Abstract
Widespread vaccination remains the best option for controlling the spread of COVID-19 and ending the pandemic. Despite the considerable disruption the virus has caused to people’s lives, many people are still hesitant to receive a vaccine. Without high rates of uptake, however, the pandemic is likely to be prolonged. Here we use two survey experiments to study how persuasive messaging affects COVID-19 vaccine uptake intentions. In the first experiment, we test a large number of treatment messages. One subgroup of messages draws on the idea that mass vaccination is a collective action problem and highlighting the prosocial benefit of vaccination or the reputational costs that one might incur if one chooses not to vaccinate. Another subgroup of messages built on contemporary concerns about the pandemic, like issues of restricting personal freedom or economic security. We find that persuasive messaging that invokes prosocial vaccination and social image concerns is effective at increasing intended uptake and also the willingness to persuade others and judgments of non-vaccinators. We replicate this result on a nationally representative sample of Americans and observe that prosocial messaging is robust across subgroups, including those who are most hesitant about vaccines generally. The experiments demonstrate how persuasive messaging can induce individuals to be more likely to vaccinate and also create spillover effects to persuade others to do so as well.
The first experiment in this study was registered at clinicaltrials.gov and can be found under the ID number NCT04460703. This study was registered at Open Science Framework (OSF) at: https://osf.io/qu8nb/?view_only=82f06ecad77f4e54b02e8581a65047d7.
1. Introduction
The global spread of COVID-19 created an urgent need for safe and effective vaccines against the disease. However, even though several successful vaccines have become available, vaccine hesitancy in the general population has the potential to limit the efficacy of vaccines as a tool for ending the pandemic. For instance, in the United States, the public’s willingness to receive a vaccine has declined from 72 % saying they would be likely to get a COVID-19 vaccine in May 2020 to 60 % of people reporting that they would receive a vaccine as of November 2020 [1]. Given the considerable amount of skepticism about the safety and efficacy of a COVID-19 vaccine, it has become increasingly important to understand how public health communication can play a role in increasing COVID-19 vaccine uptake.
Vaccination is both a self-interested and a prosocial action [[2], [3], [4], [5], [6], [7], [8], [9]]. By getting vaccinated, people protect themselves from a disease, but they also reduce the chance that they become a vector through which the disease spreads to others. If enough people receive a vaccine, the population gains protection through herd immunity, but this also creates an incentive for an individual to not get vaccinated because they can forgo vaccination and receive protection from others who do vaccinate. Recent research on vaccination in general has demonstrated that people view vaccination as a social contract and are less willing to cooperate with those who choose not to get inoculated [10]. This work also implies that highlighting the reputational costs of choosing not to vaccinate could be an effective strategy for increasing uptake. Further, appeals to herd immunity and the prosocial aspect of vaccination have been shown to increase uptake intentions [[11], [12], [13]], but emphasizing the possibility of free riding on other’s immunity reduces the willingness to get vaccinated [14].
Focusing specifically on vaccination against COVID-19, recent studies have found that messages that explain herd immunity increase willingness to receive a vaccine [15] and reduces the time that people would wait to get vaccinated when a vaccine becomes available to them [16]. However, other work has found that prosocial appeals did not increase average COVID-19 vaccination intentions [17] and the effect of prosocial concerns was present in sparsely populated places, but absent in more densely populated ones [18]. Given the current state of evidence, it is unclear whether appealing to getting a COVID-19 vaccine as a way to protect others will increase willingness to vaccinate.
Viewing vaccination through the lens of a collective action problem suggests that in addition to increasing individuals’ intentions to receive a vaccine, effective public health messages would also increase people’s willingness to encourage those close to them to vaccinate and to hold negative judgments of those who do not vaccinate. By encouraging those close to them to vaccinate, people are both promoting compliance with social norms and increasing their own level of protection against the disease. Also, by judging those who do not vaccinate more negatively, they apply social pressure to others to promote cooperative behavior. This would be consistent with theories of cooperation, like indirect reciprocity or partner choice, that rely on free riders being punished or ostracized for their past actions to encourage prosocial outcomes [[19], [20], [21], [22], [23]]. Thus, effective messaging could have outsized effects on promoting vaccination if it both causes people to vaccinate themselves and to encourage those around them to do so.
We conducted two pre-registered experiments to study how different persuasive messages affect intentions to receive a COVID-19 vaccine, willingness to persuade friends and relatives to receive one, and negative judgments of people who choose not to vaccinate. In the first experiment, we tested the efficacy of a large number of messages against an untreated control condition (see Table 1 for full text of messages). A subgroup of the messages in Experiment 1 drew on this collective action framework of vaccination and emphasized who benefits from vaccination or how choosing not to vaccinate hurts one’s social image. A second subgroup drew on contemporary arguments about restrictions on liberty and economic activity during the COVID-19 pandemic. In Experiment 2, we retested the most effective messages from Experiment 1 on a nationally representative sample of American adults. By utilizing this test and re-test design, we guard against false positive results that are observed by chance among the large number of messages tested in Experiment 1. In our analysis of both experiments, we examined whether specific messages were more effective among certain subgroups of the population.
Table 1.
