Abstract
Background
We investigated the evolving prevalence of mood and anxiety symptoms among health care workers from May 2020 to January 2021, risk factors for adverse outcomes, and characteristic modes of affective responses to pandemic-related stressors.
Methods
A total of 2307 health care workers (78.9% female, modal age 25–34 years) participated in an online survey assessing depression (Patient Health Questionnaire-9) and anxiety (Generalized Anxiety Disorder-7 scale) symptoms, demographic variables, and self-reported impact of pandemic-related stressors. A total of 334 subjects were reassessed ∼6 months later.
Results
The prevalence of clinically significant depression and anxiety was 45.3% and 43.3%, respectively, and a majority (59.9%–62.9%) of those individuals had persistent significant symptoms at 6-month follow-up. Younger age, female gender, and specific occupations (support staff > nurses > physicians) were associated with increased depressive and anxiety symptoms. The most important risk factors were social isolation and fear of contracting COVID-19. The prevalence of clinically significant mood and anxiety symptoms increased by 39.8% from May 2020 to January 2021. Patient Health Questionnaire-9 and Generalized Anxiety Disorder-7 scores were highly correlated and associated with nearly identical risk factors, suggesting that they are not capturing independent constructs in this sample. Principal component analysis identified seven orthogonal symptom domains with unique risk factors.
Conclusions
Clinically significant mood and anxiety symptoms are highly prevalent and persistent among health care workers, and are associated with numerous risk factors, the strongest of which are related to pandemic stressors and potentially modifiable. Interventions aimed at reducing social isolation and mitigating the impact of fear of infection warrant further study.
Keywords: Anxiety, COVID-19, Depression, Diagnostic heterogeneity, Stress
As an early epicenter of the COVID-19 pandemic, the New York City health care workforce faced the unprecedented demands of caring for a sudden surge in critically ill patients in April and May 2020 while simultaneously managing a variety of pandemic-related stressors at home. Epidemiological surveys have shown that depression and anxiety were common early in the pandemic (1, 2, 3, 4), with rates ranging from 9% to 15% among health care workers in Singapore (2) to 45% to 50% in Wuhan, China, in early 2020 (1). Acute stress disorder and other trauma symptoms were also common, ranging from 10% to 40% for acute stress disorder to >70% for subclinical distress and trauma symptoms (1,5,6). However, most such studies to date have been cross-sectional analyses. Thus, it is unclear to what extent adverse mental health outcomes are sustained within individuals, and whether their prevalence is changing over time. Longitudinal studies tracking outcomes after the 2002 to 2004 severe acute respiratory syndrome epidemic and other large-scale public health crises have documented sustained depression, anxiety, and posttraumatic stress disorder (7, 8, 9, 10, 11, 12, 13), underscoring the need for longitudinal data.
Importantly, individual variability is a consistent feature of all such studies (1,7,12, 13, 14): adverse mental health outcomes occur in some health care workers and first responders but not in others, despite exposure to similar stressors. What explains these individual differences? Previous studies have identified multiple risk factors for depression and anxiety among COVID-19 health care workers, including younger age, female gender, and work role (1, 2, 3, 4,15, 16, 17, 18). Importantly, health care workers are also confronted with a variety of other stressors shared by the general public, including fear of contracting COVID-19, child care, financial difficulties, and social isolation. Relatively few studies have examined the relative importance of pandemic-related stressors and perceptions of risk, both of which are potentially modifiable.
A second approach to understanding individual differences is to examine how symptoms co-occur, a question with relevance for efforts to rethink our diagnostic system (19,20). In large-scale epidemiological studies, mood and anxiety disorders exhibit high comorbidity rates (21, 22, 23, 24). Depression and anxiety symptom scores are at least moderately correlated, but factor analyses in large-scale population studies suggest that they are quantifying independent factors (25, 26, 27). However, it is unclear whether that also applies to affective responses to pandemic stressors, in which symptoms may be more closely related to stressful life events as opposed to other causes. Thus, the extent to which depression and anxiety co-occur and reflect independent constructs is unclear in this context.
Motivated by these questions, we built an online survey platform for quantifying psychiatric symptoms among health care workers using the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) self-report scales and for identifying risk factors for adverse outcomes. Participants who enrolled in May or June were reassessed ∼6 months later. A second goal of this project was to connect health care workers with mental health treatment resources if needed. Numerous studies have shown that depression and anxiety interfere with quality of life and work performance in health care settings (28, 29, 30, 31) and that health care workers may be less likely to access care due to stigma and other barriers to care (32). Thus, participants in our survey received immediate feedback on their depression and anxiety symptom scores, information on how to interpret them, and contact information for immediately accessible counseling, treatment, and other support resources.
This study had three aims. Our first aim was to define the prevalence of clinically significant mood and anxiety symptoms among health care workers in New York City and characterize changes over time in a cross-sectional analysis. Our second aim was to identify risk factors for initial and sustained adverse mental health outcomes in a longitudinal analysis of subjects assessed in spring 2020 and again ∼6 months later. Our third aim was to understand individual differences in affective responses to pandemic stressors by investigating the degree to which the PHQ-9 and GAD-7 scales capture independent constructs. Specifically, we tested 1) the extent to which PHQ-9 and GAD-7 scores were correlated within and across individuals, 2) whether risk factors for depression and anxiety were similar or distinct, and 3) whether principal components analysis could be used to understand individual differences in affective responses.
Methods and Materials
Detailed methodological and sample descriptions are provided in the Supplemental Methods. A brief summary follows.
Participants
A total of 2307 health care workers in an academic medical center participated in an online survey. All health care workers in the institution were eligible to participate, and there were no exclusion criteria. Participation in both assessments was anonymous and confidential. See the Supplemental Methods and Table S1 for demographic data and additional sample details. All procedures were approved by the Weill Cornell Institutional Review Board, and all subjects provided informed consent.
