Abstract
Objective:
The study examined (1) whether daily diabetes problems that adolescents experience were associated with parental persuasive strategies (e.g., persuading the adolescent to do more to manage diabetes), (2) whether this association was mediated through greater parental worry and lower confidence in adolescents’ abilities, and (3) how parental persuasive strategies may provide corrections for subsequent blood glucose control but reduce adolescent confidence for adolescents high in self-efficacy.
Method:
Adolescents with Type 1 diabetes (N = 180, ages 10.50–15.58 years) and their mothers (N = 176) and fathers (N = 139) completed diaries for 14 days reporting on problems experienced with diabetes, maternal and paternal use of persuasive strategies, and confidence in adolescents’ ability to manage diabetes. Parents reported their daily worry about diabetes, adolescents reported their general self-efficacy for diabetes management, and blood glucose was downloaded from glucometers.
Results:
Across reporters, multilevel modeling revealed that parents used more persuasive strategies on days when more diabetes problems were experienced. This association was mediated through parents’ greater worry and lower confidence in adolescents’ ability to manage diabetes. Lagged analyses revealed that adolescents’ perceptions of maternal persuasive strategies were associated with improvements in next-day blood glucose, but also with reductions in adolescents’ daily confidence for those high in self-efficacy.
Conclusions:
Parental persuasive strategies appear responsive to daily problems that adolescents experience in diabetes management. Mothers’ persuasive strategies may have the dual effects of correcting blood glucose levels but reducing the more self-efficacious adolescents’ confidence in their own ability to manage diabetes.
Keywords: control, diabetes, adolescent, parent, problems
Adolescent diabetes management is better when parents are involved through assisting with daily diabetes tasks (Anderson et al., 2009; Laffel et al., 2003; Wysocki et al., 2009) and monitoring their adolescents’ diabetes activities (Berg et al., 2008; Ellis et al., 2007). The challenge during adolescence, however, is how parents can remain involved in adolescents’ diabetes management without being perceived as controlling (Wiebe et al., 2005). Parenting styles characterized by psychological control (control of an adolescent’s thoughts and feelings; Barber, 1996) are associated with poorer illness management (Anderson & Coyne, 1991; Butler, Skinner, Gelfand, Berg, & Wiebe, 2007; Wiebe et al., 2005). Even parents’ well-intentioned efforts to regulate diabetes management such as miscarried helping (Anderson & Coyne, 1991) or overprotection (Holmbeck et al., 2002) can be experienced as controlling and intrusive. Little is known, however, about the process by which parents engage in efforts to regulate or influence their adolescent’s diabetes management behaviors on a daily basis, or about the effectiveness of such efforts in facilitating diabetes management.
In the present study, we explored parents’ daily efforts to persuade their adolescent to better manage his or her diabetes. Such “persuasive strategies” (Stephens et al., 2009) included reminding the adolescent to manage diabetes, trying to get the adolescent to improve diabetes management, and persuading the adolescent to do more to manage diabetes. These strategies may reflect ways in which parents monitor their child’s activities (Ellis et al., 2007) and assist with daily diabetes activities (Anderson et al., 2009), and may be helpful in promoting better diabetes control. At the same time, however, such efforts may be construed as intrusive by the developing adolescent, which could undermine adolescents’ feelings of competence (Pomerantz & Eaton, 2001; Wiebe et al., 2005). The daily diary approach, used in the present study, will illuminate how broad measures of parental involvement may translate into daily persuasive strategies and track the daily processes whereby parents’ persuasive strategies relate to the problems that adolescents have in diabetes management and to subsequent blood glucose control and adolescent confidence in management.
Parents may utilize persuasive strategies in the context of daily problems with diabetes management, problems that indicate that adolescents need assistance and may not be adhering to their regimen (Fortenberry, Wiebe, & Berg, 2012). Adolescents and parents frequently report problems related to highs and lows in blood glucose levels, forgetting to test blood glucose, and forgetting supplies while away from home (Beveridge, Berg, Wiebe, & Palmer, 2006; Fortenberry et al., 2012). Parents may naturally respond to these problems by engaging in persuasive strategies oriented toward getting adolescents to do more to manage their diabetes. Support for the idea that persuasive strategies are associated with problems that children experience comes from Pomerantz and Eaton (2001), who found that poor academic achievement appeared to elicit greater parental intrusive support.
Difficulties in diabetes management such as problems with blood glucose testing or high blood glucose values may be associated with persuasive strategies because they increase parents’ worry about adolescents’ diabetes and compromise parents’ confidence in adolescents’ abilities to manage diabetes independently. Pomerantz and Eaton (2001) found that the link between children’s lower academic achievement and greater maternal intrusive support occurred through greater maternal worry about the child’s academic achievement and greater child uncertainty. In the context of Type 1 diabetes, there is some support for the links in the proposed mediational model, although this process has not yet been examined on a daily basis. For instance, higher daily blood glucose was associated with adolescents’ lower perceptions of competence for dealing with daily diabetes problems (Fortenberry et al., 2009). In addition, higher maternal anxiety was associated with appraisals of parental overprotection among adolescents with diabetes (Cameron, Young, & Wiebe, 2007), and higher maternal depressive symptoms were associated with sustained maternal behavioral involvement across adolescence (Wiebe et al., 2011). Finally, higher maternal psychological control was associated with lower self-efficacy for diabetes tasks in adolescents (Butler et al., 2007).
Parents may engage in persuasive strategies as a way to correct problems in diabetes management, but such strategies may come at a cost to adolescents’ confidence that they can resolve problems independently (Pomerantz, Moorman, & Litwack, 2007). Such “dual-effects” have been noted among adults (Lewis & Rook, 1999), but there is little evidence for these effects in the context of pediatric chronic illness. Using a measure of parental involvement in diabetes management (which likely contains an element of parents’ attempts to regulate adolescent behavior), Helgeson, Reynolds, Siminerio, Escobar, and Becker (2007) found that adolescents whose parents were more involved displayed slower subsequent deterioration in metabolic control over time in comparison with adolescents who were more independent in diabetes management. However, more intrusive forms of involvement may undermine adolescents’ confidence in their own ability to manage illness (Holmbeck et al., 2002), especially for those adolescents who already feel competent in their abilities (Pomerantz et al., 2007). Adolescents who view themselves as highly competent may experience relatively few parental persuasive strategies, but question their own abilities when parents do intervene. In contrast, adolescents who view themselves as less competent may need and welcome such parental involvement, experience it as supportive, and develop greater self-confidence through this support (Pomerantz et al., 2007).
Research on parental involvement in diabetes management has focused on mothers’ involvement, with more recent work noting the importance of fathers’ involvement. Despite lower levels of paternal involvement in diabetes care and coping efforts around diabetes stress (Berg et al., 2009; Laffel et al., 2003), fathers are still influential in diabetes management (Berg et al., 2008; Wysocki & Gavin, 2005). For example, fathers’ monitoring efforts, although lower than mothers’ efforts, were uniquely related to adolescent metabolic control (Berg et al., 2008). With the extensive demands of daily management of Type 1 diabetes during adolescence, it is probable that both mothers’ and fathers’ use of persuasive strategies affect diabetes care.
