Abstract
Background
The Fracture Risk Assessment Tool (FRAX) is the most widely used tool for fracture prediction. It provides 10-year probabilities for hip and major osteoporotic fracture (MOF). It uses country-specific hip fracture incidence and life expectancy data, and for most countries, MOF/hip fracture incidence rate ratios (IRRs) from Malmo Sweden. However, the risk of MOF varies by age, sex, and geography. The objective is to compare the MOF/hip IRRs across countries, by sex and age.
Methods
This systematic review targeted observational studies of MOF and hip fractures in individuals >50 years (CRD42019129259). One reviewer screened potential articles. Two reviewers completed duplicate and independent data abstraction, and assessed studies quality based on population representativeness, study design and duration, definition of ethnicity and fracture characteristics. We calculated the MOF/hip IRRs [95% confidence interval] and Z-values to compare IRRs in various countries to those for Sweden.
Results
We included 27 studies, of fair to good quality in the majority, from Europe (15), US and Canada (7), Asia (3) and Australia (2). The IRRs were 2-10-fold higher in younger compared to older age categories, and in women compared to men, with few exceptions. Within Europe, and using Sweden as a reference, MOF/Hip IRRs in women 50-54 years from Finland, Italy, Netherlands, Denmark and UK were significantly lower by 38-60%. Findings were similar in men. At older ages, MOF/Hip IRRs were consistently lower in women from European countries compared to Sweden, by 10-40% and 11-51%, at 75-79 years and 85-89 years, respectively, Findings were heterogenous in men and in non-European countries.
Conclusion
The MOF/hip fracture IRR may vary between countries. The variability at older ages may affect FRAX prediction when country-specific fracture IRR are not used. Further research is needed to elucidate the implication of our findings to FRAX-derived MOF estimates in various countries.
Background
Several fracture risk assessment tools have been developed to identify high-risk individuals (1). Such tools incorporate osteoporosis related risk factors (2). The Fracture Risk Assessment Tool (FRAX) is the most widely used one. It was developed to predict the 10-year fracture risk probability, for major osteoporotic fractures (MOF) and for hip fracture, separately (3). Currently, 72 country-specific FRAX on-line calculators are available (4). These calculators incorporate country-specific fracture (MOF and/or hip) and mortality data, to derive patient specific 10-year estimates for the probability of hip and MOF fractures. However, MOF fracture data are only available for few countries, namely Mexico, UK, Switzerland, Canada, US, Japan and Sweden (5). In almost all other countries where MOF rates are not available, FRAX uses country specific hip fracture data and assumes the MOF/Hip fracture ratio is the same worldwide as in Malmo, Sweden (5). This enables a calculation of the 10-year FRAX probability estimates for MOF for individuals from these countries (5). However, the above assumption may not always apply (2, 6). Indeed, osteoporotic fracture risk varies worldwide, by geographic location, sex, ethnicity and socio-economic status (7, 8). Hip fracture rates are the highest in northern countries, such as Denmark and Sweden, and the lowest in countries in South Africa and Asia, such as Nigeria, South Africa, China, and Korea, with a difference in incidence rate exceeding 10-fold (9, 10). The variability in the incidence of morphometric vertebral fractures is even wider (7, 8). The highest rates are reported in Sweden and Switzerland, and the lowest in Hungary (7). The epidemiology of forearm fractures is no exception; the highest incidence is registered in Hungary and the lowest in Japan (7). Furthermore, within individual countries, such as the US, New Zealand and Singapore, discrepancies in hip fracture incidence were reported across various ethnicities (7). Fracture risk increases within a country with lower socio-economic status (11, 12) and decreases with higher education level, although not consistently (13).
Country-specific and ethnicity-specific secular trends in fracture risk have been also described (7, 14, 15). While a secular decline in hip fracture risk was reported in Europe, US and Canada over the second half of the 20th century, an increase in these rates was detected in Asian countries such as Japan, China, Taiwan (7, 14). All the above variations challenge the validity of FRAX assumption of using data that is almost 2 decades old, and from an exclusive caucasian northern european population to the world at large (5).
The objective of this review is to evaluate and compare the incidence rate ratios (IRR) of MOF to hip fracture, by sex and age categories, across various countries.
Methods
The protocol of this systematic review is registered on PROSPERO (CRD42019129259)(16). We conducted a systematic search on Medline, PubMed, and Embase databases, without time or language restriction until December 2016 and an update until May1st, 2018. We used the following MeSh terms and keywords: Hip Fractures; Non-Hip Fractures; Major Osteoporotic Fractures; Epidemiology; Osteoporosis. Full details of the search strategy are available in Appendix 1. We performed a manual search and review of the references listed in the included studies and review papers on the topic.
Study selection and data abstraction
We included studies conducted on post-menopausal women and men ≥ 50 years, that spanned over one year or more, and reported on the incidence and/or incident number of MOF and hip, individually or combined, by sex and age category. One reviewer screened the titles and abstracts of the retrieved citations (NC), and another one screened the potential full text papers (MC), using a standardized form. Teams of 2 reviewers (MC, HD and SS) abstracted data on pertinent variables related to the population and outcomes, in duplicate and independently, using data collection sheets prepared a priori. In case of missing data on a specific fracture site, we contacted the corresponding authors to obtain it.
Strategy for data synthesis
We calculated the IRR of incident fractures by dividing the number of incident MOF by the number of incident hip fracture, for the study period, by sex and age category, in each country. If the incident number of factures was reported on each of the MOF fractures individually, we calculated the incident number of MOF as the sum of incident hip, vertebral, humerus, and distal forearm fractures. We calculated the 95 % confidence interval (CI) of the IRR using the formula described by Rothman et al (17). We determined the statistical significance of the difference between the IRR CI between 2 given categories by calculating the Z- value (Z = (ln(IR1) - ln(IR2)) / sqrt(SD1*SD1 + SD2*SD2). Z ≤ −1.96 or Z ≥1.96 were considered statistically significant. For studies where data on incident number of fractures were not available, we used the incidence of fractures to calculate the IRR, but we were not able to calculate the 95% CI. When the fracture incidence was expressed in person/years, two reviewers derived the incidence rate using the following formula: Risk = [1- exp (-Rate x time)], using ebase (2.718), where the risk is defined as number affected/number at risk, and rate is defined as a person/year measure (18). When the MOF and Hip incidence rates were reported in a graph form without corresponding table values, we first contacted authors to get numerical study data. In case of no reply or when such data was not available, two reviewers used “Plotdigitizer”, a computer software that converts graph to numerical values (18). Plotdigitizer was used for three studies (19–21), but none of them provided the number of incident fractures. In case incidence data of more than one year were available for a given study, we calculated the average across years (22).
We were unable to compare the derived IRRs to those from Malmo Sweden, due to the unavailability of number of fractures by age and gender specific categories. We therefore compared the age and gender specific calculated MOF/Hip IRRs to those from another more recent study from Skane, Sweden (23) as a reference instead. As a sensitivity analysis, we also repeated the same analyses, by comparing the derived IRRs for various countries to those of Manitoba, Canada (6) as a reference. This is because the MOF to Hip IRR in Canada were among the highest across countries. The latter analyses were not prespecified in the protocol.
We have selected the countries with higher quality ratings (quality score ≥ 4) in case more than one study were derived from one country, for representation in the Figures. We included Sweden in all Figures as this was our pre-planned analysis.