Survey Measures
Baseline Assessment
The primary outcome measures were the PHQ-9 and GAD-7 self-report scales, assessing depression and anxiety, respectively (25,33). To identify risk factors for adverse mental health outcomes, we collected data on age, gender, marital status, occupation, redeployment status, work location, COVID-19 patient contact, remote work status, and five pandemic-related stressors. For detailed descriptions of how these data were ascertained, see the Supplemental Methods.
Follow-up Assessment
A total of 1773 individuals who participated in the survey in May or June 2020 were invited to participate in a follow-up assessment approximately 6 months after the initial assessment. A total of 334 (18.8%) of them agreed to participate in an identical follow-up assessment, and also reported on the use of support resources in the interim.
Statistical Analyses
Wilcoxon rank-sum tests and Kruskal-Wallis analyses of variance (ANOVAs) were used to test for effects of age, gender, and occupation on PHQ-9 and GAD-7 scores in Figure 1, Figure 2, Figure 3. To assess how each factor influenced risk for clinically significant depression or anxiety, PHQ-9 and GAD-7 scores were converted to a binary outcome based on a standard threshold (≥10). We then used a logistic regression model to evaluate the impact of each factor on depression or anxiety risk, while controlling for the confounding influence of other correlated risk factors. Adjusted odds ratios (ORadj) and 95% confidence intervals were calculated for risk factors found to be statistically significant after false discovery rate correction.
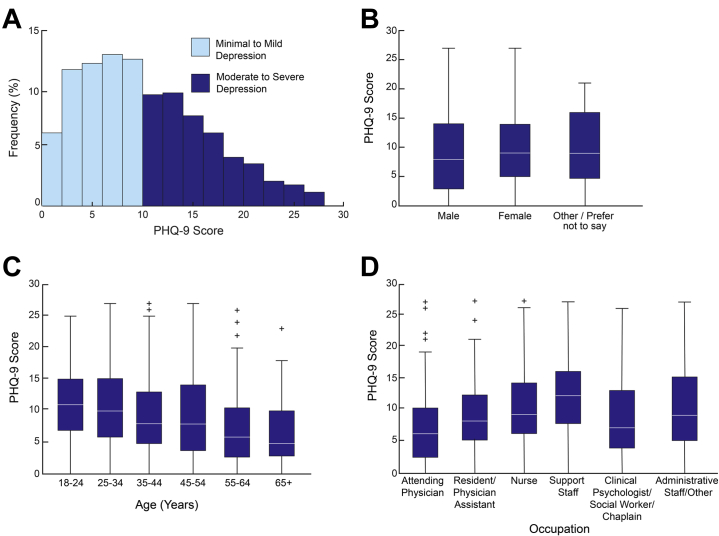
Figure 1.
Patient Health Questionnaire-9 (PHQ-9) depression scores by gender, age, and occupation. (A) Histogram of PHQ-9 depression scores in 2307 health care workers. The prevalence of moderate or severe depression was 45.3% (median PHQ-9 score = 9 [interquartile range, 5–14]). (B) PHQ-9 depression scores were modestly higher in women compared with men (Kruskal-Wallis analysis of variance χ2 = 7.5, p = .024). (C) PHQ-9 scores decreased with age (Kruskal-Wallis analysis of variance χ2 = 95.5, p = 2.18 × 10−18). (D) PHQ-9 depression varied by occupation (Kruskal-Wallis analysis of variance χ2 = 72.6, p = 2.94 × 10−14). Boxplots in panels (B–D) depict median and interquartile range, with whiskers denoting full range excluding outliers (denoted by +).
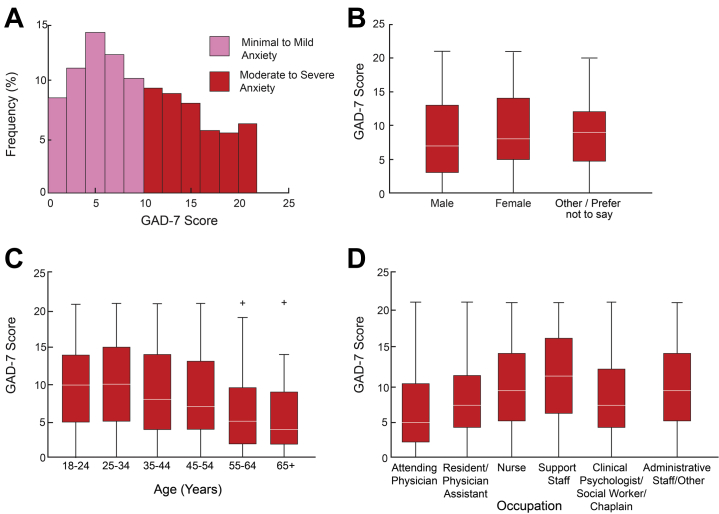
Figure 2.
Generalized Anxiety Disorder-7 (GAD-7) anxiety scores by gender, age, and occupation. (A) Histogram of GAD-7 anxiety scores in 2307 health care workers. The prevalence of moderate or severe anxiety was 43.3% (median GAD-7 score = 9 [interquartile range, 5–14]). (B) GAD-7 anxiety scores were modestly higher in women compared with men (Kruskal-Wallis analysis of variance χ2 = 15.6 p = .004). (C) GAD-7 anxiety scores decreased with age (Kruskal-Wallis analysis of variance χ2 = 138.0, p = 2.61 × 10−27). (D) GAD-7 anxiety scores varied by occupation (Kruskal-Wallis analysis of variance χ2 = 63.1, p = 2.84 × 10−12). Boxplots in (B–D) depict median and interquartile range, with whiskers denoting full range excluding outliers (denoted by +).
