from 2.5 months postoperatively.
The affected arm was fixed with an abduction brace for 6 weeks in patients undergoing arthroscopic repair. Pendulum and passive ROM activities were carried out on the first day after the surgery, passive self‐help exercises were started after 6–12 weeks, and active ROM exercises were started 12 weeks postoperatively. The elastic band was used for active strength training 3–6 months after the surgery. Nearly fully active ROM was allowed from 6 months after the surgery.
Outcome Assessment
Background variables recorded at the time of enrollment included age, sex, Body Mass Index (BMI), arm dominance, duration of symptoms, smoking, alcohol consumption, hypertension, diabetes, and ROM of the affected shoulder. The visual analogue scale (VAS), Constant‐Murley Shoulder (CMS), American Shoulder and Elbow Surgeon (ASES), and University of California, Los Angeles (UCLA) scores were used to assess clinical outcomes before and at 6, 12, and 18 months after the surgery. Two independent physiotherapists who were not involved in patients' recruitment, surgery, or rehabilitation assessed the physical examination. Routine preoperative diagnostic examinations included shoulder X‐rays and MRI. The physician responsible for inclusion examined the rotator cuff on the image of BPTRCTs according to the inclusion criteria. Routine 3.0‐T MRI (Siemens Medical Solutions, Erlangen, Germany) was performed to assess rotator cuff integrity, muscle atrophy, and fatty degeneration at 18 months after the surgery. The evaluation was conducted by three sports medicine surgeons, and the consensus was determined by the majority.
VAS Score
The VAS score is the most commonly used pain quantification questionnaire. For pain intensity, the scale is usually based on no pain (0 points) and the worst pain (10 points). One to three points were considered as mild pain, 4–6 points as moderate pain, 7–10 points as severe pain. We evaluated the preoperative and postoperative VAS scores separately.
CMS Score
The CMS score is the most widely used shoulder function scoring system in Europe, which mainly includes pain (15 points), activities of daily life (20 points), ROM (40 points), and muscle strength (25 points). A total score of less than 70 generally requires medical treatment.
ASES Score
The ASES score is a standardized evaluation system of shoulder function. It emphasizes the patient's self‐subjective assessment, including pain (50%) and life function (50%). The total score is 100, and the higher the score, the better the shoulder function.
UCLA Score
The UCLA score is mainly evaluated postoperative shoulder pain (10 points), function (10 points), and ROM (10 points), plus patient satisfaction (five points). Scores of 34–35 are considered excellent, 28–33 are good, 21–27 are average, and 20 or less are poor. Excellent and good (≥28 points) are considered satisfactory; average and poor (≤27 points) are considered unsatisfactory.
Rotator Cuff Integrity
The integrity of the rotator cuff was assessed by MRI according to Sugaya grading criteria 20 , as follows: grades I and II, sufficient thickness with low or partial high intensity; grade III, insufficient thickness without discontinuity; and grades IV and V, presence of a minor or major discontinuity. Re‐tear was defined as grades IV and V.
Muscle Atrophy
A postoperative MRI was performed after 18 months to assess muscle atrophy. Muscular atrophy was assessed on oblique sagittal images using an occupation ratio measured by dividing the cross‐sectional area of supraspinatus muscle by that of the supraspinatus fossa on the oblique sagittal view, as described by Thomazeau et al. 21 When the ratio was between 1.00 and 0.60, the muscle was considered normal or with slight atrophy (grade I); values between 0.60 and 0.40 indicated moderate atrophy (grade II); and values less than 0.40 indicated severe atrophy (grade III).
Fatty Degeneration
Fatty degeneration in supraspinatus muscle was assessed by MRI using a grading system described by Goutallier et al. 22 , with stages 0–4 as follows: grade 0, no fat; grade 1, thin fatty streaks; grade 2, heavy fat infiltration, with muscle still pre‐dominating; grade 3, even distribution of fat and muscle; and grade 4, more fat than muscle.
