Abstract
We outline a case of success in the rehabilitation of a Romanian first-division soccer player who sustained an anterior cruciate ligament (ACL) rupture with a meniscal tear during competition in the 2012–2013 season. The ligament was reconstructed with an autologous hamstrings graft and partial meniscectomy was performed. The player returned to same-level competition in 7 months and has remained at that level, free of knee injury, to the present (6 years later). Based on postoperative phase 1 as proposed by the Royal Dutch Society for Physical Therapy, we proposed a clinical progression of exercises with video demonstrations to address body functions and structures and the level of activities and participation. All phase 1 objectives were achieved, and all criteria needed to advance to phase 2 of the ACL rehabilitation process were attained.
Keywords: knee, recovery, football
Key Points
The Royal Dutch Society for Physical Therapy evidence statement is an efficient guide for the first phase of anterior cruciate ligament reconstruction rehabilitation in a professional soccer player.
For a professional soccer player pursuing rehabilitation after anterior cruciate ligament reconstruction, progressions should be based on the achievement of functional goal-based criteria rather than time-based protocols.
Anterior cruciate ligament (ACL) rupture is an increasingly troublesome injury for soccer players.1 A 15-year prospective study showed an average annual increase in the ACL injury rate of 6%, reaching 0.340 and 0.017 ACL injuries per 1000 hours during matches and training sessions, respectively.2 Researchers2 showed that 100% of professional players treated with ACL reconstruction for a total rupture returned to soccer training and more than 90% returned to match play within 1 year of ACL reconstruction. However, 3 years after such an injury, only 65% of the players had returned to their previous level of competition.2 Recently, The Royal Dutch Society for Physical Therapy (KNGF) instructed a multidisciplinary group of Dutch ACL experts to develop an evidence statement for rehabilitation after ACL reconstruction.3
CASE PRESENTATION
In this validation clinical case report, which was supported with videos and based on the KNGF evidence statement for ACL reconstruction rehabilitation, we outline the successful rehabilitation of a Romanian first-division soccer player who sustained an ACL rupture and meniscal tear during competition in the 2012–2013 season. The ligament was reconstructed with an autologous hamstrings graft, and partial meniscectomy was performed. The player returned to the same level of competition in 7 months and has remained at that level, free of knee injury, to the present (6 years later). We have found that it is more appropriate to incorporate functional goal-based criteria in the rehabilitation protocol than to use time-based protocols.3 Therefore, the duration of each phase was based on this player's rehabilitation process.
Based on the postoperative mechanical loading progressive phase 1 (3 weeks) as proposed by the KNGF (Table 1), we proposed the following progression of exercises in each level in addition to daily physiotherapy care.
Table 1.
Postoperative Phase 1: The Royal Dutch Society for Physical Therapy Evidence Statement for Anterior Cruciate Ligament Reconstruction Rehabilitation3
| Goal Phase 1:“minimal synovitis/effusion, extension 0°, voluntary quadriceps control, active dynamic gait pattern” | |
| Level of Body Functions and Structures | |
| Mobility |
Strength Training |
| Active and/or passive knee extension exercises when there is an extension deficit. Aim at an extension of 0° in 2 to 4 weeks. | Reactivation of the quadriceps: active knee extensions when seated with the legs straightened. |
| Progress from isometric quadriceps exercise to concentric and eccentric exercises provided that the knee does not react with increasing temperature, effusion, and/or pain. | |
| Heel slides to improve knee flexion. Aim at 120–130° of flexion in 4 to 6 weeks. | Closed kinetic chain quadriceps training (ROM 0-60°). |
| Open kinetic chain quadriceps exercises can be performed without resistance from week 4 in ROM 90–45°. Increase ROM by 10° each week. | |
| Concentric and eccentric strength training of the gluteal muscles, hamstrings, and calf muscles | |
| Level of Activities and Participation | |
| Walking and Bicycling |
Neuromuscular Training |
| Load the operated leg. Practice gait at different speeds and on various surfaces | Neuromuscular training on two legs. Gradually increase difficulty by adding perturbation; training on one leg; training on an increasingly difficult board; training with eyes closed; and adding tasks, such as catching and throwing a ball or answering a difficult arithmetical problem. |
| Start cycling on a home trainer when knee flexion reaches 100°. Use cycling as a warm-up and mobilization exercise. | Encourage correct quality of performance during strength training and walking. |
| Criteria to Start Phase 2: | |
| Knee extension of at least 0° and 120–130° flexion. | |
| Voluntary control of the quadriceps. | |
| Active dynamic gait pattern without crutches. | |
| Correct qualitative performance of phase 1 exercises. | |
Abbreviation: ROM, range of motion.
