Abstract
Background
Trimethylamine N-oxide (TMAO) is a microbiota-derived metabolite, which is linked to vascular inflammation and atherosclerosis in cardiovascular (CV) diseases. But its effect in infectious diseases remains unclear. We conducted a single-center prospective study to investigate association of TMAO with in-hospital mortality in septic patients admitted to an intensive care unit (ICU).
Methods
Totally 95 septic, mechanically ventilated patients were enrolled. Blood samples were obtained within 24 h after ICU admission, and plasma TMAO concentrations were determined. Septic patients were grouped into tertiles according to TMAO concentration. The primary outcome was in-hospital death, which further classified as CV and non-CV death. Besides, we also compared the TMAO concentrations of septic patients with 129 non-septic patients who were admitted for elective coronary angiography (CAG).
Results
Septic patients had significantly lower plasma TMAO levels than did subjects admitted for CAG (1.0 vs. 3.0 μmol/L, p < 0.001). Septic patients in the lowest TMAO tertile (< 0.4 μmol/L) had poorer nutrition status and were given longer antibiotic courses before ICU admission. Circulating TMAO levels correlated positively with daily energy intake, the albumin and prealbumin concentration. Compared with those in the highest TMAO tertile, septic patients in the lowest TMAO tertile were at greater risk of non-CV death (hazard ratio 2.51, 95% confidence interval 1.21–5.24, p = 0.014). However, TMAO concentration was no longer an independent predictor for non-CV death after adjustment for disease severity and nutritional status.
Conclusion
Plasma TMAO concentration was inversely associated with non-CV death among extremely ill septic patients, which could be characterized as TMAO paradox. For septic patients, the impact of malnutrition reflected by circulating TMAO levels was greater than its pro-inflammatory nature.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40560-021-00581-5.
Keywords: Trimethylamine N-oxide, Gut microbiota, Sepsis, Nutrition, Inflammation
Background
Sepsis, a life-threatening disease caused by a dysregulated host response to infection and organ dysfunction [1], is the leading cause of death in intensive care units (ICUs). Emerging evidence suggests that intestinal microbiota imbalances are associated with various inflammatory and metabolic diseases, including atherosclerosis [2], diabetes [3], obesity [4], and dyslipidemia [5], but few studies have examined the roles of microbiota or their metabolites in septic patients [6].
Trimethylamine N-oxide (TMAO) is a proinflammatory metabolite that originates from the bacterial metabolism of choline-rich foods, such as red meat and eggs [7]. Accumulating evidence suggests that TMAO is associated with vascular inflammation [8] and atherosclerosis [9]. Elevated plasma TMAO levels have been linked to worsening prognoses in patients with coronary artery disease (CAD) [9], chronic kidney disease [3], and chronic obstructive pulmonary disease [10]. Dietary supplement with choline enhances atherosclerosis in the apoE−/− mice. Elimination of intestinal microbiota by antibiotics reduces plasma TMAO concentration and mitigates its proatherosclerotic effect [11]. However, the role of TMAO in the context of infectious diseases remains unclear. In addition, no clinical data on the impacts of plasma TMAO concentrations in septic patients are currently available.
We conducted this single-center prospective observational study to investigate associations between plasma TMAO concentrations and all-cause mortality in septic patients. Detailed information about participants’ nutritional status and antimicrobial therapy, as well-known confounding factors for TMAO [9], was collected. We hypothesized that higher TMAO levels would be associated with more severe inflammation and worse outcomes in septic patients.
Methods
Study populations
This study was approved by the Research Ethics Committee of Taipei Veterans General Hospital (no. 2018-02-009AC) and conducted according to the principles expressed in the Declaration of Helsinki. All participants provided written informed consent. We prospectively screened 116 patients aged > 18 years who were admitted to the medical ICU of Taipei Veterans General Hospital, a tertiary medical center in Taiwan, between September 2018 and January 2020. Patients were admitted to the medical ICU because of various critical illnesses, including acute respiratory failure and hemodynamic instability. Sepsis and septic shock were defined according to the 2016 Surviving Sepsis Campaign guidelines [1]. Patients without sepsis, mechanical ventilation requirement, and the pre-dialysis patients, who are known to have extremely high TMAO concentrations [12], were excluded from this study. Information about enrolled patients’ age, sex, smoking history, comorbidities, nutritional status, infection causes, number and duration of previous antibiotic treatment courses was collected by detailed chart review. Blood cell counts and chemistry parameters were measured at the time of ICU admission. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation [13]. Acute Physiology and Chronic Health Evaluation II (APACHE II) [14] and Sequential Organ Failure Assessment (SOFA) scores [15] were calculated within 24 h after ICU admission. We also compared the plasma TMAO concentrations of septic patients with those without sepsis. As the non-sepsis group, we enrolled 129 subjects admitted for elective coronary angiography (CAG) whose plasma TMAO concentrations had been determined in our previous work [16]. Pre-dialysis patients and those with acute myocardial infarction (AMI) or without available C-relative protein data were excluded from this group.
Measurement of plasma TMAO concentrations
Trained registered nurses obtained blood samples from the enrolled septic patients within 24 h after ICU admission. The blood samples were centrifuged, and 200 μL plasma was mixed with TMAO-d9 isotopologues. After filtration, TMAO concentrations were quantified using a stable isotope dilution assay and high-performance liquid chromatography, with online electrospray ionization tandem mass spectrometry performed on an API 4000 Q-TRAP mass spectrometer (AB SCIEX, Framingham, MA, USA). The septic patients were allocated to tertiles according to their plasma TMAO concentrations.
Measurement and calculation of nutritional indicators
As traditional nutritional markers [17], serum albumin and prealbumin values were measured by commercial kits (Beckman Coulter, Brea, CA, USA) at the time of ICU admission. For the septic patients admitted to the ICU, detailed information about enteral and parenteral calorie and protein intakes was recorded every 8 h. Daily calorie/protein intake was defined as the average intake per day in the first 48 h of ICU admission. Because indirect calorimetry was currently unavailable in our hospital, we used weight-based equations to determine the energy requirements as the suggestion of guidelines [18, 19]. Target calorie requirements were calculated as 25–30 kcal/kg/day, adjusted by BMI [20]. Target protein requirements were calculated as 1.3 g/kg/day [18].
According to the guideline of American Society for Parenteral and Enteral Nutrition [19], we routinely used Nutrition Risk Screening 2002 (NRS-2002) score to determine the nutrition risk of patients admitted to ICU. NRS-2002 score had been used to access the nutrition risk in critically ill patients in previous studies [21–23]. Patients with NRS-2002 ≥ 5 were considered to be at high risk of malnutrition, and was associated with greater in-hospital mortality [24]. Experienced nursing staff measured the height and weight of the patients, and interviewed them or their family members to identify changes in dietary intake in the previous week, weight loss in the previous 3 months, and the severity of disease [25]. Based on these data, the patients’ body mass index (BMI) and NRS-2002 scores [25] were calculated and documented in their medical records. The nutrition risk index (NRI) was also calculated using the serum albumin and body weight values measured at ICU admission, as 1.519 × albumin (g/L) + 41.7 × (present body weight/ideal body weight) [26, 27].