Statistical Analysis
Statistical analysis was carried out using SPSS 25.0 software (IBM, Armonk, NY, USA). Quantitative data were expressed as the mean ± standard deviation, and categorical data were expressed as count and percentage. The normal distribution test (Kolmogorov–Smirnov and Shapiro–Wilk tests) was applied to determine whether all measurements conformed to a normal distribution. A chi‐square test was employed for categorical variables. Two‐independent‐sample t‐test or Mann–Whitney U tests were used to compare the quantitative data and functional scores between groups. The preoperative and postoperative functional scores were compared using paired‐two‐sample t‐test or Mann–Whitney U test. To identify the potential influencing factors on postoperative functional scores, both univariate and multivariate linear regression analysis were performed. First, the operation, age, gender, BMI, dominant side, symptom duration, smoking, alcohol consumption, and health status were evaluated by univariate analysis. Then all the variables above were incorporated into the multivariate analysis. The R × C chi‐square test was used to statistically analyze the distribution of rotator cuff integrity, muscle atrophy, and fat infiltration on MRI. P < 0.05 was considered statistically significant.
Results
Demographic Characteristics of Patients
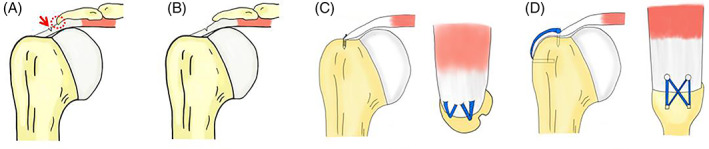
A total of 85 patients with an average age of 55.9 years (42–74 years), including 29 men and 56 women, met the inclusion criteria and were randomly divided into the debridement group (41 patients) and the repair group (43 patients). All surgical procedures were successful, and the patients were followed up for 18 months postoperatively. Seven patients were lost to follow‐up, two of whom were lost to follow‐up at 6 months after the surgery, and five were lost to follow‐up at 12 months after the surgery. Seventy‐eight patients were finally included in the analysis (35 in the debridement group and 43 in the repair group). The flow chart of the inclusion process is shown in Fig. 3. No significant differences were found in the preoperative demographic characteristics between the two groups shown in Table 1 (P > 0.050).
Fig. 3.
Flow chart of patient enrollment.
TABLE 1.
Patient characteristics at enrollment
| Variables | Debridement (n = 35) | Repair (n = 43) | P‐value |
|---|---|---|---|
| Age, mean (SD) | 55.77 (6.69) | 56.75 (8.79) | 0.143 |
| Gender, male, n (%) | 11 (31.4) | 15 (34.9) | 0.812 |
| BMI, mean (SD) | 24.08 (2.84) | 25.03 (2.99) | 0.165 |
| Dominant side, n (%) | 15 (42.9) | 21 (60.0) | 0.652 |
| Symptom duration, mean (SD) | 6.57 (4.79) | 5.37 (4.02) | 0.085 |
| Smoker, n (%) | 2 (5.7) | 5 (14.3) | 0.450 |
| Drinker, n (%) | 1 (2.9) | 2 (4.7) | 1.000 |
| Hypertension, n (%) | 6 (17.1) | 9 (20.9) | 0.777 |
| Diabetes mellitus, n (%) | 3 (8.6) | 8 (18.6) | 0.328 |
| Baseline assessment, mean (SD) | |||
| VAS score | 5.77 (1.49) | 5.49 (1.26) | 0.348 |
| CMS score | 39.46 (9.64) | 43.63 (9.86) | 0.068 |
| ASES score | 34.14 (5.91) | 33.10 (6.56) | 0.924 |
| UCLA score | 13.29 (2.34) | 12.58 (1.69) | 0.131 |
ASES, American Shoulder and Elbow Surgeons; BMI, Body Mass Index; CMS, Constant‐Murley Shoulder; SD, standard deviation; UCLA, University of California‐Los Angeles; VAS, Visual Analogue Scale.
No significant differences were found between groups.
General Results
The mean operation time was 79.91 ± 14.56 min in the debridement group and 113.58 ± 28.48 min in the repair group. One of the difficulties in the operation was to accurately measure the tear thickness, so in this study, we only estimated the percentage of the tear thickness for Ellman grade II. For the repair group, the repair methods were mainly single‐row suture (14 cases) and suture bridge technique (29 cases).
Functional Outcomes
VAS Score
The VAS score was remarkably decreased, from preoperative 5.77 ± 1.49 to postoperative 0.71 ± 0.74 points in the debridement group and from 5.49 ± 1.26 to 0.86 ± 0.82 in the repair group at the final follow‐up, indicating that the pain was significantly reduced postoperatively (P = 0.000; Table 2). But no statistically significant difference was observed in VAS scores between the two groups at 6, 12, and 18 months after the surgery (P = 0.228, P = 0.080, P = 0.463; Table 3).
