Abstract
By virtue of their regulatory role in various metabolic and biosynthetic pathways for energy status and cellular integrity, both hydro-soluble and lipo-soluble vitamins are considered to be involved in maintaining cardiovascular function in health and disease. Deficiency of some vitamins such as vitamin A, B6, folic acid, C, D, and E has been shown to be associated with cardiovascular abnormalities whereas supplementation with these vitamins has been claimed to reduce cardiovascular risk for hypertension, atherosclerosis, myocardial ischemia, arrhythmias, and heart failure. However, the data from several experimental and clinical studies for the pathogenesis of cardiovascular disease due to vitamin deficiency as well as therapy due to different vitamins are conflicting. In this article, we have attempted to review the existing literature on the role of different vitamins in cardiovascular disease with respect to their deficiency and supplementation in addition to examining some issues regarding their involvement in heart disease. Although both epidemiological and observational studies have shown some merit in the use of different antioxidant vitamins for the treatment of cardiovascular disorders, the results are not conclusive. Furthermore, in view of the complexities in the mechanisms of different cardiovascular disorders, no apparent involvement of any particular vitamin was seen in any specific cardiovascular disease. On the other hand, we have reviewed the evidence that deficiency of vitamin B6 promoted KCl-induced Ca2+ entry and reduced ATP-induced Ca2+-entry in cardiomyocytes in addition to decreasing sarcolemmal (SL) ATP binding. The active metabolite of vitamin B6, pyridoxal 5′-phosphate, attenuated arrhythmias due to myocardial infarction (MI) as well as cardiac dysfunction and defects in the sarcoplasmic reticulum (SR) Ca2+-transport in the ischemic-reperfused hearts. These observations indicate that both deficiency of some vitamins as well as pretreatments with different vitamins showing antioxidant activity affect cardiac function, metabolism and cation transport, and support the view that antioxidant vitamins or their metabolites may be involved in the prevention rather than the therapy of cardiovascular disease.
Keywords: cardiovascular diseases, vitamin deficiency, vitamin supplements, cardiac dysfunction, cardiac arrhythmias, metabolic abnormalities, oxidative stress
Introduction
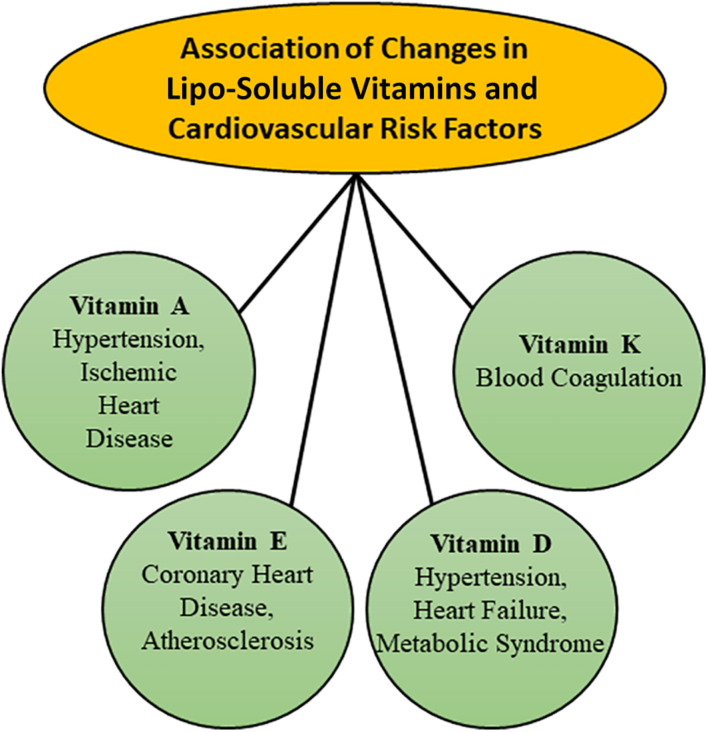
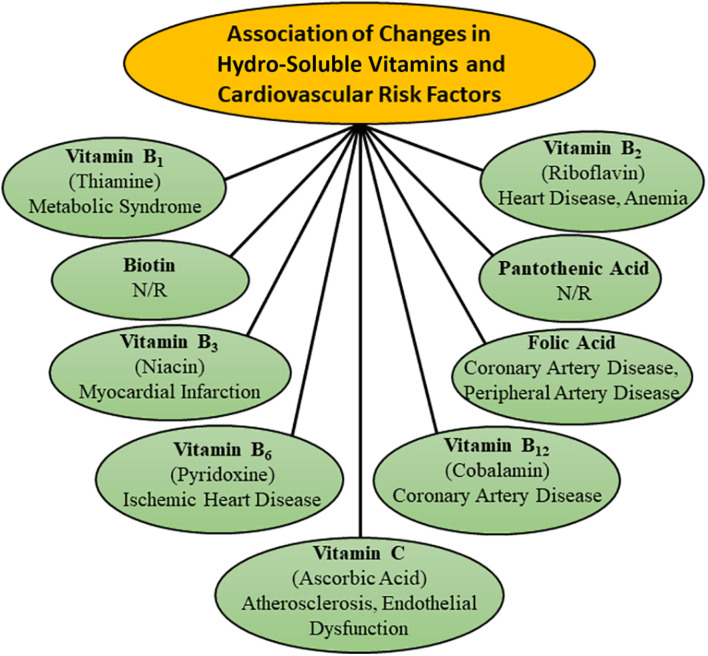
It is now well known that malnutrition over a prolonged period is one of the major factors, which is associated with the development of heart disease and thus a balanced diet with respect to proteins, carbohydrates and lipids is essential for maintaining cardiovascular health (Ivey, 1979; Farrell, 1980; Alpers et al., 1983; Young and Solomons, 1983; National Research Council (US) Committee on Diet and Health, 1989). It is also known that various proteins, carbohydrates and lipids are metabolized through different but interlinked metabolic pathways in the body for maintaining the integrity and structure of all components of the cardiovascular system as well as providing the required energy for their function. Since both lipo-soluble and hydro-soluble vitamins have been demonstrated to be intimately involved in the regulation of different metabolic processes for cellular biosynthesis and energy production, alterations in their amount are considered to result in cardiovascular abnormalities. It is pointed out that some lipo-soluble vitamins such as A, D, and E, as well as hydro-soluble vitamins such as B6 (pyridoxine), B9 (folic acid), and C have been reported to play a major role in modulating the cardiovascular function (Chasan-Taber et al., 1996; Palace et al., 1999; Pryor, 2000; Friso et al., 2004; Nemerovski et al., 2009; Moser and Chun, 2016; Stanhewicz and Kenney, 2017; Bilagi, 2018). The implications of changes in both lipo-soluble and hydro-soluble vitamins in different types of cardiovascular diseases such as hypertension, atherosclerosis, ischemic heart disease and heart failure have been depicted in Figures 1, 2, respectively. Although plasma concentrations of most vitamins stay within normal limits in healthy animals and human subjects, deficiencies of both lipo-soluble and hydro-soluble vitamins have been observed in patients with different types of heart disease (Swain and St Clair, 1997; Saremi and Arora, 2010; Pilz et al., 2011; Pawlak, 2015; Eshak and Arafa, 2018; Song and Kang, 2018; Balasubramanian et al., 2019). Thus, various vitamins are commonly recommended for the promotion of cardiovascular health.
FIGURE 1.
Associations of changes in plasma concentration of different lipo-soluble vitamins with various risk factors for the development of cardiovascular disease.
FIGURE 2.
Association of changes in plasma concentration of different hydro-soluble vitamins with various risk factors for the development of cardiovascular disease. N/R- not related.
Several experimental and observational studies have revealed usefulness of different vitamins in cardiovascular disease (Gale et al., 1995; Wilcken and Wilcken, 1998; Zittermann and Koerfer, 2008; Gori and Münzel, 2011; McGreevy and Williams, 2011; Rafnsson et al., 2011; Czeizel et al., 2013; Dosedel et al., 2021). Links between different vitamins and cardiovascular disease have been established on the basis of their effects on changes in the levels of oxidative stress, inflammation, homocysteine, lipoproteins, and nitric oxide (Rimm et al., 1993; Stanger et al., 2004; Mozos and Marginean, 2015; Farhangi et al., 2017; Stanhewicz and Kenney, 2017; Bartekova et al., 2021). Although both lipo-soluble and hydro-soluble vitamins do not exert direct actions on cardiovascular function, these are considered to affect different cardiovascular diseases upon modulating their respective risk factors. However, their beneficial effects are inconclusive and particularly, the results of various clinical trials for the treatment of heart disease with different vitamins have been disappointing (Olson, 1973; Kushi et al., 1996; Palumbo et al., 2000; Yusuf et al., 2000; Pruthi et al., 2001; Kim et al., 2002; Myung et al., 2013; Ingles et al., 2020). Thus, in view of the uncertainty of demonstrated beneficial cardiovascular effects of different vitamins, the American Heart Association has recommended consumption of vitamin-rich fresh fruits and vegetables instead of vitamins supplements.
It is pointed out that the pathogenesis of different types of cardiovascular diseases is a complex problem and molecular targets of various vitamins may be different for their effectiveness in health and disease. This article is therefore intended to analyze the existing literature to establish if there exists any relationship between a specific vitamin and a specific type of heart disease under conditions of vitamin deficiency or vitamin supplementation. Furthermore, the role of various vitamins will be examined by describing the pathophysiology of heart disease as a consequence of vitamin deficiency. In addition, evidence will be provided to emphasize the potential involvement of various vitamins in the prevention of cardiovascular abnormalities. Since oxidative stress plays a critical role in the development of cardiovascular disease and different vitamins are known to possess antioxidant activity (Dhalla et al., 2000a; Maulik and Kumar, 2012; Neri et al., 2015; van der Pol et al., 2019; Adameova et al., 2020; Bartekova et al., 2021; Ramachandra et al., 2021), the beneficial effects of different vitamins will be evaluated in association with some parameters of oxidative stress.
Vitamin Deficiency and Cardiovascular Disease
Because of the availability of most vitamins in diet including fruits, vegetables, dairy products and meat preparations, vitamin deficiency is usually not observed in healthy subjects. On the other hand, low levels of some vitamins have been detected in both men and women during the development of different types of cardiovascular abnormalities such as hypertension, atherosclerosis, diabetes, ischemic heart disease, heart failure, and stroke. However, the cause-effects of vitamin deficiency and cardiovascular disease are far from clear. Since lipo-soluble vitamins are stored in different tissues, their levels are not easily depleted whereas hydro-soluble vitamins are readily excreted from the body via the renal system. The following discussion is therefore focused on the deficiencies of only some vitamins and their associations with cardiovascular disease.
