Abstract
Introduction:
Representativeness of research populations impacts the ability to extrapolate findings. The Burn Model System (BMS) National Database is one of the largest prospective, longitudinal, multi-center research repositories collecting patient-reported outcomes after burn injury..
Objective:
This study aimed to assess if the BMS Database is representative of the population that is eligible to participate.
Design:
Data on adult burn survivors who were eligible for the BMS Database from 2015 to 2019 were analyzed.
Setting:
N/A
Participants:
Burn survivors treated at BMS centers meeting eligibility criteria for the BMS Database. Eligibility for the database is based on burn size and receipt of autografting surgery.
Interventions:
N/A
Main Outcome Measure(s):
Race, ethnicity, gender, and age were compared between individuals who did and did not enroll. Regression analysis examined the correlation between demographic characteristics and study enrollment.. Additional regression analysis examined the association between enrollment and the intersection of race, ethnicity, and gender.
Results:
A total of 982 adult burn survivors were eligible for the BMS database during the study period. Of those who were eligible, 72.1% Enrolled and 27.9% were Not Enrolled. The Enrolled group was more female and younger compared to the Not Enrolled group. In regression analyses, Black/African American burn survivors were less likely and individuals identifying as female were more likely to enroll in the BMS Database. Further, when looking at groups by race and gender and ethnicity and gender, White men and women were more likely to enroll compared to Black/African American men and women and non-Hispanic/Latino men were more likely to enroll compared to Hispanic/Latino men.
Conclusions:
This study found differences in BMS Database enrollment by race, ethnicity, and gender. Further research is warranted to investigate causes for the disparities found in this study. Additionally, strategies are needed to improve enrollment to ensure future representativeness.
Introduction
High-quality clinical research is a cornerstone of the development of evidence-based practice guidelines. Clinical investigations should be aimed at ensuring that findings address the needs of the entire target population. There is a vast amount of research demonstrating disparities in healthcare access, quality, and acute and long-term outcomes based on race, ethnicity, gender, age, and socioeconomic status—with minority groups faring worse overall.1 Healthcare disparities for people in minority racial and ethnic groups have been documented in rehabilitation medicine in general, as well as in the burn population.2–4 The presence of these disparities emphasizes the importance of ensuring individuals from all groups are equitably represented in research.
Racial and ethnic minorities may be less willing to participate in research in the United States (U.S.) due to a variety of factors, including but not limited to, mistrust of the medical system and historic mistreatment.5,6 There is limited research specifically examining consent rates of racial and ethnic minority groups compared to majority groups. Among the few studies that have examined consent rates by race and ethnicity, results are mixed.7–9 Some studies have found minority groups to be less likely to participate and some cite no differences or a greater amount of participation by Black/African American and Hispanic/Latino individuals.5,10–12 Notably, scientific research has historically excluded women and older adults when setting enrollment criteria and identifying potential research study subjects.13–15 In recent years, however, important efforts by the National Institutes of Health (NIH) and others have improved the enrollment of underserved populations in research.16–19
An exploration of the epidemiology of burns shows that some minority populations are disproportionately at risk of sustaining a burn injury.20 Disparities within the burn population show that minority individuals often experience worse outcomes.21–23 For example, research shows that African American burn survivors have increased odds of mortality after burn injury and are at higher risk of morbidity compared with non-Hispanic white individuals.21,24,25 Sex and/or gender may also be a factor as there is evidence that female burn survivors experience higher mortality and worse scores on some patient reported outcome measures compared to male survivors.24–29 Not surprisingly, age also influences outcomes, and elderly burn survivors have higher morbidity and mortality than younger survivors.30–32
Conducting longitudinal research in the burn survivor population is a vital step in understanding recovery and long-term outcomes to inform clinical care decisions. Moreover, it is imperative that the burn survivor population is adequately represented in long-term outcomes research to ensure that results are applicable to the entire target population. Underrepresentation of certain groups of burn survivors may impact the extent to which research findings can be applied to the burn population, leading to the development of evidence-based practices that are not necessarily valid for all.
As one of the largest prospective, longitudinal, multicenter research data repositories for burn survivors, the Burn Model System (BMS) National Database is a unique resource to explore the representativeness of burn survivors who choose to participate in long-term research. Therefore, the purpose of this research study was to compare demographic and clinical characteristics of enrolled vs. not enrolled burn survivors who were eligible to participate in the BMS Database. The authors hypothesized that there would be disparities in enrollment by race, ethnicity, gender, and age. Therefore, the aim of this study was to assess the extent to which the research population of the BMS Database is representative of the patient population that is eligible to participate. This study fills a gap in the existing literature by examining the extent to which burn research participants adequately represent the larger burn survivor population. More specifically, the results inform the generalizability of research using the BMS Database.
Methods
This study utilized data from the BMS Database, a prospective, longitudinal, multicenter research study funded by the National Institute on Disability, Independent Living, and Rehabilitation Research.33 The BMS Database was created in 1993 to examine functional and psychosocial outcomes following burn injury. BMS centers applied for and were funded through NIDILRR’s Disability and Rehabilitation Research Projects funding program. BMS center grants fund centers for a five year period, with the most recent cycle funding four centers from 2017–2022.33 The study population included all BMS Database eligible burn survivors aged 18 or older who received acute burn care at a BMS site from January 2015 to December 2019. To be eligible to enroll in the BMS Database during this time period, burn survivors had to receive autografting for wound closure and meet one of the following inclusion criteria:
18–64 years of age with a burn injury ≥20% total body surface area (TBSA) OR
≥65 years of age with a burn injury ≥10% TBSA OR
Any age with a burn injury to their face/neck, hands, or feet OR
Any age with a high-voltage electrical burn injury
For the purposes of this study, the data were divided into two groups: “Enrolled” includes patients who consented and were enrolled into the BMS Database; “Not Enrolled” includes patients who met BMS Database inclusion criteria but did not consent to enroll in the study. A small set of demographic and clinical characteristics are collected for all patients who meet inclusion criteria regardless of final study enrollment status. Written informed consent is obtained from all participants. Each BMS site’s Institutional Review Board approves the study and oversees data collection.