TABLE 2.
Comparison of preoperative and postoperative functional scores
| Functional score | Debridement | Repair | ||||
|---|---|---|---|---|---|---|
| Pre‐operative | 18 months | P‐value | Pre‐operative | 18 months | P‐value | |
| VAS score | 5.77 ± 1.49 | 0.71 ± 0.74 | 0.000 * | 5.49 ± 1.26 | 0.86 ± 0.82 | 0.000 * |
| CMS score | 39.46 ± 9.64 | 91.09 ± 7.02 | 0.000 * | 43.63 ± 9.86 | 91.77 ± 6.28 | 0.000 * |
| ASES score | 34.14 ± 5.91 | 92.38 ± 4.96 | 0.000 * | 33.10 ± 6.56 | 93.63 ± 3.79 | 0.000 * |
| UCLA score | 13.29 ± 2.34 | 33.86 ± 1.57 | 0.000 * | 12.58 ± 1.69 | 33.51 ± 2.27 | 0.000 * |
ASES, American Shoulder and Elbow Surgeons; CMS, Constant‐Murley Shoulder; UCLA, University of California‐Los Angeles; VAS, Visual Analogue Scale.
Significant difference (P < 0.05).
TABLE 3.
Comparison of functional scores between the two groups postoperatively
| Functional score | 6 months | 12 months | 18 months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Debridement | Repair | P‐value | Debridement | Repair | P‐value | Debridement | Repair | P‐value | |
| VAS score | 2.43 ± 0.93 | 2.65 ± 0.83 | 0.228 | 1.57 ± 0.49 | 1.37 ± 0.48 | 0.080 | 0.71 ± 0.74 | 0.86 ± 0.82 | 0.463 |
| CMS score | 69.86 ± 11.16 | 67.47 ± 12.81 | 0.394 | 82.14 ± 6.48 | 81.88 ± 7.88 | 0.878 | 91.09 ± 7.02 | 91.77 ± 6.28 | 0.664 |
| ASES score | 75.05 ± 5.20 | 73.78 ± 6.01 | 0.333 | 86.81 ± 3.97 | 88.45 ± 3.7 | 0.066 | 92.38 ± 4.96 | 93.63 ± 3.79 | 0.301 |
| UCLA score | 27.69 ± 3.14 | 26.56 ± 3.77 | 0.123 | 31.86 ± 2.37 | 32.12 ± 3.29 | 0.385 | 33.86 ± 1.57 | 33.51 ± 2.27 | 0.580 |
ASES, American Shoulder and Elbow Surgeons; CMS, Constant‐Murley Shoulder; UCLA, University of California‐Los Angeles; VAS, Visual Analogue Scale.
No significant differences were found between groups.
CMS Score
Clinical assessment showed that the preoperative and post‐operative CMS scores were 39.46 ± 9.64 and 91.09 ± 7.02 in the debridement group, 43.63 ± 9.86 and 91.77 ± 6.28 in the repair group respectively, and significant difference existed between them (P = 0.000; Table 2). No statistically significant difference was observed in CMS scores between the two groups at 6, 12, and 18 months after the surgery (P = 0.394, P = 0.878, P = 0.664; Table 3).
ASES Score
Before the surgical intervention, the mean ASES score of the patients was 34.14 ± 5.91 (debridement group) and 33.10 ± 6.56 points (repair group). At the last follow‐up after the operation, the mean ASES score was significantly improved, to 92.38 ± 4.96 (debridement group) and 93.63 ± 3.79 (repair group) (P = 0.000; Table 2). No statistically significant difference was observed in ASES scores between the two groups at 6, 12, and 18 months after the surgery (P = 0.333, P = 0.066, P = 0.301; Table 3).
UCLA Score
In the debridement group and the repair group, the preoperative scores were 13.29 ± 2.34 and 12.58 ± 1.69, and the postoperative scores were 33.86 ± 1.57 and 33.51 ± 2.27 respectively, indicating that the UCLA score was significantly improved postoperatively (P = 0.050; Table 2). There was no significant difference in UCLA score between the two groups at 6, 12, and 18 months after the surgery (P = 0.123, P = 0.385, P = 0.580; Table 3).
