Abstract
Childhood abuse and/or neglect adversely influences development of neurocognitive systems that regulate affect and behavior. Poor inhibitory control over emotional reactions is thus one potential pathway from maltreatment to suicide. Adult psychiatric inpatients completed the Childhood Trauma Questionnaire and an emotional stop-signal task indexing negative emotional action termination (NEAT): the ability to inhibit ongoing motor reactions to aversive stimuli triggered by negative affect. Clinical interviews assessed suicidal thoughts and behaviors during hospitalization (n = 131) and at follow-up assessments six months later (n = 87). Our primary aim was to examine whether maltreatment history and NEAT explain overlapping variance in suicidal behaviors (1) retrospectively and (2) six months following hospital discharge. Contrary to prediction, childhood maltreatment was unrelated to history of suicidal behaviors. However, NEAT was consistently associated with prior suicidal acts, even controlling for suicidal ideation and demographic covariates. NEAT similarly contributed to the prediction of post-discharge suicidal behaviors, whereas we found no effect of maltreatment history. The present study suggests that NEAT captures suicide risk independently of childhood maltreatment. Results implicated NEAT impairment specifically, rather than broader response inhibition deficits (e.g., to positive stimuli), in past and future suicidal behaviors. These findings provide preliminary support for NEAT as a behavioral vulnerability marker for suicide, with implications for understanding links between maltreatment history and suicidal acts.
Keywords: Child abuse, cognitive control, emotion dysregulation, suicide, trauma
Suicide is widely acknowledged as a global health crisis. Nearly one million people die by suicide each year, and suicide is a leading cause of death worldwide across all age groups (World Health Organization, 2018). These fatalities add to the tremendous international burden associated with an estimated 25–30 million suicide attempts occurring annually (Bachmann, 2018; Crosby et al., 2011). Since known risk factors only modestly predict suicidal behaviors (SBs; Franklin et al., 2017), scientific understanding of suicide pathophysiology necessary to inform intervention and prevention strategies remains limited. Accordingly, the purpose of this study was to evaluate a candidate behavioral marker of neurocognitive processes previously linked to self-injurious behaviors (i.e., aspects of inhibitory control and emotion reactivity) in a sample of patients at elevated risk for suicide.
Early life adversity, including caregiver maltreatment (i.e., emotional, physical, and sexual abuse or neglect) and other chronic stressors (e.g., poverty, institutionalization) confer vulnerability to psychological dysfunction and poor clinical outcomes (Gilbert et al., 2009; McCrory & Viding, 2015). Early abuse, neglect, and other types of chronic and/or traumatic stress increase the likelihood of subsequent SBs (see Angelakis et al., 2019 for a review). Indeed, childhood trauma may increase the risk of later attempts between three- and four-fold, according to a recent meta-analysis (Zatti et al., 2017). Child maltreatment is alarmingly common, affecting more than 1 in 8 American children (Wildeman et al., 2014), with some estimates as high as 40% (Gilbert et al., 2009).
Childhood maltreatment has established neurodevelopmental consequences that may contribute to suicide risk. Broadly, salient negative experiences that occur within sensitive developmental windows adversely influence the maturation of neurocognitive systems involved in self-regulation of cognition, emotion, and behavior (e.g., Gunnar & Quevedo, 2007; Loman et al., 2013; Maughan & Cichetti, 2002; Pollak et al., 2010; Rogosch et al., 2011; Teicher et al., 2016; Weissman et al., 2019). Neuropsychological sequalae of early life adversity include cognitive and affective control deficits that can elevate later suicide risk (Allen et al., 2019; Jollant et al., 2011; Turecki et al., 2012; Van Heeringen et al., 2014; Zhang et al., 2014). Impaired affective control may stem from dysfunction in two interactive brain networks: (1) heightened “bottom-up” emotion reactivity in subcortical (e.g., limbic, striatal) regions responsible for automatic stimulus evaluation, paired with (2) deficient “top-down” inhibitory control from frontal/cortical areas (Aldao et al., 2016; Beauchaine & Haines, 2019; Comte et al., 2016).
Deficits in controlled processing of emotional information may promote automatic, instinctive, and/or reflexive responses to emotional cues (c.f., Carver et al., 2017). Underlying affective control deficits might therefore manifest as insufficient deliberation before initiating action and/or difficulty inhibiting motor impulses motivated by powerful affective states (Carver & Johnson, 2018). The functional consequences of such deficits include dispositional traits that reflect established suicide risk factors, e.g., urgency or emotion-related impulsivity (Allen et al., 2019). Affective control impairment may thus represent a transdiagnostic pathway from childhood maltreatment to clinical outcomes like suicide (Allen et al., 2019, 2020; Berzenski, 2018; Heleniak et al., 2015; Kim & Cichetti, 2010; McCrory & Viding, 2015; McLaughlin & Lambert, 2017; Turecki et al., 2012; Weissman et al., 2019).
The current study employs a novel behavioral index of affective control to examine cognitive factors linking maltreatment and SBs within a sample of adult psychiatric inpatients. We specifically use an Emotional Stop-Signal Task (ESST; Allen & Hooley, 2015; 2019) to examine emotional response inhibition: inhibitory control over motor reactions to affective image stimuli. Emotional response inhibition may be divided into two sequential stages: (1) an earlier stage requiring suppression of emotional reactions before initiating a corresponding motor response (e.g., Schulz et al., 2007; 2009); and (2) a later stage demanding termination of an ongoing or initiated motor response following emotional reactions; in the negative valence domain, we refer to this process as negative emotional action termination (NEAT; Allen & Hooley, 2019). Preliminary evidence supports the idea that deficits in both processes may represent neurocognitive mechanisms for urgency and conceptually-related traits reflecting affective control deficits (see Allen & Hooley, 2019; Allen et al., 2019, 2020; Burke et al., 2021; Chester et al. 2016; Rochat et al., 2018). Indeed, our past research found that each stage of emotional response inhibition accounts for distinct variance in self-reported urgency, whereas impairment in the latter stage of NEAT uniquely helps explain the association between urgency and nonsuicidal self-injury (NSSI; Allen & Hooley, 2019). This finding is relevant to suicide risk, given that NSSI precludes suicidal intent by definition yet ranks among the strongest predictors of future attempts (Franklin et al., 2016). This study extends our prior work establishing NEAT dysfunction in NSSI (Allen & Hooley, 2015; 2019) by evaluating whether NEAT also contributes to SBs.