Definition of clinical outcomes
The primary outcome was in-hospital all-cause death, classified further as cardiovascular (CV) and non-CV death. Patients who died of AMI, sudden cardiac death, heart failure, stroke, or CV procedures were allocated to the CV death group [28]. Those who died of other causes, primarily sepsis and terminal cancer, were allocated to the non-CV death group. Secondary outcomes included acute kidney injury (AKI) within 48 h after ICU admission, AKI required dialysis during ICU stay, and successful ventilator weaning during hospitalization. AKI was defined according to the Kidney Disease Improving Global Outcomes criteria [29]. Patients who were ventilator independent at discharge were deemed to be weaned successfully [30]. The duration of ventilator use and lengths of ICU and hospital stays were also recorded.
Statistical analysis
Continuous variables were expressed as medians (interquartile ranges) and analyzed using the Mann–Whitney U test or Kruskal–Wallis test. Categorical variables were presented as numbers (percentages) and assessed using Fisher’s exact test or the Chi-squared test. Spearman’s rank correlation test was used to assess correlations between TMAO concentrations and nutritional indicators. Multivariate linear regression analysis was performed to investigate relationships between TMAO values and clinical factors. The incidence of in-hospital, all-cause death (further classified as CV death and non-CV death) and successful ventilator weaning were calculated. Kaplan–Meier analysis and the log-rank test was used to determine the cumulative incidences of death and successful ventilator weaning, stratified by TMAO concentrations. Cox regression analysis was performed to identify predictors of non-CV death and successful ventilator weaning. Variables with p < 0.1 in the univariate regression analysis were included in an adjusted forward-stepwise multivariate regression model. p Values < 0.05 were regarded as significant. The analyses were performed using SPSS (version 18.0; SPSS Inc., Chicago, IL, USA) and MedCalc (version 11.4.2.0; MedCalc Software, Mariakerke, Belgium).
The sample size was calculated using PASS (version 15.0.5; NCSS, LLC., Kaysville, Utah, USA). The calculation was based on assuming three independent study groups and the primary outcome was in-hospital mortality. As there is currently no data for septic patients grouped by TMAO concentrations, we estimated the sample size by data from the community-acquired pneumonia population [31]. Plasma TMAO concentration was 2.3, 3.0, and 4.1 μmol/L, respectively, in patients with varying mortality rate of community-acquired pneumonia. Using the Kruskal–Wallis test, a total sample of 45 subjects are required to achieve a power of 0.900 with a target significance of 0.050. Considering the prevalence of sepsis was 44% for the critically-ill population in our previous work [32], we need to screen at least 102 patients admitted to ICU to complete this study.
Results
TMAO concentrations and nutritional status in septic patients
One hundred and sixteen patients admitted to ICU during 2018–2020 were screened. After the exclusion of patients without sepsis (N = 14) and mechanical ventilation (N = 1) and pre-dialysis patients (N = 6), 95 septic, mechanically ventilated patients were enrolled in this study. The median age of the septic patients was 70.0 (60.0–78.0) years, and 58 (61.1%) of them were male. Respiratory tract infection was the leading cause of sepsis (80.0%), and 34 (35.8%) patients had septic shock. A flowchart of patient enrollment and classification was provided, as shown in Fig. 1. Age, sex, APACHE II and SOFA scores, and the prevalence of septic shock were similar in the groups defined by TMAO tertiles (Table 1). Patients with high TMAO concentrations (≥ 2.5 μmol/L) had higher prevalence of CAD, stroke, and peripheral arterial disease, and higher C-reactive protein (CRP) levels and lower eGFRs at the time of ICU admission. Compared with patients with high TMAO values, patients with low TMAO concentrations (< 0.4 μmol/L) had been given more and longer antibiotic treatment courses before ICU admission and had lower daily calorie and protein intakes, BMIs, albumin and prealbumin levels, NRIs, and higher NRS-2002 scores. Opposite to our hypothesis, the septic patients had significantly lower plasma TMAO concentrations than did patients admitted for CAG (1.0 vs. 3.0 μmol/L, p < 0.001; Additional file 1: Fig. 1). Relative to patients admitted for CAG, septic patients were with poor nutritional status, reflected by lower BMIs and higher NRS-2002 scores (Additional file 1: Table 1), and received more antibiotic treatments before they admitted to ICU.
Fig. 1.
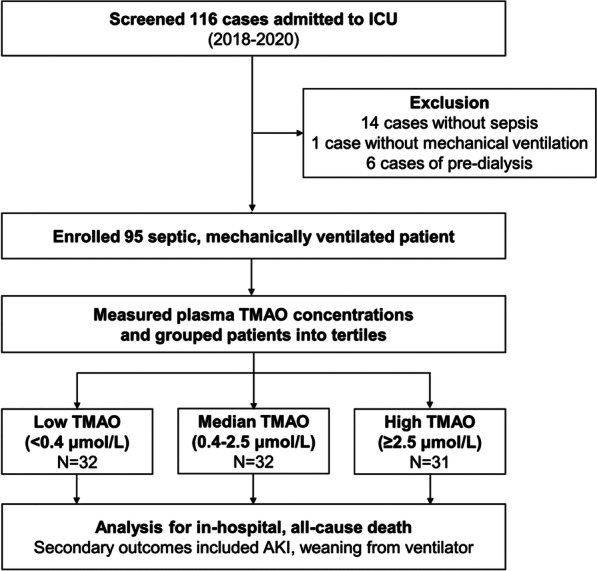
Flowchart of patient enrollment and classification. ICU intensive care unit; TMAO trimethylamine-N-oxide; AKI acute kidney injury