The primary aim of the study was to understand parents’ use of persuasive strategies in the context of adolescents’ daily diabetes problems. Adolescents and their mothers and fathers recorded daily diabetes problems, parental persuasive strategies, and their confidence in adolescents’ diabetes management for 14 consecutive days. Mothers and fathers rated their daily worry about adolescents’ diabetes. First, we examined associations between persuasive strategies and more commonly used metrics of parental involvement (behavioral involvement, monitoring, intrusive support) in Type 1 diabetes, to position our daily measure within the larger parental involvement literature. Second, we examined whether parents’ daily persuasive strategies were predicted from two aspects of daily diabetes management (problems that adolescents have with management and blood glucose levels). We hypothesized that across reporters, more daily problems in diabetes management and higher blood glucose would be associated with more frequent use of parental persuasive strategies. Third, we examined a mediational model in which daily diabetes problems related to parental persuasive strategies through increasing parental worry over adolescents’ diabetes and decreasing parental confidence in adolescents’ ability to manage problems. Finally, we examined the dual effects of persuasive strategies, predicting that such strategies would provide corrections to subsequent blood glucose but at the cost of lowering adolescents’ subsequent self-confidence for adolescents with high self-efficacy while bolstering self-confidence for adolescents with low self-efficacy.
Method
Participants
The study included 180 adolescents, 176 mothers, and 139 fathers who provided usable data to all portions of a daily diary protocol during the second wave of a longitudinal study examining parent–adolescent relationships and diabetes. In the larger study, 252 adolescents with Type 1 diabetes were recruited from a university outpatient diabetes clinic, and a second clinic conducted by a pediatric endocrinologist who followed the same treatment guidelines. Initial eligibility criteria included the following: that children be 10 through 14 years of age, diagnosed with Type 1 diabetes for at least 1 year, living with their mother, and able to read and write either English or Spanish. Reasons for not participating in the second assessment included being too busy or traveling too far. A total of 207 adolescents, 203 mothers, and 162 fathers provided diary data at Time 2. Twenty-seven adolescents did not provide usable daily blood glucose readings and thus were dropped from further analyses. Reasons for missing data included blood glucose meter not returned (n = 6), experimenter failure to issue a meter (n = 6), software malfunction (n = 5), declined the use of our meter or failed to provide readings from their own meter (n = 8), and unknown (n = 2). These 27 participants did not differ from the remaining 180 on measures of parental involvement (ps > .10). Diary participants included 98 adolescent girls and 82 boys, who were 10.50 to 15.58 years of age (M = 12.87, SD = 1.53) and had been diagnosed with Type 1 diabetes for an average of 4.45 years (SD = 2.89). Fifty-seven percent of these adolescents were on an insulin pump, and adolescents tested blood glucose an average of 5.53 (SD = 1.73) times per day. Mothers (mean age = 40.92 years) and fathers (mean age = 43.19 years) also participated in the diary portion of the study. Eighty-four percent of participating mothers and 95% of participating fathers reported being married. Most adolescents lived full time with their mothers (95%) or fathers (94%). Adolescents were primarily Caucasian (94.9%), with the majority of the households (65%) earning over $50,000 a year.
Procedures
This study was approved by the appropriate Institutional Review Board. Adolescents gave written assent, and mothers and fathers gave written informed consent and parental permission.
Participants were scheduled for a 2-hr session during which they individually completed a questionnaire packet (adolescents and mothers completed the packet in session; fathers were mailed the packet) and were trained for completion of a 14-day daily diary (fathers received training by phone). Participants completed their diaries online via a secure Website at the end of each day, and trained research assistants checked that online entries were completed and made reminder phone calls if the entry was not posted by 9 pm. Participants were paid $4 for each completed diary and $50 each for completing the questionnaire packet and training session.
Daily Diary Measure
Adolescents, mothers, and fathers completed the Web-based diary daily for 14 consecutive days. Diary items were chosen carefully because diaries require selection of a small number of items to assess constructs (Cranford et al., 2006). The 2-week time period was chosen as optimal to maximize the measurement of daily diabetes management without unduly burdening participants (Bolger, Davis, & Rafaeli, 2003). Eighty-two adolescents, 82 mothers, and 47 fathers completed all 14 diaries on consecutive days for the variables included in the present analyses, and an additional 84 adolescents, 85 mothers, and 73 fathers completed entries on 11–13 days. Participants were excluded from analyses if they had fewer than 3 days of data (Bryk & Raudenbush, 1992). Analyses were based on an average of 12.81 adolescent, 12.95 mother, and 12.27 father diary days completed.
To assess parental persuasive strategies, mothers and fathers rated on a 1 (not at all) to 5 (a lot) scale the following variables: how much did you (1) remind your child of the things he or she needs to do to manage his or her diabetes, (2) try to get your child to improve his or her diabetes, and (3) persuade your child to do more to manage his or her diabetes. These items were drawn from Stephens et al.’s (2009) measure of persuasive strategies with daily measurement (M. A. P. Stephens, personal communication, 2005). Adolescents reported separately on their perceptions of mothers’ and fathers’ daily persuasive strategies. Interitem consistency reliability of the three-item measure of persuasive strategies across days and persons by each reporter was calculated via hierarchical linear modeling (HLM) random intercept models with both time and item treated as nested levels; reliability was excellent across reporter (reliability = .95 for adolescents’ reports of mothers, .94 for adolescents’ reports of fathers, .92 for mothers’, and .87 for fathers’ self-reports). Confidence in the adolescent’s ability to manage diabetes was assessed by having mothers and fathers rate on a 1 (not at all) to 5 (a lot) scale “How confident were you in your child’s ability to manage his or her diabetes in the last 24 hours?” Mothers’ and fathers’ worry was assessed by rating on a 1 (not at all) to 5 (a lot) scale “How much did you worry about your child’s diabetes in the last 24 hours?” These latter two measures were drawn from Pomerantz and Eaton’s (2001) work on daily assessment of these constructs.
In the diary, adolescents indicated whether they experienced any of 10 problematic aspects of daily diabetes management on that day, drawn from the most commonly generated problems mentioned by adolescents and mothers in our prior studies (Beveridge et al., 2006). The problems included (1) forgetting or skipping a blood-sugar test, (2) taking the wrong amount of insulin, (3) problems with exercising or playing sports, (4) problems eating what you want to, (5) feeling bad (upset, angry, sad) because of diabetes, (6) managing diabetes away from home or family, (7) high blood sugar, (8) low blood sugar, (9) figuring out how much insulin to take based on exercise, meals/snacks, and blood sugar, and (10) problems with pump (for those on pump only). Responses were summed to compute the number of diabetes problems. Adolescents reported an average of 1.35 problems per day (SD = 1.03, range 0–5.6). The most frequently reported problems included problems with high blood sugar (.40 times per day on average), forgetting or skipping a blood sugar test (.29 times per day), problems with low blood sugar (.22 times per day), and problems in taking the wrong amount of insulin (.13 times per day).
Daily Blood Glucose
Across the 14 days of the daily diary, adolescents monitored daily blood glucose using a glucose meter provided by researchers, resulting in date- and time-stamped records. Glucose meters were returned at the end of the diary period. Blood glucose data were screened for outliers and errors in measurement. Blood glucose measures that occurred within 15 min of one another were deleted, with the later of the proximate readings retained. This procedure arose from consultations with pediatric endocrinologists, who indicated that repeated glucose tests likely reflected adolescents’ efforts to confirm the initial reading, because measurement can become increasingly inaccurate at abnormally high or low glucose levels (Saudek, Derr, & Kalyani, 2006). Daily blood glucose was calculated by averaging across the adolescent’s glucose meter readings each day. Adolescents completed an average of 4.34 blood glucose readings each day (SD = 1.88), with an average daily blood glucose level of 206.25 (SD = 57.06), which is above the 180 mg/dL level considered hyperglycemic (American Diabetes Association, 2007). Very few of the daily blood glucose values represented low values (i.e., only 1.9% of the daily average blood glucose values were below 80). Thus, when interpreting daily blood glucose averages, higher readings are interpreted as indicating poorer management.