Prior work has linked early-stage negative emotional response inhibition (i.e., suppression) deficits to childhood adversity (Johnson & Tottenham, 2015; Tottenham et al., 2010). A recent study by Capistrano and colleagues (2016) further suggests that disruption in this process may be one mechanism underpinning the association between early adversity (i.e., poverty) and internalizing symptoms. Laboratory-based behavioral tasks that incorporate affective stimuli across multiple valences (i.e., positive, negative) can help elucidate whether emotional conditions modulate cognitive control abilities (e.g., response inhibition). This approach is therefore particularly well-suited to examine neurodevelopmental sequelae of early-life stress and maltreatment. To our knowledge, however, no prior research has evaluated late-stage negative emotional response inhibition (i.e., NEAT) in relation to child maltreatment or suicide, and the majority of laboratory studies examining cognitive/affective control have been conducted in community or student samples, limiting potential clinical implications of this literature.
This present study thus sought to determine whether response inhibition deficits within negative emotional contexts, measured via ESST performance, helps explain predicted relationships between childhood maltreatment and SBs among hospitalized psychiatric inpatients. We specifically derived SB composite variables from patient interviews (see additional information below) to increase statistical variance in patient outcomes, consistent with recent literature (e.g., Armey et al., 2018). We hypothesized the following: (1) Childhood maltreatment would be positively associated with SB history; (2) Worse NEAT on the ESST (i.e., a higher proportion of commission errors to negative stimuli reflecting specific difficulty inhibiting negative reactions) would independently predict SB history in regression analyses; (3) NEAT dysfunction would partially account for relations between childhood maltreatment and SB history; and (4) childhood maltreatment would prospectively predict subsequent SBs in the six-month period following hospital discharge through NEAT (i.e., an indirect mediating effect). In sum, we conceptualize NEAT impairment as a neurobehavioral marker of emotion dysregulation, secondary to early adversity, which we predicted would explain variance in cross-sectional and longitudinal associations between childhood maltreatment and subsequent SBs.
Method
Participants and Procedures
We recruited 144 adults (84 women; 58.33%) aged 18–65 (M = 37.59, SD = 13.20) from inpatient units at a psychiatric hospital serving the metropolitan area of a mid-sized city on the east coast of the United States. Participants comprised psychiatric inpatients who completed the ESST as part of two larger studies (R01 MH108610 and R01 MH112674). Eligibility criteria included age (18–65 years), English fluency, and comfort with smartphone technology (for ecological assessment). Individuals experiencing psychotic or mood symptoms severe enough to impede study procedures were excluded from participation. Research staff regularly screened newly-admitted patient charts to identify potentially eligible individuals. Patients were cleared for participation by their treatment team and provided informed consent before completing study procedures. Bachelors’ level research assistants (supervised by a licensed clinical psychologist) conducted IRB-approved participant assessments during hospitalization. We conducted clinical interviews at each baseline session to assess psychiatric history, including suicidal thoughts and behaviors. We also administered a self-report measure of childhood maltreatment. Participants (n = 94; 66.90%) returned for follow-up sessions approximately six months post-discharge (up to 12 months; M = 5.76 , SD = 3.60), during which they completed similar procedures to the baseline session, including an interview assessment of suicidal thoughts and behaviors. Participants who completed the ESST during hospitalization but did not return for follow-up assessment were equivalent to those included in these analyses in terms of childhood maltreatment and SB history.
Measures
Columbia Suicide Severity Rating Scale (C-SSRS)
The C-SSRS (Posner et al., 2008) is a semi-structured interview that assesses lifetime and past-month history of suicidal ideation (SI) as well as SBs over the lifespan and preceding three months. We used C-SSRS ratings to determine participant eligibility and to evaluate SI and SBs, our main outcomes of interest. We calculated composite indices of lifetime and past-month SBs derived from the C-SSRS (comprising actual, aborted, and interrupted attempts), which we re-coded into binary variables, i.e., participants who reported any actual, aborted, and/or interrupted attempts were coded as “1” and those who reported none as “0”. Lifetime and past-month SI were coded according to (1) severity, i.e., the most severe type of ideation endorsed in these timeframes, with 1 = Least Severe (e.g., wish to be dead) to 5 = Most Severe (e.g., ideation with specific plan and intent); as well as (2) frequency of suicidal thinking during the worst period in each assessed timeframe, with 1 = Less than once per week to 5 = Many times each day. Interviews were conducted by trained research staff and audio-recorded; approximately 20% were independently scored by independent raters to confirm reliability (ICCs > .90).
Childhood Trauma Questionnaire (CTQ)
The CTQ (Bernstein et al., 1997) is a 28-item retrospective self-report questionnaire that measures five dimensions of childhood maltreatment: emotional, physical, and sexual abuse as well as emotional and physical neglect. Items are preceded by the prompt, “When I was growing up…” and rated on a five-point Likert scale (1 = Never true to 5 = Very often true). The CTQ has documented reliability and validity (Bernstein et al., 1997; 2003); Cronbach’s alpha in the present study was 0.91. Here, we report primary analyses using CTQ total scores for parsimony, as we obtained similar patterns of results using subscale scores that were positively correlated with SB history (i.e., emotional abuse/neglect and sexual abuse); please see supplementary materials for additional information.