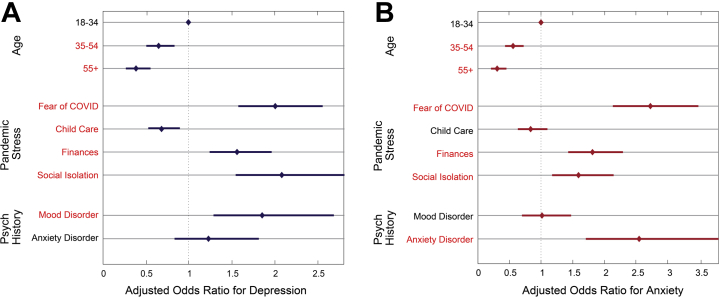
Figure 3.
Adjusted odds ratios for risk factors associated with clinically significant depression and anxiety. Adjusted odds ratios and 95% confidence intervals for statistically significant risk factors for (A) clinically significant depression (Patient Health Questionnaire-9 score ≥10) or (B) clinically significant anxiety (Generalized Anxiety Disorder-7 score ≥10), including age (35–54 years and 55+ years vs. 18–34 years [reference]), four pandemic-related stressors (fear of COVID, child care stress, financial difficulties, social isolation), and past psychiatric history. Adjusted odds ratios were derived from a logistic regression model, adjusting for gender, marital status, occupation, work location, and other variables as described in the Methods and Materials section. Odds ratios for age are reported compared with the 18- to 34-year-old age group as a reference. All other odds ratios are for binary variables. Significant risk factors are listed in red. All other risk factors were not significant. See Methods and Materials for details.
To evaluate how symptom scores changed over time in Figure 4, we first conducted a cross-sectional analysis, calculating the median PHQ-9 or GAD-7 score for all respondents on each day from May 5, 2020, to January 6, 2021. We used a sliding window of ±10 days to calculate a rolling average by day to detect trends on the order of 1–2 weeks while reducing noise due to variability in the number of subjects enrolling on a given day. To test whether changes in PHQ-9 and GAD-7 scores were related to changes in COVID-19 transmission rates, we obtained data on daily new cases from the Centers for Disease Control and Prevention (https://covid.cdc.gov/covid-data-tracker) and computed Pearson correlations between daily new cases and daily mean PHQ-9 and GAD-7 scores. In Figure 5, we used a Wilcoxon signed rank test to determine whether changes in PHQ-9 and GAD-7 scores were statistically significant in the 6-month follow-up assessment.
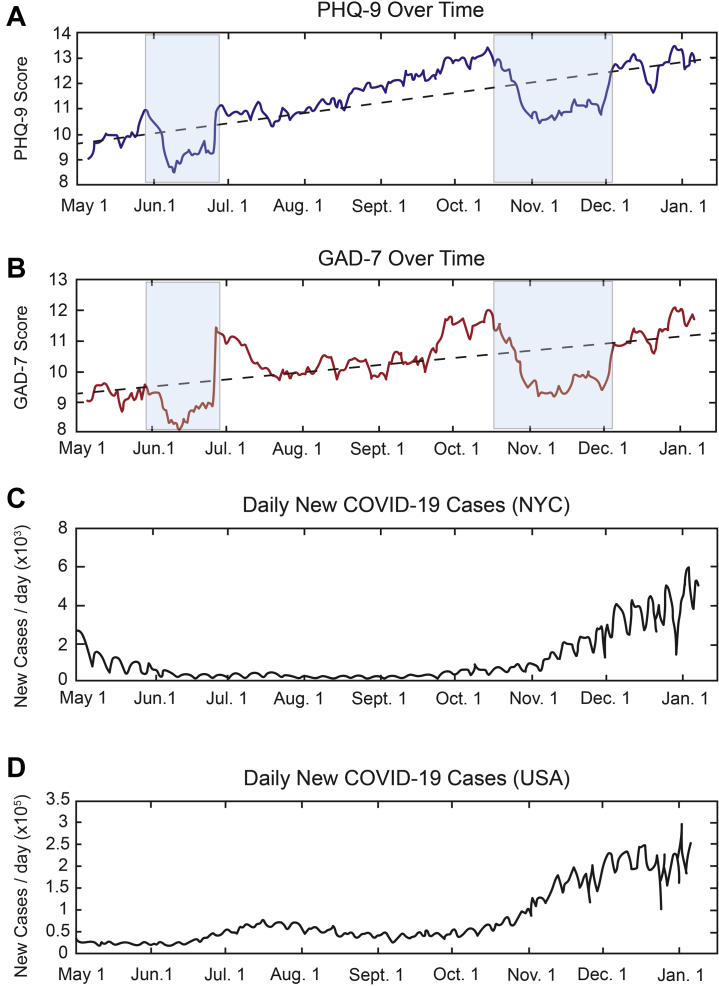
Figure 4.
Changes in depression and anxiety scores over time. (A) Patient Health Questionnaire-9 (PHQ-9) depression scores and (B) Generalized Anxiety Disorder-7 (GAD-7) anxiety scores by time. The data point for each day represents a rolling average of the median PHQ-9 or GAD-7 score across a sliding window of ±10 days, averaging over ∼900–1000 responses for each daily value in May; ∼260–300 subjects in June; ∼90–120 subjects in July; ∼45–60 subjects in August, September, October, and November; and ∼60–80 subjects in December and January. See Methods and Materials for details. Dashed lines represent linear regression of PHQ-9 and GAD-7 scores on time, explaining 53.9% and 31.5% of the variance in daily scores, respectively. The semitransparent blue boxes highlight transient decreases in mean PHQ-9 and GAD-7 symptoms, which correspond with the relaxation of social distancing requirements in New York City (NYC) in June and positive vaccine news in October and November. Changes over time in (C) local and (D) national COVID-19 transmission rates (daily new cases) as defined by the Centers for Disease Control and Prevention (https://covid.cdc.gov/covid-data-tracker).