Experimental treatment messages for Experiment 1 and Experiment 2. All messages add the prose in the table to the content of the Baseline informational control. All of the messages in the table were tested in Experiment 1. The messages that are bolded were retested in Experiment 2.
| Treatment Name | Full Text |
|---|---|
| (1) Baseline Informational Control | To end the COVID-19 outbreak, it is important for people to get vaccinated against COVID-19 whenever a vaccine becomes available. Getting the COVID-19 vaccine means you are much less likely to get COVID-19 or spread it to others. Vaccines are safe and widely used to prevent diseases and vaccines are estimated to save millions of lives every year. |
| (2) Self-Interest | Stopping COVID-19 is important because it reduces the risk that you could get sick and die. COVID-19 kills people of all ages, and even for those who are young and healthy, there is a risk of death or long-term disability. Remember, getting vaccinated against COVID-19 is the single best way to protect yourself from getting sick. |
| (3) Community Interest | Stopping COVID-19 is important because it reduces the risk that members of your family and community could get sick and die. COVID-19 kills people of all ages, and even for those who are young and healthy, there is a risk of death or long-term disability. Remember, every person who gets vaccinated reduces the risk that people you care about get sick. While you can’t do it alone, we can all protect every-one by working together and getting vaccinated. |
| (4) Community Interest + Guilt | (3) + Imagine how guilty you will feel if you choose not to get vaccinated and spread COVID-19 to someone you care about. |
| (5) Community Interest + Embarrassment | (3) + Imagine how embarrassed and ashamed you will be if you choose not to get vaccinated and spread COVID-19 to someone you care about. |
| (6) Community Interest + Anger | (3) + Imagine how angry you will be if you choose not to get vaccinated and spread COVID-19 to someone you care about. |
| (7) Not Bravery | Soldiers, fire-fighters, EMTs, and doctors are putting their lives on the line to serve others during the COVID-19 outbreak. That's bravery. But people who refuse to get vaccinated against COVID-19 when there is a vaccine available because they don't think they will get sick or aren't worried about it aren't brave, they are reckless. By not getting vaccinated, you risk the health of your family, friends, and community. There is nothing attractive and independent-minded about ignoring public health guidance to get the COVID-19 vaccine. Not getting the vaccine when it becomes available means you risk the health of others. To show strength get the vaccine so you don't get sick and take resources from other people who need them more, or risk spreading the disease to those who are at risk, some of whom can’t get a vaccine. Getting a vaccine may be inconvenient, but it works. |
| (8) Trust in Science | Getting vaccinated against COVID-19 is the most effective means of protecting your community. The only way we can beat COVID-19 is by following scientific approaches, such as vaccination. Prominent scientists believe that once available, vaccines will be the most effective tool to stop the spread of COVID-19. The people who reject getting vaccinated are typically ignorant or confused about the science. Not getting vaccinated will show people that you are probably the sort of person who doesn’t understand how infection spreads and who ignores or are confused about science. |
| (9) Personal Freedom | COVID-19 is limiting many people’s ability to live their lives as they see fit. People have had to cancel weddings, not attend funerals, and halt other activities that are important in their daily lives. On top of this, government policies to prevent the spread of COVID-19 limit our freedom of association and movement. Remember, each person who gets vaccinated reduces the chance that we lose our freedoms or government lockdowns return. While you can’t do it alone, we can all keep our freedom by getting vaccinated. |
| (10) Economic Freedom | COVID-19 is limiting many people’s ability to continue to work and provide for their families. People have lost their jobs, had their hours cut, and lost out on job opportunities because companies aren’t hiring. On top of this, government policies to prevent the spread of COVID-19 have stopped businesses from opening up. Remember, each person who gets vaccinated reduces the chance that we lose our freedoms or government lockdowns return. While you can’t do it alone, we can all keep our ability to work and earn a living by getting vaccinated. |
| (11) Community Economic Benefit | Stopping COVID-19 is important because it is wreaking havoc on our economy. Thousands of people have lost their jobs and are unable to pay their bills. Many others have been laid off by their employers and do not know when they will be called to return to work. Remember, every person who gets vaccinated reduces the risk that someone else gets sick. While you can’t do it alone, we can all end this outbreak and strengthen the national economy by working together and getting vaccinated. |
Experiment 1 was fielded in early July 2020. Participants were randomly assigned to either a placebo control condition in which they read a story about the effectiveness of bird feeders or one of eleven treatment messages. The first message is a Baseline informational control condition that describes how it is important to receive a vaccine to reduce your risk of contracting COVID-19 or spreading it to others. Informational messages have been shown to be effective at increasing COVID-19 vaccine uptake intentions [24]. This message also emphasized that vaccines are safe and estimated to save millions of lives per year. The other messages add additional content to this baseline message.
The subgroup of messages that emphasized collective action varied who would benefit from vaccination or what other people might think of someone who chooses to be a free rider by not vaccinating. Focusing on who benefits from vaccination, the second message invoked Self Interest and reinforced the idea that vaccination is a self-protecting action (“Remember, getting vaccinated against COVID-19 is the single best way to protect yourself from getting sick.”). The third message, Community Interest, instead argued that vaccination is a cooperative action to protect other people (“Stopping COVID-19 is important because it reduces the risk that members of your family and community could get sick and die.”). This message also invoked reciprocity by emphasizing the importance of every-one working together to protect others.
The fourth, fifth, and sixth messages added an invocation of an emotion, Guilt, Embarrassment, or Anger, to the Community Interest message. These messages prompted people to think about how they would feel if they chose not to get vaccinated and spread COVID-19 to someone else in the future. Emotions are thought to play a role in cooperation, either by motivating an individual to take an action because of a feeling that they experience or restraining them from taking an action because of the emotional response it would provoke in others [[25], [26], [27]]. Further, anticipated emotional states have been shown to promote various health behaviors, like vaccination [[28], [29]].
The seventh and eighth messages evoked concerns about one’s reputation and social image, which influences their attractiveness as a cooperative partner to others. The seventh, a Not Bravery message, reframed the idea that being unafraid of the virus is not a brave action, but instead selfish, and that the way to demonstrate bravery is by getting vaccinated because it shows strength and concern for others (“To show strength get the vaccine so you don’t get sick and take resources from other people who need them more”). The eighth message was a Trust in Science message that highlights that scientists believe a vaccine will be an effective way of limiting the spread of COVID-19. This message suggests that those who do not get vaccinated do not understand science and signal this ignorance to others (“Not getting vaccinated will show people that you are probably the sort of person who doesn’t understand how infection spreads and who ignores or are confused about science.”).
