Abstract
Osimertinib is a third-generation, irreversible oral EGFR-tyrosine kinase inhibitor), that potently inhibits EGFR-tyrosine kinase inhibitor-sensitizing mutations and T790M resistance mutations together with efficacy in CNS metastases in patients with non-small-cell lung cancer (NSCLC). Here we describe the rationale and design for the Phase III NeoADAURA study (NCT04351555), which will evaluate neoadjuvant osimertinib with or without chemotherapy versus chemotherapy alone prior to surgery, in patients with resectable stage II–IIIB N2 EGFR mutation-positive NSCLC. The primary end point is centrally assessed major pathological response at the time of resection. Secondary end points include event-free survival, pathological complete response, nodal downstaging at the time of surgery, disease-free survival, overall survival and health-related quality of life. Safety and tolerability will also be assessed.
Trial Registration number: NCT04351555 (ClinicalTrials.gov)
Keywords: : EGFR-TKI-sensitizing mutations, EGFR-tyrosine kinase inhibitor, neoadjuvant, non-small-cell lung cancer, osimertinib, resectable
Lay abstract
A plain language version of this article is available and is published alongside the paper online: www.futuremedicine.com/doi/suppl/10.2217/fon-2021-0549
Approximately 30% of patients with non-small-cell lung cancer (NSCLC) present with resectable disease [1–3], the primary treatment for which is surgery with curative intent [4]. However, prognosis following surgery alone remains poor with 5-year survival probabilities ranging from ∼65% for stage IIA to 24% for stage IIIB (TNM classification of lung cancer, 8th edition staging) [5], due to the occurrence of local recurrence and/or distant metastases. Owing to limited data, it remains unclear whether prognosis differs in patients harboring tumors with mutated versus wild-type EGFR [6,7]. In addition, the role of surgery in stage IIIA N2 disease is controversial, with evidence suggesting that long-term clinical benefit following surgery alone is limited and that N2 disease is potentially a systemic disease requiring multimodality therapy for optimal outcomes [8,9].
Currently, adjuvant chemotherapy is recommended for patients with resected stage II or III NSCLC who have not received neoadjuvant chemotherapy [4]. However, clinical outcomes associated with adjuvant chemotherapy, including in resected EGFR-mutated (EGFRm) NSCLC, remain suboptimal with high recurrence rates are observed. In the randomized ADJUVANT-CTONG1104 trial, patients with stage II–IIIA EGFRm NSCLC in the adjuvant chemotherapy arm had a 5-year DFS and overall survival (OS) of 23 and 51%, respectively [10]. As an advantage over adjuvant treatment, neoadjuvant treatment in resectable NSCLC has the potential to downstage the tumor and provide earlier elimination of micrometastatic disease, thereby potentially reducing the risk of disease recurrence [4,11]. Furthermore, neoadjuvant NSCLC treatment data have shown that achieving a pathological complete response (pCR) is prognostic for survival [12]. Stage I–III NSCLC meta-analyses reported that neoadjuvant chemotherapy followed by surgery statistically significantly improved OS [13,14], time to distant recurrence and recurrence-free survival versus surgery alone [13]. In addition to these favorable outcomes, no increased perioperative risk after resection has been observed with neoadjuvant chemotherapy [15]. Nevertheless, only an estimated 13–18% reduction in the relative risk of death has been demonstrated with neoadjuvant chemotherapy versus surgery alone [13,14], resulting in absolute benefit in 5-year OS of 5–6% across stages. While neoadjuvant chemotherapy appears promising in this setting, more effective, personalized treatments are needed.
Although EGFR-TKIs are effective treatments in patients with advanced EGFRm NSCLC [16], and positive efficacy data have been shown in the adjuvant setting [17], there are currently no EGFR-TKIs approved for neoadjuvant treatment of resectable EGFRm NSCLC [18]. Recent, though limited, evidence indicates that neoadjuvant EGFR-TKIs with or without chemotherapy could achieve clinically meaningful tumor responses and survival in these patients [19–23]. Small, single center, Phase II studies of stage IIIA NSCLC have demonstrated objective responses and major pathologic responses with neoadjuvant erlotinib (for EGFRm disease) [20–22]. Furthermore, a small, single-arm Phase II study assessing neoadjuvant gefitinib in stage II–IIIA EGFRm NSCLC reported an ORR of 55% and MPR of 24% [23]. In the multicenter, randomized, Phase II EMERGING-CTONG 1103 study, numerical improvements in objective response rate (ORR) and major pathological response (MPR) were observed with neoadjuvant erlotinib versus neoadjuvant chemotherapy in patients with stage IIIA N2 EGFRm NSCLC; these results are supportive of improved outcomes with neoadjuvant erlotinib versus chemotherapy [19]. Objective response and MPR rates from these previous studies suggest scope for using EGFR-TKIs in the neoadjuvant setting [19–23]. Furthermore, there is growing evidence of enhanced benefit from combining an EGFR-TKI with chemotherapy in treatment-naive metastatic EGFRm NSCLC. Adding pemetrexed and carboplatin chemotherapy to gefitinib resulted in significant improvements in the objective response rate, and significantly prolonged PFS and OS in patients with treatment-naive metastatic EGFRm NSCLC at the cost of increased toxicity [24,25]. These results suggest that the combination of EGFR-TKI and chemotherapy may be a more effective and promising preoperative treatment option than EGFR-TKI alone. Taken together, these findings highlight a need for further investigation, with a potent EGFR-TKI, with or without chemotherapy, in the neoadjuvant setting.
