Abstract
Background
Many COVID-19 survivors reported stigmatization after recovery. This study investigated the association between stigma (discrimination experiences, self-stigma and perceived affiliate stigma) and sleep quality among COVID-19 survivors six months after hospital discharge.
Methods
Participants were recovered adult COVID-19 survivors discharged between February 1 and April 30, 2020. Medical staff of five participating hospitals approached all discharged COVID-19 period during this period. A total of 199 participants completed the telephone interview during July to September, 2020. Structural equation modeling was performed to test the hypothesize that resilience and social support would mediate the associations between stigma and sleep quality.
Results
The results showed that 10.1% of the participants reported terrible/poor sleep quality, 26.1% reported worse sleep quality in the past week when comparing their current status versus the time before COVID-19. After adjusting for significant background characteristics, participants who had higher number of discrimination experience, perceived stronger self-stigma and stronger perceived affiliate stigma reported poorer sleep quality. Resilience and social support were positively and significantly associated with sleep quality. The indirect effect of self-stigma on sleep quality through social support and resilience was significant and negative. Perceived affiliate stigma also had a significant and negative indirect effect on sleep quality through social support and resilience.
Conclusions
Various types of stigma after recovery were associated with poor sleep quality among COVID-19 survivors, while social support and resilience were protective factors. Resilience and social support mediated the associations between self-stigma/perceived affiliate stigma and sleep quality.
Keywords: COVID-19 survivors, Sleep quality, Stigma, Resilience, Social support, China
1. Introduction
COVID-19 survivors encountered serious COVID-19 related stigma [[1], [2], [3], [4], [5]]. Disease characteristics (eg high infectivity, severe consequences, long incubation period, large number of asymptomatic patients, and survivors testing to be positive again for SARS-Cov-2 after recovery) as well as serious infodemic trigger great fear of COVID-19 among the general public [[6], [7], [8]]. Moreover, information exposure about the spread of the disease caused by non-compliance to the control measures may cause general public linked COVID-19 patients with negative stereotypes (eg, irresponsibility or lack of moral sense) [[6], [7], [8]]. People tend to avoid and isolate groups who are at risk of COVID-19 transmission (eg, people coming from epidemic centers, healthcare workers, COVID-19 survivors) [8]. Although the original purposes of these avoidance behaviors are for disease prevention, they may end up with discrimination and stigma against specific groups of people [9,10].
Similar to survivors of previous infectious diseases outbreak (eg, SARS, Ebola, and H1N1) [5], many COVID-19 survivors reported stigmatization after recovery. Studies in Nepal, India and Saharan Africa reported that COVID-19 survivors experienced avoidance from other people after recovery, difficulties in service utilization and employment, and being insulted, shunned, marginalized, and rejected in other aspects of their lives [[1], [2], [3], [4]]. In China, some COVID-19 survivors experienced difficulties in employment (eg, denied for job interview or fired without reasons), housing (eg, landlords refused to rent them a place or being rejected by the communities) and relationship with others (eg, avoidance from family, friends and neighbors, and verbal abuse and harassment) [7]. Moreover, there have been intentionally exposure of COVID-19 survivors' personal information (eg, identity, telephone number, and address) [7]. COVID-19 survivors may endorse these negative reactions from the public, devalue themselves, and socially withdraw, which is referred to as internalized stigma or self-stigma [11,12]. Stigma not only affects COVID-19 survivors but also those who are associated with them (eg, their family members). Such stigma-in-association has been labeled as courtesy stigma, which refers to the perceived or experienced stigma against COVID-19 survivors’ associates originated from the general public. The internalization of stigma among COVID-19 survivors is defined as perceived affiliate stigma [13,14]. According to the minority stress model, internalized stigma is proximal minority stress and the most adverse consequence of being socially excluded and discriminated [15,16]. Two meta-analysis studies revealed that internalized stigma have a significant negative effect on both mental and physical health [17,18] and is related to participation in unhealthy and nonparticipation in healthy behaviors [17].
Good sleep is part of good quality of life. High quality and efficient sleep of adequate duration helps to consolidate memory, regulate the immune system, and coordinate neuroendocrine functions [19,20]. In contrast, poor sleep quality leads to a board range of adverse outcomes, including cardiovascular diseases, poor mental health status, cognitive impairment, and even overall mortality [21,22]. Emerging evidences showed poor sleep quality among COVID-19 survivors after hospital discharge [23,24]. The results showed that 29.5% of COVID-19 survivors in Wuhan, China were bothered by sleeping disorder [23], while 40% of COVID-19 survivors in Italy reported insomnia [24]. Self-stigma was associated with poor sleep quality among people living with HIV [25]. To our knowledge, there was a lack of studies investigating the association between stigma and sleep quality among COVID-19 survivors.
Resilience is a personal protective factor, and refers to a stable trajectory of healthy functioning across time following adversity, which includes the capacity for the processes of generative experiences, cognitive flexibility, and positive emotions [26]. Resilience has been suggested to facilitate the “recovery” process for individuals to return to the state before trauma and enhance their mental health [27]. One study reported negative associations between resilience and poor mental health status among COVID-19 patients [28]. Social support from important others (eg, family members and friends) may be vital external resources for survivors to cope with their stress and negative events. It is also a key source of resilience that can facilitate individuals’ mental health [29]. The authors identified three studies investigating the association between social support and mental health among COVID-19 patients [23,30,31]. Only one study was conducted among COVID-19 survivors, and reported a significant negative association between social support and post-traumatic stress disorders [32]. Resilience and social support are potentially important protective factors of sleep quality among different population [[33], [34], [35], [36], [37], [38]], including general population during COVID-19 pandemic [38]. Researchers suggested that COVID-19-related stigma would lead to overall decreased resilience and social support [39,40]. Mediating effects of social support and resilience on the associations between encountering adverse situations and their outcomes were demonstrated in numerous studies. For instance, two studies revealed their mediating effects on the associations between COVID-19-related stressful experiences and acute stress disorder among Chinese college students [41], and between COVID-19-related fear and mental health (eg depression, anxiety and stress) among Turkish healthcare professionals [42]. In addition, mediation role of social support and resilience on the association between stigma and mental health was also shown in different groups of patients and minorities, such as people living with HIV [43,44], schizophrenic patients [45] transgender and cisgender sexual minorities [46].
In this study, we investigated the association between stigma (discrimination experiences, self-stigma and perceived affiliate stigma) and sleep quality among COVID-19 survivors six months after hospital discharge. We also hypothesized that resilience and social support would mediate the associations between stigma and sleep quality.
2. Methods
2.1. Study design
This is a secondary analysis of a cross-sectional telephone survey investigating mental health status of COVID-19 survivors six months after hospital discharge. A total of 199 COVID-19 survivors completed the telephone interview during July to September, 2020.