Hydro-Soluble Vitamin Deficiency
Deficiencies of different vitamins such as vitamin B1, B2, and B6 were seen in patients with heart failure in association with depletion of energy stores (Keith et al., 2009). Vitamin B1 deficiency has also been associated with cardiovascular disease risk factor such as diabetes, dyslipidemia, obesity, and vascular inflammation (Eshak and Arafa, 2018). Depletion of vitamin B2 in cardiovascular disease was associated with anemia and elevated concentrations of homocysteine (Powers, 2003; Balasubramanian et al., 2019). Increased concentrations of homocysteine in patients with coronary artery and peripheral artery diseases were also observed in association with deficiency of vitamins B6 and B12 (Robinson et al., 1998; Wilcken and Wilcken, 1998). Low levels of vitamin B12 and endothelial dysfunction were detected in patients with diabetes, atherosclerosis, myocardial infarction and stroke (Rafnsson et al., 2011; Woo et al., 2014; Pawlak, 2015). Folic acid deficiency has also been shown to occur in vascular disorders as well as congenital heart disease (Swain and St Clair, 1997; Czeizel et al., 2013; Stanhewicz and Kenney, 2017). In addition, deficiency of vitamin B6 has been observed in hypertension, atherosclerosis and coronary artery disease (Kok et al., 1989; Chasan-Taber et al., 1996; Herzlich, 1996; Lal et al., 1996). In fact, the animals kept on vitamin B6 deficient diet were found to show atherosclerosis (Rinehart and Greenberg, 1949), coronary artery disease (Murray et al., 1978), hypertension (Paulose et al., 1988) and increased sympathetic activity (Viswanathan et al., 1990). Cardiomyocytes obtained from B6 deficient rats (Dakshinamurti et al., 1998) showed a marked augmentation of KCl-induced increase in [Ca2+]i without any changes in the basal level of [Ca2+]i (Table 1). On the other hand, ATP-induced increase in [Ca2+]i in cardiomyocytes was depressed due to vitamin B6 deficiency and this change was associated with a decrease in sarcolemmal (SL) ATP binding (Table 1). Such alterations in cardiomyocytes from B6 deficient animals can be considered to support the view that vitamin B6 deficiency may be a risk factor for the development of some cardiovascular disorders.
TABLE 1.
KCl-induced and ATP-induced changes in [Ca2+]i in cardiomyocytes and sarcolemmal (SL) ATP binding in vitamin B6 deficient rats.
| Parameters | Control | Vitamin B6 deficient | Vitamin B6 treated |
| A. Cardiomyocytes [Ca2+]i | |||
| Basal [Ca2+]i, nM | 121 ± 8.6 | 118 ± 4.4 | 123 ± 6.4 |
| Increase in [Ca2+]i due to 30 mM to KCl, nM | 86 ± 5.1 | 129 ± 8.1* | 88 ± 5.5† |
| Increase in [Ca2+]i due to 100 μM ATP, nM | 69 ± 4.7 | 33 ± 4.5* | 64 ± 4.2† |
| Increase in [Ca2+]i due to 10 μM ATP, nM | 37 ± 5.8 | 12 ± 3.6* | – |
| B. SL ATP binding | |||
| ATP binding at 2 nM ATP, pmol/μg protein | 3.2 ± 0.25 | 2.3 ± 0.17* | – |
| ATP binding at 10 nM ATP, pmol/μg protein | 14.0 ± 0.89 | 9.1 ± 1.2* | – |
Control and vitamin B6 deficient rats were fed vitamin B6-containing or vitamin B6-deficient diet for 8 weeks before isolating cardiomyocytes or sarcolemma from the heart. For vitamin B6 treated group, 8 weeks vitamin B6-deficient rats were injected pyridoxin hydrochloride (10 mg/kg; i.p.) 24 h before the experiment. The data are taken from our paper (Dakshinamurti et al., 1998). *P < 0.05 vs. control; †P < 0.05 vs. vitamin B6 deficient group.
Although low levels of plasma vitamin C due to its decreased intake have been reported to be associated with high risk of cardiovascular disease (Ye and Song, 2008; Wang et al., 2013), the relationship between the plasma levels of vitamin C and risk for cardiovascular events is not clear at present. The risk of coronary artery in women was found to increase due to vitamin C deficiency (Osganian et al., 2003) probably as a consequence of increased oxidation of low-density lipoproteins and development of atherosclerosis (Palinski et al., 1989; Yla-Herttuala et al., 1989). On the other hand, vitamin C deficiency in elderly people was related to the risk of death from stroke rather than from the coronary artery disease (Gale et al., 1995). Nonetheless, some investigators in a population study of men observed a significant relationship between vitamin C deficiency and risk of acute myocardial infarction (NyyssOnen et al., 1997). It should be pointed out that high sensitivity of C-reactive proteins and vitamin C deficiency were seen to occur during the development of heart failure in adults (Song and Kang, 2018). Furthermore, by virtue of its antioxidant effect (Knekt et al., 2004; Bartekova et al., 2021) plasma level of vitamin C has been reported to predict the incidence of heart failure (Pfister et al., 2011).
Lipo-Soluble Vitamin Deficiency
Since vitamin D deficiency is the most common nutritional problem, extensive research efforts have been made to understand its relationship with cardiovascular disorders as well as mechanisms of its impact on cardiovascular function. Several investigators have emphasized that vitamin D deficiency plays a critical role in the pathogenesis of cardiovascular disease including hypertension, heart failure and ischemic heart disease (Wang et al., 2008; Judd and Tangpricha, 2009; Agarwal et al., 2011; Kheiri et al., 2018; Latic and Erben, 2020). It is noteworthy that congestive heart failure in vitamin D deficiency was associated with impaired systolic and diastolic functions, hypertension, and peripheral vascular disease (Kheiri et al., 2018). Low levels of vitamin D were observed to favor the development of atherosclerosis and myocardial infarction as a consequence of inflammation, autoimmunity, endothelial dysfunction, formation of foam cells, and proliferation of smooth muscle cells (Welles et al., 2014; Mozos and Marginean, 2015; Gominak, 2016). Vitamin D deficiency has also been associated with diabetes, obesity, dyslipidemia, metabolic syndrome, and hypertension (Zittermann, 2006; Perez-Castrillon et al., 2007; Muscogiuri et al., 2017). Both diabetes and hypertension as a consequence of vitamin D deficiency were related to the development of insulin resistance, elevated levels of parathyroid hormone, activation of renin-angiotensin system, abnormal nitric oxide regulation as well as increased oxidative stress and inflammatory pathway (Ku et al., 2013; Sziva et al., 2020; de la Guia-Galipienso et al., 2021). The involvement of vitamin D deficiency in cardiovascular disease is supported by experimental studies showing myocardial hypertrophy, arterial hypertension and increased activity of the renin-angiotensin system in vitamin D receptor knockout mice (Pilz et al., 2011).
Unlike deficiencies of other nutrients, vitamin E deficiency in human is rare because of the sufficient consumption of commonly available food (Olson, 1973; Pruthi et al., 2001). However, in infants and people with fat malabsorption or some genetic conditions, vitamin E deficiency has been recognized (Oski and Barness, 1969; Traber, 1999). On the other hand, varying degrees of anemia, myocardial cell damage, and cardiomyopathy due to vitamin E deficiency have been observed in various species of animals (Madsen et al., 1933; Gullickson, 1949; Gatz and Houchin, 1951; MacKenzie and MacKenzie, 1953; Fitch, 1968). Rabbits fed on vitamin E deficient diet showed several electrocardiographic abnormalities; these alterations in the heart were accompanied by a reduction in high energy phosphate and glycogen stores (Mulder et al., 1954). Heart failure associated with marked metabolic changes were also seen in animals maintained on vitamin E deficient diet (Lu et al., 1941; Gullickson and Calverley, 1946; Draper et al., 1952; Fedelesova et al., 1971). In addition, marked alterations in SL Na+-K+ ATPase and sarcoplasmic reticular (SR) Ca2+-pump ATPase as well as SR Ca2+-uptake and Ca2+-release activities were decreased in vitamin E deficient rat heart (Fedelesova et al., 1971). It should be mentioned that cardiac abnormalities due to vitamin E deficiency were accompanied by muscular dystrophy (Grigoreva and Medovar, 1959; Read and Nehorayan, 1959; Dhalla et al., 1971; Fedelesova et al., 1971). In view of the antioxidant activity of vitamin E (Bartekova et al., 2021), it is likely that the cardiac abnormalities seen in experimental animals due to vitamin E deficiency are due to the development of increased levels of oxidative stress.
Vitamin Supplementation and Cardiovascular Disease
Excellent reviews for the management of cardiovascular disease by various vitamins are available in the literature (Olson, 1973; Palace et al., 1999; Stanger et al., 2004; Moser and Chun, 2016; Georgiopoulos et al., 2017). However, the results regarding the supplementation of these nutrients in both animals and human subjects with heart disease are not conclusive. Several epidemiological and observational studies as well as animal experimentations support the use of different vitamins in diverse cardiovascular disorders but well controlled clinical studies have failed to observe their beneficial effects in any of the cardiovascular diseases. It should be noted that most of the randomized clinical trials with vitamins have been carried out to determine the therapeutic aspect of their effectiveness in delaying the progression or reducing the extent of cardiovascular diseases but much effort has not been devoted to investigate their actions in depressing the incidence of disease development. Furthermore, most of these investigations may not have employed the optimal dose of a specific vitamin for a specific disease. Thus, it is difficult to interpret such results with respect to the beneficial effects of different vitamins for the prevention or treatment of any cardiovascular disease.
Hydro-Soluble Vitamin Supplementation
Different B vitamins have been observed to show beneficial effects in preventing various cardiovascular diseases. Higher intake of vitamin B6, B12, folic acid, and riboflavin were found to decrease the risk of hypertension and lower the blood pressure in patients with hypertension (Liu et al., 2017, 2018; Psara et al., 2020). Vitamins B such as riboflavin, thiamine, folic acid as well as vitamin B6 and vitamin B12 have also been found useful in clinical trials for the management of heart failure (Witte et al., 2005; Azizi-Namini et al., 2012; van der Pol et al., 2019). Administration of both folic acid and vitamin B12 were reported to attenuate the isoproterenol-induced myocardial cell damage, as well as lower the homocysteine and oxidative stress levels in hyperhomocysteinemic rats (Hagar, 2002). Folic acid also reversed the endothelial dysfunction due to depletion of tetrahydrobiopterin in rabbit aortic rings (Moat et al., 2006). In fact, folic acid supplementation has also been shown to improve the endothelial dysfunction in patients with cardiovascular disease (Stanhewicz and Kenney, 2017).