Osimertinib
Osimertinib is a third-generation, irreversible, oral EGFR-TKI, that potently inhibits EGFR-TKI-sensitizing and T790M resistance mutations with efficacy in CNS metastases in NSCLC [26–30]. Following the positive results from the Phase III FLAURA (NCT02296125) and AURA3 (NCT02151981) studies, osimertinib is an approved first-line treatment option for locally advanced/metastatic EGFRm NSCLC and approved as treatment of patients with locally advanced/metastatic T790M-positive NSCLC who progressed on prior EGFR-TKI treatment [27,28,31–34]. The Phase III FLAURA2 (NCT04035486) study is currently recruiting and assessing efficacy and tolerability of osimertinib versus osimertinib with chemotherapy in the advanced setting. Building on the efficacy and safety data in advanced EGFRm NSCLC, adjuvant osimertinib has also demonstrated efficacy in resectable EGFRm NSCLC. In the Phase III ADAURA study, osimertinib showed a highly statistically significant and clinically meaningful DFS improvement (hazard ratio [HR]: 0.17; 99.06% CI: 0.11–0.26; p < 0.0001) versus placebo in resected stage II–IIIA EGFRm NSCLC, with or without prior adjuvant chemotherapy [17]. Similar improvements in DFS with osimertinib versus placebo were also observed in the overall patient population (stage IB–IIIA) (HR: 0.20: 99.12% CI: 0.14–0.30; p < 0.0001) [17]. This was the first targeted agent in a global trial to show statistically significant and clinically meaningful DFS improvement with adjuvant treatment for EGFRm NSCLC following surgery, demonstrating improved control of micrometastatic disease. Osimertinib has been approved by the US FDA as adjuvant treatment following tumor resection for EGFRm (Ex19del or L858R) NSCLC [35].
Taken together, these positive osimertinib data in the advanced/metastatic and adjuvant settings and the preliminary data from first- and second-generation EGFR-TKIs in the neoadjuvant setting, strongly support the rationale that neoadjuvant osimertinib may provide clinical benefit for patients with resectable EGFRm NSCLC. Indeed, preliminary data from a small Phase II study (NCT03433469) of five patients with resectable stage I–IIIA EGFRm NSCLC suggest that neoadjuvant osimertinib was well tolerated and could potentially induce pathological responses and downstaging of disease before surgery [36].
The NeoADAURA study
The Phase III NeoADAURA study (NCT04351555), sponsored by AstraZeneca, will evaluate the efficacy and safety of neoadjuvant osimertinib, as monotherapy or in combination with chemotherapy, versus chemotherapy alone in patients with resectable stage II–IIIB N2 EGFRm NSCLC, prior to surgery and adjuvant treatment (per investigator's choice, which could include adjuvant osimertinib).
Objectives
The primary objective of this study is to assess the benefit of neoadjuvant osimertinib as monotherapy or in combination with chemotherapy on centrally assessed MPR at resection, compared with neoadjuvant chemotherapy alone. Secondary objectives include event-free survival (EFS), and further efficacy assessments such as pCR, N2 to N0/N1 and N1 to N0 downstaging at the time of resection, DFS and OS. Additional secondary end points include health-related quality of life (HRQoL), MPR in patients with/without EGFRm detectable at screening in circulating tumor DNA (ctDNA), and concordance of EGFR mutation status between baseline tumor DNA and ctDNA samples and between the local and central tumor test results. The pharmacokinetics of osimertinib and its metabolites are another secondary end point. Safety and tolerability will also be assessed. Exploratory objectives include assessment of health resource use, tumor metabolism and the association of biomarkers and minimal residual disease (MRD) with clinical response.
Key eligibility criteria
Eligible patients must have histologically or cytologically documented non-squamous NSCLC with disease deemed to be completely resectable (stage II–IIIB N2, per the 8th edition of the IASLC Staging Manual in Thoracic Oncology) [37], and with tumors harboring common sensitizing EGFRm (Ex19del or L858R), either alone or in combination with other EGFR mutations (Table 1). Stage IIIB N2 disease by 8th edition staging [38] would be defined as stage IIIA by 7th edition staging [39], as used in the ADAURA study [17]. Complete surgical resection of the primary NSCLC must be deemed achievable, as assessed by a multidisciplinary team, and patients must have an Eastern Cooperative Oncology Group performance status of 0 or 1. Other key inclusion and exclusion criteria are shown in Table 1.
Table 1. . Key inclusion and exclusion criteria.
| Key inclusion criteria | Key exclusion criteria |
|---|---|
| • Written informed consent • Male or female, aged ≥18 years (or ≥20 years in Japan) • Histologically or cytologically documented non-squamous NSCLC with completely resectable disease (Stage II–IIIB N2, according to the 8th edition of the IASLC Staging Manual in Thoracic Oncology)† • Complete surgical resection of the primary NSCLC must be deemed achievable, as assessed by an MDT evaluation • A tumor which harbors either Ex19del or L858R EGFR-TKI-sensitizing mutations, either alone, or in combination with other EGFR mutations (T790M, G719X, Ex20ins, S7681 and L861Q) • ECOG PS 0/1 at enrollment, with no deterioration over the previous 2 weeks prior to baseline or day of first dosing • Adequate organ and marrow function as defined by: ○ Hemoglobin: ≥9.0 g/dL ○ Absolute neutrophil count: ≥1.5 × 109/l ○ Platelet count: ≥100 × 109/l ○ Serum bilirubin: ≤1.5 ULN ○ ALT and AST: ≤2.5 × ULN ○ Creatinine clearance: ≥50 ml/min • Life expectancy of >6 months prior to randomization |
• Prior treatment with systemic anti-cancer treatment for NSCLC, EGFR-TKI treatment or pre-operative radiotherapy • Mixed small cell and non-small-cell lung cancer histology • T4 tumors infiltrating the aorta, esophagus and/or heart • Bulky N2 disease • Candidates for segmentectomies or wedge resections only • Medical history of ILD, drug-induced ILD, radiation pneumonitis which required steroid treatment or any evidence of clinically active ILD • Severe or uncontrolled systemic diseases/active infections, history of allogeneic organ transplantation, history of primary immunodeficiency, history of another primary malignancy • Refractory nausea/vomiting, chronic GI disease, significant bowel resection that may prevent absorption of osimertinib • QTc >470 ms, clinically important abnormalities in resting ECG, factors increasing risk of QTc prolongation or arrhythmias |
IASLC Staging Manual in Thoracic Oncology 2016 [37].
ALT: Alanine transaminase; AST: Aspartate transaminase; ECG: Electrocardiogram; ECOG: Eastern Cooperative Oncology Group; EGFR-TKI: Epidermal growth factor receptor tyrosine kinase inhibitor; Ex19del: Exon 19 deletion; Ex20ins: Exon 20 insertion; GI: Gastrointestinal; IASLC: International Association for the Study of Lung Cancer; ILD: interstitial lung disease; MDT: Multidisciplinary team; NSCLC: Non-small-cell lung cancer; PS: performance status; QTc: Corrected QT interval; ULN: Upper limit of normal.
