Abstract
Context
Instrument-assisted soft tissue mobilization (IASTM) is a popular myofascial intervention used by health care professionals.
Objective
To document IASTM clinical practice patterns among health care professionals in the United States.
Design
Cross-sectional study.
Setting
Online survey.
Patients or Other Participants
A total of 853 members of the National Athletic Trainers' Association (n = 249) and the American Physical Therapy Association (n = 604).
Main Outcome Measure(s)
Responses to a 55-item electronic survey that assessed 4 areas, namely, IASTM training and experience, IASTM application, perception of IASTM in practice, and demographic information.
Results
Most (n = 705, 83%) of the 853 respondents used IASTM in their practice, and they had an average of 15 years of work experience. Approximately 86% (n = 731) reported completing some type of formal training, and 61% (n = 518) had completed some type of informal training. Respondents used >34 different IASTM tools. Seventy-one percent (n = 606) indicated either not knowing how to quantify the amount of force applied by the tool during treatment or not trying to quantify. Fifteen percent (n = 128) estimated a force ranging from 100 to 500g. The treatment time for a specific lesion and location ranged from 1 to ≤5 minutes, with an average total treatment time of 14.46 ± 14.70 minutes. Respondents used 31 different interventions before or after IASTM. Approximately 66% (n = 564) reported following treatment recommendations, and 19% (n = 162) described rarely or never following recommendations learned during training. A total of 94% (n = 801) recounted using some type of clinical outcome measure to assess their treatment. Cluster analysis identified 3 distinct cluster groupings among professionals, with most (89%, n = 729/818) indicating that IASTM was an effective treatment.
Conclusions
This survey documented the IASTM practice patterns of health care professionals. Cluster profiles characterized group differences in IASTM training and clinical application. The gaps among research, clinical practice, and training need to be bridged to establish IASTM best practices.
Keywords: Graston Technique, myofascial intervention, muscle soreness, perceived pain, recovery
Key Points
Large gaps exist among instrument-assisted soft tissue mobilization (IASTM) research, professional training, and clinical practice.
Respondents reported heterogeneity among professional experience, training, and use of IASTM in their clinical practices.
Cluster profiles identified group differences in IASTM training and application patterns.
Future researchers need to focus on developing clinical guidelines for various patient populations and conditions.
Instrument-assisted soft tissue mobilization (IASTM) is a popular myofascial intervention used by health care professionals such as athletic trainers (ATs), physical therapists, and chiropractors. Numerous options for selecting instruments and training alike are available to practitioners, as many companies (eg, Graston Technique; HawkGrips; FAKTR, Inc; Adhesion Breakers Inc; and The FIT Institute [fascial abrasion technique]) both manufacture instruments and teach their own treatment paradigms.
The popularity and growth of IASTM in clinical practice have also stimulated an emerging body of research. Recently, 3 systematic reviews in which investigators appraised IASTM randomized controlled trials by using similar search criteria were published. A consensus among the authors was that current IASTM research has mixed outcomes for treating musculoskeletal conditions, pain, and range of motion (ROM); stimulating physiological processes; and improving performance measures.1–3 For example, Lambert et al2 reviewed 7 qualified studies and concluded that IASTM may reduce pain and improve function over time (ie, <3 months) in patients with a variety of conditions, whereas Nazari et al3 reviewed 9 qualified studies and concluded that current evidence did not support the use of IASTM to improve pain, ROM, or function for individuals with or without a diagnosed condition. In a third review, Cheatham et al1 concluded that evidence may support IASTM for producing short-term changes in joint ROM but that the variability among study methods made it difficult to determine the potential therapeutic effects of IASTM. These mixed results demonstrate the variability among research methods across the IASTM research landscape, limiting the conclusions that can be drawn regarding effectiveness and the recommendations that can be given for the best-practice use of IASTM.4 The lack of consensus among researchers in the literature also points to potentially vast variability in the application of IASTM in clinical practice.
Currently, a consensus on clinical guidelines for an optimal IASTM intervention has not been reached regarding various components of treatment application, such as the type of instrument, stroke technique, treatment variables (eg, time, angle, and cadence), or applied pressure.1,4 Given these IASTM research discrepancies and the lack of best-practice recommendations, clinicians may have to rely on the specific treatment paradigms recommended by IASTM companies, reviews of clinical practice, or anecdotal recommendations to guide practice. However, the methods proposed by companies or anecdotal reports may not always be evidence based or, for the latter, follow the recommendations of the IASTM companies.1 For example, in their systematic review, Cheatham et al1 found that only 1 published clinical trial followed the Graston Technique's complete treatment paradigm, whereas other authors examined the effects of the Graston Technique without following the recommended treatment variables. Other investigators5 have reported substantial variations in IASTM applications across research and clinical practice, with substantial differences in treatment protocols (eg, treatment length and number of treatment sessions) and use of IASTM as an adjunct or stand-alone intervention. These practices may create confusion among researchers and clinicians, which further complicates the goal of achieving consensus on the optimal clinical guidelines for IASTM that produce the best outcomes.
To better understand the current use of IASTM and produce recommendations on IASTM application, we need to understand practice patterns among professionals. To our knowledge, surveillance on such patterns has not been reported in detail in the literature. Baker et al6 examined the preparation, perceptions, and clinical profile of 179 ATs who reported using IASTM but did not provide insight into specific IASTM treatment variables used by the ATs (eg, common treatment length and force used during treatment). Researchers have also not identified the practice patterns and IASTM application variables of other health care professions (eg, physical therapists and chiropractors). Understanding clinical application trends may further guide researchers and professionals in establishing a better consensus regarding clinical guidelines for IASTM. Therefore, the primary purpose of our study was to survey and document IASTM clinical practice patterns among different health care professionals in the United States. The secondary purpose was to assess clinician perceptions of instrument application for soft tissue mobilization.
METHODS
Participants
This cross-sectional survey study was certified exempt by the University Institutional Review Board at California State University Dominguez Hills (no. 17-202). All participants provided informed consent before beginning the survey.
Health care professionals were recruited via a sample of convenience using email to reach participants in 2 professional organizations. First, a distribution list from a random sample of members of the National Athletic Trainers' Association (n = 3000) was used; a total of 359 members on the distribution list started the survey (12% response rate). Second, the American Physical Therapy Association emailed the survey to all members of the orthopaedics (n = 17 811) and sports (n = 6597) sections; a total of 618 members from the orthopaedics section started the survey (3% response rate), and a total of 186 members of the sports section began the survey (3% response rate). A variety of professional members with different certifications and credentials participated in the survey.
Procedures
An electronic survey was developed using Qualtrics software (Qualtrics, LLC); the survey included newly developed items, as well as items validated in a previous IASTM survey research project.6 The survey was evaluated for content validity by 5 ATs (S.W.C., L.W.L., J.G.B., and 2 nonauthors) who had completed IASTM training, had previous survey research experience, had >5 years of clinical practice experience before data collection, and were not part of the initial survey design process. The survey was modified based on reviewer feedback to improve content and item clarity, and each member of the survey review panel approved the final version. The final version of the survey consisted of 55 items divided into 4 sections: IASTM training and experience, IASTM application, perception of IASTM in practice, and demographic information. The final survey used previously validated IASTM survey items,6 as well as original items not included in the previous survey, to gain greater insight into IASTM application (eg, force applied and treatment length) of IASTM-trained clinicians. The items from the previously validated survey6 were retained in the final version of our survey without change.