Table 1.
Baseline characteristics and nutritional status of septic patients according to plasma TMAO concentration
| Low TMAO (< 0.4 μmol/L) N = 32 |
Median TMAO (0.4–2.5 μmol/L) N = 32 |
High TMAO (≥ 2.5 μmol/L) N = 31 |
p value |
|
|---|---|---|---|---|
| Age (years) | 68.5 (61.3–79.5) | 67.5 (56.3–74.8) | 70.0 (57.0–78.0) | 0.371 |
| Male gender | 17 (53.1) | 18 (56.3) | 23 (74.2) | 0.182 |
| Smoking | 3 (9.4) | 6 (18.2) | 10 (32.3) | 0.074 |
| Disease severity | ||||
| APACHE II scores | 29 (28.0–31.0) | 28.0 (23.3–31.0) | 29.0 (24.0–32.0) | 0.742 |
| SOFA scores | 12.0 (10.0–12.8) | 11.0 (9.0–13.8) | 11.0 (9.0–12.0) | 0.662 |
| Mean arterial pressure (mmHg) | 56.7 (50.3–63.5) | 58.3 (50.2–65.0) | 53.0 (46.3–61.3) | 0.163 |
| Septic shock | 14 (43.8) | 12 (37.5) | 8 (25.8) | 0.322 |
| Causes & treatment of sepsis | ||||
| Respiratory tract infection | 26 (81.3) | 24 (75.0) | 26 (83.9) | 0.663 |
| Urinary tract infection | 0 (0.0) | 3 (9.4) | 3 (9.7) | 0.196 |
| Intra-abdominal infection | 8 (25.0) | 7 (21.9) | 3 (9.7) | 0.262 |
| Bloodstream infection | 17 (53.1) | 17 (53.1) | 9 (29.0) | 0.087 |
| Abx pre-treatment, numbers | 5.5 (3.0–7.0) | 3.0 (2.3–4.8) | 2.0 (1.0–3.0) | < 0.001 |
| Abx pre-treatment, days | 12.5 (3.3–27.8) | 3.0 (2.0–10.0) | 1.0 (1.0–4.0) | < 0.001 |
| Co-morbidities | ||||
| Hypertension | 9 (28.1) | 13 (40.6) | 15 (48.4) | 0.250 |
| Diabetic mellitus | 7 (21.9) | 8 (25.0) | 8 (25.8) | 0.928 |
| Heart failure | 4 (12.5) | 2 (6.3) | 2 (6.5) | 0.594 |
| COPD | 3 (9.4) | 3 (9.4) | 1 (3.2) | 0.561 |
| Cirrhosis | 2 (6.3) | 3 (9.4) | 0 (0.0) | 0.238 |
| Prior CAD | 1 (3.1) | 2 (6.3) | 8 (25.8) | 0.010 |
| Prior stroke or PAD | 1 (3.1) | 1 (3.1) | 5 (16.1) | 0.075 |
| Malignancy | 20 (62.5) | 15 (46.9) | 14 (45.2) | 0.313 |
| Autoimmune disease | 2 (6.3) | 6 (18.6) | 4 (12.9) | 0.322 |
| Laboratory data | ||||
| White blood cells (K) | 9.0 (3.3–15.0) | 9.6 (1.1–16.2) | 8.6 (2.1–12.4) | 0.906 |
| Hemoglobin (mg/dL) | 8.6 (7.7–9.3) | 8.8 (7.7–10.0) | 8.4 (7.6–9.8) | 0.722 |
| eGFR (mL/min/1.73m2) | 57.4 (26.4–90.3) | 43.0 (21.8–78.9) | 21.5 (7.4–35.2) | 0.001 |
| Total bilirubin (mg/dL) | 1.8 (0.7–3.1) | 1.7 (0.8–4.5) | 0.8 (0.4–1.7) | 0.008 |
| Glucose (mg/dL) | 132.0 (97.8–205.8) | 133.0 (101.3–204.0) | 147.0 (107.0–228.0) | 0.697 |
| Lactate (mg/dL) | 18.3 (8.3–25.4) | 16.7 (9.9–24.1) | 10.8 (7.2–19.8) | 0.268 |
| C-reactive protein (mg/dL) | 7.5 (3.0–13.4) | 12.2 (6.9–19.3) | 13.5 (5.9–25.0) | 0.030 |
| TMAO (μmol/L) | 0.1 (0.1–0.2) | 1.1 (0.7–1.9) | 4.7 (3.5–11.0) | < 0.001 |
| Nutritional status | ||||
| Enteral intake of calories (kcal/day) | 89.5 (0.0–623.5) | 502.0 (0.0–768.9) | 1355.5 (1055.0–1573.0) | < 0.001 |
| Enteral intake of protein (g/day) | 3.5 (0.0–25.9) | 20.0 (0.0–38.4) | 61.0 (35.0–71.0) | < 0.001 |
| Total calories (% of target) | 30.9 (12.6–51.8) | 43.5 (27.9–68.0) | 81.7 (67.1–110.3) | < 0.001 |
| Total protein (% of target) | 14.6 (0.0–53.1) | 32.0 (0.0–59.0) | 66.9 (55.4–86.2) | < 0.001 |
| Body mass index | 19.3 (17.7–20.3) | 21.3 (18.7–25.2) | 23.9 (22.4–28.6) | < 0.001 |
| Albumin (mg/dL) | 2.8 (2.6–3.2) | 2.9 (2.5–3.2) | 3.3 (2.9–3.8) | 0.001 |
| Prealbumin (mg/dL) | 6.9 (4.4–10.9) | 7.7 (5.4–13.1) | 12.0 (8.3–17.0) | 0.001 |
| Nutrition risk index | 80.1 (73.8–85.5) | 84.5 (78.5–92.4) | 98.3 (87.3–109.8) | < 0.001 |
| NRS 2002 scores | 5.0 (5.0–6.0) | 4.0 (4.0–5.8) | 4.0 (3.0–4.0) | < 0.001 |
TMAO trimethylamine-N-oxide; APACHE Acute Physiology and Chronic Health Evaluation; SOFA Sequential Organ Failure Assessment; Abx antibiotic; COPD chronic obstructive pulmonary disease; CAD coronary artery disease; PAD peripheral arterial disease; eGFR estimated glomerular filtration rate; NRS-2002 Nutritional Risk Screening 2002
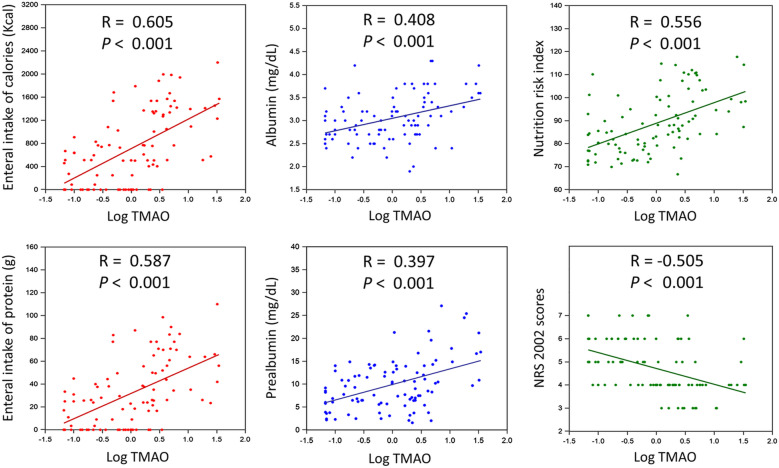
Among septic patients, plasma TMAO levels correlated significantly with enteral calorie (r = 0.605) and protein (r = 0.587) intakes, albumin (r = 0.408) and prealbumin (r = 0.397) level, NRI (r = 0.556), and NRS 2002 (r = − 0.505) scores (all p < 0.001; Fig. 2). In the univariate linear regression analyses, TMAO concentrations correlated positively with prior CAD, the CRP level, daily calorie and protein intakes, the BMI, the albumin, prealbumin level, and the NRI; and negatively with the main arterial pressure (MAP), septic shock, number and duration of previous antibiotic treatment courses, eGFR at the time of ICU admission, and NRS-2002 score (showed in Table 2). In the multivariate regression model, the MAP, septic shock, number of previous antibiotic treatment courses, eGFR, enteral calorie intake, prealbumin, and NRI remained significantly correlated with the TMAO concentration.
Fig. 2.
Correlations of (log-transformed) plasma TMAO concentrations with nutritional indicators in septic patients. TMAO trimethylamine-N-oxide; NRI nutrition risk index; NRS 2002 score nutrition risk screening 2002 scores
Table 2.