Emotional Stop-Signal Task (ESST)
The ESST (Allen & Hooley, 2015; 2019) is a two-choice emotional response inhibition paradigm, in which participants rapidly judge the valence (positive or negative) of images from International Affective Picture System (Lang et al., 2008) by keypress. A single image from one of three stimulus categories (Negative: e.g., a severely malnourished crying infant; Positive: e.g., smiling children holding puppies; Ambiguous: e.g., a couple with inscrutable facial expressions descending a flight of stairs)1 is randomly presented on each trial (N = 192). Negative and positive images are matched for arousal and valence intensity, whereas the content of ambiguous stimuli is rated as “neutral” in valence as well as neither “arousing” nor “un-arousing” (see Lang et al., 2008).
ESST participants are instructed to judge each serially-presented image as either “pleasant/positive” or “unpleasant/negative” as “quickly and accurately as possible”, responding according to their “gut reaction”. However, 25% of trials include an unpredictable auditory stop-signal presented with a variable delay (50 – 1150 ms) after the stimulus, indicating that participants should inhibit their motor response on those trials. The stop-signal delay is adjusted after each stop-signal trial to approximate a 50% commission error rate (i.e., false alarms) for the entire paradigm, an approach meant to ensure sufficient errors to derive estimates of stop-signal reaction time. Error rates are adjusted independent of stimulus valence. This dynamic tracking algorithm allows for variation between stimulus conditions, enabling us to evaluate whether commission error rates vary between different valence categories of stimuli and responses (e.g., a participant with comparable positive and negative emotional response inhibition abilities would erroneously respond to approximately half of images presented during no-signal trials, regardless of image valence).
The present study focused on inhibitory control over negative reactions or NEAT (negative emotional action termination). Extending previous research (Allen & Hooley, 2015; 2019; Allen et al., 2020), we calculated (1) NEAT as the percentage of commission errors during stop trials with negative stimuli that also reflected negative emotional reactions, i.e., behavioral responses indicating that participants correctly classified the image “negative” but were unable to inhibit this reaction despite the presence of a stop-signal. We further calculated a corresponding metric of (2) positive emotional action termination (PEAT; i.e., commission errors during stop trials with positive stimuli reflecting positive emotional reactions) to determine the specificity of hypothesized effects to NEAT; as well as (3) negative response bias (NRB), the percentage of negative emotional reactions during no-signal trials (including those with ambiguous stimuli), to confirm that predicted NEAT deficits are not simply attributable to an association between SBs and increased likelihood of negative affective judgments, e.g., as characteristic of mood disorders (e.g., Gollan et al., 2016; Murphy et al., 1999). In sum, the above ESST indices will enable us to decompose predicted relations between negative emotional response inhibition and SBs by confirming that observed associations are specific to NEAT in terms of stimulus valence (i.e., effects do not generalize to PEAT) and task condition (i.e., effects do not generalize to NRB), in order to isolate the effects of inhibitory demand over negative reactions during no-signal trials with aversive stimuli (i.e., NEAT).
ESST data were collected using Inquisit 5.0 (Millisecond, 2016) stimulus presentation software. Prior to beginning data collection, participants were provided verbal clarification of task instructions and additional practice opportunities as necessary. Session run logs were reviewed prior to data analysis, and there were no identified problems with hardware or software for participants who completed the task. Following data collection, data cleaning procedures were conducted to examine the presence and influence of potential outliers.2 . All regression models controlled for relevant task performance metrics as covariates of non-interest (i.e., accuracy, false alarms, misses, and NRB).
Analytic Plan
We first examined demographic variables and summary metrics of ESST performance (Table 1) in the entire sample of N = 144 patients; subsequent primary analyses were restricted to participants who completed both the CTQ and ESST at baseline (n = 131; 90.97%) and within that group, those who returned for follow-up (n = 87; 60.42%) out of n = 94 total cases with follow-up C-SSRS data (i.e., including seven participants who did not complete the ESST). Subsequently, we performed a set of bivariate non-parametric correlations to assess relations among C-SSRS indices, CTQ scales, and NEAT. We then used hierarchical logistic regression models (see Cohen, 1986) to test whether negative emotional response inhibition (i.e., NEAT) specifically accounts for shared variance in SBs explained by the CTQ, while controlling for stimulus valence (PEAT entered on a simultaneous step). Regression models included additional ESST performance parameters as covariates, i.e., accuracy of valence judgments of positive and negative images (Accuracy), total commission errors (False Alarms), total omission errors (Misses), and negative response bias (NRB). Note that participant responses to ambiguous stimuli during no-signal trials are included when calculating NRB but not overall accuracy, which is independent of response valence. The first step in each model included covariates (i.e., demographic variables associated with SBs, baseline SI/SB history, and task performance metrics), followed by a step in which we entered CTQ total scores, and a final step including ESST measures of emotional response inhibition, i.e., PEAT and NEAT.
Table 1.
