Graphical abstract

Keywords: Coronary sinus defect, Unroofed coronary sinus, Dilated right atrium, Dilated right ventricle
Highlights
-
•
Isolated coronary sinus defect without persistent left superior vena cava is a rare cardiac defect.
-
•
Diagnosis can be difficult in the absence of other defects in an asymptomatic child.
-
•
Missed or difficult cases to diagnose may be found incidentally in adulthood.
-
•
Surgical outcome in the absence of any other defects can be very good.
Introduction
Coronary sinus septal defect (CSSD) or unroofed coronary sinus (CS) is an uncommon heart defect that results from partial or complete unroofing of the tissue separating the CS from the left atrium, allowing the right and left atria to communicate through the defect and the CS orifice. It results from an abnormality in the development of the left atrioventricular fold.1 Coronary sinus septal defect is a very rare congenital heart defect, comprising <1% of atrial septal defects (ASDs) and only 0.1% of all congenital heart defects.2 Coronary sinus septal defect can be further classified into four subtypes: type I, completely unroofed with persistent left superior vena cava (PLSVC); type II, completely unroofed without PLSVC; type III, partially unroofed midportion; type IV, partially unroofed terminal portion.2, 3, 4 Coronary sinus septal defect is almost always associated with a PLSVC, and very few cases of isolated CSSD without left superior vena cava (SVC) have been reported in the literature.5 Most of these cases are sometimes missed or difficult to diagnose and may be found incidentally in adulthood.6 We report a case of CSSD in an asymptomatic 11-year-old whose diagnosis was initially challenging but was ultimately accomplished and who had a successful surgical repair.
Case Presentation
The patient is an 11-year-old male with a history of mild intermittent asthma and attention deficit hyperactivity disorder (ADHD) who was initially seen for the first time at 7 years of age for cardiac evaluation due to an abnormal electrocardiogram and echocardiogram. He had been newly diagnosed with ADHD, and prior to the initiation of medical treatment, the primary care provider ordered an electrocardiogram, which was abnormal.
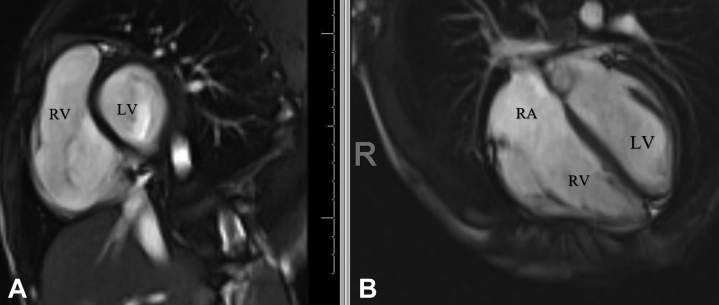
The patient was otherwise asymptomatic from the cardiac standpoint, had been growing well, and had no significant family cardiac history. His cardiac examination was otherwise unremarkable, and his electrocardiogram showed sinus rhythm with normal intervals and QRS axis, right ventricular conduction delay, and no ventricular hypertrophy. His echocardiogram during the initial office visit showed right atrial and right ventricular enlargement with concerns for an atrial-level shunt, possibly an inferior sinus venosus defect versus an inferior secundum ASD. The pulmonary venous drainage was normal. Agitated saline contrast study did not show any evidence of intracardiac shunt. Cardiac magnetic resonance imaging (MRI) was performed for further evaluation of the possible causes of the right heart dilation. The main findings included dilated right ventricle with mildly increased trabeculations (right ventricular normalized end-diastolic volume = 120 mL/m2), mildly depressed right ventricular function (right ventricular ejection fraction = 43%), and right atrial enlargement. There was no myocardial delayed enhancement of the right ventricle to suggest fibrofatty infiltration, right ventricular, or right ventricular outflow tract aneurysms. Left ventricular size and systolic function were normal, as was the pulmonary venous drainage. There was no left SVC. Even though the Qp:Qs was ~2.0 when calculated from both aortic and pulmonary artery flows and the right and left ventricular stroke volumes, no intracardiac shunts could be clearly identified at the time.