The first section contained 8 items (2 new items) designed to assess previous IASTM training and practice experience. The second section consisted of 11 items (10 new items) that assessed clinician practice patterns (eg, treatment length, treatment of specific conditions, adjunct modalities used with IASTM intervention, and pathologic conditions treated using IASTM). The third section contained 29 items used in the previously validated survey6 to assess perceptions of IASTM in practice. The first 12 items were related to 2 proposed constructs, as follows: (1) perceptions of traditional (ie, hands) mobilization and (2) perceptions of instrument-assisted forms of soft tissue mobilization. The remaining 17 items instructed respondents to compare the use of their hands with the use of instruments for producing certain outcomes. The fourth section contained 7 demographic questions (eg, sex, age, highest level of education, and primary work setting) created for the previously validated survey.6
Data Analysis
The data were downloaded from Qualtrics for analysis using SPSS (version 24; IBM Corp). The participant demographic and clinical practice profile items (eg, IASTM training, treatment length) were analyzed using descriptive statistics (mean ± SD) and frequency counts. The validity of the 2 proposed constructs (ie, perceptions of traditional mobilization and IASTM in practice) was assessed by conducting a principal component analysis (PCA) using maximum likelihood extraction and oblimin rotation. Data factorability was set a priori at a Kaiser-Meyer-Olkin value of ≥0.70, a Bartlett test of sphericity value of P ≤ .01 (recommended < .05), and an eigenvalue of ≥1.0 criterion.7 After estimation, items were eliminated if they (1) did not have substantial loadings (≥0.50); (2) had simultaneous, substantial cross-loadings (≥0.30); or (3) did not fit conceptually with the other items loading on the components. Components were extracted based on an eigenvalue of >1.0.8 To assess internal consistency, Cronbach α was estimated with an acceptable a priori value of ≥.70.7
We performed cluster analyses using a nonhierarchical (k-means) technique to assess patterns among responses to the 2 proposed constructs identified in the PCA. The k-means technique was chosen because it is less susceptible to multivariate outliers.9 Component scores were transformed to z scores to identify univariate outliers (z score of ≥3.29), and Mahalanobis distance was assessed on the component scores to identify multivariate outliers.9 After outlier identification and deletion, we conducted the k-means cluster analyses. After identifying cluster solutions using this analysis method, univariate F tests were calculated to ensure cluster groupings were different among cluster profiles for each of the components derived from the PCA.9
RESULTS
Preliminary Analysis
Of the 359 participants recruited from the National Athletic Trainers' Association membership email list who started the survey, 249 completed the survey (69% completion rate). Of the 618 members of the American Physical Therapy Association orthopaedics section who began the survey, 460 completed the survey (74% completion rate). Of the 186 members of the American Physical Therapy Association sports section who began the survey, 144 completed the survey (77% completion rate). Missing data were treated conservatively, and any respondent who did not complete the survey was removed from the final sample used for analysis. A total of 853 participant responses were included in the primary descriptive analyses. Additional participants were removed (n = 29) if a component score could not be calculated for them during the PCA or if component scores were identified as outliers (n = 6) for the cluster analysis. Unless otherwise stated, percentages were calculated from total responses to the survey (N = 853) rather than from the total responses to an item.
Participant Demographics and Training
Most (n = 705, 83%) of our 853 respondents (410 males [48%], 435 females [51%], 4 preferred not to identify [0.5%], and 4 did not respond [0.5%]; age = 40 ± 12.2 years; age range = 21–74 years) currently used IASTM in practice. Those who used IASTM in clinical practice had substantial clinical experience (15.3 ± 12.2 years; range = 0–54 years) and had been using IASTM in clinical practice for a number of years (mean = 14.92 years, median = 14 years, range = 1–40 years). Additional demographic information regarding respondent education, employment settings, and professional certifications and credentials is provided in Figure 1 and Tables 1 and 2.
Figure 1.
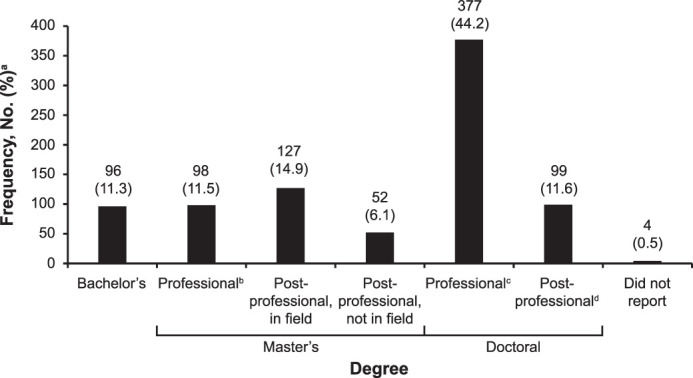
Participant-reported highest degree earned (N = 853). Adapted with permission from SLACK Incorporated.6 a Percentages were rounded, so the sum is not 100%. b Entry level. c Examples include DPT and DC. d Examples include PhD, EdD, DAT, DSc.
Table 1.
Participant-Reported Employment Setting (N = 850)*a
| Employment Setting |
Frequency, No. (%)b |
| Academic or research faculty | 70 (8.2) |
| Academic faculty clinic | 1 (0.1) |
| Chiropractic clinic | 2 (0.2) |
| Clinic, other (eg, private practice, outreach, pain, acupuncture) | 10 (1.2) |
| College or university athletic training clinic | 129 (15.2) |
| Home health | 4 (0.5) |
| Hospital | 40 (4.7) |
| Hospital, administration | 1 (0.1) |
| Hospital, other (eg, outpatient clinic) | 10 (1.2) |
| Industrial setting | 1 (0.1) |
| Middle school athletic training clinic | 1 (0.1) |
| Military | 12 (1.4) |
| Occupational health setting | 11 (1.3) |
| Performing arts | 11 (1.3) |
| Physician practice | 7 (0.8) |
| Physical therapy clinic | 457 (53.8) |
| Professional sports team athletic training clinic | 9 (1.1) |
| Secondary school athletic training clinic | 71 (8.4) |
| Other | 3 (0.4) |
Adapted with permission from SLACK Incorporated.6
Three participants did not respond.
Percentages were rounded, so the sum is not 100%.
Table 2.
