Abstract
Background
COVID-19 pandemic has disrupted access to healthcare. Delay in diagnosis and onset of care increases cancer related mortality. We aim to analyse its impact on patient profile, hospital visits, morbidity in surgically treated patients and process outcomes.
Methods
We analysed an ambi-directional cohort from 16th March to June 30, 2020 (Pandemic cohort, PC) as compared to 2019 (Pre-pandemic cohort, PPC). We measured, new patient registrations, proportion of ‘within state’ patients vs ‘rest of India’, median time to treatment decision, proportion of patients seeking ‘second opinions’, modality of initial treatment (surgery/radiotherapy/chemotherapy), 30-day post-operative morbidity/mortality and conversion of inpatient-to ‘teleconsult’ in the PC.
Results
Between the 2 cohorts, new registrations declined from 235 to 69 (70% reduction). The percentage of ‘within state’ patients increased from 41.7% to 53.6% (11.9% increase). There was a decline in second opinion consults from 25% to 16%. The median time to decision-making decreased to 16 days in PC vs 20 days in PPC (20% reduction). Surgery was the first line of treatment in 40% as compared to 34% in the PPC with a mean time to surgery of 24 days in PC compared to 36 days in PPC (33% reduction). 66 surgeries were performed in the PC compared to 132 in the PPC. Thirty day post operative morbidity needing readmission remained similar (18% PC, vs 17% PPC). Perioperative intensive care remained similar in both cohorts. Teleconsultation was deemed medically safe in 92.8% (439/473 patients).
Conclusions
The COVID 19 pandemic has substantially reduced access and onset to cancer care. Post operative morbidity and mortality did not seem to worsen with triage. Teleconsultation is an effective tool in optimizing follow up strategy.
Keywords: COVID, Access, Delay, Bone tumor, Sarcoma, Treatment, Policy, Teleconsultation
1. Introduction
SARS CoV 2 pandemic has impacted over 200 countries, over 185 million cases and over 4 million deaths.1 Due to the density of population, low and middle-income countries (LMIC) socioeconomic status, relatively poor health care infrastructure, India was prone to a rapid spread infection and mortality.2 Health systems across the world, particularly in India have diverted resources and manpower toward COVID-19 management. It has significantly overwhelmed the system leading to worsening access and care seeking.
Cancer patients comprise a unique group that needs prompt treatment despite the challenges faced by healthcare resources to accommodate the large influx of COVID-19 patients. Interruption in services due to the diversion of resources to COVID care has been shown to affect oncologic outcomes.3 Travel restrictions, fear of contracting the disease, loss of livelihood and wages, contribute to widening the gap between need and delivery of care. Our institution had triage policies to deliver uninterrupted care to new and actively treated patients, and deferring in-person visits for patients on long term follow ups and providing tele-consults in lieu.4 These standard operating protocols(SOPs) evolved with pandemic experience adapting to workload, available manpower, infrastructure and evolving evidence on disease transmission and available treatment.
Based on the changing dynamics of disease spread and workload, policies will vary depending on diverse geographical locations and individual institutions. As these changing policies may often be guided by instinct and experience rather than evidence, continuously auditing the processes and outcomes allow for real-time feedback and improvement and help make them evidence-based.
At our institute, we adopted a series of policy changes to continue offering in-person consults for all new patients with untreated or cancers on active treatment while offering remote tele-consults primarily targeting long-term follow-up patients who missed appointments due to nationwide travel restrictions.
In this article, we measure variables for provision of continued access to cancer care across 2 cohorts (pre pandemic and pandemic). We also analysed demographics of the patients and 30 day outcomes in patients who underwent surgical management during the pandemic. We also describe a triage system that other institutes/units may adapt to suit their needs. The triage system outlined here provides context to the outcome measures.
2. Material and methods
We analysed an ambi-directional cohort from 16th March to June 30, 2020(Pandemic cohort, PC) as compared to 16th March to June 30, 2019 (pre-pandemic cohort, PPC). We measured, new patient registrations, proportion of ‘within state’ patients vs ‘rest of India’ (reflecting impact of travel restrictions), median time to treatment decision, proportion of patients seeking ‘second opinions’, modality of initial treatment (surgery/radiotherapy/chemotherapy), 30 day post-operative morbidity/mortality, conversion of in person-to ‘teleconsult’ in the pandemic cohort.
We utilized existing online electronic medical records (EMR) and outpatient appointment schedules to call all eligible patients. We offered to defer an avoidable visit in patients with stable disease and functional status. These patient contacts were documented in the EMR. Any interaction that prompted concern was encouraged to seek an in person consult at TMC. All active treatment schedules for post-operative patients were continued.