2.2. Study sites
Five hospitals located in five cities in China (Wuhan, Shenzhen, Zhuhai, Dongguan and Nanning) were included as study sites. Among the five cities, Wuhan is the most affected by the pandemic whereas Nanning is the least affected. Shenzhen, Zhuhai, Dongguan had the moderate level of case load. As of November 9, 2020, the number of recovered COVID-19 patients in these Chinese cities was 46,475 in Wuhan, 72 in Nanning, 468 in Shenzhen, 109 in Zhuhai, and 100 in Dongguan [47].
2.3. Participants and data collection
Inclusion criteria were: 1) aged at least 18 years, 2) receiving confirmatory diagnosis of COVID-19, 3) being hospitalized, and 4) discharged from hospitals between February 1 and April 30, 2020. According to the COVID-19 treatment guidelines in China, recovered COVID-19 patients should be quarantined for 28 days after hospital discharge (14 days in designated facilities followed by another 14-day home-based quarantine). Medical staff who were responsible for following up discharged COVID-19 patients contacted all COVID-19 patients who were discharged between February 1 and April 30, 2020 listed in their registries. Prospective participants were screened for eligibility to join the study by the medical staff. There were 317 recovered COVID-19 patients in the registries of the five hospitals. Among these recovered patients, 27 were under 18 years old, 22 changed their telephone number, 1 deceased in car accident, and 68 refused to join the study. Consequently, a total of 199 eligible patients provided consent and completed the study. The response rate of the five study sites ranged from 63.3% to 77.8% and the overall response rate was 74.5% (199/267).
The participants were briefed about the study information and invited for a telephone interview by the medical staff. Verbal informed consent was obtained, witnessed and formally recorded. Participants were assured that identifiable information would be kept confidential, and withdrawal from study would not affect their right to use any treatment services. Trained interviewers made appointments with the participants and confirmed their informed consent before conducting the telephone interview. Each interview lasted about 35 min. The study was conducted in accordance with the Declaration of Helsinki of 1975, as revised in 2008, and the protocol was approved by the Sun Yat-sen University (Shenzhen) (Ref#2020-031).
2.4. Measures
2.4.1. Development of the questionnaire
A panel consisting of one epidemiologist, two public health researchers, a health psychologist, and a clinician was formed to develop the questionnaire used in the current study.
2.4.2. Background characteristics
Participants were asked to report on socio-demographics, such as age, gender, permanent residency status, highest educational level, relationship status, monthly personal income, employment status, and whether having a child. Characteristics of SARS-Cov-2 infection were retrieved from their medical records, including severity level of COVID-19 at hospital admission, days in hospital, ICU admission, and the use of invasive ventilation and corticosteroid therapy. In addition, participants were asked whether they had family member(s) with COVID-19 or died of COVID-19. Participants also reported mental health support services utilization during hospitalization and after hospital discharge.
2.4.3. Sleep quality
Global sleep quality over a 7-day recall period was assessed based on participants’ rating by using the validated single-item Sleep Quality Scale (SQS) (from 0 to 10), with higher score indicating better sleep quality [48]. Different cut-off scores were assigned for different levels of sleep quality (0 = terrible, 1–3 = poor, 4–6 = fair, 7–9 = good, and 10 = excellent) [48]. Compared with lengthier sleep questionnaires [eg, the Pittsburgh Sleep Quality Index (PSQI), and the Morning Questionnaire-insomnia (MQI)], this scale possessed favorable measurement characteristics to assess sleep quality [48]. This scale has been used in numerous published studies which included those conducted among Chinese populations and it was shown to be a reliable and valid measure [[49], [50], [51], [52], [53]]. Participants were also instructed to compare their current sleep quality with that before SARS-Cov-2 infection based on the following response categories: 1 = get worse, 2 = no change, 3 = get better. Furthermore, whether participants were bothered by sleep disorders was assessed by one item extracted from the PHQ-9 scale [54]. This item asked participants whether they had trouble falling or staying asleep, or sleeping too much in the past two weeks based on the following response categories: not at all, several days, more than half the days, and nearly every day.
2.4.4. Discrimination experience, self-stigma and perceived affiliate stigma
Participants were asked whether they had the following discrimination experiences, including being fired, being treated unfairly by employers, being socially excluded by co-workers, family members, friends, and neighbors/communities, being discriminated by healthcare providers, and whether there is someone who intentionally disclose their COVID-19 survivor identity (0 = no and 1 = yes). A composite indicator variable was constructed by counting the number of discrimination experience (ranging from 0 to 8).
Self-stigma was measured by the validated Chinese version of the Self-Stigma Scale [55]. Sample items included “I fear that others would know that I was infected with SARS-Cov-2”. Items were rated on Likert scale from 1 (strongly disagree) to 4 (strongly agree). The Cronbach's alpha was 0.94. One factor was identified by exploratory factor analysis, explaining for 67.3% of total variance.
A 22-item Affiliate Stigma Scale was developed and validated in Chinese population to measure the extent of self-stigmatization among associates of a targeted minority (eg, those with intellectual disability, mental illness, or HIV/AIDS) [56]. This scale measured cognitive (7 items), affective (7 items), and behavioral (8 items) dimensions of affiliate stigma. Due to the limited length of the questionnaire, we modified and used the affective dimension to measure perceived affiliate stigma among their family members. Sample items included “Your family members would feel inferior because you had infected with SARS-Cov-2”. The scale had excellent reliability in the current sample (Cronbach's alpha: 0.94). One factor was identified by exploratory factor analysis, explaining for 73.7% of total variance.
2.4.5. Resilience and social support
Resilience was measured by the 2-item Connor-Davidson Resilience Scale (CD-RISC2) [57]. The two items (“Able to adapt to change” and “Tend to bounce back after illness or hardship”) are rated on Likert scales, ranging from 1 (strongly disagree) to 5 (strongly agree). A higher total score indicates a higher level of psychological resilience. The Cronbach's alpha of the scale was 0.89 in the current sample. One factor was identified by exploratory factor analysis, explaining for 90.3% of total variance.
Social support was measured by four questions to measure the extent of received emotional and instrumental (eg financial) support from family and friends [29]. Items were rated on a 10-point Likert Scale ranging from 0 (none) to 10 (tremendous). The scale had good reliability in the current sample (Cronbach's alpha: 0.80). One factor was identified by exploratory factor analysis, explaining for 62.8% of total variance.
2.5. Statistical analysis
Global sleep quality measured by score of the single-item SQS was used as the dependent variable. The associations between independent variables of interest (discrimination experience, self-stigma, perceived affiliate stigma, resilience and social support) and the dependent variable were tested using multivariate linear regression models, after adjusted for significant background characteristics. Adjusted unstandardized coefficients (B) and their 95% confidence interval (CI) were reported.