Study design
NeoADAURA is a Phase III, randomized, controlled, multicenter, three-arm study (Figure 1). Patients will be screened at a planned 184 study sites in 23 countries: Austria, Brazil, Bulgaria, Chile, China, Germany, India, Israel, Italy, Japan, Mexico, Peru, Poland, the Russian Federation, Republic of Korea, Spain, Switzerland, Taiwan, Thailand, Turkey, UK, USA and Vietnam. The first patient was enrolled on 16 December 2020 and the estimated primary analysis is expected in the 2nd quarter of 2024.
Figure 1. . NeoADAURA study design.
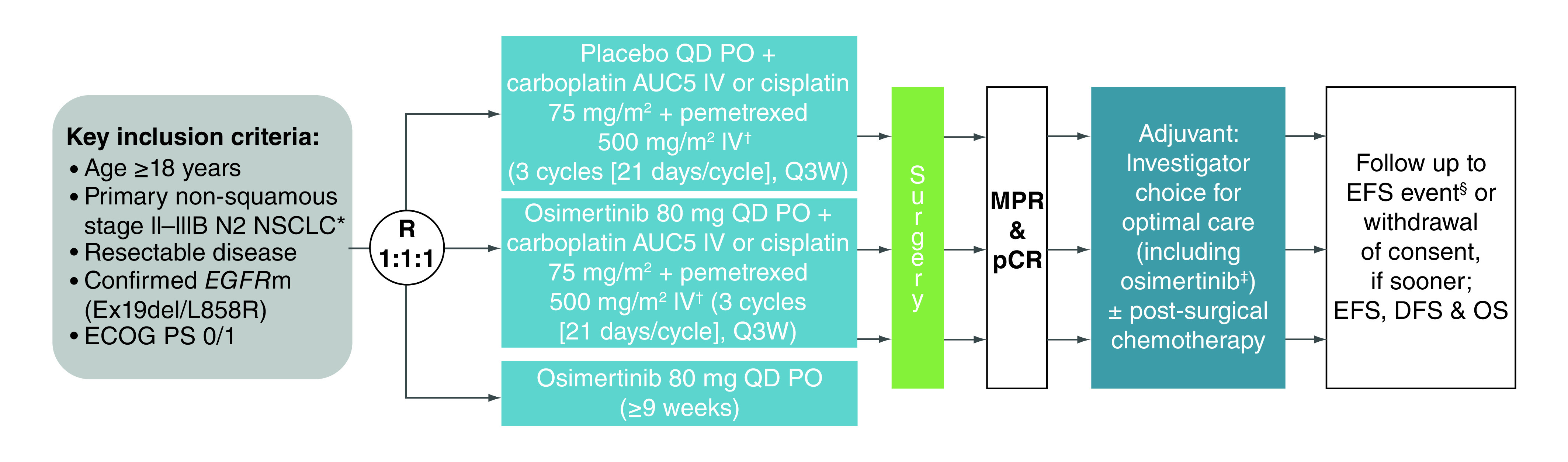
*By 8th edition of the IASLC Staging Manual in Thoracic Oncology 2016 [37].
†Investigator's choice.
‡Osimertinib will be offered for up to 3 years or until disease recurrence as a treatment choice.
§An EFS event is defined as documented disease progression that precludes surgery or requires non-protocol treatment; recurrence or a new local or distant lesion (a new primary malignancy confirmed by pathology is not considered to be an EFS event); or death due to any cause.
AUC5: Area under the curve 5; ECOG: Eastern Cooperative Oncology Group; DFS: Disease-free survival; EFS: Event-free survival; EGFRm: EGFR mutation-positive; Ex19del: Exon 19 deletion; IV: Intravenous; MPR: Major pathological response; NSCLC: Non-small-cell lung cancer; OS: Overall survival; pCR: Pathological complete response; PO: Orally; PS: Performance status; q3w: Three-times a week; qd: daily; R: Randomization.
Confirmation of EGFR mutation status will be obtained via a prospective central cobas® EGFR Mutation Test v2 (Roche Molecular Systems) using biopsy tissue at screening. Enrollment based on a pre-existing EGFR-mutation tissue test result using the cobas® EGFR Mutation Test v2 or the FoundationOne® CDx (F1CDx™; Foundation Medicine, Inc.) is also permitted.
Patients will be randomized, via an Interactive Voice/Web Response System, 1:1:1 to either: placebo once daily (qd) plus investigators' choice of platinum-based chemotherapy (three 21-day cycles of carboplatin area under the curve 5 + pemetrexed 500 mg/m2 or cisplatin 75 mg/m2 plus pemetrexed 500 mg/m2); osimertinib 80 mg qd plus investigators' choice of chemotherapy (as above); or osimertinib 80 mg qd monotherapy for ≥9 weeks. The two combination chemotherapy arms will be double-blind and the osimertinib monotherapy arm will be open-label but blinded to the sponsor. Randomization will be stratified by disease stage (II vs III), race (non-Asian vs mainland Chinese vs other Asian) and mutation type (Ex19del vs L858R).
Patient eligibility for surgery will be assessed following neoadjuvant treatment. If the patient is eligible, surgery is to be performed as soon as possible after the neoadjuvant treatment period, up to a maximum of 12 weeks following the start of neoadjuvant treatment. All patients who undergo surgery, or who do not have surgery for any reason other than disease progression, will subsequently enter the adjuvant follow-up period and be followed until the occurrence of an EFS event. In this period, the patients will receive optimal care, as defined by the Investigator and/or the multidisciplinary team; this can include osimertinib (in patients who have undergone surgery), which will be offered for up to 3 years or until disease recurrence or unacceptable toxicity. Postoperative radiotherapy and chemotherapy will be permitted prior to starting adjuvant osimertinib treatment.
All patients must provide written informed consent and the study will be conducted in accordance with the consensus ethical principles derived from international guidelines including the Declaration of Helsinki and Council for International Organizations of Medical Sciences International Ethical Guidelines and applicable International Conference on Harmonization Good Clinical Practice Guidelines.
Assessments
Mandatory tumor and plasma samples for central EGFR mutation analysis will be collected at baseline with additional plasma samples collected for retrospective quantification of MRD and/or ctDNA analysis at cycle 1 day 1 of the neoadjuvant period, the presurgical assessment (day 64), and at visit 1, week 12, week 24 and then every 24 weeks until week 264 (year 5) of the adjuvant period. Visit 1 of the adjuvant period will be at no more than 12 weeks postsurgery at the treating investigator's discretion.