All patients underwent a preoperative real-time reverse transcription-polymerase chain reaction (RT-PCR) test from nasopharyngeal and oropharyngeal swabs at least 48 h before the scheduled surgery. They were isolated at triage areas in the hospital until the results. The tests were interpreted as negative, inconclusive, and positive as per standard criteria. Two inconclusive tests were treated as positive and re swabbed on day 14.
Patients who tested positive were admitted to a dedicated COVID-19 ward and monitored for symptoms and disease severity, asymptomatic patients were offered home isolation. We triaged our elective OR lists to defer patients requiring complex surgeries likely to require multiple blood transfusions and prolonged ICU stay(non COVID related) over 1 day(>1 day).
Morbidity was defined as any post or intra operative complication which required re-admission, prolonged intensive care due to or not due to perioperative COVID positivity, and delay (over 4 weeks from surgery for chemotherapy and over 8 weeks for adjuvant radiation) in adjuvant therapy. We measured the number of in-person long term follow up outpatient visits in PPC and compared it to in-person tele consult follow up patients PC. We defined long term-follow up patients as those beyond 6 months of surgery with no active adjuvant therapy.
We outline the changes implanted in patient flow and triage process to put our measurements in perspective in Table 1.
Table 1.
Adopted changes to facilitate continuing care.
| Site of intervention | Goals | Process change |
|---|---|---|
| Outpatient clinic |
|
Teleconsultation for long term follow ups |
| Operating room waiting list |
|
|
3. Results
Sixty-nine new BST DMG cases were registered from 16th March to June 30, 2020.
This was a drastic 70% drop compared with 235 in pre-COVID 2019 period (including second opinion consultation) (Table 2).
Table 2.
Geographical distribution of new patient registration.
| COVID cohort | Pre-COVID cohort | |
|---|---|---|
| Maharashtra | 37 (53.6%) | 98 (41.7%) |
| Rest of India | 30 (43.5%) | 131 (55.7%) |
| International | 0 (0%) | 4 (1.8%) |
| Unknown | 2 (2.9%) | 2 (0.8%) |
| Total | 69 | 235 |
The ratio of patients coming from Maharashtra (home state) and those from the rest of India increased to 1.2 in the PC (37:30) compared to 0.7 (98:135) in the PPC cohort again a drop reflecting impact of travel restrictions (Table 2). Notably, no new international patients were registered during this period.
The second opinion consults made up 25% of consultation in 2019 (58 of 235) which dropped to 16% in 2020 (11 of 69), reinforcing an access barrier.
Only 58 new patients were registered (excluding second opinion consultations) in the PC compared to 177 in the PPC. Our treatment protocol did not change during COVID and our out-patient compliance (patient continuing consultation till treatment decision) ratios were similar in both cohorts, 71% (41/58) in PC compared to (136/177) 77% in PPC.
Median time to treatment decision (from date of registration to date of final treatment decision) was 16 days in 41/58 (71%) patients of the PC compared to 20 days in 136/177 (77%) of the PPC. Further analyses are restricted to the cohort who had compliance till the treatment decision.
We treated 36 [one third compared to pre-COVID cohort (108)] patients with primaries of musculoskeletal system (including squamous cell cancers) in PC.