The plan was to continue following up while evaluating for other possible etiologies of the right heart enlargement, but the patient was lost to follow-up for some time. The next time he was seen in clinic for follow-up he was 11 years old, and he continued to be reportedly asymptomatic from the cardiac standpoint and was growing well. His cardiac examination at this point was unremarkable except for a new finding of II/VI systolic ejection murmur, which was best heard at the left upper sternal border.
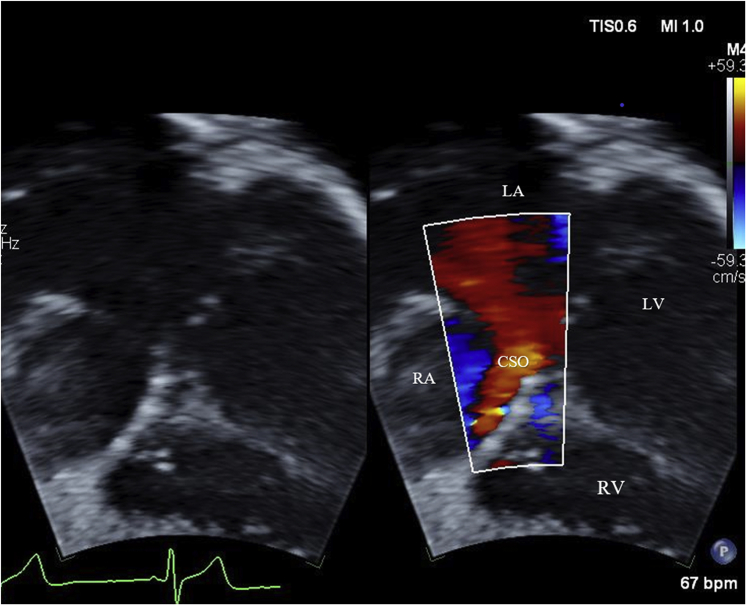
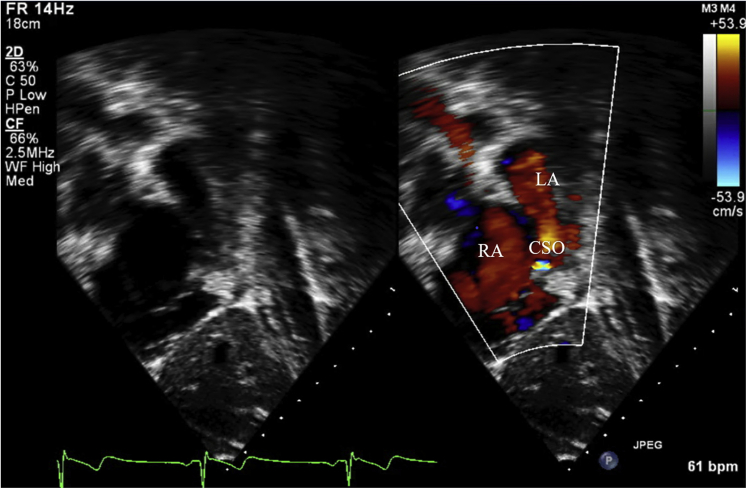
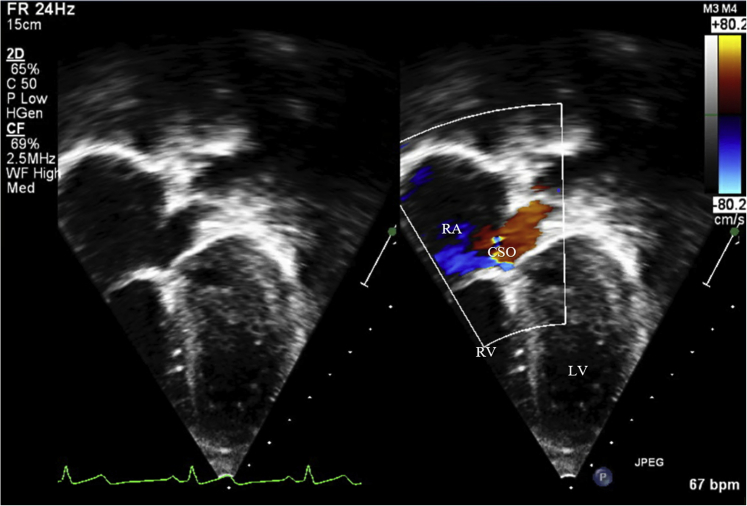
There was no significant change on his follow-up electrocardiogram, and the echocardiogram continued to show right heart dilation (Videos 1 and 2). Upon further review of the echocardiographic images, CS defect was highly suspected (Figure 1, Figure 2, Figure 3, Videos 3-6). The cardiac MRI images (Figures 4 and 5) were reviewed again in light of the follow-up echocardiogram images, and the diagnosis of CSSD was even further highly suspected.