Participant-Reported Professional Certifications and Credentials (N = 986)*a
| Professional Certification or Credential |
Frequency, No. (%) |
| Physical therapist | 598 (61) |
| Athletic trainer | 313 (32) |
| Certified strength and conditioning specialist | 23 (2) |
| Other (eg, certified hand therapist, certified Rolfer, USA Weightlifting, teacher) | 12 (1) |
| Massage therapist | 11 (1) |
| Orthopaedic-certified specialist | 11 (1) |
| Physical therapist assistant | 5 (1) |
| Fellow, American Academy of Orthopaedic Manual Physical Therapists | 3 (<1) |
| Sports-certified specialist | 3 (<1) |
| Emergency medical technician | 2 (<1) |
| Physician (MD, DO) | 2 (<1) |
| Acupuncturist | 1 (<1) |
| Chiropractor | 1 (<1) |
| Physician assistant | 1 (<1) |
Adapted with permission from SLACK Incorporated.6
Respondents could list as many credentials as were applicable.
Most respondents (n = 731, 85.7%) completed some type of IASTM training, with only 122 (14.3%) participants reporting having never completed any type of IASTM training. Most respondents (n = 436, 51.1%) completed at least 1 professional (ie, “official”) IASTM training course (Table 3). Of the 436 individuals who completed professional training, 322 (73.9%) described completing 1 official IASTM course, and 114 (26.1%) described completing ≥2 official courses. The official IASTM courses were primarily completed via live in-person training (n = 336); however, respondents also noted completing live web-based (n = 39) and previously recorded (eg, DVD) courses (n = 70). Many respondents (n = 143) also indicated they completed IASTM training as part of their degree curriculum coursework.
Table 3.
Participant-Reported Professional and Official IASTM Training Course Completed*
| IASTM Course |
Frequencya |
| Advanced continuing education unit IASTM technique course | 1 |
| AQuire/KOH educationb IASTM course | 1 |
| Astymc course | 60 |
| ConnecTX instrument assisted connective tissue therapyd course | 1 |
| Edge mobility tool IASTM course/eclectic approache course | 15 |
| FAKTR-PMf course | 6 |
| Fascial abrasion techniqueg IASTM course | 2 |
| FIBROBLASTERh IASTM course | 2 |
| Graston Techniquei course | 188 |
| Gua sha IASTM course | 2 |
| HawkGripsj IASTM course | 69 |
| IAM Toolsk IASTM training seminar | 5 |
| IASTMl technique course (eg, 2.0) | 9 |
| Medbridgem IASTM course | 5 |
| Medical Minds in Motionn IASTM course | 5 |
| Rehab Education° IASTM course | 19 |
| RockTape/RockBladesp IASTM course | 21 |
| Select medical/NovaCare rehabilitationq IASTM course | 17 |
| SMART TOOLSr IASTM course | 7 |
| Sound-assisted soft tissue mobilizations course | 23 |
| Técnica Gavilánt IASTM course | 16 |
| Vyne Educationu IASTM course | 3 |
| Other | 9 |
| I have not taken an official course | 417 |
Abbreviation: IASTM, instrument-assisted soft tissue mobilization.
Adapted with permission from SLACK Incorporated.6
Participants could identify each course they attended.
AQuire.
Performance Dynamics Inc.
ConnecTX.
EDGE Rehab and Sport Science.
FAKTR, Inc.
The FIT Institute.
FIBROBLASTER, LLC.
Graston Technique.
HawkGrips.
IAM Tools.
Mike Reinhold.
Medbridge, Inc.
Elite Healthcare.
Rehab Education, LLC.
RockTape, Inc.
NovaCare Rehabilitation.
SMART Tools Plus.
Carpal Therapy, Inc.
Técnica Gavilán LLC.
PESI.
The completion of “informal” IASTM training was also common across respondents. A total of 518 (60.7%) respondents completed some type of informal training (eg, in-service training, conference workshop), with 255 (29.9%) completing ≥2 informal IASTM trainings. The most frequent examples of informal training were short (ie, 1–2 h) continuing education courses, workshops, or learning laboratories at professional conferences or events. Other sources of informal training were preceptor or professional mentor training during their employment experience, fellowship training, clinical experiences as a student, attending IASTM research or clinical presentations, reading books (eg, textbooks and e-books) on IASTM, viewing “unofficial” online courses or videos (eg, YouTube), reviewing materials from IASTM training programs or companies provided by colleagues, and receiving treatment and instruction from a trained IASTM provider.
Participants' IASTM Practice Patterns
The use of IASTM was frequent among our respondents, with most indicating they used IASTM multiple times per day (n = 267; 31.3%), once per day (n = 101; 11.8%), or 2 to 3 times per week (n = 205; 24.0%). Other respondents described less consistent use, with the most common response rates of once per week (n = 73; 8.6%), once per month (n = 77; 9.0%), and once per year (n = 47; 5.5%). During IASTM application, respondents stated that several instruments were used to apply IASTM in their clinical practice (Table 4). Answers also varied regarding the amount of force respondents attempted to use (<100g [n = 25, 2.9%], 100 to 250g [n = 101, 11.8%], 250 to 500g [n = 27, 3.2%], and >500g [n = 5, 0.6%]) during IASTM application, as follows: “I don't know how to quantify the amount of force I apply during treatment” (n = 344, 40.3%) and “I don't try to quantify the amount of force I apply during treatment” (n = 262, 30.7%).
Table 4.
Participant-Reported Instruments Used in Practice*
| Instrument Type |
Frequency |
| Acuforce Massage Stara | 3 |
| Adhesion Breakersb instruments | 61 |
| Animal product (eg, horn, bone) | 23 |
| Astymc instruments | 91 |
| Edge Mobility Toold | 192 |
| FAKTRe instruments | 10 |
| FAT-Toolf | 4 |
| FIBROBLASTERg | 4 |
| Generic instrument | |
| Aluminum | 64 |
| Glass | 18 |
| Plastic | 125 |
| Polycarbonate | 48 |
| Stainless steel | 195 |
| Wood | 5 |
| Graston Techniqueh instruments | 220 |
| Gua sha instruments | 125 |
| HawkGripsi instrument | 160 |
| IAM toolsj | 7 |
| Myobark | 3 |
| Ellipse tool/myofascial releaserl | 7 |
| Rock bladesm | 31 |
| SMART TOOLSn | 7 |
| Sound assisted soft tissue mobilization instrument° | 36 |
| ST3 Fuzion toolsp | 3 |
| Stone instrument | 39 |
| Técnica Gavilán instrumentsq | 21 |
| Zuka toolsr | 4 |
| Other | |
| Butter knife | 2 |
| Cups | 16 |
| Reflex hammer | 6 |
| Tongue depressor | 2 |
| Silicone instrument | 5 |
| Self-made | 1 |
| Massage sticks, percussion devices, etc | 13 |
Adapted with permission from SLACK Incorporated.
STAR tool, Mobility Stars.
Adhesion Breakers Inc.
Performance Dynamics Inc.
EDGE Rehab and Sport Science.
FAKTR, Inc.
The FIT Institute.
FIBROBLASTER, LLC.
Graston Technique.
HawkGrips.
IAM Tools.
Myo-Bar, LLC.
Myofascial Releaser.
RockTape, Inc.
SMART Tools Plus.
Carpal Therapy, Inc.
Soft Tissue Therapy Tools Inc.
Técnica Gavilán LLC.
Zuka Tools, Inc.