The final three messages drew on concerns about restrictions on freedom and economic activity that were widespread during the COVID-19 pandemic. A pair of messages focused on how vaccination would allow for a restoration of Personal Freedom (“Government policies to prevent the spread of COVID-19 limit our freedom of association and movement”) or Economic Freedom (“Government policies to prevent the spread of COVID-19 have stopped businesses from opening up”). These messages take a value that is commonly invoked in individuals’ decision to not vaccinate [[30], [31]] and reframed vaccination as something that would actually restore freedoms that had been taken away. The final message, Community Economic Benefit, argues that a vaccine will help return people’s financial security and strengthen the economy This message is similar to the Community Interest messages that are described above, but instead focuses on cooperating to restore the economy (“We can all end this outbreak and strengthen the national economy by working together and getting vaccinated”).
2. Results
2.1. Experiment 1 results
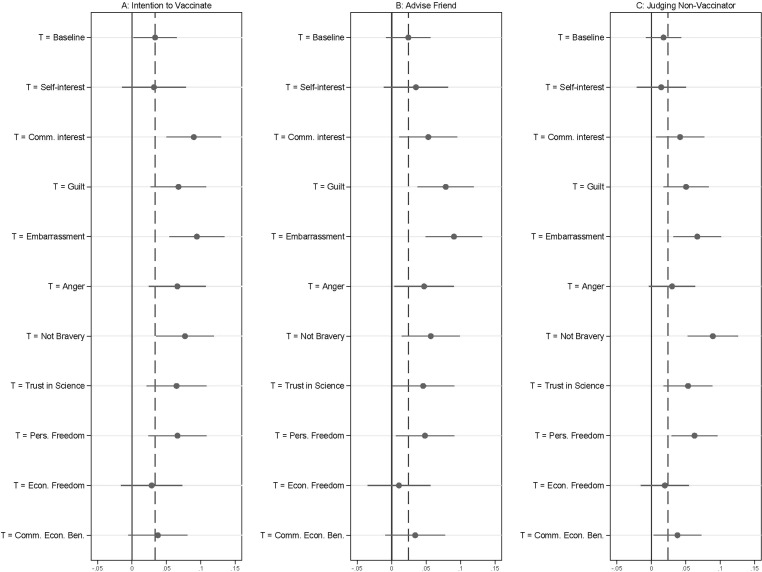
Panel A of Fig. 1 plots the effect of each vaccine message relative to the untreated control group on intention to vaccinate. The intention to vaccinate measure was formed by combining responses to a question about the likelihood of getting a COVID-19 vaccine within the first 3 months that one is available with a question about getting a vaccine within the first year that one is available. Specifically, for respondents who did not answer that they were very likely to vaccinate within the first three months that a vaccine is available to them, we asked how likely they would be to vaccinate within a year. This measure coded those who are very likely in the first three months at the highest value on the scale followed by very likely within a year descending down to very unlikely within the first year. Analyzing the vaccination item separately does not substantively change the results. All outcome variables were scored 0 to 1, with higher values indicating greater willingness to endorse the pro-vaccine action or belief (Underlying regressions appear in Table S1 and unless otherwise noted, all analyses were pre-registered).
Fig. 1.
Experiment 1. Messages that frame vaccination as a cooperative action to protect others or emphasize how non-vaccination might negatively affect one’s social image increase reported willingness to advise a friend, and judgment of non-vaccinators. Panel A displays treatment effects for the combined measure of intention to vaccinate, Panel B displays the advise a friend outcome, and Panel C displays the judging a non-vaccinator outcome. Treatment effects for both panels were estimated using OLS regression that included covariates. The effects displayed are a comparison against the placebo control baseline and are presented with 95% confidence intervals. The dashed vertical line is the effect of the Baseline informational control for each outcome.
Compared to the untreated control, the Baseline informational message was associated with modest increases in intention to vaccinate by 0.034 units (95 % CI:0.002, 0.065; p < .05). This effect represents an increase of approximately 6 % in the scale score compared to the outcome in the control condition.
By comparison, the Community Interest, Community Interest + Guilt, Embarrassment, or Anger, Not Bravery, Trust in Science and Personal Freedom messages all produce larger effects, at least qualitatively, than the Baseline informational message on the intention to vaccinate outcome. Effects for the Self-Interest, Economic Freedom, and Community Economic benefit messages were not consistently distinguishable from the untreated control group outcomes, and their effects were indistinguishable from the effects of the Baseline informational message.
The most promising messages were the Not Bravery, Community Interest, and Community Interest + Embarrassment messages. These messages were associated with effects that were statistically distinguishable from the untreated control group (Not Bravery: 0.077 units, 95 % CI: 0.035, 0.119; p < .01, Community Interest: 0.090 units, 95 % CI: 0.050, 0.129; p < .01, Community Interest + Embarrassment: 0.094 units, 95 % CI: 0.054, 0.134; p < .01) at p < .01. Moreover, their effects were always more than twice as large as the Baseline informational treatment and these differences were significant at p < .05 (two-tailed tests). The effects of the Trust in Science message and the Personal Freedom message were not statistically significant when compared to the Baseline informational message.
To put the magnitudes of the effects into context, we re-estimated our analysis after dichotomizing the intended vaccine uptake measure such that those who report they were “somewhat” or “very” likely to get the vaccine, either with three months or a year, are coded as 1 and those who do not are coded 0 (this analysis was not pre-registered). This produced a predicted rate of intended vaccination in the control group of 58.2 %. Respondents who read the Baseline informational message were 7.4 percentage points (95 % CI: 2.9 pp, 12.0 pp; p < .01) more likely to receive a vaccine. Among those assigned to the Not Bravery or Community Interest messages it was predicted to increase by 10.4 percentage points and 12.7 percentage points (Not Bravery: 95 % CI: 4.3 pp, 16.4 pp; p < .01, Community Interest: 95 % CI: 6.7 pp, 18.7 pp; p < .01) respectively, while among those assigned to the Community Interest + Embarrassment message it was predicted to increases by 15.9 percentage points (95 % CI: 10.2 pp, 21.6 pp; p < .01). This last difference was substantively large, representing a proportional increase of 27 % (0.159/0.582) compared to the control condition and a 13 % increase compared to the Baseline informational condition (0.159-0.074)/(0.582 + 0.074).
