Abstract
Background
An unprecedented shift to remote heart failure outpatient care occurred during the Covid-19 pandemic. Given challenges inherent to remote care, we studied whether remote visits (video or telephone) were associated with different patient usage, clinician practice patterns, and outcomes.
Methods
We included all ambulatory cardiology visits for heart failure at a multi-site health system from 4/1/2019–12/31/2019 (pre-Covid) or 4/1/2020–12/31/2020 (Covid era), resulting in 10,591 pre-Covid in-person, 7,775 Covid-era in-person, 1,009 Covid-era video, and 2,322 Covid-era telephone visits. We used multivariable logistic and Cox proportional hazards regressions with propensity weighting and patient clustering to study ordering practices and outcomes.
Results
Compared to in-person visits, video visits were used more often by younger (mean 64.7 years (SD 14.5) vs. 74.2 (14.1), male (68.3% vs. 61.4%), and privately insured (45.9% vs. 28.9%) individuals (p<0.05 for all). Remote visits were more frequently used by non-White patients (35.8% video, 37.0% telephone vs. 33.2% in-person). During remote visits, clinicians were less likely to order diagnostic testing (OR 0.20 (0.18–0.22) video vs. in-person, 0.18 (0.17–0.19) telephone vs. in-person) or prescribe beta-blockers (0.82 (0.68–0.99), 0.35 (0.26–0.47)), MRAs (0.69 (0.50–0.96), 0.48 (0.35–0.66)), or loop diuretics (0.67 (0.53–0.85), 0.45 (0.37–0.55)). During telephone visits, clinicians were less likely to prescribe ACE/ARB/ARNIs (0.54 (0.40–0.72)). Telephone visits but not video visits were associated with higher rates of 90-day mortality (1.82 (1.14–2.90)) and non-significant trends towards higher rates of 90-day heart failure ED visits (1.34 (0.97–1.86)) and hospitalizations (1.36 (0.98–1.89)).
Conclusions
Remote visits for heart failure care were associated with reduced diagnostic testing and GDMT prescription. Telephone but not video visits were associated with increased 90-day mortality.
Keywords: telemedicine, virtual visit, video visit, remote care, heart failure, guideline directed medical therapy
Background
The Covid-19 pandemic resulted in an unprecedented large-scale shift from in-person to remote visits for outpatient medical care. In the US, policy changes, including formalized reimbursement as well as the relaxing of licensing, HIPAA, and prescription regulations, have further encouraged this transition.1 Remarkably, the number of Medicare beneficiaries using telemedicine services grew from 13,000 individuals a week prior to the Covid-19 pandemic to nearly 1.7 million individuals a week since the last week of April 2020.2
Remote outpatient visits are especially important for heart failure patients as such patients are at particularly high risk for adverse outcomes from Covid-19.3–5 However, while limiting in-person visits may mitigate infectious risks, heart failure patients may also be particularly vulnerable to the shortcomings of remote visits. Remote care can pose unique challenges including barriers in accessing and/or using required technology, decreased clarity of communication, and an inability to perform comprehensive physical examinations.6 Heart failure patients have high rates of hospital admission and many require intensive outpatient care and monitoring to manage volume status, titrate guideline-directed medical therapies (GDMT), and decide when more advanced therapies such as mechanical circulatory support or heart transplant may be warranted. As such, impediments to ordering tests or medications as well as to monitoring patients for decompensations may significantly impact the quality of care and outcomes in this population.
However, few studies have reported the effects of remote visits on heart failure care practice patterns and outcomes.7,8 We hypothesized that because of challenges of remote care, including difficulties with assessing volume status, electrolytes, and renal function, clinicians might prescribe fewer GDMT medications and diuretics and decrease ordering of diagnostic and laboratory tests. We additionally hypothesized that these differences in care patterns might result in increases in emergency department visits, hospitalizations, and mortality. To test these hypotheses, we examined the ordering frequencies of diagnostic tests and GDMT as well as rates of 90-day emergency department visits, hospital admission, and mortality for all remote and in-person ambulatory cardiology visits for heart failure at our multi-site health system in the Covid-era period (4/1/2020–12/31/2020). We then compared these visits to those from the same period one year before, during the pre-Covid period (4/1/2019–12/31/2019).
Methods
The data for this study is available from the corresponding author upon reasonable request.
We identified all ambulatory cardiology visits with an encounter diagnosis of heart failure at our large multi-site urban health system conducted during the periods of 4/1/2019–12/31/2019 or 4/1/2020–12/31/2020. This included both in-person visits and remote visits conducted by 147 different clinicians across 31 affiliated cardiology groups. As this analysis was conducted on the visit level, a patient could have multiple visits during the study period. Remote visits consisted of either telephone or video appointment. Clinicians selected the video platform utilized for video visits; platforms included an electronic health record (EHR) based platform (Epic Systems) or third party vendor (Doximity, Zoom, or WebEx). The 4/1/2020–12/31/2020 period was chosen as remote visits were most frequent during this visit. The comparator cohort from 4/1/2019–12/31/2019 was used to minimize seasonal fluctuations in patient composition and ordering practices. We used visit-level encounter information available from the EHR to determine visit type (in-person vs. video vs. telephone), patient demographics, visit date, number of visits per patient during the study period, scheduled visit duration, encounter diagnoses, and all diagnostic and medication orders associated with each visit. We further investigated the ordering frequencies of the most common cardiology-specific diagnostic tests including electrocardiograms (ECGs), transthoracic echocardiograms, coronary computed tomography angiography, nuclear stress imaging, stress echocardiogram, exercise stress ECG, coronary artery calcium scan, cardiac magnetic resonance imaging, and external ECG monitoring tests (such as Zio patch monitors). Laboratory tests of interest included brain natriuretic peptide, lipid panel, complete blood count, metabolic panel, coagulation studies, erythrocyte sedimentation rate, and C-reactive protein tests. We linked patient records with echocardiogram data to determine heart failure characteristics including whether a patient’s heart failure was heart failure with reduced ejection fraction (HFrEF, defined as having had an LVEF ≤ 50% anytime in the past), LVEF, left ventricular end diastolic diameter, right ventricular systolic function, and right ventricular end diastolic diameter. Using EHR data from all hospitalizations in our system across all prior dates, we determined the total number of previous heart failure-related hospitalizations for each patient.
To assess ordering patterns for heart failure medications and GDMT, we looked at a sub-cohort of visits involving patients with a measured left ventricular ejection fraction ≤ 35%, determined by echocardiogram data. We defined GDMT according to the most recent ACC/AHA heart failure management guidelines.9,10 We examined prescription rates of beta-blockers (metoprolol, carvedilol, bisoprolol), ACE-inhibitors (ACEi), angiotensin receptor blockers (ARB), angiotensin receptor-neprilysin inhibitors (ARNI), mineralocorticoid receptor antagonists (MRA), hydralazine (in Black patients only), nitrates (isosorbide dinitrate or isosorbide mononitrate, in Black patients only), digoxin, and loop diuretics (furosemide, bumetanide, torsemide, and ethacrynic acid).
ED visits, hospitalizations, and deaths were derived from EHR data. We included all ED visits and hospitalizations that had an encounter diagnosis of heart failure and further limited it only to the most recent visits/admissions within 90 days of a cardiology clinic visit for heart failure. We excluded ED visits, hospitalizations, and deaths that were due to Covid-19 infection. Notably, hospitalization numbers were higher than ED visit numbers, because of a substantial number of patients who were directly admitted to the hospital without being seen in the ED.
The study protocol was approved by the Cedars-Sinai Medical Center Institutional Review Board.