Demographics, SB history, and ESST performance
| SB− (n = 77) | SB+ (n = 67) | Total (N = 144a) | ||
|---|---|---|---|---|
| n (%) | ||||
| Sex | Female | 42 (54.55) | 42 (64.62) | 84 (59.16) |
| Male | 35 (44.87) | 21 (32.31) | 56 (39.44) | |
| Non-binary | – | 2 (3.08) | 2 (1.41) | |
| Sexual Orientation | Heterosexual | 59 (78.67) | 44 (72.13) | 103 (75.74) |
| LGBQ+ | 16 (21.33) | 17 (27.87) | 33 (24.27) | |
| Race | Asian | 1 (1.28) | 4 (5.97) | 5 (3.55) |
| Black or African American | 3 (3.85) | 1 (1.49) | 4 (2.84) | |
| Multiracial/Other | 8 (10.26) | 6 (8.96) | 14 (9.93) | |
| Native American | 2 (2.56) | – | 2 (1.42) | |
| White | 62 (76.92) | 54 (80.60) | 116 (82.27) | |
| Ethnicity | Hispanic or Latinx | 8 (10.81) | 4 (6.56) | 12 (8.89) |
| Non-Hispanic | 66 (89.19) | 57 (93.44) | 123 (91.11) | |
| Marital status | Divorced or separated | 20 (26.67) | 18 (29.03) | 38 (27.74) |
| Married or cohabitating | 14 (18.67) | 8 (12.90) | 22 (16.06) | |
| Single/Never married | 39 (52.00) | 36 (58.07) | 75 (54.75) | |
| Widowed | 2 (2.67) | – | 2 (1.46) | |
| Annual Income (USD) | < $10,000 | 19 (23.08) | 22 (33.85) | 41 (27.59) |
| $10,000 – $29,999 | 21 (26.92) | 19 (27.69) | 40 (26.90) | |
| $30,000 – $49,999 | 25 (32.05) | 10 (15.39) | 35 (24.14) | |
| $50,000 – $69,999 | 4 (3.85) | 2 (3.08) | 6 (3.45) | |
| $70,000+ | 2 (2.56) | 3 (4.62) | 5 (3.45) | |
| Covariate (range) | M (SD) | |||
| Age (18–65 years) | 38.22 (12.34) | 36.85 (14.20) | 37.59 (13.20) | |
| Education (3–23 years) | 14.10 (3.20) | 13.15 (2.86) | 13.67 (3.07) | |
| ESST Accuracyb (48–100%) | 88.97 (10.00) | 86.90 (10.09) | 88.04 (10.05) | |
| ESST False Alarmsb (29–98%) | 54.98 (19.55) | 53.85 (17.49) | 54.47 (18.59) | |
| ESST Missesb (0–35%) | 7.87 (7.11) | 8.05 (7.14) | 7.95 (7.10) | |
| ESST No-signal reaction timeb (426.76–1035.53 ms) | 788.00 (100.01) | 785.19 (121.60) | 786.73 (109.83) | |
| ESST Stop-signal reaction timeb (120.56–817.41 ms) | 349.43 (162.60) | 363.46 (184.74) | 355.75 (172.38) | |
Note. SB = Suicidal Behaviors (measured at baseline); ESST = Emotional Stop-Signal Task. Accuracy calculated as the proportion of correctly classified positive and negative images during no-signal trials.
Missing data included n = 2 (sex), n = 8 (sexual orientation), n = 3 (race), n = 9 (ethnicity), n = 7 (marital status), n = 17 (income), n = 2 (age), and n = 11 (education);
A subset of participants (n = 13) were excluded from the above calculations due to outlier ESST values (e.g., more than 3 SDs from the mean); we accordingly control for relevant ESST performance metrics in subsequent correlational and regression analyses, as excluding these participants reduced statistical power but did not affect hypothesized results (please refer to supplementary materials for analytic results from regression models omitting outlier values and including demographic covariates of non-interest).
Results
SI/SBs at Baseline (N = 144) & Follow-up (n = 94)
The majority of inpatients endorsed a lifetime history of active SI (n = 99; 68.75%), whereas 11 participants (7.64%) reported no more than a wish to be dead, and about one quarter reported no previous SI (n = 34; 23.61%). Most patients also endorsed SI in the month prior to hospitalization (n = 89; 61.81%); approximately one third reported no past-month SI (n = 44; 30.56%). Just over half of participants reported no previous SBs (n = 77; 53.47%). Inpatients with lifetime SB history reported an average of 5.09 prior episodes (SD = 8.27). Over one third of patients (n = 53; 36.81%) reported at least one suicidal act in the month preceding hospitalization (M = 1.58; SD = 1.34; range = 9). We found no differences in demographic characteristics nor overall ESST performance between participants who endorsed previous SBs (at baseline) and those who did not (Table 1). 94 participants (65.28%) returned for the follow-up session; nearly one fifth of these individuals reported post-discharge SBs (M = 2.44; SD = 2.85).
ESST Performance
Overall ESST performance in this sample of adult psychiatric inpatients was comparable to prior studies in community adults (Allen & Hooley, 2015; 2019; Allen et al., 2020) and students (Burke et al., 2021); we observed no differences in overall task performance metrics as a function of SB history (see Table 1). A 3 (valence: ambiguous, positive, negative) X 2 (error type: commission, omission) repeated-measures ANOVA indicated an interaction between stimulus category and error type, F(2, 286) = 34.37, p < 0.001, partial η2 = 0.19. Results suggested that participants missed more no-signal trials (omission error rate M = 12.82%; SD = 14.21%) but made fewer false alarms (commission error rate M = 48.81%; SD = 24.07%) when ambiguous images were presented relative to positive (commission M = 57.43%, SD = 21.88%; omission M = 7.38%, SD = 11.14%) and negative stimuli (commission M = 58.62%, SD = 21.82%; omission M = 8.41%, SD = 12.46%). Another 3 (valence) x 2 (no-signal reaction time) ANOVA further indicated an effect of stimulus valence on reaction times during no-signal trials, F(1.81, 255.80) = 22.89, p < 0.001, partial η2 = 0.14. Post-hoc tests indicated that participants responded most rapidly to positive images (M = 765.53 ms, SD = 132.43 ms), followed by negative (M = 798.42 ms, SD = 127.06 ms) and ambiguous images (M = 817.97 ms, SD = 127.32 ms; all p < .05 with Bonferroni correction). Participants were generally accurate (M > 88%) in classifying the valence of positive and negative images (Table 1).
Baseline SBs, Childhood Maltreatment, & NEAT
Given an association between lifetime SB episodes and fewer years of education, r(132) = −0.20, p = 0.022, we consequently included education as a covariate in subsequent regression models. Additional analyses including other demographic covariates of non-interest (omitted for statistical power) are available in supplementary materials (e.g., Model 4b), as their inclusion did not influence our primary results or conclusions. Neither lifetime nor past-month SB history were independently associated with any other demographic variables. Lifetime SBs were positively associated with childhood maltreatment, specifically more severe emotional abuse and neglect, as well as sexual abuse history (Table 2). SBs were not correlated with childhood physical abuse or neglect, however. Bivariate analyses further revealed an association between CTQ total score and NEAT, but contrary to prediction, NEAT was not correlated with past SB episodes.
Table 2.