Risk of bias (quality) assessment
Teams of 2 reviewers (MC, HD, SS) assessed the quality of the studies, in duplicate and independently, using a modified quality score, that was previously used for the rating of the quality of hip fracture incidence studies (9, 24). The scoring was reviewed by a content expert (GEHF). This tool evaluates the following domains: population representativeness (multicenter or population based), study design (prospective or retrospective), ethnicity definition, study duration (= 1 year versus >1 year), method used to define fracture (ICD or other), whether all fractures were collected during a period of 3 years, and the definition of the included fractures as osteoporotic, or definition of the level of trauma. The last two items were added to the quality score for the purpose of this review. For each domain, judgment was done qualitatively, and a score of 0 or 1 was given depending on whether the needed information was available or not. Exceptionally, for ethnicity, a score of 2 was given if ethnicity was explicitly defined, a score of 1 if ethnicity was not defined in the paper, but only one ethnicity is dominant in that country (25–27), and a score of 0 was given if none of the aforementioned criteria were available. A summary score was derived by summing up the individual items to allow comparability, with a maximum score of 8. A study was rated of good quality if it has a score of at ≥ 6, fair if it has a score of 4-5 and poor if it scores ≤ 3. We did not use the Newcastle-Ottawa-Scale for assessing the quality of non-randomized studies, because it did not contain the key domains relevant to epidemiologic studies on fractures (28).
Results
After duplicate removal, the search methodology yielded 6,990 citations. After title and abstract screening, we excluded 6,385 citations and screened 305 full text papers. We excluded 277 papers for the reasons described in Appendix 2 (Appendix 2- List of excluded studies), thus retaining 28 eligible papers (6, 11, 19–23, 29–49), corresponding to 27 studies, as one study from UK had 2 publications(11, 49) (Figure 1- Flow Diagram).
Figure 1.

Flow diagram of the different phases of the systematic review
Abbreviations: GLOW, Global Longitudinal Study of Osteoporosis in Women; MOF, major osteoporotic fracture; SOF, Study of Osteoporotic Fractures.
A-. Studies providing data on the number of incident fractures
Eighteen studies provided data on fracture incident numbers allowing the calculation of IRR and its 95% CI, and these were as follows: one from Asia (Japan (29)), 10 from Europe (Denmark (31), Finland (30), Iceland (33), Italy (22), Netherlands (43), Spain (47, 48), Sweden (23), UK (11, 49)), 6 from the US and Canada (6, 37–40, 45), 2 from Australia (34, 36). Fourteen studies described fracture incidence in both men and women (6, 11, 22, 23, 29–31, 33, 34, 36–38, 40, 43), 2 studies in men only (39, 45) and 2 others in women only (47, 48). Twelve studies provided fracture data starting at 50 years and by 5-year categories, and thus allowed comparability of their results (6, 11, 22, 23, 29–31, 33, 34, 36, 38, 43). Six other studies presented their data differently, starting at the age of 65 years (45), or using wider age categories of 10-15 years (37, 39, 40, 45, 47, 48). Twelve studies were retrospective while six were prospective. All studies except four (29, 36, 45, 47) used ICD codes to identify fractures. All fractures were collected within the same period that started after year 2000, with the exception of 6 studies that started before (11, 23, 33, 34, 38, 40). Eleven studies were population based and representative of their respective country (11, 29–32, 34, 36, 39, 40, 43, 45), while seven others were representative of a specific region in the country (Reykjavik in Iceland (33), Catalonia in Spain (47, 48), Skane in Sweden (23), Minnesota in US (38), Manitoba in Canada (6), Ontario in Canada (37)) or not representative(22). Only four studies defined the population ethnicity (11, 45, 47, 48).
The quality of the included studies was variable: poor in one study (37), fair in 13 studies (6, 22, 23, 29, 31, 33, 36, 38, 39, 43, 45, 47, 48), and good in 4 studies (11, 30, 34, 40); The studies used to derive IRR 95% CI, providing their data by age categories of 5 years and allowing comparability had all a quality score ≥ 4 (Table 1, Appendix 3).
Table 1.
Summary of included observational studies reporting on the incidence or incident number of major osteoporotic and hip fractures (publication period 2011-2018)
| Country | Author year | Study period | Population source | Study limitations | Quality score | CI calculated |
|---|---|---|---|---|---|---|
| Asia | ||||||
| Korea | Park 2011(19) | 2005-2008 | Nationwide claims database of the Health Insurance Review and Assessment Service of Korea that covers 97% of the population | Retrospective Osteoporosis definition based on ICD- 10 codes and a cut-off value of 50 years of age |
5 | No |
| Japan | Sakuma 2008(21) | 2004 | Patients admitted to one general hospital and questionnaires were distributed to four hospitals and five doctors’ offices including the main orthopedics facility | Retrospective Study representative of Sado city but not of Japan Study duration 1 year Fracture identification not based on ICD Pathologic fracture excluded but trauma level for fracture inclusion not defined |
2 | No |
| Japan | Tsukutani 2015(29) | 2010-2012 | Medical institutions of Sakaiminato and Yonago | Fracture identification not based on
ICD Pathologic fracture excluded but trauma level for fracture inclusion not defined |
5 | Yes |
| Australia | ||||||
| Australia | Sanders 1999(34) | 1994-1996 | Geelong Osteoporosis Study, a population-based study designed to determine complete fracture rate within a defined region sufficiently large and representative of national demographics to establish reliable rates of fracture. All radiologic facilities are provided through two centralized services and the catchment population has an age distribution similar to that of the 1996 national population (Australian Bureau of Statistics) | Pathologic fractures excluded but trauma level for fracture inclusion not defined | 6 | Yes |
| Australia | Pasco 2015(36) | 2006-2007 | Barwon Statistical Division linked to major radiology centers servicing the region | Retrospective Fracture identification not based on ICD Pathologic fractures excluded but trauma level for fracture inclusion not defined |
4 | Yes |
| Europe | ||||||
| Denmark | Driessen 2016(31) | 2011 | Danish National Hospital Discharge Register (NHDR) that covers all inpatient contacts from 1977 to 1994, and from 1995 furthermore includes all outpatient visits to hospitals, outpatient clinics and emergency rooms | Retrospective Study duration 1 year High and low trauma fractures included |
4 | Yes |
| Finland | Koski 2014(30) | 2005-2006 | Five health centers serving the inhabitants of nine municipalities and from the patient records of two hospitals in Central Finland | Retrospective | 6 | Yes |
| Hungary | Pentek 2008(35) | 1999–2003 | Hungarian National Health Insurance Fund Administration that covers 100% of the population | Retrospective No definition of osteoporosis |
5 | No |
| Iceland | Siggeirsdottir 2014(33) | 1967-2008 | The prospective and ongoing population-based Reykjavik Study; part selected at random from the Icelandic National Register; the study had a 71% response rate | Population representative of the Reykjavik
area but not of Iceland No definition of osteoporosis |
5 | Yes |