Statistical Analysis
Visits were stratified by time period (pre-Covid vs. Covid-era) and visit type (in-person vs. video vs. telephone). For each visit type, patient and visit characteristics were expressed as frequency counts and percentages. We compared rates of medication and diagnostic test ordering by visit type. The differences in discrete variables between groups were evaluated by the chi-square test. Differences in continuous variables were evaluated using the t-test.
We used multivariable logistic regression to study the association between visit type and the odds of ordering diagnostic tests and heart failure medications as well as between visit type and odds of ICU admission. We used multivariable linear regression to study the association between visit type and hospital length of stay among those patients who were hospitalized within 90 days of their clinic visit. We used Cox proportional hazards models to study hazard rates of heart failure related ED visits and hospital admissions as well as mortality according to visit type. For all multivariable analyses we employed “doubly robust” estimation of causal effects, adjusting for both patient and visit covariates as well as propensity score weighting according to the propensity for being seen by remote visit.11,12 Covariates included age, sex, race, insurance status, visit length, calendar date, and specific visit diagnoses (coronary artery disease, hypertension, atrial fibrillation/flutter, diabetes mellitus, valvular disease, and chronic kidney disease). Since a patient could contribute multiple visits, we additionally clustered all analyses by patient to adjust for correlation across visits for the same patient. Lastly, we visualized incidence of ED visits, hospital admissions, and deaths binned into two month periods, displaying mean event rate and standard error estimates.
Sensitivity analyses
We conducted four sensitivity analyses to assess the robustness of our results to possible confounding. First, we compared our results when using unadjusted analyses as well as after adjustment by multivariable regression, patient clustering, and propensity weighting. Second, we repeated all analyses of GDMT prescribing patterns and HF outcomes in only those patients who were seen during both the pre-Covid and Covid eras, thus ensuring similar patient populations in the pre-Covid and Covid era groups. Third, we repeated all analyses including only outpatient visits that occurred outside of the peak Covid-19 surge months in Los Angeles (June and December), thereby reducing the contribution of effects from the pandemic. Fourth, we repeated all analyses using gastrointestinal bleeding (ICD-10 code K92) and the composite of stroke/transient ischemic attack (TIA)/thromboembolism (ICD-10 codes I60, I62, I63, I64.9, G45, I74, I26, I21, I23) as falsification endpoints as a check on whether there were additional baseline differences across patient groups that were not accounted for.
All analysis was performed with R software (version 3.4.1, Vienna, Austria). Cox proportional hazard models were conducted using the survival and survminer packages.
Results
Visit usage and characteristics
There were 11,106 outpatient cardiology visits for heart failure in the Covid-era study period (4/1/2020–12/31/2020), with 7,775 (70.0%) visits conducted in person, 1,009 (9.1%) by video, and 2,322 (20.9%) by telephone (Table 1). This is compared to 10,591 visits that were all conducted in person during the Pre-Covid study period (4/1/2019–12/31/2019). We found that patient characteristics were largely similar when comparing pre and Covid periods with some statistically significant differences that were small in magnitude (Table 1).
Table 1.
Patient and visit characteristics for all outpatient cardiology visits involving patients with a diagnosis of heart failure during either the pre-Covid (4/1/2019–12/31/2019) or Covid-Era (4/1/2020–12/31/2020)
| Pre-Covid Visits | Covid-Era Visits | Comparison p-value | ||||||
|---|---|---|---|---|---|---|---|---|
| All/In-Person | All | In-Person | Video | Telephone | Covid-Era vs. Pre-Covid | Video vs. In-Person* | Telephone vs. In-Person* | |
| N (%) | 10591 | 11106 | 7775 (70.0) | 1009 (9.1) | 2322 (20.9) | |||
| Age (mean (SD)) | 73.25 (14.85) | 73.16 (14.36) | 74.17 (14.13) | 64.71 (14.47) | 73.42 (13.90) | 0.639 | <0.001 | 0.619 |
| Male (%) | 6398 (60.4) | 6799 (61.2) | 4773 (61.4) | 689 (68.3) | 1337 (57.6) | 0.227 | <0.001 | 0.013 |
| Race (%) | 0.045 | 0.009 | <0.001 | |||||
| American Indian | 10 (0.1) | 6 (0.1) | 4 (0.1) | 1 (0.1) | 1 (0.0) | |||
| Asian | 728 (6.9) | 786 (7.1) | 557 (7.2) | 93 (9.2) | 136 (5.9) | |||
| Black | 1364 (12.9) | 1546 (13.9) | 1072 (13.8) | 122 (12.1) | 352 (15.2) | |||
| Hispanic | 837 (7.9) | 834 (7.5) | 530 (6.8) | 79 (7.8) | 225 (9.7) | |||
| White | 7082 (66.9) | 7307 (65.8) | 5196 (66.8) | 648 (64.2) | 1463 (63.0) | |||
| Other | 474 (4.5) | 506 (4.6) | 346 (4.5) | 51 (5.1) | 109 (4.7) | |||
| Pacific Islander | 12 (0.1) | 29 (0.3) | 18 (0.2) | 5 (0.5) | 6 (0.3) | |||
| Unknown | 84 (0.8) | 92 (0.8) | 52 (0.7) | 10 (1.0) | 30 (1.3) | |||
| Insurance (%) | <0.001 | <0.001 | <0.001 | |||||
| Medicaid | 243 (2.3) | 257 (2.3) | 121 (1.6) | 46 (4.6) | 90 (3.9) | |||
| Medicare | 6670 (63.0) | 6653 (59.9) | 4728 (60.8) | 467 (46.3) | 1458 (62.8) | |||
| Other | 115 (1.1) | 132 (1.2) | 95 (1.2) | 15 (1.5) | 22 (0.9) | |||
| Private | 3389 (32.0) | 3370 (30.3) | 2247 (28.9) | 463 (45.9) | 660 (28.4) | |||
| Unknown | 174 (1.6) | 694 (6.2) | 584 (7.5) | 18 (1.8) | 92 (4.0) | |||
| Encounter Diagnoses (%) | ||||||||
| Coronary Artery Disease | 4507 (42.6) | 4921 (44.3) | 3479 (44.7) | 421 (41.7) | 1021 (44.0) | 0.01 | 0.634 | 0.22 |
| Hypertension | 5208 (49.2) | 5693 (51.3) | 4046 (52.0) | 419 (41.5) | 1228 (52.9) | 0.002 | <0.001 | 0.001 |
| Atrial Fibrillation/Flutter | 4170 (39.4) | 4436 (39.9) | 3108 (40.0) | 383 (38.0) | 945 (40.7) | 0.399 | 0.398 | 0.247 |
| Diabetes Mellitus | 1493 (14.1) | 1772 (16.0) | 1315 (16.9) | 133 (13.2) | 324 (14.0) | <0.001 | 0.451 | 0.883 |
| Valvular Disease | 3317 (31.3) | 3428 (30.9) | 2475 (31.8) | 264 (26.2) | 689 (29.7) | 0.48 | 0.001 | 0.126 |
| Chronic Kidney Disease | 1644 (15.5) | 2144 (19.3) | 1469 (18.9) | 145 (14.4) | 530 (22.8) | <0.001 | 0.356 | <0.001 |
| HF Characteristics | ||||||||
| HFrEF (%) | 6144 (58.0) | 6573 (59.2) | 4377 (56.3) | 732 (72.5) | 1464 (63.0) | 0.082 | <0.001 | <0.001 |
| LVEF ≤ 35% (%) | 4778 (45.1) | 5182 (46.7) | 3414 (43.9) | 628 (62.2) | 1140 (49.1) | 0.023 | <0.001 | 0.001 |
| LVEF (mean (SD)) | 48.67 (18.12) | 48.23 (18.01) | 49.05 (17.73) | 43.51 (18.92) | 47.52 (18.22) | 0.086 | <0.001 | 0.009 |
| LVIDd (mean (SD)) | 4.87 (1.07) | 4.94 (1.06) | 4.88 (1.05) | 5.27 (1.10) | 4.97 (1.06) | <0.001 | <0.001 | <0.001 |
| RV ≥ mod depressed (%) | 1132 (10.7) | 1291 (11.6) | 821 (10.6) | 175 (17.3) | 295 (12.7) | 0.03 | <0.001 | 0.006 |
| RVIDd (mean (SD)) | 3.86 (0.82) | 3.82 (0.82) | 3.80 (0.80) | 3.91 (0.90) | 3.83 (0.83) | 0.002 | 0.141 | 0.18 |
| # Prior HF admissions (mean (SD)) | 1.01 (2.87) | 0.97 (3.06) | 0.94 (3.32) | 0.93 (1.77) | 1.08 (2.49) | 0.311 | 0.465 | 0.304 |
| # Visits/Patient for This Visit Type (mean (SD)) | 2.57 (2.42) | 2.78 (2.98) | 2.37 (2.80) | 1.56 (1.16) | 1.69 (1.43) | <0.001 | <0.001 | <0.001 |
| # Visits/Patient for All Visit Types (mean (SD)) | 2.57 (2.42) | 2.78 (2.98) | 3.05 (3.18) | 3.61 (2.97) | 3.48 (3.06) | <0.001 | <0.001 | <0.001 |
| Visit Length (min) (mean (SD)) | 31.14 (17.71) | 26.90 (15.34) | 28.25 (16.48) | 27.36 (9.70) | 22.18 (12.12) | <0.001 | <0.001 | <0.001 |
In-Person refers to Covid-Era in-person visits
When comparing remote to in-person visits during the Covid era, video and telephone visits were more likely to be with patients who were non-White (35.8% video, 37.0% telephone vs. 33.2% in-person) (Table 1). Those seen by video visits were more likely to be younger (64.7 years old (14.5) video vs. 74.2 (14.1) in-person), male (68.3% vs. 61.4%), and privately insured (45.9% vs. 28.9%), while those seen by telephone visits were more likely to be female (42.4% telephone vs. 38.6% in-person) (p<0.05 for all comparisons). Overall, remote visits were with patients with similar comorbidity profiles compared with in-person visits.