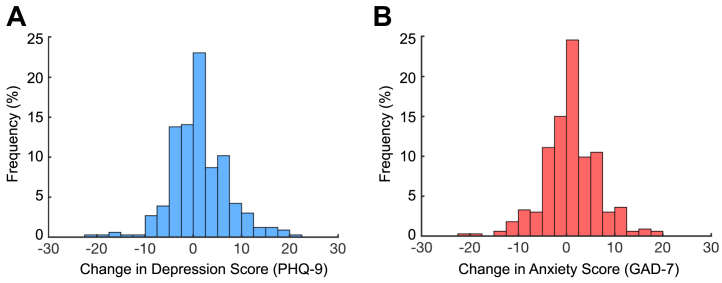
Figure 5.
Sustained depression and anxiety in a 6-month follow-up assessment. Histograms of the change (follow-up score – baseline score) in (A) Patient Health Questionnaire-9 (PHQ-9) depression scores (median = 0 [interquartile range, −2.25 to 4]) and (B) Generalized Anxiety Disorder-7 (GAD-7) anxiety scores (median = 0 [interquartile range, −2 to 4]).
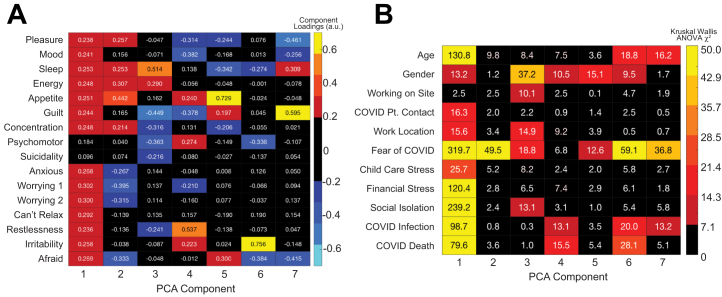
In Figure 6, we used principal component analysis (PCA) to identify a low-dimensional orthogonalized representation of depression and anxiety symptoms and how they covary. We used Kruskal-Wallis ANOVAs to test for effects of age, gender, and each of the nine factors examined in Figure S1 on component scores across individuals.
Figure 6.
Parsing heterogeneity in the affective response to pandemic stressors. Principal component analysis (PCA) identified 7 components explaining 82.0% of the variance in symptoms. (A) Heatmap depicting principal component coefficients (“loadings”) for each clinical symptom in the Patient Health Questionnaire-9 and Generalized Anxiety Disorder-7 scales. (B) Heatmap depicting how individual subject scores for each component varied with age, gender, work-related factors, and pandemic-related stressors. Warm colors denote statistically significant associations (Kruskal-Wallis analysis of variance [ANOVA] χ2, false discovery rate corrected for multiple testing). Pt., patient.
Results
Health care workers in an academic medical center in New York City were invited to participate in an online survey, which was open to enrollment from May 2020 to January 2021. Participants who enrolled in May or June were reassessed ∼6 months later. A total of 3054 individuals clicked on the email link inviting them to participate. A total of 2307 (75.5%) of these individuals completed the initial assessment (78.9% female, age 18–75 years, modal age category 25–34 years). Among the 1773 subjects who participated in May or June 2020, 334 (18.8%) participated in a follow-up assessment approximately 6 months after their initial assessment (described in detail below). In the follow-up assessment, 58.7% reported using at least one support resource listed on the referral page, including 10.5% receiving supportive counseling, 21.0% receiving individual psychotherapy or psychiatric treatment, 25.2% using at least one online resource (e.g., meditation, yoga classes), and 2.1% using group therapy. Table S1 provides additional demographic information on the sample.
Prevalence of Mood and Anxiety Symptoms Early in the Pandemic
We began by assessing the prevalence of clinically significant mood and anxiety symptoms among the 2307-subject sample, as indexed by the PHQ-9 and GAD-7, respectively. The prevalence of moderate or severe depression was 45.3% (median PHQ-9 score = 9 [interquartile range (IQR), 5–14]) (Figure 1A). Consistent with previous studies (1, 2, 3, 4), PHQ-9 depression scores were significantly higher in women compared with men (Kruskal-Wallis ANOVA χ22 = 7.5, p = .024) (Figure 1B) but only modestly so (median PHQ-9 score = 9 [IQR, 5–14] in women vs. 8 [IQR, 3–14] in men and 9 [IQR, 4.75–16] in participants who responded other/prefer not to say). PHQ-9 scores decreased strongly with age (Kruskal-Wallis ANOVA χ26 = 95.5, p = 2.18 × 10−18) (Figure 1C) and varied by occupation (Kruskal-Wallis ANOVA χ25 = 72.6, p = 2.94 × 10−14) (Figure 1D), with the highest scores in support staff (median = 12 [IQR, 7.5–16]) and the lowest scores in attending physicians (median = 6 [IQR, 3–10]).
Anxiety symptoms exhibited similar trends. The prevalence of moderate or severe anxiety was 43.3% (median GAD-7 score = 8 [IQR, 5–14]) (Figure 2A). Again, GAD-7 anxiety scores were significantly higher in women compared with men (median GAD-7 score = 8 [IQR, 5–14] in women vs. 7 [IQR, 3–13] in men and 9 [IQR, 4.75–12] in participants who responded other/prefer not to say; Kruskal-Wallis ANOVA χ22 = 15.6, p = .004) (Figure 2B) and decreased strongly with age (Kruskal-Wallis ANOVA χ26 = 138.0, p = 2.61 × 10−27) (Figure 2C). GAD-7 scores also varied by occupation (Kruskal-Wallis ANOVA χ25 = 63.1, p = 2.84 × 10−12) (Figure 2D).