Univariate and multivariate linear regression analyses of factors associated with plasma TMAO concentration (log transformation to achieve normality before analysis) in septic patients
| Univariate analysis | Multivariate analysis* | |||
|---|---|---|---|---|
| Std β | p value | Std β | p value | |
| Age | 0.018 | 0.866 | ||
| Male gender | 0.153 | 0.139 | ||
| Smoker | 0.145 | 0.161 | ||
| APACHE II scores | − 0.090 | 0.387 | ||
| SOFA scores | − 0.045 | 0.663 | ||
| Mean arterial pressure | − 0.248 | 0.015 | − 0.215 | 0.001 |
| Septic shock | − 0.202 | 0.050 | − 0.155 | 0.019 |
| Respiratory tract infection | − 0.007 | 0.943 | ||
| Urinary tract infection | 0.124 | 0.231 | ||
| Intra-abdominal infection | − 0.161 | 0.119 | ||
| Bloodstream infection | − 0.131 | 0.205 | ||
| Antibiotic pre-treatment, numbers | − 0.644 | < 0.001 | − 0.337 | < 0.001 |
| Antibiotic pre-treatment, days | − 0.375 | < 0.001 | ||
| Hypertension | 0.170 | 0.100 | ||
| Diabetic mellitus | 0.088 | 0.398 | ||
| Heart failure | − 0.030 | 0.773 | ||
| COPD | − 0.114 | 0.270 | ||
| Cirrhosis | − 0.041 | 0.691 | ||
| Prior CAD | 0.294 | 0.004 | ||
| Prior stroke or PAD | 0.145 | 0.162 | ||
| Malignancy | − 0.110 | 0.291 | ||
| Autoimmune disease | 0.113 | 0.276 | ||
| White blood cells (K) | 0.047 | 0.653 | ||
| Hemoglobin | 0.011 | 0.916 | ||
| eGFR at ICU admission | − 0.357 | < 0.001 | − 0.156 | 0.015 |
| Total bilirubin | − 0.161 | 0.120 | ||
| Glucose | 0.082 | 0.427 | ||
| Lactate | − 0.059 | 0.573 | ||
| C-reactive protein | 0.261 | 0.011 | ||
| Enteral intake of calories | 0.602 | < 0.001 | 0.279 | < 0.001 |
| Enteral intake of protein | 0.566 | < 0.001 | ||
| Total calories (% of target) | 0.573 | < 0.001 | ||
| Total protein (% of target) | 0.500 | < 0.001 | ||
| Body mass index | 0.380 | < 0.001 | ||
| Albumin | 0.397 | < 0.001 | ||
| Prealbumin | 0.456 | < 0.001 | 0.157 | 0.025 |
| Nutrition risk index | 0.519 | < 0.001 | 0.187 | 0.007 |
| NRS 2002 scores | − 0.453 | < 0.001 | ||
TMAO trimethylamine-N-oxide; APACHE Acute Physiology and Chronic Health Evaluation; SOFA Sequential Organ Failure Assessment; CAD coronary artery disease; CI confidence interval; COPD chronic obstructive pulmonary disease; PAD peripheral arterial disease; eGFR estimated glomerular filtration rate; HR hazard ratio; NRS-2002 Nutritional Risk Screening 2002
*Adjusted for variables with p < 0.1 in the univariate analysis
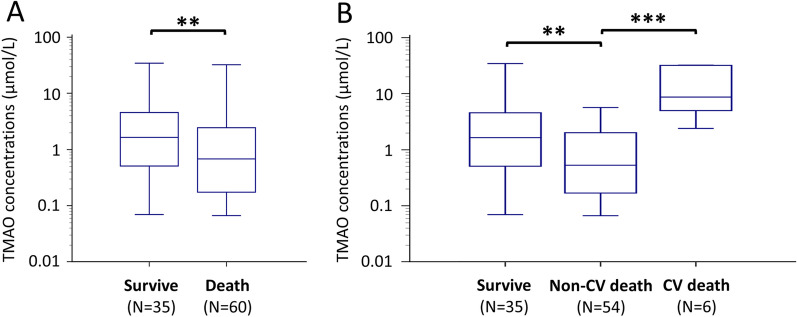
Outcomes of septic patients according to TMAO concentration
Totally 60 (63.1%) cases of all-cause death (6 CV and 54 non-CV death) occurred during hospitalization among septic patients admitted to the ICU. Compared to survivors, patients who died in hospital had lower TMAO concentrations (p = 0.0034; Fig. 3A). These concentrations were also lower among patients who died of non-CV cause than among those who died of CV cause (p < 0.001; Fig. 3B). Compared to survivors, patients died of non-CV cause were with significantly lower enteral intake of calories, total proteins, and lower prealbumin levels (Additional file 1: Table 2). In contrast, patients died of CV cause were with better nutritional conditions.
Fig. 3.
Plasma TMAO concentrations in patients classified by A in-hospital death or survival to discharge and B cause of death during hospitalization. **p < 0.05, ***p < 0.001. TMAO trimethylamine-N-oxide; CAG coronary angiography; CV cardiovascular
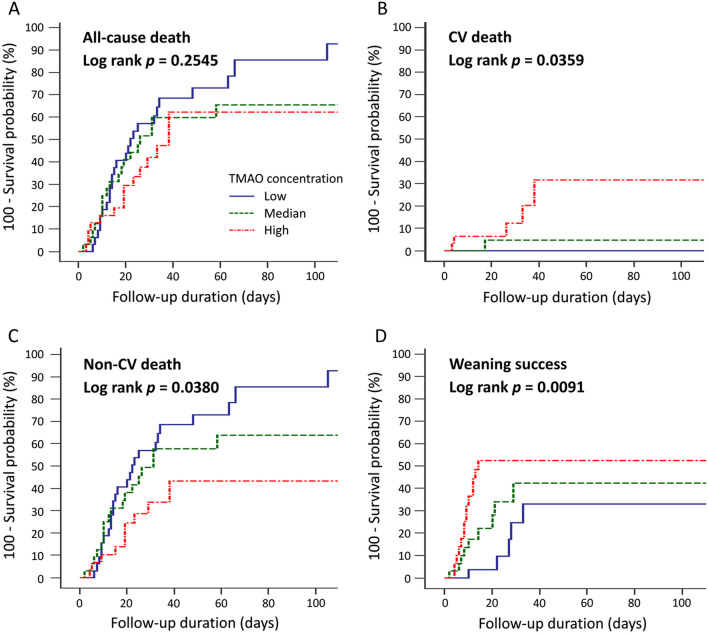
Clinical outcomes of patients grouped by TMAO tertiles are summarized in Table 3. The incidence of all-cause death did not differ significantly among the three groups. However, the incidence of CV death was significantly higher among patients with high TMAO concentrations (16.1%) than among those with low and medium concentrations (0% and 3.1%, respectively; p = 0.021). Patients with higher TMAO levels also tended to have a higher incidence of AKI within 48 h after ICU admission, although this difference was not significant. In contrast, patients with low plasma TMAO concentrations had a significantly higher incidence of non-CV death [78.1% vs. 59.4% (medium) and 32.3% (high); p = 0.001]. Patients with low TMAO concentrations also had a lower rate of successful ventilator weaning [15.6% vs. 28.1% (medium) and 45.2% (high); p = 0.036] and longer duration of ventilator use [21.5 vs. 15.5 (medium) and 12.0 (high) days; p = 0.039]. The median lengths of ICU and hospital stays among all septic patients were 11.0 and 23.0 days, respectively, and did not differ according to TMAO concentration. The cumulative incidences of death and successful ventilator weaning, stratified by TMAO concentrations, are shown in Fig. 4. Low TMAO concentrations were associated with a lower incidence of CV death (log-rank p = 0.0359), higher incidence of non-CV death (log-rank p = 0.0380), and lower rate of successful ventilator weaning (log-rank p = 0.0091).
Table 3.