| Italy | Piscitelli 2011(22) | 2004-2006 | Italian National Hospitalization Database contains information concerning all hospitalizations occurring in all Italian public hospitals | Population limited to public hospitals, not
including private hospitals No definition of osteoporosis |
4 | Yes |
| Netherlands | Klop 2015(43) | 2002-2011 | Dutch PHARMO Database Network that links drug dispensing records to hospital discharge records, general practitioner and death registration data using probabilistic linkage | Retrospective Ethnicity not defined and variable ethnicity in Netherlands No definition of osteoporosis |
4 | Yes |
| Spain | Pages-Castella 2012(20) | 2009 | SIDIAP Database (electronic medical records of a representative sample of patients attended by general practitioners (GPs) in Catalonia covering a population of more than 5.8 million patients (about 80% of the total population of Catalonia) from 274 primary care practices with 3,414 participating GPs | Retrospective Population representative of Catalonia, but not of Spain No definition of osteoporosis |
3 | No |
| Spain | Azagra 2016(47) | 2000-2010 | Catalan Health institute, primary care centers, main public provider of health services in Catalonia-Spain and covers around 83% of the 7.5 million population and has computerized medical records of their patients since 2001 | Population divided into only 2 age
categories Population representative of Catalonia, but not of Spain No definition of osteoporosis |
5 | Yes |
| Spain | Azagra 2016(48) | 2002-2012 | FRIDEX cohort a random sample of Caucasian women >40 and <90 years who understood and spoke the Spanish language | Population divided into only 2 age
categories Urban areas only included Fracture identification not based on ICD |
5 | Yes |
| Sweden | Kanis 20012 (44, 50) | 1987-19942 | National Bureau of Statistics, Stockholm; When insufficient information, rates were imputed from the distribution of fractures observed in Olmsted County, Rochester | Retrospective Study representative of Malmo but not of Sweden Data collection of each fracture over one year, and spanning over a period of > 3 years for all fractures Osteoporotic fractures were defined as those associated with low bone mineral density Fracture identification not based on ICD |
2 | No |
| Sweden | Rosengren 2014(23) | 1999-2010 | Skåne Health Care Register based on personal identification numbers and covers all inpatient and outpatient. | Study duration 1 year Study representative of Sakne, not of Sweden No definition of osteoporosis |
4 | Yes |
| Swiss | Lippuner 2008(41) | 2000 | Administrative and medical statistics database of the Swiss Federal Office of Statistics (SFOS) Swiss OsteoCare cohort: Three participating hospitals were university hospitals (Basel, Berne, and Lausanne), three cantonal hospitals (Fribourg, Lucerne, and St Gallen) and two regional hospitals (Estavayer and Riaz) | Fractures are defined by site rather than level of trauma | 8 | No |
| Swiss | Lippuner 2012(42) | 2000-2008 | Administrative and medical statistics database of the Swiss Federal Statistical Office (SFSO) supplied by all Swiss acute care hospitals, rehabilitation centers, and specialized clinics are obliged | Retrospective No definition of osteoporosis |
5 | No |
| UK | Singer 1997(32) | 1992-1993 | Accident and Emergency service in Edinburgh and the surrounding district, managed at the Royal Infirmary | Study representative of Edinburgh but not of
UK Fracture identification not based on ICD No definition of osteoporosis |
4 | No |
| UK | Curtis /Van Staa 2001(11, 49) | 1988-1998 | General Practice Research Database (GPRD), which contains the computerized medical records of 683 general practices in the UK | Retrospective No definition of osteoporosis |
6 | Yes |
| US and Canada | ||||||
| Canada | Lam 2014(6) | 2000-2007 | Manitoba Population Health Research Data Repository, which contains health-care information on nearly all residents of Manitoba, Canada | Retrospective Study representative of Manitoba but not Canada Ethnicity not defined and variable ethnicity in Canada |
5 | Yes |
| Canada | Lix 2012(40) | 1996-2006 | Canadian Multicentre Osteoporosis Study Population based | Population divided into 4 age
categories Ethnicity not defined and variable ethnicity in Canada |
6 | Yes |
| Canada | Papaioannou 2016(37) | 2002 -2012 | Canadian Institute for Health Information that is linked to all acute care facilities in Ontario | Population divided into 3 age categories,
starting age 65 years Retrospective Study representative of Ontario, not Canada Ethnicity not defined and variable ethnicity in Canada No definition of osteoporosis |
3 | Yes |
| USA | Melton 1999(38) | 1989–91 | Rochester Epidemiology Project Population based | Retrospective Study representative of Minnesota but not of the whole US Ethnicity not defined and variable ethnicity in US No definition of osteoporosis |
4 | Yes |
| USA | Ettinger 2010(46) | 2006 | For hip fracture: Nationwide Inpatient Sample (NIS) database, a large U.S. hospital discharge database; For non-hip fractures: these were as provided by Metlon 1999 (Rochester Epidemiology project, population based) | Retrospective Data collection of each fracture over one year, and spanning over a period of > 3 years for all fractures |
5 | No |
| USA | Ettinger 2013(45) | 2000-2002 | Multicenter MrOs study | Data provided starting age 65
years Fracture identification not based on ICD Fractures were included regardless of the degree of trauma |
5 | Yes |
| USA | Manthripragada 2015(39) | The database is geographically diverse, with representation from all US census regions. Enrolled individuals enrolled include employees, dependents, and retirees in the USA with primary or Medicare supplemental coverage through privately insured health plans | Population divided into 3 age
categories Retrospective Ethnicity not defined and variable ethnicity in US No definition of osteoporosis |
4 | Yes | |
Abbreviations: CI: confidence interval
Confidence interval calculated when the study provided the number of incident fractures
Kanis 2001 has same data as Kanis 2000; Fractures data in different years: Hip 1991; Forearm 1994; Proximal Humerus 1987; Clinical vertebral fractures 1993-1994
Comparison of MOF/hip IRRs across age categories and by gender within countries
We calculated IRR and 95% CI starting at the age of 50 years until age 90 or 90+ years, according to the data available in studies, by 5 years intervals, except for few studies that used different age categories and/or different age limits (37, 39, 40, 45, 47, 48).
The MOF/hip IRRs were higher at younger age categories compared to older ones, driven by low hip fracture incidence at young ages (Figure 2a and b). In particular, in both men and women, the IRRs at 50-54 years, were significantly higher than the IRRs at 80-84 years across all countries, except few, for men, −1.96 <Z < 1.96 (29, 34, 38, 40) and women, Z 0.985 (29) (Appendices 4 and 5). Similarly, when data on older age categories were available (90+years), the IRRs at 50-54 years was higher than IRRs at the extreme age category, except in men in a study from Australia where the difference did not reach statistical significance, Z 1.305 (Appendix 5). In studies where the difference was significant, in women, the IRRs at the age of 50-54 were 3-8-fold higher than the IRRs at 80-85 years. Similarly, in men, the IRRs at the age of 50-54 were 2-10-fold higher than the IRRs at 80-85 years (see Figure 2a for women and 2b for men).
Figures 2.
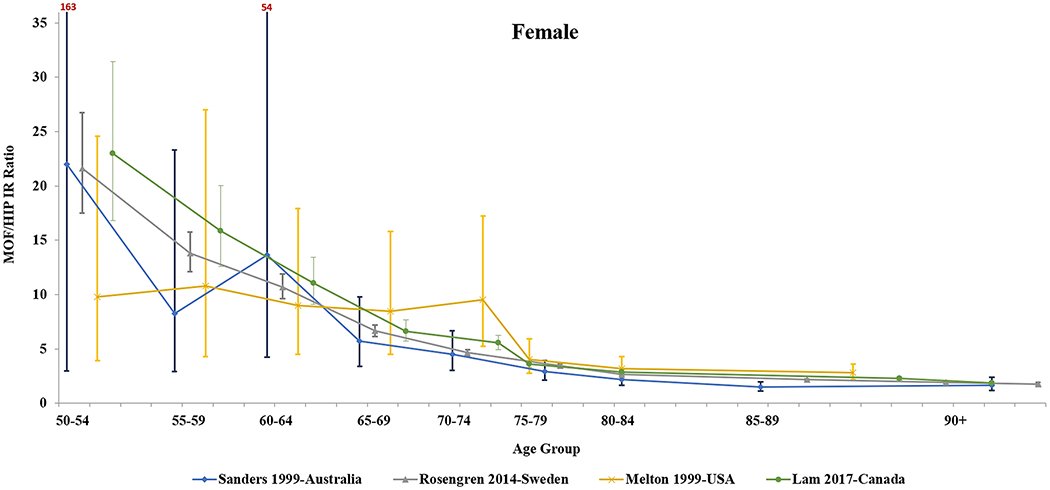

Comparison of MOF/hip incidence rate ratio and 95% confidence interval across various age categories from different countries: Australia, Sweden, USA and Canada, in women (a) and men (b).