Tumor samples collected during surgery will be locally assessed and then sent for central assessment to evaluate pathological response. Patients with tumors with ≤10% residual viable cancer cells (identified by routine hematoxylin and eosin staining) in the lung primary tumor after neoadjuvant treatment at the time of resection will be considered to have had an MPR. Patients with no residual viable tumor cells in any of the specimens (primary tumors, lymph nodes and margins) will be considered to have had a pCR. In the case of residual disease (as assessed locally), MPR will be considered as being ‘MPR (missing)’, and pCR will be considered as ‘pCR not achieved’.
Tumors will also be assessed during the screening period by mandatory contrast-enhanced computed tomography (CT) scans of chest and abdomen for disease staging and as a baseline for the post-neoadjuvant and presurgery scan. Further scans will be performed at the presurgical assessment (day 64), and at week 24 post-surgery and then every 24 weeks until the occurrence of an EFS event, death, withdrawal or the end of the study.
A mandatory whole body 18-fluorodeoxyglucose positron emission tomography scan will also be performed at baseline and at the presurgical assessment (day 64) for the exploratory end point of change in metabolic response in lesions of interest. In addition, tumor assessments of the brain will be performed at screening using contrast-enhanced magnetic resonance imaging (preferred) or CT.
Following disease recurrence or an EFS event occurring before or at the time of surgery, patients will be followed for OS every 3 months until 5 years from surgery.
HRQoL will be measured with the European Organisation for Research and Treatment of Cancer (EORTC) 30-item Core Quality of Life Questionnaire, the EORTC 13-item Lung Cancer Quality of Life Questionnaire, and the EuroQoL 5-Dimension, 5 Level health state utility index. HRQoL assessment will be performed at: cycle 1 day 1, cycle 2 day 22, cycle 3 day 43 and at the treatment discontinuation visit during the neoadjuvant period; at the presurgical assessment (day 64); at visit 1 of adjuvant treatment, week 12 post-surgery, week 24 and then every 24 weeks until week 264 (year 5) of the adjuvant period.
Adverse events (AEs) and serious AEs will be continuously assessed throughout the study and during the safety follow-up period, which will be 28 days after the last study drug dose for patients who do not undergo surgery or 90 days post-surgery. AEs of special interest to be monitored in the study are interstitial lung disease (including pneumonitis) and cardiac failure. An Independent Data Monitoring Committee will review unblinded safety data at regular intervals throughout the study, including at one planned interim analysis for MPR.
Statistical analysis
Approximately 351 patients with resectable stage II–IIIB N2 EGFRm NSCLC will be enrolled. This sample size was based on an approximate 90% power to detect a statistically significant difference in MPR of 20%, with a two-sided overall significance level of 5% when assuming a 20% MPR in the control arm.
An interim analysis for MPR is planned for when approximately half of the patients have completed surgery; the final analysis for MPR will occur after the last patient has completed surgery (~6 months after the last patient is randomized). MPR will be analyzed using a Cochran-Mantel Haenszel test, stratified by disease stage, race and mutation type, and subgroup analyses will compare the treatment effects of MPR by these three stratification factors.
EFS will be defined as the time from randomization until an event occurs, defined as: documented disease progression that precludes surgery or requires nonprotocol treatment; recurrence or a new local or distant lesion (a new primary malignancy confirmed by pathology is not considered to be an EFS event); or death due to any cause. An interim EFS analysis will occur at the same time as the MPR final analysis; the final analysis of EFS will be conducted when all patients have had the opportunity for at least 3 years follow-up post-surgery. OS will be defined as the time from randomization until death due to any cause. DFS will be defined as the time from surgery until the first instance of disease recurrence (local or distant) or death due to any cause, whichever occurs first. Nodal downstaging will be assessed in accordance with the American Joint Committee on Cancer 8th edition TNM staging system [38], and is defined as patients with baseline N2 disease becoming N1/N0 at the time of surgery or patients with baseline N1 disease becoming N0 at surgery. Downstaging will be formally assessed for patients with pathological staging available at both baseline and surgery. MRD and molecular tumor profiling will be used to evaluate molecular signals of disease progression in the adjuvant phase and will be associated with MPR, pCR, EFS, DFS and adjuvant therapies.
All of the above end points except for DFS will be assessed in the full analysis set, including all randomized patients. DFS will be assessed in the resected analysis set, which includes all randomized patients who have a complete surgical resection following neoadjuvant treatment.
Discussion & future perspective
Further treatment options are needed for patients with resectable EGFRm NSCLC as currently approved therapies fail to address the biology of this disease, leading to poor outcomes with surgery and chemotherapy alone. The NeoADAURA study will assess the efficacy and safety of neoadjuvant osimertinib in patients with resectable stage II–IIIB EGFRm NSCLC prior to surgery and adjuvant treatment as indicated. Osimertinib will be evaluated as monotherapy or in combination with chemotherapy. Combining a cytotoxic compound with a targeted treatment may provide enhanced benefit by increasing the likelihood of eliminating cancer cells not eradicated by osimertinib, with the potential to prevent disease recurrence and extend survival.
A 9-week neoadjuvant treatment period in NeoADAURA was chosen to match the three cycles of neoadjuvant chemotherapy used in previous stage I–III NSCLC trials, which were sufficient to provide a major response and favorable survival outcomes [13,40,41]. The IFCT0002 trial suggested that no improvement in pathological response resulted from increasing from two to four chemotherapy cycles in patients with resectable stage I–II NSCLC [42]. This chosen neoadjuvant treatment period therefore maximizes treatment benefit without an unacceptable delay in surgery. Following neoadjuvant treatment, surgery is encouraged to take place as soon as feasible, within a 3-week maximum time period, following resolution of any AEs that could impact surgery. However, osimertinib treatment is permitted beyond 9 weeks until just before surgery at the investigator's discretion. This is to avoid potential tumor flare resulting from treatment cessation, as previously documented in patients with EGFRm NSCLC who discontinued erlotinib/gefitinib [43].