Clinical outcomes of septic patients according to plasma TMAO concentration
| Low TMAO (< 0.4 μmol/L) N = 32 |
Median TMAO (0.4–2.5 μmol/L) N = 32 |
High TMAO (≥ 2.5 μmol/L) N = 31 |
p value |
|
|---|---|---|---|---|
| Primary outcomes | ||||
| In-hospital, all-cause death | 25 (78.1) | 20 (62.5) | 15 (48.4) | 0.050 |
| Cardiovascular death* | 0 (0) | 1 (3.1) | 5 (16.1) | 0.021 |
| Non-cardiovascular death† | 25 (78.1) | 19 (59.4) | 10 (32.3) | 0.001 |
| Secondary outcomes | ||||
| Acute kidney injury (AKI) | 9 (28.1) | 13 (40.6) | 18 (58.1) | 0.054 |
| AKI required dialysis | 3 (9.4) | 7 (21.9) | 9 (29.0) | 0.142 |
| Weaning success | 5 (15.6) | 9 (28.1) | 14 (45.2) | 0.036 |
| Length of ventilator usage, days | 21.5 (12.3–33.0) | 15.5 (8.3–28.3) | 12.0 (6.0–23.0) | 0.039 |
| Length of ICU stay, days | 13.0 (8.3–20.0) | 10.5 (6.3–19.5) | 10.0 (7.0–16.0) | 0.332 |
| Length of hospitalization, days | 21.5 (13.0–34.8) | 23.5 (10.5–50.0) | 26.0 (19.0–37.0) | 0.906 |
TMAO trimethylamine-N-oxide; ICU intensive care unit
*Patients died of myocardial infarction, sudden cardiac death, heart failure, stroke, or CV procedures
†Patients died of other causes, primarily sepsis and terminal cancer
Fig. 4.
Kaplan–Meier curves for the cumulative incidences of A all-cause death, B CV death, C non-CV death, and D ventilator weaning success in septic patients according to the plasma TMAO concentration. CV cardiovascular; TMAO trimethylamine-N-oxide
Independent predictors of non-CV death and successful ventilator weaning
Compared with patients with high TMAO levels, patients with low plasma TMAO concentrations were at significantly greater risk of non-CV death, according to the univariate Cox regression analysis [hazard ratio (HR) 2.51, 95% confidence interval (CI) 1.21–5.24, p = 0.014]. However, TMAO was no more associated with non-CV death in the multivariate model adjusting septic shock, total bilirubin, enteral intake of calories, enteral intake of protein, total calories, and total protein (Additional file 1: Table 3). In fact, the significant association between TMAO and non-CV death remained even after adjusting the APACHE II and SOFA scores (adjusted HR 2.48, 95% CI 1.10–5.61, p = 0.029, in Additional file 1: Table 4). However, the strength of the association diminished after further adjusting the NRS-2002 score (adjusted HR 1.99, 95% CI 0.86–4.50, p = 0.108). On the other hand, NRS-2002 score was significantly associated with non-CV death in the multivariate regression analysis (adjusted HR 1.35, 95% CI 1.01–1.81, p = 0.046). Plasma TMAO concentration was not an independent predictor for non-CV death in the multivariate regression model. Independent predictors for non-CV death were the APACHE II and SOFA scores, respiratory tract infection, malignancy, lactate concentration, and NRS-2002 score (Table 4).
Table 4.
Factors associated with non-cardiovascular death among septic patients in univariate and multivariate analyses
| Univariate | Multivariate* | |||
|---|---|---|---|---|
| Crude HR (95% CI) | p | Adjusted HR (95% CI) | p | |
| Plasma TMAO | ||||
| High (≥ 2.5 μmol/L) | Ref | Ref | ||
| Median (0.4–2.5 μmol/L) | 1.80 (0.83–3.91) | 0.137 | ||
| Low (< 0.4 μmol/L) | 2.51 (1.21–5.24) | 0.014 | ||
| Age | 1.00 (0.98–1.02) | 0.753 | ||
| Male gender | 1.61 (0.90–2.88) | 0.112 | ||
| Smoker | 1.11 (0.57–2.16) | 0.765 | ||
| APACHE II scores | 1.11 (1.05–1.16) | < 0.001 | 1.11 (1.04–1.18) | 0.001 |
| SOFA scores | 1.22 (1.12–1.32) | < 0.001 | 1.18 (1.06–1.31) | 0.002 |
| Mean arterial pressure | 0.99 (0.97–1.01) | 0.374 | ||
| Septic shock | 1.74 (0.99–3.06) | 0.053 | ||
| Respiratory tract infection | 0.50 (0.26–0.94) | 0.031 | 0.31 (0.16–0.62) | 0.001 |
| Urinary tract infection | 0.50 (0.12–2.05) | 0.333 | ||
| Intra-abdominal infection | 1.59 (0.83–3.04) | 0.164 | ||
| Bloodstream infection | 0.91 (0.53–1.57) | 0.731 | ||
| Antibiotic pre-treatment, numbers | 1.07 (0.95–1.20) | 0.271 | ||
| Antibiotic pre-treatment, days | 1.01 (0.99–1.02) | 0.342 | ||
| Hypertension | 0.67 (0.38–1.20) | 0.180 | ||
| Diabetic mellitus | 1.06 (0.56–1.98) | 0.868 | ||
| Heart failure | 0.69 (0.21–2.22) | 0.532 | ||
| COPD | 1.19 (0.43–3.32) | 0.738 | ||
| Cirrhosis | 1.23 (0.38–3.95) | 0.731 | ||
| Prior CAD | 1.00 (0.36–2.80) | 0.998 | ||
| Prior stroke or PAD | 0.33 (0.08–1.38) | 0.129 | ||
| Malignancy | 1.82 (1.04–3.20) | 0.037 | 2.08 (1.14–3.79) | 0.018 |
| Autoimmune disease | 0.39 (0.12–1.25) | 0.114 | ||
| White blood cells (K) | 0.99 (0.96–1.03) | 0.743 | ||
| Hemoglobin | 0.97 (0.84–1.12) | 0.667 | ||
| eGFR at ICU admission | 1.00 (1.00–1.01) | 0.457 | ||
| Total bilirubin | 1.06 (1.01–1.11) | 0.014 | ||
| Glucose | 1.00 (1.00–1.00) | 0.945 | ||
| Lactate | 1.02 (1.01–1.03) | 0.003 | 1.02 (1.01–1.03) | 0.002 |
| C-reactive protein | 0.98 (0.95–1.01) | 0.231 | ||
| Enteral intake of calories | 1.00 (1.00–1.00) | 0.064 | ||
| Enteral intake of protein | 0.99 (0.98–1.00) | 0.087 | ||
| Total calories (% of target) | 0.99 (0.99–1.00) | 0.088 | ||
| Total protein (% of target) | 0.99 (0.99–1.00) | 0.099 | ||
| Body mass index | 0.97 (0.92–1.03) | 0.359 | ||
| Albumin | 0.78 (0.47–1.31) | 0.354 | ||
| Prealbumin | 0.92 (0.87–0.97) | 0.002 | ||
| Nutrition risk index | 0.98 (0.96–1.01) | 0.156 | ||
| NRS 2002 scores | 1.26 (0.99–1.60) | 0.057 | 1.43 (1.10–1.86) | 0.008 |
HR hazard ratio; CI confidence interval; TMAO trimethylamine-N-oxide; Ref reference; APACHE Acute Physiology and Chronic Health Evaluation; SOFA Sequential Organ Failure Assessment; COPD chronic obstructive pulmonary disease; CAD coronary artery disease; PAD peripheral arterial disease; eGFR estimated glomerular filtration rate; NRS-2002 Nutritional Risk Screening 2002
*Adjusted for variables with p < 0.1 in the univariate analysis
Compared with patients with high TMAO levels, patients with low plasma TMAO concentrations had a significantly lower successful ventilator weaning rate (HR 0.23, 95% CI 0.08–0.65, p = 0.005). The plasma TMAO concentration remained an independent predictor of successful ventilator weaning after adjustment for the APACHE II score and CRP concentration in the multivariate regression model (adjusted HR 0.32, 95% CI 0.11–0.91, p = 0.033; showed in Additional file 1: Table 5).
