Abstract
Background:
Multiple techniques for fixing a graft to the patella in medial patellofemoral ligament (MPFL) reconstruction have been described; however, no single technique has been shown to be superior to another.
Purpose/Hypothesis:
The purpose of this study was to compare the biomechanical performance of 2 different patellar fixation techniques: suture anchor (SA) and transosseous suture (TS) fixation. The hypothesis was that there would be no significant differences between the groups in ultimate failure load, stiffness, or elongation.
Study Design:
Controlled laboratory study.
Methods:
In this study, a new TS technique was biomechanically compared with the SA technique for MPFL reconstruction using 24 fresh-frozen mature porcine patellae and porcine flexor profundus tendons. The specimens were randomized into 2 groups undergoing MPFL reconstruction using either the SA technique or the TS technique (n = 12 per group). Fixation with TS was completed using 3 No. 2 UltraBraid sutures and three 2-mm transosseous tunnels. SA reconstruction was completed using 2 parallel 3.5-mm titanium SAs with 2 No. 2 UltraBraid sutures. We preconditioned each graft using a force between 5 and 20 N before cyclic loading. Then, the specimens were biomechanically tested (1000 cycles; 5-100 N; 1 Hz) and loaded under tension at 200 mm/min until failure. The ultimate failure load, stiffness, elongation, and failure mode were recorded for each specimen. The Shapiro-Wilk test and independent t tests were used to assess the data.
Results:
The TS technique resulted in a significantly higher mean failure load than did the SA technique (496.18 ± 93.15 vs 399.43 ± 105.35 N; P = .03). The TS technique resulted in less stiffness than did the SA technique (55.42 ± 7.92 vs 72.11 ± 10.64 N/mm; P < .01). There was no significant difference between the groups in elongation. None of the graft fixation/patellar complexes failed during cyclic testing in either group. During the load-to-failure test, the most common mode of failure in the SA group was an anchor being pulled out of the bone, whereas that in the TS group was rupture of the suture material.
Conclusion:
MPFL reconstruction with 3 TSs provided a higher load to failure than did the commonly used fixation method involving SAs.
Keywords: biomechanics, MPFL reconstruction, patellar instability, suture anchor, transosseous suture
Acute patellar dislocation typically occurs in young, active patients, and conservative treatment has usually been the first choice for the first instance of patellar dislocation. 11,12,16,18,22,23 However, a redislocation rate of >30% after conservative treatment has been reported. 17,20,24 –26 Surgical treatment is generally recommended for recurrent patellar dislocation. 17,18,40,42 Biomechanical studies have demonstrated that the medial patellofemoral ligament (MPFL) is the primary soft tissue that prevents lateral patellar displacement. 1,2,8,13,37 Recently, MPFL reconstruction has gained attention because it has yielded good results in clinical trials involving patients in whom nonoperative treatment for recurrent patellar instability has failed. §
Various techniques have been described in the literature for the fixation of a graft to the patella in MPFL reconstruction, with successful functional and clinical outcomes. 7,10,19,28,34,36,39 However, none of these techniques has been shown to be superior to the others. The commonly used MPFL reconstruction procedure on the patellar side involves bone tunnels, 7,15,22,28 interference screws, 10,15,27,29,34 or anchors for graft fixation to the patella. 15,28,29,38,39 The loss of patellar fixation is a particularly problematic cause of MPFL reconstruction failure in the clinic. 34 A devastating complication of patellar bone tunnel techniques is a patellar fracture, which is associated with transverse tunnels that completely pass through the patella. 4,7,21,31 Hence, the suture anchor (SA) technique, which has been reported by many other surgeons, can be used instead of the patellar bone tunnel technique to avoid patellar fractures; however, some concerns remain regarding the relatively low ultimate strength of fixation using the SA technique. 15,28,29,38
The transosseous suture (TS) technique for MPFL reconstruction was initially introduced for the repair of patellar tendon or quadriceps tendon ruptures as an implant-free technique, and Zhang et al 41 applied this technique for MPFL reconstruction. 42 The purpose of the present study was to compare the elongation, ultimate failure load, and stiffness of the TS fixation technique with those of the SA fixation technique. We hypothesized that graft fixation achieved using the TS technique would not differ significantly in biomechanical properties (elongation, ultimate failure load, and stiffness) from that achieved using the conventional SA technique.