The set of de-identified data collected for all clinically eligible burn survivors includes BMS site, inclusion criteria, age at the time of burn injury, gender (defined as male/female), race, and ethnicity. Importantly, the BMS Database does not account for the gender spectrum and uses the term “gender” to apply to the binary terms female and male (which are usually designated as “sex” terms). In the BMS Database, race is reported in the categories of Black/African American, Asian, Caucasian, American Indian/Alaskan Native, Native Hawaiian or other Pacific Islander, more than one race, and other. For the purposes of analysis, race categories were collapsed into Caucasian, Black/African American, Asian, and Other (American Indian/Alaskan Native, Native Hawaiian or other Pacific Islander, more than one race, and other). Ethnicity is reported as Hispanic/Latino and Not Hispanic/Latino. Race and ethnicity data for unenrolled but eligible patients were added to data collection in 2015. Further details regarding data collection, inclusion criteria, and data sites can be found at http://burndata.washington.edu.33 This study conforms to all STROBE guidelines and reports the required information accordingly (see Supplementary Checklist).
Data Analysis
Descriptive statistics compared demographic and clinical characteristics of the Enrolled and Not Enrolled groups. To assess differences between the two groups, non-parametric Wilcoxon Mann Whitney tests were used for continuous variables (age), with age coded into categories (18–39, 40–59, 60–79, and 80+) to account for non-linearity of the data. Chi-square (gender and ethnicity) and Fisher’s exact tests (race, inclusion criteria, BMS site) were used for categorical variables. Poisson regression analysis was used to evaluate the association between enrollment status and demographic characteristics, controlling for BMS site and inclusion criteria. Adjusted rate ratios (RR) and 95% confidence intervals, robust standard errors and p-values are reported for all variables in the model. A p-value less than 0.05 was considered statistically significant. Model diagnostics examined fit and adequacy of the model. Further, the raw data on race and ethnicity of the BMS Database eligible population was compared to the U.S. population using the 2018 U.S. Census.
A secondary analysis examined whether there were statistical differences between the Enrolled and Not Enrolled groups by race and gender combined as well as ethnicity and gender combined. Rates of enrollment of Black/African American women were compared with White/Caucasian women; an analogous comparison was performed for men. Additionally, rates of enrollment of Hispanic/Latino/a men and women were compared with Not Hispanic/Latino/a men and women. Poisson regression analyses, similar to the main analysis model, examined the association between enrollment status and the intersectional groups described above.
Results
Demographic Characteristics
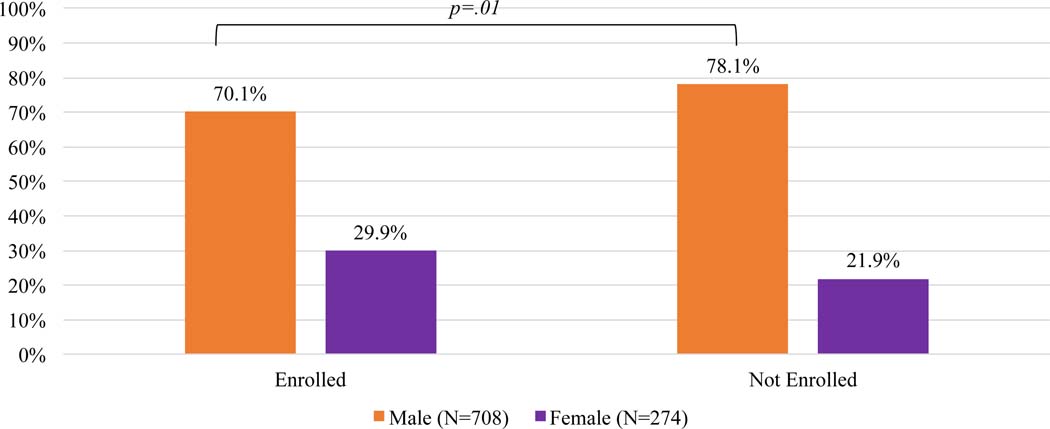
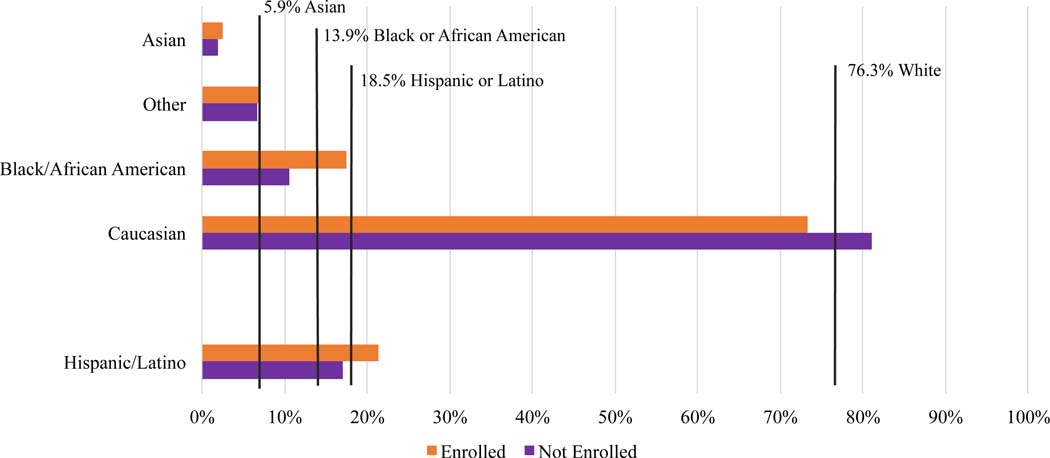
A total of 982 burn survivors age 18–99 years old were eligible for the BMS Database between January 2015 and December 2019 and were included in the study. Of those who were eligible, 708 (72.1%) Enrolled and 274 (27.9%) were Not Enrolled. The Enrolled group was significantly younger (45.8 vs. 48.8 years; p=0.03) with fewer men (70.1% vs. 78.1%; p=0.01) than the Not Enrolled group. (Figure 1) There were no significant differences in race or ethnicity between the Enrolled and Not Enrolled groups. The distribution of BMS site and inclusion criteria were significantly different between the groups (p<0.001). There were more hand/face/feet burns in the Not Enrolled group compared to the Enrolled group (72.3% versus 64.5%; p<0.001). This data is shown in Table 1. Compared to the United States Census, the percentage of the Enrolled BMS Database population is only representative of the U.S. Hispanic/Latino population. (Figure 2)
Figure 1:
Enrolled and Non-Enrolled Participants in the Burn Model System National Database by Gender