Because parental persuasive strategies may be responsive to both lows and highs in blood glucose rather than to average fluctuations across days, we also calculated an average daily risk range (ADDR) score that indicated experiences of high and low blood glucose levels each day. Following the procedure described by McCall, Cox, Crean, Gloster, & Kovatchev (2006) and Kovatchev, Otto, Cox, Gonder-Frederick, and Clarke (2006), we separated blood glucose readings into scores above and below 112.5 mg/dL (the medical standard recommended). Each was normalized into a scale of risk from 0 (indicating no risk) to 100 (indicating highest possible risk), on the basis of the deviance of each reading from the recommended level. High and low risk values were then averaged within days. This process creates a metric of risk at which lower risk represents being close to the medical standard and higher risk represents increases or decreases away from that standard.
Questionnaire Measures
Parental monitoring.
Adolescents, mothers, and fathers completed a scale of parental monitoring for diabetes management developed by the authors (see Berg et al., 2008). This scale consisted of 6 items to capture how much mothers and fathers “really” know about different aspects of the child’s diabetes management (e.g., blood sugar readings; how much insulin they’ve taken) using a 1 (doesn’t know) to 5 (knows everything) scale. The average across the 6 items was computed. The scale showed excellent reliability in the current sample (α ≥ .88 for all reporters).
Diabetes responsibility scale.
A revised version of the Diabetes Responsibility and Conflict Scale (Rubin, Young-Hyman, & Peyrot, 1989) was included to assess parents’ and adolescents’ perceptions of who is responsible for completing 23 aspects of diabetes management (e.g., who determines the insulin dose). Original items were updated and several items were added by a certified diabetes educator and an adolescent on an insulin pump to reflect current regimens and technologies. Items referring to urine testing were replaced with blood glucose testing, and items about insulin were modified to be relevant to both multiple daily injections and insulin pump regimens. For each item, adolescents rated the parent’s level of responsibility for completing the tasks (e.g., 1 = I do it alone, 3 = I share equally with my parents, 5 = My parent does it alone). An average score across items was computed. Both the original (Rubin et al., 1989) and modified scales display high reliability (α ≥ .92 for all reporters in this study).
Intrusive support.
Pomerantz and Eaton’s (2001) intrusive support scale was modified to capture how often parents helped with diabetes care over the past week without the adolescent asking for assistance (e.g., How often did your mom check over your glucometer readings without you asking her to do so?). Adolescents reported separately on mothers and fathers, and parents reported their own behavior. Four items were rated on a 1 = never to 4 = all of the time scale, with an average score computed (α > .82 for all reporters).
Diabetes self-efficacy.
Adolescents completed the Self-Efficacy for Diabetes Self-Management scale (SEDM; Iannotti et al., 2006), reporting their confidence in managing 10 diabetes situations from 1 = not at all sure to 10 = completely sure (αs for all reporters >.88).
Data Analysis
Analyses were conducted with HLM6 (Raudenbush, Bryk, & Condon, 2004) using two different analytic approaches. For most reported results, adolescent reports of mothers and fathers, and mothers’ and fathers’ reports of themselves, were modeled in separate analyses because mediation testing procedures with random effects have not been extended to the triadic case. Analyses predicting daily mothers’ reports of persuasive strategies from adolescents’ reports (b = .20, SE = .03, p < .01) and fathers’ reports from adolescents’ reports (b = .12, SE = .03, p < .01) indicated significant associations among reporters. Thus, when comparing effects across parents, we modeled both parents simultaneously in stacked models to generate a proper comparison while accounting for the family dependency.
We first present models depicting the associations among parental persuasive strategies and other metrics of parental involvement. These analyses provided information about between-subjects variables that distinguished between those who reported more versus less persuasive strategies across the 14 days; such information was important to facilitate the interpretation of the persuasive strategies construct. Second, within-subject Level 1 associations of mothers’, fathers’, and adolescents’ reports of persuasive strategies were predicted from day, number of problems, and blood glucose. Third, mediation models examined whether the daily associations between diabetes management problems (number of problems and blood glucose) and parental persuasive strategies were mediated through parental worry and confidence in their adolescents’ ability to manage diabetes. Finally, 24-hr lagged effects examined whether parental persuasive strategies predicted subsequent-day blood glucose or adolescent self-confidence.
The mediation models were examined using Bauer, Preacher, and Gil’s (2006) procedure, appropriate for mediation in multilevel models. The procedure adjusts for the covariance between the indirect mediation paths that may exist in time-varying models (e.g., covariance between the coefficients for the number of problems – mother’s worry path and the mother’s worry – mother’s persuasive strategies path) (Bauer et al., 2006; Kenny, Korchmaros, & Bolger, 2003). We examined mediation via parental worry and confidence in two separate mediation models because Bauer et al.’s (2006) technique has not been expanded to the simultaneous multiple mediator case.
Daily predictor variables were person-mean centered, and Level 2 variables were grand centered. In the multilevel models, restricted maximum likelihood estimation was used to account for missing diary days, with the assumption that these days were missing at random. The effect of age was not significant in predicting overall mean levels of persuasive strategies for any reporter, nor did it moderate the relationships between number of problems and persuasive strategies or any lagged effects (ps range from .13 to .62). Thus, age will not be reported further. We examined time since diagnosis and pump status in all models. Longer time since diagnosis was associated with adolescents’ reports of greater mothers’ persuasive strategies, adolescents’ reports of greater fathers’ persuasive strategies, and mothers’ reports of her own greater persuasive strategies (ps < .01). Time since diagnosis did not moderate the association between number of problems and persuasive strategies for any reporter. Because analyses including versus excluding time since diagnosis and pump status were the same, we report the results of models excluding these covariates.
Results
Preliminary Analyses of the Daily Parental Persuasive Strategies Measure
To relate daily parental persuasive strategies to more standard metrics of parental involvement, we examined mothers’, fathers’, and adolescents’ reports of persuasive strategies predicted from adolescents’ and parents’ views of diabetes responsibility, intrusive support, and parental diabetes monitoring. Adolescents who reported mothers’ greater use of persuasive strategies across the 2-week diary also reported higher parental diabetes responsibility (b = .53, SE = .10, t = 5.03, p < .01) and intrusive support (b = .44, SE = .09, t = 4.79, p < .01), but not maternal monitoring. Adolescents who reported greater paternal persuasive strategies also reported greater parental diabetes responsibility (b = .28, SE = .11, t = 2.49, p < .01), intrusive support (b = .44, SE = .09, t = 4.90, p < .01), and paternal monitoring (b = .19, SE = .07, t = 2.66, p < .01). For analyses of mothers’ reports of her own persuasive strategies, higher persuasive strategies were associated with mothers’ reports of higher parental responsibility (b = .57, SE = .09, t = 6.28, p < .01) and intrusive support (b = .31, SE = .07, t = 4.37, p < .01), but not maternal monitoring (p > .30). Similarly, paternal reports of his own persuasive strategies were associated with fathers’ reports of higher parental responsibility (b = .19, SE = .07, t = 2.66, p < .01), intrusive support (b = .39, SE = .11, t = 3.54, p < .01), and paternal monitoring (b = .19, SE = .07, t = 2.66, p < .01).