Turning to the other regarding outcomes that focused on spurring action by others, Panel B plots the effects of each vaccine message relative to the untreated control for advising a friend to receive a vaccine and Panel C plots the effects for negatively judging someone who refuses to receive one. Here, the effect of the Baseline informational intervention was modest and statistically insignificant. However, the Not Bravery, Trust in Science, Personal Freedom, Community Interest, Community Interest + Guilt, and Community Interest + Embarrassment messages had larger effects on both outcomes that were statistically distinguishable from the control outcome.
The most promising message was the Community Interest + Embarrassment message for the advise a friend outcome, which was associated with a 0.09 unit increase in the scale outcome (95 % CI: 0.049, 0.132; p < .01 two-tailed test), an effect that represents an increase of 27 % compared to the mean scale score in the control group. The effect was 0.067 units compared to the Baseline informational message (95 % CI: 0.027, 0.105; p = .001, two-tailed test). We conducted a similar exercise to the one describe above to gauge the relative magnitude of these treatment effects. For the Community Interest + Embarrassment message we estimated a 15 percentage point increase (95 % CI: 0.088, 0.209; p < .01, two tailed test,) in a binary intention to advise others to vaccinate outcome, a proportional increase of 27 % compared to the control group baseline of 53 % (0.15/0.53). This effect was also 6 percentage points larger than the effect of the baseline message (95 % CI: 0.008, 0.121; p = .03, two-tailed test).
The most promising outcome for the negative judgment of non-vaccinators was the Not Bravery message, which had an effect of 0.09 scale points (95 % CI: 0.052, 0.126; p < .01, two-tailed test) compared to the untreated control and 0.072 scale points versus the Baseline information (95 % CI: 0.037, 0.106; p < .01 Baseline message, two-tailed tests). This corresponded to a 21 % increase compared to the scale outcome in the control group (0.09/0.43). These are both substantively and statistically meaningful effects. The Community Interest, Community Interest + Guilt, Community Interest + Embarrassment, Trust in Science, and Personal Freedom messages all produced effects that were statistically distinguishable from the control condition.
We also investigated the robustness of these findings to sample restrictions and whether certain subgroups were more responsive to specific treatment messages (reported in Figures S2-S12). Results were generally robust to restricting the sample to those who were over the 10th percentile and under the 90th percentile for completion time. For subgroup analyses, those scoring low in liberty endorsement appeared more responsive to the Baseline treatment and to the Not Bravery message than are those who scored high in liberty endorsement. Those who report being less likely to take risks appeared robustly more responsive to the Not Bravery message than those who were high in risk taking. Those who were high in risk taking appear more responsive to the Personal Freedom message with regard to their own behavioral intentions. Certain groups appeared generically easier to persuade (Democrats rather than Republicans, an important divide that has emerged during the pandemic [32], and Women rather than Men), but there were no clear differences in which treatments appeared most effective across these groups. We explored the robustness of these subgroup differences in Experiment 2.
Taken together, the most successful messages in Experiment 1 were those that were theoretically motivated by viewing vaccination as a collective action problem. Consistent with previous work that demonstrates that prosocial appeals are effective in promoting vaccination, the Community Interest message and Community Interest + Guilt, Embarrassment, or Anger messages increased COVID-19 vaccine uptake intentions. Moving beyond who benefits from vaccination, the Not Bravery and Trust in Science messages that invoked concerns about one’s social image if they choose not to vaccinate also increased uptake intentions. All of the collective action oriented messages increased intentions to advise a friend to vaccinate and negative judgments of those who do not, potentially creating spillover effects that induce others to vaccinate. In addition to this subgroup of messages, we found that reframing vaccination as a way to restore freedom was also effective, though the other messages motivated by contemporary debates about the pandemic were generally no more effective than the Baseline condition.
2.2. Experiment 2 results
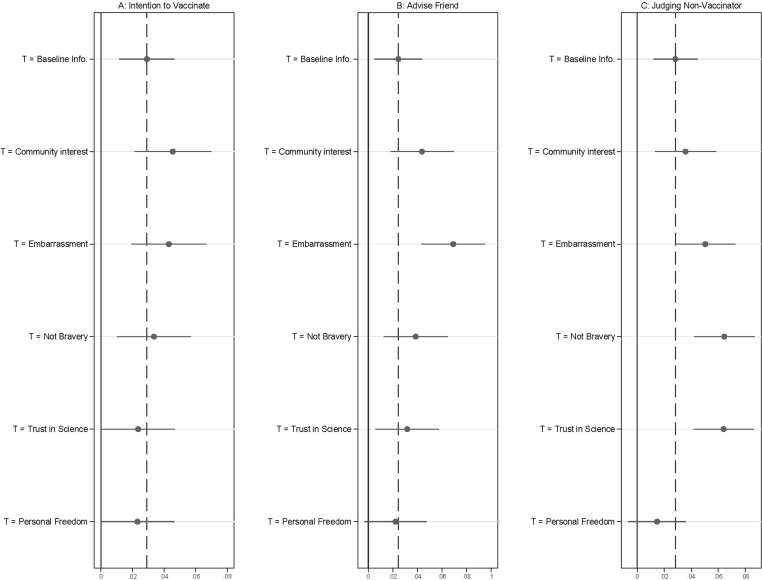
Experiment 2 tested the subset of the best performing messages from Experiment 1 on a nationally representative sample in September 2020. Notably, in the several month period between Experiment 1 and Experiment 2, the public had grown increasingly skeptical of a potential COVID-19 vaccine [1]. Panel A of Fig. 2 plots the effect of each vaccine message, relative to the untreated control group, on the same measure of intention to vaccinate used in Experiment 1. (The model specifications shown in the figure were from our pre-registered specifications, underlying regression appear in Table S2.). Given that we observed the messages from Experiment 1 were effective at increasing vaccine uptake, we pre-registered directional hypotheses for Experiment 2 that tested whether the effects could be replicated on a nationally representative sample. Accordingly, we report one-tailed hypothesis tests and 90 % confidence intervals in the results presented below. Results largely confirmed the patterns observed in Experiment 1.