Table 1:
Demographic and Clinical Characteristics of Enrolled and Not Enrolled Burn Survivors in the Burn Model System National Database
| Enrolled (n=708) | Not Enrolled (n=274) | p-value | Total Eligible (n=982) | |
|---|---|---|---|---|
| Age at time of burn injury, mean years (SD) | 45.8 (16.2) | 48.8 (18.1) | p=0.03 | |
|
| ||||
| Gender, % male (n) | 70.1 (496) | 78.1 (214) | p=0.01 | 72.3 (710) |
|
| ||||
| Race, % (n) | ||||
| Black/African American | 10.5 (72) | 17.5 (43) | p=0.07 | 12.7 (115) |
| Asian | 1.9 (13) | 2.4 (6) | 2.0 (19) | |
| Caucasian | 81.0 (553) | 73.2 (180) | 78.9 (733) | |
| Other | 6.6 (45) | 6.9 (17) | 6.7 (62) | |
|
| ||||
| Ethnicity, % (n) | ||||
| Hispanic/Latino | 17.0 (115) | 21.3 (34) | p=0.20 | 17.8 (149) |
| Not Hispanic/Latino | 83.0 (563) | 78.8 (126) | 82.2 (689) | |
|
| ||||
| Inclusion criteria, % (n) | ||||
| 10%+ TBSA burned, 65+years | 5.0 (35) | 8.0 (22) | p<0.001 | 5.8 (57) |
| 20%+ TBSA burned, 19–64 years | 24.2 (171) | 17.9 (49) | 22.4 (220) | |
| 20%+ TBSA burned, 0–18 years | 2.3 (16) | 1.5 (4) | 2.0 (20) | |
| Electric/high voltage/lightning | 4.1 (29) | 0.4 (1) | 3.1 (30) | |
| Hand/face/feet burn | 64.5 (456) | 72.3 (198) | 66.7 (654) | |
|
| ||||
| BMS Site | ||||
| A | 32.8 (232) | 22.3 (61) | p<0.001 | 29.8 (293) |
| B | 32.6 (231) | 34.3 (94) | 33.1 (325) | |
| C | 1.6 (11) | 0.4 (1) | 1.2 (12) | |
| D | 33.1 (234) | 43.1 (118) | 35.8 (352) | |
“Other” race includes American Indian, Native Hawaiian or Pacific Islander, more than 1 race, and other Standard Deviation (SD)
Total Body Surface Area (TBSA)
Non-parametric t-tests (Wilcoxon Mann Whitney) was used for age; chi-squared tests were used for gender and ethnicity; Fisher’s exact tests were used for race, inclusion criteria, and BMS site. P-value<0.05 is considered significant and significant values are bolded in the table.
Figure 2:
Racial and Ethnic Demographics of Enrolled and Not Enrolled Burn Survivors in the Burn Model System National Database Compared to the US Census34
Regression Analysis
In the Poisson regression model, Black/African American race and gender were significant predictors of enrollment into the BMS Database (Table 2). Ethnicity and age were not found to be significant predictors of enrollment. Individuals who identified as Black/African American were 0.82 times less likely than those identifying as White/Caucasian (p=0.005) to enroll into the database and female burn survivors were 1.07 times more likely to enroll as male burn survivors (p<0.04). In addition, burn survivors with electrical/high voltage/lightning injury were 1.29 times more likely as those with other burn etiology to enroll (p=0.02). The comparison was with older patients who had greater than 10% total body surface area burns (Table 2). BMS site was not a predictor of enrollment in the BMS Database.
Table 2:
Poisson Regression Assessing Association between Enrollment and Characteristics of the Study Population
| Adjusted Rate Ratios (95% CI) | Robust S.E. | p-value | |
|---|---|---|---|
| Age (compared to 18–39) | |||
| 40–59 years | 1.01 (0.95–1.08) | 0.03 | 0.68 |
| 60–79 years | 0.93 (0.84–1.03) | 0.05 | 0.16 |
| >80 years | 0.77 (0.52–1.15) | 0.16 | 0.20 |
| Gender (compared to male) | |||
| Female | 1.07 (1.00–1.14) | 0.04 | 0.04 |
| Race (compared to White/ Caucasian) | |||
| Black/African American | 0.82 (0.72–0.94) | 0.06 | 0.01 |
| Other | 0.88 (0.77–1.00) | 0.06 | 0.05 |
| Ethnicity (compared to nonHispanic) | |||
| Hispanic/Latino | 0.91 (0.82–1.01) | 0.05 | 0.08 |
| Criteria (compared to 10%+ TBSA burned, 65+ years) | |||
| 20%+ TBSA burned, 19–64 years | 1.08 (0.87–1.34) | 0.12 | 0.47 |
| 20%+ TBSA burned, 0–18 years | 1.13 (0.73–1.74) | 0.25 | 0.59 |
| Electric/ high voltage/ lightning | 1.29 (1.04–1.59) | 0.14 | 0.02 |
| Hand/face/feet burn | 1.10 (1.00–1.14) | 0.11 | 0.36 |
Total Body Surface Area (TBSA)
Analysis also controlled for Burn Model System site
P-value <0.05 is considered statistically significant and significant results are bolded in the table.
