Statins have been demonstrated to reduce major adverse cardiovascular events, including mortality. About half of patients meeting guideline-based indications for statin therapy have not been prescribed the medication.1 Recently, the coronavirus disease 2019 (COVID-19) pandemic brought about structural changes in care delivery, including rapid adoption of telemedicine for primary and hyperlipidemia care.2 Quality of care delivered via telemedicine visits during the COVID-19 pandemic has not been well-evaluated. In this study, our objective was to evaluate statin prescribing rates for eligible patients before and during the COVID-19 pandemic while care was being delivered through in-person and telemedical channels.
We conducted a retrospective evaluation of statin prescribing rates by primary care physicians (PCPs) at 28 Penn Medicine practice sites in Pennsylvania and New Jersey from October 2019 to September 2020 for patients eligible but not already prescribed a statin. The data that support the findings of this study are available from the corresponding author upon reasonable request. Eligibility criteria developed by our health system were defined as: 1) clinical ASCVD (atherosclerotic cardiovascular disease) diagnosis; 2) history of familial hyperlipidemia; or 3) meeting United States Preventive Services Task Force (USPSTF) guidelines for statin therapy which includes age 40–75 years, at least 1 cardiovascular risk factor (e.g., dyslipidemia, diabetes, hypertension, smoking), and 10-year ASVCD risk score ≥ 10%. Patients were excluded if they: 1) were already prescribed a statin; 2) were allergic to statins; 3) had a glomerular filtration rate less than 30 mL/min or were on dialysis; 4) had a prior adverse reaction to statins (including significant liver dysfunction, rhabdomyolysis or other intolerance to statin); 5) were pregnant; 6) were breastfeeding; 7) were on hospice or at the end-of-life; or 8) were on a Proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor medication. Monthly changes in the rate of new statin prescribing were evaluated throughout the study period. Multivariate models considering monthly interactions were fit using generalized estimating equations clustered by PCPs alone and adjusted for age, sex, race/ethnicity, median household income, and statin-intensity indication (moderate or high).3 This study was approved by the University of Pennsylvania Institutional Review Board. Analyses were conducted by using R version 4.0.2 (R Foundation for Statistical Computing).
The sample comprised 158 PCPs and 20,374 patient encounters with mean (SD) patient age of 65.8 (11.0) years; 49.4 % were male. Clinical ASCVD diagnosis, history of familial hyperlipidemia, and 10-year ASCVD risk score ≥10% were observed in 5442 (26.7%), 104 (0.5%), and 14930 (73.3%) encounters, respectively. In-person visit volumes declined during the start of the COVID-19 pandemic while telemedicine visit volumes increased. Telemedicine visits peaked in April 2020 and accounted for 21.9% (N=4467) of the visits during the study period. Among in-person visits, the overall new statin prescribing rate was 3.1%, decreasing from March but recovering to the previous level around August (Figure). The overall statin prescribing rate for telemedicine visits was 3.2%. In adjusted models, statin prescribing rates were significantly higher during telemedicine visits than in-person visits during April 2020 (odds ratio, 2.10; 95% CI, [1.01–4.37]; p-value = 0.047) and May 2020 (odds ratio, 2.32; 95% CI[1.02–5.29]; p-value=0.044). There was no significant difference in prescribing rates between telemedicine and in-person visits during the rest of the study period.
Figure. Prescription rate among eligible patients.
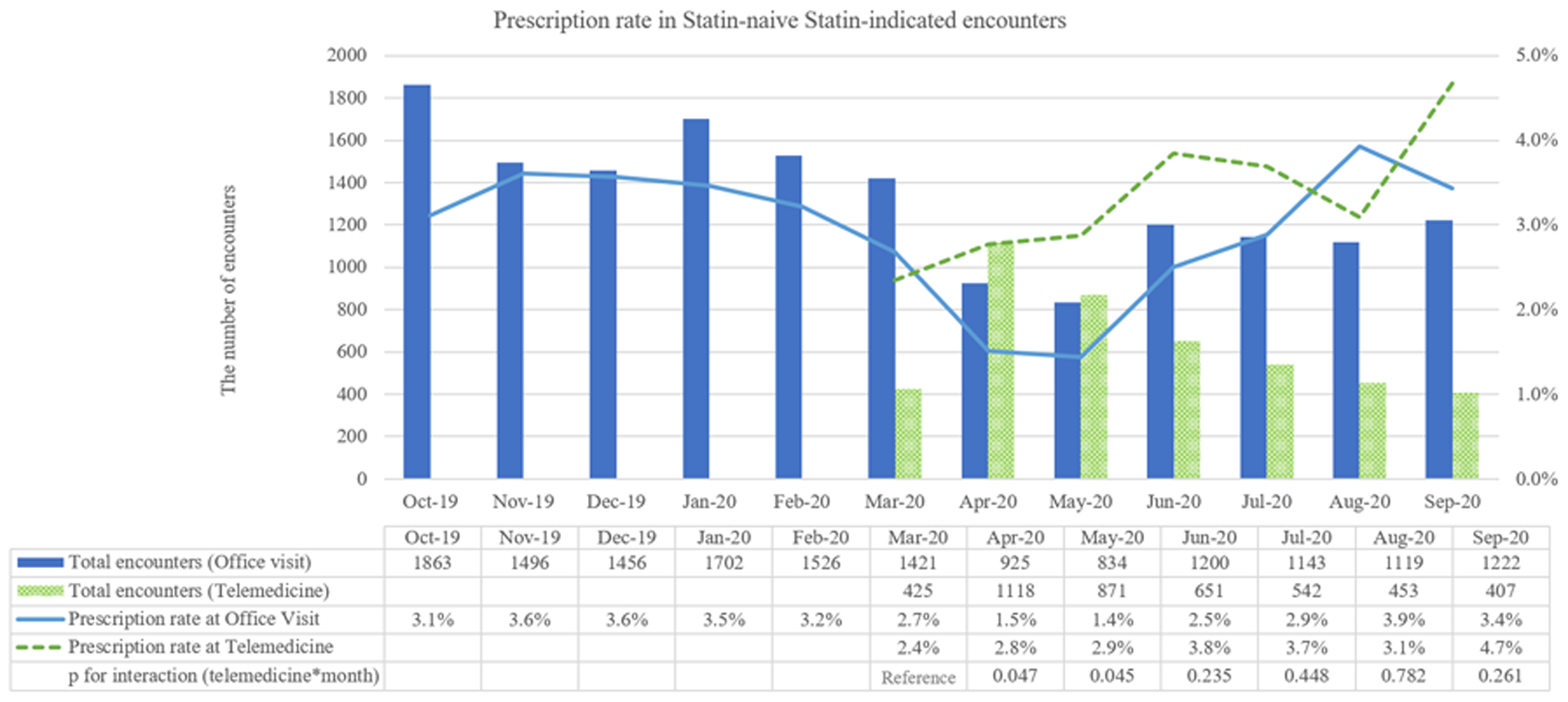