Respondents reported typically treating a specific lesion and location for <1 minute (n = 47, 5.5%), 1 to 2 minutes (n = 189, 22.2%), 2 to 3 minutes (n = 215, 25.2%), 3 to 5 minutes (n = 212, 24.9%), or ≥5 minutes (n = 92, 10.8%); the average IASTM treatment application for a specific lesion was 3.15 ± 1.12 minutes (median = 3 minutes, mode = 3 minutes). The average time for a complete IASTM treatment was 14.46 ± 14.70 minutes (range = 1–60 minutes, median = 10 minutes, mode = 5 minutes), with an average of 2.36 specific lesions and locations (range = 1–15 locations, median = 2 locations, mode = 2 locations) treated during an individual IASTM session. Respondents observed that they used other modalities before or after IASTM application (Table 5) as part of a complete treatment protocol and used a number of clinical measures to assess IASTM effectiveness (Table 6).
Table 5.
Participant-Reported Treatments Applied Before or After Instrument Application
| Treatment |
Instrument-Assisted Soft Tissue Mobilization, No. |
|
| Before |
After |
|
| Aerobic exercise or dynamic movement | 78 | 11 |
| Bicycle, treadmill, or upper body exercise | 16 | 2 |
| Continuous ultrasound | 118 | 20 |
| Pulsed ultrasound | 47 | 14 |
| Diathermy | 8 | 1 |
| Hot pack | 297 | 72 |
| Cold pack | 14 | 155 |
| Warm whirlpool | 7 | 0 |
| Contrast bath | 1 | 0 |
| Compression unit (eg, Game Ready) | 0 | 3 |
| Concentric exercise | 263 | 477 |
| Eccentric exercise | 223 | 505 |
| Corrective exercise | 0 | 6 |
| Functional exercise | 0 | 9 |
| Massage | 284 | 210 |
| Manual soft tissue mobilization | 10 | 10 |
| Light therapy | 63 | 63 |
| Laser (class IV) therapy | 0 | 1 |
| Stretching | 284 | 586 |
| Proprioceptive neuromuscular facilitation techniques | 2 | 4 |
| Joint mobilizations | 11 | 12 |
| Thrust manipulation | 2 | 2 |
| Dry needling | 12 | 2 |
| Foam rolling | 3 | 1 |
| Cupping | 2 | 3 |
| Electrical stimulation | 2 | 5 |
| Iontophoresis | 0 | 1 |
| Kinesiology tape | 1 | 7 |
| Taping or bracing | 0 | 6 |
| Mechanical diagnosis and therapy | 1 | 1 |
| Neurodynamics | 1 | 2 |
| None | 7 | 7 |
| Varied based on patient need | 9 | 7 |
Table 6.
Participant-Reported Clinical Measures Used to Assess Instrument-Assisted Soft Tissue Mobilization Treatment Effectiveness (N = 853)
| Clinical Measure |
No. by Response |
|
| Yes |
No |
|
| Joint range of motion (eg, goniometer measurement) | 555 | 298 |
| Pain pressure threshold | 247 | 606 |
| Patient-reported outcome scale (eg, pain scale) | 639 | 214 |
| Movement testing (eg, Functional Movement Screen, selective functional movement assessment) | 222 | 631 |
| Strength testing (eg, manual muscle test) | 189 | 664 |
| Functional testing (eg, balance test) | 218 | 635 |
| I do not commonly assess treatment effectiveness | 52 | 801 |
| Othera | ||
| Sport-specific testing | 1 | |
| Palpate tissue texture changes | 7 | |
| Girth measurements | 1 | |
| Gait assessment | 2 | |
| Neural tension tests | 2 | |
| Flexibility assessment | 3 | |
| Observe scar improvement | 1 | |
| Observe skin color (eg, petechiae) changes | 1 | |
| Functional asterisk sign | 3 | |
| Subjective patient-reported improvement | 5 | |
Other was an open response box, with participants listing any additional tests used.
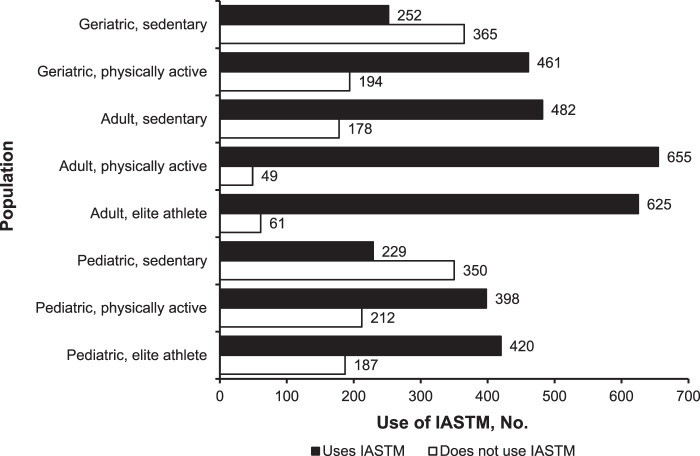
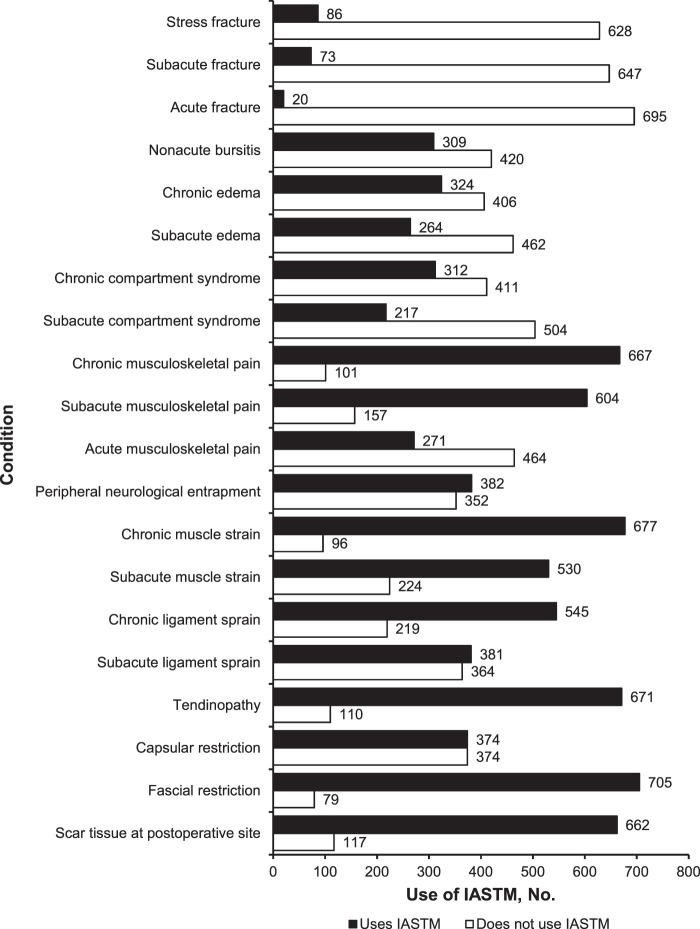
Respondents rarely indicated recommending multiple IASTM treatments per day (n = 9, 1.1%) or spaced treatments, such as 1 treatment per month (n = 24, 2.8%), to their patients. They reported more often recommending 1 treatment per day (n = 73, 8.6%), 1 treatment every couple of days (n = 533, 62.5%), or 1 treatment per week (n = 111, 13.0%). Regarding treatment protocol guidelines during IASTM training, most respondents indicated they always (n = 80; 9.4%), usually (n = 308; 36.1%), or sometimes (n = 176; 20.6%) followed the advice. However, several respondents commented that they either rarely (n = 61, 7.2%) or never (n = 101, 11.8%) followed the training recommendations. Respondents also stated they would use IASTM as part of their treatment protocol to treat a variety of patient populations (Figure 2) and conditions (Figure 3).