Risk Factors for Adverse Mental Health Outcomes
To identify risk factors for adverse mental health outcomes among the 2307 health care workers in our initial assessment sample, we performed two analyses. First, we investigated how mood and anxiety symptoms varied continuously with factors associated with COVID-19 exposure risk, fear of contracting COVID-19, and other pandemic-related stressors. Unexpectedly, mood symptoms did not differ among subjects working on site versus at home and varied only modestly with factors related to COVID-19 exposure at work (Figure S1A, B). Mood symptoms varied most strongly with self-reported fear of contracting COVID-19 and with social isolation stress, among other pandemic-related stressors (Figure S1C). Anxiety symptoms exhibited the same patterns (Figure S1D–F).
Importantly, not all factors associated with depression and anxiety were independent. For example, both scores varied with age and occupation, and attending physicians tended to be older than nurses. Thus, we used logistic regression to quantify the independent impact of each risk factor on the likelihood of presenting with clinically significant mood or anxiety (score ≥10), while controlling for the influence of all other variables in our model. The strongest risk factors for clinically significant depression (Figure 3A) were self-reported fear of contracting COVID-19 (ORadj = 2.01), social isolation (ORadj = 2.08), financial difficulties (ORadj = 1.56), and a mood disorder diagnosis history (ORadj = 1.86). Interestingly, while 25.7% of our sample reported feeling “very much” or “extremely” affected by pandemic-related child care difficulties, these participants were significantly less likely to present with significant depressive symptoms (ORadj = 0.68). Older participants (ORadj = 0.39–0.65) were also less likely to be depressed. Neither gender nor any factor related to COVID-19 exposure was significantly associated with risk for depression in this model, after controlling for the influence of other variables. Remarkably similar risk factors were identified for clinically significant anxiety (Figure 3B).
Changes in Mood and Anxiety Symptoms Over Time
To better understand how mood and anxiety symptoms changed over the course of the pandemic, we performed two analyses. First, in a cross-sectional analysis, we found that changes in PHQ-9 and GAD-7 scores were highly correlated over time (r = 0.764, p < 1 × 10−50). Both tended to increase approximately linearly from May 2020 to January 2021, with two exceptions: there was a transient decrease in mean PHQ-9 and GAD-7 scores in June and again from mid-October to late November (Figure 4A, B). Changes in local and national COVID-19 transmission rates were only modestly correlated with changes in mean PHQ-9 and GAD-7 scores, explaining 14.2% to 18.9% of the variance in depression scores and 11.1% to 12.5% of the variance in anxiety scores (Figure 4C, D). In a secondary exploratory analysis, reasoning that health care workers’ awareness of changes in local and national transmission rates may exhibit some delay, we tested whether changes in transmission rates explained changes in mean PHQ-9 and GAD-7 scores after a 7-day delay. Again, we found only modest correlations, explaining 10.9% to 19.8% of the variance in depression scores and 9.3% to 13.4% of the variance in anxiety scores. Instead, changes in PHQ-9 and GAD-7 scores were best explained by a simple linear model predicting gradually increasing scores over time, and explaining 53.9% of the variance in depression scores and 31.5% of the variance in anxiety scores. Overall, the prevalence of clinically significant mood and anxiety symptoms increased from 41.3% and 42.7% in May to 54.7% and 59.7% in December and January, respectively (Figure 4A, B).
Although several studies have reported similarly high rates of depression and anxiety among health care workers early in the pandemic (1,3), relatively few have examined long-term outcomes, so it is unclear whether depression and anxiety symptoms are sustained over prolonged periods within individual subjects. Among the 1773 subjects who enrolled in the study in May or June 2020, 334 participated in a 6-month follow-up assessment. They did not differ significantly with respect to baseline PHQ-9 (p = .528, Wilcoxon rank-sum test) or GAD-7 (p = .161, Wilcoxon rank-sum test) scores, compared with subjects who participated only in the baseline assessment, nor did they differ with respect to age, gender, on-site work status, COVID patient contact, work location, or any pandemic-related stressors (p = .184–.92, Wilcoxon rank-sum test). However, subjects who agreed to participate in the 6-month follow-up assessment were modestly less likely to report being at least somewhat affected by fear of contracting COVID-19 (63.3% vs. 72.5%; p = .0011 by Wilcoxon rank-sum test).
A longitudinal analysis of mental health outcomes among these 334 subjects revealed three findings. First, at the group level, the prevalence of moderate or severe depression or anxiety in the 6-month follow-up assessment was similar to the baseline assessment (Figure S2A, B). Second, a repeated-measures analysis of within-subject changes in symptoms showed that there was a small but statistically significant decrease in both depression (Wilcoxon signed rank test, z = 2.55, p = .011) and anxiety (z = 2.30, p = .021) symptoms after 6 months. However, these effects were small, and the median change on both scales was zero (ΔPHQ-9 median = 0 [IQR, −2.25 to 4], ΔGAD-7 median = 0 [IQR, −2 to 4]). Both PHQ-9 and GAD-7 scores were largely stable over time at the group level but more variable at the individual level, with ∼10% of subjects’ reporting changes in symptoms by 10 to 20 points but most (72.1%) changing by <5 points (Figure 5A, B). Third, this meant that a majority (59.9%–62.9%) of participants with clinically significant depression or anxiety at baseline also had clinically significant depression or anxiety symptoms at follow-up (Figure S2C, D), indicating that sustained, clinically significant depression or anxiety symptoms are a persistent problem in this sample.
Parsing Heterogeneity in the Affective Response to Pandemic Stressors
The GAD-7 and PHQ-9 assessments were designed to screen for and quantify the severity of major depression and generalized anxiety disorder, respectively (25,33). In large-scale validation studies, GAD-7 and PHQ-9 scores were correlated, but factor analysis confirmed distinct dimensions (25). However, it is unclear whether that also applies to affective responses to pandemic stressors in this population, in which symptoms may be more closely related to stressful life events as opposed to other causes. To what extent do these tools quantify independent diagnostic constructs among health care workers during the COVID-19 pandemic? To answer this question, we first analyzed the degree to which depression and anxiety symptoms tended to co-occur within subjects and to covary over time. PHQ-9 and GAD-7 scores were highly correlated in the baseline sample (r = 0.764, p < 1 × 10−50) (Figure S3A) and covaried over time within subjects, such that changes in PHQ-9 scores were highly correlated with changes in GAD-7 scores in the 334-subject follow-up sample (r = 0.681, p = 7.88 × 10−42) (Figure S3B).