Methods
Specimen Preparation
After receiving ethics committee approval, we conducted testing using 24 fresh-frozen mature porcine patellae and porcine flexor profundus tendons (90-kg healthy male pigs aged 12 months). The porcine patellae and porcine flexor tendons were obtained from the Department of Animal Science, China Medical University. The porcine patella has been reported to have a similar density to that of the young human patella and has been used as a model for biomechanical properties in previous studies. 9,15,29 Using a random-number generator, we divided the specimens into 2 groups of 12: the SA fixation group and the TS fixation group.
Before beginning the surgical technique, dual-energy x-ray absorptiometry scans were performed to ensure there were equal bone mineral densities between the 2 groups (TS group, 24.13 ± 0.96 kg/m2; SA group, 24.08 ± 1.09 kg/m2; P = .92). The tendon and bone specimens were stored at –20°C and thawed at room temperature for 12 hours before biomechanical testing. All specimens underwent 1 freeze-thaw cycle before experimental testing. The tendons were kept moist with a saline spray (every 5 minutes) during preparation and testing. For graft preparation, the tendons were adjusted to the same diameter (5 mm) and length (∼200 mm) using surgical scissors. The free ends of the grafts in both groups were clamped in a custom-made clamp (Figure 1). The custom-made clamp allowed for the tendon to achieve a strong fixation and reduced preparation time via screw fixation.
Figure 1.
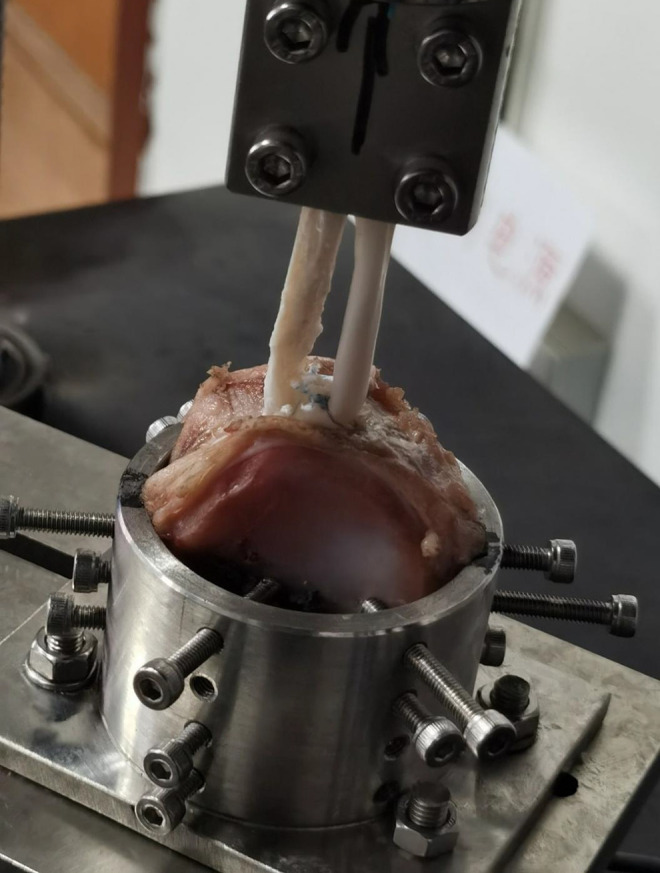
A specimen fixed in the testing machine. The patella was fixed to the base of the testing frame using several screws, while the free ends of the soft tissue graft were clamped in a custom-made clamp.
Transosseous Suture Group
The TS fixation method used for MPFL reconstruction has been described previously. 41 Similar to the technique used in the SA group, a bony trough was made in the medial border of the patella. A small eyelet-passing pin that was 2 mm in diameter was used to create 3 tunnels to allow the sutures to be passed through the patella. Three No. 2 UltraBraid sutures (Smith & Nephew) were then laterally passed through the 3 patellar tunnels using a small eyelet-passing pin. One suture was passed through the proximal and middle drill holes, 1 was passed through the middle and distal holes, and 1 was passed through the proximal and distal holes. There was a distance of 15 mm between the proximal and distal holes. First, the 2 sutures in the central tunnel were fixed, and then the sutures in both the upper patellar tunnel and the lower patellar tunnel were fixed. The graft was fixed at the medial side of the patella with these 3 No. 2 UltraBraid sutures using a surgeon’s knot followed by 5 manual knots. Figure 2A illustrates the TS method used for MPFL reconstruction.