Figure 1.
Subxiphoid long-axis view on transthoracic echocardiogram. CSO, CS ostium; LV, Left ventricle; RV, right ventricle.
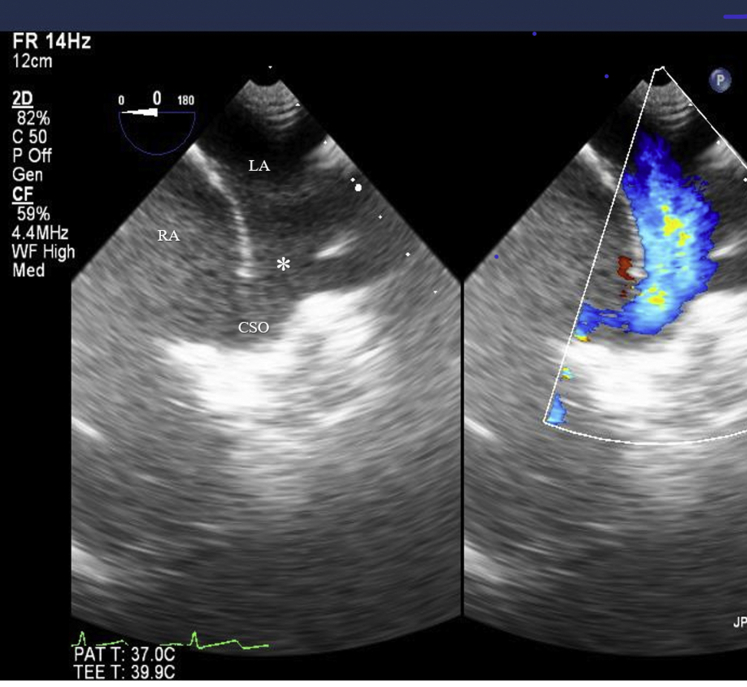
Figure 2.
Subxiphoid short-axis view on transthoracic echocardiogram. CSO, CS ostium; LA, left atrium; RA, right atrium.
Figure 3.
Apical four-chamber view (sweeping more posteriorly) on a transthoracic echocardiogram showing the dilated distal segment of the coronary sinus and ostium (CSO). LV, Left ventricle; RA, right atrium; RV, right ventricle.
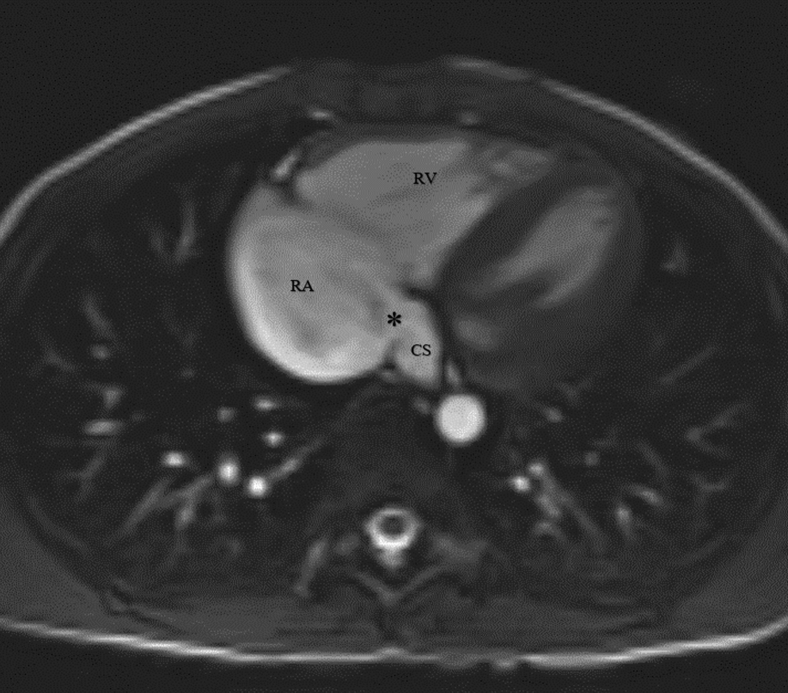
Figure 4.
