ABSTRACT
Background: Evidence from high-income countries (HICs) has documented a higher rate of post-traumatic stress disorder (PTSD) in females than males. However, data are limited on sex differences in PTSD from low- and middle-income countries (LMICs), despite particularly high levels of trauma experienced by LMIC youth.
Objectives: In a sample of adolescents from an impoverished South African community, we examined sex differences in PTSD, as well as co-occurring depression, adolescent age, and the type and extent of trauma exposure as potential contributors to female vulnerability.
Methods: Participants were recruited from high schools in the Khayelitsha area of Cape Town. Self-reported trauma exposure, PTSD and depressive symptoms were measured in 797 adolescents (62% female) aged 13–17 years. Poisson regressions were used to examine Risk Ratios (RR) based on probable PTSD diagnoses, and linear regressions were applied to assess posttraumatic stress symptom (PTSS) severity.
Results: 92% of adolescents reported trauma exposure, of whom 28% had probable PTSD. Prevalence of PTSD was higher for females than for males, even when controlling for total trauma exposure (RR = 1.71, p < .001) and co-occurring depressive symptoms (RR = 1.45, p = .005). By contrast, sex differences in depression were eliminated after controlling for co-occurring PTSS. There was little evidence of age effects on the emergence of sex differences. At lower thresholds of interpersonal trauma, females showed higher levels of PTSS compared to males, but no sex differences were found at high levels of exposure.
Conclusion: Higher PTSD rates are observed in adolescent females in a high adversity-LMIC sample suggesting sex differences are robust across international contexts. Sex differences in PTSD are unlikely to be explained by co-occurring depression and in this context sex differences in depression may be secondary to trauma and PTSD. However, exposure to significant interpersonal trauma appears to overrule any specific female vulnerability.
KEYWORDS: LMICs; childhood/adolescence; PTSD; sex-differences, trauma
HIGHLIGHTS
Sex differences in post-traumatic stress disorder are observed in adolescence from a high-adversity LMIC.
Greater female risk occurs even when adjusting for trauma exposure and depressive symptoms.
Females also show greater vulnerability to lower thresholds of interpersonal trauma.
Abstract
Antecedentes: La evidencia de una tasa más alta del trastorno de estrés postraumático (TEPT) ha sido documentada en países de ingresos altos (PIAs). Sin embargo, la evidencia respecto a las diferencias según el sexo es limitada en países con ingresos bajos o medios (PIBMs) a pesar de los niveles altos de trauma que experimenta su población joven.
Objetivos: Evaluamos las diferencias según género en el TEPT, además de la depresión comórbida, la edad del adolescente y el tipo y la duración de la exposición al trauma como potenciales contribuyentes a la vulnerabilidad femenina en una muestra de adolescentes de una comunidad pobre de Sudáfrica.
Métodos: Se reclutaron a los participantes de los colegios de secundaria del área de Khayelitsha de la Ciudad del Cabo. Se midieron la exposición autorreportada al trauma, los síntomas del TEPT y los síntomas de la depresión en 797 adolescentes (62% mujeres) entre los 13 y los 17 años. Se emplearon las regresiones de Poisson para evaluar el riesgo relativo (RR) basado en los diagnósticos probables del TEPT y se emplearon regresiones lineales para evaluar la severidad de los síntomas de estrés postraumático (SEPTs).
Resultados: El 92% de los adolescentes reportó exposición al trauma, del cual un 28% tenía un probable TEPT. La prevalencia del TEPT era más alta en mujeres que en varones, incluso luego de controlar el efecto de la exposición total al trauma (RR = 1.71, p < .001) y de los síntomas de la depresión comórbida (RR = 1.45, p = .005). Por el contrario, las diferencias según el sexo en la depresión fueron eliminadas luego de controlar el efecto de los SEPTs comórbidos. Había poca evidencia de que la edad tenga efecto sobre el origen de la diferencia según el sexo. Al emplear puntos de corte más bajos para medir el trauma interpersonal, las mujeres mostraron niveles más altos de SEPTs en comparación con los hombres; no obstante, no se encontraron diferencias según el sexo con niveles más elevados de exposición.
Conclusión: Se observan tasas del TEPT más altas en mujeres adolescentes en una muestra alta en exposición a la adversidad en un PIBM, lo que sugiere que las diferencias según el sexo son robustas y transversales a los contextos internacionales. Es poco probable que las diferencias según el sexo en el TEPT se expliquen por la depresión comórbida y, en este contexto, la depresión podría ser secundaria al trauma y al TEPT. Sin embargo, la exposición a un trauma interpersonal significativo impresiona anular cualquier vulnerabilidad femenina específica.
PALABRAS CLAVE: PIBM, infancia/adolescencia, TEPT, diferencias según el sexo, trauma
Abstract
背景: 来自高收入国家 (HIC) 的证据表明, 女性的创伤后应激障碍 (PTSD) 发生率高于男性。然而, 关于中低收入国家 (LMIC) 的PTSD 性别差异的数据有限, 尽管LMIC青年经历的创伤程度特别高。
目的: 在一个来自南非贫困社区的青少年样本中, 我们考查了 PTSD 的性别差异, 以及作为导致女性易感潜在因素的并发抑郁, 青少年年龄以及创伤暴露的类型和程度。
方法: 参与者从开普敦卡雅利沙地区的高中招募。在 797 名 13-17 岁的青少年 (62% 为女性) 中测量了自我报告的创伤暴露, PTSD 和抑郁症状。使用泊松回归考查基于可能 PTSD 诊断的风险比 (RR), 并应用线性回归来评估创伤后应激症状 (PTSD) 的严重程度。
结果: 92% 的青少年报告了创伤暴露, 其中28% 的青少年患有可能 PTSD。即使控制了总创伤暴露 (RR = 1.71, p< .001) 和并发抑郁症状 (RR = 1.45, p= .005), 女性的 PTSD 患病率也高于男性。相比之下, 在控制了并发 PTSD 后, 抑郁的性别差异被消除了。几乎没有证据表明年龄对性别差异的出现有影响。在较低的人际创伤阈值下, 与男性相比, 女性表现出更高水平的 PTSS, 但在高暴露水平下没有发现性别差异。
结论: 在一个高逆境-LMIC 样本中观察到青春期女性的 PTSD 发生率较高, 这表明在国际环境中性别差异稳健。 PTSD 的性别差异不太可能用并发抑郁来解释, 在这种情况下, 抑郁的性别差异可能继发于创伤和 PTSD。然而, 重大人际创伤暴露似乎可以控制任何特定的女性易感性。
关键词: LMIC, 童年/青春期, PTSD, 性别差异
1. Introduction
Epidemiological surveys have consistently documented a higher prevalence of posttraumatic stress disorder (PTSD) in females versus males, with women being at least twice as likely to develop PTSD during their lifetime (Ditlevsen & Elklit, 2010; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Merikangas et al., 2010; Tolin & Foa, 2006; Trickey, Siddaway, Meiser-Stedman, Serpell, & Field, 2012). In addition to being more prevalent, PTSD in women tends to be more severe and chronic with higher comorbidity rates with depression and anxiety disorders often reported (Breslau, Davis, Andreski, Peterson, & Schultz, 1997; Kilpatrick et al., 2013; Tolin & Foa, 2006).