Structural equation modeling (SEM) was performed to test the proposed mediation model. Bootstrapping analyses were used to test the mediation effects. All significant background characteristics were controlled for in the model. Discrimination experience, self-stigma, and perceived affiliate stigma were covariated. Goodness of fit was tested by using the chi-square tests, the Comparative Fit Index (CFI), the Non-Normed Fit Index (NNFI), and the root mean square error of approximation (RMSEA). A CFI and NNFI greater than 0.90 and RMSEA lower than 0.08 indicated acceptable goodness to fit [58]. Standardized path coefficients (β) and unstandardized path coefficients (B) were reported. SPSS version 24.0 (IBM Corporation) and AMOS was used to conduct all analyses, with a P value < 0.05 indicating statistical significance.
3. Results
3.1. Background characteristics
Slightly more than half of the participants were female (53.3%, n = 106) and aged 41 years or older (53.8%, n = 107). Regarding highest education attained, 43.2% of the participants attained college education (n = 86), while 28.6% for senior high school (n = 57) and 26.6% for junior high school or below (n = 53). For employment status, 40.2% of the participants were full-time employed (n = 80), 16.1% were freelancers (n = 31), 7.5% were students (n = 15), 27.6% were retired (n = 55), and 8.5% were unemployed (n = 17). Most of the participants were married or cohabited with a partner (81.9%, n = 163), without permanent residency of the city (73.4%, n = 146), with personal income less than RMB 6000 (approximately USD 900) per month (74.4%, n = 148), and having at least one child (80.4%, n = 160).
According to their medical record, 55.8% of participants were at moderate level of severity at hospital admission (n = 111), 57.3% spent no more than 28 days in hospital (n = 114), 97.5% without ICU admission (n = 194), and 96.5% and 87.9% did not undergo invasive ventilation (n = 192) or corticosteroid therapy (n = 175). Among the participants, 44.7% (n = 89) reported having at least one family member infected with COVID-19, and 1.5% (n = 3) had a family member died of COVID-19.
Less than half of the participants received mental health support services during hospitalization (n = 85, 42.7%) or after discharge (n = 44, 22.1%) (Table 1 ).
Table 1.
Background characteristics of the participants (n = 199).
| n | % | |
|---|---|---|
| Socio-demographics | ||
| Age group (years) | ||
| 18–30 | 33 | 16.6 |
| 31–40 | 59 | 29.6 |
| 41–50 | 35 | 17.6 |
| 51–60 | 33 | 16.6 |
| >60 | 39 | 19.6 |
| Gender | ||
| Male | 93 | 46.7 |
| Female | 106 | 53.3 |
| Relationship status | ||
| Currently single | 36 | 18.1 |
| Married/cohabited with a partner | 163 | 81.9 |
| Permanent resident of the city | ||
| No | 146 | 73.4 |
| Yes | 53 | 26.6 |
| Having at least one child | ||
| No | 39 | 19.6 |
| Yes | 160 | 80.4 |
| Employment status | ||
| Full-time employment | 80 | 40.2 |
| Freelancer | 31 | 16.1 |
| Student | 15 | 7.5 |
| Retiree | 55 | 27.6 |
| Unemployed | 17 | 8.5 |
| Monthly personal income (RMB) | ||
| No stable income | 71 | 35.7 |
| <3000 | 25 | 12.6 |
| 3000–5999 | 52 | 26.1 |
| 6000–9000 | 24 | 12.1 |
| ≥10,000 | 27 | 13.6 |
| Highest education attained | ||
| Junior high or below | 53 | 26.6 |
| Senior high | 57 | 28.6 |
| College and above | 86 | 43.2 |
| Refuse to disclose | 3 | 1.5 |
| Variables related to SARS-Cov-2 infection | ||
| Severity level of COVID-19 at hospital admission | ||
| Asymptomatic | 3 | 1.5 |
| Mild | 42 | 21.1 |
| Moderate | 111 | 55.8 |
| Severe | 24 | 12.1 |
| Critical | 1 | 0.5 |
| No record | 18 | 9.0 |
| Days in hospital (days) | ||
| ≤14 | 22 | 11.1 |
| 15–28 | 92 | 46.2 |
| 29–42 | 49 | 24.6 |
| >42 | 11 | 5.5 |
| No record | 25 | 12.6 |
| ICU admission | ||
| No | 194 | 97.5 |
| Yes | 5 | 2.5 |
| Undergo invasive ventilation | ||
| No | 192 | 96.5 |
| Yes | 7 | 3.5 |
| Undergo corticosteroid therapy | ||
| No | 175 | 87.9 |
| Yes | 24 | 12.1 |
| Having a family member infected with COVID-19 | ||
| No | 110 | 55.3 |
| Yes | 89 | 44.7 |
| Having a family member died of COVID-19 | ||
| No | 196 | 98.5 |
| Yes | 3 | 1.5 |
| Mental health service utilization | ||
| Receiving mental health support services during hospitalization | ||
| No | 114 | 57.3 |
| Yes | 85 | 42.7 |
| Receiving mental health support services after hospital discharge | ||
| No | 155 | 77.9 |
| Yes | 44 | 22.1 |
3.2. Sleep quality
The mean score of global sleep quality measured by the single-item SQS was 6.9 (SD: 2.3), with 10.1% of the participants reported terrible/poor sleep quality (n = 20) and 26.6% reported fair sleep quality in the past week (n = 53). When comparing their current status with that before SARS-Cov-2 infection, 26.1% of the participants reported worse sleep quality (n = 52) and 72.9% reported no change (n = 145). Concerning whether they were bothered by sleeping disorder in the past two weeks, 19.6% of the participants reported several days (n = 39), 7.0% reported more than half the days (n = 14) and another 7% reported nearly every day (n = 14) (Table 2 ).
Table 2.
Sleep quality and other psychosocial variables among the participants (n = 199).