Fig. 2.
Experiment 2. The Not Bravery, Community Interest, and Community Interest + Embarrassment messages increase both intentions to vaccinate and other-regarding outcomes. Panel A displays treatment effects for intentions to vaccinate, Panel B displays the advise a friend, and Panel C displays the judging a non-vaccinator outcomes. Treatment effects for both panels were estimated using OLS regression that included covariates. The effects displayed are a comparison against the placebo control baseline and are presented with 90 % confidence intervals. The dashed vertical line is the effect of the Baseline informational control for each outcome.
The Baseline informational treatment was associated with a modest increase, 0.029 units, in intention to vaccinate (90 % CI: 0.011, 0.046; p < .01, one-tailed test). This effect was a 6 % increase of the observed scale outcome in the untreated control group.
The Community Interest and Community Interest + Embarrassment messages were associated with qualitatively larger effects on intended vaccine uptake. These messages were associated with increases of 0.045 units (90 % CI: 0.021, 0.070; p < .01, one-tailed test) and 0.043 units (90 % CI: 0.019, 0.067; p < .01, one-tailed test), respectively. As with Experiment 1, we recoded those who stated they were “somewhat” or “very” likely to receive the vaccine as 1 and those who did not report that they were likely to receive it as 0 (this analysis was not pre-registered: for consistency we report 90 % confidence intervals). This binary measure produced a predicted rate of intended vaccination in the control group of 51.4 %. Intended uptake was 3.3 percentage points higher in the Baseline information condition (90 % CI: 0.5 pp, 6.0 pp; p < .05, one-tailed test), 3.5 percentage points higher in the Community Interest + Embarrassment condition (90 % CI: −0.1 pp, 7.0 pp; p = .06, one-tailed test), and 5 percentage points higher in the Community Interest condition (90 % CI: 1.3 pp, 0.8.7 pp; p < .05, one-tailed test). The latter effect was proportionally large—10 % compared to the baseline predict rate in the control group (0.050/0.514).
On average, the Not Bravery, Trust in Science, and Personal Freedom messages were approximately as effective as the informational content to which they were added in increasing intention to vaccinate, which differs from Experiment 1 where they modestly outperformed the Baseline informational condition.
Turning to other regarding outcomes, Panel B of Fig. 2 plots effects for advice given to others and Panel C does so for negative judgments of non-vaccinators. The Baseline informational treatment was again associated with statistically significant increases in each outcome. For these outcomes, the Not Bravery, Trust in Science, and both Community Interest messages produced effects that were at least descriptively larger than the Baseline treatment. The effects for the Personal Freedom message were smaller than the Baseline informational treatment, a result that again diverged from Experiment 1.
In terms of advising others to vaccinate, the most effective message was the Community Interest + Embarrassment message, which was also the most effective message in Experiment 1. This effect was 0.07 scale points (90 % CI: 0.043, 0.095; p < .01, one-tailed test), an increase of 14 % compared to the control group average scale score of 0.51 (0.07/0.51). This effect was also statistically distinguishable from the effect of the Baseline informational treatment (difference = 0.045; 90 % CI: 0.020, 0.069; p < .01, one-tailed test). When dichotomizing the advise a friend outcome to better describe the magnitude of the effect, we estimated that the Community interest + Embarrassment message was associated with a 10 percentage point increase (90 % CI: 0.064, 0.140; p < .01, one-tailed test) in intention to advise others to vaccinate compared to the control group, a proportional increase of 27 % compared to the control group baseline of 38 % (0.10/0.38). This effect was approximately 6 points larger than the effect of the Baseline message (90 % CI: 0.026, 0.099; p < .01, one-tailed test).
In terms of judging non-vaccinators, the largest effects were for the Not Bravery and Trust in Science messages, with each effect also statistically distinguishable from the Baseline message. Notably, in this sample the Trust in Science message had large effects on beliefs and actions toward others but appeared ineffective in changing an individual’s own intended vaccination behavior. The Not Bravery message was also the most effective message in this regard in Experiment 1.
We examined three pre-registered differences in subgroup treatment effects to test the patterns observed in Experiment 1. First, confirming Experiment 1 we found that those who did not endorse liberty values were more responsive to the Not Bravery message (compared to the baseline message) than those who endorsed liberty values for the three outcome measures. Second, we did not confirm either preregistered prediction with regard to differences in treatment effects by risk taking that were observed in Experiment 1.
The remaining subgroup comparisons were not pre-registered. Beginning with gender, in comparison to the untreated control, women responded more to the Trust in Science and Community Interest + Embarrassment message than did men (all five outcomes), while men responded more to the Not Bravery and Community Interest (without embarrassment) messages. Democrats were more responsive than Republicans across the board to the different treatment messages, while Republicans appeared to react only to the Community Interest and Community Interest + Embarrassment messages (magnitudes similar to those of Democrats). We observed a similar pattern for differences by baseline vaccine confidence, measured pre-treatment with a multi-item battery of questions [33]. Those high in vaccine confidence responded to all messages, while those low in confidence responded reliably only to the Community Interest messages.
3. Discussion
Overall, the results point both to a set of effective messages and the potential efficacy of specific messages for some particular subgroups. On average, a simple informational intervention is effective, but it is even more effective to add language framing vaccine uptake as protecting others and as a cooperative action. Not only does emphasizing that vaccination is a prosocial action increase uptake, but it also increases people’s willingness to pressure others to do so, both by direct persuasion and negative judgment of non-vaccinators. The latter social pressure effects may be enhanced by highlighting how embarrassing it would be to infect someone else after failing to vaccinate. The Not Bravery and Trust in Science messages had substantial effects on other regarding outcomes and for some subgroups, but do not appear to be as effective as the Community Interest messages in promoting own vaccination behavior. Importantly, in distinct samples fielded several months apart, the Community Interest, Community Interest + Embarrassment, and the Not Bravery messages produced substantively meaningful increases for all outcomes measures relative to the untreated control, and in some instances did so in comparison to the Baseline information condition.