These analyses reveal that parents who used more daily persuasive strategies also took more responsibility for their adolescents’ diabetes management, were more likely to be perceived as intrusive in their efforts, and for fathers were more aware of their adolescents’ diabetes management. These results provide validity for our measure of daily persuasive strategies, suggesting that it taps daily the various ways that parents are involved in diabetes care, and suggests that a component of this daily involvement may be somewhat intrusive.
Problems With Daily Diabetes Management and Parental Persuasive Strategies
We next examined whether problems with diabetes management were associated with persuasive strategies. Models predicting adolescents’ and parents’ reports of persuasive strategies from blood glucose and number of daily problems are presented in Table 1. Across all models, on days when adolescents or parents reported that adolescents experienced more problems with diabetes, adolescents and parents reported that the parent engaged in more persuasive strategies. Analyses comparing the mother and father intercept revealed that adolescents reported that mothers used more persuasive strategies than did fathers (t = 9.17, p < .01). Similarly, mothers reported that they utilized more persuasive strategies than did fathers (t = 7.54, p < .01).
Table 1.
Same-Day Parental Persuasive Strategies Predicted From Blood Glucose and Diabetes Problems
| Variable | b | SE | t | Variance |
|---|---|---|---|---|
| Adolescent report (AR) of mothers’ persuasive strategies | ||||
| Intercept | 2.29 | .08 | 29.96* | .86* |
| Day | −0.03 | .005 | −5.92* | .003* |
| Blood glucose | 0.0002 | .0002 | 0.85 | .00 |
| AR no. of problems | 0.080 | .02 | 4.62* | .02* |
| Adolescent report of father’s persuasive strategies | ||||
| Intercept | 1.65 | .07 | 23.5* | .69* |
| Day | −0.008 | .005 | −1.71 | .002* |
| Blood glucose | −0.00001 | .0002 | −0.06 | .000 |
| AR no. of problems | 0.06 | .01 | 3.70* | .01* |
| Mother’s report (MR) of mothers’ persuasive strategies | ||||
| Intercept | 2.49 | .07 | 35.25* | .65* |
| Day | −0.02 | .005 | −3.76* | .002* |
| Blood glucose | 0.0001 | .0003 | 0.39 | .000 |
| MR no. of problems | 0.23 | .02 | 12.41* | .02* |
| Father’s report (FR) of father’s persuasive strategies | ||||
| Intercept | 1.91 | .07 | 28.00* | .46* |
| Day | −0.01 | .005 | −2.77* | .001* |
| Blood glucose | −0.0003 | .0003 | −1.29 | .000 |
| FR no. of problems | 0.25 | .02 | 11.85* | .02* |
p < .01.
Daily blood glucose was not associated with same-day parental persuasive strategies. We also examined daily ADDR, because parental persuasive strategies may be responsive to greater risk involving both low and high BG values (Kovatchev et al., 2006), rather than just high values. Similar analyses as described above were used with ADDR as the metric of blood glucose. These analyses did not yield significant associations with parental persuasive strategies via any reporter (range ps > .76 to .98).
Mediating Role of Parental Worry and Confidence in Adolescent
To examine whether the associations between number of problems and parental persuasive strategies were mediated through parental worry and confidence in their adolescents’ ability to manage diabetes, we conducted four mediational analyses (i.e., two each for mothers’ and fathers’ reports of persuasive strategies). Analyses were not conducted for adolescents’ reports of persuasive strategies because adolescents did not report on parental worry. Mediation was tested using 95% confidence intervals (CIs), with zero falling outside this confidence interval, indicating that the population mediation effect was not zero. Confidence interval tests indicated that significant mediation was present for all models. For mothers’ report of persuasive strategies (see Figure 1), maternal worry significantly mediated the association between mother reports of number of problems and persuasive strategies (95% CI = .03, .06). Similarly, maternal confidence in her adolescent’s ability to manage diabetes problems mediated the association between number of problems and persuasive strategies (95% CI = .02, .05). Analyses for fathers’ reports of his own persuasive strategies (see Figure 2) were similar in that both his worry (95% CI = .03, .07) and confidence in his adolescent’s diabetes management (95% CI = .01, .04) mediated the association between number of problems and persuasive strategies.
Figure 1.
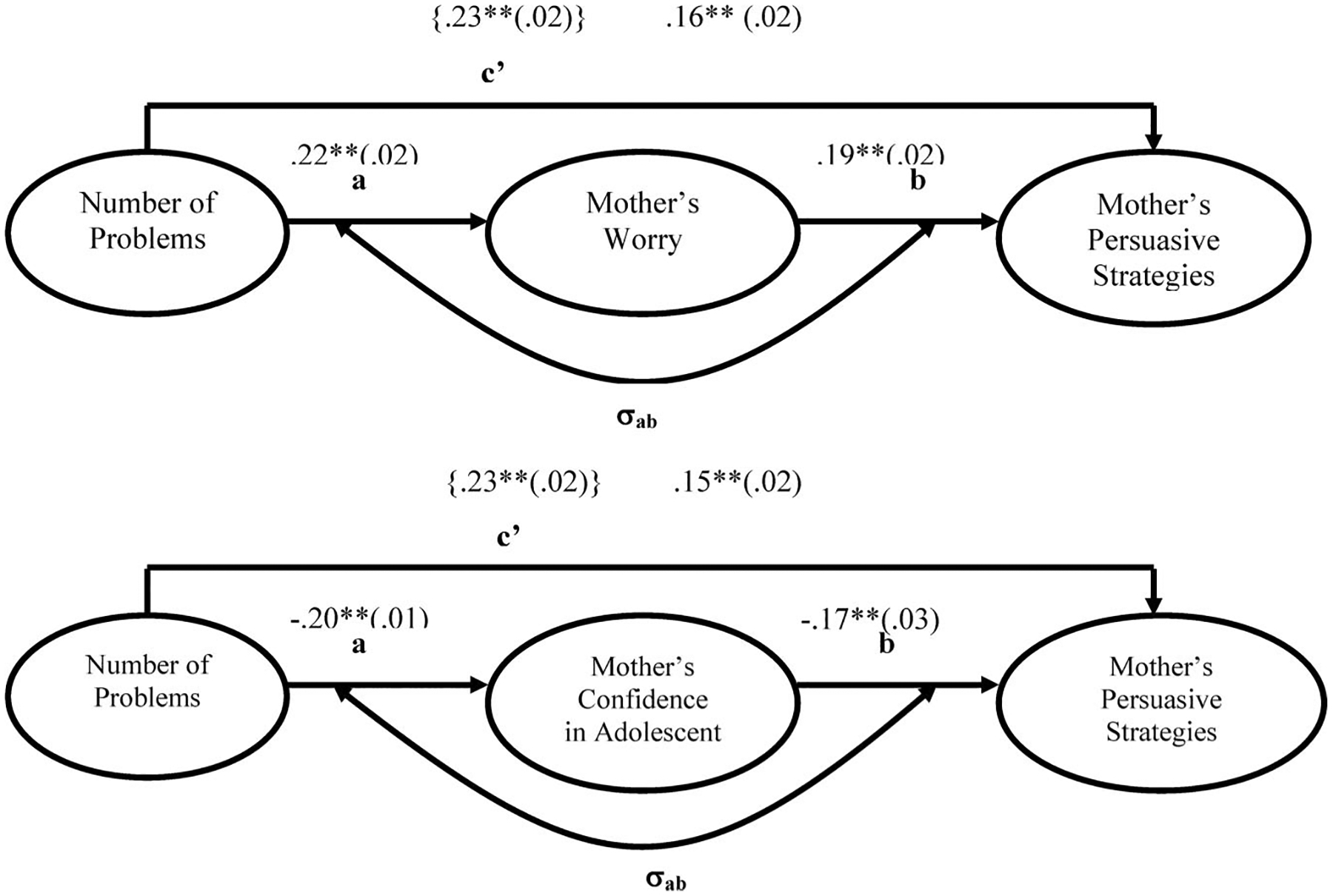
Maternal worry and confidence in adolescent diabetes management mediate the relationship between number of problems and mother’s report of persuasive strategies. Note that bracketed coefficients represent coefficients from the Level 1 equation, which do not include Pathways a and b simultaneously in the model. All other coefficients are from the simultaneous model. Standard errors of the coefficients are in parentheses. ** p < .01.