(A) Cardiac MRI image showing right ventricular dilation in short axis. (B) Cardiac image showing right atrial (RA) and right ventricular (RV) enlargement in four-chamber view. LV, Left ventricle.
Figure 5.
Cardiac MRI image showing the coronary sinus (CS) and the dilated coronary sinus orifice (asterisk). RA, right atrium; RV, right ventricle.
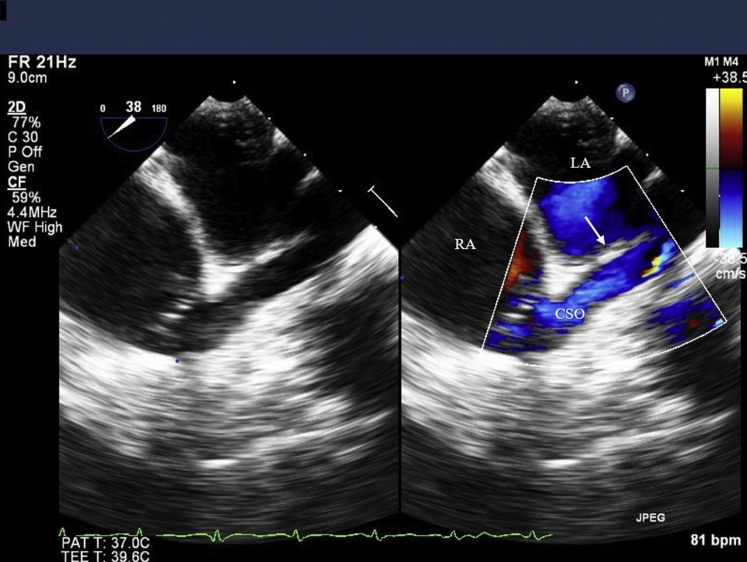
Surgical repair was performed, and the preoperative transesophageal echocardiogram (TEE) (Figure 6, Video 7) clearly showed CSSD with partial unroofing of the CS (just proximal to the ostium); the defect measured 16 mm with left-to-right shunting. The ostium of the CS was dilated, measuring 11 mm. There was right atrial and right ventricular dilation. The remainder of the atrial septum was intact. The finding was confirmed by direct inspection intraoperatively, and the defect was closed with a pericardial patch (Figure 7, Video 8). The postoperative course was uneventful, and the patient has been doing well on subsequent follow-up appointments with no concerns.
Figure 6.
Zoomed mid esophageal four-chamber view on a transesophageal echocardiogram showing the coronary sinus defect (asterisk) and the dilated coronary sinus ostium (CSO). LA, Left atrium; RA, right atrium.
Figure 7.
Zoomed mid esophageal four-chamber view on a transesophageal echocardiogram showing post-surgical repair of the coronary sinus defect with a pericardial patch. The arrow shows the location where the coronary sinus defect used to be. LA, left atrium; RA, right atrium.
Discussion
Coronary sinus septal defect is an uncommon cardiac defect that results from partial or complete unroofing of the tissue separating the CS from the left atrium, allowing the right and left atria to communicate through the defect and the CS orifice.2 The interatrial communication, however, is through the orifice of the CS, which is located below and posterior to the fossa ovale. Patients with partial or complete unroofing of the CS without a PLSVC exhibit signs and symptoms identical to those with a secundum ASD. They are therefore asymptomatic and may remain undiagnosed until later in life. They may come to medical attention due to abnormal auscultatory findings or diagnostic studies such as electrocardiogram, chest radiograph, echocardiogram, computed tomography scan, or MRI.6
In this patient, even though the initial imaging studies revealed right heart dilation, higher right ventricular stroke volume matching pulmonary artery flow, and Qp:Qs of ~2, suggesting likely atrial-level shunt, no shunt was able to be identified even after the agitated contrast study. An agitated saline contrast study can be negative for a right-to-left shunt in patients such as this case due to various factors including inadequate injection, inadequate provocative maneuvers such as Valsalva and coughing, and inability to increase right atrial pressure to greater than left atrial pressure. In this particular case, the injection and the technique were felt to be adequate, but it is possible the measures that were taken were inadequate to increase the right atrial pressure to greater than the left atrial pressure. The anatomy or the location and size of the shunt may also contribute to the false-negative results in contrast echocardiography in such cases, especially in the absence of persistent left SVC draining into the CS.