Thresholding the scores to identify subjects with clinically significant depression or anxiety revealed high comorbidity rates (Figure S3C). Overall, 80.1% of the sample met criteria for either both diagnoses (PHQ-9 and GAD-7 scores ≥10) or neither diagnosis (PHQ-9 and GAD-7 scores <10). A total of 79.3% of participants with probable GAD also had probable depression, and 75.8% of participants with probable depression also had probable GAD. Furthermore, most of the remaining participants who met criteria for just one diagnosis had subclinical symptoms of the other diagnosis that were just short of the 10-point threshold: 95.6% of participants with probable depression had subthreshold anxiety symptoms (GAD-7 score >7), and 97.2% of participants with probable GAD had subthreshold depression (PHQ-9 score >7). In contrast to previous studies in which depression and anxiety were more independent (25), 67.5% of individuals in our sample with severe anxiety also had severe depression (PHQ-9 score ≥15), and 97.6% had at least subthreshold depression symptoms. These results indicate that the PHQ-9 and GAD-7 scales are not capturing independent constructs in this particular context.
However, there was substantial individual variability in the affective response to pandemic stressors. Participants presented with varying combinations of symptoms from both inventories, and 22.3% reported minimal or absent symptoms in both domains (PHQ-9 score <5, GAD-7 score <5), despite significant stress. To better understand individual differences in affective responses, we used PCA to identify a low-dimensional orthogonalized representation of depression and anxiety symptoms. PCA identified 7 components explaining 82.0% of the variance in symptoms (Figure S3D). Component 1 explained 53.7% of the variance and was defined by modest loadings on almost all symptoms (Figure 6A), in agreement with the observation that PHQ-9 and GAD-7 total scores were highly correlated. However, additional components defined independent symptom domains. For example, component 2 explained 7.8% of the variance and was defined by high levels of anhedonia and neurovegetative depressive symptoms (sleep, energy, appetite) and low levels of anxiety and worrying. Component 3 explained 5.5% of the variance and was defined by high levels of insomnia and anergia and low levels of other depressive symptoms.
Furthermore, whereas PHQ-9 and GAD-7 total scores were associated with nearly identical risk factors (Figure 3), the individual component scores were associated with distinct risk factors (Figure 6B). Component 1, with modest loadings on most symptoms, was associated with the same risk factors that predicted PHQ-9 and GAD-7 total scores in Figure 3. In contrast, component 2 was strongly associated only with self-reported fear of contracting COVID-19 and to a lesser extent with working on site, predicting higher levels of anxiety and worrying and low anhedonia and neurovegetative depressive symptoms. Component 3 was strongly associated with gender and working on site, such that women working on site had high component 3 scores and relatively specific sleep and energy problems, without other depressive symptoms. Components 4 to 7 were likewise associated with specific combinations of risk factors. Thus, while PHQ-9 and GAD-7 total scores are highly effective screening tools for DSM diagnoses, our results indicate that these diagnoses are largely overlapping in COVID-19 health care workers and are not distinct constructs. Data-driven dimensionality reduction techniques offer a complementary approach for understanding heterogeneity in the affective response to pandemic-related stressors and the specific contributions of distinct risk factors.
Discussion
Our results support four key conclusions. First, they demonstrate high prevalence rates for clinically significant depression and anxiety among health care workers in New York City, confirming previous reports from other locations (1, 2, 3, 4). These rates appear to be increasing over time, from 41% to 43% in May to 55% to 60% by the end of 2020. Waxing and waning COVID-19 transmission rates explain some of these changes, but they were best explained by a simple linear model predicting gradual increases over time. Interestingly, there were two exceptions to this long-term trend, marked by transient decreases in depression and anxiety in June and again in mid-October through late November. Our data do not speak to the underlying causes of either the gradually increasing trend over time or these transient dips, but it is noteworthy that they coincide with a relaxation of social distancing requirements in New York City in June and positive vaccine news in late October, respectively.
Second, a major novel feature of this report compared with previous studies is that clinically significant depression and anxiety were sustained in a significant proportion of individuals at the 6-month follow-up assessment. This finding is especially important because few studies have tracked health care workers longitudinally during the pandemic, so it was unclear to what extent these symptoms persist. Our longitudinal data confirm the previously underappreciated point that depression and anxiety symptoms are often highly persistent among health care workers, even 6 months after the peak of the pandemic in New York City. This finding also mirrors results from longitudinal studies of health care workers in the 2002 to 2004 severe acute respiratory syndrome epidemic (8, 9, 10, 11) and first responders in other contexts (7,12, 13, 14), and underscores how adverse mental health outcomes could be sustained problems for a significant proportion of the health care workforce.
Third, individual differences in affective responses were explained in part by multiple risk factors. Confirming previous reports (1, 2, 3, 4,15, 16, 17, 18), they show that younger age, female gender, and specific occupations (nurses and hospital support staff > attending physicians) were associated with a higher risk for both depression and anxiety. Unexpectedly, factors associated with COVID-19 exposure risk—including work location and contact with COVID-19 patients—were only modestly related to symptoms. In contrast, potentially modifiable factors that have not been extensively studied in past work, including fear of contracting COVID-19 and various pandemic-related stressors, especially social isolation and financial difficulties, were much stronger risk factors. At least one previous report found that a lack of social support was strongly associated with depression, generalized anxiety disorder, and posttraumatic stress disorder among health care workers in the pandemic (34).