Prevention of cardiovascular diseases by B vitamins may be associated with the treatment of hypertriglyceridemia as niacin was observed to decrease total cholesterol and triglycerides (Feingold, 2000). Vitamin B complex containing B1, B2, and B6 as well as vitamin B12 and folic acids were found to reduce atherosclerosis and ischemic heart disease by their anti-inflammatory actions (Hodzic, 2018). Both folic acid and vitamin B12 have been reported to delay the early onset of coronary artery disease by reducing plasma homocysteine levels (Pancharuniti et al., 1994). Furthermore, folic acid and antioxidant vitamins reduced the risk of endothelial dysfunction in patients with coronary artery disease (Title et al., 2000; Long et al., 2020). Administration of folic acid as well as vitamin B6 and B12 reversed the endothelial dysfunction in patient with hyperhomocysteinemia due to methionine loading (Haynes, 2002), In fact, treatment of hyperhomocysteinemia with these vitamins is considered to be the mainstay therapy (Guthikonda and Haynes, 2006). However, it should be pointed out that meta-analysis of data from several clinical trials with vitamin B6, vitamin B12, and folic acid did not show any evidence of their protective effects for the progression of atherosclerosis (Bleys et al., 2006).
It should be pointed out that pyridoxal 5′-phosphate (PLP), an active metabolite of vitamin B6, was shown to possess excellent potentials for the treatment of ischemic heart disease (Serfontein et al., 1985; Ellis and McCully, 1995; Dhalla et al., 2000a; Kandzari et al., 2005; Dhalla et al., 2013). In this regard, it is noteworthy that PLP was found to prevent the formation of oxyradicals and lipid peroxidation due to H2O2 (Kannan and Jain, 2004). Furthermore, this agent was shown to depress ATP-induced increase in [Ca2+]i in cardiomyocytes as well as SL ATP-binding (Wang et al., 1999). Not only did PLP reduced the I/R-induced cardiac dysfunction, it was also observed to reduce infarct size (Dhalla et al., 2000b; Kandzari et al., 2005). Administration of PLP was shown to decrease ischemia injury in patients subsequent to coronary angioplasty and coronary bypass surgery (Kandzari et al., 2003; Tardif et al., 2007). However, PLP did not show beneficial effects in a large clinical trial in high risk patients undergoing coronary artery bypass graft surgery (Carrier et al., 2008; Mehta et al., 2008). While the exact reasons for the failure of PLP in preventing different cardiovascular events in advanced ischemic heart disease are not clear, pretreatment of animals with PLP has been demonstrated (Dhalla et al., 2013) to attenuate arrhythmias, incidence of ventricular tachycardia and mortality (Table 2) due to myocardial infarction (MI). In addition, I/R-induced cardiac dysfunction as well as changes in SR Ca2+-uptake and Ca2+-release activities (Table 3) were prevented by pretreatment of rats with PLP (Dhalla et al., 2013). Thus, in view of these observations, it is evident that PLP may prove beneficial in the prevention rather that the therapy of ischemic heart disease.
TABLE 2.
Effects of vitamin B6 and its metabolite, pyridoxal 5′-phosphate (PLP) on myocardial infarction (MI) induced arrhythmias and mortality in rats.
| Parameters | Untreated MI | Vitamin B6 treated MI | PLP treated MI |
| ST segment, mV | 0.18 ± 0.02 | 0.19 ± 0.01 | 0.10 ± 0.02* |
| QTc interval, ms | 554 ± 26 | 566 ± 31 | 437 ± 22* |
| Time of onset of arrhythmias, s | 45 ± 9.6 | 47 ± 8.4 | 125 ± 11.2* |
| Number of PVC, % | 5.0 | 5.2 | 1.4* |
| Incidence of ventricular tachycardia, % | 67 | 61 | 12* |
| Mortality within first day of MI, % | 35 | 30 | 16* |
Treatment of rats with or without vitamin B6 (50 mg/kg, daily) or PLP (25 mg/kg, daily) was started 2 days before inducing MI by occluding the coronary artery. The electrocardiographic changes in ST segment, QTc interval, and PVC (premature ventricular contraction) and mortality were monitored during the first day of inducing MI. The data are taken from our paper (Dhalla et al., 2013). *P < 0.05 vs. untreated group.
TABLE 3.
Effects of vitamin B6 metabolite, pyridoxal 5′-phosphate (PLP), on cardiac function and sarcoplasmic reticular (SR) Ca2+-transport in rat hearts subjected to ischemia-reperfusion (I/R).
| Parameters | Control | Untreated I/R | 25 μM PLP treated I/R |
| A. Cardiac function | |||
| LVDP, mm Hg | 118 ± 5.4 | 39 ± 2.1* | 96 ± 5.2† |
| LVEDP, mm Hg | 7.8 ± 0.6 | 62 ± 3.7* | 25 ± 3.1† |
| +dP/dt, mm Hg/s | 2680 ± 134 | 488 ± 16.7* | 2278 ± 87† |
| –dP/dt, mm Hg/s | 2346 ± 125 | 396 ± 15.4* | 2042 ± 7.4† |
| B. SR Ca2+-transport | |||
| Ca2+ uptake, nmoles Ca2+/mg/min | 28.6 ± 0.77 | 7.9 ± 0.46* | 20.4 ± 0.65† |
| Ca2+ release, nmoles/mg/15 s | 7.2 ± 0.24 | 2.3 ± 0.18* | 5.9 ± 0.23† |
I/R in isolated perfused rat hearts were induced by 30 min of global ischemia followed by 30 min of reperfusion. PLP was present in the reperfusion medium 10 min before the induction of I/R and was also present throughout the reperfusion period. The data are taken from our paper (Dhalla et al., 2013). *P < 0.05 vs. control group. †P < 0.05 vs. untreated group.
Epidemiologic studies have shown that vitamin C reduces atherosclerosis by improving endothelial function and lipid profile as well as inhibiting the oxidation of low density lipoproteins in patients with ischemic heart disease (Moser and Chun, 2016). Higher intake of vitamin C was also shown to decrease the risk of ischemic heart disease in an individual with prevalence of heavy smoking (Nam et al., 2003). Vitamin C administration to patients with ischemic heart disease was observed to restore coronary flow and prevent the reinduction of coronary constriction (McNulty et al., 2007). This vitamin also provided protection against I/R- mediated oxidative stress in human subjects (Davis et al., 2016). The beneficial effects of vitamin C were also seen for attenuating the ischemic heart disease in mice by modulating hyperlipidemia and high density lipoprotein remodeling (Contreras-Duarte et al., 2018). In contrast to its positive effects in the area of ischemic heart disease, several studies regarding the effects of vitamin C on other cardiovascular diseases are controversial. Some investigators have observed reduction in blood pressure in patients with hypertension upon vitamin C supplementation (Rodrigo et al., 2008; Das, 2019) whereas others did not find any reduction in the rate of adverse outcomes related to pregnancy-related hypertension (Roberts et al., 2010). Although vitamin C has been shown to decrease vulnerability of the heart to postoperative atrial fibrillation due to oxidative damage (Rodrigo et al., 2010), promotion of atrial fibrillation due to atrial-tachycardia remodeling in dogs was unaffected by this intervention (Shiroshita-Takeshita et al., 2004). Likewise, negative results were obtained regarding the effects of vitamin C on endothelial dysfunction and atherosclerosis associated with oxidative stress (Antoniades et al., 2003; Gori and Münzel, 2011). Therefore, it appears that vitamin C may be beneficial for the treatment of ischemic heart disease as a consequence of its antioxidant activity but its use for the therapy of other cardiovascular diseases cannot be indicated with certainty at the present time.
Lipo-Soluble Vitamin Supplementation
Vitamin A and its precursors, α-carotene or β-carotene, were claimed to exert beneficial effects in the development of different cardiovascular diseases (Palace et al., 1999). Increases in the level of serum vitamin A by treatment with this nutrient was shown to decrease both systolic and diastolic blood pressures in patients with hypertension (Chen et al., 2002). Prolonged use of vitamin A was also observed to reduce atherosclerosis in both animals and patients as a consequence of its antioxidant and anti-inflammatory actions (Ozkanlar and Akcay, 2012; Ruiz-León et al., 2019). Supplementation of vitamin A was reported to lower the oxidative stress level in diabetic patients with ischemic heart disease (Altoum et al., 2018). Ischemia-reperfusion (I/R) induced infract size was reduced and the post-ischemic cardiac function recovery was improved by β-carotene in Zucker diabetic rats (Csepanyi et al., 2018), Furthermore, treatment with β-carotene protected the myocardium from advance glycation end product-induced SR stress, apoptosis and autophagy (Zhao et al., 2020). However, β-carotene did not show any beneficial effect on metabolic syndrome in high-fat fed rats (Poudyal et al., 2010).
Administration of vitamin D (calcitriol) in patients with hypertension and heart failure has been shown to exert beneficial effects by inhibiting the renin-angiotensin system and parathyroid hormone secretion, as well as acting directly on vitamin D receptors present in vascular smooth muscle cells, endothelial cells and cardiomyocytes (Nemerovski et al., 2009; Lin et al., 2019). Meta-analysis of several observational studies has revealed that there occurs an inverse relationship between the elevated levels of 25-hydroxyvitamin D (a precursor of calcitriol) and reduction of risk of cardiovascular disease such as myocardial infarction, heart failure and aortic stenosis (Zittermann and Koerfer, 2008; Grandi et al., 2010). Treatment of patients with vitamin D was observed to decrease the progression of coronary artery disease and development of acute myocardial infarction by suppressing the intracellular NF-kB pathway (Legarth et al., 2019). Supplementation of 25-hydroxyvitamin D has been reported to attenuate the development of atherosclerosis by lowering the serum levels of total cholesterol, triglycerides and low density lipoproteins, as well as increasing high density lipoproteins, and endothelial nitric oxide production (Surdu et al., 2021). Vitamin D administration has also been observed to lower different markers of oxidative stress and inflammation in high fat-diet induced obese rats (Farhangi et al., 2017). On the other hand, various clinical studies failed to show any beneficial effects of vitamin D treatment in preventing the ischemic heart disease or reducing its mortality (Bostick et al., 1999; Jarrah et al., 2018; Ingles et al., 2020). In addition, some randomized controlled trials in chronic heart failure and other cardiovascular disease have not shown inconclusive and contradictory results with vitamin D treatment (McGreevy and Williams, 2011; Tsugawa, 2015; Brinkley et al., 2017).