Discussion
This prospective study investigated the relationships of TMAO concentrations and mortality in septic patients. Septic patients had significantly lower plasma TMAO concentrations than did subjects admitted for CAG. Compared with those in the highest TMAO tertile, septic patients in the lowest TMAO tertile were at greater risk of in-hospital death and unsuccessful ventilator weaning, which may be characterized as the TMAO paradox. However, the strength of the association diminished after adjustment for the disease severity and NRS-2002 score. The inverse association between plasma TMAO and non-CV death was confounded by the nutritional status. Patients in the lowest TMAO tertile had poorer nutrition status and were given longer antibiotic treatment courses before ICU admission. TMAO concentrations correlated positively with the daily energy intake, albumin and prealbumin concentrations. These findings indicate that TMAO, a microbiota-derived metabolite, may be a novel risk biomarker and a nutritional indicator for septic patients; and provide new insight into the impact of malnutrition in the septic population.
TMAO has been reported to stimulate intracellular reactive oxygen species production and release inflammatory cytokines [8]. Although some in vitro findings suggest that TMAO has protective effects, such as protein [33] and nucleic acid [34] stabilization, elevated TMAO concentrations are generally considered to be harmful and have been linked to various CV diseases [2–5, 9]. Contrary to our hypothesis, septic patients in the lowest TMAO tertile were at greater risk of non-CV death and unsuccessful ventilator weaning than were those in higher tertiles. Three rationales may explain the inverse association between the TMAO concentration and adverse outcomes. The first explanation is the impact of malnutrition. As TMAO originates from the bacterial metabolism of dietary choline or carnitine [7], its concentration depends largely on enteral nutrition. Septic patients in the lowest TMAO tertile had lower BMIs and higher NRS-2002 scores, which suggest premorbid malnutrition and thus increased vulnerability to acute stress. Malnutrition was also reported to be associated with intestinal dysbiosis and metabolic endotoxemia [35], which may further deteriorate sepsis. Another explanation is the influence of antibiotic treatment before ICU admission. In a previous study, plasma TMAO concentrations became undetectable after 1 week of broad-spectrum antibiotic treatment [9]. The median duration of pre-ICU admission antibiotic treatment among septic patients in our study was 3 days. This treatment thus considerably reduced TMAO concentrations. The third explanation involves the influence of organ dysfunction during sepsis. Sepsis may result in intestinal dysfunction and dysbiosis [36], which directly reduced the enteral intake and attenuated the production of bacterial metabolites. Moreover, trimethylamine, the precursor of TMAO, was converted into TMAO by liver enzymes (flavin-containing monooxygenase-3) [7]. Sepsis-associated liver dysfunction may also suppress the conversion and decrease TMAO concentration. Finally, TMAO is eliminated by kidneys [12]. Both sepsis-associated AKI and dialysis may affect its plasma concentration [37]. Theses explanations were supported by the results of our analyses. Enteral intake of calories, the numbers of previous antibiotic treatment courses, eGFR, and NRI (composed of albumin and BMI) were all independently correlated with plasma TMAO concentration in the multivariate regression analysis. However, only the nutritional indicator, NRS-2002 score, was independently associated with non-CV death. For septic patients, the impact of malnutrition was somewhat greater than those of inflammation or previous antibiotic treatment.
Several pieces of clinical evidence support the association between TMAO and nutrition. The dietary content may modulate the production of TMAO; plasma TMAO concentrations have been found to increase with high-protein [38] and high-fat [39] diets, and to decrease upon supplementation with indigestible carbohydrates [40]. Circulating TMAO levels have been found to correlate positively with energy intake [41], the consumption of animal proteins [41], the BMI [4, 41], and the albumin concentration [42]. Compatible with these previous observations, plasma TMAO concentrations correlated positively with septic patients’ daily calorie and protein intakes, BMIs, and albumin concentrations in this study. Not surprisingly, they also correlated with other nutritional indicators, including the NRI and NRS-2002 score. These findings suggest that septic patients with low plasma TMAO levels have both acute and chronic disease-related malnutrition. As a potential nutritional indicator, TMAO has obvious weak point. The measurement of plasma TMAO is expensive and easy to be influenced by the antibiotic therapy. Nevertheless, TMAO has the strengths to reflect the absorption of animal proteins (including fishes, eggs, and meats) [43] and gut microbiota metabolism [44], which cannot not be substituted by other biomarkers.
TMAO may play different roles in CV and infectious diseases. Choline-rich diets and TMAO are frequently reported to be risk factors for CV diseases [2, 3, 9]. In contrast, we observed an inverse association between the circulating TMAO level and non-CV death among septic patients in this study. One observational study suggested that plasma TMAO levels correlated positively with long-term mortality in a population of patients with community-acquired pneumonia without CAD [31]. However, those patients had much less-severe disease and higher BMIs and plasma TMAO values at the time of enrollment (median, 3.0 μmol/L) than did our septic patients. In another study, circulating TMAO concentrations were lower in untreated patients with human immunodeficiency virus infection and increased significantly after treatment initiation (from 1.28 to 2.30 μmol/L), eventually becoming similar to those of healthy subjects [45]. The inverse association between the TMAO concentration and non-CV death in our study may be seen only in the advanced stage of sepsis or in extremely ill patients. Changes in the plasma TMAO concentration at different stages of sepsis should be examined in further longitudinal studies.
Several limitations of this study should be addressed. First, the study was conducted at a single center with small patient groups. The clinical significance of the TMAO concentration for all-cause mortality should be investigated in a large-scale study. In addition, the septic patients enrolled in this study were geriatric and had relatively severe disease, which limits the generalizability of our results. Second, in the absence of indirect calorimetry, we used weight-based equations to determine the energy requirements, which may be less accurate in critically ill patients. On top of that, we only used the BMI, NRI, and NRS-2002 score, which routinely calculated in our hospital, to screen for nutrition risk among the septic patients. Other nutritional indicators, such as muscle mass, body fat, and other body composition measurements, are not included in the diagnostic criteria for malnutrition [46]. Third, we did not obtain stool samples to analyze the microbiome of enrolled patients. Septic and critically ill patients were reported to have decreased intestinal microbiota diversity [6], and gut dysbiosis was also linked to reduced TMAO levels in previous observation [47]. An additional study with bioinformatic analysis should be performed to confirm the association between dysbiosis and plasma TMAO in septic patients.
Conclusions
The circulating TMAO level is associated inversely with non-CV death among extremely ill septic patients, as the TMAO paradox. For these patients, the impact of malnutrition is somewhat greater than the pro-inflammatory effect of TMAO. This study provides indirect evidence for the impact of malnutrition on intestinal microbiota. Further studies are need to investigate the relationship between intestinal dysfunction, nutritional status, and gut microbiota in the septic population.
Supplementary Information
Additional file 1: Figure 1. Plasma TMAO concentrations in patients classified by A reason for hospitalization (sepsis vs. elective CAG) and B sepsis and different severity of CAD. Table 1. Baseline characteristics, TMAO concentrations, and outcomes of septic patients and patients admitted for elective CAG. Table 2. Plasma TMAO concentrations and nutritional indicators of patients classified by different causes of death during hospitalization. Table 3. Univariate and multivariate Cox regression analyses to investigate the relationships between TMAO, septic shock, total bilirubin, enteral intake of calories, enteral intake of protein, total calories, total protein, and non-cardiovascular death among septic patients. Table 4. Univariate and multivariate Cox regression analyses to investigate the relationships between TMAO, disease severity, antibiotic pre-treatment, nutritional risk scores, and non-CV death among septic patients. Table 5. Univariate and multivariate Cox regression analyses of factors associated with weaning success among septic patients
Acknowledgements
The authors would like to acknowledge Ms. Li-Shu Wang in assisting statistical analysis.