Figure 2.
Participant-reported use of instrument-assisted soft tissue mobilization (IASTM) as part of the treatment protocol with different populations.
Figure 3.
Participant-reported use of instrument-assisted soft tissue mobilization as part of the treatment protocol with different conditions.
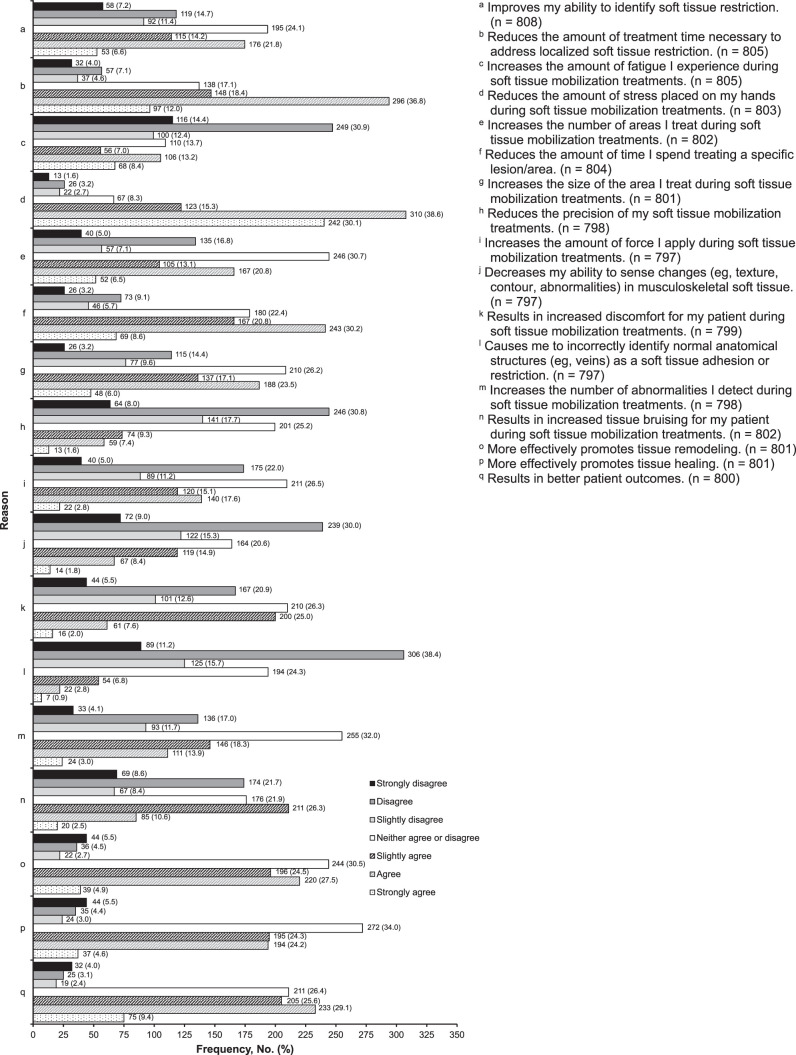
Respondents replied to items designed to compare perceptions of using instruments versus one's hands to apply soft tissue mobilization. Most agreed that instruments reduced the time needed to reach treatment goals and improved treatment precision while reducing clinician fatigue and stress on the hands. Substantial agreement regarding perceptions of instruments as more effective for promoting tissue remodeling, tissue healing, and patient outcomes was present among those who responded to each item (Figure 4). Answers were more neutral, or in slight agreement, with respect to instrument use increasing the number of sites treated, the treatment force used, the tissue abnormalities found, and patient discomfort and bruising among those who responded to each item (Figure 4).
Figure 4.
Frequency of agreement with reasons for applying soft tissue mobilization via instruments compared with hands. Percentages were rounded, so the sum in some rows does not equal 100%. *Adapted with permission from SLACK Incorporated.6
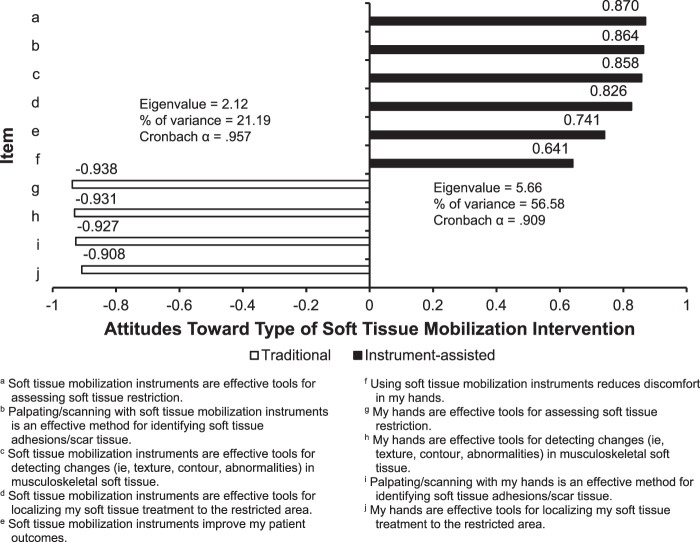
Principal Component Analysis
Initial PCA resulted in the removal of 2 items (17%) that exhibited substantial cross-loadings and poor conceptual fit on a component. Data factorability of the final solution was met with a Kaiser-Meyer-Olkin value of 0.891 and a Bartlett test of sphericity that was different ( = 7787.61, P < .001). The final PCA solution revealed a 2-component structure that consisted of 10 survey items (Figure 5). The first component contained 6 items that represented attitudes toward the use of instruments (ie, “attitudes toward the use of instruments for soft tissue mobilization”; instrument assisted). The second component contained 4 items related to the use of one's hands for soft tissue mobilization (ie, “attitudes toward the use of one's hands for soft tissue mobilization”; traditional). All items included in the final component structure had substantial loadings (ie, primary loading of ≥0.64) on a single factor, without simultaneous, substantial cross-loadings (ie, all cross-loadings of ≤0.30). The components extracted had eigenvalues of >1.0 and Cronbach α values of >.90 (Figure 5).