Our findings are consistent with the idea that vaccination is often treated as a social contract in which people are expected to vaccinate and those who do not are sanctioned [10]. In addition to messages emphasizing the prosocial element of vaccination, we observed that messages that invoked reputational concerns were successful at altering judgment of those who would free ride on the contributions of others. This work could also help explain why social norm effects appear to overwhelm the incentive to free ride when vaccination rates are higher [[34], [35]]. That is, messages that increased intentions to vaccinate also increased the moralization of non-vaccinators suggesting that they are fundamentally linked to one another. These messages will need to be adapted in specific cultural contexts with relevant partners, such as community leaders.
The robust effect of the Community Interest message advances our current understanding of whether public health messaging that deploys prosocial concerns could be effective at increasing COVID-19 vaccine uptake. The results of both experiments presented here support prior work that demonstrated the effectiveness of communication that explains herd immunity on promoting vaccination [[15], [16]]. It also suggests that a detailed explanation of herd immunity may not be necessary to induce prosocial behavior.
Beyond the theoretical contribution, the results have practical implications for vaccine communication strategies for increasing COVID-19 vaccine acceptance. We identified multiple effective messages that provide several evidence-based options to immunization programs as they develop their vaccine communication strategies. Importantly, the insights into differential effectiveness of various messages by subgroup (e.g. men vs women) could inform messaging targeted to specific groups. Understanding heterogeneous treatment effects and the mechanisms that cause differential responses to persuasive messaging strategies requires additional testing and theoretical development. We view this as a promising avenue for future work.
The experiments presented here are not without limitations. First, we measured intentions to vaccinate at a time when a vaccine was not currently available and the effectiveness and side effects of potential vaccines were not known. This also meant that we could not observe actual vaccination behavior, which is ultimately the outcome of interest. While intentions predict behavior in many contexts [[36], [37]] including vaccination [[38], [39], [40]], past research examining the effect of behavioral nudges on COVID-19 vaccine uptake has produced divergent evidence when testing the effect of the same treatments in the field on behavior and in a survey experiment on a behavioral intention [41]. This observation highlights the need for field testing messages that have shown to be successful on increasing uptake intentions in survey experiments to ascertain whether they also increase vaccine uptake. It may be that field tests reveal certain messages are particularly less effective than in the survey context, or that messages are uniformly less effective. Second, given the rapidly evolving nature of the COVID-19 pandemic, attitudes about vaccines may have changed since the experiments were fielded which could also change the efficacy of the messages that we tested. Third, we cannot be sure whether, or how long, the effects we observe here persist. Finally, we only tested text-based messages, but public health messaging is delivered through many mediums, like public service announcements, videos, and images. Future work can adapt the successful messaging strategies found here and test their efficacy when delivered in alternative formats.
Efforts to vaccinate individuals against COVID-19 are currently underway in the United States and it remains important to convince the mass public of the safety and efficacy of COVID-19 vaccines to ensure that the threshold for herd immunity is reached. Our experiments provide robust evidence that appealing to protecting others has effects on intentions to get vaccinated and to apply social pressure to others to do so as well.
4. Materials and methods
4.1. Ethics statement
The experiments reported here were fielded under an exemption granted by the Yale University IRB. Informed consent was obtained from participants and they were informed that they could stop the study at any time. Data was collected anonymously and contained no personally identifiable information.
4.2. Experiment 1
Participants and Procedure. Participants were recruited by the vendor Luc.id to take a survey. Of those who were recruited, 4,361 participants completed the survey. An examination of attrition during the survey reveals that attrition was balanced across groups which minimizes concerns that the treatment effects estimated in the main manuscript are affected by attrition. The survey was programmed using the survey software Qualtrics. The survey was fielded between July 3, 2020 and July 8, 2020.
Experimental Design. Participants first completed basic demographic and pre-treatment attitudinal questions and were asked about their experience with COVID-19. After this, participants read a treatment message. They were required to spend at least 20 s on the survey page that contained the message to given them an adequate amount of time to read it. We allocated 2/15 of the sample to the untreated control condition and 1/5 of the sample to the Information baseline condition due to the number of comparisons that would utilize these conditions. Each of the remaining conditions received 1/15 of the sample. The design and analysis were pre-registered at ClinicalTrials.gov (protocol ID: 2000027983).
Outcome Measures. For COVID-19 vaccine uptake intentions, participants were asked “How likely are you to get a COVID-19 vaccine within the first 3 months that it is available to you?” and “How likely are you to get a COVID-19 vaccine in the first year that it is available to you?” Respondents answered this question on a five-point scale with end points of “Extremely unlikely” and “Extremely likely.” The main text describes how these items were combined for analysis. Turning to the likelihood of advising someone to vaccinate, respondents were asked “How likely are you to advise a close friend or relative to get vaccinated against COVID-19 once a vaccine becomes available?” Respondents also answered this question on a five-point scale with end points of “Extremely unlikely” and “Extremely likely.” Finally, for judging someone who chooses not to vaccinate, respondents read “we would like you to think about a friend or relative who chose not to receive a COVID-19 vaccine when it is available. What would you think about this person? Are they…”. This prompt was followed by four traits: trustworthy, selfish, likeable, and competent. The response options were “not at all”, “slightly”, “somewhat”, “mostly”, and “very.”