Fourth, although the GAD-7 and PHQ-9 scales have a useful dynamic range for quantifying affective responses to pandemic stressors, they do not appear to measure fully independent constructs in this population. GAD-7 and PHQ-9 scores were highly correlated both across individuals at a single point in time (r = 0.764) and within individuals assessed repeatedly (r = 0.681). Most individuals with clinically significant depression also had clinically significant anxiety (75.8%) and vice versa (79.3%), and the vast majority (89.8%–93.2%) who screened positively for one diagnosis had at least subthreshold symptoms of the other diagnosis. In previous studies, depression and anxiety scores were also highly correlated, but confirmatory factor analyses have repeatedly identified at least two factors representing depression and anxiety (25, 26, 27). These differences might be explained in part by differences in the populations being studied and the role of pandemic-related stressors versus other factors driving affective responses.
While many studies have confirmed that the PHQ-9 and GAD-7 are highly effective screening tools for major depression and generalized anxiety disorder (25,33), our results suggest that these DSM diagnoses do not capture independent affective responses to pandemic stressors—a conclusion supported by markedly high comorbidity rates (21, 22, 23) and diagnostic instability over time in recent longitudinal studies (24). PCA identified seven orthogonal components explaining 82% of the variance in our sample. The first component was defined by modest loadings on almost all symptoms, consistent with the conclusion that the affective response to pandemic stress involves correlated changes in both scales in many individuals, and this component shared most of the same risk factors that were identified for both depression and anxiety in Figure 3. Importantly, however, this component explained only about half the variance in the sample. The remaining components were defined by distinct clinical symptom domains (e.g., anhedonia and neurovegetative symptoms in component 2, sleep and energy in component 3, restlessness and irritability in component 4) and were associated with distinct risk factors. These findings lend support to current efforts to use PCA and related data-driven approaches to understand individual differences in affective responses independent of our existing diagnostic categories (35, 36, 37, 38, 39).
Several limitations should also be noted. First, our results may be affected by selection biases. Our sample of 2307 health care workers is large, encompassing most health care occupations and a wide range of ages, but it is not a random sample—subjects self-selected for participation—and may not be representative of all health care workers. Likewise, the 334 subjects who agreed to participate in the 6-month follow-up assessment constituted 18.8% of the 1773 subjects who were eligible, so the longitudinal outcomes may not be representative of the sample as a whole. Mitigating these concerns, our prevalence estimates in May 2020 at the height of the crisis in New York City are remarkably similar to those reported in Wuhan in January 2020. Subjects in the 6-month follow-up assessment did not differ systematically from subjects lost to follow-up on most baseline demographic and clinical measures. Still, selection biases could have influenced our results, and may account in part for the fact that the gender effects in our sample (which was 78.9% female) were smaller than those observed in other reports. Second, participants in the initial assessment received feedback on their symptom scores and treatment referral information. A total of 58.7% of participants in the 6-month follow-up assessment reported using at least one of these resources. To the extent that counseling and other treatments improve symptoms, our follow-up assessment may underestimate the prevalence of sustained mood and anxiety disorders in individuals who are not in treatment. Estimates of the evolving prevalence of depression and anxiety may also be less stable for our sample in late 2020, when each daily data point was a rolling average of ∼60 to 80 subjects, compared with in May and June, when each daily data point was a rolling average of ∼260 to 1000 subjects. Third, our data do not speak to the prevalence of trauma symptoms and substance use disorders, which have been documented in recent studies (1, 2, 3,15,34). Finally, we did not assess individual psychological and personality characteristics or factors such as race and ethnicity, education, and socioeconomic status, all of which could influence mood and anxiety and their maintenance over time. Future studies will be needed to address these questions.
These limitations notwithstanding, our findings add to a growing literature indicating that depression, anxiety, and other psychiatric disorders are a significant—and possibly growing—problem among health care workers during the pandemic (1, 2, 3, 4). Other studies confirm that pandemic stress effects on depression and anxiety are not limited to health care workers and may be comparably prevalent in the general population (40,41). Combined with other recent studies (34), they suggest that interventions aimed at potentially modifiable risk factors—including social isolation and fear of contracting COVID-19—are worth investigating. Finally, our results indicate that PCA and other data-driven approaches may be useful for parsing heterogeneity and understanding individual differences in affective responses to pandemic-related stressors.
Acknowledgments and Disclosures
This work was supported by the National Institute of Mental Health (Grant Nos. MH109685 [to CL], MH118451 [to CL], MH118388 [to CL], and MH123154 [to CL]), the National Institute on Drug Abuse (Grant No. DA047851 [to CL]), the Rita Allen Foundation (to CL), and the Hope for Depression Research Foundation (to CL).
CL serves on the Scientific Advisory Board of Delix Therapeutics and has formerly served as a consultant to Compass, PLC. All other authors report no biomedical financial interests or potential conflicts of interest.
Footnotes
Supplementary material cited in this article is available online at https://doi.org/10.1016/j.bpsgos.2021.08.008.
Contributor Information
Benjamin Zebley, Email: bez2005@med.cornell.edu.
Conor Liston, Email: col2004@med.cornell.edu.