Solid blue bars represent total number of office visits, while dotted green bars represent total number of telemedicine visits. Solid blue line represents statin prescription rate during office visits, while dotted green line represents statin prescription rate during telemedicine visits.
In this study, we found that overall statin prescribing rates were low, presenting an opportunity to improve the delivery of care. Decreased rates of in-person visits during the COVID-19 pandemic were offset by an increased rate of telemedicine visits. During the early pandemic period (April 2020 to May 2020), statin prescription rates were the same or higher during telemedicine visits as compared to in-person visits. This may indicate hyperlipidemia management is an effective use case for telemedical care delivery, particularly as the management of this condition does not always require a physical examination.4 Clinicians may also have had more time during telemedicine visits to address chronic conditions like hyperlipidemia as compared to in-person visits. This study has several limitations, including its observational design in a single academic health system and selection bias due to its retrospective nature. As the volume of telemedicine visits decreased in later months, we may have had less power to test for differences in prescribing rates relative to in-person visits. Additionally, among several available guidelines for management of hyperlipidemia, our health system adopted USPSTF guidelines in clinical practice, which could result in limited generalizability. Finally, the overall statin prescribing rate during this study may have been lower due to patient difficulty in obtaining cholesterol testing during the COVID-19 pandemic, which we were not able to directly assess.5 Future studies are needed to examine quality of care as clinicians and patients gain more experience with telemedicine.
Acknowledgments:
Dr. Mizuno had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding Support:
This project was funded by National Institute on Aging (R33AG057380) and the University of Pennsylvania Health System through the Penn Medicine Nudge Unit. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Non-standard Abbreviations and Acronyms
- COVID-19
coronavirus disease 2019
- PCPs
primary care physicians
- ASCVD
atherosclerotic cardiovascular disease
- USPSTF
United States Preventive Services Task Force
- PCSK9
Proprotein convertase subtilisin/kexin type 9
Footnotes
Conflict of Interest Disclosures: Dr. Patel is founder of Catalyst Health, a technology and behavior change consulting firm and is on the medical advisory board for Healthmine Services, Life.io, and Holistic Industries. The remaining authors have nothing to disclose.
References
- 1.Salami JA, Warraich H, Valero-Elizondo J, Spatz ES, Desai NR, Rana JS, Virani SS, Blankstein R, Khera A, Blaha MJ, Blumenthal RS, Lloyd-Jones D and Nasir K. National Trends in Statin Use and Expenditures in the US Adult Population From 2002 to 2013: Insights From the Medical Expenditure Panel Survey. JAMA Cardiol. 2017;2:56–65. [DOI] [PubMed] [Google Scholar]
- 2.Nouri S, Khoong EC, Lyles CR and Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catalyst Innovations in Care Delivery. 2020;1 (3). URL: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123. Last access date; 2021-08-02. [Google Scholar]
- 3.Eberly LA, Khatana SAM, Nathan AS, Snider C, Julien HM, Deleener ME and Adusumalli S. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic. Circulation. 2020;142:510–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomez T, Anaya YB, Shih KJ and Tarn DM. A Qualitative Study of Primary Care Physicians’ Experiences With Telemedicine During COVID-19. J Am Board Fam Med. 2021;34:S61–s70. [DOI] [PubMed] [Google Scholar]
- 5.Gumuser ED, Haidermota S, Finneran P, Natarajan P and Honigberg MC. Trends in cholesterol testing during the COVID-19 pandemic: COVID-19 and cholesterol testing. Am J Prev Cardiol. 2021;6:100152. [DOI] [PMC free article] [PubMed] [Google Scholar]