Due to its antioxidant and anti-inflammatory properties as well as its ability to improve immune system and low risk of any adverse effects on human health, vitamin E (α-tocopherol) is most widely used nutritional supplement (Pryor, 2000; Khadangi and Azzi, 2019; van der Pol et al., 2019; Wallert et al., 2019). In fact, several observational and experimental studies have supported the use of vitamin E for the treatment of cardiovascular disease (Pryor, 2000). Supplementation of vitamin E has been reported to reduce blood pressure in patients with essential hypertension (Rodrigo et al., 2008) and prevent complications of pregnancy-associated hypertension (Roberts et al., 2010). Some studies have revealed that treatment with vitamin E delayed the progression and attenuated the extent of atherosclerosis as well as endothelial dysfunction (Salonen et al., 2000; Antoniades et al., 2003; Gori and Münzel, 2011). In fact, α-tocopherol was found to prevent ischemia-reperfusion induced cardiac dysfunction and damage as a consequence of reduction in oxidative stress and inflammation (Nagel et al., 1997; Wallert et al., 2019). Vitamin E supplement also reduced the risk of coronary artery disease in men (Rimm et al., 1993) and produced beneficial effects in ischemic heart disease in mice (Contreras-Duarte et al., 2018). The beneficial effect of vitamin E in myocardial infarction was associated with modulation of different mechanisms (Zarkasi et al., 2019; Ziegler et al., 2020). Pretreatments of rats with vitamin E has also been shown to prevent MI-induced changes in cardiac function as well as ventricular arrhythmias (Sethi et al., 2000). Furthermore, catecholamine-induced arrhythmias, myocardial cell damage, lipid peroxidation and subcellular abnormalities were attenuated by pretreatment of animals with vitamin E (Dhalla et al., 1996; Sethi et al., 2009a,b). These observations suggest that vitamin E is beneficial as a cardioprotective intervention against different pathological stimuli.
In spite of strong support for the beneficial effects of vitamin E, several clinical trials have yielded inconclusive and conflicting results. One study has shown that low doses of vitamin E supplementation decreased the risk of angina in patients without previously diagnosed coronary artery disease whereas high doses decreased myocardial infarction and cardiovascular death (Spencer et al., 1999). The beneficial effects of different doses of vitamin E were dependent upon not only the appropriate dose but also on α- or β- tocopherol forms for inhibiting the release of proinflammatory cytokines as well as activities of 5-lipoxygenase, cyclooxygenase, and tyrosine kinase enzymes (Singh et al., 2005). On the other hand, high doses of vitamin E were also observed to increase the risk of coronary artery disease and myocardial infarction (Wang and Xu, 2019). Conflicting results regarding the beneficial effects of vitamin E treatment for atherosclerosis and coronary artery calcification have been reported in the literature (Antoniades et al., 2003; Machado et al., 2019). Although consumption of vitamin E has been demonstrated to lower the risk of coronary heart disease in middle-aged to older men and women, the primary and secondary cardiovascular events were not affected (Saremi and Arora, 2010). Furthermore, coronary heart disease in postmenopausal women was not modified by vitamin E supplementation (Kushi et al., 1996). In fact, prolonged treatment of high risk patients with vitamin E did not show any effect on different cardiovascular events (Yusuf et al., 2000). However, it is interesting to point out that treatment with vitamin E has been shown to exert beneficial effects on heart disease but certain groups of population and subjects maintained on nutritionally adequate diet do not exhibit additional protection with vitamin E supplement (Chow, 1991). In addition, the protective role of vitamin E in coronary heart disease is evident when patients with no established cardiovascular disease were assessed (Pruthi et al., 2001). Thus, in view of the above-mentioned observations it appears that vitamin E supplementation may play a critical role for the prevention rather than the therapy of cardiovascular disease.
Conclusion
In this article we have reviewed the pros and cons regarding the role of both lipo-soluble and hydro-soluble vitamins in modifying different cardiovascular diseases such as hypertension, atherosclerosis, ischemic heart disease and heart failure. We have examined the issues related to the association of deficiencies of some vitamins with the development of cardiovascular disease as well as the beneficial effects of some vitamin supplementations for the improvement of cardiovascular function in both humans and animals. Although several epidemiological, observational and experimental studies have revealed beneficial effects of some vitamins showing antioxidant, anti-inflammatory, and auto-immune activities in attenuating cardiovascular disorders, results from well controlled clinical investigations are inconsistent, inconclusive and conflicting. In view of such discrepancies in the experimental and clinical observations, no meaningful conclusion can be made for the use of different vitamins in the treatment of cardiovascular disease. It appears that most of the clinical trials with vitamins in cardiovascular disease have been carried out without measuring their plasma levels before initiating the therapy. It is possible that the beneficial effects of these nutrients may only be seen in patients with low levels of plasma vitamins before starting the treatment and this may have been one of the reasons for the failure of relatively large double blind clinical trials with different vitamins. It is also likely that the use of antioxidant vitamins may be beneficial for the prevention of cardiovascular abnormalities due to different pathological stimuli. This view is based on observations that pretreatment of animals with vitamin B6 and vitamin E attenuated the I/R-induced injury or coronary occlusion induced alterations in cardiac function, myocardial metabolism, Ca2+-handling by cardiomyocytes, and ventricular arrhythmias. Pretreatment of animals with vitamins A, C, B6, and E was also observed to depress the catecholamine-induced ventricular arrhythmias. These positive observations provide an appropriate stimulus for carrying out extensive research work for dose-response and cause-effect relationships with various vitamins to establish their specificity in preventing different cardiovascular diseases. It should be recognized that vitamins do not exert any action in healthy individuals and it is the deficiency of some particular vitamin which leads to the development of a particular cardiovascular abnormality. Thus, it would be prudent to examine the effectiveness of vitamins in patients under conditions when their plasma levels are low. Perhaps some new strategies for the treatment of cardiovascular patients be developed to establish the role of some vitamins as a specific adjunct therapy for a specific disease.
Author Contributions
Both authors have contributed equally in the preparation of this article and approved its submission for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank are also due to Ms. Andrea Opsima for typing this manuscript.
Abbreviations
- SL
sarcolemma
- SR
sarcoplasmic reticulum
- ATP
adenosine triphosphate
- [Ca2+]i
intracellular concentration of free calcium
- ATPase
adenosine triphosphatase
- PLP
pyridoxal 5 ′ -phosphate
- MI
myocardial infarction
- PVC
premature ventricular contraction
- I/R
ischemia-reperfusion
- LVDP
left ventricular developed pressure
- LVEDP
left ventricular end diastolic pressure
- +dP/dt
rate of change in contraction
- –dP/dt
rate of change in relaxation.
Funding
The infrastructural support for this work was provided by the St. Boniface Hospital Research Foundation.
References
- Adameova A., Shah A. K., Dhalla N. S. (2020). Role of oxidative stress in the genesis of ventricular arrhythmias. Int. J. Mol. Sci. 21:4200. 10.3390/ijms21124200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal M., Phan A., Willix R., Jr., Barber M., Schwarz E. R. (2011). Is vitamin D deficiency associated with heart failure? A review of current evidence. J. Cardiovasc. Pharmacol. Ther. 16 354–363. 10.1177/1074248410390214 [DOI] [PubMed] [Google Scholar]
- Alpers D. H., Clouse R. E., Stenson W. F. (1983). Manual of Nutritional Therapeutics. Boston: Little, Brown and Company. 457. [Google Scholar]
- Altoum A. E. A., Osman A. L., Babker A. (2018). Comparative study of levels of selective oxidative stress markers (malondialdehyde, zinc, and antioxidant vitamins A, E, and C) in ischemic and non-ischemic heart disease patients suffering from type-2 diabetes. Asian J. Pharm. Clin. Res. 11 508–510. 10.22159/ajpcr.2018.v11i8.27772 [DOI] [Google Scholar]
- Antoniades C., Tousoulis D., Tentolouris C., Toutouzas P., Stefanadis C. (2003). Oxidative stress, antioxidant vitamins, and atherosclerosis. From basic research to clinical practice. Herz 28 628–638. 10.1007/s00059-003-2417-8 [DOI] [PubMed] [Google Scholar]
- Azizi-Namini P., Ahmed M., Yan A. T., Keith M. (2012). The role of B vitamins in the management of heart failure. Nutr. Clin. Pract. 27 363–374. 10.1177/0884533612444539 [DOI] [PubMed] [Google Scholar]