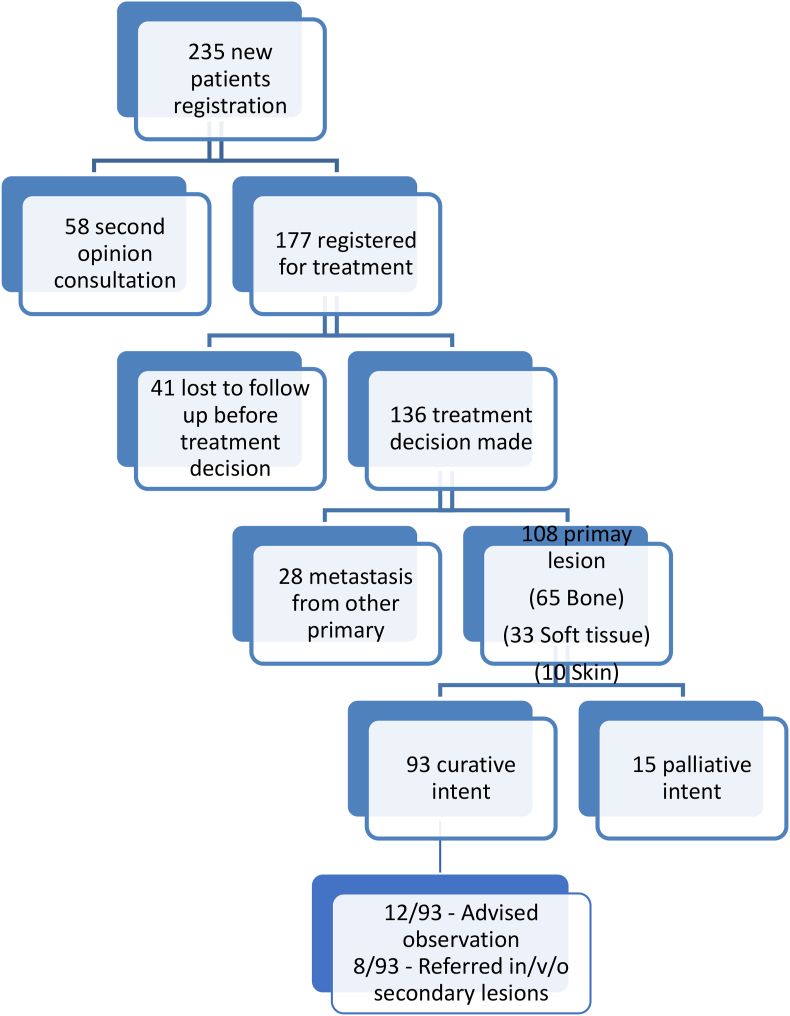
Primaries of the musculoskeletal system treated with palliative intent in both cohorts were similar; 6/36 (17%) in the PC compared to 15/108 (14%) in the PPC. The remaining analyses is restricted to 30 from the PC and 93 from the PCC which were treated with curative intent (Fig. 1 and Fig. 2).
Fig. 1.
New BST registration (PC)
MSKS: Musculoskeletal System, STL: Soft tissue lesion.
Fig. 2.
New BST registration (PPC)
MSKS: Musculoskeletal System, STL: Soft tissue lesion.
The proportion of patients with Chemotherapy as the first line of treatment was similar in both cohorts, 10/30 (33%) patients in the PC and 31/93 (33%) PPC. Time to start chemotherapy (after treatment decision) for those treated at our hospital was 5 days in PC [1 lost to follow up (LTFU) excluded] compared to 9 days (2 LTFU excluded) in the PPC (Table 3).
Table 3.
Comparison of PC and PPC results.
| Variables | Results | |
|---|---|---|
| Pandemic cohort | Pre-pandemic cohort | |
| Number of registrations | 69 | 235 |
| Maharashtra vs Rest of India | 37 vs 30 (2 - unknown) | 98 vs 131 (2 – unknown) |
| Second opinion | 11 (16%) | 58 (25%) |
| First modality of treatment | Chemotherapy – 33% | Chemotherapy – 33% |
| Surgery – 40% | Surgery – 34% | |
| Radiotherapy – 3% | Radiotherapy – 6% | |
| Rest – Referred out | Rest – Referred out | |
| Mean time to initiate treatment | 16 days | 20 days |
| Patients underwent surgery | 66 | 132 |
| Meantime to surgery | 24 days | 36 days |
| Meantime to chemotherapy | 5 days | 9 days |
| 30 day morbidity/mortality | 12/66 (18%) | 23/132 (17%) |
Surgery was the first line of treatment in 12/30 (40%) in the PC and 32/93 (34%) in the PPC. We referred out only 2/12 (17%) of patients in the PC as compared to 19/32 (59%) in the PPC. Meantime to surgery was 24 days in the PC (1 LTFU excluded and 1 turned COVID positive pre-surgery) compared to 36 days (5 LTFU excluded) in the PPC (Table 3).
3.1. Surgeries
We performed 66 surgeries in PC, compared to 132 in the PPC (50% reduction). In PC, we prioritized limb salvage surgeries which comprised 75% (52/69) of all surgeries compared to 60% (79/132) in the PPC. Surgeries requiring post-operative ICU care (>1 day), requiring multiple blood transfusions, duration >8 h, viz. free flaps and internal hemipelvectomies were deferred during the initial period of the PC, to triage manpower, ICU and scarce blood product utilization, such surgeries were 4/66 (6%) surgeries in PC compared to 12/132 (9%) in PPC cohort Thirty day post operative morbidity was similar for both cohort 12/66 (18%) in COVID cohort compared to 23/132 (17%) in pre COVID cohort. There was no 30 day mortality in either cohort. Infection(including culture positive or unequivocal clinical, deep and superficial) (4/66 in PC and 10/132 in PPC) and soft tissue complications (4/66 in PC and 8/132 in PPC) were leading cause of morbidity with comparable proportion in both cohorts. Comparison of PC and PPC variables are given in Table 3.