Sex differences in PTSD have also been observed in studies of adolescent samples, whereas there is equivocal evidence of such effects in children. Results from a large meta-analysis of 64 studies found that female sex became a stronger risk factor as age increased, based on samples of children aged 6–18 years (Trickey et al., 2012). Similarly, longitudinal data from the UK ALSPAC cohort evidenced higher levels of PTSD symptoms in females versus males at ages 13 and 15 years, but not at ages 8 and 10 years (Haag et al., 2020). The emergence of sex differences throughout development suggests that the mechanism of PTSD formation may potentially be explained through changes in neuroendocrine, hormonal and stress response systems that are naturally affected during puberty (e.g. changes in adrenal androgens and sex steroids), which can seemingly impact neuroplasticity (Holder & Blaustein, 2014) and heighten female vulnerability to trauma and stress (e.g. see Garza & Jovanovic, 2017). The age-related effect may also reflect the emergence of differential psychological responses to stressful events, such as the tendency of female adolescents to engage in rumination (Hampel & Petermann, 2005).
The characteristics of the traumatic experiences have also been implicated in the reported sex differences in PTSD, with women at an increased risk of experiencing certain types of interpersonal trauma, and/or showing increased susceptibility to PTSD following exposure to such events (Alisic et al., 2014; Cortina & Kubiak, 2006; Nöthling, Simmons, Suliman, & Seedat, 2017). In principle, higher rates of PTSD may develop following interpersonal trauma because it is more often chronic, erodes social support, and/or leads to more self-blame and other maladaptive cognitions (Hetzel-Riggin & Roby, 2013). In children and adolescents, interpersonal violence, including sexual and physical violence, has been shown to present a higher conditional risk for PTSD when compared with non-interpersonal traumatic events (Alisic et al., 2014; Luthra et al., 2009). However, it is unclear whether sex differences in PTSD are particularly strong following interpersonal versus non-interpersonal trauma. Alternatively, the disproportionately higher risk of PTSD in females may be secondary to well-established sex differences in depression that also emerge during adolescence (Wade, Cairney, & Pevalin, 2002) given that depressive symptoms overlap considerably with PTSD symptoms (American Psychiatric Association, 2013) and are an extremely common sequelae of trauma exposure (Flory & Yehuda, 2015).
Research into sex differences in PTSD has provided valuable insight into more efficient prevention and treatment strategies (Ascienzo, Sprang, & Royse, 2021; Olff, Langeland, Draijer, & Gersons, 2007), yet more gender- and sex-sensitive research and reporting is needed (e.g. see the gender policy of the European Association of Science Editors). Further, the vast scope of scientific discourse stems from high-income countries (HICs), despite the World Health Organization reporting that 80% of people likely to experience a mental disorder in their lifetime reside in LMICs. Consequently, the majority of evidence in the extant literature derives from young people at relatively low risk of trauma and PTSD (Haag et al., 2020; Trickey et al., 2012). Little attention has been given to examining the prevalence of PTSD according to sex in children from LMICs, where exposure to trauma can be both frequent and persistent (Seedat, Nyamai, Njenga, Vythilingum, & Stein, 2004; Suliman, Kaminer, Seedat, & Stein, 2005). For example, one study shows how 91% of urban youth in South Africa had directly or vicariously experienced a traumatic event, with a high proportion witness to domestic abuse and/or a violent crime (Suliman et al., 2005). How sex differences in PTSD present among children living in contexts where exposure to significant trauma is commonplace is underexplored. Considering the possible array of psychological, emotional, behavioural, and cognitive difficulties faced post-trauma, more precise information regarding the emergence of sex differences in LMIC youth samples could assist with the creation of more efficient screening and resource allocation for both prevention and treatment.
In the current cross-sectional study, we examined sex differences in PTSD and posttraumatic stress symptoms (PTSS) in young people (13–17 years) living in an impoverished peri-urban community in Cape Town, South Africa, where rates of childhood trauma exposure are markedly high. First, we examined sex differences in risk of PTSD and the severity of post-traumatic stress symptoms (PTSS). Examination of sex differences in both PTSD and PTSS is important to establish whether sex differences are evident dependent on diagnostic thresholds, which may have important clinical implications, as well as subthreshold manifestations across the entire range of symptoms. Second, due to the high comorbidity of PTSD with depression, we also sought to examine whether sex differences in PTSS were independent of depressive symptoms, and vice versa. Third, we explored whether sex differences in this LMIC youth sample replicate findings from high-income countries in which females are at greater risk of PTSD in the later stages of adolescence. Finally, we examined sex differences in PTSD and PTSS according to the cumulative number of both interpersonal and non-interpersonal traumatic experiences and hypothesized that any sex differences in PTSD may be particularly salient due to interpersonal trauma exposure.