Figure 2.
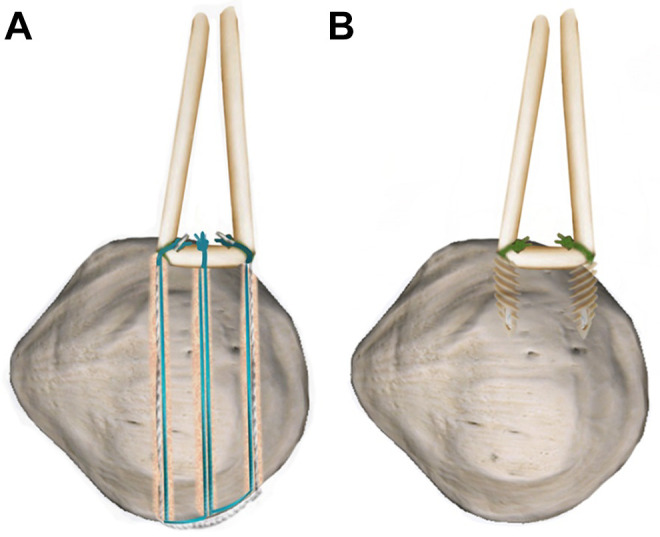
Computer drawing of the 2 patellar fixation techniques: (A) the transosseous suture technique and (B) the suture anchor technique.
Suture Anchor Group
The medial margin of each patella was exposed. A bony trough was made in the medial border of the patella using nucleus forceps to model the clinical scenario. We drilled two 3.5-mm titanium SAs (TwinFix; Smith & Nephew), each of which was loaded with 2 No. 2 preloaded UltraBraid sutures (Smith & Nephew). These SAs were then seated at the proximal and distal ends of the sulcus (Figure 2B). To place these anchors, the appropriate drill guide was used to create a pilot hole, and then the anchor was placed. There was a distance of 15 mm between the 2 SAs. The central portion of the graft was then attached to the bony trough. The suture was wrapped around the tendon, tension was applied to the sutures, and the graft was secured to the medial patella using a surgeon’s knot followed by 5 manual knots.
Biomechanical Testing
A material testing system (model 5565; Instron) was used to apply pretension and maximally load the MPFL grafts. The biomechanical testing method used has been described by Lenschow et al, 15 Russ et al, 28 and Russo et al. 29 The porcine patella was fixed in a metal mold fixing frame, and the proximal ends of the graft were then fixed in a custom-made clamp (see Figure 1). The distance between the medial margin of the patella and the distal end of the clamp was 55 mm. This distance has been shown to be equivalent to the length of the intact native MPFL. 1,2,37 The tensile force applied to the graft was in the line of pull parallel to the SA or TS, in accordance with the “worst-case scenario” for graft testing. We first applied a preload of 5 to 20 N for 10 cycles to reduce any tissue hysteresis. Subsequently, we performed cyclic loading for 1000 cycles using loads between 5 and 100 N at 1 Hz. Finally, a load-to-failure test at 200 mm/min was carried out in the final load-to-failure test. These parameters were selected on the basis of a previous study. 15 The elongation caused by the load was recorded continuously by the control software of the testing machine. Tissues were kept moist with a saline spray during preparation and testing. The stiffness was calculated as the slope of the linear region of the load-elongation curve corresponding to the steepest straight-line tangent to the curve. Failure was defined as a sudden deviation from the linear curve of load versus displacement. The ultimate failure load and mode of failure were also recorded.
Statistical Analysis
Statistical analysis was performed using SPSS Version 20.0 (IBM Corp). The continuous variables are expressed as the means and standard deviations. We used the Shapiro-Wilk test to assess the normality of the data within the groups. Independent-samples t tests were used to compare the elongation, stiffness, and load to failure between the 2 test groups. The significance level was set at P <.05.
Results
Elongation
The elongation was 3.83 ± 0.87 mm in the TS group compared with 3.36 ± 0.74 mm in the SA group after 1000 cycles (Table 1). There was no significant difference between the groups (P = .17 ). None of the graft fixation/patellar complexes failed during cyclic testing in either group.
Table 1.