Subgroup Analysis
To enable a deeper understanding of the data set, we calculated the differences in postoperative VAS,CMS,ASES,and UCLA scores between the two groups for age, gender, and BMI (Tables S1–S4). The VAS score of the patients over 60 years old was better than that of the repair group at 12 months after arthroscopic debridement (Mean = 1.71 vs 1.22; P = 0.021; Table S1), but the ASES score was worse than that of the repair group (Mean = 85.48 vs 89.30; P = 0.003; Table S3). The CMS score of female patients at 6 months after operation in the debridement group was better than that in the repair group (Mean = 48.27 vs 41.14; P = 0.024; Table S2). The VAS score of the patients with BMI > 26 in the debridement group was better than that in the repair group at 6 months after operation (Mean = 2.00 vs 2.61; P = 0.041; Table S1).
Independent Influence Factors
Further, we searched for influencing factors on postoperative functional scores. Therefore, univariate analysis and multivariate analysis were successively used to evaluate different factors (operation, gender, BMI, dominant side, symptom duration, smoking, alcohol consumption, and health status) on postoperative functional scores at 6, 12, and 18 months. The univariate analysis showed that age was associated with decreased CMS scores at 6 months postoperatively (β = −0.24, P = 0.035), symptom duration was associated with increased VAS scores at 12 months postoperatively (β = 0.269, P = 0.017), diabetes was associated with decreased VAS scores at 18 months postoperatively (β = −0.201, P = 0.078), and was associated with decreased CMS (β = −0.273, P = 0.016), ASES (β = −0.236, P = 0.037), and UCLA (β = −0.244, P = 0.032) scores at 12 months postoperatively. Further multivariate analysis results showed that symptom duration was related to the increased VAS score at 12 months after operation (β = 0.249, P = 0.038), and diabetes was related to the decreased CMS (β = −0.295, P = 0.022), ASES (β = −0.243, P = 0.049) and UCLA (β = −0.267, P = 0.032) scores at 12 months postoperatively. However, in the multivariate analysis, the influence of operation on postoperative functional scores did not change.
MRI Outcomes
The assessment results of rotator cuff integrity (according to the Sugaya grading system) after 18 months, shown by MRI, were as follows: in the debridement group, 28 patients were grades I and II and three were grade III; in the repair group, 34 rotator cuffs were grade I or II and eight were grade III; and no re‐tear of grades IV and V was found in both groups. The R × C chi‐square test showed no significant difference in cuff integrity between the debridement and repair groups (P > 0.050, Table 4). MRI findings of muscle atrophy and steatosis are also shown in Table 4. No difference was found in the distribution of muscle atrophy or steatosis in the two groups (P > 0.050). The MRI scan of three typical patients was shown in Figs 4, 5, 6.
TABLE 4.
MRI outcomes of debridement group and repair group 18 months postoperative
| Variables | Debridement (n = 35) | Repair (n = 43) | Total |
|---|---|---|---|
| Integrity | |||
| Grade I–II | 32 | 38 | 70 |
| Grade III | 3 | 5 | 8 |
| Grade IV–V | 0 | 0 | 0 |
| Atrophy | |||
| Grade I | 34 | 41 | 75 |
| Grade II | 1 | 2 | 3 |
| Grade III | 0 | 0 | 0 |
| Fatty infiltration | |||
| Grade 0 | 27 | 30 | 57 |
| Grade 1 | 8 | 13 | 21 |
| Grade 2–4 | 0 | 0 | 0 |
The R × C chi‐square test was used for statistical analysis. No statistically significant differences were found.
Fig. 4.

(A) Preoperative MRI scan of a 52‐year old man with Ellman grade II BPTRCTs, showing high intensity signal on the bursal side of the supraspinatus tendon (arrow). (B) MRI scan of 18 months after operation, showing partial high signal in the supraspinatus tendon, which was consistent with Sugaya grade II (arrow). (C) MRI shows slight atrophy (grade I) of the supraspinatus muscles without fat infiltration (grade 0) 18 months after operation.
Fig. 5.
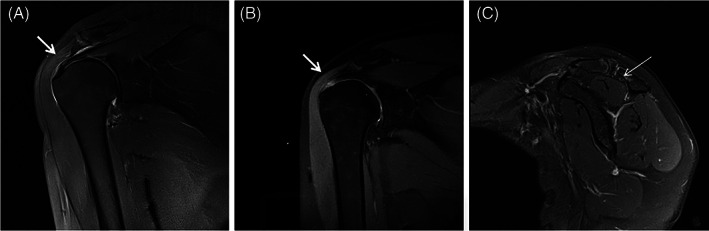
Images of a 47‐year‐old woman undergoing arthroscopic debridement before and 18 months after operation. (A) MRI before operation, showing high intensity signal on the bursal side of the supraspinatus tendon (arrow). (B) MRI at 18 months postoperatively, showing insufficient thickness without discontinuity in the supraspinatus tendon (Sugaya grade III). (C) MRI shows moderate atrophy (grade II) of the supraspinatus muscles without fat infiltration (grade 0) at 18‐month follow‐up.