| n (%) | Mean (SD) | |
|---|---|---|
| Sleep quality | ||
| Score of the single-item sleep quality scale (SQS) | 6.9 (2.3) | |
| Terrible (0) | 3 (1.5) | |
| Poor (1–3) | 17 (8.5) | |
| Fair (4–6) | 53 (26.6) | |
| Good (7–9) | 108 (54.2) | |
| Excellent (10) | 18 (9.0) | |
| Whether you have trouble falling or staying asleep, or sleeping too much in the past two weeks (an item of the PHQ-9) | ||
| Not at all | 132 (66.3) | |
| Several days | 39 (19.6) | |
| More than half the days | 14 (7.0) | |
| Nearly every day | 14 (7.0) | |
| Self-reported change in sleep quality comparing current status with that before COVID-19 | ||
| Got worse | 52 (26.1) | |
| No change | 145 (72.9) | |
| Got better | 2 (1.0) | |
| Psychosocial variables | ||
| Discrimination experience due to the identity of COVID-19 survivor after hospital discharge (%Yes) | ||
| Being fired | 16 (8.0) | |
| Being treated unfairly by employers | 17 (8.5) | |
| Being socially excluded by co-workers | 25 (12.6) | |
| Being socially excluded by family members | 15 (7.5) | |
| Being socially excluded by friends | 47 (23.6) | |
| Being socially excluded by neighbors or communities | 70 (35.2) | |
| Being discriminated by healthcare providers | 18 (9.0) | |
| Others intentionally exposing your COVID-19 survivor identity | 75 (37.7) | |
| Number of discrimination experience | 1.8 (1.9) | |
| Self-stigma Scale (SSS)a | 18.6 (6.9) | |
| Affective dimension of the Affiliate Stigma Scaleb | 13.8 (5.5) | |
| The 2-item Connor-Davidson Resilience Scalec | 7.5 (1.9) | |
| Social Support Scaled | 11.7 (5.5) | |
Self-stigma Scale, 9 items, Cronbach's alpha: 0.94, one factor was identified by exploratory factor analysis, explaining for 67.3% of total variance.
Affective dimension of the Affiliate Stigma Scale, 7 items, Cronbach's alpha: 0.94, one factor was identified by exploratory factor analysis, explaining for 73.7% of total variance.
The 2-item Connor-Davidson Resilience Scale, 2 items, Cronbach's alpha: 0.89, one factor was identified by exploratory factor analysis, explaining for 90.3% of total variance.
Social Support Scale, 4 items, Cronbach's alpha: 0.80, one factor was identified by exploratory factor analysis, explaining for 62.8% of total variance.
3.3. Discrimination experience, self-stigma, perceived affiliate stigma, resilience and social support
Over 30% of the participants had experience of social exclusion from neighbors or communities (35.2%) or having others intentionally disclosing their COVID-19 survivor identity (37.7%). Relative fewer of them had other discrimination experiences, such as being fired (8.0%) or treated unfairly by employers (8.5%), being socially excluded by co-workers (12.6%), family members (7.5%) or friends (23.6%), or being discriminated by healthcare providers (9.0%). The mean scores and the standard deviation (SD) for the Self-Stigma Scale, the affective dimension of the Affiliate Stigma Scale, the CD-RISC2 Scale, and the Social Support Scale were presented in Table 2.
3.4. Factors associated with sleep quality
Older participants (51–60 years: B: −1.12, 95%CI: −2.21, −0.03, P = 0.04; >60 years: B: −1.37, 95%CI: −2.42, −0.32, P = 0.01; reference group: 18–30 years) and those who were retired (B: −1.20, 95%CI: −1.97, −0.42, P = 0.003; reference group: full-time employment) reported poorer sleep quality (Table 3 ).
Table 3.
Associations between background characteristics and sleep quality (n = 199).
| Unadjusted Ba (95%CI) | P valuea | |
|---|---|---|
| Socio-demographics | ||
| Age group (years) | ||
| 18–30 | Ref | |
| 31–40 | −0.17 (−1.14, 0.79) | 0.73 |
| 41–50 | −0.66 (−1.74, 0.42) | 0.23 |
| 51–60 | −1.12 (−2.21, −0.03) | 0.04 |
| >60 | −1.37 (−2.42, −0.32) | 0.01 |
| Gender | ||
| Male | Ref | |
| Female | −0.30 (−0.95, 0.34) | 0.35 |
| Relationship status | ||
| Currently single | Ref | |
| Married/cohabited with a partner | −0.60 (−1.43, 0.23) | 0.16 |
| Highest education attained | ||
| Junior high or below | Ref | |
| Senior high | −0.69 (−1.55, 0.17) | 0.11 |
| College and above | −0.05 (−0.84, 0.74) | 0.90 |
| Refuse to disclose | 0.87 (−1.80, 3.54) | 0.52 |
| Permanent residents of the city | ||
| No | Ref | |
| Yes | 0.05 (−0.68, 0.78) | 0.89 |
| Monthly personal income (¥) | 0.19 (−0.03, 0.42) | 0.09 |
| Employment status | ||
| Full-time employment | Ref | |
| Free-lanced | −0.13 (−1.05, 0.80) | 0.79 |
| Students | 0.15 (−1.05, 1.40) | 0.81 |
| Retired | −1.20 (−1.97, −0.42) | 0.003 |
| Unemployed | 0.16 (−1.02, 1.35) | 0.79 |
| Having at least one child | ||
| No | Ref | |
| Yes | −0.64 (−1.44, 0.17) | 0.12 |
| Variables related to SARS-Cov-2 infection | ||
| Severity level of COVID-19 at hospital admission | ||
| Asymptomatic/mild | Ref | Ref |
| Moderate | −0.05 (−0.81, 0.80) | 0.99 |
| Severe/critical | −0.57 (−1.71, 0.55) | 0.32 |
| No record | 0.25 (−1.02, 1.51) | 0.70 |
| Days in hospital (days) | ||
| ≤14 | Ref | Ref |
| 15-28 | 0.26 (−0.82, 1.34) | 0.64 |
| 29-42 | 0.70 (−0.47, 1.87) | 0.24 |
| >42 | 0.46 (−1.22. 2.13) | 0.59 |
| No record | 0.50 (−0.83, 1.82) | 0.46 |
| ICU admission | −1.56 (−3.60, 0.48) | 0.13 |
| Undergo invasive ventilation | −1.25 (−2.99, 0.48) | 0.16 |
| Undergo corticosteroid therapy | −0.82 (−1.79, 0.16) | 0.10 |
| Having a family member infected with COVID-19 | −0.17 (−0.81, 0.48) | 0.61 |
| Having a family member died of COVID-19 | 0.75 (−1.88, 3.39) | 0.57 |
| Mental health service utilization | ||
| Receiving mental health support services during hospitalization | −0.30 (−0.95, 0.35) | 0.36 |
| Receiving mental health support services after hospital discharge | 0.48 (−0.29, 1.25) | 0.22 |
95%CI: 95% confidence interval.
Ref: reference.
Unadjusted B: unstandardized coefficients.
After controlling for these significant background characteristics, higher number of discrimination experience (adjusted B: −0.29, 95%CI: −0.46, −0.11, P = 0.001), perceived stronger self-stigma (adjusted B: −0.13, 95%CI: −0.17, −0.08, P < 0.001) and perceived affiliate stigma (adjusted B: −0.09, 95%CI: −0.15, −0.03, P = 0.002) reported poorer sleep quality. Resilience (adjusted B: 0.22, 95%CI: 0.05, 0.39, P = 0.01) and social support (adjusted B: 0.08, 95%CI: 0.05, 0.11, P < 0.001) were positively and significantly associated with sleep quality (Table 4 ).
Table 4.