Spearman’s rho correlations (n = 131)
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | |
|---|---|---|---|---|---|---|---|---|
|
1. Lifetime SBs (M = 2.37; SD = 6.17) |
– | |||||||
|
2. Past-month SBs (M = 0.58; SD = 1.11) |
0.84*** | – | ||||||
|
3. CTQ Total (M = 48.33; SD = 22.15) |
0.29*** | 0.18* | – | |||||
|
4. CTQ Emotional Abuse (M = 11.58; SD = 5.95) |
0.33*** | 0.17* | 0.79*** | – | ||||
|
5. CTQ Emotional Neglect (M= 11.17; SD = 5.34) |
0.28** | 0.20* | 0.77*** | 0.47*** | – | |||
|
6. CTQ Physical Abuse (M = 8.50; SD = 5.54) |
0.16 | 0.13 | 0.62*** | 0.52*** | 0.31*** | – | ||
|
7. CTQ Physical Neglect (M = 8.29; SD = 4.40) |
0.14 | 0.10 | 0.77*** | 0.49*** | 0.67*** | 0.34*** | – | |
|
8. CTQ Sexual Abuse (M = 8.79; SD = 6.17) |
0.19* | 0.15 | 0.63*** | 0.46*** | 0.25** | 0.46*** | 0.39*** | – |
|
9. NEAT (M = 52.75; SD = 21.99) |
0.08 | −0.01 | 0.19* | 0.16 | 0.13 | 0.06 | 0.16 | 0.08 |
Note. CTQ = Childhood Trauma Questionnaire; NEAT = Negative Emotional Action Termination, i.e., percentage of negative false alarms to negative stimuli on the Emotional Stop-Signal Task;
p < .05;
p < .01;
p < .001.
SB History Classification
Model 1 controlled for years of education, SI, and ESST performance metrics as covariates (Table 3). In contrast to correlational analyses, we did not find a main effect of CTQ total score entered on Step 1. As hypothesized, the addition of NEAT on Step 2 was significant: Greater NEAT (i.e., lower values, which reflect commission error rates) was associated with reduced SB likelihood, such that participants whose performance ranked one standard deviation below average were more than twice as likely to endorse SB history than those ranked one standard deviation above the mean (see Figure 1A). In contrast, PEAT was not linked to prior SBs.
Table 3.
Binary logistic regressions classifying SB history (Model 1) & predicting SB risk (Model 2)
| Model 1: Cross-sectional (N = 131) | Model 2: Longitudinal (n = 87) | |||||
|---|---|---|---|---|---|---|
| Covariates | B (SE) | Odds Ratio (95% CI) | Wald | B (SE) | Odds Ratio (95% CI) | Wald |
| Education | −0.01 (0.08) | 1.00 (0.85–1.17) | 0.00 | 0.24 (0.10) | 1.03 (0.85–1.24) | 0.05 |
| SI Frequency (lifetime) | −0.17 (0.34) | 0.92 (0.48–1.79) | 0.08 | −0.62 (0.68) | 0.48 (0.13–1.84) | 2.04 |
| SI Frequency (past-month) | −0.15 (0.31) | 0.93 (0.51–1.70) | 0.07 | 0.33 (0.64) | 1.48 (0.42–5.18) | 0.64 |
| SI Severity (lifetime) | 2.05 (0.44) | 3.04 (1.27–7.26) | 27.26* | 0.86 (0.71) | 2.96 (0.74–11.86) | 2.99 |
| SI Severity (past-month) | 1.37 (0.44) | 2.05 (0.87 – 4.86) | 3.81 | −0.29 (0.83) | 0.67 (0.13–3.42) | 0.36 |
| SB History (lifetime) | – | – | – | 0.03 (1.46) | 0.63 (0.04–10.86) | 0.11 |
| SB History (past-month) | – | – | – | 0.07 (1.20) | 2.11 (0.20–22.07) | 0.30 |
| Accuracy | −1.03 (0.02) | 0.94 (0.91 – 0.98) | 5.52** | 0.13 (0.01) | 0.99 (0.96–1.02) | 0.38 |
| False Alarms | −0.36 (0.02) | 0.98 (0.95–1.02) | 1.60 | −0.18 (0.04) | 0.93 (0.87–1.00) | 3.73* |
| Misses | −0.26 (0.04) | 0.98 (0.91–1.05) | 0.98 | 0.40 (0.04) | 1.04 (0.96–1.14) | 0.95 |
| NRB | −0.25 (0.03) | 0.98 (0.92–1.04) | 0.51 | 0.24 (0.03) | 1.03 (0.96–1.09) | 0.45 |
| Step 1: Childhood maltreatment | ||||||
| CTQ Total | 0.40 (0.01) | 1.02 (1.00–1.05) | 1.33 | 0.33 (0.02) | 1.01 (0.97–1.05) | 0.20 |
| Model fit: χ2(117) = 91.48, p < 0.001, McFadden R2 = 0.52 | χ2(74) = 57.62, p < 0.001, McFadden R2 = 0.48 | |||||
| Step 2: Emotional response inhibition | ||||||
| PEAT | 0.20 (0.01) | 1.01 (0.96–1.06) | 0.14 | 0.15 (0.06) | 1.08 (0.96–1.21) | 2.57 |
| NEAT * | 1.04 (0.02) | 1.05 (1.00–1.10) | 4.05* | 0.23 (0.04) | 1.09 (1.01–1.17) | 5.02* |
| Full model fit: χ2(115) = 96.19, p < 0.001, McFadden R2 = 0.55 | χ2(72) = 64.60, p < 0.01, McFadden R2 = 0.54 | |||||
Note. 95% CI = 95% Confidence interval (odds ratio scale); SI = Suicidal Ideation; NRB = Negative Response Bias, i.e., the proportion of negative judgments during no-signal trials, regardless of stimulus valence; PEAT = Positive Emotional Action Termination, i.e., percentage of positive false alarms to positive stimuli presented during stop-signal trials on the Emotional Stop-Signal Task. All predictor variables measured at baseline; standardized parameter estimates with robust standard errors are shown at entry step;
p < .05;
p < .01;
p < .001.