- Balasubramanian S., Christodoulou J., Rahman S. (2019). Disorders of riboflavin metabolism. J. Inherit. Metab. Dis. 42 608–619. 10.1002/jimd.12058 [DOI] [PubMed] [Google Scholar]
- Bartekova M., Adameova A., Gorbe A., Ferenczyova K., Pechanova O., Lazou A., et al. (2021). Natural and synthetic antioxidants targeting cardiac oxidative stress and redox signaling in cardiometabolic diseases. Free. Radic. Biol. Med. 169 446–477. 10.1016/j.freeradbiomed.2021.03.045 [DOI] [PubMed] [Google Scholar]
- Bilagi U. (2018). Vitamin D and heart disease. J. Assoc. Physicians India 66 78–83. [PubMed] [Google Scholar]
- Bleys J., Edgar R., II., Pastor-Barriuso R., Appel L. J., Guallar E. (2006). Vitamin-mineral supplementation and the progression of atherosclerosis: a meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 84 880–887. 10.1093/ajcn/84.4.880 [DOI] [PubMed] [Google Scholar]
- Bostick R. M., Kushi L. H., Wu Y., Meyer K. A., Sellers T. A., Folsom A. R. (1999). Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women. Am. J. Epidemiol. 149 151–161. 10.1093/oxfordjournals.aje.a009781 [DOI] [PubMed] [Google Scholar]
- Brinkley D. M., Ali O. M., Zalawadiya S. K., Wang T. J. (2017). Vitamin D and heart failure. Curr. Heart. Fail. Rep. 14 410–420. 10.1007/s11897-017-0355-7 [DOI] [PubMed] [Google Scholar]
- Carrier M., Emery R., Kandzari D. E., Harringtion R., Guertin M. C., Tardif J. C. (2008). Protective effect of pyridoxal-5′-phosphate (MC-1) on perioperative myocardial infarction is independent of aortic cross clamp time: results from the MEND-CABG trial. J. Cardiovasc. Surg. 49 249–253. [PubMed] [Google Scholar]
- Chasan-Taber L., Selhub J., Rosenberg I. H., Malinow M. R., Terry P., Tishler P. V., et al. (1996). A prospective study of folate and vitamin B6 and risk of myocardial infarction in US physicians. J. Am. Coll. Nutr. 15 136–43. 10.1080/07315724.1996.10718578 [DOI] [PubMed] [Google Scholar]
- Chen J., He J., Hamm L., Batuman V., Whelton P. K. (2002). Serum antioxidant vitamins and blood pressure in the United States population. Hypertension 40 810–816. 10.1161/01.hyp.0000039962.68332.59 [DOI] [PubMed] [Google Scholar]
- Chow C. K. (1991). Vitamin E and oxidative stress. Free Radic. Biol. Med. 11 215–232. 10.1016/0891-5849(91)90174-2 [DOI] [PubMed] [Google Scholar]
- Contreras-Duarte S., Chen P., Andía M., Uribe S., Irarrázaval P., Kopp S., et al. (2018). Attenuation of atherogenic apo B-48-dependent hyperlipidemia and high density lipoprotein remodeling induced by vitamin C and E combination and their beneficial effect on lethal ischemic heart disease in mice. Biol. Res. 51 34–36. 10.1186/s40659-018-0183-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csepanyi E., Czompa A., Szabados-Furjesi P., Lekli I., Balla J., Balla G., et al. (2018). The effects of long-term, low- and high-dose beta-carotene treatment in zucker diabetic fatty rats: the role of HO-1. Int. J. Mol. Sci. 19:1132. 10.3390/ijms19041132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeizel A. E., Dudas I., Vereczkey A., Banhidy F. (2013). Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects. Nutrients 5 4760–4775. 10.3390/nu5114760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakshinamurti S., Wang X., Musat S., Dandekar M., Dhalla N. S. (1998). Alterations of KCI- and ATP-induced increase in [Ca2+]i in cardiomyocytes from vitamin B6 deficient rats. Can. J. Physiol. Pharmacol. 76 837–842. 10.1139/cjpp-76-9-837 [DOI] [PubMed] [Google Scholar]
- Das U. N. (2019). Vitamin C for type 2 diabetes mellitus and hypertension. Arch. Med. Res. 50 11–14. 10.1016/j.arcmed.2019.05.004 [DOI] [PubMed] [Google Scholar]
- Davis J. L., Paris H. L., Beals J. W., Binns S. E., Giordano G. R., Scalzo R. L., et al. (2016). Liposomal-encapsulated ascorbic acid: influence on vitamin C bioavailability and capacity to protect against ischemia-reperfusion injury. Nutr. Metab. Insig. 9 25–30. 10.4137/NMI.S39764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Guia-Galipienso F., Martinez-Ferran M., Vallecillo N., Lavie C. J., Sanchis-Gomar F., Pareja-Galeano H. (2021). Vitamin D and cardiovascular health. Clin. Nutr. 40 2946–2957. 10.1016/j.clnu.2020.12.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhalla K. S., Rupp H., Beamish R. E., Dhalla N. S. (1996). Mechanisms of alterations in cardiac membrane Ca2+ transport due to excess catecholamines. Cardiovasc. Drugs. Ther. 10 231–238. 10.1007/BF00120492 [DOI] [PubMed] [Google Scholar]
- Dhalla N. S., Elmoselhi A. B., Hata T., Makino N. (2000a). Status of myocardial antioxidants in ischemia–reperfusion injury. Cardiovasc. Res. 47 446–456. 10.1016/S0008-6363(00)00078-X [DOI] [PubMed] [Google Scholar]
- Dhalla N. S., Sethi R., Dakshinamurti K. (2000b). Treatment of cardiovascular and related pathologies. US Patent 6:259. [Google Scholar]
- Dhalla N. S., Fedelesova M., Toffler I. (1971). Biochemical alterations in the skeletal muscle of vitamin E deficient rats. Can. J. Physiol. 49 1202–1208. [DOI] [PubMed] [Google Scholar]
- Dhalla N. S., Takeda S., Elimban V. (2013). Mechanisms of the beneficial effects of vitamin B6 and pyridoxal 5-phosphate on cardiac performance in ischemic heart disease. Clin. Chem. Lab. Med. 51 535–543. 10.1515/cclm-2012-0553 [DOI] [PubMed] [Google Scholar]
- Dosedel M., Jirkovsky E., Macakova K., Krcmova L. K., Javorska L., Pourova J., et al. (2021). Vitamin C-sources, physiological role, kinetics, deficiency, use, toxicity, and determination. Nutrients 13:615. 10.3390/nu13020615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draper H. H., James M. F., Johnson B. C. (1952). Tri-o-cresyl phosphate as a vitamin E antagonist for the rat and lamb. J. Nutr. 47 583–599. 10.1093/jn/47.4.583 [DOI] [PubMed] [Google Scholar]
- Ellis J. M., McCully K. S. (1995). Prevention of myocardial infarction by vitamin B6. Res. Commun. Mol. Pathol. Pharmacol. 89 208–220. [PubMed] [Google Scholar]
- Eshak E. S., Arafa A. E. (2018). Thiamine deficiency and cardiovascular science. Nutr. Metab. Cardiovasc. Dis. 28 965–972. 10.1016/j.numecd.2018.06.013 [DOI] [PubMed] [Google Scholar]
- Farhangi M. A., Nameni G., Hajiluian G., Mesgari-Abbasi M. (2017). Cardiac tissue oxidative stress and inflammation after vitamin D administrations in high fat- diet induced obese rats. BMC Cardiovasc. Disord. 17:161. 10.1186/s12872-017-0597-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell P. M. (1980). “Deficiency states, pharmacological effects, and nutrient requirements” in Vitamin E: a Comprehensive Treatise, Basic and Clinical Nutrition. ed. Machlin L. J. (New York: Marcell Dekker; ). 20–630. [Google Scholar]
- Fedelesova M., Sulakhe P. V., Yates J. C., Dhalla N. S. (1971). Biochemical basis heart function. IV. Energy metabolism and calcium transport in hearts of vitamin E deficient rats. Can. J. Physiol. Pharmacol. 49 909–918. 10.1139/y71-126 [DOI] [PubMed] [Google Scholar]
- Feingold K. R. (2000). Triglyceride Lowering Drugs. Marylan: NCBI. https://www.ncbi.nlm.nih.gov/books/NBK425699/ [PubMed] [Google Scholar]
- Fitch C. D. (1968). Experimental anemia in primates due to vitamin E deficiency. Vitam Horm. 26 501–514. 10.1016/s0083-6729(08)60768-2 [DOI] [PubMed] [Google Scholar]
- Friso S., Girelli D., Martinelli N., Olivieri O., Lotto V., Bozzini C., et al. (2004). Low plasma vitamin B-6 concentrations and modulation of coronary artery disease risk. Am. J. Clin. Nutr. 79 992–998. 10.1093/ajcn/79.6.992 [DOI] [PubMed] [Google Scholar]
- Gale C. R., Martyn C. N., Winter P. D., Cooper C. (1995). Vitamin C and risk of death from stroke and coronary heart disease in cohort of elderly people. Brit. Med. J. 310 1563–1566. 10.1136/bmj.310.6994.1563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatz A. J., Houchin O. B. (1951). Studies on the heart of vitamin E deficient rabbits. Anat. Rec. 110 249–265. 10.1002/ar.1091100209 [DOI] [PubMed] [Google Scholar]
- Georgiopoulos G., Chrysohoou C., Vogiatzi G., Magkas N., Bournelis I., Bampali S., et al. (2017). Vitamins in heart failure: friend or enemy? Curr. Pharm. Des. 23 3731–3742. 10.2174/1381612823666170321094711 [DOI] [PubMed] [Google Scholar]
- Gominak S. C. (2016). Vitamin D deficiency changes the intestinal microbiome reducing B vitamin production in the gut. The resulting lack of pantothenic acid adversely affects the immune system, producing a “pro-inflammatory” state associated with atherosclerosis and autoimmunity. Med. Hypoth. 94 103–107. 10.1016/j.mehy.2016.07.007 [DOI] [PubMed] [Google Scholar]
- Gori T., Münzel T. (2011). Oxidative stress and endothelial dysfunction: therapeutic implications. Ann. Med. 43 259–272. 10.3109/07853890.2010.543920 [DOI] [PubMed] [Google Scholar]
- Grandi N. C., Brietling L. P., Brenner H. (2010). Vitamin D and cardiovascular disease: systematic review and meta-analysis of prospective studies. Prev. Med. 51 228–233. 10.1016/j.ypmed.2010.06.013 [DOI] [PubMed] [Google Scholar]
- Grigoreva V. A., Medovar E. N. (1959). Studies on the components of the adenylic system in skeletal and cardiac muscles in experimental muscular dystrophy (Russian text). Ukr. Biokhim, Zh. 31 351–368. [Google Scholar]
- Gullickson T. W. (1949). The relation of vitamin E to reproduction in dairy cattle. Ann. N. Y. Acad. Sci. 52 256–259. [Google Scholar]
- Gullickson T. W., Calverley C. E. (1946). Cardiac failure in cattle on vitamin E-free rations as revealed by electrocardiograms. Science 104 312–313. 10.1126/science.104.2701.312 [DOI] [PubMed] [Google Scholar]