With regards to heart failure characteristics, remote visits had a higher proportion of patients with HFrEF (72.5% video, 63.0% telephone vs. 56.3% in-person) with a higher proportion of patients with an LVEF ≤ 35% (62.2%, 49.1% vs. 43.9%), more dilated left ventricles at end diastole (mean 5.3 cm (SD 1.1), 5.0 (1.1) vs. 4.9 (1.1)) as well as higher percentage with at least moderate RV dysfunction (17.3%, 12.7% vs. 10.6%). Nevertheless, patients seen across the different visit types had a similar number of prior heart failure admissions (0.9 admissions (1.8), 1.1 (3.5) vs. 0.9 (3.3)). Patients seen by remote visit had shorter visit durations (27.4 minutes (9.7), 22.2 (12.1) vs. 28.3 (16.5)) but more total visits during the study period (3.6 visits (3.0), 3.5 (3.1) vs. 3.1 (3.2)).
Diagnostic testing
Multivariable analyses adjusting for patient and visit characteristics showed that clinicians ordered significantly fewer tests per visit in the Covid era compared to pre-Covid (OR 0.51 (95% CI 0.48–0.54)) (Table 2). This reduction in ordering held true for electrocardiograms (0.51 (0.47–0.54)), stress echocardiograms (0.38 (0.26–0.55)), and most laboratory tests. We found a further decrease in test ordering when comparing Covid-era remote visits to Covid-era in-person visits (0.20 (0.18–0.22) video vs. in-person, 0.18 (0.17–0.19) telephone vs. in-person), with the same pattern of reduction occurring across multiple diagnostic and lab tests.
Table 2.
Ordering frequency of diagnostic tests during clinic visits
| Pre-Covid Visits | Covid-Era Visits | Odds Ratio (95% Confidence Interval) | ||||||
|---|---|---|---|---|---|---|---|---|
| All/In-Person | All | In-Person | Video | Telephone | Covid vs. Pre-Covid (Ref) | Video vs. In-Person* (Ref) | Telephone vs. In-Person* (Ref) | |
| N | 10591 | 11106 | 7775 | 1009 | 2322 | |||
| Diagnostic Tests | ||||||||
| Any Diagnostic Test | 7624 (72.0%) | 6009 (54.1%) | 5092 (65.5%) | 325 (32.2%) | 592 (25.5%) | 0.51 (0.48–0.54) | 0.20 (0.18–0.22) | 0.18 (0.17–0.19) |
| Electrocardiogram | 3092 (29.2%) | 1903 (17.1%) | 1873 (24.1%) | 4 (0.4%) | 26 (1.1%) | 0.51 (0.47–0.54) | 0.02 (0.01–0.03) | 0.05 (0.05–0.06) |
| Transthoracic Echocardiogram | 1650 (15.6%) | 1473 (13.3%) | 1262 (16.2%) | 75 (7.4%) | 136 (5.9%) | 0.93 (0.86–1.01) | 0.37 (0.32–0.43) | 0.36 (0.32–0.40) |
| Coronary CT Angiogram | 34 (0.3%) | 36 (0.3%) | 34 (0.4%) | 1 (0.1%) | 1 (0.0%) | 1.21 (0.75–1.95) | 0.34 (0.14–0.84) | 0.06 (0.02–0.25) |
| Nuclear Stress Imaging | 201 (1.9%) | 183 (1.6%) | 165 (2.1%) | 7 (0.7%) | 11 (0.5%) | 0.91 (0.74–1.12) | 0.24 (0.15–0.40) | 0.32 (0.24–0.43) |
| Stress Echocardiogram | 101 (1.0%) | 40 (0.4%) | 29 (0.4%) | 5 (0.5%) | 6 (0.3%) | 0.38 (0.26–0.55) | 0.73 (0.36–1.47) | 0.47 (0.25–0.86) |
| Exercise Stress Test | 16 (0.2%) | 5 (0.0%) | 4 (0.1%) | 1 (0.1%) | 0 (0.0%) | 0.14 (0.05–0.42) | 1.87 (0.36–9.69) | - |
| Coronary Artery Calcium Scan | 7 (0.1%) | 1 (0.0%) | 1 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.11 (0.01–0.94) | - | - |
| Cardiac MRI | 57 (0.5%) | 43 (0.4%) | 35 (0.5%) | 2 (0.2%) | 6 (0.3%) | 0.92 (0.61–1.38) | 0.28 (0.11–0.73) | 0.67 (0.38–1.20) |
| External ECG Monitor | 234 (2.2%) | 195 (1.8%) | 162 (2.1%) | 14 (1.4%) | 19 (0.8%) | 0.85 (0.70–1.03) | 0.62 (0.45–0.85) | 0.47 (0.36–0.61) |
| Laboratory Tests | ||||||||
| Brain Natriuretic Peptide | 3558 (33.6%) | 2768 (24.9%) | 2473 (31.8%) | 79 (7.8%) | 216 (9.3%) | 0.69 (0.65–0.73) | 0.19 (0.16–0.22) | 0.24 (0.22–0.26) |
| Lipids | 1173 (11.1%) | 1124 (10.1%) | 985 (12.7%) | 38 (3.8%) | 101 (4.3%) | 0.94 (0.86–1.03) | 0.23 (0.19–0.29) | 0.34 (0.30–0.38) |
| Complete Blood Count | 2621 (24.7%) | 2153 (19.4%) | 1893 (24.3%) | 89 (8.8%) | 171 (7.4%) | 0.75 (0.70–0.80) | 0.33 (0.29–0.37) | 0.26 (0.24–0.28) |
| Metabolic Panel | 4867 (46.0%) | 3848 (34.6%) | 3311 (42.6%) | 178 (17.6%) | 359 (15.5%) | 0.68 (0.64–0.72) | 0.26 (0.23–0.29) | 0.27 (0.25–0.29) |
| Coagulation Tests | 880 (8.3%) | 562 (5.1%) | 493 (6.3%) | 41 (4.1%) | 28 (1.2%) | 0.64 (0.57–0.72) | 0.61 (0.50–0.74) | 0.22 (0.18–0.27) |
| ESR or CRP | 580 (5.5%) | 540 (4.9%) | 484 (6.2%) | 20 (2.0%) | 36 (1.6%) | 0.96 (0.84–1.08) | 0.30 (0.23–0.40) | 0.26 (0.21–0.31) |
In-Person refers to Covid-Era in-person visits
Odds ratios were adjusted by age, sex, race, insurance status, calendar date, visit length, and visit diagnoses (coronary artery disease, hypertension, atrial fibrillation/flutter, diabetes mellitus, valvular disease, and chronic kidney disease).