Model diagnostics checked the fit and adequacy of the regression model. Overdispersion was ruled out using negative binomial regression as a comparison model. Outlying or high leverage points were also examined; no observations were removed from the model. Robust standard errors were used to control for mild violation of underlying assumptions.
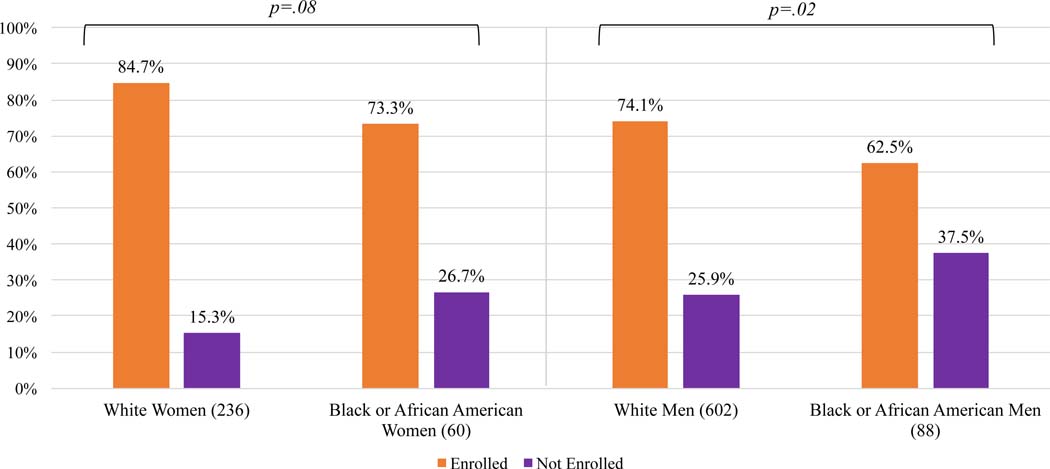
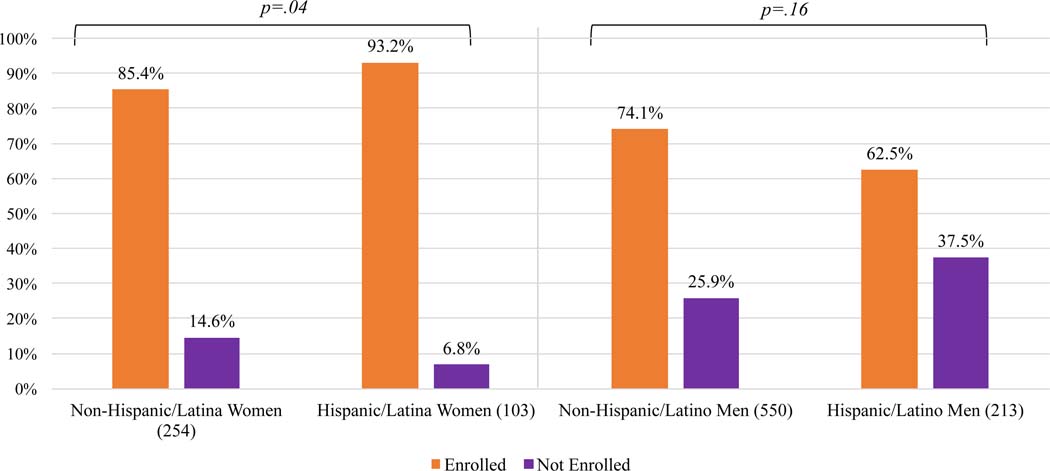
Secondary Analysis
Significantly more White women and men as well as Hispanic/Latina women enrolled in the BMS Database compared to Black/African American women and men and Not Hispanic/Latina women. (Figures 2 and 3) Additionally, regression analyses found that Black/African American women and men were 0.83 and 0.81 times less likely to enroll compared to their White counterparts, respectively. Hispanic/Latino men were 0.75 times less likely to enroll compared to non-Hispanic/Latino men. (Table 3)
Figure 3:
Comparison of Race Among Men and Women Eligible to Participate in the Burn Model System National Database
Table 3:
Poisson Regression Analyses Assessing Association Between Enrollment and a Combination of Race and Gender as well as Ethnicity and Gender
| Adjusted Rate Ratios (95% CI) | Robust S.E. | p-value | |
|---|---|---|---|
| Women (compared to White) | |||
| Black/African American | 0.83 (0.71–0.98) | 0.07 | 0.03 |
| Men (compared to White) | |||
| Black/African American | 0.81 (0.69–0.96) | 0.07 | 0.01 |
| Women (compared to NonHispanic/Latina) | |||
| Hispanic/Latina | 1.00 (0.89–1.21) | 0.06 | 0.98 |
| Men (compared to NonHispanic/Latino) | |||
| Hispanic/Latino | 0.75 (0.58–0.97) | 0.10 | 0.03 |
p-value<0.05 is considered statistically significant and significant results are bolded in the table.