Comparison of the Structural Properties Between the Transosseous Suture and Suture Anchor Groups a
| TS Group | SA Group | P | |
|---|---|---|---|
| Elongation, mm | 3.83 ± 0.87 | 3.36 ± 0.74 | .17 |
| Stiffness, N/mm | 55.42 ± 7.92 | 72.11 ± 10.64 | <.01 |
| Ultimate load, N | 496.18 ± 93.15 | 399.43 ± 105.35 | .03 |
a Data are reported as mean ± SD. Bold P values indicate a statistically significant difference between groups (P < .05). SA, suture anchor; TS, transosseous suture.
Stiffness
The specimens repaired using the SA technique had an average pullout stiffness of 72.11 ± 10.64 N/mm. The specimens repaired using the TS technique had an average stiffness of 55.42 ± 7.92 N/mm. The TS technique resulted in less stiffness than did the SA technique (P < .01).
Maximum Load to Failure
During load-to-failure testing, the grafts placed using TS fixation required significantly more force to fail than did the grafts placed using SA fixation. The average maximum load-to-failure values in the SA and TS groups were 399.43 ± 105.35 N and 496.18 ± 93.15 N, respectively. The difference between the 2 groups was statistically significant (P = .03).
Failure Mode
In the SA group, 7 reconstructions failed because of the anchor being pulled out of the medial edge of the patella, while 4 reconstructions failed because of rupture of the suture material; suture knot failure was the reason for failure in the remaining specimen. In the TS group, 10 reconstructions failed because of rupture of the suture material; in the remaining 2 reconstructions, the constructs failed because of rupture of the tendon itself near the clamp.
Discussion
The purpose of this study was to compare the elongation, stiffness, and ultimate failure load between a commonly used SA fixation technique and a new TS fixation technique for MPFL reconstruction under cyclic loading and load-to-failure testing. In the present study, the most important finding was that the ultimate failure load for the TS technique (496.18 ± 93.15 N) was greater than that of SA fixation (399.43 ± 105.35 N) (P = .03). Therefore, this TS fixation technique may be a very effective and useful method for MPFL reconstruction in clinical practice.
While multiple MPFL reconstruction techniques have been described, the ideal graft fixation technique for MPFL reconstruction on the patellar side remains controversial. ∥ The TS technique for MPFL reconstruction was initially introduced for the repair of patellar or quadriceps tendon rupture, 3 and Zhang et al 41 applied this technique for MPFL reconstruction. In the previous study 41 , 29 patients with recurrent patellar dislocation were treated with the TS patellar fixation technique for MPFL reconstruction. No cases of recurrent dislocation were observed in any of the patients within a minimum of 2 years. All outcome scores (International Knee Documentation Committee score and Lysholm score) improved significantly from the preoperative to the postoperative period. The TS technique for MPFL reconstruction allows the placement of anchors in tunnels with diameters smaller than those of patellar tunnels made using traditional techniques and theoretically minimizes the risk of patellar fractures. Furthermore, a remarkable advantage of the TS technique for MPFL reconstruction is the cost, as this technique does not require implants.
Only a few biomechanical studies comparing the biomechanical properties of different patellar fixation methods for MPFL reconstruction have been performed. 10,15,28,29 Lenschow et al 15 evaluated 5 patellar fixation techniques (transverse tunnel, SA, interference screw, medial bone bridge, and TS techniques) for MPFL reconstruction in the porcine patella. They reported that the load to biomechanical failure was 539.5 ± 159.6 N in the TS group, which was significantly higher than that in the SA group (401.5 ± 96.1 N). The most common failure mode in our study in the SA group was anchor pullout; however, the most common failure mode in the study by Lenschow et al 15 in the SA group was rupture of the suture material (6/10 specimens). This inconsistency might be attributed to the bony trough that was made in the medial border of the patella using nucleus forceps to model the clinical scenario in our study (the SAs were placed in the cancellous bone of the patella) and difference in high-strength sutures used in our study. Russ et al 28 compared the ultimate failure load and stiffness of 2 different MPFL patellar fixation techniques: SA fixation and interference screw fixation. The mean failure load was significantly higher in the interference screw group (299.25 ± 99.87 N) than in the SA group (201.54 ± 63.14 N). The mean stiffness was also significantly lower in the SA group (20.60 ± 6.78 N/mm) than in the interference screw group (34.66 ± 10.74 N/mm). The authors recommended using interference screw fixation based on the ultimate load and stiffness results. Russo et al 29 compared 4 techniques for MPFL reconstruction: (1) an interference screw technique, (2) an SA technique, (3) a converging tunnel technique, and (4) a 2-bone tunnel technique. They found that the converging tunnel technique demonstrated a higher maximum load (264 ± 58 N) than did the SA technique (154 ± 14 N) and the interference screw technique (160 ± 24 N). Raoulis et al 26 compared the maximum load to failure and the stiffness of 3 MPFL reconstruction techniques in 12 pairs of fresh-frozen cadaveric knees: (1) SA fixation, (2) interference screw fixation, and (3) suture knot patellar fixation. They found no significant difference in the load to failure among the 3 techniques. The mean ultimate loads with suture knot, SA, and interference screw fixation were 253.5 N, 243 N, and 263.2 N, respectively. In the present study, the ultimate failure load for the TS technique was 496.18 ± 93.15 N, which is greater than that reported for the MPFL in a normal knee with a mean tensile strength of 208 N. 1 Furthermore, this TS fixation technique can be a very effective and useful method for MPFL reconstruction in clinical practice. 41,42
Clinically, the optimal MPFL graft stiffness is unknown, and it remains unclear what the ideal stiffness should be after MPFL reconstruction. Theoretically, the graft should have a similar stiffness to the native MPFL. Grafts with greater stiffness exhibit a greater tendency to resist elongation. A reconstructed graft that is thicker and stronger than a natural MPFL may lead to excessive tensioning of the graft and medial patellar overload, resulting in cartilage tears and degeneration; thus, overtensioning of the joint should be considered in clinical practice. 29
The TS technique offers some advantages. First, the TS technique does not require implants and is theoretically less expensive than other techniques (such as those involving suspension buttons, biodegradable screws, and metallic anchors). At our institution, the cost for 2 SAs for MPFL reconstructions is approximately US $1000, and 3 No. 2 UltraBraid sutures cost approximately US $120. Second, TS fixation for MPFL reconstruction at the patellar side provides a higher load to failure than fixation via SAs. The higher ultimate failure load with the TS technique than with the SA technique might protect the reconstructed ligament during the accelerated rehabilitation process, although the magnitude by which the load to failure was higher may not be clinically significant.
Limitations
There are certain limitations to this investigation. First, the results were obtained in a biomechanical study performed on porcine patellar and graft specimens because of the limited availability of young human bone. However, porcine bones have been used in multiple biomechanical studies evaluating different fixation techniques at the knee joint because the porcine patella has a trabecular bone density similar to that of human patellar bone. 15,29 Second, the linear pullout test used to evaluate reconstructions in the present study did not take into account the normal movement and dynamic patellofemoral contact pressure for reconstruction of the MPFL. The straight-line pullout may have differential effects on anchors versus suture tunnels; since the anchors failed most commonly by anchor pullout, it is possible that the results would be different if the direction of pull were different. Third, biological factors, such as healing at the bone-implant interface, could not be considered in this study. Fourth, the SA technique involves 2 knots, whereas the TS technique involves 3 knots and thus more points of fixation, which could affect the results. Fifth, the TS technique carries a potentially greater risk of fracture, a need for an additional lateral incision to retrieve and tie the sutures, and a risk for errant pin placement through the articular cartilage or anterior cortex. Sixth, we did not measure the intact native construct as a reference for our surgical techniques. Although this comparison cannot be made, we believe this TS fixation technique is significantly stronger than native tissue.
Conclusion
Our study showed that MPFL reconstruction with TS provides a higher load to failure than does SA fixation.
Footnotes
Final revision submitted April 10, 2021; accepted June 8, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from China Medical University.