Odds ratios comparing remote vs. in-person visits during the Covid-Era were additionally adjusted by propensity weighting for remote visit
GDMT prescription
To assess rates of GDMT prescription, we studied a subset of visits involving patients with heart failure and an ejection fraction ≤ 35% (N= 9960 visits: 5182 Pre-Covid in-person, 3414 Covid-era in-person, 628 Covid-era video, 1140 Covid-era telephone). We found that after multivariable adjustment for patient and visit characteristics, during patient visits, clinicians in the Covid era compared to the pre-Covid era were less likely to prescribe any GDMT (OR 0.80 (0.72–0.90)) with specific reductions in the prescribing rates of beta-blockers (0.83 (0.73–0.94)) and ACE/ARB/ARNIs (0.58 (0.47–0.72)) (Figure 1).
Figure 1.
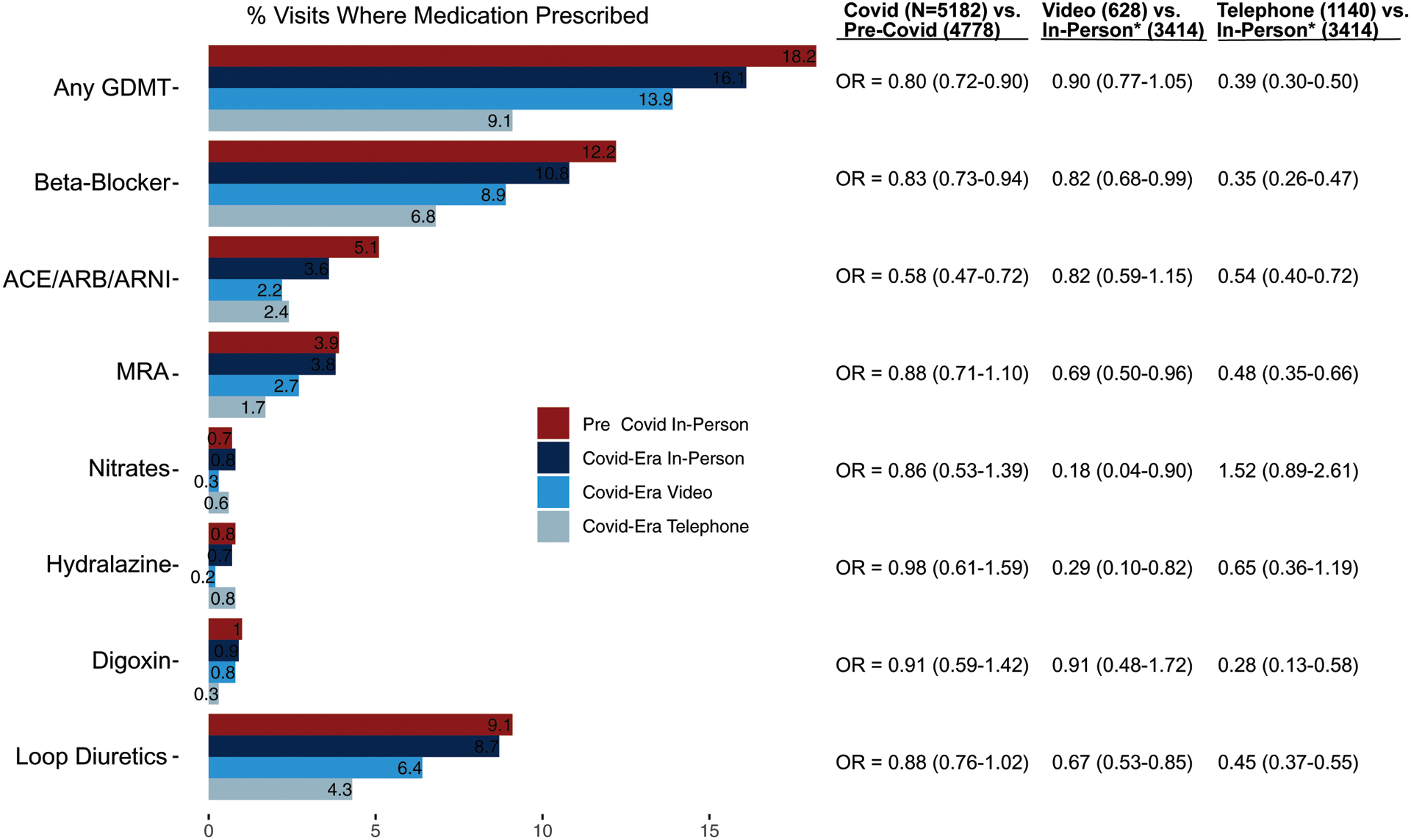
Rates of heart failure medication prescription during clinic visits for patients with heart failure with a left ventricular ejection fraction ≤ 35%.
*In-Person refers to Covid-Era in-Person visits
GDMT includes evidence-based Beta Blocker, ACEi, ARB, ARNI, MRA, Hydralazine or Nitrates (if patient identified as black), or digoxin
Beta blocker = metoprolol, carvedilol, bisoprolol, or nebivolol
Nitrates = isosorbide dinitrate or isosorbide mononitrate
Odds ratios were adjusted by propensity score weighting as well as age, sex, race, insurance status, calendar date, visit length, and visit diagnoses (coronary artery disease, hypertension, atrial fibrillation/flutter, diabetes mellitus, valvular disease, and chronic kidney disease).
Abbreviations: GDMT = guideline directed medical therapy, ACEi = angiotensin converting enzyme inhibitor, ARB = angiotensin receptor blocker, MRA = mineralocorticoid receptor antagonist, Ref = reference
When comparing video to in-person visits during the Covid era, clinicians prescribed fewer beta-blockers (0.82 (0.68–0.99)), MRAs (0.69 (0.50–0.96)), nitrates (0.18 (0.04–0.90)), hydralazine (0.29 (0.10–0.82)), and loop diuretics (0.67 (0.53–0.85)). When comparing telephone to in-person visits during the Covid era, clinicians were significantly less likely to prescribe any GDMT (0.39 (0.30–0.50)), including beta-blockers (0.35 (0.26–0.47)), ACE/ARB/ARNI (0.54 (0.40–0.72)), MRAs (0.48 (0.35–0.66)), digoxin (0.28 (0.13–0.58)), and loop diuretics (0.45 (0.37–0.55)).