Supplementary Material
References
- 1.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan B.Y.Q., Chew N.W.S., Lee G.K.H., Jing M., Goh Y., Yeo L.L.L., et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173:317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., Rossi A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benfante A., Di Tella M., Romeo A., Castelli L. Traumatic stress in healthcare workers during COVID-19 pandemic: A review of the immediate impact. Front Psychol. 2020;11:569935. doi: 10.3389/fpsyg.2020.569935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Serrano-Ripoll M.J., Meneses-Echavez J.F., Ricci-Cabello I., Fraile-Navarro D., Fiol-deRoque M.A., Pastor-Moreno G., et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J Affect Disord. 2020;277:347–357. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagamine M., Giltay E.J., Shigemura J., van der Wee N.J., Yamamoto T., Takahashi Y., et al. Assessment of factors associated with long-term posttraumatic stress symptoms among 56 388 first responders after the 2011 Great East Japan Earthquake. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.18339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bai Y., Lin C.-C., Lin C.-Y., Chen J.-Y., Chue C.-M., Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55:1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- 9.Chua S.E., Cheung V., Cheung C., McAlonan G.M., Wong J.W.S., Cheung E.P.T., et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004;49:391–393. doi: 10.1177/070674370404900609. [DOI] [PubMed] [Google Scholar]
- 10.McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W.T., Sham P.C., et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 11.Lancee W.J., Maunder R.G., Goldbloom D.S., Coauthors for the Impact of SARS Study Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv. 2008;59:91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zvolensky M.J., Kotov R., Schechter C.B., Gonzalez A., Vujanovic A., Pietrzak R.H., et al. Post-disaster stressful life events and WTC-related posttraumatic stress, depressive symptoms, and overall functioning among responders to the World Trade Center disaster. J Psychiatr Res. 2015;61:97–105. doi: 10.1016/j.jpsychires.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Smid G.E., Mooren T.T.M., van der Mast R.C., Gersons B.P.R., Kleber R.J. Delayed posttraumatic stress disorder: Systematic review, meta-analysis, and meta-regression analysis of prospective studies. J Clin Psychiatry. 2009;70:1572–1582. doi: 10.4088/JCP.08r04484. [DOI] [PubMed] [Google Scholar]
- 14.Neria Y., Nandi A., Galea S. Post-traumatic stress disorder following disasters: A systematic review. Psychol Med. 2008;38:467–480. doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rossi R., Socci V., Pacitti F., Mensi S., Di Marco A., Siracusano A., Di Lorenzo G. Mental health outcomes among healthcare workers and the general population during the COVID-19 in Italy. Front Psychol. 2020;11:608986. doi: 10.3389/fpsyg.2020.608986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen J., Liu X., Wang D., Jin Y., He M., Ma Y., et al. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc Psychiatry Psychiatr Epidemiol. 2021;56:47–55. doi: 10.1007/s00127-020-01954-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Insel T., Cuthbert B., Garvey M., Heinssen R., Pine D.S., Quinn K., et al. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 20.Casey B.J., Craddock N., Cuthbert B.N., Hyman S.E., Lee F.S., Ressler K.J. DSM-5 and RDoC: Progress in psychiatry research? Nat Rev Neurosci. 2013;14:810–814. doi: 10.1038/nrn3621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler R.C., Berglund P., Demler O., Jin R., Koretz D., Merikangas K.R., et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 22.Merikangas K.R., Akiskal H.S., Angst J., Greenberg P.E., Hirschfeld R.M.A., Petukhova M., Kessler R.C. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry. 2007;64:543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krueger R.F. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 24.Caspi A., Houts R.M., Ambler A., Danese A., Elliott M.L., Hariri A., et al. Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the Dunedin Birth Cohort Study. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 26.Bjelland I., Dahl A.A., Haug T.T., Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 27.Lovibond P.F., Lovibond S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 28.Pereira-Lima K., Mata D.A., Loureiro S.R., Crippa J.A., Bolsoni L.M., Sen S. Association between physician depressive symptoms and medical errors: A systematic review and meta-analysis. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.16097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kalmbach D.A., Fang Y., Arnedt J.T., Cochran A.L., Deldin P.J., Kaplin A.I., Sen S. Effects of sleep, physical activity, and shift work on daily mood: A prospective mobile monitoring study of medical interns. J Gen Intern Med. 2018;33:914–920. doi: 10.1007/s11606-018-4373-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang Y., Forger D.B., Frank E., Sen S., Goldstein C. Day-to-day variability in sleep parameters and depression risk: A prospective cohort study of training physicians. NPJ Digit Med. 2021;4:28. doi: 10.1038/s41746-021-00400-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosen T., Zivin K., Eisenberg D., Guille C., Sen S. The cost of depression-related presenteeism in resident physicians. Acad Psychiatry. 2018;42:84–87. doi: 10.1007/s40596-017-0867-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Center C., Davis M., Detre T., Ford D.E., Hansbrough W., Hendin H., et al. Confronting depression and suicide in physicians: A consensus statement. JAMA. 2003;289:3161–3166. doi: 10.1001/jama.289.23.3161. [DOI] [PubMed] [Google Scholar]
- 33.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hennein R., Mew E.J., Lowe S.R. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS One. 2021;16 doi: 10.1371/journal.pone.0246602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Drysdale A.T., Grosenick L., Downar J., Dunlop K., Mansouri F., Meng Y., et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2016;23:28–38. doi: 10.1038/nm.4246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xia C.H., Ma Z., Ciric R., Gu S., Betzel R.F., Kaczkurkin A.N., et al. Linked dimensions of psychopathology and connectivity in functional brain networks. Nat Commun. 2018;9:3003. doi: 10.1038/s41467-018-05317-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grosenick L., Shi T.C., Gunning F.M., Dubin M.J., Downar J., Liston C. Functional and optogenetic approaches to discovering stable subtype-specific circuit mechanisms in depression. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4:554–566. doi: 10.1016/j.bpsc.2019.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mihalik A., Ferreira F.S., Rosa M.J., Moutoussis M., Ziegler G., Monteiro J.M., et al. Brain-behaviour modes of covariation in healthy and clinically depressed young people. Sci Rep. 2019;9:11536. doi: 10.1038/s41598-019-47277-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Price R.B., Lane S., Gates K., Kraynak T.E., Horner M.S., Thase M.E., Siegle G.J. Parsing heterogeneity in the brain connectivity of depressed and healthy adults during positive mood. Biol Psychiatry. 2017;81:347–357. doi: 10.1016/j.biopsych.2016.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.