= 7787.61, P < .001). The final PCA solution revealed a 2-component structure that consisted of 10 survey items (Figure 5). The first component contained 6 items that represented attitudes toward the use of instruments (ie, “attitudes toward the use of instruments for soft tissue mobilization”; instrument assisted). The second component contained 4 items related to the use of one's hands for soft tissue mobilization (ie, “attitudes toward the use of one's hands for soft tissue mobilization”; traditional). All items included in the final component structure had substantial loadings (ie, primary loading of ≥0.64) on a single factor, without simultaneous, substantial cross-loadings (ie, all cross-loadings of ≤0.30). The components extracted had eigenvalues of >1.0 and Cronbach α values of >.90 (Figure 5).
Figure 5.
Principal component analysis pattern matrix loadings. Adapted with permission from SLACK Incorporated.6
Cluster Analysis
We conducted a cluster analysis to assess patterns among respondents for the 2 proposed constructs identified in the PCA (ie, instrument-assisted and traditional approaches). Univariate outliers (n = 6) were identified and removed from the sample before analysis. A 3-cluster solution was accepted because it met the analysis procedure criteria (eg, univariate F tests that were different).9 The 3-cluster solution was also accepted because it theoretically represented distinct profiles regarding perceptions of instrument-assisted versus traditional soft tissue mobilization (Figure 6).
Figure 6.
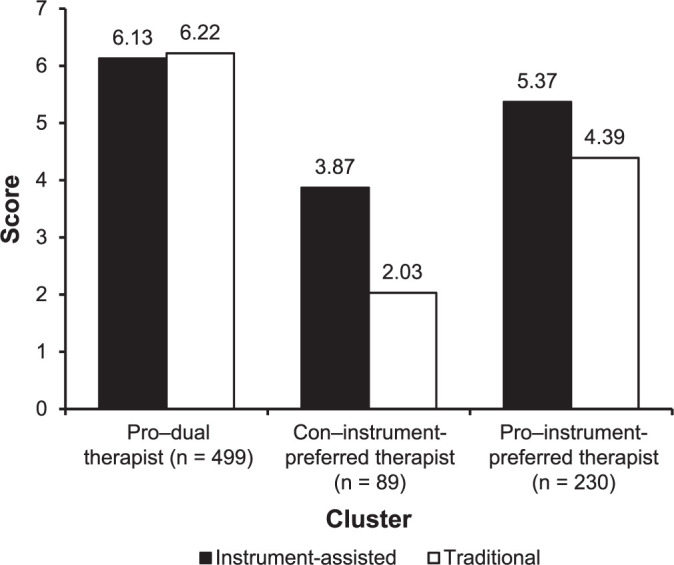
Cluster analysis solution. Profile scores on the 2 components of the principal component analysis. The solution presents mean scores for each component by cluster grouping.
Cluster 1 was labeled pro–dual therapist because mean scores indicated substantial agreement that both instrument-assisted and traditional approaches were effective (Figure 6). Members of this cluster profile had strong positive mean scores (instrument assisted = 6.13 ± 0.59, traditional = 6.22 ± 0.55) on the 2 components. The pro–dual therapist group contained 499 (61%) of the participants (n = 818); 476 (95%) in this cluster indicated IASTM application was part of their clinical practice. Members of this cluster reported completing 1.84 ± 0.88 official and 2.18 ± 1.21 informal courses, using IASTM for 15.18 ± 4.28 years, and treating 2.52 ± 1.45 lesions and locations over an IASTM treatment time of 13.01 ± 12.93 minutes.
Cluster 2 was labeled con–instrument-preferred therapist because mean scores described attitudes that were either more neutral toward or against the clinical effectiveness of both instrument-assisted and traditional approaches. However, the scores reflected a preference for instruments over traditional approaches, as reflected in a higher mean score (Figure 6). Members of this cluster profile had neutral mean scores for the instrument-assisted component (3.87 ± 1.26) and their scores indicated disagreement about the effectiveness of the traditional component (2.03 ± 0.81). The con–instrument-preferred therapist group contained 89 (11%) of the participants (n = 818); 50 (56%) in this cluster noted that IASTM application was part of their practice. Members of this cluster described completing 1.29 ± 0.64 official and 1.74 ± 0.94 informal courses, using IASTM for 13.74 ± 2.75 years, and treating 1.66 ± 0.91 lesions and locations during an IASTM treatment time of 17.02 ± 17.29 minutes.
Cluster 3 was labeled pro–instrument-preferred therapist because mean scores indicated agreement with or neutral attitudes toward the effectiveness of the instrument-assisted and traditional approaches. However, scores showed a preference for instruments over traditional approaches (Figure 6). Members of this cluster profile displayed mean scores on the instrument-assisted component (5.37 ± 0.92) that demonstrated agreement that the instruments were effective for soft tissue mobilization. Mean scores were more neutral for the effectiveness of the traditional component (4.39 ± 0.72). The pro–instrument-preferred therapist group contained 230 (28%) of the participants (n = 818), with 169 (74%) in this cluster indicating that IASTM application was part of their practice. Members of this cluster reported completing 1.45 ± 0.85 official and 1.96 ± 1.1 informal courses, using IASTM for 14.69 ± 5.12 years, and treating 2.21 ± 1.72 lesions and locations over an IASTM treatment time of 17.21 ± 17.19 minutes.
DISCUSSION
We are the first to document specific IASTM clinical practice patterns among 853 respondents from different health care professions in the United States, and our study is the largest survey detailing the professional training and perceptions of clinicians who use IASTM. Several findings emerged from the survey regarding clinician training for, application patterns of, and perceptions of IASTM therapy.
Participant Demographics and Training
Most participants related substantial clinical experience in general (experience = 15.3 ± 12.2 years) and with IASTM (mean = 14.92 years, median = 14 years). Approximately 86% of respondents stated they had completed some type of formal IASTM training through live professional continuing education, web-based courses, degree curriculum coursework, or recorded training videos. Approximately 14% admitted never completing any type of formal IASTM training. Sixty-one percent of respondents also described completing some type of informal training through short (ie, 1–2 hour) continuing education courses, conference workshops, clinical presentations, professional mentorship training, textbook or e-books, unofficial online courses, and self-study using unofficial websites or online videos. Our results support those of previous researchers6,10 who advised health care professionals to seek informal training to enhance clinical skills.
Currently, >10 major IASTM tool manufacturers offer some type of formal professional training using their tools and own preferred approach.4 Although professionals are completing formal training, the lack of consensus on best-practice recommendation and differences in how manufacturers teach their techniques may result in wide variability of applications among those who have completed formal training. For example, some tool manufacturers teach a multimodal treatment approach, whereas others may teach only the IASTM tool portion of an intervention strategy.1 Furthermore, many informal sources exist for IASTM training, and our findings suggest that professionals search for or completion of informal training may be driven by personal preference versus evidence. Inconsistent research methods and results, gaps in the knowledge base, and variations or questionable quality of formal and informal sources of information make it a challenge to disseminate accurate information or provide best-practice recommendations to the many clinicians who use IASTM in their clinical practice. The variability between what is taught in formal courses and what occurs in practice may also be a reason why clinicians seek or complete multiple courses of additional formal and informal training.6 However, given that many instrument manufacturers sell instruments without requiring formal training before purchase, clinicians may seek informal training or mentorship from more experienced clinicians to bridge the gap in their knowledge.