An important consideration for a neoadjuvant agent is that treatment-related toxicities do not interfere with surgery or delay surgery, currently a key factor in determining the timing of neoadjuvant or adjuvant therapy. Preliminary results from the small study mentioned above indicate that neoadjuvant osimertinib was well tolerated, with no SAEs reported, and no unscheduled delay to surgery [36], in line with the well-characterized tolerability profile of osimertinib monotherapy in advanced EGFRm NSCLC [27,28,31,32] and as adjuvant treatment for resected stage IB–IIIA EGFRm NSCLC [17]. While data are limited regarding the combination of osimertinib with chemotherapy, results from the safety run-in (n = 30) of the FLAURA2 study demonstrated that first-line osimertinib plus chemotherapy was well tolerated in patients with advanced/metastatic EGFRm NSCLC with a similar toxicity profile to chemotherapy alone and osimertinib alone, and with no new safety signals identified (Planchard et al. Manuscript in preparation).
EFS is a validated end point in the curative setting, defined as time from randomization until occurrence of an EFS event (documented disease progression preventing surgery or requiring nonprotocol therapy, recurrence or a new lesion [local or distant] or death from any cause). Powering a study for EFS as the primary end point, like OS, requires a large population; >1100 patients to provide sufficient power for EFS and MPR as co-primary end points. The proportion of patients with EGFRm NSCLC tumors is relatively small, varying between ∼14 and 24% in Europe and the USA, and ∼38% in Asia [44]; resulting in a likely recruitment time of ∼9 years. EFS was therefore selected as a secondary end point. The primary end point, MPR, was chosen due to evidence supporting its use as a surrogate for OS [12,45,46] in neoadjuvant studies in resectable NSCLC. MPR correlates with OS and is an independent prognostic factor in patients with resectable stage I–III NSCLC undergoing neoadjuvant treatment [47,48]. In patients with resectable disease, MPR has also been shown to reflect treatment effect and capture the magnitude of the treatment benefit on survival, further supporting its utility as a surrogate [12]. NeoADAURA will collect data on EFS, DFS and OS (secondary end points), to observe the long-term benefits of study treatments. pCR will also be assessed as a secondary end point and has been shown to be a prognostic factor for long-term outcomes in patients with NSCLC undergoing neoadjuvant treatment and surgery [49]. However, pCR rates in NSCLC trials have been variable and low (0–16%), thus requiring a large population to power for clinically meaningful changes between arms, making this an unsuitable primary end point [12]. Treatment response in involved lymph nodes and the primary tumor, is a key clinical outcome. Nodal downstaging with neoadjuvant treatment in patients with stage IIIA–N2 NSCLC prior to surgery has been associated with improved survival [22]. As such, N2 to N0/N1 and N1 to N0 downstaging at the time of surgery is another important secondary end point in NeoADAURA. For exploratory analyses, tumor tissue, plasma and blood samples will be tested for MRD to evaluate their association with clinical response. This will further improve understanding of the impact of neoadjuvant treatment on the disease, may identify suitable patients for further adjuvant treatment, and provide data on the efficacy of adjuvant treatment. Patients also have an option to contribute a plasma sample for genomics initiative research. These samples will be used to explore how genetic variations may affect clinical parameters, risk and prognosis of disease and the response to medications.
In the advanced/metastatic EGFRm NSCLC setting, EGFR testing and EGFR-TKI treatment are recommended standard practice [16]; this personalized medicine approach should now be considered for resectable EGFRm NSCLC. To this end, EGFR testing will be key to appropriately treating all patients with NSCLC at the time of diagnosis. With potential positive results from NeoADAURA, the positive outcomes from ADAURA [17] and subsequent FDA approval of adjuvant osimertinib in patients with resectable EGFRm NSCLC [35], earlier EGFR testing will be needed and is expected to increase. However, some challenges are expected as EGFR testing is not currently recommended in patients with stage I–IIIA NSCLC [4] and therefore not routinely performed in clinical practice. EGFR testing for resectable disease where neoadjuvant treatment is planned will require rapid turnaround times to prevent delays in treatment. In NeoADAURA, EGFR testing will be conducted centrally. Collecting a biopsy may be challenging in resectable disease due to tumors not easily accessible to biopsy or insufficient tissue from smaller biopsies. An alternative approach may be liquid biopsy although its role in EGFR testing in resectable disease is unclear. However, the use of liquid biopsy as a reliable test for future patient selection will be assessed in NeoADAURA: a concordance analysis is planned to retrospectively compare EGFR mutation status from baseline plasma samples with tissue biopsy samples.
To date, treatment options are limited for stage II–IIIB EGFRm NSCLC with small absolute benefits observed with neoadjuvant chemotherapy [13,14]. While trials of neoadjuvant immunotherapy plus chemotherapy in resectable stage IB–IIIA NSCLC have shown high MPR and partial response rates (50–85% and 57–72%, respectively) [50], increasing evidence indicates that immunotherapy has limited efficacy for patients with EGFRm NSCLC [51,52]. Therefore treatment approaches such as EGFR-TKIs, with or without chemotherapy, are needed for these patients [51,52]. As such, NeoADAURA offers targeted treatment to patients who are predominantly excluded from neoadjuvant immunotherapy trials [51]. The potential benefits of neoadjuvant osimertinib treatment with or without chemotherapy are shrinking the tumor, so improving surgical outcomes, downstaging the disease, thus improving prognosis and clearing micrometastases, thereby reducing the risk of disease recurrence. Therefore, NeoADAURA may improve outcomes in resectable stage II–IIIB EGFRm NSCLC and help establish personalized medicine in this setting. Furthermore, NeoADAURA outcomes will help to define the role of neoadjuvant osimertinib in the treatment of resectable EGFRm NSCLC, either as monotherapy or in combination with chemotherapy, in comparison with standard of care (SoC) chemotherapy alone. This will inform the need for chemotherapy in this population and evaluate any possible synergy of osimertinib with chemotherapy, potentially further changing the SoC approach to patients with resectable EGFRm NSCLC.
Conclusion
The Phase III, randomized, multicenter NeoADAURA study will assess neoadjuvant osimertinib as monotherapy or in combination with chemotherapy, versus SoC chemotherapy alone, followed by surgery and adjuvant treatment as indicated (per investigator's choice, including osimertinib for up to 3 years) in patients with resectable stage II–IIIB EGFRm NSCLC. The results will help to further define the role of neoadjuvant targeted treatment, particularly neoadjuvant osimertinib treatment, in resectable EGFRm NSCLC. The results of NeoADAURA have the potential to enrich the treatment options and inform clinical practice of neoadjuvant treatment in this setting.
Executive summary.