Analysis. We used OLS regression with robust Huber-White standard errors and indicators for assigned treatment to estimate treatment effects. We use robust standard errors to address the heteroscedasticity observed when estimating our primary analysis models without them. We included covariates as described in the Supplementary Materials. Comparisons across treatments are from linear combination of coefficients tests. For the subgroup analyses, we restricted the sample to the stated criteria and estimate the model specified here on the subsample. For liberty endorsement and risk taking, we determined who was high and low by splitting the sample at the mean.
4.3. Experiment 2
Participants and Procedure. Participants (n = 5,014) were recruited by the vendor YouGov/Polimetrix. YouGov provides subjects using a sampling procedure that is designed to match a number of Census demographics. To determine the sample size, we conducted a power analysis to detect effects that were 80 % as large as those observed in Experiment 1. The experiment was fielded between September 9, 2020 and September 22, 2020.
Experimental Design. Participants first completed basic demographic and pre-treatment attitudinal questions and were asked about their experience with COVID-19. Participants were randomly assigned to one of seven conditions: the untreated control, the Information baseline control, Community Interest, Community Interest + Anticipated Embarrassment, Not Bravery, Trust in Science, or Personal Freedom. As in Experiment 1, more participants were assigned to the untreated control condition and the Baseline information control condition, 1/5 and 3/10 of the sample respectively. The remaining five conditions each received 1/10 of the sample. Participants were required to spend at least 30 s on the survey page that had the treatment message. The design and analysis were pre-registered at Open Science Framework.
Outcome Measures. The outcome measurement was the same as described in Experiment 1 with the exception of intelligent being added to the judgment of a non-vaccinator scale.
Analysis. We used the same modeling approach described above to produce the results displayed in Fig. 2. We included covariates as described in the Supplementary Materials. For subgroup analyses, we estimated OLS regression models with an indicator variable if a person was a member of a subgroup (e.g. high endorsement of liberty) and zero otherwise.
CRediT authorship contribution statement
Erin K. James: Conceptualization, Writing- original draft, Writing- review and editing. Scott E. Bokemper: Conceptualization, Data curation, Formal analyses. Alan S. Gerber: Conceptualization, Writing- review and editing. Saad B. Omer: Conceptualization, Writing- review and editing. Gregory A. Huber: Conceptualization, Data curation, Formal analyses, Writing- original draft, Writing- review and editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
The authors would like to acknowledge support for the Tobin Center for Economic Policy at Yale University. EKJ and SBO were supported by the Yale Institute for Global Health.
SEB, ASG, and GAH received support from the Institution for Social and Policy Studies and the Center for the Study of American Politics at Yale University.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.10.039.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Funk C., Tyson A. (Pew Research Center Science & Society); 2020. Intent to get a COVID-19 vaccine rises to 60% as confidence in research and development process increases. [Google Scholar]
- 2.Bauch C.T., Galvani A.P., Earn D.J.D. Group interest versus self-interest in smallpox vaccination. Proc Natl Acad Sci. 2003;100(18):10564–10567. doi: 10.1073/pnas.1731324100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauch C.T., Earn D.J.D. Vaccination and the theory of games. Proc Natl Acad Sci. 2004;101(36):13391–13394. doi: 10.1073/pnas.0403823101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Böhm R., Betsch C., Korn L. Self-rational non-vaccination: Experimental evidence from an interactive vaccination game. J Econ Behav Organ. 2016;131:183–195. [Google Scholar]
- 5.Böhm R., Betsch C., Korn L., Holtmann C. Exploring and promoting prosocial vaccination: a cross-cultural experiment on vaccination of health care personnel. Biomed Res Int:6870984. 2016;2016:1–9. doi: 10.1155/2016/6870984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chapman G.B., et al. Using game theory to examine incentives in influenza vaccine behavior. Psychol Sci. 2012;23(9):1008–1015. doi: 10.1177/0956797612437606. [DOI] [PubMed] [Google Scholar]
- 7.Galvani A.P., Reluga T.C., Chapman G.B. Long-standing influenza vaccination policy is in accord with individual self-interest but not with the utilitarian optimum. Proc Natl Acad Sci. 2007;104(13):5692–5697. doi: 10.1073/pnas.0606774104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wells C.R., Huppert A., Fitzpatrick M.C., Pandey A., Velan B., Singer B.H., et al. Prosocial polio vaccination in Israel. Proc Natl Acad Sci. 2020;117(23):13138–13144. doi: 10.1073/pnas.1922746117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shim E., Chapman G.B., Townsend J.P., Galvani A.P. The influence of altruism on influenza vaccination decisions. J R Soc Interface. 2012;9(74):2234–2243. doi: 10.1098/rsif.2012.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korn L., Böhm R., Meier N.W., Betsch C. Vaccination as a social contract. Proc Natl Acad Sci. 2020;117(26):14890–14899. doi: 10.1073/pnas.1919666117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Betsch C., Böhm R., Korn L., Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav. 2017;1(3):0056. [Google Scholar]
- 12.Betsch C., Böhm R. Moral values do not affect prosocial vaccination. Nat Hum Behav. 2018;2(12):881–882. doi: 10.1038/s41562-018-0478-1. [DOI] [PubMed] [Google Scholar]