Outcomes
Lastly, we quantified the incidence of heart failure-related ED visits and hospital admissions as well as death within 90 days of outpatient cardiology clinic visits for heart failure (Figure 2). We found that patients had similar rates of 90-day heart failure related ED visits (HR 0.92 (0.78–1.10)), hospitalizations (0.91 (0.76–1.09)), and mortality (1.14 (0.82–1.57)) when comparing Covid-era to pre-Covid visits after multivariable adjustment for patient and visit characteristics. Among those who were hospitalized, patients in the Covid era had a longer hospital length of stay (mean difference 1.15 days (95% CI 0.08–2.22)) and greater chance for requiring ICU care (OR 1.46 (1.05–2.02)).
Figure 2.
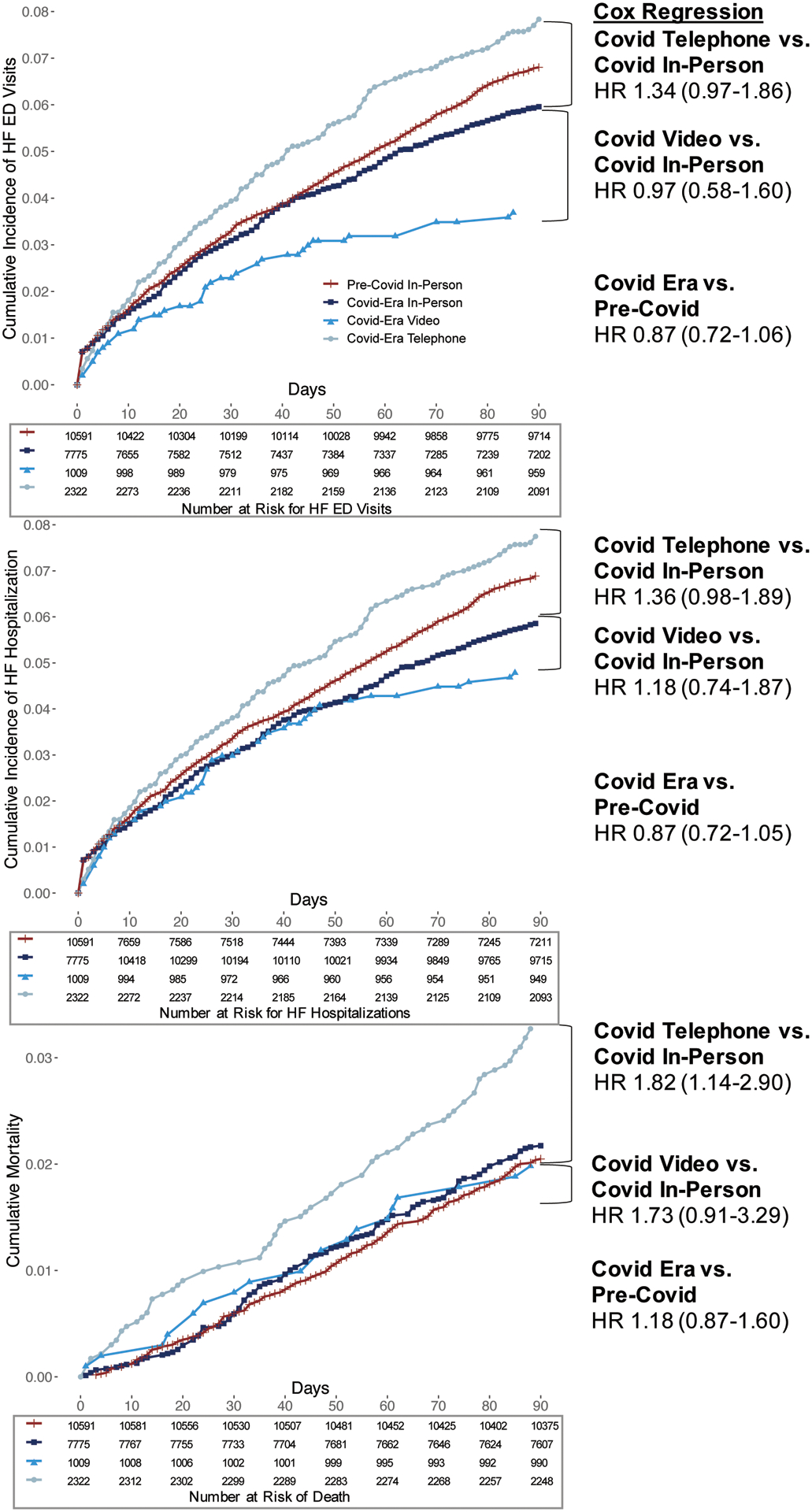
Cumulative incidence of heart failure related emergency department visits, hospital admissions, and mortality over 90 days after outpatient visit for heart failure.
Hazard ratios are from Cox proportional hazards models with adjustment for age, sex, race, insurance status, calendar date, visit length, and visit diagnoses (coronary artery disease, hypertension, atrial fibrillation/flutter, diabetes mellitus, valvular disease, and chronic kidney disease) as well as clustering by patient. Comparisons of remote vs. in-person visits were additionally adjusted by propensity weighting for remote visit
Abbreviations: ED = emergency department, HR = hazard ratio, HF = heart failure
During the Covid era, patients seen by video compared to those seen in-person did not have significantly different rates of 90-day ED visits (0.94 (0.62–1.41)), hospitalization (1.13 (0.76–1.68)), or mortality rates (1.74 (0.82–3.71)), although the overall number of events was low. Those seen by telephone compared to those seen in-person had higher hazard rates for mortality (HR 1.82 (1.14–2.90)) and trended toward higher hazard rates for heart failure related ED visits (1.34 (0.97–1.86)) and hospitalizations (1.36 (0.98–1.89)). Among those hospitalized for heart failure in the Covid era, when compared to patients seen as an outpatient by in-person visit, those seen by remote visit did not have significantly different hospital lengths of stay (mean difference 2.52 days (95% CI −0.20–5.24) video vs. in-person, −0.64 (−2.2–0.90) telephone vs. in-person). The chance of ICU admission was higher after a video visit (OR 2.25 (1.02– 4.96)) or a telephone visit (1.91 (1.13– 3.23)).
When stratifying our data by time, we found that the incidence of 90-day heart failure related ED visits, hospitalizations, and mortality were similar or lower for Covid-era clinic visits from April to August compared to pre-Covid visits during the same months (Figure 3). However, from September through December, Covid-era telephone visits resulted in higher rates of ED visits, hospitalizations, and mortality.
Figure 3.