4. Discussion
COVID-19 pandemic has impacted the health care system significantly. Poor health infrastructure, fewer trained personnel, travel restrictions, loss of wages and jobs are a few of the major factors which lead to compromised health care delivery across the country.5 Major resources were diverted to bridge this gap therefore care of patients suffering from non-COVID illness especially cancer was compromised.3 Non-standardization of oncology care in the COVID era due to the unforeseen nature of pandemic crisis also contributed to compromised in cancer care.6 Predicted cancer-related mortality due to delayed or denied care, prompted various oncology institutes to continue cancer care even in peak pandemic.4
Our Institute continued routine, emergency oncologic care and COVID care under one roof, with no breaks throughout the pandemic, with safe and sustainable outcomes. The administrative measures taken to enable this have been published elsewhere.4 We reported early outcomes of the major cancer surgery performed through the pandemic.7
The demography of patients treated in the pandemic year was different than the control group of 2019. We had less than one-third of new case registrations, 69 cases from March 16, 2020 to June 30, 2020 compared to 235 new case registrations during the same period in 2019, reflecting our patient pool that has a significant nationwide footprint and an inevitable pool of patients that were denied care. We are likely to see its impact on mortality and stage migration in the coming times.
We had younger patients, lower ASA grades, lesser predicted blood loss and lower hospital stay. This was aligned with the diversion of resources to pandemic care and shortage of blood products across the city,8 as a consequence of the cancellation of blood donation camps due to social distancing norms. Staff sparing, attrition and travel restrictions for patients due to a lockdown in the early pandemic days led to prudent reduced allocated OR time, resource optimization, leading to a lesser number of surgeries. Rationing care through the pandemic has made continuity of cancer care for all a casualty. Continuing cancer care through the pandemic was a conscious and proactive decision made by Tata Memorial Centre.4 Department of BST saw 69 new registrations in 2020 and any conscious slowdown of care would invariably have led to suboptimal cancer outcomes. Prioritizing care in patients with curable cancers guided the triage process. Our study did not measure the societal and financial impact of delaying this care in cancer survivors who arguably contribute more to the labour economy.
The process and philosophy were extended to outpatient visits to reduce the in-transit and in-hospital risk of contracting disease. This attempt at reducing overcrowding is crucial in LMICs, especially institutes like TMC, where crowd management and social distancing is an unsurmountable challenge. We encouraged teleconsultation for survivors who have been disease-free for over 1 year. Patients on active treatment, adjuvant or neo-adjuvant, at a remote centre, had teleconsultation to maintain continuity of care. A dedicated point of care team was deputed for organizing teleconsultations at an institutional level. The British Orthopaedic Association has suggested that patient-initiated follow-up should be the standard with appointments given out only in unavoidable circumstances.9 Existing appointments should either be cancelled, postponed or conducted remotely via tele consultation. Sarcoma treatment during the covid-19 pandemic is a new challenge.10 This patient population is often immunocompromised and potentially more susceptible to viral complications. Government guidelines highlight the need to minimize patient exposure to unnecessary hospital visits. However, those guidelines lack practical recommendations on ways to manage triage and diagnosis of new cancer patients. Furthermore, there are no reports on the efficiency of the guidelines. One of the main issues in treating musculoskeletal tumours is the complexity and variability of presentation. We offer a triage model, used in a quaternary-referral musculoskeletal oncology centre, that allows us to maintain an open pathway for referral of new patients while minimizing exposure risks. A multidisciplinary approach and analysis of existing investigations allow for a pre-clinic evaluation. The model identifies 3 groups of patients: Patients with suspected high-grade malignancy, or benign cases with aggressive features, both in need of further evaluation in the clinic and prompt treatment, Patients with low-grade malignancy and benign cases whose treatment is not urgent, that are managed during the pandemic by telemedicine, with reassurance and information about their illness or Patients who can be managed by their local medical professionals In comparison to a pre-pandemic period, that approach resulted in a higher ratio of malignant-to-benign conditions for new patients seen in the clinic (3:4 vs. 1:3 respectively), thus using available resources more efficiently and prioritizing patients with suspected high-grade malignancy. We believe that this triage system could be applied in other surgical oncology fields during a pandemic.