Reproduced from Br J Sports Med, van Melick N, van Cingel RE, Brooijmans F, et al. 50 (24), 1506–1515, 2016, with permission from BMJ Publishing Group Ltd.
To achieve the proposed objectives with respect to body functions and structures, our criterion was to start with seated, active knee flexion-extension in combination with electrostimulation, heel slides to improve knee flexion, and the legs straightened at the end of extension (see Supplemental Video 1, available online at http:dx.doi.org/10.4085/1062-6050-164-21.S1) during the first 5 days of postoperative rehabilitation, progressing from 2 to 4 sets. (Table 2). We then used the same exercise in a horizontal closed kinetic chain (CKC) manner with manual grips that allowed the player to autonomously improve knee flexion (Supplemental Video 2) during the next 5 days of postoperative rehabilitation, advancing from 2 to 4 sets (Tables 2 and 3). Near the end of this phase, we introduced the same exercise in vertical CKC fashion with a FitBALL (Ball Dynamics) on the back that allowed the athlete to continue improving knee flexion (Supplemental Video 3) during the last 11 days of this phase, progressing from 2 to 4 sets during the first 5 days and alternating 2 and 4 sets during the last 6 days (Tables 3 and 4). We used electrostimulation because, when combined with conventional rehabilitation, it may be more effective for improving muscle strength in the first phase of ACL rehabilitation4 while not affecting gains in knee extension and flexion or inducing pain or effusion.3 We prescribed these exercises in 3.5-minute repetitions (reps), which is the recommended duration for improving muscle strength. Recovery time between sets was 5 minutes, so we used this interval for concentric and eccentric strength training of the gluteal (Supplemental Video 4), adductor (Supplemental Video 5), and hamstrings muscles (Supplemental Video 6). At the end of this phase, we added the calf muscles (Supplemental Video 7). The progression in volume was from 2 times with 8 reps to 3 times with 10 reps, combined with a gradual load increase from very low to medium and 3 to 5 minutes of rest between sets (Tables 2, 3, and 4).
Table 2.
Postoperative Rehabilitation Week 1: Progression of Strength Exercises
| Exercises |
Sets or Reps by Day |
||||||
| 1 |
2 |
3 |
4 |
5 |
6 |
7 |
|
| Level of body functions and structures | |||||||
| Seated active knee flexion-extension with heel slides + ESM | 2 × 3.5-min ESM | 2 × 3.5-min ESM | 3 × 3.5-min ESM | 3 × 3.5-min ESM | 4 × 3.5-min ESM | ||
| Horizontal closed kinetic chain with manual grips + ESM | 2 × 3.5-min ESM | 2 × 3.5-min ESM | |||||
| Gluteal strength training | 2 × 8 reps (−) | 2 × 8 reps (−) | 3 × 8 reps (−) | 2 × 8 reps (+) | |||
| Adductor strength training | 2 × 8 reps (−) | 2 × 8 reps (−) | 2 × 8 rep (+) | ||||
| Hamstrings strength training | 1 × 8 reps (−) | 1 × 8 reps (−) | 1 × 8 reps (−) | 2 × 8 reps (−) | |||
| Level of activities and participation: displacement progression | |||||||
| Anterior-posterior direction | 2 × 4 reps (−) | 2 × 4 reps (−) | 1 × 4 reps (−) | 1 × 4 reps (−) | 2 × 4 reps (+) | 2 × 4 reps (+) | 2 × 4 reps (+) |
| Lateral direction | 1 × 4 reps (−) | 1 × 4 reps (−) | 1 × 4 reps (−) | 2 × 4 reps (+) | 2 × 4 reps (+) | ||
| Diagonal direction | 1 × 4 reps (−) | 1 × 4 reps (−) | 1 × 4 reps (−) | 2 × 4 reps (+) | 2 × 4 reps (+) | ||
Abbreviations: (−), very low load or velocity of displacement; (+), low load or velocity of displacement; ESM, electrostimulation.
Table 3.