Discussion
It was hypothesized that there would be significant disparities based on race, ethnicity, gender, and age between the patient population that was eligible to be part of the BMS Database and that which enrolled in the Database. After comparing Enrolled and Not Enrolled burn survivors who met clinical eligibility to participate in a lifelong longitudinal study of post-burn outcomes, race and gender were found to be significant predictors of enrollment. Further, an examination of the intersectionality of race and gender as well as ethnicity and gender among the eligible population showed significant findings. Black/African American burn survivors were less likely to enroll than White burn survivors and female burn survivors were more likely to enroll than men. White men and White women were more likely to enroll compared to Black/African American men and women and Hispanic/Latino men were less likely to enroll compared to Not Hispanic/Latino men. Regarding age, while the Enrolled group was younger than the Not Enrolled group, age was not a significant predictor of enrollment in the regression analysis.
In this study, burn survivors meeting inclusion criteria for the BMS Database who are Black/African American were found to be 0.82 times less likely than White individuals to enroll. There is a wealth of literature examining the long-term impacts of historical mistreatment of Black/African Americans in research as well as current health disparities for this population, which has understandably resulted in mistrust of healthcare and research institutions.3,6,34–36 Hispanic/Latino men were 0.75 times less likely to enroll in the BMS Database than Not Hispanic/Latino men. A 2006 review of research studies, however, found nonsignificant differences in consent rates by race and ethnicity indicating that these groups may be just as willing to participate in research when given the opportunity.5 Further, there is evidence that minority burn survivors experience injury-related sequelae differently. Scar quality and healing, for example, has been found to be impacted by skin color and those with darker skin tones often experience worse scar quality.37 Along similar lines, Black/African Americans have also been found to be more likely to develop severe contractures after their burn injury.38 Given these differences, it is important to ensure equal representation of minorities in studies especially those examining the long-term implications of injury.20–22,24,25
Burn survivors identifying as female were 1.07 times more likely than those identifying as male to enroll in the BMS Database. Since females differ in anatomy and physiology from people who are biologically male, there are important reasons why the inclusion of both sexes is important in clinical research. Historically, male participants have been overrepresented in research, so this finding suggests that the BMS Database is capturing those who might have previously been overlooked for a study of this kind.39–41 Within the burn population, female survivors have been shown to have higher mortality compared to their male counterparts.24–26 In addition, burn injuries have been shown to negatively affect women’s overall long-term health and quality of life more than men.28,29,42 Social determinants of health (e.g., socioeconomic factors, geography, education, access to nutritious food) may also be experienced differently by men and women, leading to differences in their outcomes.43,44 Further, when examining intersectional identities by race and gender, female burn survivors who were Black/African American were less likely to enroll than their White counterparts.
Regarding age, the results were mixed. The Enrolled group was significantly younger than the Not Enrolled group, as the average age of the two groups were 45.8 years and 48.8 years, respectively. However, age was not found to be a significant predictor of enrollment when controlling for the other demographic variables as well as inclusion criteria and BMS site in the regression analysis. Given known disparities among elderly injury populations, it is important to ensure equitable inclusion of this population.
Although examining the impact of injury type on enrollment status was not the primary aim of this study, results demonstrated that individuals with electrical injury were found to be 1.29 more likely to enroll as eligible burn survivors over the age of 65 years old with burns size greater than or equal to 10% total body surface area. Electrical injuries are complicated in nature and short-term as well as long-term sequelae have been documented.45–47 There is little evidence to aid in the understanding of why this population is more likely to participate in this study. Electrical injuries are more likely to be experienced by young, White men and it is possible that these individual demographic characteristics impact enrollment more than the type of injury.45 However, the younger age group was not found to be more or less likely than older age groups to enroll in the BMS database.
Disparities in enrollment are likely multifactorial and may be related to the individual participant or the organization conducting the research. Individuals may not want to participate based on concerns for their own safety and/or a mistrust of the healthcare system. On the other hand, structural and organizational unconscious bias is often a factor in various disparities and may impact enrollment. For instance, how much time a healthcare professional spends explaining the enrollment process and benefits may be a factor. If an individual is reluctant to participate for any reason, it may be that additional time is needed to delve into reasons for this and address any concerns. It is important for clinicians and researchers to understand and be able to identify cultural differences among potential participants. Additionally, enrollment may be affected if the process is not presented in someone’s primary language. Health literacy is also an important issue that may contribute to health disparities, including clinical trial enrollment. An Institute of Medicine report titled “Health Literacy: A Prescription to End Confusion” defines the term health literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions”.48 Given the results of this study, there is an opportunity for the BMS to further investigate and address the issues of representativeness in this longitudinal database and consider how this impacts the interpretation of results.
Additionally, subject attrition in a study, whether pre-inclusion or post-inclusion is a significant factor that not only diminishes the generalizability but may also produce bias in study findings. Two previous studies examined post-inclusion participation in the BMS Database and identified sociodemographic risk factors to identify individuals at high risk for attrition, and the resulting potential sources of bias in the database.49,50 The current study goes a step further by examining and comparing eligible-enrolled participants with those eligible but not enrolled in the BMS Database.. Identifying significant factors related to recruitment and retention strategies and materials that are specifically designed for individuals in the longitudinal database. Further, the BMS is currently working to enhance the understanding of recruitment and retention barriers for minority groups by conducting a qualitative study investigating reasons participants choose to enroll in the BMS Database. Using one-on-one, semi-structured interviews, this study will assess barriers and facilitators of participation in research and the outcome of this study will be the development of new or modification of existing recruitment and retention strategies and materials specifically targeted to burn survivors from specific underrepresented groups. In addition, the authors recommend that future research with the BMS Database should consider reporting the limitation that database participants are not necessarily representative of eligible subjects, particularly in terms of race, ethnicity, and gender.