Abbreviations
- AKI
Acute kidney injury
- AMI
Acute myocardial infarction
- APACHE II
Acute Physiology and Chronic Health Evaluation II
- BMI
Body mass index
- CAD
Coronary artery disease
- CAG
Coronary angiography
- CI
Confidence interval
- CRP
C-reactive protein
- CV
Cardiovascular
- HR
Hazard ratio
- MAP
Mean arterial pressure
- NRI
Nutrition risk index
- NRS-2002
Nutrition Risk Screening 2002
- SOFA
Sequential Organ Failure Assessment
- TMAO
Trimethylamine N-oxide
Authors' contributions
Conceptualization: RHC, PSW; data curation: SFL, RYL, YLT, YWL, MRK, JYG, RYC; formal analysis: RHC, PSW, SCW; funding acquisition: PHH; investigation: RHC, SCW, CHW; methodology: SCW, CHW, PHH; Project administration: PHH, SJL; resources: RHC, PHH, SJL; Software: RHC, SCW; supervision and validation: PHH, SJL; writing—original draft: RHC, PSW. All authors had full access to the study data and take responsibility for the integrity of the data and the accuracy of the analysis. All authors read and approved the final manuscript.
Funding
This study was supported, in part, by research grants from the Ministry of Science and Technology of Taiwan (Grant No. MOST 106-2314-B-350-001-MY3); the Novel Bioengineering and Technological Approaches to Solve Two Major Health Problems in Taiwan program, sponsored by the Taiwan Ministry of Science and Technology Academic Excellence Program (Grant No. MOST 108-2633-B-009-001); the Ministry of Health and Welfare (Grant No. MOHW106-TDU-B-211-113001); and Taipei Veterans General Hospital (Grant Nos. V105C-207, V106C-045, V108C-195, V109B-010, and V109D50-003-MY3-1). The funding institutions took no part in the study design, data collection or analysis, publication intent, or manuscript preparation.
Availability of data and materials
The data sets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of Taipei Veterans General Hospital (no. 2018-02-009AC) and conducted according to the principles expressed in the Declaration of Helsinki. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 2.Yamashita T, Emoto T, Sasaki N, Hirata KI. Gut microbiota and coronary artery disease. Int Heart J. 2016;57(6):663–671. doi: 10.1536/ihj.16-414. [DOI] [PubMed] [Google Scholar]
- 3.Al-Obaide MAI, Singh R, Datta P, Rewers-Felkins KA, Salguero MV, Al-Obaidi I, et al. Gut microbiota-dependent trimethylamine-N-oxide and serum biomarkers in patients with T2DM and advanced CKD. J Clin Med. 2017;6(9):86. doi: 10.3390/jcm6090086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dehghan P, Farhangi MA, Nikniaz L, Nikniaz Z, Asghari-Jafarabadi M. Gut microbiota-derived metabolite trimethylamine N-oxide (TMAO) potentially increases the risk of obesity in adults: an exploratory systematic review and dose-response meta-analysis. Obes Rev. 2020;21(5):e12993. doi: 10.1111/obr.12993. [DOI] [PubMed] [Google Scholar]
- 5.Fu J, Bonder MJ, Cenit MC, Tigchelaar EF, Maatman A, Dekens JA, et al. The gut microbiome contributes to a substantial proportion of the variation in blood lipids. Circ Res. 2015;117(9):817–824. doi: 10.1161/CIRCRESAHA.115.306807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lankelma JM, van Vught LA, Belzer C, Schultz MJ, van der Poll T, de Vos WM, et al. Critically ill patients demonstrate large interpersonal variation in intestinal microbiota dysregulation: a pilot study. Intensive Care Med. 2017;43(1):59–68. doi: 10.1007/s00134-016-4613-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeisel SH, daCosta KA, Youssef M, Hensey S. Conversion of dietary choline to trimethylamine and dimethylamine in rats: dose-response relationship. J Nutr. 1989;119(5):800–804. doi: 10.1093/jn/119.5.800. [DOI] [PubMed] [Google Scholar]
- 8.Sun X, Jiao X, Ma Y, Liu Y, Zhang L, He Y, et al. Trimethylamine N-oxide induces inflammation and endothelial dysfunction in human umbilical vein endothelial cells via activating ROS-TXNIP-NLRP3 inflammasome. Biochem Biophys Res Commun. 2016;481(1–2):63–70. doi: 10.1016/j.bbrc.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368(17):1575–1584. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ottiger M, Nickler M, Steuer C, Bernasconi L, Huber A, Christ-Crain M, et al. Gut, microbiota-dependent trimethylamine-N-oxide is associated with long-term all-cause mortality in patients with exacerbated chronic obstructive pulmonary disease. Nutrition. 2018;45:135–41 e1. doi: 10.1016/j.nut.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Yamashita T, Kasahara K, Emoto T, Matsumoto T, Mizoguchi T, Kitano N, et al. Intestinal immunity and gut microbiota as therapeutic targets for preventing atherosclerotic cardiovascular diseases. Circ J. 2015;79(9):1882–1890. doi: 10.1253/circj.CJ-15-0526. [DOI] [PubMed] [Google Scholar]
- 12.Hai X, Landeras V, Dobre MA, DeOreo P, Meyer TW, Hostetter TH. Mechanism of prominent trimethylamine oxide (TMAO) accumulation in hemodialysis patients. PLoS ONE. 2015;10(12):e0143731. doi: 10.1371/journal.pone.0143731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. doi: 10.1097/00003246-198510000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 16.Chou RH, Chen CY, Chen IC, Huang HL, Lu YW, Kuo CS, et al. Trimethylamine N-oxide, circulating endothelial progenitor cells, and endothelial function in patients with stable angina. Sci Rep. 2019;9(1):4249. doi: 10.1038/s41598-019-40638-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keller U. Nutritional laboratory markers in malnutrition. J Clin Med. 2019;8(6):775. doi: 10.3390/jcm8060775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1):48–79. doi: 10.1016/j.clnu.2018.08.037. [DOI] [PubMed] [Google Scholar]
- 19.McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enter Nutr. 2016;40(2):159–211. [DOI] [PubMed]
- 20.McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enter Nutr. 2009;33(3):277–316. [DOI] [PubMed]
- 21.Sheean PM, Peterson SJ, Chen Y, Liu D, Lateef O, Braunschweig CA. Utilizing multiple methods to classify malnutrition among elderly patients admitted to the medical and surgical intensive care units (ICU) Clin Nutr. 2013;32(5):752–757. doi: 10.1016/j.clnu.2012.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lomivorotov VV, Efremov SM, Boboshko VA, Nikolaev DA, Vedernikov PE, Deryagin MN, et al. Prognostic value of nutritional screening tools for patients scheduled for cardiac surgery. Interact Cardiovasc Thorac Surg. 2013;16(5):612–618. doi: 10.1093/icvts/ivs549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Terekeci H, Kucukardali Y, Top C, Onem Y, Celik S, Oktenli C. Risk assessment study of the pressure ulcers in intensive care unit patients. Eur J Intern Med. 2009;20(4):394–397. doi: 10.1016/j.ejim.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Lew CCH, Yandell R, Fraser RJL, Chua AP, Chong MFF, Miller M. Association between malnutrition and clinical outcomes in the intensive care unit: a systematic review [formula: see text] JPEN J Parenter Enter Nutr. 2017;41(5):744–758. doi: 10.1177/0148607115625638. [DOI] [PubMed] [Google Scholar]