- 13.Sprengholz P., Betsch C. Herd immunity communication counters detrimental effects of selective vaccination mandates: Experimental evidence. EClinicalMedicine. 2020;22:100352. doi: 10.1016/j.eclinm.2020.100352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Betsch C., Böhm R., Korn L. Inviting free-riders or appealing to prosocial behavior? Game-theoretical reflections on communicating herd immunity in vaccine advocacy. Health Psychol. 2013;32(9):978–985. doi: 10.1037/a0031590. [DOI] [PubMed] [Google Scholar]
- 15.Pfattheicher S, Petersen MB, & Böhm R. Information about herd immunity through vaccination and empathy promote COVID-19 vaccination intentions. PsyArXiv [preprint]. 2020. [DOI] [PubMed]
- 16.Trueblood JS, Sussman AB, O’Leary D. The role of risk preferences in responses to messaging about COVID-19 vaccine uptake. Social Psychology and Personality Science. 2021 doi: 10.1177/1948550621999622. [DOI] [Google Scholar]
- 17.Duquette N. Heard” immunity: Messages emphasizing the safety of others increase intended uptake of a COVID-19 vaccine in some groups. Covid Economics. 2020:39. [Google Scholar]
- 18.Jung H., Albarracin D. Proceedings of the National Academy of Sciences 118:e2007538118. 2020. Concerns for others increase the likelihood of vaccination against influenza and COVID-19 more in sparsely rather than densely populated areas. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delton A.W., Cosmides L., Guemo M., Roberston T.E., Tooby J. The psychosemantics of free riding: Dissecting the architceture of a moral concept. J Pers Soc Psychol. 2012;102(6):1252–1270. doi: 10.1037/a0027026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nowak M.A., Sigmund K. Evolution of indirect reciprocity. Nature. 2005;437(7063):1291–1298. doi: 10.1038/nature04131. [DOI] [PubMed] [Google Scholar]
- 21.Boyd R., Richerson P.J. The evolution of reciprocity in sizable groups. J Theor Biol. 1988;132(3):337–356. doi: 10.1016/s0022-5193(88)80219-4. [DOI] [PubMed] [Google Scholar]
- 22.Barclay P., Willer R. Partner choice creates competitive altruism in humans. Proceedings of the Royal Society B: Biological Sciences. 2007;274(1610):749–753. doi: 10.1098/rspb.2006.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiyonari T., Barclay P. Cooperation in social dilemmas: Free riding may be thwarted by second-order reward rather than by punishment. J Pers Soc Psychol. 2008;95(4):826–842. doi: 10.1037/a0011381. [DOI] [PubMed] [Google Scholar]
- 24.Davis C.J., Golding M., McKay R. Efficacy information influences intention to take COVID-19 vaccine. British Journal of Health Psychology. 2021 doi: 10.1111/bjhp.12546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frank RH. Passions within reason: The strategic role of the emotions (W W Norton & Co, New York, NY, US) 1988; pp xiii, 304-xiii, 304.
- 26.Fessler D & Haley KJ. The strategy of affect: Emotions in human cooperation 12. The Genetic and Cultural Evolution of Cooperation, P. Hammerstein, ed: 2003; 7-36.
- 27.Sell A, Tooby J, & Cosmides L (2009) Formidability and the logic of human anger. Proceedings of the National Academy of Sciences 106(35):15073. [DOI] [PMC free article] [PubMed]
- 28.Chapman G.B., Coups E.J. Emotions and preventive health behavior: Worry, regret, and influenza vaccination. Health Psychol. 2006;25(1):82–90. doi: 10.1037/0278-6133.25.1.82. [DOI] [PubMed] [Google Scholar]
- 29.Brewer N.T., DeFrank J.T., Gilkey M.B. Anticipated regret and health behavior: A meta-analysis. Health Psychol. 2016;35(11):1264–1275. doi: 10.1037/hea0000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amin A.B., Bednarczyk R.A., Ray C.E., Melchiori K.J., Graham J., Huntsinger J.R., et al. Association of moral values with vaccine hesitancy. Nat Hum Behav. 2017;1(12):873–880. doi: 10.1038/s41562-017-0256-5. [DOI] [PubMed] [Google Scholar]
- 31.Kalimeri K, et al. Human values and attitudes towards vaccination in social media. in Companion Proceedings of The 2019 World Wide Web Conference (Association for Computing Machinery, San Francisco, USA), 2019. pp 248–254.
- 32.Bokemper S.E., Huber G.A., Gerber A.S., James E.K., Omer S.B. Timing of COVID-19 vaccine approval and endorsement by public figures. Vaccine. 2021;39(5):825–829. doi: 10.1016/j.vaccine.2020.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Larson HJ, Schulz WS, Tucker JD, & Smith DM. Measuring vaccine confidence: introducing a global vaccine confidence index. PLoS currents 2015; 7. [DOI] [PMC free article] [PubMed]
- 34.McKillop C.N., Leonard T., Pruitt S.L., Tiro J.A. Do traditional economic theories of free riding behavior explain spatial clustering of HPV vaccine uptake? SSM - Population Health. 2019;8:100421. doi: 10.1016/j.ssmph.2019.100421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verelst F, Kessels R, Willem L, & Beutels P. No such thing as a free-rider? Understanding multicountry drivers of childhood and adult vaccination. medRxiv:2020.2012.2007.20245118. 2020. [DOI] [PMC free article] [PubMed]
- 36.Chandon P., Morwitz V.G., Reinartz W.J. Do intentions really predict behavior? Self-generated validity effects in survey research. Journal of Marketing. 2005;69(2):1–14. [Google Scholar]
- 37.Eccles M.P., Hrisos S., Francis J., Kaner E.F., Dickinson H.O., Beyer F., et al. Do self-reported intentions predict clinicians' behaviour: a systematic review. Implementation Science. 2006;1(1) doi: 10.1186/1748-5908-1-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.daCosta DiBonaventura M., Chapman G.B. Moderators of the intention–behavior relationship in influenza vaccinations: Intention stability and unforeseen barriers. Psychology and Health. 2005;20(6):761–774. [Google Scholar]
- 39.Fall E., Izaute M., Chakroun-Baggioni N. How can the health belief model and self-determination theory predict both influenza vaccination and vaccination intention? A longitudinal study among university students. Psychology & health. 2018;33(6):746–764. doi: 10.1080/08870446.2017.1401623. [DOI] [PubMed] [Google Scholar]
- 40.Lehmann B.A., Ruiter R.A.C., Chapman G., Kok G. The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine. 2014;32(51):6986–6991. doi: 10.1016/j.vaccine.2014.10.034. [DOI] [PubMed] [Google Scholar]
- 41.Dai H., et al. Behavioral nudges increase COVID-19 vaccinations. Nature. 2021;597:404–409. doi: 10.1038/s41586-021-03843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.