Magnetic resonance imaging is an excellent noninvasive imaging technique for evaluating etiologies for right heart dilation because of its ability to visualize cardiac and extracardiac anatomy; to obtain data on ventricular volumetrics, valvar function, flow quantification, and derivation of Qp:Qs; and to obtain multiplanar imaging, wide field of view, good spatiotemporal resolution, and high inherent contrast resolution.7 However, there may be limitations in visualizing thin structures and defects due to suboptimal spatial resolution, particularly if the structure or defect was positioned in between acquired slices or the thicker slices obtained in cine-imaging. An atrial-level shunt such as this case may be missed visually, even though Qp:Qs is suggestive of a shunt, due to various factors including the anatomy, size, and location of the defect. Transesophageal echocardiogram can more accurately be used to delineate these posterior cardiac structures, and it yields an accurate and comprehensive view of the CS and surrounding structures8,9 as demonstrated in the intraoperative images in this case. The superior resolution of TEE played a key role in this case.
With the pulmonary venous drainage being normal and ruling out valvar and myocardial causes of the isolated right heart dilation, some form of shunt was still suspected. Some of the differentials that were also considered included extracardiac shunts (pulmonary/systemic arteriovenous connections) or coronary artery fistula to the CS or right atrium.10
The orifice of the CS in CSSD can be large due to the left-to-right shunt (Figures 1 and 3), resulting in a sizeable defect in the inferior aspect of the atrial septum near the entry of the inferior vena cava. This could explain why inferior sinus venosus defect or inferior secundum ASD was suspected after the initial echocardiogram. The dilated orifice of the CS with the associated increased shunting into the right atrium was the clue in the subsequent follow-up echocardiogram that ultimately led to thorough review of that area in the various studies leading to the diagnosis.
Coronary sinus septal defect is rare, and when it occurs in isolation, the diagnosis can sometimes be difficult.2 Even though it may be diagnosed by transthoracic echocardiogram and/or TEE with color Doppler, cardiac catheterization, multidetector cardiac computed tomography, or cardiac MRI,5 a higher index of suspicion is needed to pursue other imaging modalities after the initial transthoracic echocardiogram. The physiology of this defect is similar to that of secundum ASD with right heart dilation, and the other associated long-term complications and other consequences such as brain abscess or cerebral emboli may result from a right-to-left shunt.1,11,12 Even though there has been a rare case of spontaneous closure of CSSD that was in association with other congenital heart defects,13 early diagnosis of this lesion is important to the prognosis of the patient. Unfortunately, the diagnosis is often difficult because of nonspecific clinical features.
Conclusion
An isolated CSSD is a very rare congenital heart defect, and it can easily be missed especially in younger patients. It therefore needs to be included in the differentials when evaluating for possible atrial-level shunts.
Acknowledgment
The research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under award no. P20GM121334.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest: None.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2021.07.005.
Supplementary Data
Apical four-chamber view on transthoracic echocardiogram showing the right atrial and ventricular dilation.
Parasternal short-axis view on the transthoracic echocardiogram showing right ventricular dilation.
Subxiphoid long-axis view on transthoracic echocardiogram showing dilated CS ostium.
Subxiphoid short-axis view on transthoracic echocardiogram showing coronary dilated sinus ostium.
Apical four-chamber view on transthoracic echocardiogram, more posteriorly and showing the dilated distal segment of the CS and the ostium.
Apical four-chamber view on transthoracic echocardiogram, more posteriorly and showing the dilated distal segment of the CS and the ostium and the dilated right atrium and right ventricle.
Midesophageal four-chamber view on TEE showing the CS defect.
Midesophageal four-chamber view on TEE postsurgical repair of the CS defect.