- Guthikonda S., Haynes W. G. (2006). Homocysteine: role and implications in atherosclerosis. Curr. Atheroscler. Rep. 8 100–106. 10.1007/s11883-006-0046-4 [DOI] [PubMed] [Google Scholar]
- Hagar H. H. (2002). Folic acid and vitamin B(12) supplementation attenuates isoprenaline-induced myocardial infarction in experimental hyperhomocysteinemic rats. Pharmacol. Res. 46 213–219. 10.1016/s1043-6618(02)00095-6 [DOI] [PubMed] [Google Scholar]
- Haynes W. G. (2002). Hyperhomocysteinemia, vascular function and atherosclerosis: effects of vitamins. Cardiovasc. Drugs Ther. 16 391–399. 10.1023/A:1022130217463 [DOI] [PubMed] [Google Scholar]
- Herzlich B. C. (1996). Plasma homocysteine, folate, vitamin B6 and coronary artery diseases risk. J. Am. Coll. Nutr. 15 109–110. [DOI] [PubMed] [Google Scholar]
- Hodzic E. (2018). Potential anti-inflammatory treatment of ischemic heart disease. Med. Arch. 72 94–98. 10.5455/medarh.2018.72.94-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingles D. P., Cruz Rodriguez J. B., Garcia H. (2020). Supplemental vitamins and minerals for cardiovascular disease prevention and treatment. Curr. Cardiol. Rep. 22:22. 10.1007/s11886-020-1270-1 [DOI] [PubMed] [Google Scholar]
- Ivey M. (1979). “Nutritional supplement, minerals and vitamin products” in Handbook of Non-Prescription Drugs 6th Edn. eds Welch J., Rasmussen M. T., Goldstein S. W., Kelly J. (Washington: American Pharmaceutical Association; ). 141–174. [Google Scholar]
- Jarrah M. I., Mhaidat N. M., Alzoubi K. H., Alrabadi N., Alsatari E., Khader Y., et al. (2018). The association between the serum level of vitamin D and ischemic heart disease: a study from Jordan. Vasc. Health Risk Manag. 14 119–127. 10.2147/VHRM.S167024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd S. E., Tangpricha V. (2009). Vitamin D deficiency and risk for cardiovascular disease. Am. J. Med. Sci. 338 40–44. 10.1097/MAJ.0b013e3181aaee91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandzari D. E., Dery J. P., Armstrong P. W., Douglas D. A., Zettler M. E., Hidinger G. K., et al. (2005). MC-1 (pyridoxal 5′-phosphate): novel therapeutic applications to reduce ischaemic injury. Expert. Opin. Ivestig. Drugs 14 1435–1442. 10.1517/13543784.14.11.1435 [DOI] [PubMed] [Google Scholar]
- Kandzari D. E., Labinaz M., Cantor W. J., Madan M., Gallup D. S., Hasselblad V., et al. (2003). Reduction of myocardial ischemic injury following coronary intervention (the MC-1 to eliminate necrosis and damage trial). Am. J. Cardiol. 92 660–664. 10.1016/s0002-9149(03)00818-x [DOI] [PubMed] [Google Scholar]
- Kannan K., Jain S. K. (2004). Effect of vitamin B6 on oxygen radicals, mitochondrial membrane potential, and lipid peroxidation in H2O2-treated U937 monocytes. Free Radic. Biol. Med. 36 423–428. 10.1016/j.freeradbiomed.2003.09.012 [DOI] [PubMed] [Google Scholar]
- Keith M. E., Walsh N. A., Darling P. B., Hanninen S. A., Thirugnanam S., Leong-Pi H., et al. (2009). B-vitamin deficiency in hospitalized patients with heart failure. J. Am. Diet. Assoc. 109 1406–1410. 10.1016/j.jada.2009.05.011 [DOI] [PubMed] [Google Scholar]
- Khadangi F., Azzi A. (2019). Vitamin E – the next 100 years. IUBMB Life 71 411–415. 10.1002/iub.1990 [DOI] [PubMed] [Google Scholar]
- Kheiri B., Abdalla A., Osman M., Ahmed S., Hassan M., Bachuwa G. (2018). Vitamin D deficiency and risk of cardiovascular diseases: a narrative review. Clin. Hypertens. 24:9. 10.1186/s40885-018-0094-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M. K., Sasaki S., Sasazuki S., Okubo S., Hayashi M., Tsugane S. (2002). Lack of long-term effect of vitamin C supplementation on blood pressure. Hypertension 40 797–803. 10.1161/01.HYP.0000038339.67450.60 [DOI] [PubMed] [Google Scholar]
- Knekt P., Ritz J., Pereira M. A., O’Reilly E., Augustsson K., Fraser G. E., et al. (2004). Antioxidant vitamins and coronary heart disease risk: a pooled analysis of 9 cohorts. Am. J. Clin. Nutr. 80 1508–1520. 10.1093/ajcn/80.6.1508 [DOI] [PubMed] [Google Scholar]
- Kok F. J., Schrijver J., Hofman A., Witteman J. C. M., Kruyssen D., Remme W. J., et al. (1989). Low vitamin B6 status in patients with acute myocardial infarction. Am. J. Cardiol. 63 513–513. 10.1016/0002-9149(89)90890-4 [DOI] [PubMed] [Google Scholar]
- Ku Y. C., Liu M. E., Ku C. S., Liu T. Y., Lin S. L. (2013). Relationship between vitamin D deficiency and cardiovascular disease. World J. Cardiol. 5 337–346. 10.4330/wjc.v5.i9.337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushi L. H., Folsom A. R., Prineas R. J., Mink P. J., Wu Y., Bostick R. M. (1996). Dietary antioxidant vitamins and death from coronary heart disease in postmenopausal women. N. Engl. J. Med. 334 1156–1162. 10.1056/NEJM199605023341803 [DOI] [PubMed] [Google Scholar]
- Lal K. J., Dakshinamurti K., Thliveris J. (1996). The effect of vitamin B6 on the systolic blood pressure of rats in various animal models of hypertension. J. Hypertens. 14 355–363. 10.1097/00004872-199603000-00013 [DOI] [PubMed] [Google Scholar]
- Latic N., Erben R. G. (2020). Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure. Int. J. Mol. Sci. 21:6483. 10.3390/ijms21186483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legarth C., Grimm D., Krüger M., Infanger M., Wehland M. (2019). Potential beneficial effects of vitamin D in coronary artery disease. Nutrients 12:99. 10.3390/nu12010099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L., Zhang L., Li C., Gai Z., Li Y. (2019). Vitamin D and vitamin D receptor: new insights in the treatment of hypertension. Curr. Protein Pept. Sci. 20 984–995. 10.2174/1389203720666190807130504 [DOI] [PubMed] [Google Scholar]
- Liu C., Liu C., Wang Q., Zhang Z. (2018). Supplementation of folic acid in pregnancy and the risk of preeclampsia and gestational hypertension: a meta-analysis. Arch. Gynecol. Obstet. 298 697–704. 10.1007/s00404-018-4823-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R., Mi B., Zhao Y., Li Q., Yan H., Dang S. (2017). Effect of B vitamins from diet on hypertension. Arch. Med. Res. 48 187–194. 10.1016/j.arcmed.2017.03.011 [DOI] [PubMed] [Google Scholar]
- Long P., Liu X., Li J., He S., Chen H., Yuan Y., et al. (2020). Circulating folate concentrations and risk of coronary artery disease: a prospective cohort study in Chinese adults and a Mendelian randomization analysis. Am. J. Clin. Nutr. 111 635–643. 10.1093/ajcn/nqz314 [DOI] [PubMed] [Google Scholar]
- Lu G. D., Emerson G. A., Evans H. M. (1941). Phosphorus metabolism of the musculature of E-deficient suckling rats. Am. J. Physiol. 133 367–368. [Google Scholar]
- Machado A. D., Andrade G. R. G., Levy J., Ferreira S. S., Marchioni D. M. (2019). Association between vitamins and minerals with antioxidant effects and coronary artery calcification in adults and older adults: a systematic review. Curr. Pharm. Des. 25 2474–2479. 10.2174/1381612825666190722101954 [DOI] [PubMed] [Google Scholar]
- MacKenzie J. B., MacKenzie C. G. (1953). Vitamin E activity of alpha-tocopherylhydroquinone and muscular dystrophy. Proc. Soc. Exp. Biol. Med. 84 388–392. 10.3181/00379727-84-20655 [DOI] [PubMed] [Google Scholar]
- Madsen L. L., McCay C. M., Maynard L. A. (1933). Possible relationship between cod liver oil and muscular degeneration of herbivora fed synthetic diets. Proc. Soc. Exp. Biol. Med. 30 1434–1438. [Google Scholar]
- Maulik S. K., Kumar S. (2012). Oxidative stress and cardiac hypertrophy: a review. Toxicol. Mech. Methods 22 359–366. 10.3109/15376516.2012.666650 [DOI] [PubMed] [Google Scholar]
- McGreevy C., Williams D. (2011). New insights about the vitamin D and cardiovascular disease. Ann. Intern. Med. 155 820–826. 10.7326/0003-4819-155-12-201112200-00004 [DOI] [PubMed] [Google Scholar]
- McNulty P. H., Robertson B. J., Tulli M. A., Hess J., Harach L. A., Scott S., et al. (2007). Effect of hyperoxia and vitamin C on coronary blood flow in patients with ischemic heart disease. J. Appl. Physiol. 102 2040–2045. 10.1152/japplphysiol.00595.2006 [DOI] [PubMed] [Google Scholar]
- Mehta R. H., Alexander J. H., Emery R., Ellis S. J., Hasselblad V., Khalil A., et al. (2008). A randomized, double-mind, placebo-controlled, multicenter study to evaluate the cardioprotective effects of MC-1 in patients undergoing high-risk coronary artery bypass graft surgery: mC-1 eliminate necrosis and damage in coronary artery bypass graft surgery trial (MEND-CABG) II–study design and rationale. Am. Heart J. 155 600–608. 10.1016/j.ahj.2008.01.002 [DOI] [PubMed] [Google Scholar]
- Moat S. J., Clarke Z. L., Madhavan A. K., Lewis M. J., Lang D. (2006). Folic acid reverses endothelial dysfunction induced by inhibition of tetrahydrobiopterin biosynthesis. Eur. J. Pharmacol. 530 250–258. 10.1016/j.ejphar.2005.11.047 [DOI] [PubMed] [Google Scholar]
- Moser M. A., Chun O. K. (2016). Vitamin C and heart health: a review based on findings from epidemiologic studies. Int. J. Mol. Sci. 17:1328. 10.3390/ijms17081328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozos I., Marginean O. (2015). Links between vitamin D deficiency and cardiovascular diseases. Biomed. Res. Intl. 2015:109275. 10.1155/2015/109275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulder A. G., Gatz A. J., Tigerman B. (1954). Phosphate and glycogen determination in the hearts of vitamin E deficient rabbits. Am. J. Physiol. 196 246–248. 10.1152/ajplegacy.1954.179.2.246 [DOI] [PubMed] [Google Scholar]