The training data revealed the diversity among trained professionals and the many different methods of learning IASTM. This diversity in education and training may explain the gap between research and clinical practice or the widely varied application approaches used in clinical trials and case studies or series research.1,5 It is also possible that variations occur because of differences in recommendations provided by IASTM instrument manufacturers. Our results showed that clinicians often completed formal training from multiple providers. Another source of variation among manufacturers is the reliance on research conducted on other IASTM techniques to support their specific IASTM application. For example, a manufacturer may teach a certain IASTM treatment strategy using its tools but rely on other IASTM research to support the techniques, and attendees may not be aware of the differences. In many cases, these differences result in course content that is not evidence based because referenced studies using different instruments or techniques may not truly support the effectiveness of a specific IASTM protocol. Clinicians should consider these variables when integrating IASTM into their clinical practice. In a recent clinical commentary, Cheatham et al4 attempted to address these concerns by urging researchers and clinicians to develop a consensus on clinical practice guidelines to bridge the gap between research and clinical practice. The overall findings suggest that clinicians who use IASTM should complete some form of IASTM training to guide their practice.
Respondent IASTM Practice Patterns
Our survey also included items designed to assess patterns among health care professionals regarding IASTM application procedures. For frequency of treatment, approximately 43% (n = 368) of respondents reported using IASTM ≥1 times per day. Respondents also indicated using >34 different IASTM tools in their practice. Interestingly, 71% (n = 606) commented on not knowing how to quantify the amount of force applied or not trying to quantify the force applied during IASTM treatment. Another 15% (n = 128) described using a compression force with the tool that ranged from 100 to 500g, which is similar to forces (250–300g) that promoted healing in laboratory animals when IASTM was applied after a ligamentous injury.11 The treatment time used for a specific lesion and location ranged from 1 to ≥5 minutes, with an average total IASTM treatment time of approximately 14 minutes. Our findings revealed that clinicians used treatment times that were similar to those used in research protocols of 40 seconds to 18 minutes.5
Respondents also noted that their IASTM application was often combined with other interventions or modalities; 31 other interventions were used before or after IASTM treatment (Table 5). An IASTM intervention was often combined with exercise, manual therapy, or another modality (eg, ultrasound). Our observation that clinicians who applied IASTM with manual therapy techniques is similar to previous results.6 However, our findings were unique in characterizing respondent perceptions of how often treatment recommendations from their IASTM training were followed. Approximately 66% of participants related following treatment recommendations at some level of commitment (ie, sometimes, usually, or always), and 19% rarely or never followed recommendations learned in their training. Therefore, clinicians frequently deviate from training recommendations, which may help to explain the variations in previous clinical trial and case study research.1,5
Another novel finding in our study was how often clinicians tracked treatment outcomes when using IASTM. Most respondents (94%) said they used some type of clinical measure to assess the efficacy of their IASTM treatment; 16 measures were cited. Several of these were consistent with measures used in ASTM research.4 The most common measures were patient-reported outcomes (eg, pain scale) and ROM assessment. The use of these measures is not surprising given that IASTM is often purported to decrease pain and increase ROM in training programs and that these are the outcomes most consistently reported by researchers to support IASTM effectiveness.1,5 In addition, our results showed that 6% (n = 52) of respondents described not using any clinical measures to assess IASTM effectiveness (Table 6). Thus, clinicians may rely on 1 or 2 clinical measures to assess treatment effectiveness, which is congruent with other findings on the use of clinical measures to assess rehabilitative progress.12
Respondents indicated using IASTM to treat a variety of populations (n = 8 populations) and conditions (n = 20 conditions), which is consistent with the results of previous researchers who suggested ATs use IASTM to treat a variety of conditions and often select instruments over their hands to provide soft tissue mobilization techniques (Figures 2 and 3).6
In summary, the survey data revealed continued heterogeneity in professional practice patterns. This corresponds with the previous subsection in which we discussed the diversity among IASTM education and training offerings that teach clinical practice strategies. Most professionals displayed an attempt to follow the guidelines from the training received from a specific manufacturer but also indicated a willingness to deviate from these recommendations. Hence, clinicians may follow recommendations from manufacturers that are not always based on the best evidence; however, the findings could also reflect that clinicians deviate from manufacturers' recommendations they decide are not based on evidence or biological plausibility. Furthermore, it may be reasonable to presume that an IASTM treatment will be modified according to a patient's clinical presentation and needs or to a clinician's expertise when the training recommendations are deemed inappropriate for a specific clinical circumstance.
A closer connection among research, training, and clinical practice guidelines is warranted. The willingness to deviate from training recommendations, combined with the variations in training, may explain the inconsistencies in the literature regarding treatment effectiveness. For example, Cheatham et al1 found a discrepancy in the IASTM research using the Graston Technique. This technique uses a sequential multimodal protocol,1 yet in 5 clinical trials, the researchers reported using a modified version of the technique that excluded parts of the treatment protocol. This information supports the need for more universal consensus among the research, IASTM education, and practice patterns, with a focus on determining how variations in application (eg, force, rate) affect treatment outcomes.
Perceptions of IASTM Effectiveness
Our secondary purpose was to assess clinician perceptions regarding the use of instruments in clinical practice, with a focus on comparing the use of their hands versus instruments. Instrument manufacturers have proposed that, compared with using one's hands, using instruments can improve soft tissue application. The general response from our sample was that using instruments was as effective as or more effective than using one's hands for soft tissue mobilization. Most of our respondents agreed that using instruments reduced treatment time, decreased fatigue and stress placed on a clinician's hands, improved tissue healing and remodeling, increased the precision of their treatment, and resulted in better patient outcomes (Figure 4). The majority did not indicate that using instruments increased the number of areas treated, size of the area treated, amount of force used during treatment, or amount of patient discomfort during soft tissue mobilization. These results are consistent with those previously reported regarding the perceptions of ATs who use instruments.6
Our survey was also designed to assess 2 proposed constructs concerning perceptions of IASTM. We were able to examine individual patterns regarding clinical perception and group individuals based on their responses to the constructs.9 Our analysis revealed a 10-item solution, with 6 items in an instrument-assisted factor and 4 items in a traditional factor (Figure 5). This factor solution was similar to that reported by Baker et al6 in a sample of ATs; however, our solution had 2 more items (ie, “Soft tissue mobilization instruments improve my patient outcomes” and “Using soft tissue mobilization instruments reduces discomfort in my hands”) in the instrument-assisted factor.
Our cluster analysis revealed 3 distinct cluster groupings: (1) a group that agreed their hands and instruments were equally effective tools for applying soft tissue mobilization (ie, pro–dual therapist), (2) a group that moderately agreed with the concept that instruments were effective while remaining more neutral regarding the use of their hands (ie, pro–instrument-preferred therapist), and (3) a group that did not indicate support for soft tissue mobilization with either approach but offered more support for the use of instruments over their hands (ie, con–instrument-preferred therapist). Members of the pro–dual therapist group described completing more IASTM training, formal and informal, than the other 2 cluster groupings. Respondents in this group used IASTM in clinical practice more than the other 2 cluster groups (95% versus 56% for con–instrument-preferred therapist or 74% for pro–instrument-preferred therapist) and applied IASTM to more locations during shorter treatment sessions. Of note, the largest 2 cluster groups (ie, pro groups; 89% of respondents) supported instrument use, indicating that most respondents perceived instruments to be effective tools for soft tissue mobilization.