Fig. 6.
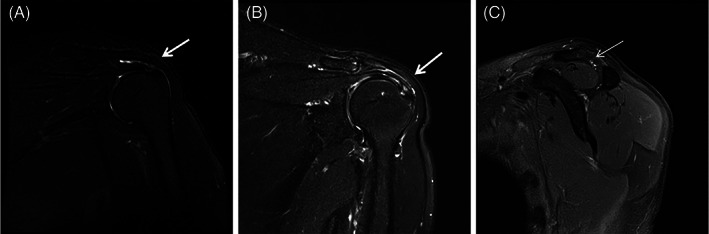
A case of Ellman grade II BPTRCTs undergoing arthroscopic repair. (A) A 67‐year‐old man complained of left shoulder pain with limited movement, and MRI showed a bursa‐side tear of supraspinatus tendon (arrow). (B) 18 months after arthroscopic reapir, the MRI shows the thickness of the supraspinatus tendon was insufficient, but without discontinuity (Sugaya grade III). (C) MRI shows slight atrophy (grade I) of the supraspinatus muscles with thin fatty streaks (grade 1) at 18‐month follow‐up.
Complications
No obvious surgery‐related complications were found in the two groups. One and three patients developed shoulder stiffness in the debridement and repair groups 6 months after the operation, respectively. The main manifestation was the limitation of abduction activity of the shoulder joint. These patients were treated with nonsteroidal anti‐inflammatory drugs and shoulder strengthening exercises as instructed. The symptoms gradually disappeared during follow‐up.
Discussion
Treatment Options for Ellman Grade II BPTRCTs
The arthroscopic repair can rebuild the anatomical structure by sutured tendons, and hence the shoulder joint can obtain a more stable structure. Numerous studies have reported impressive results of arthroscopic repair for tear thickness of less than 50% of PTRCTs 19 , 23 . Zafra et al. 24 compared two suture techniques for treating PTRCTs, both of which could relieve the patient's pain and improve the function. Fukushi et al. 23 found that arthroscopic repair significantly improved the prognosis of BPTRCTs and APTRCTs. However, arthroscopic repair also had some disadvantages, such as increased postoperative pain, longer immobilization time, higher risk of postoperative shoulder stiffness, and so forth. In this study, three patients (6.98%) in the repair group suffered from shoulder stiffness of different degrees, which was higher compared with one patient (2.86%) in the debridement group.
Other studies also confirmed the efficacy of arthroscopic debridement in treating partial tears 2 , 13 , 19 . The therapeutic mechanisms underlying arthroscopic debridement may be as follows: (i) removing subacromial hyperplastic tissue and inflammatory tissue, which relieved pain and reduced the pressure in the subacromial space, thus making sufficient space to accommodate the rotator cuff and repair tissue; (ii) cleaning up the stump without destroying the integrity of the rotator cuff, thus providing a structural condition conducive to tendon healing; and (iii) avoiding postoperative pain caused by suture anchor repairs and reducing postoperative immobilization time 18 , 25 .
Previously, the debridement and repair results for PTRCTs were directly compared only in a few studies, while prospective trials were conducted. Both methods achieved good therapeutic effects, at the final follow‐up in this study, similar to a previous retrospective study 18 . In addition, the functional score in the debridement group after 6 months was not significantly better compared with that in the repair group. It was possible that the randomization in this prospective study avoided the exclusion of some patients who underwent repair after the debridement surgery failed, thus reducing the result bias in the debridement group.
Clinical Evaluation
The main finding of the present study was that arthroscopic debridement achieved a considerable therapeutic effect for Ellman grade II BPTRCTs. The arthroscopic debridement removed the subacromial hyperplastic tissue and the inflammatory synovium, cleaned the stump of the tendon, and preserved the healthy tissue; no difference was observed in the prognosis compared with the arthroscopic repair at follow‐ups (3, 6, 12, and 18 months postoperatively). In this study, both groups underwent debridement, including acromioplasty. The results showed that the patient's pain was significantly relieved and the functional scores were significantly improved. Besides, the anatomical structure of the tendon was not reconstructed; however, the study found that the abduction function of the shoulder joint of the patients in the debridement group also improved.