The data points for specific age groups by country are not aligned on the vertical axis, but spread and spaced, for better visualization. From left to right, the first set of points correspond to the age group 50-54 years, the second set of points correspond to the age group 55-59 years, and the same applies for the other data points.
Abbreviations: IRR, incidence rate ratio; MOF, major osteoporotic fracture.
At 50-54 years, the IRRs in women were 1.1-2 fold higher than in men in some studies (6, 11, 22, 23, 31), the largest difference was in Canada (6), while the difference did not reach statistical significance in several other studies(30, 33, 34, 36, 38, 40, 43) (Appendix 5). Similarly, at 80-84 years, the IRRs in women were significantly higher by 1.3-1.6 fold in women compared to men in some studies (11, 22, 23, 31, 36, 43), the largest difference in Australia (36), while there was no significant differences in other studies(6, 29, 30, 33, 34, 38) (see Figure 3 for comparison of Sweden and UK as an example).
Figure 3.
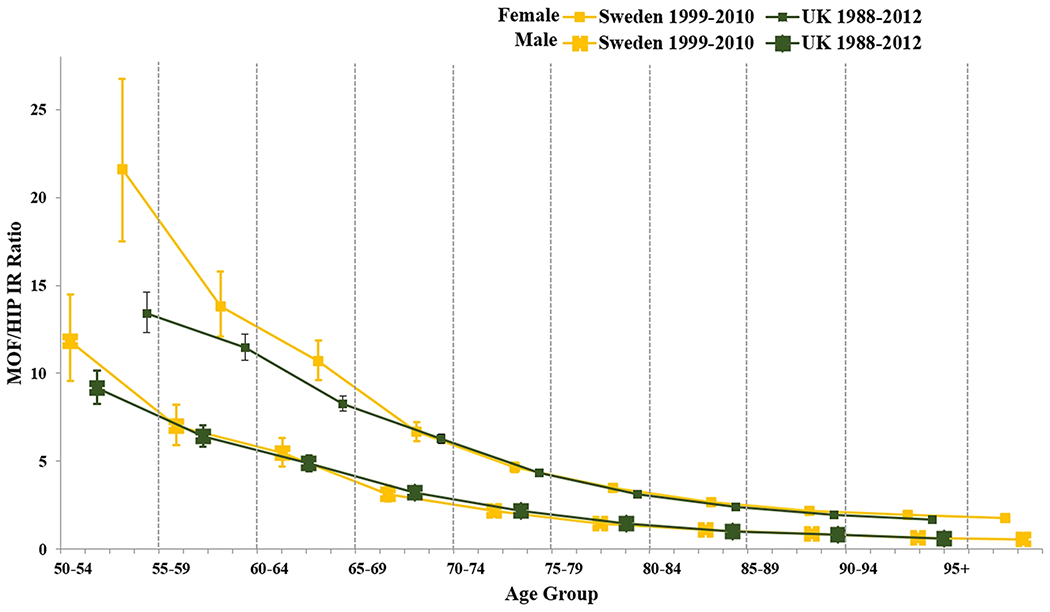
Comparison of MOF/hip incidence rate ratio and 95% confidence interval across various age categories and between gender, in Sweden and UK.
The data points for specific age groups by country are not aligned on the vertical axis, but spread and spaced, for better visualization. From left to right, the first set of points correspond to the age group 50-54 years, the second set of points correspond to the age group 55-59 years, and the same applies for the other data points.
Abbreviations: IRR, incidence rate ratio; MOF, major osteoporotic fracture.
Comparison of MOF/hip IRR across age categories and by gender to one country
Comparison to Sweden:
Within the European countries, the MOF/Hip IRRs in women 50-54 years from Finland, Italy, Netherlands, Denmark and UK were significantly lower, by 38-60%, than IRRs in Sweden, while in Iceland they were comparable (Figures 3, 4a and 5). The IRR in men 50-54 years from Italy and Iceland was similar to that in Sweden, and significantly lower by 20-63% in Finland, Netherland, Denmark and UK (Figures 3, 4b and 5). At older age categories, the differences in IRR for European countries, in comparison to Sweden, became homogenous in women. They were significantly lower in women from Finland, Italy, Netherlands, Iceland and UK, by 10-40% at 75-79 years, and by 11-51%at 85-89 years, compared to Sweden. It remains heterogenous in men (Figure 5, Appendix 5).
Figure 4.
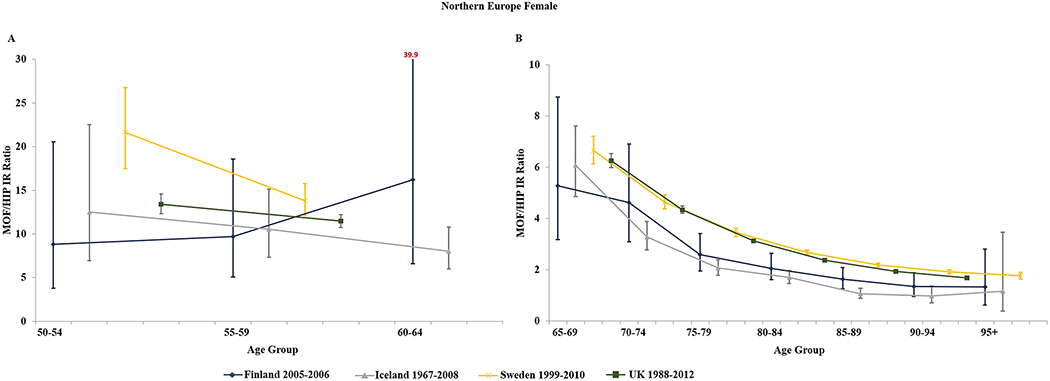

Comparison of MOF/hip incidence rate ratio and 95% confidence interval across various age categories in European countries, in women (a) and men (b).
The data points for specific age groups by country are not aligned on the vertical axis, but spread and spaced, for better visualization. From left to right, the first set of points correspond to the age group 50-54 years, the second set of points correspond to the age group 55-59 years, and the same applies for the other data points. For some confidence intervals, the upper limit is not horizontal as it exceeds the Y-axis limit shown in the figure.
Abbreviations: IRR, incidence rate ratio; MOF, major osteoporotic fracture
Figure 5:

Statistical comparison of incidence rate ratios (IRR) using the Z-test1, by gender and by age categories (years), for each individual country compared to Sweden (A), or Canada (B), as a reference
A- Statistical comparison of IRR using the Z-test, by gender and by age categories, for each individual country compared to Sweden (Rosengren et al).
B- Statistical comparison of IRR using the Z-test, by gender and by age categories, for each individual country compared to Canada (Lam et al).