Background & rationale
Treatment options for patients with resectable non-small-cell lung cancer (NSCLC) are limited and long-term outcomes remain poor, with 5-year survival probabilities ranging from ∼65% for stage IIA to 24% for stage IIIB disease; it remains unclear if patients with EGFR-mutated (EGFRm) versus wild-type tumors have a different prognosis.
Adjuvant chemotherapy is recommended in all patients with resected stage II–III NSCLC; clinical benefit, though limited, has been demonstrated for neoadjuvant chemotherapy versus surgery alone in stage I–III disease.
Despite previous studies with neoadjuvant EGFR-tyrosine kinase inhibitors (EGFR-TKIs) indicating improvements in outcomes, no EGFR-TKIs are currently approved for neoadjuvant treatment in resectable EGFRm NSCLC. However, the ADAURA study results and subsequent US FDA approval of osimertinib as adjuvant treatment, suggest scope for osimertinib as neoadjuvant treatment.
EGFR-TKIs in the locally advanced/metastatic setting have manageable toxicities, suggesting that their use as neoadjuvant treatment may not delay surgery.
The efficacy and tolerability of the EGFR-TKI osimertinib in the locally advanced/metastatic and resectable disease settings support its evaluation as neoadjuvant treatment in resectable NSCLC.
Osimertinib
Osimertinib is a third-generation, irreversible oral EGFR-TKI with proven CNS efficacy in NSCLC.
In the locally advanced/metastatic setting, osimertinib is approved for first-line treatment of EGFRm NSCLC and treatment of T790M-positive NSCLC with disease progression on prior EGFR-TKI therapy.
In resectable NSCLC, adjuvant osimertinib showed statistically significant disease-free survival improvement versus placebo in stage IB-IIIA EGFRm disease, with or without adjuvant chemotherapy. These results led to FDA approval of osimertinib as adjuvant treatment for EGFRm NSCLC.
Neoadjuvant combination of osimertinib and chemotherapy may optimize elimination of micrometastases and tumor downstaging before surgical treatment.
NeoADAURA study
NeoADAURA is a Phase III, randomized, controlled, multicenter study assessing neoadjuvant osimertinib with or without chemotherapy in resectable EGFRm NSCLC.
Eligible patients must have completely resectable stage II–IIIB N2 EGFRm (Ex19del or L858R) NSCLC with an Eastern Cooperative Oncology Group performance status 0 or 1 at enrollment.
Patients will be randomized 1:1:1 to receive either placebo plus chemotherapy, osimertinib plus chemotherapy or osimertinib monotherapy, followed by surgery and adjuvant treatment (adjuvant osimertinib for up to 3 years is permitted).
The primary end point is major pathological response at the time of resection.
Secondary end points include event-free survival, pathological complete response, N2 to N0/N1 and N1 to N0 downstaging at resection, disease-free survival and overall survival.
Conclusion
Results from NeoADAURA will help to define the role of neoadjuvant osimertinib in resectable EGFRm NSCLC.
Acknowledgments
Thanks to all the patients and their families.
Footnotes
Author contributions
Conception and design: S Dacic, C Blakely, C Escriu, A Walding and JE Chaft. Drafting the manuscript: all authors. Manuscript writing: A Walding, JE Chaft. Final approval of the manuscript: all authors. Agree to be accountable for all aspects of the work, which includes ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: all authors.
Financial & competing interests disclosure
This trial (NCT04351555) was funded by AstraZeneca, the manufacturer of osimertinib. The funder contributed to the conception and design of the trial; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication and as such are included in the author list and acknowledgments. M Tsuboi – advisory boards: AstraZeneca, MSD, Novartis; honoraria received from promotional activities: AstraZeneca KK, Bristol-Myers Squibb KK, Chugai Pharmaceutical Co Ltd, Eli Lilly Japan, Johnson & Johnson Japan, Medtronic Japan, Ono Pharmaceutical Co Ltd, Taiho Pharma, Teijin Pharma. W Weder – consultant: AstraZeneca, Medtronic. C Escriu – speakers bureau: AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, MSD, Pfizer; advisory boards: AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, MSD. C Blakely – advisory board: Blueprint Medicines, Bayer; consultant: Amgen. J He – nothing to disclose. S Dacic – advisory board: AstraZeneca, Takeda, Janssen; consultant: AstraZeneca. Y Yatabe – advisory boards: AstraZeneca, Daiichi-Sankyo, MSD, Amgen, Takeda; honoraria received from promotional activities: Alilent/Dako, AstraZeneca, Chugai Pharma, MDS, Novartis, Pfizer, Roche/Ventana, Thermo Fisher Scientific. L Zeng – ownership or stock interests: AstraZeneca; employment: AstraZeneca. A Walding – ownership or stock interests: AstraZeneca; employment: AstraZeneca. JE Chaft – consultant: AstraZeneca, Flame Biosciences, Genentech, Merck, Novartis, Jannsen. Cancer Center Support Grant P30 CA00874. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
The authors would like to acknowledge S Cotterill of Ashfield MedComms, an Ashfield Health company, and C McCleverty contracted to Ashfield MedComms, for medical writing support that was funded by AstraZeneca in accordance with Good Publications Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Ethical conduct of research
The study will be conducted in accordance with the consensus ethical principles derived from international guidelines including the Declaration of Helsinki and Council for International Organizations of Medical Sciences International Ethical Guidelines and applicable International Conference on Harmonization Good Clinical Practice Guidelines.