References
- 1. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215–220. [DOI] [PubMed] [Google Scholar]
- 2. Aframian A, Smith TO, Tennent TD, Cobb JP, Hing CB. Origin and insertion of the medial patellofemoral ligament: a systematic review of anatomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3755–3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Black JC, Ricci WM, Gardner MJ, et al. Novel augmentation technique for patellar tendon repair improves strength and decreases gap formation: a cadaveric study. Clin Orthop Relat Res. 2016;474(12):2611–2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bonazza NA, Lewis GS, Lukosius EZ, Roush EP, Black KP, Dhawan A. Effect of transosseous tunnels on patella fracture risk after medial patellofemoral ligament reconstruction: a cadaveric study. Arthroscopy. 2018;34(2):513–518. [DOI] [PubMed] [Google Scholar]
- 5. Buckens CF, Saris DB. Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med. 2010;38(1):181–188. [DOI] [PubMed] [Google Scholar]
- 6. Chouteau J. Surgical reconstruction of the medial patellofemoral ligament. Orthop Traumatol Surg Res. 2016;102(1)(suppl):S189–S194. [DOI] [PubMed] [Google Scholar]
- 7. Christiansen SE, Jacobsen BW, Lund B, Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24(1):82–87. [DOI] [PubMed] [Google Scholar]
- 8. Conlan T, Garth WP, Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. [DOI] [PubMed] [Google Scholar]
- 9. Donahue TL, Gregersen C, Hull ML, Howell SM. Comparison of viscoelastic, structural, and material properties of double-looped anterior cruciate ligament grafts made from bovine digital extensor and human hamstring tendons. J Biomech Eng. 2001;123(2):162–169. [DOI] [PubMed] [Google Scholar]
- 10. Hapa O, Akşahin E, Özden R, et al. Aperture fixation instead of transverse tunnels at the patella for medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):322–326. [DOI] [PubMed] [Google Scholar]
- 11. Hinton RY, Sharma KM. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am. 2003;34(3):385–396. [DOI] [PubMed] [Google Scholar]
- 12. Johnson DS, Turner PG. Management of the first-time lateral patellar dislocation. Knee. 2019;26(6):1161–1165. [DOI] [PubMed] [Google Scholar]
- 13. LaPrade MD, Kallenbach SL, Aman ZS, et al. Biomechanical evaluation of the medial stabilizers of the patella. Am J Sports Med. 2018;46(7):1575–1582. [DOI] [PubMed] [Google Scholar]
- 14. Lee DY, Park YJ, Song SY, Hwang SC, Park JS, Kang DG. Which technique is better for treating patellar dislocation? A systematic review and meta-analysis. Arthroscopy. 2018;34(11):3082–3093.e1. [DOI] [PubMed] [Google Scholar]
- 15. Lenschow S, Schliemann B, Gestring J, Herbort M, Schulze M, Kösters C. Medial patellofemoral ligament reconstruction: fixation strength of 5 different techniques for graft fixation at the patella. Arthroscopy. 2013;29(4):766–773. [DOI] [PubMed] [Google Scholar]
- 16. Lewallen L, McIntosh A, Dahm D. First-time patellofemoral dislocation: risk factors for recurrent instability. J Knee Surg. 2015;28(4):303–309. [DOI] [PubMed] [Google Scholar]
- 17. Matic GT, Magnussen RA, Kolovich GP, Flanigan DC. Return to activity after medial patellofemoral ligament repair or reconstruction. Arthroscopy. 2014;30(8):1018–1025. [DOI] [PubMed] [Google Scholar]
- 18. Mistry JB, Bonner KF, Gwam CU, Thomas M, Etcheson JI, Delanois RE. Management of injuries to the medial patellofemoral ligament: a review. J Knee Surg. 2018;31(5):439–447. [DOI] [PubMed] [Google Scholar]
- 19. Nomura E, Inoue M. Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthroscopy. 2003;19(5):e47. [DOI] [PubMed] [Google Scholar]
- 20. Nwachukwu BU, So C, Schairer WW, Green DW, Dodwell ER. Surgical versus conservative management of acute patellar dislocation in children and adolescents: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):760–767. [DOI] [PubMed] [Google Scholar]
- 21. Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39(12):2647–2655. [DOI] [PubMed] [Google Scholar]
- 22. Parikh SN, Wall EJ. Patellar fracture after medial patellofemoral ligament surgery: a report of five cases. J Bone Joint Surg Am. 2011;93(17):e97 (1-8). [DOI] [PubMed] [Google Scholar]
- 23. Petri M, Ettinger M, Stuebig T, et al. Current concepts for patellar dislocation. Arch Trauma Res. 2015;4(3):e29301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Petri M, Liodakis E, Hofmeister M, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg. 2013;133(2):209–213. [DOI] [PubMed] [Google Scholar]