2. Methods
2.1. Participants and procedures
Participants were recruited by the Masiphuplisane Research Centre from four randomly selected high schools in the Khayelitsha area of Cape Town. Schools in South Africa are ranked from Quintile 1 to 5 for the purpose of fair resource allocation, with Quintile 1 being the ‘poor/impoverished’ school and Quintile 5 being a ‘wealthy/affluent’ school. In the current study, three schools were characterized Quintile 2, and one was Quintile 3. In participating schools, information sheets and opt-out consent forms were sent to parents and caregivers of Grade 8–12 classes. Where parental consent was obtained, questionnaires were completed individually in classrooms during school hours in the presence of a trained researcher and social worker. Questionnaires took approximately 15 minutes to complete and comprised measures of PTSD and depression. Non-participating students (and those without parental consent, n = 7 in total) were given a different activity to perform.1 Students were informed of the voluntary nature of the study and about school safeguarding procedures regarding disclosure of risky events (e.g. sexual assault). After the questionnaires were administered, participants received a debrief sheet containing contact details for relevant mental health service centres. Initially, 859 participants aged between 13 and 17 years were enrolled. Sixty-two participants did not specify their sex and were therefore excluded from further analyses resulting in available data from 797 respondents (37.8% male; 62.2% female). The larger proportion of girls is likely attributable to a greater likelihood of boys dropping out of school to seek employment and is similar to previous school studies conducted in South Africa (Seedat et al., 2004). The excluded sample based on sex did not differ from the study sample in terms of age, school, grade or living arrangements; thus, the representativeness of the target population was not affected.
2.2. Ethical considerations
Ethical approval was obtained from the Western Cape Education Department, and from the University of Bath research and ethics committees. Participants provided informed consent, and parents or caregivers of each participant were provided with researcher contact details and information leaflets with the option to opt out on behalf of their child at least 1 week prior to data collection in schools.
2.3. Measures
2.3.1. Demographic data
Brief demographic information was collected from each participant including the participant’s sex, age, school grade, and living arrangements (i.e. who they live with). All questionnaires administered were translated from English to isiXhosa and then back-translated to English.
2.3.2. Trauma exposure – UCLA-RI
The UCLA Traumatic Stress Disorder Reaction Index for children and adolescents (UCLA-RI) was used to screen for exposure to traumatic events. Adolescents reported whether they had experienced 11 traumatic events (yes/no); which event was the most worrisome; and age at the time of the focal event. Five questions comprised interpersonal traumas, e.g. ‘Being beaten up, shot at or threatened to be hurt badly in your town’, whereas six were non-interpersonal, e.g. ‘Being in another kind of disaster, like a fire, tornado, or hurricane’ (see Supplementary Table 1). Items relating to sexual violence were not included in the trauma screening due to ethical concerns. Specifically, sexual trauma is associated with considerable stigma in South Africa, and as questionnaire responses could potentially be observed by others in the classroom, we did not consider this a safe context for adolescents to disclose such exposure. However, an additional item (Q12) enquired about an occurrence of a traumatic event not previously described, which provided an opportunity to disclose sexual violence, and written responses were coded depending on whether they were indicative of interpersonal or non-interpersonal trauma. Scores were generated to capture the total number of traumatic events the child endorsed (possible range 0–12) and the number of interpersonal (0–6) and non-interpersonal (0–7) events. Both interpersonal and non-interpersonal trauma scores were transformed from continuous variables into factor variables to reduce the positive skew from fewer respondents reporting very high numbers of events, with no events coded as 0 (base category), 1 event = low, 2 events = moderate, and 3+ events = high severity.
2.3.3. PTSS and PTSD – CPSS-SR
Self-reported symptoms of post-traumatic stress were assessed using the Child PTSD Symptom Scale – Self Report for DSM-5 (CPSS-SR-5), an age-appropriate questionnaire with established validity, high internal consistency, and test–retest reliability. Participants are asked to think about the experience on the trauma screen they identify as being the most significant and upsetting and answer 20 PTSD symptom items rated on a 5-point scale about how often the problem has bothered them in the last month from 0 = ‘Not at all’ to 4 = ‘Six or more times a week /severe’. Responses were summed up to create PTSS scores between 0 and 80 (Cronbach’s α = 0.92). A diagnosis of probable PTSD as a binary outcome (present/absent) was created if PTSS total scores were greater than 31, as per the recommended guidelines.
2.3.4. Depressive symptoms
We used the 10-item Center for Epidemiological Studies Depression Scale for Children (CES-D-10), which is a valid, reliable screening tool for South African populations (Baron, Davies, & Lund, 2017). Participants rated the depressive symptoms they had experienced in the last week on a Likert scale, from 0 = ‘Rarely or none of the time’ to 3 = ‘All of the time (5–7 days a week’). Two of the questions are phrased positively and reverse scored. Total scores range from 0–30 (Cronbach’s α = 0.76).
2.4. Statistical analysis
Statistical analyses were conducted using Stata, version 16.1 (Statacorp, College Station, TX). We initially examined the frequency and type of trauma exposures in the sample. As PTSD, by definition, can only be measured in individuals who have been exposed to a qualifying trauma, subsequent analyses were conducted in those exposed to at least one traumatic experience, bringing the analytic sample to 735. Initial analyses involved comparing males (coded 0) and females (coded 1) using independent t-tests and Pearson’s chi-square tests of independence (Table 1). The association between sex and probable PTSD diagnosis (absent/present) was then assessed using Poisson regression with robust error variance (Zou, 2004), unadjusted and adjusted for total trauma exposure. Sex differences in PTSS were investigated using linear regression, also unadjusted and adjusted for total trauma exposure. In additional models, we controlled for depressive symptoms to examine whether sex differences in PTSD could be explained by an overlap with depression, and conversely reran the same models with depressive symptoms as the dependent variable with adjustment for PTSS. To investigate whether females and males differed in their risk of PTSD based on age, we operationalized age as a factor variable (due to some evidence of a nonlinear relationship between age and probable PTSD in males) and computed statistical tests for interactions between sex and age categories with subsequent reporting of simple effects. Evidence for an interaction effect was set at p < .10 (Sterne et al., 2001). To investigate whether males and females differed in their risk for PTSD and PTSS symptoms according to the frequency of interpersonal trauma, sex by interpersonal trauma interactions were computed. As the majority of the sample had also experienced non-interpersonal trauma, the risk for PTSD from multiple interpersonal traumas was conducted by controlling for non-interpersonal traumas coded the same way as the interpersonal variables defined above. Finally, a similar analysis was conducted to investigate whether sex differences in PTSD and PTSS emerged due to the frequency of non-interpersonal trauma as the variable of interest, adjusting for exposures to interpersonal trauma.