Figure 2.
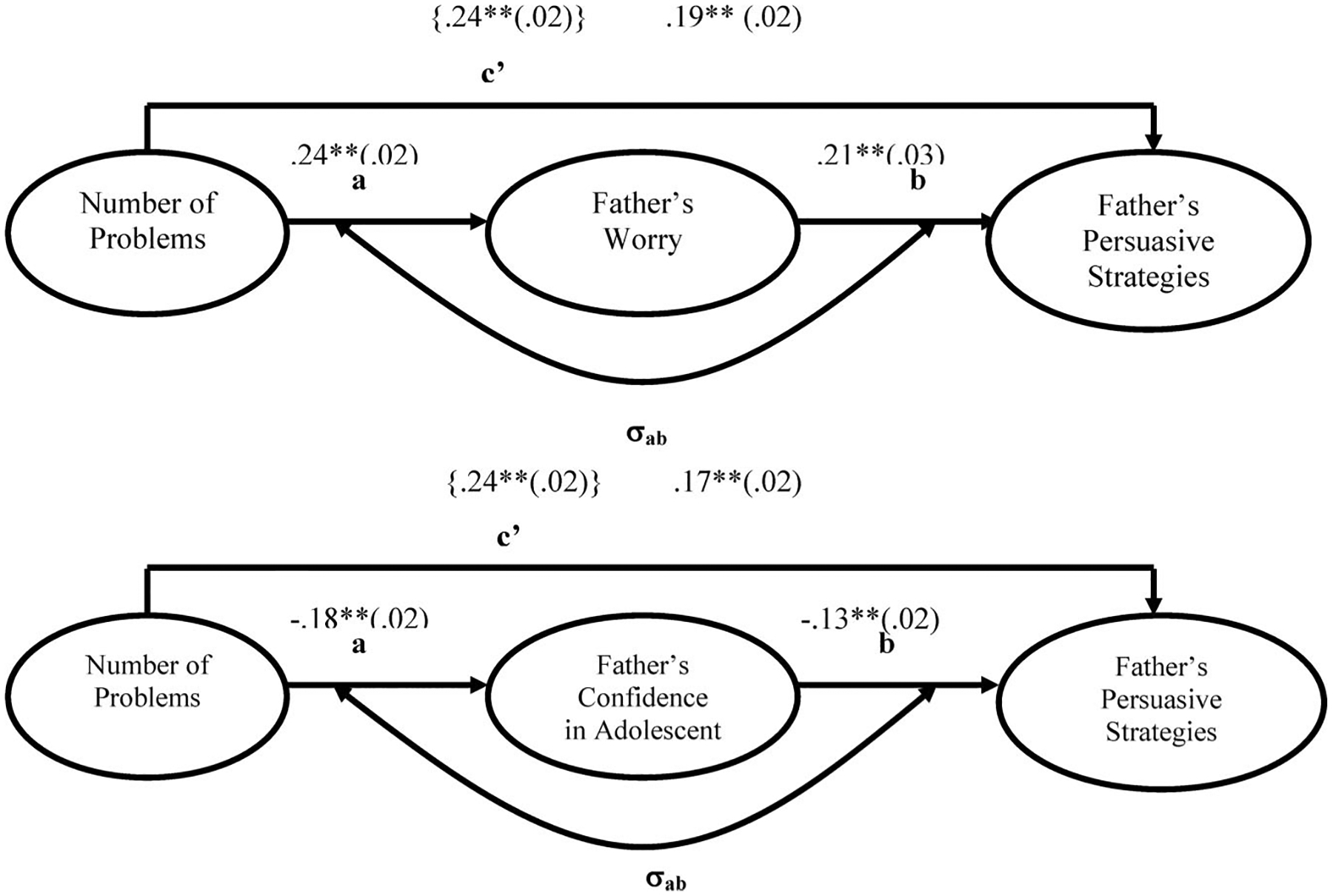
Paternal worry and confidence in adolescent diabetes management mediates the relationship between number of problems and father’s report of persuasive strategies. Note that bracketed coefficients represent coefficients from the Level 1 equation, which does not include Pathways a and b simultaneously in the model. All other coefficients are from the simultaneous model. Standard errors of the coefficients are in parentheses. ** p < .01.
Parental Persuasive Strategies as a Predictor of Subsequent Diabetes Management
To examine whether persuasive strategies predicted next-day changes in blood glucose, multiple HLM analyses were conducted predicting next-day blood glucose from previous-day’s persuasive strategies, while controlling for the previous day’s blood glucose. Only one lagged effect was significant. Adolescents’ reports of mothers’ persuasive strategies predicted a decrease in the next day’s blood glucose (b = −5.00, SE = 2.43, t = −2.05, p < .05). All other lagged effects were not significant (p >.15). Models predicting next-day adolescent report of problems from previous-day adolescent report of persuasive strategies were also conducted. Previous-day adolescent report of mother’s persuasive strategies trended toward predicting reductions in next day’s teen problems, controlling for prior day’s problems (b = −.07, SE = .04, t = −1.93, p = .055). No trends were found for adolescent report of father’s persuasive strategies (p > .30).
A similar model was tested predicting next-day adolescent self-confidence from the previous day’s persuasive strategies, while controlling for previous day’s self-confidence. Although there was no significant fixed, or average, effect, there was significant variability in this effect. Further analyses revealed that this association was moderated by adolescents’ self-efficacy (b = −.04, SE = .02, t = −2.07, p < .05). For adolescents with higher self-efficacy for diabetes (see Figure 3), reports of maternal persuasive strategies on a given day were associated with reductions in their confidence in their ability to manage diabetes the next day. For adolescents with lower self-efficacy, mothers’ persuasive strategies were associated with changes toward greater adolescent confidence the next day. Similar analyses conducted on adolescents’ reports of father’s persuasive strategies on next-day confidence revealed neither fixed nor random effects.
Figure 3.