- 25. Puzzitiello RN, Waterman B, Agarwalla A, et al. Primary medial patellofemoral ligament repair versus reconstruction: rates and risk factors for instability recurrence in a young, active patient population. Arthroscopy. 2019;35(10):2909–2915. [DOI] [PubMed] [Google Scholar]
- 26. Raoulis VA, Zibis A, Chiotelli MD, et al. Biomechanical evaluation of three patellar fixation techniques for MPFL reconstruction: load to failure did not differ but interference screw stabilization was stiffer than suture anchor and suture-knot fixation. Published online January 2, 2021. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-020-06389-4 [DOI] [PubMed] [Google Scholar]
- 27. Regalado G, Lintula H, Kokki H, Kröger H, Väätäinen U, Eskelinen M. Six-year outcome after non-surgical versus surgical treatment of acute primary patellar dislocation in adolescents: a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):6–11. [DOI] [PubMed] [Google Scholar]
- 28. Russ SD, Tompkins M, Nuckley D, Macalena J. Biomechanical comparison of patellar fixation techniques in medial patellofemoral ligament reconstruction. Am J Sports Med. 2015;43(1):195–199. [DOI] [PubMed] [Google Scholar]
- 29. Russo F, Doan J, Chase DC, Farnsworth CL, Pennock AT. Medial patellofemoral ligament reconstruction: fixation technique biomechanics. J Knee Surg. 2016;29(4):303–309. [DOI] [PubMed] [Google Scholar]
- 30. Saccomanno MF, Sircana G, Fodale M, Donati F, Milano G. Surgical versus conservative treatment of primary patellar dislocation: a systematic review and meta-analysis. Int Orthop. 2016;40(11):2277–2287. [DOI] [PubMed] [Google Scholar]
- 31. Sanchis-Alfonso V, Montesinos-Berry E, Ramirez-Fuentes C, Leal-Blanquet J, Gelber PE, Monllau JC. Failed medial patellofemoral ligament reconstruction: causes and surgical strategies. World J Orthop. 2017;8(2):115–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Saper MG, Meijer K, Winnier S, Popovich J, Jr, Andrews JR, Roth C. Biomechanical evaluation of classic solid and all-soft suture anchors for medial patellofemoral ligament reconstruction. Am J Sports Med. 2017;45(7):1622–1626. [DOI] [PubMed] [Google Scholar]
- 33. Schöttle P, Schmeling A, Romero J, Weiler A. Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2009;129(3):305–309. [DOI] [PubMed] [Google Scholar]
- 34. Schöttle PB, Hensler D, Imhoff AB. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):147–151. [DOI] [PubMed] [Google Scholar]
- 35. Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Song SY, Kim IS, Chang HG, Shin JH, Kim HJ, Seo YJ. Anatomic medial patellofemoral ligament reconstruction using patellar suture anchor fixation for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2431–2437. [DOI] [PubMed] [Google Scholar]
- 37. Trinh TQ, Ferrel JR, Bentley JC, Steensen RN. The anatomy of the medial patellofemoral ligament. Orthopedics. 2017;40(4):e583–e588. [DOI] [PubMed] [Google Scholar]
- 38. Tsushima T, Tsukada H, Sasaki S, et al. Biomechanical analysis of medial patellofemoral ligament reconstruction: FiberTape with knotless anchors versus a semitendinosus tendon autograft with soft anchors. J Orthop Sci. 2019;24(4):663–667. [DOI] [PubMed] [Google Scholar]
- 39. Valkering KP, Rajeev A, Caplan N, Tuinebreijer WE, Kader DF. An evaluation of the effectiveness of medial patellofemoral ligament reconstruction using an anatomical tunnel site. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3206–3212. [DOI] [PubMed] [Google Scholar]
- 40. Wang SN, Qin CH, Jiang N, Wang BW, Wang L, Yu B. Is surgical treatment better than conservative treatment for primary patellar dislocations? A meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg. 2016;136(3):371–379. [DOI] [PubMed] [Google Scholar]
- 41. Zhang H, Ye M, Liang Q. Clinical outcomes after medial patellofemoral ligament reconstruction with suture fixation of the gracilis tendon via transosseous tunnels. Orthop J Sports Med. 2020;8(2):2325967119900373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ye M, Zhang H, Liang Q. Clinical outcomes after medial patellofemoral ligament reconstruction using transosseous sutures versus suture anchors: a prospective nonrandomized controlled trial. Orthop J Sports Med. 2020;8(5):2325967120917112. [DOI] [PMC free article] [PubMed] [Google Scholar]