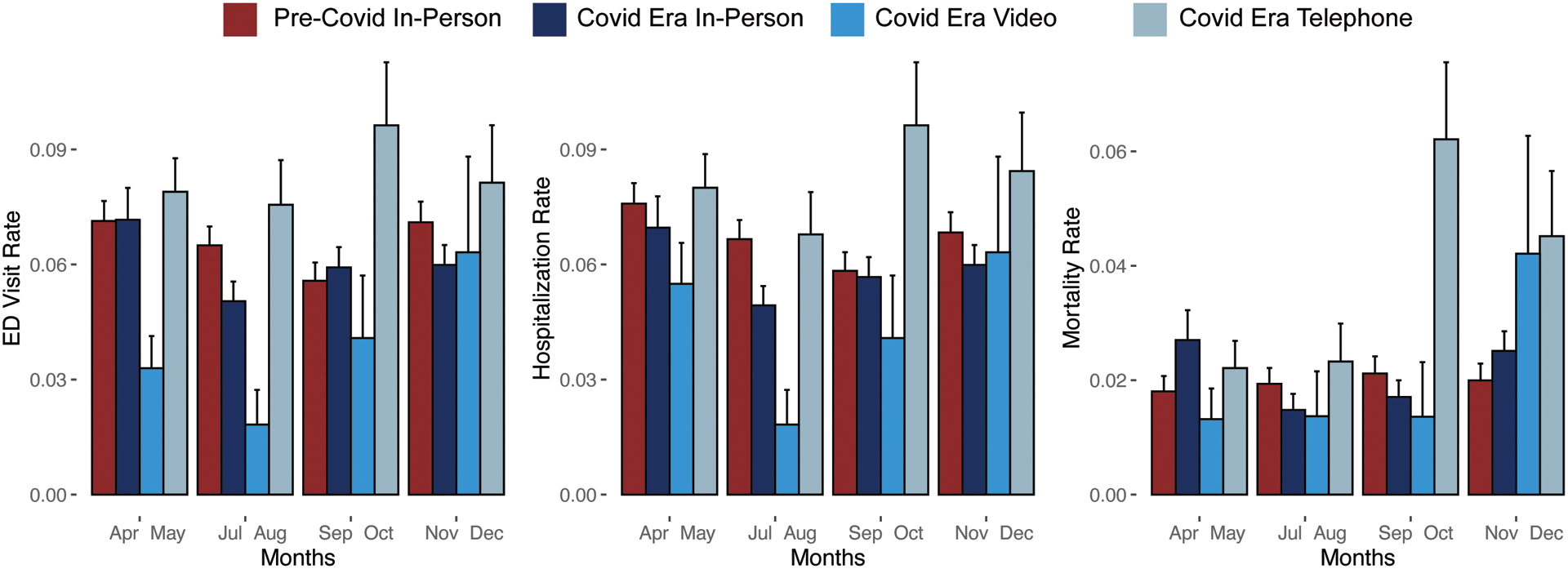
Incidence over time of heart failure related emergency department visits, hospital admissions, and mortality over 90 days after outpatient visit for heart failure
Error bars represent standard error
Sensitivity Analyses
We saw similar results with regards to GDMT prescribing patterns and HF outcomes in unadjusted analyses as well as after adjustment by multivariable regression, patient clustering, and propensity weighting (Figure 4, Supplemental Table 1). We also found consistent results after restricting our dataset to only those patients who were seen during both the pre-Covid and Covid periods, as well as after restricting our sample to only patient seen during months when the pandemic was least severe (non-Covid-19-surge months) (Figure 4, Supplemental Table 1). In considering falsification endpoints, we found no statistically significant differences across patient groups in the combined incidence of stroke/TIA/thromboembolism: Pre-Covid vs. Covid-era (HR 1.05 (95% CI 0.75–1.48)), Covid-era video vs. Covid-era in-person (2.51 (0.17–37.5)), Covid-era telephone vs. Covid-era in-person (0.62 (0.28–1.35)). There were also no significant differences in incidence of gastrointestinal bleeding: Pre-Covid vs. Covid-era (1.38 (0.96–1.97)), Covid-era video vs. Covid-era in-person (1.23 (0.71–2.15)), Covid-era telephone vs. Covid-era in-person (0.51 (0.19–1.36)).
Figure 4.
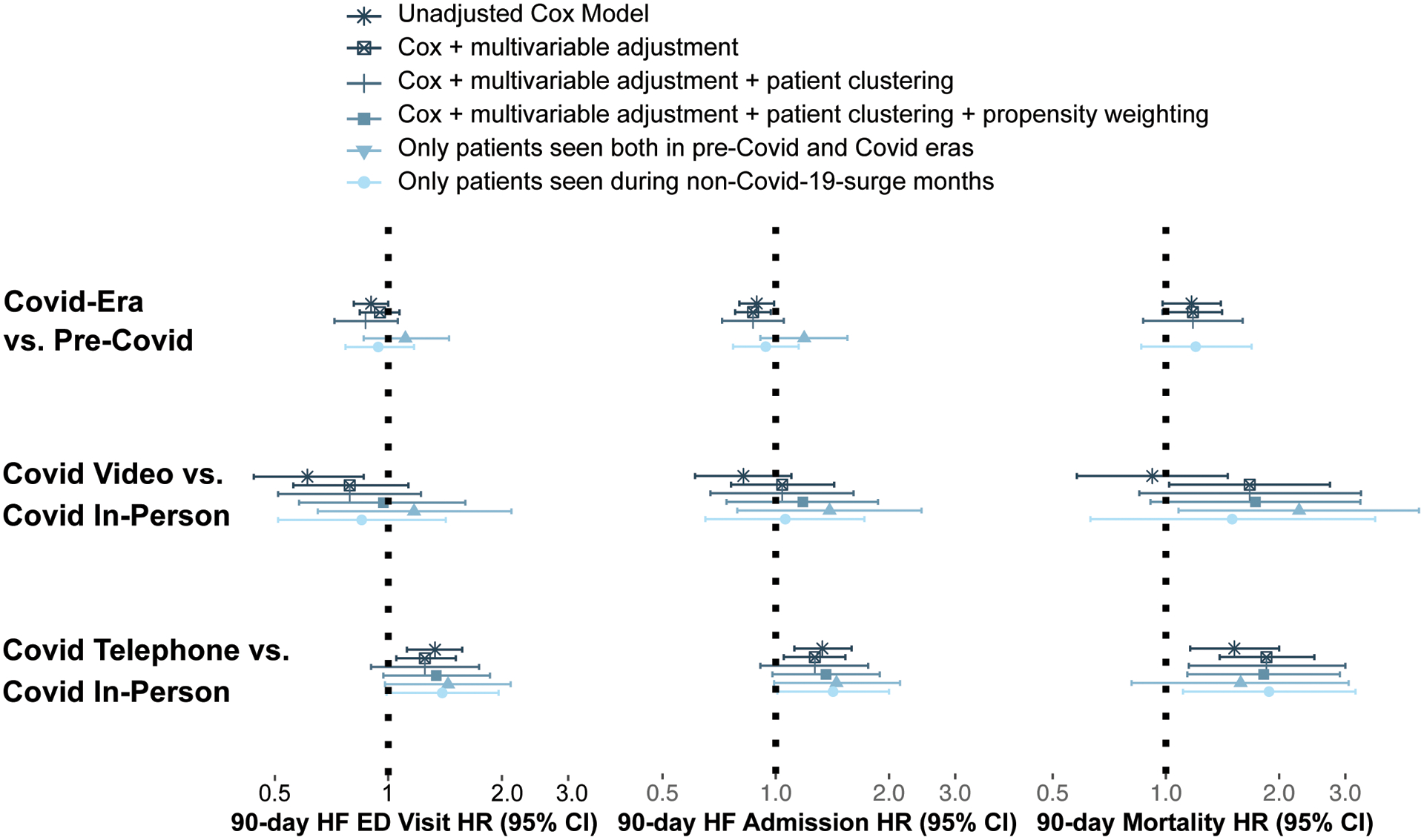
Sensitivity analysis of hazard rates of 90-day heart failure emergency department visits, hospitalization, and mortality after outpatient visit for heart failure.. Multivariable adjustment adjusted for age, sex, race, insurance status, calendar date, visit length, and visit diagnoses (coronary artery disease, hypertension, atrial fibrillation/flutter, diabetes mellitus, valvular disease, and chronic kidney disease).
Propensity weighting was calculated based on propensity for being seen by remote visit according to above patient characteristics.