- Murray J. C., Fraser D. R., Levene C. I. (1978). The effect of pyridoxine on lysyl oxidase activity in the chick. Exp. Mol. Pathol. 28 301–308. 10.1016/0014-4800(78)90004-7 [DOI] [PubMed] [Google Scholar]
- Muscogiuri G., Annweiler C., Duval G., Karras S., Tirabassi G., Salvio G., et al. (2017). Vitamin D and cardiovascular disease: from atherosclerosis to myocardial infarction and stroke. Int. J. Cardiol. 230 577–584. 10.1016/j.ijcard.2016.12.053 [DOI] [PubMed] [Google Scholar]
- Myung S. K., Ju W., Cho B., Oh S. W., Park S. M., Koo B. K., et al. (2013). Efficacy of vitamin and antioxidant supplements in prevention of cardiovascular disease: systematic review and meta-analysis of randomised controlled trials. Brit. Med. J. 346:f10. 10.1136/bmj.f10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagel E., Meyer zu Vilsendorf A., Bartels M., Pichlmayr R. (1997). Antioxidative vitamins in prevention of ischemia/reperfusion injury. Int. J. Vitam. Res. 67 298–306. [PubMed] [Google Scholar]
- Nam C. M., Oh K. W., Lee K. H., Jee S. H., Cho S. Y., Shim W. H., et al. (2003). Vitamin C intake and risk of ischemic heart disease in a population with a high prevalence of smoking. Null 22 372–378. 10.1080/07315724.2003.10719320 [DOI] [PubMed] [Google Scholar]
- National Research Council (US) Committee on Diet and Health (1989). Diet and Health: implications for Reducing Chronic Disease Risk. Washington: National Academies Press. [PubMed] [Google Scholar]
- Nemerovski C. W., Dorsch M. P., Simpson R. U., Bone H. G., Aaronson K. D., Bleske B. E. (2009). Vitamin D and cardiovascular disease. Pharmacotherapy 29 691–708. 10.1592/phco.29.6.691 [DOI] [PubMed] [Google Scholar]
- Neri M., Fineschi V., Di Paolo M., Pomara C., Riezzo I., Turillazzi E., et al. (2015). Cardiac oxidative stress and inflammatory cytokines response after myocardial infarction. Curr. Vasc. Pharmacol. 13 26–36. 10.2174/15701611113119990003 [DOI] [PubMed] [Google Scholar]
- NyyssOnen K., Parviainen M. T., Salonen R., Tuomilehto J., Salonen J. T. (1997). Vitamin C deficiency and risk of myocardial infarction: prospective population study of men from eastern Finland. BMJ 314 634–638. 10.1136/bmj.314.7081.634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson R. E. (1973). Vitamin E and its relation to heart disease. Circulation 48 179–184. 10.1161/01.cir.48.1.179 [DOI] [PubMed] [Google Scholar]
- Osganian S. K., Stampfer M. J., Rimm E., Spiegelman D., Hu F. B., Manson J. E., et al. (2003). Vitamin C and risk of coronary heart disease in women. J. Am. Coll. Cardiol. 42 246–252. 10.1016/s0735-1097(03)00575-8 [DOI] [PubMed] [Google Scholar]
- Oski F. A., Barness L. A. (1969). Vitamin E deficiency: a previously unrecognized cause for hemolytic anemia in the premature infant. J. Pediatr. 70 211–220. 10.1016/s0022-3476(67)80416-5 [DOI] [PubMed] [Google Scholar]
- Ozkanlar S., Akcay F. (2012). Antioxidant vitamins in atherosclerosis–animal experiments and clinical studies. Adv. Clin. Exp. Med. 21 115–123. [PubMed] [Google Scholar]
- Palace V. P., Khaper N., Qin Q., Singal P. K. (1999). Antioxidant potential of vitamin A and carotenoids and their relevance to heart disease. Free Rad. Biol. Med. 26 746–761. 10.1016/s0891-5849(98)00266-4 [DOI] [PubMed] [Google Scholar]
- Palinski W., Rosenfeld M. E., Yla-Herttuala S., Gurtner G. C., Socher S. S., Butler S. W., et al. (1989). Low-density lipoprotein undergoes oxidative modification in vivo. Proc. Natl. Acad. Sci. 86 1372–1376. 10.1073/pnas.86.4.1372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palumbo G., Avanzini F., Alli C., Roncaglioni M. C., Ronchi E., Cristofari M., et al. (2000). Effects of vitamin E on clinic and ambulatory blood pressure in treated hypertensive patients. Am. J. Hypertens. 13 564–567. 10.1016/S0895-7061(00)00244-2 [DOI] [PubMed] [Google Scholar]
- Pancharuniti N., Lewis C. A., Sauberlich H. E., Perkins L. L., Go R. C., Alvarez J. O., et al. (1994). Plasma homocyst(e)ine, folate, and vitamin B-12 concentrations and risk for early-onset coronary artery disease. Am. J. Clin. Nutr. 59 940–948. 10.1093/ajcn/59.4.940 [DOI] [PubMed] [Google Scholar]
- Paulose C. S., Dakshinamurti K., Packer S., Stephens N. L. (1988). Sympathetic stimulation and hypertension in pyridoxine-deficient adult rat. Hypertension 11 387–391. 10.1161/01.hyp.11.4.387 [DOI] [PubMed] [Google Scholar]
- Pawlak R. (2015). Is vitamin B12 deficiency a risk factor for cardiovascular disease in vegetarians? Am. J. Prev. Med. 48 e11–26. 10.1016/j.amepre.2015.02.009 [DOI] [PubMed] [Google Scholar]
- Perez-Castrillon J. L., Vega G., Abad L., Sanz A., Chaves J., Hernandez G., et al. (2007). Effects of atorvastatin on vitamin D levels in patients with acute ischemic heart disease. Am. J. Cardiol. 99 903–905. 10.1016/j.amjcard.2006.11.036 [DOI] [PubMed] [Google Scholar]
- Pfister R., Sharp S. J., Luben R., Wareham N. J., Khaw K. T. (2011). Plasma vitamin C predicts incident heart failure in men and women in European prospective investigation into cancer and nutrition-norfolk prospective study. Am. Heart J. 162 246–253. 10.1016/j.ahj.2011.05.007 [DOI] [PubMed] [Google Scholar]
- Pilz S., Tomaschitz A., Drechsler C., de Boer R. A. (2011). Vitamin D deficiency and heart disease. Kidney Inter. Suppl. 1 111–115. [Google Scholar]
- Poudyal H., Panchal S., Brown L. (2010). Comparison of purple carrot juice and β-carotene in a high-carbohydrate, high-fat diet-fed rat model of the metabolic sydrome. Br. J. Nutr. 104 1322–1332. 10.1017/S0007114510002308 [DOI] [PubMed] [Google Scholar]
- Powers H. J. (2003). Riboflavin (vitamin B-2) and health. Am. J. Clin. Nutr. 77 1352–1360. 10.1093/ajcn/77.6.1352 [DOI] [PubMed] [Google Scholar]
- Pruthi S., Allison T. G., Hensrud D. D. (2001). Vitamin E supplementation in the prevention of coronary heart disease. Mayo Clin. Proc. 76 1131–1136. 10.4065/76.11.1131 [DOI] [PubMed] [Google Scholar]
- Pryor W. A. (2000). Vitamin E and heart disease: basic science to clinical intervention trials. Free Radic. Biol. Med. 28 141–164. 10.1016/s0891-5849(99)00224-5 [DOI] [PubMed] [Google Scholar]
- Psara E., Pentieva K., Ward M., McNulty H. (2020). Critical review of nutrition, blood pressure and risk of hypertension through the lifecycle: do B vitamins play a role? Biochimie 173 76–90. [DOI] [PubMed] [Google Scholar]
- Rafnsson S. B., Saravanan P., Bhopal R. S., Yajnik C. S. (2011). Is a low blood level of vitamin B12 a cardiovascular and diabetes risk factor? A systematic review of cohort studies. Eur. J. Nutr. 50 97–106. 10.1007/s00394-010-0119-6 [DOI] [PubMed] [Google Scholar]
- Ramachandra C. J. A., Cong S., Chan X., Yap E. P., Yu F., Hausenloy D. J. (2021). Oxidative stress in cardiac hypertrophy: from molecular mechanism to novel therapeutic targets. Free. Radic. Biol. Med. 166 297–312. 10.1016/j.freeradbiomed.2021.02.040 [DOI] [PubMed] [Google Scholar]
- Read W. O., Nehorayan S. (1959). Effect of vitamin E deficiency on creatine phosphokinase of heart and skeletal muscle. Am. J. Physiol. 196 1286–1288. 10.1152/ajplegacy.1959.196.6.1286 [DOI] [PubMed] [Google Scholar]
- Rimm E. B., Stamper M. J., Ascherio A., Giovannucci E., Colditz G. A., Willett W. C. (1993). Vitamin E consumption and the risk of coronary heart disease in men. N. Engl. J. Med. 328 1450–1456. 10.1056/NEJM199305203282004 [DOI] [PubMed] [Google Scholar]
- Rinehart J. F., Greenberg L. D. (1949). Arteriosclerotic lesions in pyridoxine deficient monkeys. Am. J. Pathol. 25 481–491. [PMC free article] [PubMed] [Google Scholar]
- Roberts J. M., Myatt L., Spong C. Y., Thom E. A., Hauth J. C., Leveno K. J., et al. (2010). Vitamins C and E to prevent complications of pregnancy-associated hypertension. N. Engl. J. Med. 362 1282–1291. 10.1056/NEJMoa0908056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson K., Arheart K., Refsum H., Brattstrom L., Boers G., Ueland P., et al. (1998). Low circulating folate and vitamin B6 concentrations: risk factors for stroke, peripheral vascular disease, and coronary artery disease. European COMAC Group. Circulation 97 437–443. 10.1161/01.cir.97.5.437 [DOI] [PubMed] [Google Scholar]
- Rodrigo R., Prat H., Passalacqua W., Araya J., Bächler J. P. (2008). Decrease in oxidative stress through supplementation of vitamins C and E is associated with a reduction in blood pressure in patients with essential hypertension. Clin. Sci. 114 625–634. 10.1042/CS20070343 [DOI] [PubMed] [Google Scholar]
- Rodrigo R., Vinay J., Castillo R., Cereceda M., Asenjo R., Zamorano J., et al. (2010). Use of vitamins C and E as a prophylactic therapy to prevent postoperative atrial fibrillation. Int. J. Cardiol. 138 221–228. 10.1016/j.ijcard.2009.04.043 [DOI] [PubMed] [Google Scholar]
- Ruiz-León A. M., Lapuente M., Estruch R., Casas R. (2019). Clinical advances in immunonutrition and atherosclerosis: a review. Front. Immunol. 10:837. 10.3389/fimmu.2019.00837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salonen J. T., Nyyssonen K., Salonen R., Lakka H. M., Kaikkonen J., Porkkala-Sarataho E., et al. (2000). Antioxidant supplementation in atherosclerosis prevention (ASAP) study: a randomized trial of the effect of vitamins E and C on 3-year progression of carotid atherosclerosis. J. Intern. Med. 248 377–386. 10.1046/j.1365-2796.2000.00752.x [DOI] [PubMed] [Google Scholar]