Figure 1. Conditional probability of SB history (panel A) & risk (panel B).
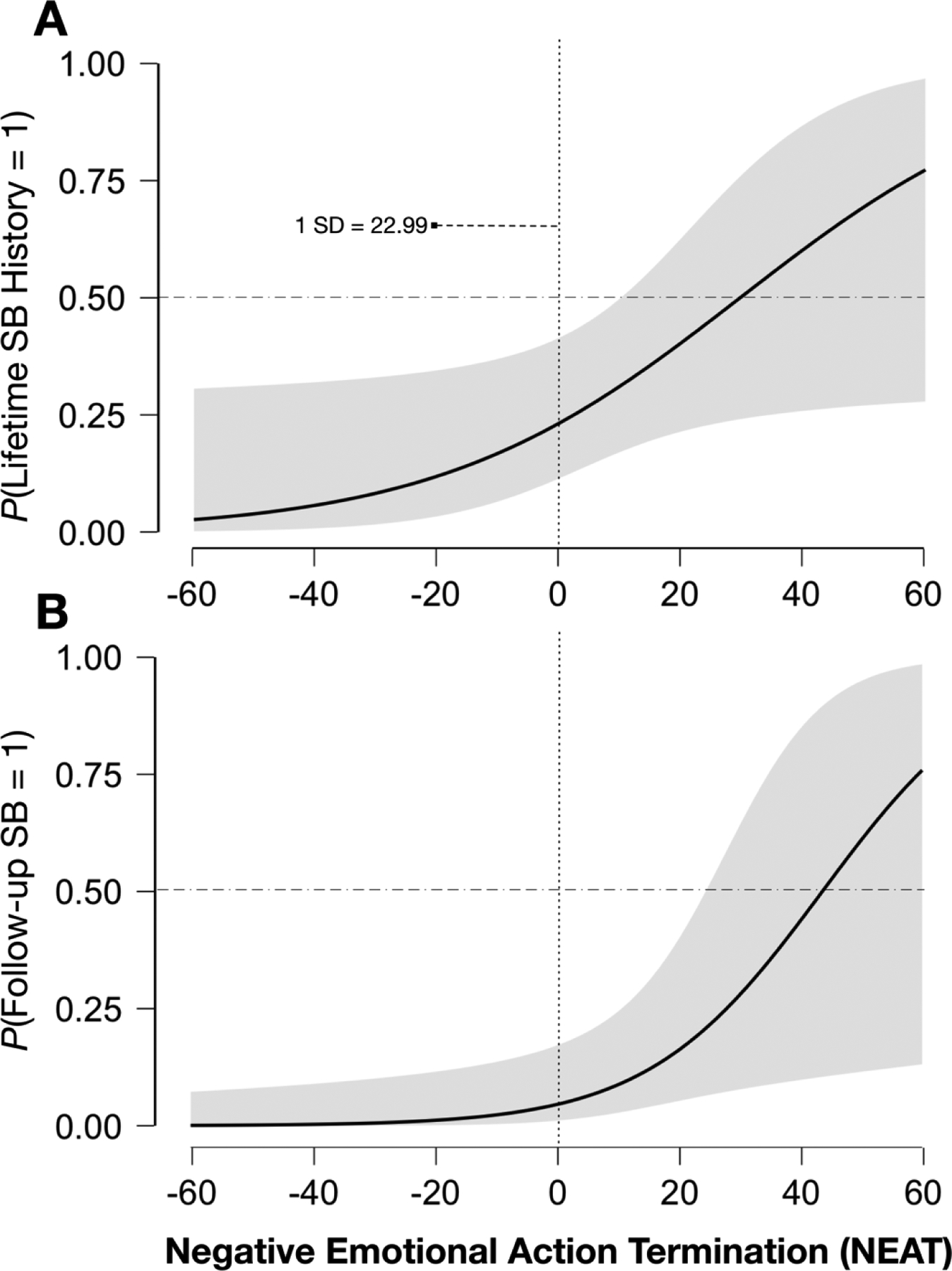
Note. Figure 1 depicts the probability (on an odds-ratio scale) of endorsing suicidal behaviors (SBs; 0 = negative, 1 = positive) at baseline (A) and follow-up (B), with mean-centered NEAT estimates controlling for relevant covariates (see Table 3). Higher NEAT values reflect worse negative emotional response inhibition, e.g., a positive value of “20” reflects negative emotional response inhibition performance approximately one standard deviation below average; shaded area represents 95% confidence intervals.
Follow-up SB Prediction
Eighty-seven participants who completed both the CTQ and ESST at baseline returned for at least one subsequent follow-up assessment session. Most of these participants reported no SBs in the interim (n = 78; 82.98%), whereas six of the 13 participants who made attempts reported multiple SBs. Prior to performing regressions to evaluate prospective effects of emotional response inhibition on post-discharge SBs, we conducted analyses comparing participants who did (n = 87) and did not (n = 44) return for follow-up assessments (who also completed the CTQ at baseline and the ESST at both assessments). A series of multivariate ANOVAs confirmed these groups’ statistical equivalence on: (1) Demographic characteristics (age, years of education) and CTQ scores, F(3, 124) = 0.20, p = 0.895; (2) Lifetime SBs and SI frequency/severity, F(3, 127) = 0.65, p = 0.584; and (3) baseline ESST performance metrics of accuracy, error rates, reaction time, and emotional response inhibition (e.g., PEAT/NEAT), F(9, 121) = 1.63, p = 0.113. Study completers and non-completers were similarly equivalent in terms of sex, X2 (2, N = 131) = 1.58, p = 0.453, Cramer’s V = 0.11; sexual orientation, X2 (1, N = 131) = 0.001, p = 0.971, Cramer’s V = 0.003; race, X2 (4, N = 130) = 5.85, p = 0.211, Cramer’s V = 0.21; ethnicity, X2 (1, N = 130) = 0.06, p = 0.809, Cramer’s V = 0.02; and marital status, X2 (3, N = 131) = 2.31, p = 0.510, Cramer’s V = 0.11. However, participants who returned for follow-up assessments reported lower income, X2 (4, N = 123) = 1.58, p = 0.453, Cramer’s V = 0.11. Additionally, non-heterosexual participants were more likely to report SBs after index hospitalization, t(87) = −2.32, p = 0.023, Cohen’s d = −0.57. We accordingly included income and sexual orientation as covariates in regression Model 4b (see supplementary materials) to bolster Model 2’s prospective statistical power, given that their inclusion did not affect our primary results (i.e., hypothesized effect of NEAT) and resulted in loss of participants with missing data.