Table 1.
Sample characteristics of trauma-exposed participants
| All (n = 735) |
Males (n = 275) | Females (n = 460) |
Male vs. female | |
|---|---|---|---|---|
| Age in years (M ± SD) | 15.37 ± 1.31 | 15.52 ± 1.28 | 15.28 ± 1.32 | t = −2.28, p = .023 |
| Age at focal event (M ± SD) | 12.52 ± 2.78 | 12.68 ± 2.69 | 12.43 ± 2.84 | t = −1.10, p = .27 |
| Time since focal trauma (M ± SD years) | 2.85 ± 2.60 | 2.84 ± 2.54 | 2.85 ± 2.63 | t = −0.09, p = .93 |
| School quintile 2, %, [N] | 81.1%, [596] | 84.7%, [233] | 78.9%. [363] | χ2 (1) = 3.79, p = .51 |
| Trauma scores (M ± SD) | ||||
| Total trauma | 3.45 ± 1.98 | 3.64 ± 2.03 | 3.34 ± 1.95 | t = −1.99, p = .048 |
| Interpersonal trauma | 1.73 ± 1.21 | 1.77 ± 1.22 | 1.70 ± 1.20 | t = −0.71, p = .48 |
| Non-interpersonal trauma | 1.67 ± 1.22 | 1.83 ± 1.31 | 1.57 ± 1.15 | t = −2.78, p = .006 |
| *PTSD diagnosis, %, [N] | 27.6% [203] | 20.4%, [56] | 32.0%, [147] | χ2 (1) = 11.57, p < .001 |
| CPSS scores (M ± SD) | 21.38 ± 16.97 | 18.67 ± 15.65 | 23.00 ± 15.96 | t = 3.59, p < .001 |
| CES-D-10, (M ± SD) | 7.87 ± 5.14 | 7.34 ± 5.02 | 8.19 ± 5.19 | t = 2.18, p = .030 |
*PTSD diagnoses are based on the recommended cut-off from the CPSS-SR (>31).
3. Results
3.1. Participant information
The majority (92.2%) of the 797 young people who completed questions reported exposure to at least one trauma, and this was similar for males (91.4%, n = 275) and females (92.7%, n = 460, χ2(1) = 0.50, p = .481). The proportion of males and females reporting any interpersonal (males 81.1%, n = 244; females 80.2%, n = 398; χ2(1) = 0.08, p = .776) or non-interpersonal trauma (males 77.4%, n = 233; females 76.6%, n = 380; χ2(1) = 0.07, p = .796) was also similar.
Sample characteristics for the trauma-exposed participants (n = 735) are reported in Tables 1; 37.8% were male and 62.2% were female. Sample mean age was 15.4 years (SD = 1.31, range 13 to 17 years) and males were slightly older than females. The median number of traumas endorsed by participants was 3 (range 1–11), and males reported higher overall and non-interpersonal trauma scores compared to females. The average amount of time since the focal traumatic event was 2.8 years and ‘witnessing someone in their town being beaten up, shot at, or killed’ was the most common worst event that anchored 26.3% of males’ and 23.4% of females’ PTSD assessments (ST1). Further details relating to the proportion of participants who reported exposure to specific traumas are also provided in ST1.
3.2. Sex differences in PTSD
For the 735 children and adolescents who had been exposed to trauma, 27.6% (n = 203) had probable PTSD based on their CPSS scores. Poisson regression was performed to explore sex differences in incidence.
In an unadjusted model, females were more likely to meet criteria for probable PTSD compared to males (RR = 1.57, SE = 0.22, 95% CI = 1.20–2.05, p < .001). When the model was adjusted for total trauma exposure, this effect increased, with females being 71% more likely to meet symptom criteria for PTSD when compared to males (RR = 1.71, SE = 0.22, 95% CI = 1.33–2.20, p < .001). As expected, total trauma scores were also associated with PTSD (RR = 1.29, SE = 0.03, 95% CI = 1.23–1.34, p < .001).
The mean PTSS score for this sample was 21.4, which is of moderate severity. In a preliminary linear regression analysis, higher PTSS scores were found in females compared to males [β = 4.34, SE = 1.21, 95% CI = 1.97–6.71; model F(1,733) = 12.89, p < .001, R2 = 0.02]. When this model was adjusted for total trauma scores (β = 3.68, SE = 0.26, 95% CI = 3.16–4.19, p < .001), the sex difference in PTSS was retained [β = 5.44, SE = 1.08, 95% CI = 3.32–7.55, p < .001; model F(2,732) = 106.03, p < .001, R2 = 0.22].
3.3. Comorbidity in symptoms of PTSD and depression
As expected, females showed higher levels of depressive symptoms than males (Table 1), and symptoms of depression and PTSS were moderately correlated (r = 0.64, N = 735). We therefore examined whether sex differences in PTSD in adolescents were explained by an overlap with depressive symptoms, and vice versa. Utilizing the previous models from Section 3.2, we additionally adjusted models for depression scores obtained from the CES-D-10.
Females were still at an increased risk of PTSD compared to males, although the relative risk decreased from 71% to 45% (RR = 1.45, SE = 0.17, 95% CI = 1.15–1.83, p = .002). Similarly, females versus males reported greater PTSS scores when depressive symptoms were controlled [β = 3.51, SE = 0.89, 95% CI = 1.76–5.26, p < .001: model F(3,731) = 220.62, p < .001, R2 = 0.48]. Finally, a similar model was run with depressive symptoms as the outcome variable which, as expected, identified a sex effect (β = 1.14, SE = 0.36, 95% CI = 0.43–1.85, p = .002, R2 = 0.15), with females showing greater depressive symptoms than males. However, sex differences in CESD-D-10 scores were eliminated by adjusting for PTSS scores (β = 0.10, SE = 0.30, 95% CI = −0.50–0.70, p = .74).
3.4. Influence of age on sex differences in PTSD
Next, we examined our hypothesis in which we expected that female versus male risk of PTSD and PTSS increases through adolescence. We performed Poisson and linear regressions and present unadjusted models and models adjusted for total trauma exposure and depressive symptoms.