The main causes of BPTRCTs include endogenous degeneration and exogenous causes such as acromion impingement 26 . Numerous studies suggested that bursal‐side tears were mainly caused by subacromial impingement 10 , 20 , 26 , 27 , 28 . In this study, arthroscopy revealed that almost all patients had subacromial impingement and coracoacromial ligament wear. Some studies showed that although acromioplasty could relieve the impingement, it could not prevent further degeneration of the rotator cuff 29 , 30 . Gartsman and O'connor 31 and Milano et al. 32 suggested that acromioplasty did not affect functional recovery after arthroscopic repair. Other studies emphasized the importance of acromioplasty and argued that acromioplasty could effectively expand the subacromial space and relieve shoulder pain 33 . Also, Bigliani et al. 34 considered that insufficient subacromial decompression might lead to the failure of rotator cuff repair. It was believed that the removal of the subacromial impingement was a problem that must be solved. Hence, a debridement including acromioplasty was performed in both groups. After debridement, the study determined whether to suture the rotator cuff. It showed that the results of the two treatments were equivalent at 6, 12, and 18 months after the surgery. Therefore, arthroscopic debridement might be good enough for Ellman grade II BPTRCTs.
Independent Influencing Factor Analysis and Subgroup Analysis of Functional Results
Univariate and multivariate analysis show that preoperative symptom duration and diabetes are related to the results of postoperative functional scores, but the two variables do not affect the outcome of functional scores based on operation methods. These prove that the result of our function scores is credible.
Our subgroup analysis of age, sex, and BMI suggests that arthroscopic debridement may have an advantage in female and overweight patients. In addition, although arthroscopic debridement in elderly patients had more advantages in pain relief, it was worse than arthroscopic repair in terms of functional recovery. However, the sample size of subgroups is relatively small, and further clinical trials are needed to verify these findings.
Radiological Results
During the final follow‐up, MRI was used to assess the integrity of the rotator cuff, as well as supraspinatus atrophy and fatty degeneration. Although some studies suggested that debridement might lead to a higher failure rate 14 , 23 , no patients progressed to a full‐thickness tear in the present study. Only a small number of patients had mild muscle atrophy and fatty degeneration. However, such good MRI results might deteriorate over time.
Limitations
The present study had only an 18‐month follow‐up, and therefore the short follow‐up time was one of the study limitations. Besides, study participants were limited to Ellman grade II BPTRCTs to make the study more comparable. However, it was not possible to summarize the treatment options for other types of PTRCTs (such as articular‐side tears, intra‐tendinous tears, etc.). Finally, when assessing the grade of PTRCTs, it was considered that the included tears were all grade II; however, the presence of a small portion of grade I or grade III could not be ruled out. Future multicenter design with a large cohort is needed for further investigation.
Conclusions
A total of 78 patients with Ellman grade II BPTRCTs randomly underwent arthroscopic debridement or repair, achieving a good prognosis after 18 months of treatment. Moreover, no statistically significant differences were found in functional scores and MRI results between the two groups at 6‐, 12‐, and 18‐month follow‐ups. In summary, the study suggested that repair surgery was unnecessary for Ellman grade II BPTRCTs because debridement alone could achieve clinically satisfactory results.
Authorship declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and all authors are in agreement with the manuscript.
Supporting information
Table S1 Subgroup analysis of VAS score for age, gender and BMI.
Table S2 Subgroup analysis of CMS score for age, gender and BMI.
Table S3 Subgroup analysis of ASES score for age, gender and BMI.
Table S4 Subgroup analysis of UCLA score for age, gender and BMI.
Table S5 Associations between preoperative variables and postoperative functional scores at 6, 12, and 18 weeks. (Uni‐variate analysis).
Table S6 Associations between preoperative variables and postoperative functional scores at 6, 12, and 18 weeks. (Multi‐variate analysis).
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 31872310).
Disclosure: The authors declare no conflict of interest.