Data-sharing statement
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca's data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure
Open access
This work is licensed under the Attribution-NonCommercial-NoDerivatives 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Le Chevalier T. Adjuvant chemotherapy for resectable non-small-cell lung cancer: where is it going? Ann. Oncol. 21(Suppl. 7), vii196–198 (2010). [DOI] [PubMed] [Google Scholar]
- 2.Datta D, Lahiri B. Preoperative evaluation of patients undergoing lung resection surgery. Chest 123(6), 2096–2103 (2003). [DOI] [PubMed] [Google Scholar]
- 3.Cagle PT, Allen TC, Olsen RJ. Lung cancer biomarkers: present status and future developments. Arch. Pathol. Lab. Med. 137(9), 1191–1198 (2013). [DOI] [PubMed] [Google Scholar]
- 4.Postmus PE, Kerr KM, Oudkerk M et al. Early-stage and locally advanced (non-metastatic) non-small-cell lung cancer: ESMO Clinical Practice Guidelines. Ann. Oncol. 28(Suppl. 4), iv1–iv21 (2017). [DOI] [PubMed] [Google Scholar]
- 5.Goldstraw P, Chansky K, Crowley J et al. The IASLC Lung Cancer Staging Project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J. Thorac. Oncol. 11(1), 39–51 (2016). [DOI] [PubMed] [Google Scholar]
- 6.Zhou X, Cai L, Liu J et al. Analyzing EGFR mutations and their association with clinicopathological characteristics and prognosis of patients with lung adenocarcinoma. Oncol. Lett. 16(1), 362–370 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang Z, Wang T, Zhang J et al. Prognostic value of epidermal growth factor receptor mutations in resected non-small-cell lung cancer: a systematic review with meta-analysis. PLoS ONE 9(8), e106053 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao Y, Wang W, Liang H et al. The optimal treatment for stage IIIA-N2 non-small-cell lung cancer: a network meta-analysis. Ann. Thorac. Surg. 107(6), 1866–1875 (2019). [DOI] [PubMed] [Google Scholar]
- 9.Albain KS, Swann RS, Rusch VW et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a Phase III randomised controlled trial. Lancet 374(9687), 379–386 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhong WZ, Wang Q, Mao WM et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II–IIIA (N1-N2) EGFR-mutant NSCLC: final overall survival analysis of CTONG1104 Phase III trial. J. Clin. Oncol. 39(7), 713–722 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhai H, Zhong W, Yang X, Wu YL. Neoadjuvant and adjuvant epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI) therapy for lung cancer. Transl. Lung Cancer Res. 4(1), 82–93 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hellmann MD, Chaft JE, William WN Jr et al. Pathological response after neoadjuvant chemotherapy in resectable non-small-cell lung cancers: proposal for the use of major pathological response as a surrogate endpoint. Lancet Oncol. 15(1), e42–50 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.NSCLC Meta-analysis Collaborative Group. Preoperative chemotherapy for non-small-cell lung cancer: a systematic review and meta-analysis of individual participant data. Lancet 383(9928), 1561–1571 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]; • Systematic review and meta-analysis of patient-level data showing the utility of preoperative chemotherapy for resectable NSCLC.
- 14.Burdett S, Stewart LA, Rydzewska L. A systematic review and meta-analysis of the literature: chemotherapy and surgery versus surgery alone in non-small-cell lung cancer. J. Thorac. Oncol. 1(7), 611–621 (2006). [PubMed] [Google Scholar]; • Systematic review and study-level meta-analysis showing significant clinical benefit of preoperative chemotherapy plus surgery versus surgery alone in patients with NSCLC.
- 15.Brunelli A, Rocco G, Szanto Z, Thomas P, Falcoz PE. Morbidity and mortality of lobectomy or pneumonectomy after neoadjuvant treatment: an analysis from the ESTS database. Eur. J. Cardiothorac. Surg. 57(4), 740–746 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Planchard D, Popat S, Kerr K et al. Metastatic non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. ESMO Guidelines Committee; (2020). https://www.esmo.org/guidelines/lung-and-chest-tumours/clinical-practice-living-guidelines-metastatic-non-small-cell-lung-cancer [DOI] [PubMed] [Google Scholar]
- 17.Wu YL, Tsuboi M, He J et al. Osimertinib in resected EGFR-mutated non-small-cell lung cancer. N. Engl. J. Med. 383(18), 1711–1723 (2020). [DOI] [PubMed] [Google Scholar]
- 18.Lv C, Ma Y, Feng Q et al. Does neoadjuvant targeted therapy provide an opportunity for resectable EGFR-mutant lung cancer: a real-world retrospective study. J. Thorac. Dis. 12(10), 5324–5335 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhong WZ, Chen KN, Chen C et al. Erlotinib versus gemcitabine plus cisplatin as neoadjuvant treatment of stage IIIA-N2 EGFR-mutant non-small-cell lung cancer (EMERGING-CTONG 1103): a randomized Phase II study. J. Clin. Oncol. 37(25), 2235–2245 (2019). [DOI] [PubMed] [Google Scholar]
- 20.Xiong L, Li R, Sun J et al. Erlotinib as neoadjuvant therapy in stage IIIA (N2) EGFR mutation-positive non-small-cell lung cancer: a prospective, single-arm, Phase II study. Oncologist 24(2), 157–e164 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiong L, Lou Y, Bai H et al. Efficacy of erlotinib as neoadjuvant regimen in EGFR-mutant locally advanced non-small-cell lung cancer patients. J. Int. Med. Res. 48(4), 10.1177/0300060519887275 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhong W, Yang X, Yan H et al. Phase II study of biomarker-guided neoadjuvant treatment strategy for IIIA-N2 non-small-cell lung cancer based on epidermal growth factor receptor mutation status. J. Hematol. Oncol. 8, 54 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Y, Fu F, Hu H et al. Gefitinib as neoadjuvant therapy for resectable stage II–IIIA non-small-cell lung cancer: a Phase II study. J. Thorac. Cardiovasc. Surg. (2020). [DOI] [PubMed] [Google Scholar]
- 24.Hosomi Y, Morita S, Sugawara S et al. Gefitinib alone versus gefitinib plus chemotherapy for non-small-cell lung cancer with mutated epidermal growth factor receptor: NEJ009 study. J. Clin. Oncol. 38(2), 115–123 (2020). [DOI] [PubMed] [Google Scholar]; • Randomized Phase III trial showing significantly improved response rates, PFS and OS with the EGFR-TKI gefitinib plus carboplatin and pemetrexed chemotherapy versus gefitinib alone in patients with advanced EGFRm NSCLC.
- 25.Noronha V, Patil VM, Joshi A et al. Gefitinib versus gefitinib plus pemetrexed and carboplatin chemotherapy in EGFR-mutated lung cancer. J. Clin. Oncol. 38(2), 124–136 (2020). [DOI] [PubMed] [Google Scholar]; • Randomized Phase III trial showing significantly improved response rates, PFS and OS with the EGFR-TKI gefitinib plus carboplatin chemotherapy versus gefitinib alone in patients with advanced EGFRm NSCLC.