We are the first researchers to cluster clinicians into groups based on their perceptions of instrument use. Overall, this analysis may be more enlightening than other descriptive data. Essentially, our cluster analysis results revealed that clinicians were likely to fall into 1 of 3 categories regarding the effectiveness of instruments and soft tissue mobilization. Based on the results, a large group of clinicians had a positive outlook on soft tissue mobilization and believed that treatments could be effectively applied with either instruments or their hands to more locations and lesions over shorter periods. A substantial but smaller portion of clinicians also endorsed the use of soft tissue mobilization in clinical practice; they believed that using instruments was slightly more effective than using their hands but applied those treatments to fewer locations over a longer period than the first group. The third group was less likely to use instruments or soft tissue mobilization in general in their practice. This group favored instruments over their hands for soft tissue mobilization treatments but had less IASTM training and experience than the other 2 groups. This group was also likely to treat fewer locations over a longer treatment duration. Therefore, it may be valuable to explore the reasons or concerns driving the cluster groupings. Examining the factors or experiences that influence beliefs or clinical practice (eg, clinicians who are more likely to apply manual therapies over other interventions and the effect of instrument advertising on clinician perceptions) and their potential mediators may be important for understanding clinical practice patterns and perceptions regarding instrument application for soft tissue mobilization.
Practice Implications and Future Research
No universal consensus exists on clinical guidelines for the optimal IASTM intervention, including the type of instrument, stroke technique, treatment variables (eg, time, angle, and cadence), or applied pressure.1 Our results support the idea that heterogeneity exists among health care professionals regarding clinical practice patterns. The inconsistencies may be due to (1) diversity of respondent training and experience, (2) heterogeneity among available IASTM educational and training offerings, and (3) lack of adherence to recommended treatment paradigms. However, variations in clinical practice will continue to exist until universal guidelines are developed. Future researchers should attempt to bridge the gaps among research, training, and clinical practice. This may be accomplished by conducting research to answer questions regarding clinical guidelines, particularly for different groups of patients. Investigators should also try to determine how IASTM can be integrated into a multimodal treatment program for different pathologic conditions. Additionally, researchers should assess how modes of instruction or types of training affect practice patterns and patient outcomes.
Limitations
Several limitations of this study need to be discussed. First, the survey was sent to a sample of health care professionals that included physical therapists and ATs. The electronic survey was sent via email; however, other methods of survey sampling, such as mailings or social media, might have produced a higher response rate and different results. Second, the survey asked questions regarding specific areas of IASTM. Different questions might have revealed different ideas of how health care professionals use IASTM in their practice. Third, this survey was sent to individuals with membership in specific organizations; therefore, the results may not completely represent the perceptions and practices of nonmembers or other health care professionals. Still, the results provide some insight into responses from these professionals. Fourth, this was the first survey to document responses regarding IASTM among different health care professionals who work in diverse clinical settings. Patient demographics and practice patterns may have influenced their beliefs and use of IASTM.
CONCLUSIONS
This was the first survey to document IASTM practice patterns among health care professionals. These results support the existence of large gaps among IASTM research, professional training, and clinical practice. Respondents reported heterogeneity among professional experience, training, and use of IASTM in their clinical practice. Cluster profiles of clinicians indicated group differences in IASTM training and application patterns. This diversity poses a concern because of inconsistencies in the literature and training, as well as a lack of best-practice recommendations for IASTM application. Future researchers need to focus on developing clinical guidelines for different patient populations and pathologic conditions.
REFERENCES
- 1.Cheatham SW, Lee M, Cain M, Baker R. The efficacy of instrument assisted soft tissue mobilization: a systematic review. J Can Chiropr Assoc . 2016;60(3):200–211. [PMC free article] [PubMed] [Google Scholar]
- 2.Lambert M, Hitchcock R, Lavallee K, et al. The effects of instrument-assisted soft tissue mobilization compared to other interventions on pain and function: a systematic review. Phys Ther Rev . 2017;22(1–2):76–85. doi: 10.1080/10833196.2017.1304184. [DOI] [Google Scholar]
- 3.Nazari G, Bobos P, MacDermid JC, Birmingham T. The effectiveness of instrument-assisted soft tissue mobilization in athletes, participants without extremity or spinal conditions, and individuals with upper extremity, lower extremity, and spinal conditions: a systematic review. Arch Phys Med Rehabil . 2019;100(9):1726–1751. doi: 10.1016/j.apmr. 2019.01.017. [DOI] [PubMed] [Google Scholar]
- 4.Cheatham SW, Baker R, Kreiswirth E. Instrument assisted soft-tissue mobilization: a commentary on clinical practice guidelines for rehabilitation professionals. Int J Sports Phys Ther . 2019;14(4):670–682. [PMC free article] [PubMed] [Google Scholar]
- 5.McMurray J, Landis S, Lininger K, Baker RT, Nasypany A, Seegmiller J. A comparison and review of indirect myofascial release therapy, instrument-assisted soft tissue mobilization, and active release techniques to inform clinical decision making. Int J Athl Ther Train . 2015;20(5):29–34. doi: 10.1123/ijatt. 2015-0009. [DOI] [Google Scholar]
- 6.Baker RT, Start A, Larkins L, Burton D, May J. Exploring the preparation, perceptions, and clinical profile of athletic trainers who use instrument-assisted soft tissue mobilization. Athl Train Sports Health Care . 2018;10(4):169–180. doi: 10.3928/19425864-20180201-02. [DOI] [Google Scholar]
- 7.Leech NL, Barrett KC, Morgan GA. IBM SPSS for Intermediate Statistics: Use and Interpretation 5th ed. Routledge; 2014.
- 8.Tabachnick BG, Fidell LS. Using Multivariate Statistics 6th ed. Pearson; 2013.
- 9.Grimm LG, Yarnold PR. Reading and Understanding More Multivariate Statistics American Psychological Association; 2000.
- 10.Armstrong KJ, Weidner TG. Formal and informal continuing education activities and athletic training professional practice. J Athl Train . 2010;45(3):279–286. doi: 10.4085/1062-6050-45.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loghmani MT, Warden SJ. Instrument-assisted cross-fiber massage accelerates knee ligament healing. J Orthop Sports Phys Ther . 2009;39(7):506–514. doi: 10.2519/jospt.2009.2997. [DOI] [PubMed] [Google Scholar]
- 12.Nicholas P, Hefford C, Tumilty S. The use of the Patient-Specific Functional Scale to measure rehabilitative progress in a physiotherapy setting. J Man Manip Ther . 2012;20(3):147–152. doi: 10.1179/2042618612y.0000000006. [DOI] [PMC free article] [PubMed] [Google Scholar]