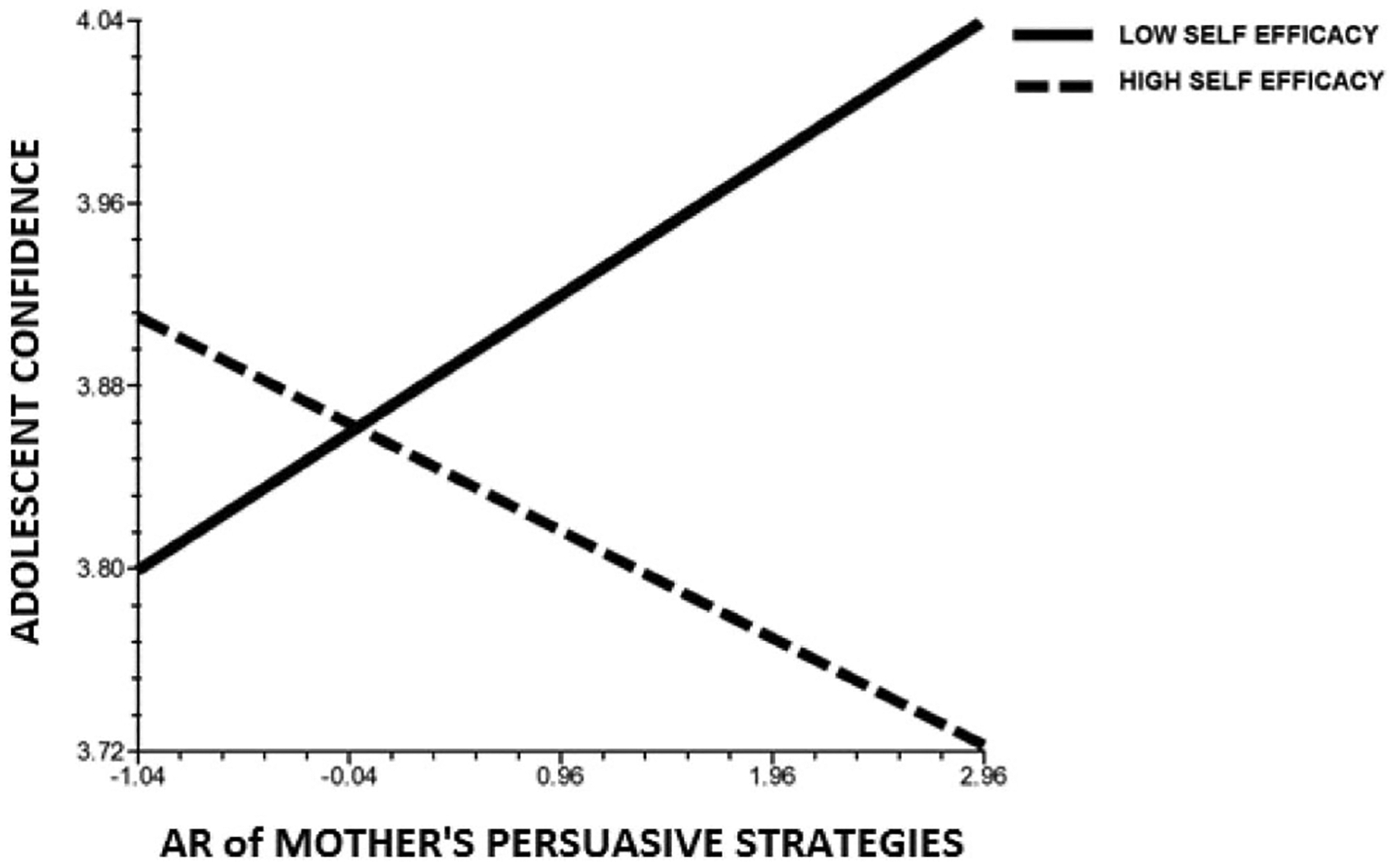
Adolescent self-efficacy as a moderator of the daily association between next-day adolescent confidence and previous-day adolescent report (AR) of mother’s persuasive strategies (controlling for previous day’s adolescent confidence).
Discussion
The results add to the literature on parental involvement in diabetes management by providing a window into the daily context of adolescents’ diabetes management and the role that problems with management, parental worry and confidence, and parental persuasive strategies play in regulating blood glucose and adolescent confidence. Parental persuasive strategies occur as a function of daily diabetes problems, and evidence indicates that use of these strategies arises from parents’ worry and low confidence in adolescents’ abilities. Mothers’ persuasive strategies were important for providing changes toward better blood glucose levels, but undermined self-confidence for those adolescents with high self-efficacy while bolstering self confidence for those low in self-efficacy. Parents may use diabetes problems as an indicator of how much they need to be involved on a daily basis, which may provide corrections for blood glucose and affect adolescents’ confidence differentially as a function of adolescents’ self-efficacy.
The use of parental persuasive strategies is one way that parents are involved on a daily basis in diabetes management. Parental persuasive strategies were most consistently associated with behavioral and intrusive forms of involvement, suggesting that being behaviorally involved may allow parents to be perceived by the adolescent as more intrusively involved. These results provide validity for our measure of persuasive strategies as one way that parents are involved in daily diabetes management.
Our findings suggest that parents use daily diabetes problems as information to guide their efforts to influence adolescents’ diabetes management on a daily basis. In fact, parents’ perceptions of adolescents’ management problems appeared to be stronger guides to their daily involvement than did actual blood glucose levels. That is, there was no same-day association of persuasive strategies with either average blood glucose levels or metrics of blood glucose fluctuations that take into account the importance of both hyperglycemic and hypoglycemic fluctuations (Kovatchev et al., 2006). This could occur if parents are unaware of average blood glucose levels, either because they are not monitoring their adolescents’ diabetes or because adolescents are not disclosing such information. These results suggest that the recognition of problems in diabetes management by adolescents and their parents may be central for understanding processes of daily regulation.
The results also suggest that the process whereby daily diabetes problems are associated with higher parental persuasive strategies occur at least partially through greater parental worry and lower confidence in their adolescent’s ability to manage diabetes. Although previous work has linked maternal trait anxiety and depressive symptoms to aspects of maternal intrusive involvement in diabetes (Cameron et al., 2007; Wiebe et al., 2011), this study is the first to demonstrate the link between parental worry and persuasive strategies on a daily basis. Daily problems were also linked to parental persuasive strategies through lower parental confidence concerning adolescents’ ability to manage their diabetes.
The analyses of persuasive strategies were largely consistent across mothers’ and fathers’ involvement, as well as across reporters, lending considerable strength to our results. Consistent with measures of parental involvement measured on a broad scale of months or weeks (Berg et al., 2008; Holmbeck et al., 2002), all reporters perceived mothers as more involved than fathers on a daily basis. Despite these mean differences, however, both mothers’ and fathers’ persuasive strategies were associated with the number of daily problems, and this association was mediated through parental worry and confidence in adolescents’ ability to manage diabetes. The fact that fathers’ worry was a part of this process is important because very little work has examined fathers’ affective processes in the context of diabetes management (see Butler et al., 2009, for an exception). Thus, mothers’ and fathers’ persuasive strategies may arise out of a similar process whereby diabetes problems provide important information to parents that a more directive form of involvement is needed, and this direction arises from their greater worry and lower confidence in their adolescents’ ability to manage diabetes independently.