1 The Z test used the following formula: Z = (ln (IRR1) – ln (IRR2)) / sqrt (SD1 X SD1 + SD2 X SD2).If Z < −1.96 or Z > 1.96, then we reject the null hypothesis of equality, and the IRRs are significantly different for each individual country compared to Sweden (A) or Canada (B), by age groups, and are represented by grey colored boxes. A light grey box indicates an IRR that is significantly lower than Sweden or Canada, and a dark grey box indicates an IRR that is significantly higher than Sweden or Canada. Non-significant results are represented by the white colored boxes. The comparison to Sweden was pre-specified in the protocol, the comparison to Canada was added, as a sensitivity analysis post-hoc.
Abbreviations: IRR, incidence rate ratio; MOF, major osteoporotic fracture.
Across continents, the IRRs in men and women at 50-54 years from Canada, Australia and US were similar to that in Sweden. The results were quite heterogenous at older ages, when comparing the derived IRRs in women above age 70 years to those from Sweden, whereas the data in men was more sketchy. Noteworthy, the IRRs in one study from Australia were higher than those in Sweden in older women (Figure 5, Appendix 5).
Comparison to Canada:
When using the Canadian Manitoba data(6) as a reference, the MOF/hip IRRs at 50-54 years were significantly lower for both men and women from Finland and Denmark by 30-60%, and for women only from Italy, Netherlands and UK, by 41-54% (Figure 5, Appendix 5). For the age categories 70-85 years, most European countries exhibited significant differences by comparison to Canada, in both genders. At older ages 85+ year, there were significant differences for women from all European countries (with lower IRR by 14-28%) compared to Canada, while the rates in men were similar with the exception of Iceland and the Netherlands. For non-European countries, the only significant difference in IRR was noted between Canada and one study from Australia that showed significantly higher IRR in women above 75 years (Figure 5, Appendix 5).
B-. Studies not providing data on the number of incident fractures
We identified 9 studies that provided fracture incidence rates (without number of incident), both in men and women, and by age category, from which we were able to calculate the MOF/hip IRR, but not the IRR 95% CI (19–21, 32, 35, 41, 42, 44, 46). These studies were distributed as follows: 2 studies from Asia (Korea (19), Japan (21)); 6 studies from Europe (Hungary (35); Spain, Catalonia (20); Sweden (44); Switzerland (41, 42); Edinburgh, UK (32)) and one from US (46). All but 2 were retrospective studies (32, 41). Fractures were identified through ICD-9 or 10 codes in 7 studies (19, 20, 35, 41, 42, 46, 49). Only one study reported the population ethnicity (41). Data on fractures at MOF sites were collected within the same period for all fractures in 7 studies, while the period differed across fracture sites for the remaining 2 studies (44, 46). For instance, the data from Malmo Sweden spread over an 8-year period, with fracture incidence rates at the hip collected in 1991, forearm in 1994, proximal humerus in 1987, and for clinical vertebral in 1993-1994 (44, 50). The US FRAX study reported on hip fracture derived from the Nationwide Inpatient Sample (NIS) in 2006, and the non-hip fractures were derived from the Rochester Epidemiology Project 1989-1991 (46). Five studies collected data from nationwide registries (Korea (19), Hungary (35), Swiss (41, 42), US (46)). Four other studies were representative of specific regions in a given country such as Sado city in Japan (21), Catalonia in Spain (20), Malmo in Sweden (44, 50), and Edinburgh in UK (32). The quality score of these studies was poor in 3 (20, 21, 44), fair in 4 (19, 32, 35, 42), and good in 2 (41, 46) (Appendix 3).
The MOF/Hip IRRs were higher in younger age categories compared to older age categories, higher in women compared to men, and varied across countries. However, we were not able to assess for the statistical significance of these differences (Appendix 4).
Discussion
We have shown that MOF/hip IRRs are higher in women compared to men and decrease with age. However, these findings were heterogenous across regions and countries. Importantly, age and gender-specific MOF/hip IRRs varied significantly across European countries in comparison to Sweden, and these variations were consistent in women at 50-54 years and above age 70 years. Differences between Sweden and non-European countries were quite heterogenous. Our findings may have important implications to the derived estimated MOF incidence rates for many countries where the Malmo Sweden MOF/Hip IRRs are used to derive country specific FRAX derived estimates. It is possible that the magnitude of the differences in MOF/hip IRR, at younger age groups, for some countries (Europe) may not have an impact on the estimated incidence rates using FRAX, of sufficient clinical significance to affect recommendations. However, differences in fracture risk estimates might have important clinical implications, in the older age categories, a particularly high-risk population, where such estimates would have a major impact on clinical decision making, at the individual and public health level. This possibility cannot be assessed because the exact algorithm that uses derived IRRs in the FRAX calculator is not known.
Because of the lack of valid fracture incidence data at the 4 MOF skeletal sites in several countries worldwide, FRAX assumes that MOF/Hip IRRs are similar across regions to ones derived from a fracture registry from Malmo Sweden (5). FRAX calculator therefore uses the Malmo MOF/hip IRRs to derive 10-year MOF estimates for almost all country specific calculators (5), with the exception, to the best of our knowledge, of Iceland (33) , and Switzerland (51, 52). In fact, several countries with available MOF data (UK, US, Canada and Japan) have imputed incidence rates for one or more non-hip fracture based on the Malmo, Sweden data. This is because they detected important limitations of their country specific non-hip fracture epidemiology (44, 46, 50, 53–57).
Several studies have reported FRAX validation in various countries, comparing actual versus expected MOF rates using the Malmo data as a surrogate to derive IRRs. One study from Iceland (N, 18,872; follow up 26 years) showed similarities between observed and expected MOF rates (33). Another one on the development of FRAX Maldova (N 209,010; follow up 24 months) revealed very similar observed and expected incidence rates for humerus and forearm fractures, but comparisons for other MOF were not provided (58). Conversely, other studies from Canada (59), Spain (60), Australia (61), and France (especially in the elderly) (62) reported differences in the predicted versus the actual MOF incident fractures. Although such findings may be explained by differences in fracture identification methods, more notoriously challenging for vertebral fractures, and possibly by secular trends in fracture rates, true differences in MOF/hip IRRs may be contributing. The best action for countries that lack good quality data on fracture incidence is unknown. In the absence of high quality country specific hip fracture data, the International Society of Clinical densitometry (ISCD) recommended “a country-specific FRAX model can be built using hip fracture incidence rates from a surrogate country, but with incorporation of country-specific mortality rates. Grade: Fair” (63). It assumed the use of the Malmo data for IRRs to derive MOF estimates. Furthermore, there are only a handful of countries that have MOF data, let alone good quality data. Prospective cohort studies that compare observed and estimated fracture incidence rates (from FRAX derived estimates) may be the best strategy to gain insight into the validity of nation specific FRAX calculators. The differences we observed between various countries and Sweden were not consistent across all countries and all age groups. They were mostly noted in women at older age categories (> 70 years), and for countries in Europe (Finland, Netherlands, UK, Italy, Iceland and Denmark). They were less consistent in Asia, Australia and US. Previous data from the GLOW study showed significant differences in the incidence of hip and MOF between various regions, with higher rates of hip fractures and lower rates of MOF in Northern America (included cities: Seattle, Los Angeles, New York, Worcester, Cincinnati, Pittsburgh, Birmingham) compared to Northern and Southern Europe (included countries: UK, Belgium, France, Spain, Netherlands, Italy, Germany) (64). The MOF to hip ratios in Northern America were lower than those derived from Europe, and the ratios across all GLOW regions were higher than in Malmo, Sweden (64). We were not able to compare our country-specific findings to those derived from the GLOW study, as in the latter, results from different countries were pooled together (64). Canadian MOF/Hip rate ratios, derived from the Manitoba population-based cohort, were reported to be higher than those derived from the Swedish data, in both men and women (6). However, these results were based on observation rather than statistical testing (6). Although the reference country was Sweden similar to our study, the data were derived from the Malmo registry (44), while ours were derived from Skåne Health Care Register (23).