Poisson regression found no main effects of age (χ2(4) = 6.24, p = .18) and no significant interaction between age and sex, (χ2(4) = 5.47, p = .24) in relation to a probable PTSD diagnosis. When the model was adjusted for total trauma and depressive symptoms, findings were the same (age: (χ2(4) = 5.71, p = .22; age × sex: (χ2(4) = 2.68, p = .61). As illustrated in Figure 1(a), post hoc simple effects demonstrated that females were more likely than males to meet criteria for PTSD at 17 years, (χ2(1) = 7.28, p = .007), but not at any other age.
Figure 1.
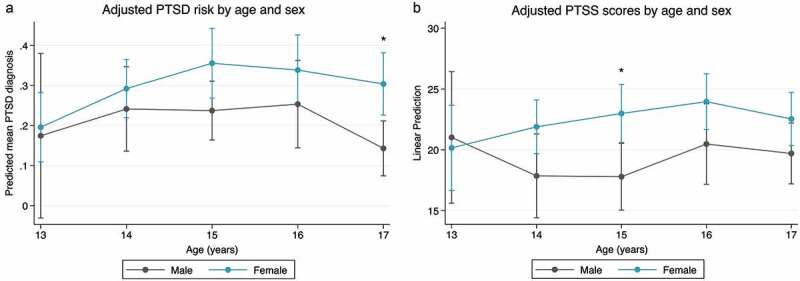
Adjusted associations between PTSD risk and PTSS scores according to age and sex. Models are controlled for depressive symptoms and total trauma scores. Plots show least squares means and bars show the 95% confidence intervals. Post-hoc simple effects show females are at a greater risk of a probable PTSD diagnosis at age 17 years compared to males and exhibit higher symptoms at age 15 years, although a main sex × age interaction effect was not observed for either measure
Similarly, in an unadjusted linear regression model, there was no interaction between sex and age for PTSS [F(4,707) = 0.52, p = .72], and no main effect of age [F(4,707) = 0.45, p = .77; model F(9,707) = 1.92, p = .05, R2 = 0.02], with these null findings related to age being replicated in the adjusted model [age: F(4,705) = 0.76, p = .55; age × sex: F(4,705) = 0.70, p = .59; model F(11,705) = 58.32, p < .001, R2 = 0.48]. Analysis of post-hoc simple effects showed greater PTSS scores in females compared to males at age 15, (χ2(1) = 7.28, p = .005) (Figure 1(b)), but not at any other age.
3.5. Impact of interpersonal trauma exposures on PTSD risk
Next, we investigated whether exposure to interpersonal traumatic events conferred increased risk for PTSD and PTSS in females relative to males. No exposure to an interpersonal trauma was coded as 0 (base), with 1, 2, or 3+ indicating low, moderate, and high exposure levels, respectively. All models were adjusted for depressive symptoms, age, and non-interpersonal trauma scores.
There was no evidence of an interaction between sex and interpersonal trauma scores on PTSD risk [χ2(3) = 4.42, p = .22], although as expected, analysis of main effects indicated that female sex [χ2(1) = 7.36, p = .001], and greater levels of interpersonal trauma [χ2(3) = 12.85, p = .005] conferred greater risk for PTSD. In contrast, there was a significant interaction between sex and interpersonal trauma scores on PTSS scores [F(3,704) = 2.40, p = .067; model F(12,704) = 52.25, p < .001, R2 = 0.46]. Analyses of simple contrasts indicated that females were more likely to possess greater symptoms when exposed to both low [F(1,704) = 4.22, p = .040] and moderate [F(1,704) = 15.09, p < .001] levels of interpersonal trauma compared to males (Figure 2(a)). No sex differences were observed at high levels of interpersonal trauma [F(1,704) = 0.01, p = .97] or when no incidences of interpersonal trauma were reported [F(1,704) = 1.51, p = .22].
Figure 2.
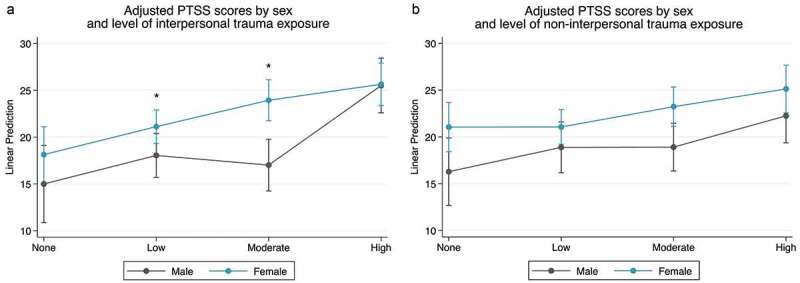
Sex differences in posttraumatic stress symptoms (PTSS). (a) A significant interaction between sex and the severity or frequency of interpersonal trauma was found highlighting female’s greater vulnerability to lower levels of exposure; in contrast (b) shows no significant interaction between sex and levels of non-interpersonal trauma exposure
3.6. Impact of non-interpersonal trauma exposures on PTSD risk
We similarly examined whether sex differences exist in PTSD and PTSS related to the number of exposures to non-interpersonal traumatic events, adjusting for co-occurring interpersonal trauma. There was no evidence of an interaction between sex and non-interpersonal trauma scores on PTSD risk [χ2(3) = 2.62, p = .45], and main effects indicated that female sex [χ2(1) = 8.08, p = .005], but non-interpersonal trauma [χ2(3) = 2.72, p = .44] conferred greater risk for PTSD. Similarly, no interaction was observed between sex and non-interpersonal trauma scores on PTSS scores, (F(3,706) = 0.43, p = .73) (Figure 2(b)), but female sex [F(1,701) = 13.79, p < .001] and higher non-interpersonal trauma scores (F(3,701) = 3.94, p = .008) were each associated with higher PTSS [model F(10,706) = 61.42, p < .001, R2 = 0.46].
4. Discussion
The primary aim of this study was to determine the contribution of self-reported sex on the conditional risk of PTSD and PTSS in young people from an impoverished community in South Africa. We demonstrate that adolescent females located within a LMIC context are subjected to a greater risk of PTSD and possess higher PTSS symptoms than males, which is supportive of previous studies conducted in HICs. Co-occurring depressive symptoms did not account for the reported sex differences in PTSD, whereas sex differences in depression were eliminated by controlling for by trauma exposure and co-occurring PTSS. Contrary to hypotheses, we did not find robust evidence to suggest that female risk was heightened with increasing age. Finally, we found evidence that females were more susceptible to PTSS following low or moderate traumatic exposures to interpersonal traumatic events when compared to males, whereas no sex differences were observed when high levels of interpersonal violence exposures were encountered. No sex differences in PTSS were observed for the cumulative effect of non-interpersonal traumatic experiences.