- Saremi A., Arora R. (2010). Vitamin E and Cardiovascular disease. Am. J. Ther. 17 e56–65. 10.1097/MJT.0b013e31819cdc9a [DOI] [PubMed] [Google Scholar]
- Serfontein W. J., Ubbink J. B., De Villiers L. S., Rapley C. H., Becker P. J. (1985). Plasma pyridoxal-5-phosphate level as risk index for coronary artery disease. Atherosclerosis 55 357–361. 10.1016/0021-9150(85)90113-3 [DOI] [PubMed] [Google Scholar]
- Sethi R., Adameova A., Dhalla K. S., Khan M., Elimban V., Dhalla N. S. (2009a). Modification of epinephrine-induced arrhythmias by N-Acetyl-L-Cysteine and vitamin E. J. Cardiovasc. Pharmacol. Ther. 14 134–142. 10.1177/1074248409333855 [DOI] [PubMed] [Google Scholar]
- Sethi R., Rehsia N. S., Jindal K., Dhalla K. S., Elimban V., Dhalla N. S. (2009b). Antiarrhythmic effects of some antioxidant vitamins in rats injected with epinephrine. Cardiovasc. Toxicol. 9 177–184. 10.1007/s12012-009-9051-5 [DOI] [PubMed] [Google Scholar]
- Sethi R., Takeda N., Nagano M., Dhalla N. S. (2000). Beneficial effects of vitamin E treatment in acute myocardial infarction. J. Cardiovasc. Pharmacol. Therapeut. 5 51–58. 10.1177/107424840000500107 [DOI] [PubMed] [Google Scholar]
- Shiroshita-Takeshita A., Gernot S., Joel L., Stanley N. (2004). Effect of simvastatin and antioxidant vitamins on atrial fibrillation promotion by atrial-tachycardia remodeling in dogs. Circulation 110 2313–2319. 10.1161/01.CIR.0000145163.56529.D1 [DOI] [PubMed] [Google Scholar]
- Singh U., Devaraj S., Jialal I. (2005). Vitamin E, oxidative stress, and inflammation. Annu. Rev. Nutr. 25 151–174. 10.1146/annurev.nutr.24.012003.132446 [DOI] [PubMed] [Google Scholar]
- Song E. K., Kang S. K. (2018). Vitamin C deficiency, high-sensitivity C-reactive protein, and cardiac event-free survival in patients with heart failure. J. Cardiovasc. Nurs. 33 6–12. 10.1097/JCN.0000000000000389 [DOI] [PubMed] [Google Scholar]
- Spencer A. P., Carson D. S., Crouch M. A. (1999). Vitamin E and coronary artery disease. Arch. Intern. Med. 159 1313–1320. 10.1001/archinte.159.12.1313 [DOI] [PubMed] [Google Scholar]
- Stanger O., Herrmann W., Pietrzik K., Fowler B., Geisel J., Dierkes J., et al. (2004). Clinical use and rational management of homocysteine, folic acid, and B vitamins in cardiovascular and thrombotic diseases. Z. Kardiol. 93 439–453. 10.1007/s00392-004-0075-3 [DOI] [PubMed] [Google Scholar]
- Stanhewicz A. E., Kenney W. L. (2017). Role of folic acid in nitric oxide bioavailability and vascular endothelial function. Nutr. Rev. 75 61–70. 10.1093/nutrit/nuw053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surdu A. M., Pînzariu O., Ciobanu D. M., Negru A. G., Căinap S. S., Lazea C., et al. (2021). Vitamin D and its role in the lipid metabolism and the development of atherosclerosis. Biomedicines 9:172. 10.3390/biomedicines9020172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swain R. A., St Clair L. (1997). The role of folic acid in deficiency states and prevention disease. J. Fam. Pract. 44 138–144. [PubMed] [Google Scholar]
- Sziva R. E., Fontányi Z., Pál É, Hadjadj L., Monori-Kiss A., Horváth E. M., et al. (2020). Vitamin D deficiency induces elevated oxidative and biomechanical damage in coronary arterioles in male rats. Antioxidants 9:997. 10.3390/antiox9100997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tardif J. C., Carrier M., Kandzari D. E., Emery R., Cote R., Heinonen T., et al. (2007). Effects of pyridoxal 5′-phosphate (MC-1) in patients undergoing high-risk coronary artery bypass surgery: results of the MEND-CABG randomized study. J. Thorac. Cardiovasc. Surg. 133 1604–1611. 10.1016/j.jtcvs.2007.01.049 [DOI] [PubMed] [Google Scholar]
- Title L. M., Cummings P. M., Giddens K., Genest J. J., Jr., Nassar B. A. (2000). Effect of folic acid and antioxidant vitamins on endothelial dysfunction in patients with coronary artery disease. J. Am. Coll. Cardiol. 36 758–765. 10.1016/s0735-1097(00)00809-3 [DOI] [PubMed] [Google Scholar]
- Traber M. G. (1999). “Vitamin E” in Modern Nutrition in Health and Disease, 9th Edn. (eds) Shils M. E., Olson J. A., Shike M., Ross A. C. (Baltimore: Williams & Wilkins; ). 347–362. [Google Scholar]
- Tsugawa N. (2015). Cardiovascular diseases and fat soluble vitamins: vitamin D and vitamin K. J. Nutr. Sci. Vitaminol. 61:170. 10.3177/jnsv.61.S170 [DOI] [PubMed] [Google Scholar]
- van der Pol A., van Gilst W. H., Voors A. A., van der Meer P. (2019). Treating oxidative stress in heart failure: past, present and future. Eur. J. Heart. Fail. 21 425–435. 10.1002/ejhf.1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanathan M., Paulose C. S., Lak K. J., Sharma S. K., Dakshinamurti K. (1990). Alterations in brain stem alpha 2 adrenoceptors and acitivty in pryridoxine-deficient rat model of hypertension. Neurosci. Lett. 111 201–205. 10.1016/0304-3940(90)90368-j [DOI] [PubMed] [Google Scholar]
- Wallert M., Ziegler M., Wang X., Maluenda A., Xu X., Yap M. L., et al. (2019). α-Tocopherol preserves cardiac function by reducing oxidative stress and inflammation in ischemia/reperfusion injury. Redox Biol. 26:101292. 10.1016/j.redox.2019.101292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T. J., Pencina M. J., Both S. L., Jacques P. F., Ingelsson E., Lanier K., et al. (2008). Vitamin D deficiency and risk of cardiovascular disease. Circulation 117 503–511. 10.1161/CIRCULATIONAHA.107.706127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T., Xu L. (2019). Circulating Vitamin E levels and risk of coronary artery disease and myocardial infarction: a mendelian randomization study. Nutrients 11:2153. 10.3390/nu11092153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Dakshinamurti K., Musat S., Dhalla N. S. (1999). Pyridoxal 5′-phosphate is an ATP-receptor antagonist in freshly isolated rat cardiomyocytes. J. Moll. Cell. Cardiol. 31 1063–1072. 10.1006/jmcc.1999.0936 [DOI] [PubMed] [Google Scholar]
- Wang Y., Chun O. K., Wo S. (2013). Plasma and dietary antioxidant status as cardiovascular disease risk factors: a review of human studies. Nutrients 5 2969–3004. 10.3390/nu5082969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welles C. C., Whooley M. A., Karumanchi S. A., Hod T., Thadhani R., Berg A. H., et al. (2014). Vitamin D deficiency and cardiovascular events in patient swith coronary heart disease: data from the heart and soul study. Am. J. Epidemiol. 179 1279–1287. 10.1093/aje/kwu059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcken D. E., Wilcken B. (1998). B vitamins and homocysteine in cardiovascular disease and aging. Ann. N. Y. Acad. Sci. 854 361–370. 10.1111/j.1749-6632.1998.tb09916.x [DOI] [PubMed] [Google Scholar]
- Witte K. K. A., Nikitin N. P., Parker A. C., von Haehling S., Volk H., Anker S. D., et al. (2005). The effect of micronutrient supplementation on quality-of-life and left ventricular function in elderly patients with chronic heart failure. Eur. Heart J. 26 2238–2244. 10.1093/eurheartj/ehi442 [DOI] [PubMed] [Google Scholar]
- Woo K. S., Kwok T. C. Y., Celermajer D. S. (2014). Vegan diet, subnormal vitamin B-12 status and cardiovascular health. Nutrients 6 3259–3273. 10.3390/nu6083259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Z., Song H. (2008). Antioxidant vitamins intake and the risk of coronary heart disease: meta-analysis of cohort studies. Eur. J. Cardiovasc. Prev. Rehabil. 15 26–34. 10.1097/HJR.0b013e3282f11f95 [DOI] [PubMed] [Google Scholar]
- Yla-Herttuala S., Palinski W., Rosenfeld M. E., Parthasarathy S., Carew T. E., Butler S., et al. (1989). Evidence for the presence of oxidatively modified low density lipoprotein in atherosclerotic lesions of rabbit and man. J. Clin. Invest. 84 1086–1095. 10.1172/JCI114271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young V. R., Solomons N. W. (1983). “Nonnutrients factors in metabolism” in Manual of Clinical Nutrition. (ed). Paige D.M. (New Jersey: Nutrition Publications, Pleasantville; ). 3.1–3.13. [Google Scholar]
- Yusuf S., Dagenais G., Pogue J., Bosch J., Sleight P. (2000). Vitamin E supplementation and cardiovascular events in high-risk patients. N. Engl. J. Med. 342 154–160. 10.1056/NEJM200001203420302 [DOI] [PubMed] [Google Scholar]
- Zarkasi K. A., Jen-Kit T., Jubri Z. (2019). Molecular understanding of the cardiomodulation in myocardial infarction and the mechanism of vitamin E protections. Mini Rev. Med. Chem. 19 1407–1426. 10.2174/1389557519666190130164334 [DOI] [PubMed] [Google Scholar]
- Zhao G., Zhang X., Wang H., Chen Z. (2020). Beta carotene protects H9c2 cardiomyocytes from advanced glycation end product-induced endoplasmic reticulum stress, apoptosis and autophagy via the PI3K/Akt/mTOR signaling pathway. Ann. Transl. Med. 8:647. 10.21037/atm-20-3768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler M., Wallert M., Lorkowski S., Peter K. (2020). Cardiovascular and metabolic protection by vitamin E: a matter of treatment strategy? Antioxidants 9:935. 10.3390/antiox9100935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zittermann A. (2006). Vitamin D and disease prevention with special reference to cardiovascular disease. Prog. Biophys. Mol. Biol. 92 39–48. 10.1016/j.pbiomolbio.2006.02.001 [DOI] [PubMed] [Google Scholar]
- Zittermann A., Koerfer R. (2008). Vitamin D in the prevention and treatment of coronary heart disease. Curr. Opin. Clin. Nutr. Metab. Care 11 752–757. 10.1097/MCO.0b013e328312c33f [DOI] [PubMed] [Google Scholar]