An important consideration is the variability of fracture risk by ethnicity, within the same country. The approach to this complex problem would be as one of the following options, either splitting calculator by ethnicity as is the case of FRAX US, Singapore, China (4), or lumping all ethnicities in a given country in one calculator, as the quality of data for individual ethnicities might be a limitation. For instance, Canada, India and Israel are known to have variable ethnicities, but they have adopted one FRAX calculator, to all ethnicities (4). Noteworthy, the ISCD position in 2011 recommended the use of ethnicity specific FRAX calculators for US Asians, Blacks and Hispanics, and the US Caucasian FRAX calculator US Native American women, until additional data becomes available (Grade: Fair) (63).
Our study has some limitations. We compared MOF/Hip IRRs to a study from Sweden, but not to the Malmo Sweden data, because information on the number of fractures in that study is not available(44, 50). Such data is crucial to derive the confidence intervals for the age and gender specific IRRs. Other limitations are inherent to the studies themselves. These include sub-optimal study design, and lack of a clear definition for fragility fracture, or level of trauma involved. Four studies excluded traumatic or pathologic fractures (6, 21, 29, 34), nine intended to include specifically osteoporotic fractures (19–22, 40, 41, 43, 44, 46), but in reality only one provided an explicit and appropriate definition of fragility fractures (30). However, although low trauma fractures have been traditionally used to define osteoporosis, some data show that traumatic fractures seem to be associated with low bone mineral density and increased fracture risk (65, 66) The definition of MOF was also quite variable across studies. While MOF are recognized as fractures occurring at proximal femur, clinical vertebra, proximal humerus and distal forearm or wrist, some studies defined it differently, by including distal radius only for forearm fractures (29, 30), or total humerus (31), or humerus fractures, without further details on location (6, 22, 34, 37, 39, 40, 47, 48). The majority of the studies defined vertebral fractures as clinical (6, 11, 22, 29–31, 33, 36, 40, 43, 45, 47) while few others did not specify that (37–39, 48). One study reported on vertebral fractures identified from the radiologist’s report, but without further details (34). Seven studies provided data on MOF fracture incidence at each skeletal site separately and also at all four major osteoporotic fractures combined together (31, 33, 40, 43, 45, 47, 48). We used the latter data for our results. Two studies provided only data on MOF fractures combined (6, 45). All the remaining studies provided individual fracture data per site (11, 22, 23, 29, 30, 34, 36, 38, 39). Therefore, our calculation of MOF, as the sum of the incidence of the 4 fractures, and therefore the IRR, might have been inflated, due to double counting of patients who had experienced more than one fracture. This might be also the case when MOF were combined in the studies themselves, unless only “first” fractures were considered (6, 33, 34, 36, 45). Finally, our results showed wide confidence intervals in younger individuals, driven by the small number of events in such age categories.
Although we would expect that the MOF/hip IRR decreases with age, we did not detect a significant difference when comparing younger (50-54 years) to older (80-85 years), for few studies from US, Australia, and Japan (29, 34, 38). Similarly, gender dimorphism in the MOF/hip incidence rate ratio was not consistently present across countries. The reasons for such unexpected findings are not totally clear, but could be explained by methods to identify MOF fractures (ie x-ray review, or ICD codes that might lead to misclassification most notably for incident clinical vertebral fractures). Other factors might be related to the representativeness of the cohort used, and sample size considering fractures are relatively uncommon at younger age groups. Only one previous study from Manitoba Canada has compared MOF/hip ratio across all age categories and showed that it decreases with age, based on the comparison of the 95% CI (6). The same study, using participants’ data, showed that the OR of any MOF to hip was 13-52% lower in men compared to women, across 50-90+ years (6). Such estimates are within the range we report across age groups in men compared to women in our study. Finally, we did not identify any study from the Middle East or North Africa to conduct such analyses. Similarly, we were not able to take into account secular trends that could impact the actual MOF/Hip IRRs if derived across wide periods when performing comparisons across countries. Indeed, the epidemiologic studies included in this manuscript spread from 1999-2017 for most with the exception of Iceland (registry started in 1967).
Our study has important strengths. It sheds light on an assumption that has major implications on an important and widely used fracture risk assessment calculator worldwide. We are unaware of any studies systematically evaluating the variability in MOF/hip ratio, with calculation of CIs to allow comparisons between countries, and that applied a critical appraisal of the quality of studies available. We did not use the Newcastle quality assessment instrument (67) because it did not contain the key domains relevant to epidemiologic studies on fractures. It is possible that the quality of studies may have been underestimated due to the fact that authors omitted information on important domains. Noteworthy, the studies used to compare IRR across countries had a quality score ≥ 4. Our study also fills an important knowledge gaps on the epidemiology of major osteoporotic fractures worldwide that needs to be addressed (2, 5, 68).
Conclusion
The MOF/hip fracture IRRs vary across some countries, and mostly in women above age 70 years. This variability may affect the 10-year fracture risk prediction using FRAX. This would depend on the impact of observed differences on derived FRAX MOF estimates. Therefore, the assumption that MOF/Hip IRR is similar to the one derived from Malmo Sweden may not be valid universally. There is a necessity for country specific data for FRAX to be optimally useful. Further research is needed to validate our findings and elucidate the clinical implication of such findings.
Supplementary Material
Acknowledgments
Authors who replied to our emails and provided missing data whenever available: A. Papaioannou, B. Atkinson, B. Leslie, C. Kennedy, D. Goltzman, F. de Vries, J. Driessen, K. Lippuner, K. Siggeirsdóttir, LJ. Melton, S. Morin, T. Van Staa.
Funding
Research reported in this publication was in part supported by the Fogarty International Center and Office of Dietary Supplements of the National Institutes of Health under Award Number D43 TW009118; PI Ghada El-Hajj Fuleihan. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure Page
All authors declare having no conflict of interest with regards to the submitted work.
Contributor Information
Marlene Chakhtoura, Calcium Metabolism & Osteoporosis Program, American University of Beirut Medical Center, Beirut, Lebanon.
H Dagher, Calcium Metabolism & Osteoporosis Program, American University of Beirut Medical Center, Beirut, Lebanon.
S Sharara, Calcium Metabolism & Osteoporosis Program, American University of Beirut Medical Center, Beirut, Lebanon.
S Ajjour, Calcium Metabolism & Osteoporosis Program, American University of Beirut Medical Center, Beirut, Lebanon.
JA Cauley, Department of Epidemiology, Graduate School of Public Health, University of Pittsburgh, Pennsylvania.
Z Mahfoud, Weill Cornell Medicine-Qatar, Education City, Doha, Qatar.
R Boudreau, Department of Epidemiology, Graduate School of Public Health, University of Pittsburgh, Pennsylvania.
Ghada El Hajj Fuleihan, Calcium Metabolism & Osteoporosis Program, American University of Beirut Medical Center, Beirut, Lebanon.