Non-Covid-19-surge months excluded outpatient visits during peak months of the Covid-19 pandemic in Los Angeles (June, December)
Abbreviations: HF = heart failure, ED = emergency department, HR = hazard ratio, CI = confidence interval
Discussion
In this study of 21,697 outpatient cardiology visits for heart failure, we compared the patient characteristics, ordering practices, and patient outcomes for individuals seen by remote and in-person visits in the Covid era to those seen by in-person visits in the Pre-Covid era. We found that compared to in-person visits in the Covid era, remote (video and telephone) visits were more frequently used by patients from racial and ethnic minority groups, but that video visits were more often used by male, younger, and privately insured patients. Remote visits were more frequently with patients who had HFrEF, severe left ventricular dysfunction, and at least moderate RV dysfunction, although these patients on average did not have more prior hospitalizations compared to those seen in-person. During remote visits, clinicians ordered fewer diagnostic tests and less GDMT and loop diuretics, with this reduction in ordering being more pronounced during telephone visits compared to video visits. With the lower testing and prescribing frequencies, patients seen by telephone visit had higher rates of 90-day mortality with trends towards higher 90-day rates of heart failure ED visits and hospitalizations when compared to those seen by in-person visits. There was no difference in outcomes with video visits, although the total number of recorded events were low. This is one of the first reports of changes in practice patterns and patient outcomes associated with the transition from in-person to remote heart failure care in the Covid era.
While remote heart failure care has been in use for years, its widespread adoption during the Covid-19 pandemic has laid the foundations for telemedicine to become a standard and significant component of future heart failure care.1 Telemedicine interventions can be effective for monitoring patients for decompensation, ensuring safe transitions from inpatient to outpatient settings, and titrating GDMT.13–20 However, while many of these findings were in carefully monitored trial settings, the Covid era represents one of the first opportunities to observe and study the effects of remote heart failure care on a large scale and in the real world. Moreover, almost all prior studies examined the effects of specific individual interventions and almost none to-date have described the effects of using remote visits as the primary form of outpatient heart failure care. Describing the effects of this transition to remote care is important to benchmark the effectiveness of current telemedicine practices and identify best practices as well as areas for potential improvement. We focused on three important areas to assess the efficacy of remote heart failure care: (1) patient usage of care, (2) testing and prescribing patterns, and (3) patient outcomes within 90 days of outpatient visit.
Patient usage of remote heart failure care
As the use of telemedicine grows, a concern has developed around disparities in access to these services, driven by the “Digital Divide”.21,22 Individuals who are older, poorer, less educated, from racial and ethnic minority groups, and with chronic medical conditions have historically had less access to the internet and therefore potentially, telemedicine services. We found that some of these trends were true in our heart failure population, but only for video visits. Compared to patients seen in person, patients who used video visits were more often male, on average 10 years younger, and were 17% more likely to have private insurance, a proxy for higher socioeconomic status. In contrast, there were no significant demographic differences for patients who were seen by telephone versus in-person during the Covid era. This may be because telephone visits require less advanced equipment and understanding compared to video visits. We also found that patients from racial and ethnic minority groups accessed both video and telephone visits more frequently than in-person ones. Patients using remote visits also had similar and sometime even higher rates of cardiovascular comorbidities as well as left and right ventricular dysfunction, indicating both patient and clinician comfort with remote care for even the sickest heart failure patients.
Testing and prescribing patterns
Clinicians on average ordered substantially fewer diagnostic and laboratory tests in the Covid era and during remote visits: about one-half of tests compared to pre-Covid and one-fifth of tests during a remote visit compared to an in-person one. This may be attributed to lower test availability during the Covid period as well as patient and clinician fears of Covid-19 exposure. Furthermore, since many tests are performed on-site during in-person visits, remote visits posed an additional logistical inconvenience that likely further limited testing.
We observed similar decreases in the prescription of heart failure medications. For patients with a left ventricular ejection fraction ≤ 35%, clinicians prescribed one-fifth less GDMT during the Covid era compared to pre-Covid. During the Covid era, compared to in-person visits, clinicians were less likely to prescribe beta-blockers, MRAs, or loop diuretics during both video and telephone visits. Clinicians were also less likely during telephone visits to prescribe any GDMT at all or ACE/ARB/ARNIs. The reductions in medication prescriptions could be explained by the observed decrease in laboratory testing, as patient reluctance to venture outside of the home for electrolyte and renal function assessment may have hindered clinicians from prescribing or titrating ACE/ARB/ARNIs, MRAs, and loop diuretics. Clinicians may have also felt less comfortable with assessing heart rate, blood pressure, symptoms, and degree of heart failure decompensation during remote visits, which may partially explain why prescribing was especially depressed during telephone visits, which lack the visual information provided during in-person and video visits. Early concerns about ACE/ARB/ARNIs enhancing the susceptibility of patients to Covid-19 infection through the ACE receptor may have played a potential role in early decreases in prescription of these medications, although society guidelines were issued in March, before the study period, that addressed these concerns.23 Future qualitative studies are needed to better understand the heightened therapeutic inertia noted during remote visits in the Covid era.
Differences in 90-day outcomes
Early reports from other centers had shown that heart failure admissions were reduced during the first months of the pandemic. However, heart failure patients that were admitted had more severe symptoms and higher mortality, suggesting that patients might be delaying appropriate management of heart failure decompensations.24–30 In our study, we observed that patients in the Covid era compared to the pre-Covid era had similar rates of 90-day heart failure related ED visits, admissions, and mortality when considering the entire study period together. However, consistent with these earlier reports, when stratifying outcomes by time, rates of adverse outcomes were initially similar or lower in the Covid era compared to pre-Covid, but then rose as the pandemic progressed. In addition, heart failure patients admitted in the Covid era had longer hospital lengths of stay and more ICU care.
The worse outcomes seen in the Covid era were most pronounced in patients who had preceding telephone visits, findings that were consistent across multiple sensitivity analyses. Thus, it appears possible that the reduction in testing and GDMT prescription observed with telephone visits in particular was associated with measurable harms regarding heart failure ED visits, hospitalizations, and mortality. We did not see the same outcome trends with video visits, although the overall number of video visits may not have been large enough to have detected a significant difference in adverse events.
Several limitations merit consideration. While we studied a large cohort involving multiple sites over several months, our patient sample was still limited to a single medical system and geographical location. Our patient population was diverse but predominantly covered by private insurance or Medicare and lived in an urban center, which may not reflect patient populations most affected by the “Digital Divide”. For assessing GDMT prescriptions, we were unable to distinguish whether prescriptions represented medication titration or continuation, which may be an important distinction for future more detailed studies on prescribing behaviors. For outcomes, we do not know if patients visited hospitals outside of our medical system, although our center is one of the major providers in the area and ED visits or hospitalizations outside of our center should not have disproportionately affected a particular patient group in our cohort. As our study is observational, patient selection for remote visits was not randomized and therefore potentially subject to bias. However, the transition to remote care was widespread, affecting most patients during the Covid pandemic and therefore introducing quasi-experimental conditions. We found that patients seen across the different visit types had similar rates of comorbidities and number of prior heart failure hospitalizations. We additionally confirmed that our observed results appeared to be consistent across several methods of adjustment for patient demographics and comorbidities as well as when restricting the patient sample to only those patients seen both in the pre-Covid and Covid periods and to those seen during non-Covid-19-surge months. Falsification endpoints also served as reassuring controls and demonstrated similar rates of stroke/TIA/thromboembolism and gastrointestinal bleeding across the patient groups. Nevertheless, we acknowledge that unaccounted confounding factors may still exist and it is plausible that different results may be observed if patients were randomized to different types of visits. Ultimately, our findings reflect real world practice patterns with the observed differences in outcomes likely being a combination of both the patients that use remote visits as well as real differences in clinical care patterns due to the nature of remote visits. Future randomization studies would be helpful for complementing our findings.
Conclusion
In a large study of outpatient cardiology visits for patients with heart failure, we found that the expansive transition of outpatient heart failure care to remote visits in the Covid era was associated with reductions in diagnostic test ordering and GDMT prescription, especially with telephone visits. These changes in care patterns occurred in conjunction with significant increases in 90-day mortality and trends towards increases in HF ED visits and hospitalizations for patients seen by telephone visits but not by video visits.