References
- 1. Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res, 1990, 254: 64–74. [PubMed] [Google Scholar]
- 2. Liem D, Alci S, Dedy N, Steinbeck J, Marquardt B, Möllenhoff G. Clinical and structural results of partial supraspinatus tears treated by subacromial decompression without repair. Knee Surg Sports Traumatol Arthrosc, 2008, 16: 967–972. [DOI] [PubMed] [Google Scholar]
- 3. Yang S, Park HS, Flores S, et al. Biomechanical analysis of bursal‐sided partial thickness rotator cuff tears. J Shoulder Elbow Surg, 2009, 18: 379–385. [DOI] [PubMed] [Google Scholar]
- 4. Chung SW, Kim JY, Yoon JP, Lyu SH, Rhee SM, Oh SB. Arthroscopic repair of partial‐thickness and small full‐thickness rotator cuff tears: tendon quality as a prognostic factor for repair integrity. Am J Sports Med, 2015, 43: 588–596. [DOI] [PubMed] [Google Scholar]
- 5. Kwon OS, Kelly JI. Outcome analysis of arthroscopic treatment of partial thickness rotator cuff tears. Indian J Orthop, 2014, 48: 385–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jeong JY, Park KM, Sundar S, Yoo JC. Clinical and radiologic outcome of arthroscopic rotator cuff repair: single‐row versus transosseous equivalent repair. J Shoulder Elbow Surg, 2018, 27: 1021–1029. [DOI] [PubMed] [Google Scholar]
- 7. Ranalletta M, Rossi LA, Bertona AB, et al. Arthroscopic transtendon repair of partial‐thickness articular‐side rotator cuff tears. Art Ther, 2016, 32: 1523–1528. [DOI] [PubMed] [Google Scholar]
- 8. Shin SJ, Kook SH, Rao N, Seo MJ. Clinical outcomes of modified Mason–Allen single‐row repair for Bursal‐sided partial‐thickness rotator cuff tears: comparison with the double‐row suture‐bridge technique. Am J Sports Med, 2015, 43: 1976–1982. [DOI] [PubMed] [Google Scholar]
- 9. Xiao J, Cui GQ. Clinical and magnetic resonance imaging results of arthroscopic repair of intratendinous partial‐thickness rotator cuff tears. Chin Med J (Engl), 2015, 128: 1496–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Xiao J, Cui G. Clinical and structural results of arthroscopic repair of bursal‐side partial‐thickness rotator cuff tears. J Shoulder Elbow Surg, 2015, 24: e41–e46. [DOI] [PubMed] [Google Scholar]
- 11. Yoo JS, Heo K, Park SG, Ham HJ, Seo JB. The supraspinatus occupation ratios of both the ≥ 50% articular‐ and bursal‐side partial‐thickness rotator cuff tears were low and the infraspinatus occupation ratio of the ≥ 50% bursal‐side partial‐thickness rotator cuff tears was low. Knee Surg Sports Traumatol Arthrosc, 2019, 27: 3871–3880. [DOI] [PubMed] [Google Scholar]
- 12. Strauss EJ, Salata MJ, Kercher J, et al. Multimedia article. The arthroscopic management of partial‐thickness rotator cuff tears: a systematic review of the literature. Art Ther, 2011, 27: 568–580. [DOI] [PubMed] [Google Scholar]
- 13. Park JY, Yoo MJ, Kim MH. Comparison of surgical outcome between bursal and articular partial thickness rotator cuff tears. Orthopedics, 2003, 26: 387–390. [DOI] [PubMed] [Google Scholar]
- 14. Cordasco FA, Backer M, Craig EV, Klein D, Warren RF. The partial‐thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med, 2002, 30: 257–260. [DOI] [PubMed] [Google Scholar]
- 15. Wolff AB, Magit DP, Miller SR, Wyman J, Sethi PM. Arthroscopic fixation of bursal‐sided rotator cuff tears. Arthroscopy, 2006, 22: 1247.e1–1247.e4. [DOI] [PubMed] [Google Scholar]
- 16. Yamamoto N, Mineta M, Kawakami J, Sano H, Itoi E. Risk factors for tear progression in symptomatic rotator cuff tears: a prospective study of 174 shoulders. Am J Sports Med, 2017, 45: 2524–2531. [DOI] [PubMed] [Google Scholar]
- 17. Matthewson G, Beach CJ, Nelson AA, et al. Partial thickness rotator cuff tears: current concepts. Adv Orthop, 2015, 2015: 458786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhang Y, Zhai S, Qi C, et al. A comparative study of arthroscopic débridement versus repair for Ellman grade II bursal‐side partial‐thickness rotator cuff tears. J Shoulder Elbow Surg, 2020, 29: 2072–2079. [DOI] [PubMed] [Google Scholar]