References
- 1.Kanis JA, Harvey NC, Johansson H, et al. FRAX Update. J Clin Densitom, 2017. 20(3):360–367. [DOI] [PubMed] [Google Scholar]
- 2.El-Hajj Fuleihan G, Chakhtoura M, Cauley JA, and Chamoun N. Worldwide Fracture Prediction. Journal of Clinical Densitometry, 2017. 20(3):397–424. [DOI] [PubMed] [Google Scholar]
- 3.Kanis JA, Johnell O, Oden A, et al. FRAX™ and the assessment of fracture probability in men and women from the UK. Osteoporosis International, 2008. 19(4):385–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanis JA. Fracture Risk Assessment Tool. Available from: https://www.sheffield.ac.uk/FRAX/. (Accessed in January 2021).
- 5.Kanis JA, Hans D, Cooper C, et al. Interpretation and use of FRAX in clinical practice. Osteoporosis International, 2011. 22(9):2395–2411. [DOI] [PubMed] [Google Scholar]
- 6.Lam A, Leslie WD, Lix LM, et al. Major Osteoporotic to Hip Fracture Ratios in Canadian Men and Women With Swedish Comparisons: A Population-Based Analysis. Journal of Bone and Mineral Research, 2014. 29(5):1067–1073. [DOI] [PubMed] [Google Scholar]
- 7.Cauley JA, Chalhoub D, Kassem AM, and El Hajj Fuleihan G. Geographic and ethnic disparities in osteoporotic fractures. Nature Reviews. Endocrinology, 2014. 10(6):338–351. [DOI] [PubMed] [Google Scholar]
- 8.Ballane G, Cauley JA, Luckey MM, and El-Hajj Fuleihan G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporosis International, 2017. 28(5):1531–1542. [DOI] [PubMed] [Google Scholar]
- 9.Kanis JA, Oden A, McCloskey EV, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos International, 2012. 23(9):2239–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sibai A, Nasser W, Ammar W, et al. Hip fracture incidence in Lebanon: a national registry-based study with reference to standardized rates worldwide. Osteoporosis International, 2011. 22(9):2499–2506. [DOI] [PubMed] [Google Scholar]
- 11.Curtis EM, van der Velde R, Moon RJ, et al. Epidemiology of fractures in the United Kingdom 1988–2012: Variation with age, sex, geography, ethnicity and socioeconomic status. Bone (New York, N.Y.), 2016. 87:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navarro MC, Sosa M, Sosa M, et al. Poverty is a risk factor for osteoporotic fractures. Osteoporosis International, 2009. 20(3):393–398. [DOI] [PubMed] [Google Scholar]
- 13.Crandall CJ, Han W, Greendale GA, et al. Socioeconomic status in relation to incident fracture risk in the Study of Women’s Health Across the Nation. Osteoporosis International, 2014. 25(4):1379–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper C, Cole ZA, Holroyd CR, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporosis International, 2011. 22(5):1277–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ballane G, Cauley JA, Luckey MM, and El Hajj Fuleihan G. Secular Trends in Hip Fractures Worldwide: Opposing Trends East Versus West: Secular Trends in hip fracture worldwide. Journal of Bone and Mineral Research, 2014. 29(8):1745–1755. [DOI] [PubMed] [Google Scholar]
- 16.Chakhtoura M, Dagher H, Sharara S, et al. Major osteoporotic fracture to hip fracture incidence rate ratios: a systematic review of observational studies. 2019; Available from: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=129259. (Accessed in January 2021). [DOI] [PMC free article] [PubMed]
- 17.Rothman KJ, Greenland S, and Lash TL, Modern epidemiology: Third edition. 2011. [Google Scholar]
- 18.PlotDigitizer. 2015; Available from: http://plotdigitizer.sourceforge.net/. (Accessed in January 2021).
- 19.Park C, Ha Y-C, Jang S, et al. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. Journal of Bone and Mineral Metabolism, 2011. 29(6):744–751. [DOI] [PubMed] [Google Scholar]
- 20.Pagès-Castellà A, Carbonell-Abella C, Avilés FF, et al. Burden of osteoporotic fractures in primary health care in Catalonia (Spain): a population-based study. BMC Musculoskeletal Disorders, 2012. 13(1):79–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sakuma M, Endo N, Oinuma T, et al. Incidence and outcome of osteoporotic fractures in 2004 in Sado City, Niigata Prefecture, Japan. Journal of Bone and Mineral Metabolism, 2008. 26(4):373–378. [DOI] [PubMed] [Google Scholar]
- 22.Piscitelli P, Brandi ML, Chitano G, et al. Epidemiology of fragility fractures in Italy. Clinical Cases in Mineral and Bone Metabolism, 2011. 8(2):29–34. [PMC free article] [PubMed] [Google Scholar]
- 23.Rosengren BE, Karlsson M, Petersson I, and Englund M. The 21st-Century Landscape of Adult Fractures: Cohort Study of a Complete Adult Regional Population. Journal of Bone and Mineral Research, 2015. 30(3):535–542. [DOI] [PubMed] [Google Scholar]
- 24.Cauley JA, El Hajj Fuleihan G, Arabi A, et al. Official positions for FRAX® clinical regarding international differences: from joint official positions development conference of the international society for clinical densitometry and international osteoporosis foundation on FRAX®. Journal of Clinical Densitometry, 2011. 14(3):240–262. [DOI] [PubMed] [Google Scholar]
- 25.Infoplease. Available from: https://www.infoplease.com/. (Accessed in January 2021).
- 26.IndexMundi. 2020; Available from: https://www.indexmundi.com/. (Accessed in January 2021).
- 27.WorldAtlas. 2021; Available from: https://www.worldatlas.com/. (Accessed in January 2021).