Associations between psychosocial variables and sleep quality among the participants (n = 199).
| Unadjusted Ba (95%CI) | P values | Adjusted Bb (95%CI) | P values | |
|---|---|---|---|---|
| Number of discrimination experience | −0.22 (−0.39, −0.06) | 0.009 | −0.29 (−0.46, −0.11) | 0.001 |
| Self-stigma Scale (SSS) | −0.13 (−0.17, −0.08) | <0.001 | −0.13 (−0.17, −0.08) | <0.001 |
| Affective dimension of the Affiliate Stigma Scale | −0.09 (−0.15, −0.03) | 0.003 | −0.09 (−0.15, −0.03) | 0.002 |
| The 2-item Connor-Davidson Resilience Scale | 0.24 (0.07, 0.41) | 0.006 | 0.22 (0.05, 0.39) | 0.01 |
| Social Support Scale | 0.08 (0.05, 0.11) | <0.001 | 0.08 (0.05, 0.11) | <0.001 |
95%CI: 95% confidence interval.
Unadjusted B: unstandardized coefficients.
Adjusted B: unstandardized coefficients adjusted for socio-demographic characteristics (age group and employment status).
3.5. Testing the mediation effects of resilience and social support in the associations between discrimination experience/self-stigma/perceived affiliate stigma and sleep quality
3.5.1. Model testing
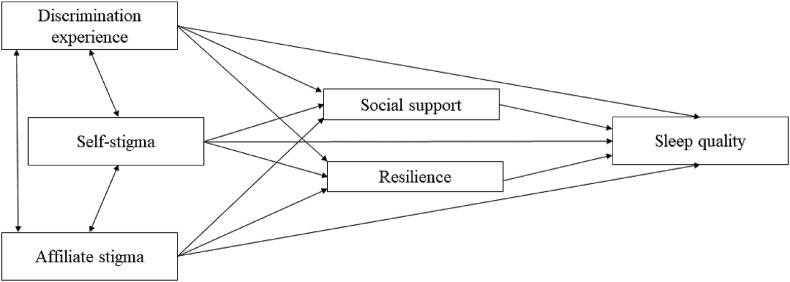
The proposed model fitted the data well (chi-square = 25.14, df = 18, P = 0.12, CFI = 0.97, NNFI = 0.94, RMSEA = 0.04) (Fig. 1 ).
Fig. 1.
The proposed mediation model of sleep quality.
3.5.2. Path coefficients
Self-stigma (B = −0.35, β = −0.25, P = 0.001) and affective dimension of the perceived affiliate stigma (B = −0.30, β = −0.17, P = 0.02) were significantly and negatively associated with social support. Self-stigma was negatively associated with resilience (B = −0.04, β = −0.15, P = 0.08). Social support (B = 0.04, β = 0.15, P = 0.02) and resilience (B = 0.14, β = 0.12, P = 0.06) were positively associated with sleep quality. In addition, self-stigma was negatively associated with sleep quality (B = −0.10, β = −0.29, P < 0.001).
3.5.3. Mediation effects
The indirect effect of self-stigma on sleep quality through social support and resilience was significant and negative (B = −0.02, β = −0.06, P = 0.05). Perceived affiliate stigma also had a significant and negative indirect effect on sleep quality through social support and resilience (B = −0.02, β = −0.04, P = 0.03).
4. Discussion
COVID-19 might have long-term impact on survivors’ sleep quality. In this study, the prevalence of terrible/poor sleep quality was much higher than healthy Chinese factory workers during the pandemic (10% versus 3.7%) [6]. As compared to a group of COVID-19 survivors who were recently discharged from hospital, the prevalence of sleep disorders in the past two weeks was slightly higher in our sample (33.7% versus 29.2%) [54]. Moreover, about one quarter of the participants reported a decrease in sleep quality as compared to the time before they were hospitalized.
The results showed that elderly COVID-19 survivors were more vulnerable to poorer sleep quality. Previous studies showed that sleep cycle of elderly people were changing, such as decreased total sleep time, increased time spent falling asleep at sleep onset, sleep fragmentation, and daytime sleep [59]. Those having low income and without fixed income reported poorer sleep quality. Financial difficulties is a risk factor of sleep quality [60]. Although COVID-19 treatment is free in China, hospitalization and subsequent quarantine may affect the work of the survivors, and may increase financial difficulties. Future programs should consider providing financial assistance to COVID-19 survivors who have financial difficulties. Since the majority of the participants were discharged before the China government started providing mental health support services to all COVID-19 patients [61], only 42.7% of our participants received such services during hospitalization. Moreover, mental health support services after hospital discharged were under-utilized by COVID-19 survivors, as they had to request such services [61]. It is also unclear whether such mental health support services targeted sleep quality, as the results showed a non-significant association between mental health support service utilization and sleep quality. Given its importance, future services should pay more attention to sleep quality among COVID-19 survivors.
COVID-19 related stigma is one of the key concerns among survivors that need to be urgently addressed [62]. Similar to findings in other countries, many COVID-19 survivors in this study experienced social exclusion originating from friends, neighbors and communities [[1], [2], [3], [4]]. In line with new reports, about 40% of the participants' personal information was intentionally exposed by others [7]. Having more discrimination experiences was associated with poorer sleep quality among COVID-19 survivors. A systematic review demonstrates consistent evidence that discrimination is associated with poorer sleep outcomes [63]. The Chinese government is actively making efforts to reduce discrimination against COVID-19 patients or survivors. In the early phase of the outbreak, health authorities would disclose some information about the COVID-19 patients (eg, age, gender, place of living and working, and travel history) for the purpose of contact tracing. Recently, health authorities omitted information that can be used to identify the patients to better protect their privacy. On the other hand, China is implementing guideline for protecting privacy of COVID-19 patients and imposing penalty for unauthorized disclosure of patients’ personal information [7]. In future, carefully designed stigma-reduction messages to foster empathy while simultaneously transforming public health measures into normal and sustained practices should be disseminated to the general public [64].
COVID-19 survivors were likely to endorse negative reactions from others. Both self-stigma and perceived affiliate stigma were associated with poorer sleep quality in this study. Such findings extended minority stress model [65] in understanding the associations of self-stigma and perceived affiliate stigma with mental health problems among COVID-19 survivors. Empowerment intervention, support group, and cognitive behavioral therapy (CBT) may be useful to facilitate cognitive restructuring and reduce self-devaluation and social withdrawal of COVID-19 survivors and their family members [66].