These efforts align with a broader movement within the field of research to ensure the inclusion of underrepresented populations. The NIH has been addressing the inclusion of underrepresented groups in clinical trials for more than a quarter of a century; it recently updated and expanded policies for Inclusion Across the Lifespan and Inclusion of Women and Minorities policies, which outline that studies should not be designed to exclude individuals based on race, ethnicity, gender, or age unless there is a specific scientific or ethical reason to do so.16,17 Similarly, the Health Services and Research Administration states in their 2019–2022 Strategic Plan that the organization will use evidence-based research to address health disparities and the Food and Drug Administration is finalizing a policy statement that enrollment of underrepresented populations in clinical trials should be broadened.18,19 These practices aim to hold researchers accountable for transparency in the design and conduct of research; to ensure studies are fair and equitable; and to guarantee that results address the needs of entire disease populations. Thus, this study fits well into an existing and expanding body of literature that is aimed at ensuring the equitable inclusion of representative patient populations in research.
Study Limitations
An important limitation of this study is the circumscribed number of variables collected on individuals who do not enroll in the BMS Database. Information on socioeconomic status in addition to long-term patient reported outcomes are not collected for those who do not enroll in the study, so it is not possible to compare the two populations beyond basic demographic characteristics and clinical inclusion criteria that are appropriate to collect on unenrolled eligible subjects. Further, we do not have any information on why eligible participants choose not to participate. This information will be collected in the future, however. The BMS Database was created in 1993 and variables used to define race, ethnicity, and gender may not be representative of today’s norms. Race and ethnicity categories are consistent with what is currently used in research studies examining other trauma populations (https://www.tbindsc.org/ and https://www.nscisc.uab.edu/). Gender is consistent with what is currently being used in the National Burn Repository.51 Additionally, the BMS Database is limited in its geographical reach and therefore generalizability to the national burn population with centers in Boston, Massachusetts, Dallas, Texas, Galveston, Texas, and Seattle, Washington. However, the BMS Database has been shown to be representative of the general United States population.52 Due to the format of the inclusion criteria variable, it is not possible to examine burn size as an isolated variable. Finally, the retrospective study design potentially limits the interpretation and generalizability of the results.
Conclusions
In this study, disparities in enrollment in the BMS Database by race, ethnicity, and gender were found. Several groups of minority burn survivors were found to be less likely to enroll than White burn survivors including Black/African American men and women as well as Hispanic/Latino men. Female burn survivors were more likely to enroll than male burn survivors. It is important for clinicians and researchers to recognize that the BMS Database is limited in its representativeness of diverse populations; this should improve the understanding of burn recovery and guide decisions about interventions and resource allocation. The results of the current study underscore issues of transparency, equity, and representativeness of data in the BMS Database and begin to shine a light on these issues in burn and rehabilitation research more generally. More research is needed to determine causality regarding the underrepresentation of various populations in the BMS Database and future efforts are needed to address these disparities.
Figure 4:
Comparison of Ethnicity Among Men and Women Eligible to Participate in the Burn Model System National Database
Acknowledgements:
This work was supported by the National Institute on Disability, Independent Living, and Rehabilitation Research (grant #s 90DPBU0001, 90DPBU0002, 90DBPU0004). NIDILRR is a center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Footnotes
Conflicts of Interest: Dr. Schneider reports grants from NIDILRR during the conduct of the study and grants from NIDILRR and the Dept of Defense outside of the submitted work. Dr. Silver reports grants from Arnold P Gold Foundation and Binational Science Foundation outside of the submitted work. Dr. Ryan reports grants from NIDILRR and Shriner’s Hospitals for Children during the conduct of this study. Dr Zafonte reports receiving royalties from 1) Oakstone for an educational CD- Physical Medicine and Rehabilitation a Comprehensive Review;2) Springer/Demos publishing for serving as co- editor of the text Brain Injury Medicine. Dr Zafonte serves on the Scientific Advisory Board of Myomo, Oxeia Biopharma, ElMINDA and Biodirection. Dr. Gibran, Ms. Carrougher, and Ms. McMullen report grants from NIDILRR during the conduct of this study. No other authors have any conflicts to disclose.