The lagged analyses indicated that adolescents’ views of maternal persuasive strategies may have dual effects of facilitating corrections to high blood glucose, but reducing adolescents’ confidence in their ability to manage diabetes problems for adolescents with high self-efficacy. Adolescents high in self-efficacy may place a greater emphasis on independence, with persuasive strategies reflecting a lack of fit between their perceived independence and parental involvement (see Martire, Stephens, & Schulz, 2011, for similar results with couples). For adolescents with low self-efficacy, however, maternal persuasive strategies were beneficial for their subsequent confidence (see also Pomerantz et al., 2007), suggesting that such strategies may be viewed by adolescents as supportive. Adolescents’ perceptions of mothers’ persuasive strategies may have been more predictive than those of fathers’ strategies, because of their higher frequency. These lagged effects occurred for adolescent reports of mothers, but not for mother reports of her own persuasive strategies, suggesting that it is adolescents’ perceptions that may be most informative for understanding their own self-regulatory behavior. Persuasive strategies, as with other forms of parental involvement, may be a construct that is best measured in the “eye of the beholder,” especially during adolescence when such perceptions are affected by adolescents’ developing autonomy and self-efficacy (Pomerantz et al., 2007; Soenens & Vansteenkiste, 2010). The results were consistent with Stephens et al.’s (2009) findings that persuasive strategies were beneficial for health outcomes, and with recent work by Franks and Iida (2010) that daily spousal persuasive strategies were associated with subsequent higher distress. These lagged effects, however, should be interpreted with caution because many of the associations were not significant. It is possible that the associations between persuasive strategies and subsequent blood glucose and adolescent confidence happen on a smaller time scale than a 1-day lag.
The results should be considered in the context of some limitations. First, although our results are consistent with the hypothesized mediational process whereby parental persuasive strategies arise from problems with diabetes management that lead to parental worry and less confidence in the adolescent’s ability to manage diabetes, the fact that these are same-day associations limits our ability to address directionality of associations. Future research using experience-sampling methodologies in which parental persuasive strategies, problems, blood glucose, worry, and adolescent confidence can be measured more frequently within a single day may facilitate conclusions regarding temporal process. Second, we were not able to test mediation simultaneously for both parental worry and confidence in adolescent’s abilities. These two mediators are related, and a simultaneous test would allow us to understand their unique effects. Third, our results are limited to the measure of parental persuasive strategies used in the present study. Although analyses suggested that this measure reflects how parents are behaviorally and potentially intrusively involved in diabetes care on a daily basis, additional work is needed to discern how persuasive strategies relate to more aversive aspects of parental control such as psychological control (Soenens & Vansteenkiste, 2010) and overprotection (Anderson & Coyne, 1991; Holmbeck et al., 2002). In addition, research is needed on how positive forms of daily parental involvement such as collaboration and support may correct blood glucose without affecting adolescents’ self-confidence (Wiebe et al., 2005; Wysocki et al., 2009). Finally, our results are restricted in generalizability as our sample of families included predominantly intact, White, English-speaking, middle-class participants.
In summary, the study adds significantly to the literature by showing how parents’ use of persuasive strategies appears responsive to daily diabetes management problems, and how maternal persuasive strategies especially may provide corrections for blood glucose but at the cost of future adolescent confidence for those who already feel competent to manage diabetes problems. The results point toward possibilities for family intervention that involve dealing with diabetes management problems in an autonomy-supportive manner while maintaining oversight so that problems with management are resolved. Slight modifications in mothers’ efforts to regulate their adolescents may be important because mothers’ use of persuasive strategies was important for changes toward better next-day blood glucose. Such interventions may require a normalization of daily diabetes problems (e.g., “problems will happen”) such that problems do not spark excessive parental worry or undermine parents’ confidence in their adolescent’s general abilities to manage diabetes, especially for adolescents who are confident in their own independent abilities. In addition, parental persuasive strategies may be most effectively utilized when their use is matched to the competence level of the adolescent so that competent adolescents can maintain their confidence in their independent diabetes management. Viewing problems as teachable moments by parents may provide the scaffolding needed to foster independent problem-solving abilities (Wysocki et al., 2008).
Acknowledgments
Research was supported by grant R01 DK063044 from the National Institute of Diabetes and Digestive and Kidney Diseases.
References
- American Diabetes Association. (2007). Standards of medical care in diabetes—2007. Diabetes Care, 30, S4–S41. doi: 10.2337/dc07-S004 [DOI] [PubMed] [Google Scholar]
- Anderson BJ, & Coyne JC (1991). “Miscarried helping” in the families of children and adolescents with chronic diseases. In Johnson JH & Johnson SB (Eds.), Advances in child health psychology (pp. 167–177). Gainesville, FL: University of Florida. [Google Scholar]
- Anderson BJ, Holmbeck G, Iannotti RJ, McKay SV, Lochrie A, Volkening LK, & Laffel LK (2009). Dyadic measures of the parent–child relationship during the transition to adolescence and glycemic control in children with type 1 diabetes. Families, Systems, & Health, 27, 141–152. doi: 10.1037/a0015759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber BK (1996). Parental psychological control: Revisiting a neglected construct. Child Development, 67, 3296–3319. doi: 10.2307/1131780 [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, & Gil KM (2006). Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychological Methods, 11, 142–163. doi: 10.1037/1082-989X.11.2.142 [DOI] [PubMed] [Google Scholar]
- Berg CA, Butler JM, Osborn P, King G, Palmer DL, Butner J, … Wiebe DJ (2008). Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care, 31, 678–683. doi: 10.2337/dc07-1678 [DOI] [PubMed] [Google Scholar]
- Berg CA, Skinner M, Ko K, Butler J, Palmer D, Butner J, & Wiebe DJ (2009). The fit between stress appraisal and dyadic coping in predicting perceived coping effectiveness for adolescents with Type 1 diabetes. Journal of Family Psychology, 23, 521–530. doi: 10.1037/a0015556 [DOI] [PubMed] [Google Scholar]
- Beveridge RM, Berg C, Wiebe D, & Palmer DL (2006). Mother and adolescent representations of illness ownership and stressful events surrounding diabetes. Journal of Pediatric Psychology, 31, 818–827. doi: 10.1093/jpepsy/jsj094 [DOI] [PubMed] [Google Scholar]
- Bolger N, Davis A, & Rafaeli E (2003). Diary methods: Capturing life as it is lived. Annual Review of Psychology, 54, 579–616. doi: 10.1146/annurev.psych.54.101601.145030 [DOI] [PubMed] [Google Scholar]
- Bryk A, & Raudenbush S (1992). Advanced quantitative techniques used in the social sciences: Vol. 1. Hierarchical linear models. London, UK: Sage. [Google Scholar]