- 25.Kondrup J, Rasmussen HH, Hamberg O, Stanga Z, Ad Hoc EWG. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321–336. doi: 10.1016/S0261-5614(02)00214-5. [DOI] [PubMed] [Google Scholar]
- 26.Lu YW, Lu SF, Chou RH, Wu PS, Ku YC, Kuo CS, et al. Lipid paradox in patients with acute myocardial infarction: potential impact of malnutrition. Clin Nutr. 2019;38(5):2311–2318. doi: 10.1016/j.clnu.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 27.Buzby GP, Williford WO, Peterson OL, Crosby LO, Page CP, Reinhardt GF, et al. A randomized clinical trial of total parenteral nutrition in malnourished surgical patients: the rationale and impact of previous clinical trials and pilot study on protocol design. Am J Clin Nutr. 1988;47(2 Suppl):357–365. doi: 10.1093/ajcn/47.2.357. [DOI] [PubMed] [Google Scholar]
- 28.Hicks KA, Mahaffey KW, Mehran R, Nissen SE, Wiviott SD, Dunn B, et al. 2017 Cardiovascular and stroke endpoint definitions for clinical trials. Circulation. 2018;137(9):961–972. doi: 10.1161/CIRCULATIONAHA.117.033502. [DOI] [PubMed] [Google Scholar]
- 29.Palevsky PM, Liu KD, Brophy PD, Chawla LS, Parikh CR, Thakar CV, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am J Kidney Dis. 2013;61(5):649–672. doi: 10.1053/j.ajkd.2013.02.349. [DOI] [PubMed] [Google Scholar]
- 30.Wu YK, Kao KC, Hsu KH, Hsieh MJ, Tsai YH. Predictors of successful weaning from prolonged mechanical ventilation in Taiwan. Respir Med. 2009;103(8):1189–1195. doi: 10.1016/j.rmed.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 31.Ottiger M, Nickler M, Steuer C, Odermatt J, Huber A, Christ-Crain M, et al. Trimethylamine-N-oxide (TMAO) predicts fatal outcomes in community-acquired pneumonia patients without evident coronary artery disease. Eur J Intern Med. 2016;36:67–73. doi: 10.1016/j.ejim.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 32.Guo JY, Chou RH, Kuo CS, Chao TF, Wu CH, Tsai YL, et al. The paradox of the glycemic gap: does relative hypoglycemia exist in critically ill patients? Clin Nutr. 2021;40(7):4654–4661. doi: 10.1016/j.clnu.2021.06.004. [DOI] [PubMed] [Google Scholar]
- 33.Ma J, Pazos IM, Gai F. Microscopic insights into the protein-stabilizing effect of trimethylamine N-oxide (TMAO) Proc Natl Acad Sci USA. 2014;111(23):8476–8481. doi: 10.1073/pnas.1403224111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gluick TC, Yadav S. Trimethylamine N-oxide stabilizes RNA tertiary structure and attenuates the denaturating effects of urea. J Am Chem Soc. 2003;125(15):4418–4419. doi: 10.1021/ja0292997. [DOI] [PubMed] [Google Scholar]
- 35.Fuke N, Nagata N, Suganuma H, Ota T. Regulation of gut microbiota and metabolic endotoxemia with dietary factors. Nutrients. 2019;11(10):2277. doi: 10.3390/nu11102277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fay KT, Ford ML, Coopersmith CM. The intestinal microenvironment in sepsis. Biochim Biophys Acta. 2017;1863(10 Pt B):2574–83. [DOI] [PMC free article] [PubMed]
- 37.Wang S, Xiao C, Liu C, Li J, Fang F, Lu X, et al. Identification of biomarkers of sepsis-associated acute kidney injury in pediatric patients based on UPLC-QTOF/MS. Inflammation. 2020;43(2):629–640. doi: 10.1007/s10753-019-01144-5. [DOI] [PubMed] [Google Scholar]
- 38.Mafra D, Borges NA, Cardozo L, Anjos JS, Black AP, Moraes C, et al. Red meat intake in chronic kidney disease patients: two sides of the coin. Nutrition. 2018;46:26–32. doi: 10.1016/j.nut.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 39.Boutagy NE, Neilson AP, Osterberg KL, Smithson AT, Englund TR, Davy BM, et al. Short-term high-fat diet increases postprandial trimethylamine-N-oxide in humans. Nutr Res. 2015;35(10):858–864. doi: 10.1016/j.nutres.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 40.Zhang C, Yin A, Li H, Wang R, Wu G, Shen J, et al. Dietary modulation of gut microbiota contributes to alleviation of both genetic and simple obesity in children. EBioMedicine. 2015;2(8):968–984. doi: 10.1016/j.ebiom.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barrea L, Annunziata G, Muscogiuri G, Laudisio D, Di Somma C, Maisto M, et al. Trimethylamine N-oxide, Mediterranean diet, and nutrition in healthy, normal-weight adults: also a matter of sex? Nutrition. 2019;62:7–17. doi: 10.1016/j.nut.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 42.Kaysen GA, Johansen KL, Chertow GM, Dalrymple LS, Kornak J, Grimes B, et al. Associations of trimethylamine N-oxide with nutritional and inflammatory biomarkers and cardiovascular outcomes in patients new to dialysis. J Ren Nutr. 2015;25(4):351–356. doi: 10.1053/j.jrn.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lombardo M, Aulisa G, Marcon D, Rizzo G, Tarsisano MG, Di Renzo L, et al. Association of urinary and plasma levels of trimethylamine N-oxide (TMAO) with foods. Nutrients. 2021;13(5):1426. doi: 10.3390/nu13051426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, et al. Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013;19(5):576–585. doi: 10.1038/nm.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Missailidis C, Neogi U, Stenvinkel P, Troseid M, Nowak P, Bergman P. The microbial metabolite trimethylamine-N-oxide in association with inflammation and microbial dysregulation in three HIV cohorts at various disease stages. AIDS. 2018;32(12):1589–1598. doi: 10.1097/QAD.0000000000001813. [DOI] [PubMed] [Google Scholar]
- 46.Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49–64. doi: 10.1016/j.clnu.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 47.Yin J, Liao SX, He Y, Wang S, Xia GH, Liu FT, et al. Dysbiosis of gut microbiota with reduced trimethylamine-N-oxide level in patients with large-artery atherosclerotic stroke or transient ischemic attack. J Am Heart Assoc. 2015 doi: 10.1161/JAHA.115.002699. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure 1. Plasma TMAO concentrations in patients classified by A reason for hospitalization (sepsis vs. elective CAG) and B sepsis and different severity of CAD. Table 1. Baseline characteristics, TMAO concentrations, and outcomes of septic patients and patients admitted for elective CAG. Table 2. Plasma TMAO concentrations and nutritional indicators of patients classified by different causes of death during hospitalization. Table 3. Univariate and multivariate Cox regression analyses to investigate the relationships between TMAO, septic shock, total bilirubin, enteral intake of calories, enteral intake of protein, total calories, total protein, and non-cardiovascular death among septic patients. Table 4. Univariate and multivariate Cox regression analyses to investigate the relationships between TMAO, disease severity, antibiotic pre-treatment, nutritional risk scores, and non-CV death among septic patients. Table 5. Univariate and multivariate Cox regression analyses of factors associated with weaning success among septic patients
Data Availability Statement
The data sets generated during and analyzed during the current study are available from the corresponding author on reasonable request.