References
- 1.Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94(8):666–668. [PMC free article] [PubMed] [Google Scholar]
- 2.Flores LE, Verduzco-Gutierrez M, Molinares D, Silver JK. Disparities in Health Care for Hispanic Patients in Physical Medicine and Rehabilitation in the United States: A Narrative Review. Am J Phys Med Rehabil. 2020;99(4):338–347. doi: 10.1097/PHM.0000000000001342 [DOI] [PubMed] [Google Scholar]
- 3.Odonkor CA, Esparza R, Flores LE, et al. Disparities in Health Care for Black Patients in Physical Medicine and Rehabilitation in the United States: A Narrative Review. PM R. October 2020. doi: 10.1002/pmrj.12509 [DOI] [PubMed] [Google Scholar]
- 4.Pierce BS, Perrin PB, Pugh M, et al. Racial/Ethnic Disparities in Longitudinal Trajectories of Community Integration After Burn Injury. Am J Phys Med Rehabil. 2020;99(7):602–607. doi: 10.1097/PHM.0000000000001378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wendler D, Kington R, Madans J, et al. Are racial and ethnic minorities less willing to participate in health research? PLoS Med. 2006;3(2):e19. doi: 10.1371/journal.pmed.0030019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underserved. 2010;21(3):879–897. doi: 10.1353/hpu.0.0323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson EE, Neighbors HW, Munday C, Jackson JS. Recruitment and retention of African American patients for clinical research: an exploration of response rates in an urban psychiatric hospital. J Consult Clin Psychol. 1996;64(5):861–867. doi: 10.1037//0022-006x.64.5.861 [DOI] [PubMed] [Google Scholar]
- 8.Bartlett C, Davey P, Dieppe P, Doyal L, Ebrahim S, Egger M. Women, older persons, and ethnic minorities: factors associated with their inclusion in randomised trials of statins 1990 to 2001. Heart. 2003;89(3):327–328. doi: 10.1136/heart.89.3.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kressin NR, Meterko M, Wilson NJ. Racial disparities in participation in biomedical research. J Natl Med Assoc. 2000;92(2):62–69. [PMC free article] [PubMed] [Google Scholar]
- 10.George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(2):e16–31. doi: 10.2105/AJPH.2013.301706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farmer DF, Jackson SA, Camacho F, Hall MA. Attitudes of African American and low socioeconomic status white women toward medical research. J Health Care Poor Underserved. 2007;18(1):85–99. doi: 10.1353/hpu.2007.0008 [DOI] [PubMed] [Google Scholar]
- 12.BeLue R, Taylor-Richardson KD, Lin J, et al. African Americans and participation in clinical trials: differences in beliefs and attitudes by gender. Contemp Clin Trials. 2006;18(1):85–99. doi: 10.1016/j.cct.2006.08.001 [DOI] [PubMed] [Google Scholar]
- 13.McMurdo MET, Witham MD, Gillespie ND. Including older people in clinical research. BMJ. 2005;331(7524):1036–1037. doi: 10.1136/bmj.331.7524.1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mody L, Miller DK, McGloin JM, et al. Recruitment and retention of older adults in aging research. J Am Geriatr Soc. 2008;56(12):2340–2348. doi: 10.1111/j.1532-5415.2008.02015.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herrera AP, Snipes SA, King DW, Torres-Vigil I, Goldberg DS, Weinberg AD. Disparate inclusion of older adults in clinical trials: priorities and opportunities for policy and practice change. Am J Public Health. 2010;100 Suppl(Suppl 1):S105–12. doi: 10.2105/AJPH.2009.162982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inclusion of Women and Minorities as Participants in Research Involving Human Subjects | grants.nih.gov.. https://grants.nih.gov/policy/inclusion/women-and-minorities.htm. Accessed September 23, 2020.
- 17.Inclusion Across the Lifespan | grants.nih.gov. https://grants.nih.gov/policy/inclusion/lifespan.htm. Accessed September 23, 2020.
- 18.(No Title). https://www.hrsa.gov/sites/default/files/hrsa/about/strategic-plan/hrsa-strategic-plan.pdf. Accessed September 23, 2020.
- 19.Enhancing the Diversity of Clinical Trial Populations — Eligibility Criteria, Enrollment Practices, and Trial Designs Guidance for Industry | FDA. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enhancing-diversity-clinical-trial-populations-eligibility-criteria-enrollment-practices-and-trial. Accessed September 23, 2020.
- 20.Peck MD. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns. 2011;37(7):1087–1100. doi: 10.1016/j.burns.2011.06.005 [DOI] [PubMed] [Google Scholar]
- 21.Chen JH, Nosanov LB, Carney BC, Vigiola Cruz M, Moffatt LT, Shupp JW. Patient and social characteristics contributing to disparities in outcomes after burn injury: application of database research to minority health in the burn population. Am J Surg. 2018;216(5):863–868. doi: 10.1016/j.amjsurg.2018.01.028 [DOI] [PubMed] [Google Scholar]
- 22.Fagenholz PJ, Sheridan RL, Harris NS, Pelletier AJ, Camargo CAJ. National study of Emergency Department visits for burn injuries, 1993 to 2004. J Burn care Res Off Publ Am Burn Assoc. 2007;28(5):681–690. doi: 10.1097/BCR.0B013E318148C9AC [DOI] [PubMed] [Google Scholar]
- 23.Edelman LS. Social and economic factors associated with the risk of burn injury. Burns. 2007;33(8):958–965. doi: 10.1016/j.burns.2007.05.002 [DOI] [PubMed] [Google Scholar]
- 24.Bedri H, Romanowski KS, Al-Ramahi G, et al. A national study of the effect of race, socioeconomic status, and gender on burn outcomes. J Burn Care Res. 2017;38(3):161–168. doi: 10.1097/BCR.0000000000000416 [DOI] [PubMed] [Google Scholar]
- 25.Murphy S, Clark DE, Carter DW. Racial disparities exist among burn patients despite insurance coverage. Am J Surg. 2019;218(1):47–50. doi: 10.1016/j.amjsurg.2018.08.013 [DOI] [PubMed] [Google Scholar]
- 26.Kerby JD, McGwin GJ, George RL, Cross JA, Chaudry IH, Rue LW 3rd. Sex differences in mortality after burn injury: results of analysis of the National Burn Repository of the American Burn Association. J Burn Care Res. 2006;27(4):452–456. doi: 10.1097/01.BCR.0000225957.01854.EE [DOI] [PubMed] [Google Scholar]