- 26.Cross DA, Ashton SE, Ghiorghiu S et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 4(9), 1046–1061 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mok TS, Wu Y-L, Ahn M-J et al. Osimertinib or platinum–pemetrexed in EGFR T790M–positive lung cancer. N. Engl. J. Med. 376(7), 629–640 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soria JC, Ohe Y, Vansteenkiste J et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N. Engl. J. Med. 378(2), 113–125 (2018). [DOI] [PubMed] [Google Scholar]
- 29.Wu YL, Ahn MJ, Garassino MC et al. CNS efficacy of osimertinib in patients with T790M-positive advanced non-small-cell lung cancer: data from a randomized Phase III trial (AURA3). J. Clin. Oncol. 36(26), 2702–2709 (2018). [DOI] [PubMed] [Google Scholar]
- 30.Reungwetwattana T, Nakagawa K, Cho BC et al. CNS response to osimertinib versus standard epidermal growth factor receptor tyrosine kinase inhibitors in patients with untreated EGFR-mutated advanced non-small-cell lung cancer. J. Clin. Oncol. 36, 3290–3297 (2018). [DOI] [PubMed] [Google Scholar]
- 31.Ramalingam SS, Vansteenkiste J, Planchard D et al. Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC. N. Engl. J. Med. 382(1), 41–50 (2020). [DOI] [PubMed] [Google Scholar]
- 32.Papadimitrakopoulou VA, Mok TS, Han JY et al. Osimertinib versus platinum-pemetrexed for patients with EGFR T790M advanced NSCLC and progression on a prior EGFR-tyrosine kinase inhibitor: AURA3 overall survival analysis. Ann. Oncol. 31(11), 1536–1544 (2020). [DOI] [PubMed] [Google Scholar]
- 33.U.S. Food and Drug Administration. TAGRISSO® Highlights of Prescribing Information. (2018). https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/208065s008lbl.pdf
- 34.European Medicines Agency. Tagrisso, INN-osimertinib. (2016). https://www.ema.europa.eu/en/documents/product-information/tagrisso-epar-product-information_en.pdf
- 35.US Food and Drug Administration. FDA approves osimertinib as adjuvant therapy for non-small-cell lung cancer with EGFR mutations. (2020). https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-osimertinib-adjuvant-therapy-non-small-cell-lung-cancer-egfr-mutations#:∼:text=On%20December%2018%2C%202020%2C%20the,exon%2021%20L858R%20mutations%2C%20as
- 36.Rotow J, Urisman A, Mccoach C et al. P1.14-58 A phase II study to evaluate neoadjuvant osimertinib for surgically resectable, EGFR-mutant non-small-cell lung cancer. J. Thorac. Oncol. 14(10), S578 (2019). [Google Scholar]
- 37.IASLC Staging Manual in Thoracic Oncology. 2nd Edition. Editorial Rx Press, North Fort Myers, FL, USA: (2016). [Google Scholar]
- 38.AJCC Cancer Staging Manual. 8th Edition. Springer International Publishing; (2017). [Google Scholar]
- 39.AJCC Cancer Staging Handbook. 7th Edition. Springer, London, UK: (2010). [Google Scholar]
- 40.Pisters KMW, Vallières E, Crowley JJ et al. Surgery with or without preoperative paclitaxel and carboplatin in early-stage non–small-cell lung cancer: Southwest Oncology Group Trial S9900, an intergroup, randomized, Phase III trial. J. Clin. Oncol. 28(11), 1843–1849 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Betticher DC, Hsu Schmitz SF, Totsch M et al. Prognostic factors affecting long-term outcomes in patients with resected stage IIIA pN2 non-small-cell lung cancer: 5-year follow-up of a Phase II study. Br. J. Cancer 94(8), 1099–1106 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Westeel V, Quoix E, Puyraveau M et al. A randomised trial comparing preoperative to perioperative chemotherapy in early-stage non-small-cell lung cancer (IFCT 0002 trial). Eur. J. Cancer 49(12), 2654–2664 (2013). [DOI] [PubMed] [Google Scholar]
- 43.Chaft JE, Oxnard GR, Sima CS, Kris MG, Miller VA, Riely GJ. Disease flare after tyrosine kinase inhibitor discontinuation in patients with EGFR-mutant lung cancer and acquired resistance to erlotinib or gefitinib: implications for clinical trial design. Clin. Cancer Res. 17(19), 6298–6303 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang YL, Yuan JQ, Wang KF et al. The prevalence of EGFR mutation in patients with non-small-cell lung cancer: a systematic review and meta-analysis. Oncotarget 7(48), 78985–78993 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Blumenthal GM, Bunn PA Jr, Chaft JE et al. Current status and future perspectives on neoadjuvant therapy in lung cancer. J. Thorac. Oncol. 13(12), 1818–1831 (2018). [DOI] [PubMed] [Google Scholar]; •• Review article providing a comprehensive overview of the neoadjuvant treatment landscape in NSCLC.
- 46.Pataer A, Kalhor N, Correa AM et al. Histopathologic response criteria predict survival of patients with resected lung cancer after neoadjuvant chemotherapy. J. Thorac. Oncol. 7(5), 825–832 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Study showing that the percentage of viable tumor cells predicts OS and DFS in patients with resected NSCLC after neoadjuvant chemotherapy, therefore supporting the use of MPR as primary endpoint and surrogate for OS.
- 47.Cascone T, Gold KA, Swisher SG et al. Induction cisplatin docetaxel followed by surgery and erlotinib in non-small-cell lung cancer. Ann. Thorac. Surg. 105(2), 418–424 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weissferdt A, Pataer A, Vaporciyan AA et al. Agreement on major pathological response in NSCLC patients receiving neoadjuvant chemotherapy. Clin. Lung Cancer 21(4), 341–348 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Melek H, Çetinkaya G, Özer E et al. Pathological complete response after neoadjuvant/induction treatment: where is its place in the lung cancer staging system?†. Eur. J. Cardiothorac. Surg. 56(3), 604–611 (2019). [DOI] [PubMed] [Google Scholar]
- 50.Ren S, Wang C, Shen J, Zhu C. Neoadjuvant immunotherapy with resectable non-small-cell lung cancer: recent advances and future challenges. J. Thorac. Dis. 12(4), 1615–1620 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Proto C, Ferrara R, Signorelli D et al. Choosing wisely first line immunotherapy in non-small-cell lung cancer (NSCLC): what to add and what to leave out. Cancer Treat. Rev. 75, 39–51 (2019). [DOI] [PubMed] [Google Scholar]
- 52.Bruno D, Dowlati A. Immunotherapy in EGFR mutant non-small-cell lung cancer: when, who and how? Transl. Lung Cancer Res. 8(5), 710–714 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]