Postoperative Rehabilitation Week 2: Progression of Strength Exercises
| Exercises |
Sets or Reps by Day |
||||||
| 8 |
9 |
10 |
11 |
12 |
13 |
14 |
|
| Level of body functions and structures | |||||||
| Horizontal closed kinetic chain with manual grips + ESM | 3 × 3.5-min ESM | 3 × 3.5-min ESM | 4 × 3.5-min ESM | ||||
| Vertical closed kinetic chain with a FitBALL on back + ESM | 2 × 3.5-min ESM | 2 × 3.5-min ESM | 3 × 3.5-min ESM | 3 × 3.5-min ESM | |||
| Gluteal strength training | 3 × 8 reps (+) | 3 × 8 reps (+) | 3 × 8 reps (+) | ||||
| Adductor strength training | 3 × 8 reps (+) | 3 × 8 reps (+) | 3 × 8 reps (+) | ||||
| Hamstrings strength training | 3 × 8 reps (+) | 3 × 8 reps (+) | 3 × 8 reps (+) | ||||
| Level of activities and participation: displacement progression | |||||||
| Anterior-posterior direction | 2 × 4 reps (+) | 2 × 4 reps (+) | 3 × 4 reps (++) | 3 × 4 reps (++) | |||
| Lateral direction | 2 × 4 reps (+) | 2 × 4 reps (+) | 3 × 4 reps (++) | 3 × 4 reps (++) | |||
| Diagonal direction | 2 × 4 reps (+) | 2 × 4 reps (+) | 3 × 4 reps (++) | 3 × 4 reps (++) | |||
| Volitionally controlled center-of-mass movements in water in backward direction | 6 × 4 reps (+) | 6 × 4 reps (+) | 9 × 4 reps (+) | ||||
Abbreviations: (+), low load or velocity of displacement; (++), medium load or velocity of displacement; ESM, electrostimulation.
Ball Dynamics.
Table 4.
Postoperative Rehabilitation During Week 3: Progression of Strength Exercises
| Exercises |
Sets or Reps by Day |
||||||
| 15 |
16 |
17 |
18 |
19 |
20 |
21 |
|
| Level of body functions and structures | |||||||
| Vertical closed kinetic chain with a fit-ball on back + ESM | 4 × 3.5-min ESM | 2 × 3.5-min ESM | 4 × 3.5-min ESM | 2 × 3.5-min ESM | 4 × 3.5-min ESM | 2 × 3.5-min ESM | 4 × 3.5-min ESM |
| Gluteal strength training | 3 × 8 reps (++) | 3 × 10 reps (++) | 3 × 10 reps (++) | 3 × 10 reps (++) | |||
| Adductor strength training | 3 × 8 reps (++) | 3 × 10 reps (++) | 3 × 10 reps (++) | 3 × 10 reps (++) | |||
| Hamstrings strength training | 3 × 8 reps (++) | 3 × 10 reps (++) | 3 × 10 reps (++) | ||||
| Calf strength training | 2 × 8 reps (−) | 2 × 8 reps (−) | 2 × 8 reps (−) | ||||
| Level of activities and participation: displacement progression | |||||||
| Anterior-posterior direction | 4 × 4 reps (++) | 4 × 4 reps (++) | 4 × 4 reps (++) | ||||
| Lateral direction | 4 × 4 reps (++) | 4 × 4 reps (++) | 4 × 4 reps (++) | ||||
| Diagonal direction | 4 × 4 reps (++) | 4 × 4 reps (++) | 4 × 4 reps (++) | ||||
| Volitionally controlled center-of-mass movements in water in backward direction | 9 × 4 reps (++) | 12 × 4 reps (++) | 12 × 4 reps (++) | 12 × 4 reps (++) | |||
Abbreviations: (−), very low load or velocity of displacement; (++), medium load or velocity of displacement; ESM, electrostimulation.
To achieve the proposed objectives in the level of activities and participation (Table 1), we pursued immediate weight bearing5 to allow an early start on volitionally controlled center-of-mass movements with a progression of exercises in the anterior-posterior (Supplemental Videos 8, 9, 10, 11, and 12), lateral (Supplemental Videos 13 and 14), and diagonal (Supplemental Videos 15 and 16) directions, which favored loading the affected leg in the correct gait pattern with no pain, effusion, or increase in temperature during walking or shortly after walking3 and with a gradual increase in velocity displacement from very low to medium, with 3 to 5 minutes of rest between sets (Tables 2, 3, and 4). Once the wound had closed, we prescribed water exercises 3 to 4 times a week with mobility exercises that included perturbations, training 1 leg for longer periods, increasing difficulty, and beginning backward movements (Supplemental Videos 17, 18, and 19)3 with a progressive increase in velocity displacement from low to medium and 3 to 5 minutes of rest between sets (Tables 3 and 4).