Rates of trauma exposure in the current sample (92%) are extremely high, consistent with previously published estimates from similar settings (Seedat et al., 2004; Suliman et al., 2005). The prevalence of probable PTSD in trauma-exposed individuals is also notably high at 28%. By comparison, a meta-analysis of 72 articles (N = 3563) found the overall rate of PTSD in trauma-exposed children and young people to be 16%, but notably only three studies from LMICs were included (Alisic et al., 2014). The mean time elapsed since the focal trauma exposure and the assessment in the current sample was almost 3 years, suggesting that young people were coping with chronic posttraumatic distress without structured psychological care. These observations reaffirm the urgent need for further study of LMIC youth, as markedly high levels of trauma exposure and PTSD relative to studies of HIC populations mean that they are extremely poorly represented by the extant literature.
In models unadjusted for potentially confounding variables, we found that young females were 57% more likely to report PTSD compared to males, with this difference in risk being greater (71%) when models were adjusted for total trauma exposure. This reported increased risk of PTSD in females is lower than the commonly reported two- to threefold increased risk from studies predominantly conducted in high-income nations (Ditlevsen & Elklit, 2010; Kessler et al., 1995; Tolin & Foa, 2006; Trickey et al., 2012). Notably, two national surveys of US adolescents found a three- to fourfold higher incidence of PTSD among adolescent females versus males aged 13–18 years (Merikangas et al., 2010; McLaughlin et al., 2013). However, the majority of previous research into developmental sex differences in PTSD has been conducted in HIC populations in which adolescent exposure to multiple traumas is uncommon (e.g. McLaughlin et al., 2013). By contrast, many South African youth live in conditions characterized by high levels of ongoing threat and repeated traumatic exposures; adolescents in the current study reported exposure to a median of three different trauma types. Counter to expectations, we found no evidence of an age by sex interaction in relation to a probable PTSD diagnosis and PTSS, whereas previous studies have suggested that females are particularly vulnerable to PTSD in later adolescence in comparison to younger children (Haag et al., 2020; Trickey et al., 2012). Some evidence suggests that females may have a greater likelihood of a probable PTSD diagnosis at age 17 compared to males, but a non-significant interaction term suggests larger sample sizes of participants at each age are needed for further investigation.
This study suggests that the higher prevalence of PTSD in females does not appear to be explained by an overlap with depressive symptoms, despite the well-established emergence of sex differences in depressive symptoms during adolescence (Wade et al., 2002). When co-occurring depressive symptoms were controlled, PTSD and PTSS were still evidently greater in females, albeit with a slight reduction in the relative risk for PTSD from 71% to 45%. This is remarkable, given the extent of overlap between PTSD and depressive symptoms and well-established comorbidity between these conditions. Importantly, the expected sex differences in depressive symptoms which were also evident in our sample in unadjusted analyses were wholly eliminated by controlling for co-occurring PTSS. One important consideration here is that the lifetime prevalence of both PTSS and depressive symptoms were not available, and both are known to fluctuate over time. As such, although our findings suggest that sex differences in depressive symptoms may be secondary to sex differences in vulnerability to PTSD in youth exposed to high levels of trauma, longitudinal data that examines the sequential emergence of these problems may provide a different perspective.
We found some evidence that females in the current study were more vulnerable to developing PTSS than males at lower levels of exposure to interpersonal trauma, but there was no evidence of sex differences at the highest levels of exposure or due to exposure to non-interpersonal trauma events. This is in accordance with a ceiling effect that has been proposed for sex differences in PTSD, whereby high levels of PTSS following particularly toxic traumas in both males and females will overrule any specific female vulnerability to traumatic stress (Gavranidou & Rosner, 2003). In other words, the overall smaller magnitude of sex differences could reflect a diminishing influence of sex as trauma intensity increases. This is supported by the fact that biological sex only accounted for 2% of the total variance in PTSS symptoms, whereas the total trauma exposure explained 20%. These observations reinforce the critical importance of addressing the consequences of exposure to multiple traumas for mental health among young people, particularly among LMIC populations likely to be affected by such experiences. For example, exposure to multiple types of interpersonal traumatic events (over 3 events) increased the risk of PTSD by ~115% in females in the trauma-exposed sample.
Many theories have been put forward to explain the sex disparity in the prevalence of PTSD and associated symptoms, including gender roles, genetic predisposition, and hormonal influences including the menstrual cycle and hormonal contraception. For example, increased susceptibility to PTSD in females may reflect an increased vulnerability in the formation of emotional memories due to the influence of sex hormones and resulting increases in brain plasticity that may facilitate over-consolidation of traumatic experiences (Li & Graham, 2017). Further, boys tend to engage in externalizing rather than internalizing behaviours following trauma, which may result in a higher prevalence of conduct disorders (Tolin & Foa, 2006) which should be the subject of further study. Additionally, researchers are examining whether sex differences in stress reactivity and the endocrine response may bias women and men towards different psychopathology (Bangasser, Eck, & Ordoñes Sanchez, 2019; Blanco et al., 2018; Zimmerman et al., 2020). Further study of the mechanisms underlying the emergence of sex difference in PTSD is critical and can inform a wider understanding of females’ vulnerability to stress-related mental health disorders.