All patients who needed revision of non-critical reconstructive failure were deferred to prioritize patients with active cancer treatment. However 30 day morbidity was same for both cohorts as SOP were followed stringently during COVID era too, and we infer, that safe continuity of care is an achievable and sustainable goal for most institutes. Patients were not able to reach us due to travel restriction and hence we were able to accommodate newly registered patients for surgery in a shorter time (24 days in PC compared to 36 days in PPC).
With the novel coronavirus disease (COVID-19) being declared a global pandemic by the World Health Organization, the Indian healthcare sector is at the forefront to deliver optimal care. Patients with cancer especially are at serious risk for increased chances of morbidity and mortality due to their immunocompromised state. Currently there is a paucity of definitive guidelines for the management of sarcomas during the pandemic in a resource-constrained and diverse population setting like India. Health care professionals from various specialties involved in the management of sarcomas have collaborated to discuss various aspects of evidence-based sarcoma management during the COVID-19 pandemic.6 This article provides structured recommendations for Health care personals to adapt to the situation, optimize treatment protocols with judicious use of all resources while providing evidence-based treatment for sarcoma patients.
Being retrospective in nature, over a relatively short time period, this ambi-directional observational cohort study may underestimate the denial or deferral of care as we were unable to document lack of care, stage migration, denied care in the population who were unable to reach us. However, this data does point toward the care gap that had widened through the pandemic despite our best efforts to ameliorate it. This was demonstrated in the first National Cancer Grid study conducted in India, across over 40 institutes.11
Pandemic preparedness has led to an acute overhaul and optimization of many legacy inefficiencies within hospital systems. Despite the best efforts of institutes to ensure continued care, the widening gap of availability of care and worsened access to care is likely to worsen cancer outcomes in the coming years. These best practices could also be used in pandemic free times to maximize efficiency, cost-effectiveness without compromising patient safety or care.
Contributor Information
Ashwin Prajapati, Email: ashwinprajapatitmc@gmail.com.
Srinath Gupta, Email: srigups@gmail.com.
Prakash Nayak, Email: nayakprakash@gmail.com.
Ashish Gulia, Email: aashishgulia@gmail.com.
Ajay Puri, Email: docpuri@gmail.com.
References
- 1.Alanagreh L., Alzoughool F., Atoum M. vol. 9. 2020. (The Human Coronavirus Disease Covid-19: Its Origin, Characteristics, and Insights into Potential Drugs and its Mechanisms). Pathogens. MDPI AG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rammohan A., Rela M. COVID-19: could India still escape? Journal of Global Health. 2020 Jun;10(1) doi: 10.7189/jogh.10.010372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jazieh A.R., Akbulut H., Curigliano G. Impact of the COVID-19 pandemic on cancer care: a global collaborative study. JCO Global Oncology. 2020 Nov 28;(6):1428–1438. doi: 10.1200/GO.20.00351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pramesh C.S., Badwe R.A. Cancer management in India during covid-19. N Engl J Med. 2020 May 14;382(20):e61. doi: 10.1056/NEJMc2011595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goel I., Sharma S., Kashiramka S. Effects of the COVID-19 pandemic in India: an analysis of policy and technological interventions. Health Policy and Technology. 2021 Mar;10(1):151. doi: 10.1016/j.hlpt.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gulia A., Tiwari A., Arora R.S., Gupta S., Raja A. Sarcoma care practice in India during COVID pandemic: a nationwide survey. Indian J Orthop. 2020 Dec;54(Suppl 2):350–357. doi: 10.1007/s43465-020-00206-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shrikhande S v., Chaudhary A, Krishnamurthy A, et al. Surgical oncology practice in the wake of COVID-19 crisis. Vol. 11, Indian Journal of Surgical Oncology. p. 762–768. [DOI] [PMC free article] [PubMed]
- 8.Divya N.S., Vanishree H.R., Jaikar S.K.B. Impact of COVID 19 pandemic on blood transfusion services at a rural based district Hospital Blood-Bank, India. Indian J Pathol Oncol. 2021 Feb 15;8(1):50–54. [Google Scholar]
- 9.British Orthopaedic guidelines Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. https://www.boa.ac.uk/resources/covid-19-boasts-combined1.html
- 10.ESMO guidelines Sarcomas in the COVID-19 era | ESMO. https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic/sarcomas-in-the-covid-19-era
- 11.Ranganathan P., Sengar M., Chinnaswamy G. Impact of COVID-19 on cancer care in India: a cohort study. Lancet Oncol. 2021 Jul 1;22(7):970–976. doi: 10.1016/S1470-2045(21)00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]