In line with previous studies conducted in other population [[33], [34], [35], [36], [37], [38]], resilience and social support are two significant protective factors of sleep quality among COVID-19 survivors. Indeed, both resilience and social support are important coping resources that can help individuals to adaptively cope with difficulties and stress [65]. Consistent with our hypothesis, resilience and social support mediated the associations between self-stigma/perceived affiliate stigma and sleep quality. Similar mediation effects were also observed in previous studies [[43], [44], [45], [46]]. It is possible that self-stigma and perceived affiliate stigma would diminish coping resources of COVID-19 survivors and hence lead to poor sleep quality. Enhancing resilience and social support may be useful to mitigate the effects of stigma on sleep quality among COVID-19 survivors. Strengths-based CBT may be a useful strategy to build up resilience [67]. It is also important to provide COVID-19 related health education to general public and family members of the survivors, so as to reduce unrealistic fears and stigma toward COVID-19 survivors. These approaches may improve social support for COVID-19 survivors.
This was one of the first studies looking at associations between COVID-19 related stigma and sleep quality among COVID-19 survivors. It had the strengths of recruiting survivors in multiple Chinese cities. However, it also had some limitations. First, the relatively small sample size limited the statistical power. Second, COVID-19 survivors were recruited in five Chinese cities, generalization should be made cautiously to other geographic locations in China. Third, we were not able to collect information from survivors who refused to participate in the study. Those who refused to complete the survey may have different characteristics from the participants. Selection bias existed. Fourth, parts of the data were self-reported, and verification was not feasible. Recall bias may have occurred. Moreover, we did not collect information about history of psychiatric disorders, which was a significant factor of post-discharge sleep quality. Furthermore, this was a cross-sectional study and could not establish causal relationship.
5. Conclusion
COVID-19 might have long-term impact on survivors’ sleep quality. Number of discrimination experiences, self-stigma and perceived affiliate stigma were associated with poor sleep quality among COVID-19 survivors, while social support and resilience were protective factors. Resilience and social support mediated the associations between self-stigma/perceived affiliate stigma and sleep quality. Reducing discrimination and stigma originated from general public, and reducing self-devaluation, improving resilience and social support among COVID-19 survivors might be useful strategies to improve sleep quality among COVID-19 survivors.
Credit author statement
Leiwen Fu: Conceptualization, Investigation, Formal analysis, Writing – original draft, Writing – review & editing, Visualization. Bingyi Wang: Investigation, Formal analysis, Writing – original draft, Writing – review & editing. Paul Shing Fong Chan: Methodology, Formal analysis, Writing – original draft, Writing – review & editing. Dan Luo: Investigation, Formal analysis, Writing – review & editing. Weiran Zheng: Investigation, Writing – review & editing. Niu Ju: Investigation, Writing – review & editing. Yuqing Hu: Investigation, Writing – review & editing. Xin Xiao: Investigation, Writing – review & editing. Hui Xu: Investigation, Writing – review & editing. Xue Yang: Investigation, Writing – review & editing. Yuan Fang: Investigation, Writing – review & editing. Zhijie Xu: Investigation, Writing – review & editing. Ping Chen: Investigation, Writing – review & editing. Jiaoling He: Investigation, Writing – review & editing. Hongqiong Zhu: Investigation, Writing – review & editing. Huiwen Tang: Investigation, Writing – review & editing. Dixi Huang: Investigation, Writing – review & editing. Zhongsi Hong: Investigation, Writing – review & editing. Xiaojun Ma: Investigation, Writing – review & editing. Yanrong Hao: Investigation, Writing – review & editing. Lianying Cai: Investigation, Writing – review & editing. Jianrong Yang: Investigation, Writing – review & editing. Jianhui Yuan: Investigation, Writing – review & editing. Yaoqing Chen: Investigation, Writing – review & editing. Fei Xiao: Investigation, Writing – review & editing. Zixin Wang: Supervision, Methodology, Project administration, Writing – review & editing, Validation. Shupei Ye: Supervision, Methodology, Writing – review & editing, Validation. Huachun Zou: Supervision, Methodology, Project administration, Writing – review & editing, Validation, Funding acquisition.
Funding
This study was supported by the Natural Science Foundation of China Excellent Young Scientists Fund [82022064], Natural Science Foundation of China International/Regional Research Collaboration Project [72061137001], Natural Science Foundation of China Young Scientist Fund [81703278], the Australian National Health and Medical Research Commission (NHMRC) Early Career Fellowship [APP1092621], the National Science and Technology Major Project of China [2018ZX10721102], the Sanming Project of Medicine in Shenzhen [SZSM201811071], the High Level Project of Medicine in Longhua, Shenzhen [HLPM201907020105], the National Key Research and Development Program of China [2020YFC0840900] and the Guangxi Medical and Health Appropriate Technology Development and Application Project [S2020124]. All funding parties did not have any role in the design of the study or in the explanation of the data.
Acknowledgements
We are grateful to Dr. Yusheng Jie from the Third Affiliated Hospital of Sun Yat-sen University for his support. We gratefully acknowledge the contributions of all participants in the present research.
Footnotes
The authors declare having no conflict of interest related to this work.
The ICMJE Uniform Disclosffigure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.10.020.
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
References
- 1.Singh R., Subedi M. COVID-19 and stigma: social discrimination towards frontline healthcare providers and COVID-19 recovered patients in Nepal. Asian J Psychiatr. Oct 2020;53:102222. doi: 10.1016/j.ajp.2020.102222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adom D.M.J. The psychological distress and mental health disorders from COVID-19 stigmatization in Ghana. Social Sciences & humanities open [preprint] https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3599756 [DOI] [PMC free article] [PubMed]
- 3.Dubey S., Biswas P., Ghosh R., et al. Psychosocial impact of COVID-19. Diabetes Metab Synd. Sep-Oct 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Logie C.H. Lessons learned from HIV can inform our approach to COVID-19 stigma. J Int AIDS Soc. May 2020;23(5) doi: 10.1002/jia2.25504. ARTN e25504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muhidin S., Vizheh M., Moghadam Z.B. Anticipating COVID-19-related stigma in survivors and health-care workers: lessons from previous infectious diseases outbreaks - an integrative literature review. Psychiatry Clin Neurosci. Nov 2020;74(11):617–618. doi: 10.1111/pcn.13140. [DOI] [PubMed] [Google Scholar]
- 6.Pan Y., Xin M., Zhang C., et al. Associations of mental health and personal preventive measure compliance with exposure to COVID-19 information during work resumption following the COVID-19 outbreak in China: cross-sectional survey study. J Med Internet Res. Oct 8 2020;22(10) doi: 10.2196/22596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu L. More attention should be given to COVID-19-related stigma after the pandemic is under controlled. 2020. https://news.gmw.cn/2020-06/14/content_33910290.htm?from=search Available at: Accesssed on Feburary 2, 2021.