- 27.Lawrence JW, Mason ST, Schomer K, Klein MB. Epidemiology and impact of scarring after burn injury: a systematic review of the literature. J Burn Care Res. 2012;33(1):136–146. doi: 10.1097/BCR.0b013e3182374452 [DOI] [PubMed] [Google Scholar]
- 28.Al Ghriwati N, Sutter M, Pierce BS, Perrin PB, Wiechman SA, Schneider JC. Two-Year Gender Differences in Satisfaction With Appearance After Burn Injury and Prediction of Five-Year Depression: A Latent Growth Curve Approach. Arch Phys Med Rehabil. 2017;98(11):2274–2279. doi: 10.1016/j.apmr.2017.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levi B, Kraft CT, Shapiro GD, et al. The Associations of Gender With Social Participation of Burn Survivors: A Life Impact Burn Recovery Evaluation Profile Study. J Burn Care Res. 2018;39(6):915–922. doi: 10.1093/jbcr/iry007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abu-Sittah GS, Chahine FM, Janom H. Management of burns in the elderly. Ann Burns Fire Disasters. 2016;29(4):249–245. [PMC free article] [PubMed] [Google Scholar]
- 31.Jeschke MG, Peck MD. Burn Care of the Elderly. J Burn care Res Off Publ Am Burn Assoc. 2017;38(3):e625–e628. doi: 10.1097/BCR.0000000000000535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pham TN, Carrougher GJ, Martinez E, et al. Predictors of Discharge Disposition in Older Adults With Burns: A Study of the Burn Model Systems. J Burn care Res Off Publ Am Burn Assoc. 2015;36(6):607–612. doi: 10.1097/BCR.0000000000000216 [DOI] [PubMed] [Google Scholar]
- 33.Goverman J, Mathews K, Holavanahalli RK, et al. The National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Twenty Years of Contributions to Clinical Service and Research. J Burn Care Res. 2017;38(1):e240–e253. doi: 10.1097/BCR.0000000000000361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hughes TB, Varma VR, Pettigrew C, Albert MS. African Americans and Clinical Research: Evidence Concerning Barriers and Facilitators to Participation and Recruitment Recommendations. Gerontologist. 2017;57(2):348–358. doi: 10.1093/geront/gnv118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC); 2003. doi: 10.17226/12875 [DOI] [PubMed] [Google Scholar]
- 36.Warren RC, Forrow L, Hodge DAS, Truog RD. Trustworthiness before Trust - Covid-19 Vaccine Trials and the Black Community. N Engl J Med. 2020;383(22):e121. doi: 10.1056/NEJMp2030033 [DOI] [PubMed] [Google Scholar]
- 37.Wallace HJ, Fear MW, Crowe MM, Martin LJ, Wood FM. Identification of factors predicting scar outcome after burn in adults: A prospective case-control study. Burns. 2017;43(6):1271–1283. doi: 10.1016/j.burns.2017.03.017 [DOI] [PubMed] [Google Scholar]
- 38.Goverman J, Mathews K, Goldstein R, et al. Adult Contractures in Burn Injury: A Burn Model System National Database Study. J Burn Care Res. 2017;38(1):e328–e336. doi: 10.1097/BCR.0000000000000380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woitowich NC, Beery A, Woodruff T. A 10-year follow-up study of sex inclusion in the biological sciences. Elife. 2020;9. doi: 10.7554/eLife.56344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu KA, Mager NAD. Women’s involvement in clinical trials: historical perspective and future implications. Pharm Pract (Granada). 2016;14(1):708. doi: 10.18549/PharmPract.2016.01.708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Duma N, Vera Aguilera J, Paludo J, et al. Representation of Minorities and Women in Oncology Clinical Trials: Review of the Past 14 Years. J Oncol Pract. 2018;14(1):e1–e10. doi: 10.1200/JOP.2017.025288 [DOI] [PubMed] [Google Scholar]
- 42.Chin TL, Carrougher GJ, Amtmann D, et al. Trends 10 years after burn injury: A Burn Model System National Database study. Burns. 2018;44(8):1882–1886. doi: 10.1016/j.burns.2018.09.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vlassoff C. Gender differences in determinants and consequences of health and illness. J Health Popul Nutr. 2007;25(1):47–61. [PMC free article] [PubMed] [Google Scholar]
- 44.Regitz-Zagrosek V. Sex and gender differences in health. Science & Society Series on Sex and Science. EMBO Rep. 2012;13(7):596–603. doi: 10.1038/embor.2012.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maghsoudi H, Adyani Y, Ahmadian N. Electrical and lightning injuries. J Burn care Res Off Publ Am Burn Assoc. 2007;28(2):255–261. doi: 10.1097/BCR.0B013E318031A11C [DOI] [PubMed] [Google Scholar]
- 46.Dokov W. Assessment of risk factors for death in electrical injury. Burns. 2009;35(1):114–117. doi: 10.1016/j.burns.2008.05.005 [DOI] [PubMed] [Google Scholar]
- 47.Stockly OR, Wolfe AE, Espinoza LF, et al. The impact of electrical injuries on long-term outcomes: A Burn Model System National Database study. Burns. 2020;46(2):352–359. doi: 10.1016/j.burns.2019.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Institute of Medicine. Health Literacy: A Prescription to End Confusion. (Nielsen-Bohlman L, Panzer AM, Kindig DA, eds.). Washington, DC: The National Academies Press; 2004. doi: 10.17226/10883 [DOI] [PubMed] [Google Scholar]
- 49.Holavanahalli RK, Lezotte DC, Hayes MP, et al. Profile of patients lost to follow-up in the burn injury rehabilitation model systems’ longitudinal database. J Burn Care Res. 2006;27(5):703–712. doi: 10.1097/01.BCR.0000238085.87863.81 [DOI] [PubMed] [Google Scholar]
- 50.Bamer AM, McMullen K, Gibran N, et al. Factors Associated with Attrition of Adult Participants in a Longitudinal Database: A National Institute on Disability, Independent sLiving, and Rehabilitation Research Burn Model System Study. J Burn Care Res. 2020;41(2):270–279. doi: 10.1093/jbcr/irz186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.American Burn Association NBR Advisory Committee. National Burn Repository 2017 Update. 2017;13(312). [Google Scholar]
- 52.Lezotte DC, Hills RA, Heltshe SL, et al. Assets and Liabilities of the Burn Model System Data Model: A Comparison With the National Burn Registry. Arch Phys Med Rehabil. 2007;88(12 SUPPL. 2). doi: 10.1016/j.apmr.2007.09.011 [DOI] [PubMed] [Google Scholar]