Results of this study should be considered in the context of several limitations. First, we focused on self-reported sex and did not measure participant’s gender identity, or gender role orientation, an omission that should be addressed in future work (Christiansen & Berke, 2020). Second, the size of the groups organized by age and sex were not equal, with a smaller sample size at age 13, which may have compromised the outcome of age-related sex differences, and fewer males than females participated overall due to fewer males staying in the school system. Third, the use of self-report instruments in a school classroom setting instead of an assessment by a clinician or mental health professional could have overestimated the severity of symptoms (Carlson et al., 2011; Suliman et al., 2005). Nevertheless, the administration of questionnaires in a large classroom setting instead enabled a large amount of data to be collected. Moreover, in settings such as South Africa where considerable stigma are attached to mental health problems, it is also possible that face-to-face interviews would lead to underreporting. Fourth, the omission of explicit items assessing sexual violence due to ethical concerns and resource availability to make appropriate referrals meant that the full extent of sexual violence encountered may have not been captured. Only 1.6% of respondents [n = 13] specifically mentioned being a victim or target of rape or sexual assault spontaneously under ‘other’ trauma. Given that 10% of boys and 15% of girls (aged 15–17 years) have previously reported some lifetime sexual victimization in South Africa (Ward, Artz, Leoschut, Kassanjee, & Burton, 2018) it appears likely that exposure to sexual violence has been underestimated. Another limitation is that the extent of trauma exposure was measured by summing the different types of events that adolescents reported, which will underestimate the number of actual events experienced for young people who experienced more than one exposure to the same type of event. A recent large, cross-national (US–Mexico) trauma study demonstrated that while the number of trauma event types typically correlates very highly with actual event counts, this association is reduced at extremely high levels of trauma exposure (Rasmussen et al., 2020). Nonetheless, in the same study, the different types of trauma experienced were a stronger predictor of PTSD than the overall quantity of events. Finally, the cross-sectional design limits the ability to make causal inferences especially with regard to the sequential emergence of both PTSS and depressive symptoms. Longitudinal data that also considers the impact of other prior childhood adversities and/or prior disorders will likely contribute to a greater understanding of developmental sex-differences in the emergence of PTSD.
5. Conclusions
The current study of a large sample of students from an impoverished LMIC context, who had experienced a complex range of traumas, adds important information to the existing literature regarding potential sex differences in risk of PTSD during adolescence. Our findings indicate that the higher PTSD rates in adolescent females are likely to be robust across international contexts. However, the relatively small magnitude of sex effects relative to studies of HIC adolescent samples and the lack of systematic changes with age warrant further investigation. Depressive symptoms did not account for the observed sex differences in PTSD or PTSS, and sex differences in depressive symptoms were eliminated by controlling for PTSS, suggesting that in a high adversity context sex differences in depression may be secondary to trauma and PTSD. Lower thresholds of interpersonal trauma incurred higher rates of PTSS in females versus males with our data supporting a proposed ceiling effect in which significant interpersonal traumas experienced by both sexes will overrule any specific female vulnerability. Overall, developmental sex differences in PTSD remain largely unexplained, and further examination of the determinants of female vulnerability and/or male resilience during adolescence could help derive novel preventative measures and interventions.
Supplementary Material
Funding Statement
This work was funded by Research England (RH/SH) and MRC grant MR/T002816/1 (SH). This publication is the work of the authors, and they will serve as guarantors for the contents of this paper.
Note
While official participation rates were not formally monitored, there was very high uptake for participants who attended school on the day of data collection with almost all children participating. Overall, weekly attendance at these schools is typically ~65%.
Data availability
The data that support the findings of this study are available on request from the corresponding author [LVH]. The data are not publicly available due to [restrictions, e.g., their containing information that could compromise the privacy of research participants].
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed here.
References
- Alisic, E., Zalta, A. K., van Wesel, F., Larsen, S. E., Hafstad, G. S., Hassanpour, K., & Smid, G. E. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. British Journal of Psychiatry, 204(5), 335–11. doi: 10.1192/bjp.bp.113.131227 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Ascienzo, S., Sprang, G., & Royse, D. (2021). Gender differences in the PTSD symptoms of polytraumatized youth during isolated phases of trauma-focused cognitive behavioral therapy. Psychological Trauma. doi: 10.1037/tra0001028 [DOI] [PubMed] [Google Scholar]
- Bangasser, D. A., Eck, S. R., & Ordoñes Sanchez, E. (2019). Sex differences in stress reactivity in arousal and attention systems. Neuropsychopharmacology, 44(1), 129–139. doi: 10.1038/s41386-018-0137-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron, E. C., Davies, T., & Lund, C. (2017). Validation of the 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10) in Zulu, Xhosa and Afrikaans populations in South Africa. BMC Psychiatry, 17(1), 6. doi: 10.1186/s12888-016-1178-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco, C., Hoertel, N., Wall, M. M., Franco, S., Peyre, H., Neria, Y., … Limosin, F. (2018). Toward understanding sex differences in the prevalence of posttraumatic stress disorder: Results from the National Epidemiologic Survey on alcohol and related conditions. The Journal of Clinical Psychiatry, 79(2), 16m11364. doi: 10.4088/JCP.16m11364 [DOI] [PubMed] [Google Scholar]
- Breslau, N., Davis, G. C., Andreski, P., Peterson, E. L., & Schultz, L. R. (1997). Sex differences in posttraumatic stress disorder. Archives of General Psychiatry, 54(11), 1044–1048. doi: 10.1001/archpsyc.1997.01830230082012 [DOI] [PubMed] [Google Scholar]