Hierarchical logistic regression results were consistent with cross-sectional findings, revealing a main effect NEAT but not CTQ score in the prediction of SBs, after controlling for education and baseline SI/SB history. Indeed, NEAT was the only significant predictor in the full model, which accurately classified 86% of patients’ post-discharge SB status. Results suggested that participants whose baseline inhibitory control over negative emotional reactions to aversive images on the ESST (i.e., NEAT) was relatively poor (i.e., one standard deviation below average) were nearly four times more likely to report subsequent suicidal acts compared to those with superior NEAT (i.e., scores one standard deviation above average; see Figure 1B). Given that the observed CTQ-SB correlation was not evident in regression models after controlling for suicidal thoughts (possibly due to low statistical power), we did not pursue follow-up mediation analyses as planned. Comparable with cross-sectional results (Model 1), estimated SB risk was unrelated to positive emotional response inhibition (PEAT) in longitudinal regression (Model 2).
Discussion
Childhood maltreatment is a well-established risk factor for suicide (Angelakis et al., 2019) that detrimentally impacts neurocognitive development (Teicher et al., 2016). Few studies have explored potential patterns of cognitive deficits underlying this link. We addressed this gap in the literature by examining blunted inhibition of motor responses to negative affective stimuli (specifically those reflecting negative emotional reactions, i.e., NEAT) as a possible explanatory factor for SBs in hospitalized psychiatric inpatients. Unexpectedly, we found that ESST performance explained unique variance in SBs apart from childhood maltreatment in cross-sectional and longitudinal models, suggesting that NEAT indexes a suicide risk process independent of early trauma. Observed effects were fairly robust and specific to negative stimuli and responses, persisting even after controlling for SI, general task performance indices, negativity bias (i.e., NRB), and positive valence conditions (i.e., PEAT). Results suggest that difficulty controlling negative reactions to aversive stimuli – or NEAT impairment specifically, rather than broader inhibitory deficits to emotional stimuli – may be most relevant to suicide risk. Our findings have important implications for elucidating the nature of relationships between maltreatment history and SBs among high-risk patients. These results further provide preliminary support for NEAT as a behavioral marker of suicide risk, which putatively reflects neurocognitive deficits in affective control manifesting as emotion dysregulation and related traits (Allen et al., 2019; Allen & Hooley, 2019).
Our central aim was to evaluate whether NEAT helps account for associations between childhood maltreatment and SBs. As predicted, maltreatment and NEAT were independently related to previous SBs. However, the association between maltreatment and SB history was non-significant after controlling for relevant covariates. This finding contrasts with recent research indicating that trauma exposure differentiates individuals with suicide attempt history from those endorsing only SI (Burke et al., 2020). However, our ability to detect hypothesized maltreatment-suicide relationships may have been limited by a modestly-sized sample (comprising entirely high-risk psychiatric inpatients) endorsing a restricted range of SI. Alternatively, maltreatment may contribute to suicide via ideation rather than conferring specific risk for attempts (c.f., Klonsky & May, 2015) or by increasing the likelihood of psychopathology more broadly, thereby enhancing the likelihood of multi-final clinical outcomes like suicide (see Allen et al., 2019). Nevertheless, replication in diverse samples with more variation in suicidal thoughts and behaviors is needed to determine generalizability.
Our secondary aim was to examine NEAT as a predictor of future suicide risk. We again observed no maltreatment-suicide link in longitudinal regression predicting post-discharge SBs, with non-significant effects of childhood maltreatment comparable in magnitude to cross-sectional Model 1. Results indicated that, in contrast, ESST performance reflecting the top quartile of NEAT impairment (i.e., 75th percentile) increased future SB risk by more than 2.25 times (relative to the lowest quartile). These unexpected findings suggest that NEAT captures aspects of suicide risk largely unrelated to early adversity. Since inhibitory control is, to some extent, genetically linked (e.g., Friedman et al., 2008), NEAT may be a candidate marker of patients’ propensity to transition from ideation-to-action (Klonsky & May, 2015). Lending support to this interpretation, NEAT more robustly predicted post-discharge SBs than childhood maltreatment – an established suicide vulnerability factor – even after controlling for known demographic correlates, baseline SB history, and recent ideation.
Critically, we observed a pattern of findings specific to NEAT, beyond general impulsive responsivity to emotional stimuli. NEAT also prospectively predicted SBs after accounting for other behavioral indices of impulsivity (i.e., overall response inhibition, positive emotional response inhibition, omission errors), emotional interpretations (e.g., accuracy in identifying the valence of stimuli), and negativity bias (i.e., NRB). Although salient stimuli may interfere with response inhibition regardless of valence, findings suggest that difficulties inhibiting ongoing motor reactions to negative affective stimuli might especially typify suicide vulnerability among psychiatric inpatients.
Results implicate heightened reactivity and/or diminished cognitive control as potential characteristics of individuals with elevated suicide risk, particularly in response to aversive emotional content. The precise neurocognitive mechanisms for these proposed deficits remain unknown, however. Research identifying the temporospatial features of cognitive processes and associated neural substrates underlying negative emotional response inhibition is therefore warranted. We consider NEAT to represent the behavioral outcome of a complex sequence of mental operations that may be differentially impacted in childhood maltreatment and suicide, e.g., early-stage attentional capture, interference control, and stimulus evaluation; intermediate stages of inhibitory cue detection and action selection; and most proximally to behavior, cognitive control processes responsible for motor response inhibition itself (i.e., action suppression and termination). This study highlights the importance of exploring distinct contexts under which emotion processing deficits might contribute to SBs, underscoring the importance of examining multivalent task conditions to fully elucidate patterns of neurocognitive risk for suicide.