- 19. Dwyer T, Razmjou H, Henry P, Misra S, Maman E, Holtby R. Short‐term outcomes of arthroscopic debridement and selected acromioplasty of Bursal‐ vs articular‐sided partial‐thickness rotator cuff tears of less than 50. Orthop J Sports Med, 2018, 6: 2325967118792001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full‐thickness rotator cuff repair: single‐row versus dual‐row fixation. Art Ther, 2005, 21: 1307–1316. [DOI] [PubMed] [Google Scholar]
- 21. Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand, 1996, 67: 264–268. [DOI] [PubMed] [Google Scholar]
- 22. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre‐ and postoperative evaluation by CT scan. Clin Orthop Relat Res, 1994, 304: 78–83. [PubMed] [Google Scholar]
- 23. Fukushi R, Horigome K, Yamashita T. Clinical outcomes following arthroscopic repair of articular vs. bursal partial‐thickness rotator cuff tears with follow‐up of 2 years or more. JSES Int, 2020, 4: 352–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zafra M, Uceda P, Muñoz‐Luna F, Muñoz‐López RC, Font P. Arthroscopic repair of partial‐thickness articular surface rotator cuff tears: single‐row transtendon technique versus double‐row suture bridge (transosseous equivalent) fixation: results from a prospective randomized study. Arch Orthop Trauma Surg, 2020, 140: 1065–1071. [DOI] [PubMed] [Google Scholar]
- 25. Beard DJ, Rees JL, Cook JA, et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo‐controlled, three‐group, randomised surgical trial. Lancet, 2018, 391: 329–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ogata S, Uhthoff HK. Acromial enthesopathy and rotator cuff tear. A radiologic and histologic postmortem investigation of the coracoacromial arch. Clin Orthop Relat Res, 1990, 254: 39–48. [PubMed] [Google Scholar]
- 27. Andarawis‐Puri N, Ricchetti ET, Soslowsky LJ. Rotator cuff tendon strain correlates with tear propagation. J Biomech, 2009, 42: 158–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Uchiyama Y, Hamada K, Khruekarnchana P, et al. Surgical treatment of confirmed intratendinous rotator cuff tears: retrospective analysis after an average of eight years of follow‐up. J Shoulder Elbow Surg, 2010, 19: 837–846. [DOI] [PubMed] [Google Scholar]
- 29. Bernstein J. Open acromioplasty does not prevent the progression of an impingement syndrome to a tear. J Bone Joint Surg Br, 1999, 81: 743. [PubMed] [Google Scholar]
- 30. Kartus J, Kartus C, Rostgård‐Christensen L, Sernert N, Read J, Perko M. Long‐term clinical and ultrasound evaluation after arthroscopic acromioplasty in patients with partial rotator cuff tears. Art Ther, 2006, 22: 44–49. [DOI] [PubMed] [Google Scholar]
- 31. Gartsman GM, O'connor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one‐year outcomes. J Shoulder Elbow Surg, 2004, 13: 424–426. [DOI] [PubMed] [Google Scholar]
- 32. Milano G, Grasso A, Salvatore M, Zarelli D, Deriu L, Fabbriciani C. Arthroscopic rotator cuff repair with and without subacromial decompression: a prospective randomized study. Art Ther, 2007, 23: 81–88. [DOI] [PubMed] [Google Scholar]
- 33. Packer NP, Calvert PT, Bayley JI, Kessel L. Operative treatment of chronic ruptures of the rotator cuff of the shoulder. J Bone Joint Surg Br, 1983, 65: 171–175. [DOI] [PubMed] [Google Scholar]
- 34. Bigliani LU, Cordasco FA, McIlveen SJ, Musso ES. Operative treatment of failed repairs of the rotator cuff. J Bone Joint Surg Am, 1992, 74: 1505–1515. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Subgroup analysis of VAS score for age, gender and BMI.
Table S2 Subgroup analysis of CMS score for age, gender and BMI.
Table S3 Subgroup analysis of ASES score for age, gender and BMI.
Table S4 Subgroup analysis of UCLA score for age, gender and BMI.
Table S5 Associations between preoperative variables and postoperative functional scores at 6, 12, and 18 weeks. (Uni‐variate analysis).
Table S6 Associations between preoperative variables and postoperative functional scores at 6, 12, and 18 weeks. (Multi‐variate analysis).