References
- 1.Rose A.G., Beckman C.B., Edwards J.E. Communication between coronary sinus and left atrium. Br Heart J. 1974;36:182–185. doi: 10.1136/hrt.36.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joffe D.C., Rivo L., Oxorn D.C. Coronary sinus atrial septal defect. Anesth Analg. 2008;107:1163–1165. doi: 10.1213/ane.0b013e3181806974. [DOI] [PubMed] [Google Scholar]
- 3.Ootaki Y., Yamaguch M., Yoshimura N., Oka S., Yoshida M., Hasegawa T. Unroofed coronary sinus syndrome: diagnosis, classification, and surgical treatment. J Thorac Cardiovasc Surg. 2003;126:1655–1656. doi: 10.1016/s0022-5223(03)01019-5. [DOI] [PubMed] [Google Scholar]
- 4.Kirklin J.W., Barratt-Boyes B.G., Desley J.W. Wiley; New York: 1986. Cardiac Surgery: Morphology, Diagnostic Criteria, Natural History, Techniques, Results, and Indications. [Google Scholar]
- 5.Gajjar T.P., Rao J.N., Desai N.B. Echocardiographic diagnosis and surgical closure of coronary sinus type of atrial septal defect. J Card Surg. 2011;26:653–656. doi: 10.1111/j.1540-8191.2011.01340.x. [DOI] [PubMed] [Google Scholar]
- 6.Chaturvedi A., Dubinsky T.J., Maki J.H. MR findings of a rare defect, coronary sinus ASD. Int J Cardiovasc Imaging. 2012;28:429–430. doi: 10.1007/s10554-010-9670-8. [DOI] [PubMed] [Google Scholar]
- 7.Rajiah P., Kanne J.P., Cardiac M.R.I. Part 1. Cardiovascular shunts. AJR Am J Roentgenol. 2011;197:W603–W620. doi: 10.2214/AJR.10.7257. [DOI] [PubMed] [Google Scholar]
- 8.Sun T., Fei H.W., Huang H.L., Chen O.D., Zhen Z.C., Zhang C.J. Transesophageal echocardiography for coronary sinus imaging in partially unroofed coronary sinus. Echocardiography. 2014;31:74–82. doi: 10.1111/echo.12302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silvestry F.E., Cohen M.S., Armsby L.B., Burkule N.J., Fleishman C.E., Hijazi Z.M. Guidelines for the echocardiographic assessment of atrial septal defect and patent foramen ovale: from the American Society of Echocardiography and Society for Cardiac Angiography and Interventions. J Am Soc Echocardiogr. 2015;28:910–958. doi: 10.1016/j.echo.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Beitzke D., Wolf F., Edelhauser G., Lammer J., Loewe C. Right heart dilatation in adult congenital heart disease: imaging appearance on cardiac magnetic resonance. Br J Radiol. 2011;84:188–193. doi: 10.1259/bjr/13711325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quaegebeur J., Kirklin J.W., Pacifico A.D., Bargeron L.M.J. Surgical experience with unroofed coronary sinus. Ann Thorac Surg. 1979;27:418–425. doi: 10.1016/s0003-4975(10)63339-5. [DOI] [PubMed] [Google Scholar]
- 12.Babapoor-Farrokhran S., Kalla A., Bozorgnia B., Amanullah A. Wide unroofed coronary sinus and cryptogenic stroke: a case report. Eur Heart J Case Rep. 2020;4:1–6. doi: 10.1093/ehjcr/ytaa421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watanabe M., Ono S., Okada Y., Inoue Y., Kobayashi T., Suzuki T. Spontaneous closure of an unroofed coronary sinus. Pediatr Int. 2004;46:722–725. doi: 10.1111/j.1442-200x.2004.01990.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Apical four-chamber view on transthoracic echocardiogram showing the right atrial and ventricular dilation.
Parasternal short-axis view on the transthoracic echocardiogram showing right ventricular dilation.
Subxiphoid long-axis view on transthoracic echocardiogram showing dilated CS ostium.
Subxiphoid short-axis view on transthoracic echocardiogram showing coronary dilated sinus ostium.
Apical four-chamber view on transthoracic echocardiogram, more posteriorly and showing the dilated distal segment of the CS and the ostium.
Apical four-chamber view on transthoracic echocardiogram, more posteriorly and showing the dilated distal segment of the CS and the ostium and the dilated right atrium and right ventricle.
Midesophageal four-chamber view on TEE showing the CS defect.
Midesophageal four-chamber view on TEE postsurgical repair of the CS defect.