Discussion
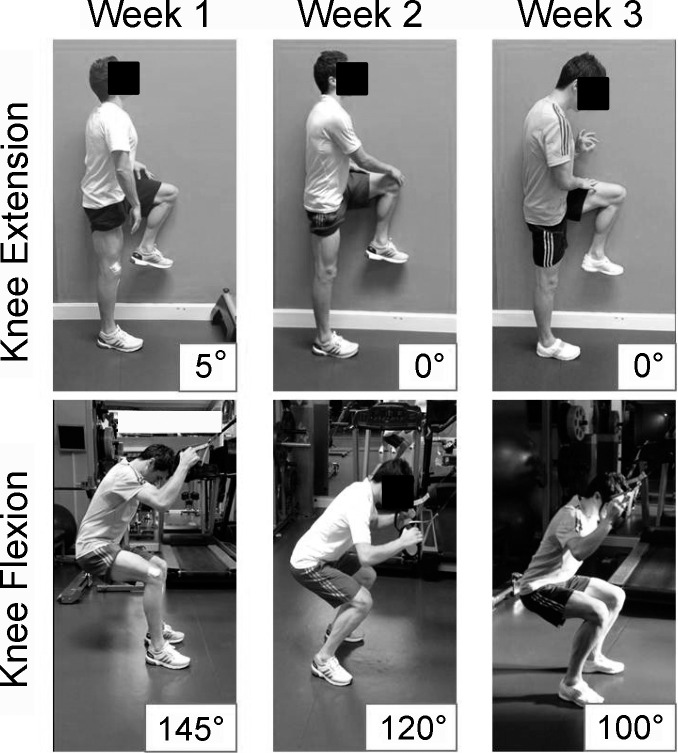
No clear guidelines exist regarding the recommended quantity and quality of movement during postoperative ACL reconstruction rehabilitation.3 Based on the criteria proposed by the KNGF (Table 1), our recommendations for starting phase 2 are as follows: (1) knee extension at 0° measured in CKC manner (Supplemental Video 20), (2) knee flexion of at least 120° to 130° measured in CKC fashion (Supplemental Video 21), and (3) correct qualitative performance of walking (Supplemental Video 22). At the end of the first week of postoperative rehabilitation, the athlete achieved 5° of knee extension and 145° of knee flexion (Figure 1). During the second week, he accomplished the objectives of this phase with 0° of knee extension and 120° of knee flexion, having previously attained 0° of knee extension and 100° of knee flexion.
Figure 1.
Improvement of knee extension-flexion angle week by week.
CLINICAL BOTTOM LINE
The KNGF evidence statement is an efficient guide for the first phase of ACL reconstruction rehabilitation in a professional soccer player. The proposed objectives during this first phase of the rehabilitation are appropriate for the circumstances and correspond to the biological and personal needs of the professional soccer athlete. Nevertheless, it makes more sense to progress based on the achievement of functional goal-based criteria in the rehabilitation protocol than to use time-based protocols.
Supplementary Material
SUPPLEMENTAL MATERIAL
Supplemental Videos. Video Demonstrations. Found at DOI: http:dx.doi.org/10.4085/1062-6050-164-21.S1
REFERENCES
- 1.Rekik RN, Tabben M, Eirale C, et al. ACL injury incidence, severity and patterns in professional male soccer players in a Middle Eastern league. BMJ Open Sport Exerc Med . 2018;4(1):e000461. doi: 10.1136/bmjsem-2018-000461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walden M, Hagglund M, Magnusson H, Ekstrand J. ACL injuries in men's professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med . 2016;50(12):744–750. doi: 10.1136/bjsports-2015-095952. [DOI] [PubMed] [Google Scholar]
- 3.van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med . 2016;50(24):1506–1515. doi: 10.1136/bjsports-2015-095898. [DOI] [PubMed] [Google Scholar]
- 4.Taradaj J, Halski T, Kucharzewski M, et al. The effect of neuromuscular electrical stimulation on quadriceps strength and knee function in professional soccer players: return to sport after ACL reconstruction. Biomed Res Int . 2013;2013:802534. doi: 10.1155/2013/802534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tyler TF, McHugh MP, Gleim GW, Nicholas SJ. The effect of immediate weightbearing after anterior cruciate ligament reconstruction. Clin Orthop Relat Res . 1998;(357):141–148. doi: 10.1097/00003086-199812000-00019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.