- 8.Duan W., Bu H., Chen Z. COVID-19-related stigma profiles and risk factors among people who are at high risk of contagion. Soc Sci Med. Dec 2020;266:113425. doi: 10.1016/j.socscimed.2020.113425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson B.B. Hazard avoidance, symbolic and practical: the case of Americans' reported responses to Ebola. J Risk Res. 2019;22(3):346–363. [Google Scholar]
- 10.Lau J.T., Wang Z., Kim Y., et al. Anticipated negative responses by students to possible Ebola virus outbreak, guangzhou, China. Emerging Infectious Diseases. Jan 2016;22(1):154–156. doi: 10.3201/eid2201.150898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang X., Mak W.W. The differential moderating roles of self-compassion and mindfulness in self-stigma and well-being among people living with mental illness or HIV. Mindfulness. 2017;8(3):595–602. doi: 10.1007/s12671-016-0635-4. 2017/06/01. [DOI] [Google Scholar]
- 12.Yang X., Mak W.W., Ho C.Y., et al. Self-in-love versus self-in-stigma: implications of relationship quality and love attitudes on self-stigma and mental health among HIV-positive men having sex with men. AIDS Care. Jan 2017;29(1):132–136. doi: 10.1080/09540121.2016.1200714. [DOI] [PubMed] [Google Scholar]
- 13.Chiu M.Y., Yang X., Wong H.T., et al. The mediating effect of affective stigma between face concern and general mental health - the case of Chinese caregivers of children with intellectual disability. Res Dev Disabil. Jan 2015;36C:437–446. doi: 10.1016/j.ridd.2014.10.024. [DOI] [PubMed] [Google Scholar]
- 14.Yang X. No matter how I think, it already hurts: self-stigmatized feelings and face concern of Chinese caregivers of people with intellectual disabilities. J Intellect Disabil. Dec 2015;19(4):367–380. doi: 10.1177/1744629515577909. [DOI] [PubMed] [Google Scholar]
- 15.Meyer I.H. Minority stress and mental health in gay men. J Health Soc Behav. Mar 1995;36(1):38–56. [PubMed] [Google Scholar]
- 16.Meyer I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological bulletin. Sep 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pascoe E.A., Richman L.S. Perceived discrimination and health: a meta-analytic review. Psychological Bulletin. Jul 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mak W.W.S., Poon C.Y.M., Pun L.Y.K., et al. Meta-analysis of stigma and mental health. Soc Sci Med. Jul 2007;65(2):245–261. doi: 10.1016/j.socscimed.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 19.Stickgold R. Neuroscience: a memory boost while you sleep. Nature. Nov 30 2006;444(7119):559–560. doi: 10.1038/nature05309. [DOI] [PubMed] [Google Scholar]
- 20.Ibarra-Coronado E.G., Pantaleón-Martínez A.M., Velazquéz-Moctezuma J., et al. The bidirectional relationship between sleep and immunity against infections. J Immunol Res. 2015;2015:678164. doi: 10.1155/2015/678164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grandner M.A., Sands-Lincoln M.R., Pak V.M., et al. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat Sci Sleep. 2013;5:93–107. doi: 10.2147/NSS.S31063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li L., Wu C., Gan Y., et al. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. Nov 5 2016;16(1):375. doi: 10.1186/s12888-016-1075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong Y.C., Su T., Jiao P.Q., et al. Prevalence and factors associated with depression and anxiety of hospitalized patients with COVID-19. MedRxiv. 2020 doi: 10.1101/2020.03.24.20043075. [DOI] [Google Scholar]
- 24.Mazza M.G., De Lorenzo R., Conte C., et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. Oct 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fekete E.M., Williams S.L., Skinta M.D. Internalised HIV-stigma, loneliness, depressive symptoms and sleep quality in people living with HIV. Psychol Health. 2018;33(3):398–415. doi: 10.1080/08870446.2017.1357816. [DOI] [PubMed] [Google Scholar]
- 26.Bonanno G.A. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. Jan 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 27.Lepore S., Revenson T. Lawrence Erlbaum Associates Publishers; Mahwah: 2006. Resilience and posttraumatic growth: recovery, resistance, and reconfiguration; pp. 24–46. [Google Scholar]
- 28.Zhang J., Yang Z., Wang X., et al. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: a cross-sectional study. J Clin Nurs. Jul 23 2020 doi: 10.1111/jocn.15425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang X., Wang Q., Wang X., et al. Direct and indirect associations between interpersonal resources and posttraumatic growth through resilience among women living with HIV in China. AIDS Behav. Jun 2020;24(6):1687–1700. doi: 10.1007/s10461-019-02694-3. [DOI] [PubMed] [Google Scholar]
- 30.Sun N., Wei L., Wang H., et al. Qualitative study of the psychological experience of COVID-19 patients during hospitalization. J Affect Disord. Aug 24 2020;278:15–22. doi: 10.1016/j.jad.2020.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Qi R., Chen W., Liu S., et al. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: prevalence and associated biopsychosocial risk factors. MedRxiv. May 11 2020 doi: 10.1101/2020.05.08.20031666. [DOI] [Google Scholar]
- 32.Cai X., Hu X., Ekumi I.O., et al. Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am J Geriatr Psychiatr : Off J Am Assoc Geriatric Psychiatry. Oct 2020;28(10):1030–1039. doi: 10.1016/j.jagp.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li G.P., Kong L.H., Zhou H.Y., et al. Relationship between prenatal maternal stress and sleep quality in Chinese pregnant women: the mediation effect of resilience. Sleep Med. Sep 2016;25:8–12. doi: 10.1016/j.sleep.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 34.Bardwell W.A., Profant J., Casden D.R., et al. The relative importance of specific risk factors for insomnia in women treated for early-stage breast cancer. Psycho-Oncology. Jan 2008;17(1):9–18. doi: 10.1002/pon.1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Birtel M.D., Wood L., Kempa N.J. Stigma and social support in substance abuse: implications for mental health and well-being. Psychiat Res. Jun 2017;252:1–8. doi: 10.1016/j.psychres.2017.01.097. [DOI] [PubMed] [Google Scholar]
- 36.Tomfohr L.M., Edwards K.M., Madsen J.W., et al. Social support moderates the relationship between sleep and inflammation in a population at high risk for developing cardiovascular disease. Psychophysiology. Dec 2015;52(12):1689–1697. doi: 10.1111/psyp.12549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Grey R.G.K., Uchino B.N., Trettevik R., et al. Social support and sleep: a meta-analysis. Health Psychol. Aug 2018;37(8):787–798. doi: 10.1037/hea0000628.supp. [DOI] [PubMed] [Google Scholar]