- Carlson, K. F., Kehle, S. M., Meis, L. A., Greer, N., MacDonald, R., Rutks, I., … Wilt, T. J. (2011). Prevalence, assessment, and treatment of mild traumatic brain injury and posttraumatic stress disorder: A systematic review of the evidence. The Journal of Head Trauma Rehabilitation, 26(2), 103–115. doi: 10.1097/HTR.0b013e3181e50ef1 [DOI] [PubMed] [Google Scholar]
- Christiansen, D. M., & Berke, E. T. (2020). Gender- and sex-based contributors to sex differences in PTSD. Current Psychiatry Reports, 22(4), 19. doi: 10.1007/s11920-020-1140-y [DOI] [PubMed] [Google Scholar]
- Cortina, L. M., & Kubiak, S. P. (2006). Gender and posttraumatic stress: Sexual violence as an explanation for women’s increased risk. Journal of Abnormal Psychology, 115(4), 753–759. doi: 10.1037/0021-843X.115.4.753 [DOI] [PubMed] [Google Scholar]
- Ditlevsen, D. N., & Elklit, A. (2010). The combined effect of gender and age on post traumatic stress disorder: Do men and women show differences in the lifespan distribution of the disorder? Annals of General Psychiatry, 9(1), 32. doi: 10.1186/1744-859X-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flory, J. D., & Yehuda, R. (2015). Comorbidity between post-traumatic stress disorder and major depressive disorder: Alternative explanations and treatment considerations. Dialogues in Clinical Neuroscience, 17(2), 141–150. doi: 10.31887/DCNS.2015.17.2/jflory [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garza, K., & Jovanovic, T. (2017). Impact of gender on child and adolescent PTSD. Current Psychiatry Reports, 19(11), 87. doi: 10.1007/s11920-017-0830-6 [DOI] [PubMed] [Google Scholar]
- Gavranidou, M., & Rosner, R. (2003). The weaker sex? Gender and post-traumatic stress disorder. Depression and Anxiety, 17(3), 130–139. doi: 10.1002/da.10103 [DOI] [PubMed] [Google Scholar]
- Haag, K., Fraser, A., Hiller, R., Seedat, S., Zimmerman, A., & Halligan, S. L. (2020). The emergence of sex differences in PTSD symptoms across development: Evidence from the ALSPAC cohort. Psychological Medicine, 50(10), 1755–1760. doi: 10.1017/S0033291719001971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampel, P., & Petermann, F. (2005). Age and gender effects on coping in children and adolescents. Journal of Youth and Adolescence, 34(2), 73–83. doi: 10.1007/s10964-005-3207-9 [DOI] [Google Scholar]
- Hetzel-Riggin, M. D., & Roby, R. P. (2013). Trauma type and gender effects on PTSD, general distress, and peritraumatic dissociation. Journal of Loss & Trauma, 18(1), 41–53. doi: 10.1080/15325024.2012.679119 [DOI] [Google Scholar]
- Holder, M. K., & Blaustein, J. D. (2014). Puberty and adolescence as a time of vulnerability to stressors that alter neurobehavioral processes. Frontiers in Neuroendocrinology, 35(1), 89–110. doi: 10.1016/j.yfrne.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kilpatrick, D. G., Resnick, H. S., Milanak, M. E., Miller, M. W., Keyes, K. M., & Friedman, M. J. (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26(5), 537–547. doi: 10.1002/jts.21848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, S. H., & Graham, B. M. (2017). Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry, 4(1), 73–82. doi: 10.1016/S2215-0366(16)30358-3 [DOI] [PubMed] [Google Scholar]
- Luthra, R., Abramovitz, R., Greenberg, R., Schoor, A., Newcorn, J., Schmeidler, J., … Chemtob, C. M. (2009). Relationship between type of trauma exposure and posttraumatic stress disorder among urban children and adolescents. Journal of Interpersonal Violence, 24(11), 1919–1927. doi: 10.1177/0886260508325494 [DOI] [PubMed] [Google Scholar]
- McLaughlin, K. A., Koenen, K. C., Hill, E. D., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2013). Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 52(8), 815–830.e14. doi: 10.1016/j.jaac.2013.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas, K. R., He, J. P., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., … Swendsen, J. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49(10), 980–989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nöthling, J., Simmons, C., Suliman, S., & Seedat, S. (2017). Trauma type as a conditional risk factor for posttraumatic stress disorder in a referred clinic sample of adolescents. Comprehensive Psychiatry, 76, 138–146. doi: 10.1016/j.comppsych.2017.05.001 [DOI] [PubMed] [Google Scholar]
- Olff, M., Langeland, W., Draijer, N., & Gersons, B. P. (2007). Gender differences in posttraumatic stress disorder. Psychological Bulletin, 133(2), 183–204. doi: 10.1037/0033-2909.133.2.183 [DOI] [PubMed] [Google Scholar]
- Rasmussen, A., Romero, S., Leon, M., Verkuilen, J., Morales, P., Martinez-Maganalles, S., & García-Sosa, I. (2020). Measuring trauma exposure: Count versus variety of potentially traumatic events in a binational sample. Journal of Traumatic Stress, 33(6), 973–983. doi: 10.1002/jts.22563 [DOI] [PubMed] [Google Scholar]
- Seedat, S., Nyamai, C., Njenga, F., Vythilingum, B., & Stein, D. J. (2004). Trauma exposure and post-traumatic stress symptoms in urban African schools. Survey in CapeTown and Nairobi. The British Journal of Psychiatry, 184, 169–175. doi: 10.1192/bjp.184.2.169 [DOI] [PubMed] [Google Scholar]
- Suliman, S., Kaminer, D., Seedat, S., & Stein, D. J. (2005). Assessing post-traumatic stress disorder in South African adolescents: Using the child and adolescent trauma survey (CATS) as a screening tool. Annals of General Psychiatry, 4(1), 2. doi: 10.1186/1744-859X-4-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin, D. F., & Foa, E. B. (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132(6), 959–992. doi: 10.1037/0033-2909.132.6.959 [DOI] [PubMed] [Google Scholar]
- Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., & Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32(2), 122–138. doi: 10.1016/j.cpr.2011.12.001 [DOI] [PubMed] [Google Scholar]
- Wade, T. J., Cairney, J., & Pevalin, D. J. (2002). Emergence of gender differences in depression during adolescence: National panel results from three countries. Journal of the American Academy of Child and Adolescent Psychiatry, 41(2), 190–198. doi: 10.1097/00004583-200202000-00013 [DOI] [PubMed] [Google Scholar]
- Ward, C. L., Artz, L., Leoschut, L., Kassanjee, R., & Burton, P. (2018). Sexual violence against children in South Africa: A nationally representative cross-sectional study of prevalence and correlates. The Lancet Global Health, 6(4), e460–e468. doi: 10.1016/S2214-109X(18)30060-3 [DOI] [PubMed] [Google Scholar]
- Zimmerman, A., Halligan, S., Skeen, S., Morgan, B., Fraser, A., Fearon, P., & Tomlinson, M. (2020). PTSD symptoms and cortisol stress reactivity in adolescence: Findings from a high adversity cohort in South Africa. Psychoneuroendocrinology, 121, 104846. doi: 10.1016/j.psyneuen.2020.104846 [DOI] [PubMed] [Google Scholar]
- Zou, G. (2004). A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology, 159(7), 702–706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author [LVH]. The data are not publicly available due to [restrictions, e.g., their containing information that could compromise the privacy of research participants].