- 28.Stang A Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European Journal of Epidemiology, 2010. 25(9):603–605. [DOI] [PubMed] [Google Scholar]
- 29.Tsukutani Y, Hagino H, Ito Y, and Nagashima H. Epidemiology of fragility fractures in Sakaiminato, Japan: incidence, secular trends, and prognosis. Osteoporosis International, 2015. 26(9):2249–2255. [DOI] [PubMed] [Google Scholar]
- 30.Koski AM, Patala A, Patala E, and Sund R. Incidence of osteoporotic fractures in elderly women and men in Finland during 2005–2006: a population-based study. Scandinavian Journal of Surgery, 2014. 103(3):215–221. [DOI] [PubMed] [Google Scholar]
- 31.Driessen JH, Hansen L, Eriksen SA, et al. The epidemiology of fractures in Denmark in 2011. Osteoporosis International, 2016. 27(6):2017–2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Singer BR, McLauchlan GJ, Robinson CM, and Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. Journal of Bone and Joint Surgery. British volume, 1998. 80(2):243. [DOI] [PubMed] [Google Scholar]
- 33.Siggeirsdottir K, Aspelund T, Johansson H, et al. The incidence of a first major osteoporotic fracture in Iceland and implications for FRAX. Osteoporosis International, 2014. 25(10):2445–2451. [DOI] [PubMed] [Google Scholar]
- 34.Sanders KM, Seeman E, Ugoni AM, et al. Age- and Gender-Specific Rate of Fractures in Australia: A Population-Based Study. Osteoporosis International, 1999. 10(3):240–247. [DOI] [PubMed] [Google Scholar]
- 35.Péntek M, Horváth C, Boncz I, et al. Epidemiology of osteoporosis related fractures in Hungary from the nationwide health insurance database, 1999–2003. Osteoporosis International, 2007. 19(2):243–249. [DOI] [PubMed] [Google Scholar]
- 36.Pasco JA, Lane SE, Brennan-Olsen SL, et al. The Epidemiology of Incident Fracture from Cradle to Senescence. Calcified Tissue International, 2015. 97(6):568–576. [DOI] [PubMed] [Google Scholar]
- 37.Papaioannou A, Kennedy CC, Ioannidis G, et al. Comparative trends in incident fracture rates for all long-term care and community-dwelling seniors in Ontario, Canada, 2002–2012. Osteoporosis International, 2016. 27(3):887–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Melton LJ III, Crowson CS, and O’Fallon WM. Fracture Incidence in Olmsted County, Minnesota: Comparison of Urban with Rural Rates and Changes in Urban Rates Over time. Osteoporosis International, 1999. 9(1):29–37. [DOI] [PubMed] [Google Scholar]
- 39.Manthripragada AD, O’Malley CD, Gruntmanis U, et al. Fracture incidence in a large cohort of men age 30 years and older with osteoporosis. Osteoporosis International, 2015. 26(5):1619–1627. [DOI] [PubMed] [Google Scholar]
- 40.Lix LM, Azimaee M, Osman BA, et al. Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health, 2012. 12(1):301–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lippuner K, Johansson H, Johansson H, et al. Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporosis International, 2009. 20(7):1131–1140. [DOI] [PubMed] [Google Scholar]
- 42.Lippuner K, Grifone S, Grifone S, et al. Comparative trends in hospitalizations for osteoporotic fractures and other frequent diseases between 2000 and 2008. Osteoporosis International, 2012. 23(3):829–839. [DOI] [PubMed] [Google Scholar]
- 43.Klop C, Welsing PMJ, Leufkens HGM, et al. The Epidemiology of Hip and Major Osteoporotic Fractures in a Dutch Population of Community-Dwelling Elderly: Implications for the Dutch FRAX(R) Algorithm. PloS One, 2015. 10(12):e0143800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kanis J, Oden A, Johnell O, et al. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporosis International, 2001. 12(5):417–427. [DOI] [PubMed] [Google Scholar]
- 45.Ettinger B, Ensrud KE, Ensrud KE, et al. Performance of FRAX in a cohort of community-dwelling, ambulatory older men: the Osteoporotic Fractures in Men (MrOS) study. Osteoporosis International, 2013. 24(4):1185–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ettinger B, Black DM, Dawson-Hughes B, Pressman AR, and Melton LJ. Updated fracture incidence rates for the US version of FRAX. Osteoporosis International, 2009. 21(1):25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Azagra R, Zwart M, Encabo G, et al. Rationale of the Spanish FRAX model in decision-making for predicting osteoporotic fractures: an update of FRIDEX cohort of Spanish women. BMC Musculoskeletal Disorders, 2016. 17(1):262–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Azagra R, Zwart M, Aguyé A, et al. Fracture experience among participants from the FROCAT study: what thresholding is appropriate using the FRAX tool? Maturitas, 2015. 83:65–71. [DOI] [PubMed] [Google Scholar]
- 49.van Staa TP, Dennison EM, Leufkens HGM, and Cooper C. Epidemiology of fractures in England and Wales. Bone (New York, N.Y.), 2001. 29(6):517–522. [DOI] [PubMed] [Google Scholar]
- 50.Kanis J, Johnell O, Oden A, et al. Long-term risk of osteoporotic fracture in Malmö. Osteoporosis International, 2000. 11(8):669–674. [DOI] [PubMed] [Google Scholar]
- 51.Suhm N, Lamy O, Lippuner K, and OsteoCare study g. Management of fragility fractures in Switzerland: results of a nationwide survey. Swiss Medical Weekly, 2008. 138(45–46):674–683. [DOI] [PubMed] [Google Scholar]
- 52.Lippuner K, Golder M, and Greiner R. Epidemiology and direct medical costs of osteoporotic fractures in men and women in Switzerland. Osteoporosis International, 2004. 16(S02):S8–S17. [DOI] [PubMed] [Google Scholar]
- 53.DeLusignan S, Teasdale S, Little D, et al. Comprehensive computerised primary care records are an essential component of any national health information strategy: report from an international consensus conference. Informatics in Primary Care, 2004. 12(4):255–264. [DOI] [PubMed] [Google Scholar]
- 54.Melton LJ and Kallmes DF. Epidemiology of Vertebral Fractures: Implications for Vertebral Augmentation. Academic Radiology, 2006. 13(5):538–545. [DOI] [PubMed] [Google Scholar]
- 55.Fujiwara S, Kasagi F, Masunari N, et al. Fracture Prediction From Bone Mineral Density in Japanese Men and Women. Journal of Bone and Mineral Research, 2003. 18(8):1547–1553. [DOI] [PubMed] [Google Scholar]
- 56.Dawson-Hughes B, Looker AC, Tosteson ANA, et al. The potential impact of new National Osteoporosis Foundation guidance on treatment patterns. Osteoporosis International, 2010. 21(1):41–52. [DOI] [PubMed] [Google Scholar]
- 57.Kanis JA, Johansson H, Oden A, et al. The effects of a FRAX® revision for the USA. Osteoporosis International, 2009. 21(1):35–40. [DOI] [PubMed] [Google Scholar]
- 58.Zakroyeva A, Lesnyak O, Cazac V, et al. Epidemiology of osteoporotic fracture in Moldova and development of a country-specific FRAX model. Archives of Osteoporosis, 2020. 15(1):13–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fraser LA, Langsetmo L, Berger C, et al. Fracture prediction and calibration of a Canadian FRAX® tool: a population-based report from CaMos. Osteoporosis International, 2010. 22(3):829–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.González-Macías J, Marin F, Vila J, and Díez-Pérez A. Probability of fractures predicted by FRAX® and observed incidence in the Spanish ECOSAP Study cohort. Bone (New York, N.Y.), 2011. 50(1):373–377. [DOI] [PubMed] [Google Scholar]
- 61.Holloway-Kew KL, Zhang Y, Betson AG, et al. How well do the FRAX (Australia) and Garvan calculators predict incident fractures? Data from the Geelong Osteoporosis Study. Osteoporosis International, 2019. 30(10):2129–2139. [DOI] [PubMed] [Google Scholar]
- 62.Sornay-Rendu E, Munoz F, Delmas PD, and Chapurlat RD. The FRAX tool in French women: How well does it describe the real incidence of fracture in the OFELY cohort. Journal of Bone and Mineral Research, 2010. 25(10):2101–2107. [DOI] [PubMed] [Google Scholar]
- 63.Hans DB, Kanis JA, Baim S, et al. Joint Official Positions of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX®. Executive Summary of the 2010 Position Development Conference on Interpretation and Use of FRAX® in Clinical Practice. Journal of Clinical Densitometry, 2011. 14(3):171–180. [DOI] [PubMed] [Google Scholar]
- 64.Pfeilschifter J, Cooper C, Watts NB, et al. Regional and age-related variations in the proportions of hip fractures and major fractures among postmenopausal women: the Global Longitudinal Study of Osteoporosis in Women. Osteoporosis International, 2011. 23(8):2179–2188. [DOI] [PubMed] [Google Scholar]
- 65.Mackey, Liu LY, Cawthon P, et al. High-trauma fractures and low bone mineral density in older women and men. JAMA 2007; 298(20): 2381–2388. [DOI] [PubMed] [Google Scholar]
- 66.Leslie W, Schousboe J, Morin S, et al. Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporos Int 2020; 31(6): 1059–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wells G 2019; Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. (Accessed in January 2021).
- 68.Kanis JA, Johansson H, Harvey NC, and McCloskey EV. A brief history of FRAX. Archives of Osteoporosis, 2018. 13(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