- 38.Grey I., Arora T., Thomas J., et al. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiat Res. Nov 2020 doi: 10.1016/j.psychres.2020.113452. 293doi:ARTN 113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ransing R., Ramalho R., de Filippis R., et al. Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: drivers, facilitators, manifestations, and outcomes across the world. Brain Behav Immun. Oct 2020;89:555–558. doi: 10.1016/j.bbi.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abdelhafiz A.S., Alorabi M. Social stigma: the hidden threat of COVID-19. Front Public Health. 2020;8:429. doi: 10.3389/fpubh.2020.00429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ye Z., Yang X.Y., Zeng C.B., et al. Resilience, social support, and coping as mediators between COVID-19-related stressful experiences and acute stress disorder among college students in China. Appl Psychol-Hlth We. Dec 2020;12(4):1074–1094. doi: 10.1111/aphw.12211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yildirim M., Arslan G., Ozaslan A. Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: exploring the mediating effects of resilience and coronavirus fear. Int J Ment Health Addiction. Nov 16 2020 doi: 10.1007/s11469-020-00424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heckman T.G., Anderson E.S., Sikkema K.J., et al. Emotional distress in nonmetropolitan persons living with HIV disease enrolled in a telephone-delivered, coping improvement group intervention. Health Psychol. Jan 2004;23(1):94–100. doi: 10.1037/0278-6133.23.1.94. [DOI] [PubMed] [Google Scholar]
- 44.Logie C., James L., Tharao W., et al. Associations between HIV-related stigma, racial discrimination, gender discrimination, and depression among HIV-positive african, caribbean, and black women in ontario, Canada. Aids Patient Care St. Feb 2013;27(2):114–122. doi: 10.1089/apc.2012.0296. [DOI] [PubMed] [Google Scholar]
- 45.Kim E.Y., Jang M.H. The mediating effects of self-esteem and resilience on the relationship between internalized stigma and quality of life in people with schizophrenia. Asian Nurs Res. Oct 2019;13(4):257–263. doi: 10.1016/j.anr.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 46.Logie C.H., Lacombe-Duncan A., Wang Y., et al. Adapting the psychological mediation framework for cisgender and transgender sexual minorities in Jamaica: implications from latent versus observed variable approaches to sexual stigma. Soc Sci Med. Jan 2020;245:112663. doi: 10.1016/j.socscimed.2019. ARTN 112663. [DOI] [PubMed] [Google Scholar]
- 47.National Health Commission of The People's Republic of China Update of the COVID-19 pandemic in China (november 9, 2020) 2020. http://www.nhc.gov.cn/xcs/yqfkdt/202011/663e3753744f41d0b506324fa719d1be.shtml Available at: [DOI] [PMC free article] [PubMed]
- 48.Snyder E., Cai B., DeMuro C., et al. A new single-item sleep quality scale: results of psychometric evaluation in patients with chronic primary insomnia and depression. J Clin Sleep Med. 2018;14(11):1849–1857. doi: 10.5664/jcsm.7478. PII.jc-18-00127.10.5664/jcsm.7478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Serlachius A., Schache K., Boggiss A., et al. Coping skills mobile app to support the emotional well-being of Young people during the COVID-19 pandemic: protocol for a mixed methods study. JMIR Res Protocols. Oct 8 2020;9(10) doi: 10.2196/23716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pan Y., Xin M., Zhang C., et al. Associations between COVID-19 specific information exposure, mental health and self-reported compliance with personal preventive measures: evidence from a cross-sectional study at the initial phase of work resumption following the COVID-19 outbreak in China. J Med Internet Res. Sep 13 2020 doi: 10.2196/22596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gupta R., Grover S., Basu A., et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatr. 2020;62(4):370–378. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Badahdah A., Khamis F., Al Mahyijari N., et al. The mental health of health care workers in Oman during the COVID-19 pandemic. Int J Soc Psychiatr. Jul 8 2020 doi: 10.1177/0020764020939596. 20764020939596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shrestha C., Ghimire C., Acharya S., et al. Mental wellbeing during the lockdown period following the COVID-19 pandemic in Nepal: a descriptive cross-sectional study. J Nepal Med Assoc JNMA. 2020;58(230):744–750. doi: 10.31729/jnma.5498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wu C., Hu X., Song J., et al. Mental health status and related influencing factors of COVID-19 survivors in Wuhan, China. Clin Transl Med. Jun 5 2020;(2):10. doi: 10.1002/ctm2.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mak W.W., Cheung R.Y. Self-stigma among concealable minorities in Hong Kong: conceptualization and unified measurement. Am J Orthopsychiatry. Apr 2010;80(2):267–281. doi: 10.1111/j.1939-0025.2010.01030.x. [DOI] [PubMed] [Google Scholar]
- 56.Mak W.W.S., Cheung R.Y.M. Affiliate stigma among caregivers of people with intellectual disability or mental illness. J Appl Res Intellect Disabil. 2008;21(6):532–545. [Google Scholar]
- 57.Vaishnavi S., Connor K., Davidson J.R. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatr Res. Aug 30 2007;152(2–3):293–297. doi: 10.1016/j.psychres.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mcdonald R.P., Moon-Ho Ringo H. Principles and practice in reporting structural equation analyses. Psychol Methods. 2002;7(1):64. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- 59.Chen C.J., Hsu L.N., McHugh G., et al. Predictors of sleep quality and successful weaning from mechanical ventilation among patients in respiratory care centers. J Nurs Res : JNR. Mar 2015;23(1):65–74. doi: 10.1097/jnr.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 60.Hall M., Buysse D.J., Nofzinger E.A., et al. Financial strain is a significant correlate of sleep continuity disturbances in late-life. Biological Psychology. Feb 2008;77(2):217–222. doi: 10.1016/j.biopsycho.2007.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Government of People Republic of China Plans to provide psychological support and social services for COVID-19 patients and their family members, and people under quarantine. 2020. http://www.gov.cn/xinwen/2020-04/08/content_5500131.htm Available at:
- 62.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. Jul 2020;20(7):782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Slopen N., Lewis T.T., Williams D.R. Discrimination and sleep: a systematic review. Sleep Med. Feb 2016;18:88–95. doi: 10.1016/j.sleep.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Logie C.H., Turan J.M. How do we balance tensions between COVID-19 public health responses and stigma mitigation? Learning from HIV research. AIDS Behav. Jul 2020;24(7):2003–2006. doi: 10.1007/s10461-020-02856-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Meyer I.H. Resilience in the study of minority stress and health of sexual and gender minorities. Psychol Sex Orientat Gend Divers. 2015;2(3):209–213. doi: 10.1037/sgd0000132. [DOI] [Google Scholar]
- 66.Mittal D., Sullivan G., Chekuri L., et al. Empirical studies of self-stigma reduction strategies: a critical review of the literature. Psychiatr Serv. Oct 2012;63(10):974–981. doi: 10.1176/appi.ps.201100459. [DOI] [PubMed] [Google Scholar]
- 67.Padesky C.A., Mooney K.A. Strengths-based cognitive-behavioural therapy: a four-step model to build resilience. Clin Psychol Psychother. Jul-Aug 2012;19(4):283–290. doi: 10.1002/cpp.1795. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1