Supplementary Material
Acknowledgements
The authors would like to acknowledge Brian Claggett Ph.D. for his assistance and advice with regards to the statistical methods for this manuscript.
Funding
This works was supported by the following grants:
NIH T32 5T32HL116273-07
NCI/NIAID U54 CA260591
NIH/NHLBIK23HL153888
The Erika J. Glazer Family Foundation
Funding sources had no involvement in study design, data collection, or analysis
Footnotes
Disclosures
The authors have no conflicts of interest to declare.
References
- 1.Gorodeski EZ, Goyal P, Cox ZL, Thibodeau JT, Reay RE, Rasmusson K, Rogers JG, Starling RC. Virtual Visits for Care of Patients with Heart Failure in the Era of COVID-19: A Statement from the Heart Failure Society of America. J Card Fail. 2020;26:448–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verma S Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19 | Health Affairs [Internet]. Health Affairs. [cited 2020 Oct 12];Available from: https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/ [Google Scholar]
- 3.DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld J, Jessup M. Considerations for Heart Failure Care During the COVID-19 Pandemic. JACC Heart Fail. 2020;8:681–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal S, Garcia-Telles N, Aggarwal G, Lavie C, Lippi G, Henry BM. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): Early report from the United States. Diagnosis (Berl). 2020;7:91–96. [DOI] [PubMed] [Google Scholar]
- 5.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Albert NM, Prasun MA. Telemedicine in Heart Failure during COVID-19: Like it, Love It or Lose It? Heart Lung. 2020;49:A11–A12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McIlvennan CK, Allen LA, Devore AD, Granger CB, Kaltenbach LA, Granger BB. Changes in Care Delivery for Patients With Heart Failure During the COVID-19 Pandemic: Results of a Multicenter Survey. J Card Fail. 2020;26:635–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.UMAPATHI P, CUOMO K, RILEY S, HUBBARD A, MENZEL K, SAUER E, GILOTRA NA. Transforming Ambulatory Heart Failure Care in the Coronavirus Disease-19 Era: Initial Experience From a Heart Failure Disease Management Clinic. J Card Fail. 2020;26:637–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJV, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WHW, Tsai EJ, Wilkoff BL, American College of Cardiology Foundation, American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–239. [DOI] [PubMed] [Google Scholar]
- 10.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137–e161. [DOI] [PubMed] [Google Scholar]
- 11.Olmos A, Govindasamy P. A Practical Guide for Using Propensity Score Weighting in R. Practical Assessment, Research, & Evaluation. 2015;20:8. [Google Scholar]
- 12.Funk MJ, Westreich D, Wiesen C, Stürmer T, Brookhart MA, Davidian M. Doubly Robust Estimation of Causal Effects. Am J Epidemiol. 2011;173:761–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohebali D, Kittleson MM. Remote monitoring in heart failure: current and emerging technologies in the context of the pandemic. Heart. 2021;107:366–372. [DOI] [PubMed] [Google Scholar]
- 14.Pekmezaris R, Tortez L, Williams M, Patel V, Makaryus A, Zeltser R, Sinvani L, Wolf-Klein G, Lester J, Sison C, Lesser M, Kozikowski A. Home Telemonitoring In Heart Failure: A Systematic Review And Meta-Analysis. Health Affairs (Project Hope). 2018;37:1983–1989. [DOI] [PubMed] [Google Scholar]
- 15.Kitsiou S, Paré G, Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: an overview of systematic reviews. Journal of Medical Internet Research. 2015;17:e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abraham WT, Adamson PB, Bourge RC, Aaron MF, Costanzo MR, Stevenson LW, Strickland W, Neelagaru S, Raval N, Krueger S, Weiner S, Shavelle D, Jeffries B, Yadav JS, CHAMPION Trial Study Group. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet. 2011;377:658–666. [DOI] [PubMed] [Google Scholar]
- 17.Gorodeski Eiran Z., Moennich Laurie Ann, Riaz Haris, Jehi Lara, Young James B., Tang W.H. Wilson. Virtual Versus In-Person Visits and Appointment No-Show Rates in Heart Failure Care Transitions. Circulation: Heart Failure. 2020;13:e007119. [DOI] [PubMed] [Google Scholar]
- 18.Thibodeau Jennifer T, Gorodeski Eiran Z Telehealth for Uptitration of Guideline-Directed Medical Therapy in Heart Failure. Circulation. 2020;142:1507–1509. [DOI] [PubMed] [Google Scholar]
- 19.Ware P, Ross HJ, Cafazzo JA, Boodoo C, Munnery M, Seto E. Outcomes of a Heart Failure Telemonitoring Program Implemented as the Standard of Care in an Outpatient Heart Function Clinic: Pretest-Posttest Pragmatic Study. J Med Internet Res. 2020;22:e16538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Artanian V, Rac VE, Ross HJ, Seto E. Impact of Remote Titration Combined With Telemonitoring on the Optimization of Guideline-Directed Medical Therapy for Patients With Heart Failure: Protocol for a Randomized Controlled Trial. JMIR Res Protoc. 2020;9:e19705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee R Digital Divides 2015 [Internet]. Pew Research Center; 2015. [cited 2020 Oct 13]. Available from: https://www.pewresearch.org/internet/2015/09/22/digital-divides-2015/
- 22.Eberly LA, Khatana SAM, Nathan AS, Snider C, Julien HM, Deleener ME, Adusumalli S. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic: Bridging or Opening the Digital Divide? Circulation. 2020;142:510–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bozkurt B, Kovacs R, Harrington B. Joint HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19. J Card Fail. 2020;26:370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bromage DI, Cannatà A, Rind IA, Gregorio C, Piper S, Shah AM, McDonagh TA. The impact of COVID-19 on heart failure hospitalization and management: report from a Heart Failure Unit in London during the peak of the pandemic. Eur J Heart Fail. 2020;22:978–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersson C, Gerds T, Fosbøl E, Phelps M, Andersen J, Lamberts M, Holt A, Butt JH, Madelaire C, Gislason G, Torp-Pedersen C, Køber L, Schou M. Incidence of New-Onset and Worsening Heart Failure Before and After the COVID-19 Epidemic Lockdown in Denmark: A Nationwide Cohort Study. Circ Heart Fail. 2020;13:e007274. [DOI] [PubMed] [Google Scholar]
- 26.Colivicchi F, Di Fusco SA, Magnanti M, Cipriani M, Imperoli G. The Impact of the Coronavirus Disease-2019 Pandemic and Italian Lockdown Measures on Clinical Presentation and Management of Acute Heart Failure. J Card Fail. 2020;26:464–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hall ME, Vaduganathan M, Khan MS, Papadimitriou L, Long RC, Hernandez GA, Moore CK, Lennep BW, McMullan MR, Butler J. Reductions in Heart Failure Hospitalizations During the COVID-19 Pandemic. J Card Fail. 2020;26:462–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cox ZL, Lai P, Lindenfeld J. Decreases in acute heart failure hospitalizations during COVID-19. Eur J Heart Fail. 2020;22:1045–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moayedi Y, Alba AC, Lee DS, Wijeysundera HC, Ross HJ. The Next Wave of Health Care Strain Related to COVID-19: Heart Failure Patients Coming Back in Force-We Must Not Fail Them. Can J Cardiol. 2020;36:993–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cannata A, Bromage DI, Rind IA, Gregorio C, Bannister C, Albarjas M, Piper S, Shah AM, McDonagh TA. Temporal trends in decompensated heart failure and outcomes during COVID-19: A multisite report from heart failure referral centres in London. Eur J Heart Fail [Internet]. 2020. [cited 2021 Mar 11];Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7461082/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