- Butler JM, Berg CA, Gelfand D, Fortenberry KT, Foster C, & Wiebe DJ (2009). Parental and adolescent perceptions of adolescent efficacy for diabetes management: The association of depressed mood, and mothers and fathers views. Journal of Family Psychology, 23, 611–614. doi: 10.1037/a0016141 [DOI] [PubMed] [Google Scholar]
- Butler JM, Skinner M, Gelfand D, Berg CA, & Wiebe DJ (2007). Maternal parenting style and adjustment in adolescents with type 1 diabetes. Journal of Pediatric Psychology, 32, 1227–1237. doi: 10.1093/jpepsy/jsm065 [DOI] [PubMed] [Google Scholar]
- Cameron LD, Young MJ, & Wiebe DJ (2007). Maternal trait anxiety and diabetes control in adolescents with type 1 diabetes. Journal of Pediatric Psychology, 32, 733–744. doi: 10.1093/jpepsy/jsl053 [DOI] [PubMed] [Google Scholar]
- Cranford JA, Shrout PE, Iida M, Rafaeli E, Yip T, & Bolger N (2006). A procedure for evaluating sensitivity to within-person change: Can mood measures in diary studies detect change reliability? Personality and Social Psychology Bulletin, 32, 917–929. doi: 10.1177/0146167206287721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis DA, Podolski CL, Frey M, Naar-King S, Wang B, & Moltz K (2007). The role of parental monitoring in adolescent health outcomes: Impact on regimen adherence in youth with Type 1 diabetes. Journal of Pediatric Psychology, 32, 1–11. doi: 10.1093/jpepsy/jsm009 [DOI] [PubMed] [Google Scholar]
- Fortenberry KT, Butler JM, Butner J, Berg CA, Upchurch R, & Wiebe DJ (2009). Perceived diabetes task competence mediates the relationship of both negative and positive affect with blood glucose in adolescents with type 1 diabetes. Annals of Behavioral Medicine, 37, 1–9. doi: 10.1007/s12160-009-9086-7 [DOI] [PubMed] [Google Scholar]
- Fortenberry KT, Wiebe DJ, & Berg CA (2012). Perceptions of treatment control moderate the daily association between negative affect and diabetes problems among adolescents with Type 1 diabetes. Psychology & Health, 27, 294–309. [DOI] [PubMed] [Google Scholar]
- Franks MM, & Iida M (2010, November). Spouses’ daily support and control and patients’ daily dietary adherence and diabetes anxiety. Paper presented at Gerontological Society of America Meetings, New Orleans, LA. [Google Scholar]
- Helgeson VS, Reynolds KA, Siminerio L, Escobar O, & Becker D (2007). Parent and adolescent distribution of responsibility for diabetes self-care: Links to health outcomes. Journal of Pediatric Psychology, 33, 497–508. doi: 10.1093/jpepsy/jsm081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck GN, Johnson SZ, Wills KE, McKernon W, Rose B, Erklin S, & Kemper T (2002). Observed and perceived parental overprotection in relation to psychosocial adjustment in preadolescents with a physical disability: The mediational role of behavioral autonomy. Journal of Consulting and Clinical Psychology, 70, 96–110. doi: 10.1037/0022-006X.70.1.96 [DOI] [PubMed] [Google Scholar]
- Iannotti RJ, Schneider S, Nansel TR, Haynie DL, Plotnick LP, Clark LM, … Simons-Morton B (2006). Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. Journal of Developmental and Behavioral Pediatrics, 27, 98–105. doi: 10.1097/00004703-200604000-00003 [DOI] [PubMed] [Google Scholar]
- Kenny DA, Korchmaros JD, & Bolger N (2003). Lower level mediation in multilevel models. Psychological Methods, 8, 115–128. doi: 10.1037/1082-989X.8.2.115 [DOI] [PubMed] [Google Scholar]
- Kovatchev BP, Otto E, Cox D, Gonder-Frederick L, & Clarke W (2006). Evaluation of a new measure of blood glucose variability in diabetes. Diabetes Care, 29, 2433–2438. doi: 10.2337/dc06-1085 [DOI] [PubMed] [Google Scholar]
- Laffel LM, Connell A, Vangsness L, Goebel-Fabbi A, Mansfield A, & Anderson BJ (2003). General quality of life in youth with Type 1 diabetes: Relationship to patient management and diabetes-specific family conflict. Diabetes Care, 26, 3067–3073. doi: 10.2337/diacare.26.11.3067 [DOI] [PubMed] [Google Scholar]
- Lewis MA, & Rook KS (1999). Social control in personal relationships: Impact on health behaviors and psychological distress. Health Psychology, 18, 63–71. doi: 10.1037/0278-6133.18.1.63 [DOI] [PubMed] [Google Scholar]
- Martire LM, Stephens MAP, & Schulz R (2011). Independence centrality as a moderator of the effects of spousal support on patient well-being and physical functioning. Health Psychology, 30, 651–655. doi: 10.1037/a0023006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall AL, Cox DJ, Crean J, Gloster M, & Kovatchev BP (2006). A novel analytical method for assessing glucose variability: Using CGMS in type 1 diabetes mellitus. Diabetes Technology & Therapeutics, 6, 644–653. [DOI] [PubMed] [Google Scholar]
- Pomerantz EM, & Eaton MM (2001). Maternal intrusive support in the academic context: Transactional socialization processes. Developmental Psychology, 37, 174–186. doi: 10.1037/0012-1649.37.2.174 [DOI] [PubMed] [Google Scholar]
- Pomerantz EM, Moorman EA, & Litwack SD (2007). The how, whom, and why of parents’ involvement in children’s academic lives: More is not always better. Review of Educational Research, 77, 373–410. doi: 10.3102/003465430305567 [DOI] [Google Scholar]
- Raudenbush S, Bryk A, & Congdon R (2004). HLM 6: Hierarchical linear and nonlinear modeling. Chicago, IL: Scientific Software International. [Google Scholar]
- Rubin RR, Young-Hyman D, & Peyrot M (1989). Parent–child responsibility and conflict in diabetes care. Diabetes Care, 38, 28A. [Google Scholar]
- Saudek CD, Derr RL, & Kalyani RR (2006). Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. Journal of the American Medical Association, 295, 1688–1697. doi: 10.1001/jama.295.14.1688 [DOI] [PubMed] [Google Scholar]
- Soenens B, & Vansteenkiste M (2010). A theoretical upgrade of the concept of parental psychological control: Proposing new insights on the basis of self-determination theory. Developmental Review, 30, 74–99. doi: 10.1016/j.dr.2009.11.001 [DOI] [Google Scholar]
- Stephens MAP, Fekete EM, Franks MM, Rook KS, Druley JA, & Greene K (2009). Spouses’ use of pressure and persuasion to promote osteoarthritis patients’ medical adherence after orthopedic surgery. Health Psychology, 28, 48–55. doi: 10.1037/a0012385 [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Berg CA, Gelfand D, Butler J, Korbel C, Fortenberry KT, & McCabe J (2011). Longitudinal associations of maternal depressive symptoms, maternal involvement, and diabetes management across adolescence. Journal of Pediatric Psychology, 36, 837–846. doi: 10.1093/jpepsy/jsr002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe DJ, Berg CA, Korbel C, Palmer DL, Beveridge RM, Upchurch R, … Donaldson DL (2005). Children’s appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology, 30, 167–178. doi: 10.1093/jpepsy/jsi004 [DOI] [PubMed] [Google Scholar]
- Wysocki T, & Gavin L (2005). Paternal involvement in the management of pediatric chronic diseases: Associations with adherence, quality of life, and health status. Journal of Pediatric Psychology, 31, 501–511. doi: 10.1093/jpepsy/jsj042 [DOI] [PubMed] [Google Scholar]
- Wysocki T, Iannotti R, Weissberg-Benchell J, Laffel L, Hood K, Anderson B, & Chen R (2008). Diabetes problem solving by youths with type 1 diabetes and their caregivers: Measurement, validation and longitudinal associations with glycemic control. Journal of Pediatric Psychology, 33, 875–884. doi: 10.1093/jpepsy/jsn024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Nansel TR, Holmbeck GN, Chen R, Laffel L, Anderson BJ, & Weissberg-Benchell J (2009). Collaborative involvement of primary and secondary caregivers: Associations with youths’ diabetes outcomes. Journal of Pediatric Psychology, 34, 869–881. doi: 10.1093/jpepsy/jsn136 [DOI] [PMC free article] [PubMed] [Google Scholar]