An alternative interpretation of our findings emphasizes resilience rather than risk. Specifically, the conditional probability of endorsing post-discharge SBs suggests that NEAT indexes the likelihood of not endorsing suicidal acts more accurately than detecting individuals at greatest risk. In other words, longitudinal regression Model 2 identified the vast majority (93.1%) of negative SB cases while correctly classifying 86.3% of SB cases overall, indicating that lower baseline NEAT values (reflecting better negative emotional response inhibition) are fairly specific in predicting SB absence six months later, whereas higher values may be insufficiently sensitive to detect SB vulnerability following hospital discharge. Follow-up SB risk was unequivocally reduced in patients with above-average negative emotional response inhibition (i.e., low NEAT scores), whereas we obtained wide confidence intervals at higher NEAT values, indicating that Model 2 poorly characterized suicide risk among those with deficient negative emotional response inhibition. Stronger negative emotional response inhibition – especially when faced with unpleasant, provocative stimuli – might thus be appropriately conceptualized as a protective factor against suicide. This interpretation is consistent with the observed correlation between childhood adversity and NEAT: Exposure to early maltreatment likely confers SB susceptibility and might separately impact affect regulation via NEAT dysfunction, yet individuals with superior negative emotional response inhibition may be less likely to engage in suicidal acts regardless of maltreatment history. Recent research reporting reduced depression risk among maltreated children who demonstrate enhanced recruitment of frontoparietal circuits to downregulate limbic reactivity (Rodman et al., 2020) provides additional support for this possibility. More work is necessary to conclude whether better NEAT promotes resilience in the presence of established vulnerability factors.
With respect to clinical implications, present findings suggest that NEAT can help differentiate psychiatric patients at greatest risk for future SBs from those who may be more resilient to suicidal urges post-discharge. As such, treatment approaches in short-term hospital settings focused on helping patients develop mindfulness strategies to promote earlier recognition of suicidal urges (often accompanying negative affect) might promote this post-discharge resiliency; for example, by enabling patients to employ distress tolerance skills to “ride out” these urges. Nevertheless, future research is needed to replicate these findings and explicate precisely how NEAT contributes to suicide risk will help determine the potential utility of such approaches.
This study has several limitations. First, the restricted range of suicidal thoughts and behaviors in this high-risk sample may have limited our ability to detect variance in attempts shared by NEAT and maltreatment. However, this limitation underscores the need for improved predictive models among established psychiatric patients with elevated suicide risk, e.g., those endorsing previous attempts and/or SI severe enough to necessitate hospitalization. Second, while our results suggest NEAT performance predicts subsequent suicide risk, we are unable to make causal inferences regarding NEAT’s role in suicide risk without experimental evidence. Although we conceptualize NEAT as a behavioral indicator of “dispositional” vulnerability, more work is required to determine its stability over time, and critically, its plasticity in response to intervention. Third, participant attrition was considerable, likely due to the nature of our high-risk inpatient sample (e.g., unstable housing and employment) and follow-up length (i.e., time elapsed since hospital discharge). Modest retention rates may have introduced a self-selection bias potentially influencing these findings; however, the results of attrition analyses somewhat mitigate this concern and participant retention was consistent with the extant literature in this population (e.g., Cha et al., 2010; Handley et al., 2016; Miller et al., 2017; Yaseen et al., 2014). Fourth, diminished sample size at follow-up limited statistical power to test for the presence of a mediating effect. Nevertheless, additional research with a larger longitudinal sample is needed to confirm replicability of our findings. Finally, our sample predominantly included White participants; additional studies are necessary to ascertain the degree to which findings generalize to diverse populations.
This research also involves key strengths. We examined an objective behavioral marker of affective/neurocognitive processes theorized to mediate the trauma-suicide link in a unique, high-risk sample of hospitalized psychiatric patients. We also rigorously assessed the specificity of NEAT’s association with SBs by examining alternative emotional conditions across valence and condition. Moreover, we validated results cross-sectionally and longitudinally, demonstrating NEAT’s predictive utility in modeling suicide risk in the six months following psychiatric hospital discharge.
Conclusion
These findings advance our understanding of complex relations among child maltreatment, emotion dysregulation, and suicide. Results suggest that negative emotional response inhibition deficits do not capture suicide risk induced by childhood maltreatment among psychiatric inpatients. We instead found evidence for an independent contribution of NEAT in classifying SB history and predicting post-discharge SBs, supporting its candidacy as a behavioral marker of altered neurocognition involved in emotion dysregulation and suicide; however, more targeted research is needed to identify its neurobiological underpinnings. This study also suggests that NEAT may be protective in mitigating suicide risk associated with early adversity. Replication and extension of these results in larger, more diverse samples is warranted. Future work consistent with present findings would encourage further exploration of NEAT’s clinical utility, given considerable implications of identifying objective behavioral markers to inform risk assessment and screening – perhaps even serving as novel intervention targets – among severely suicidal patients.
Supplementary Material
Highlights.
Maltreatment may confer suicide risk via poor emotional response inhibition (ERI).
We evaluated hospitalized psychiatric inpatients’ suicidal behaviors (SBs).
SB history was linked specifically to negative ERI impairment.
Worse negative ERI correlated with maltreatment and predicted SBs six months later.
Deficient negative ERI may comprise a novel behavioral marker of suicide risk.
Acknowledgements:
The authors wish to thank the participants in this study and their treatment teams on the Butler Hospital inpatient service. We also thank research assistants Alyson Randall, Jessica Sandler, Catarina Carosa, Timothy Mayer, William Kelner, and David Schillinger (Butler Hospital) for their roles in data collection, as well as Olivia Goldstein and Marlee Neugass (Oberlin College) for their aid in preparing this manuscript.
Financial support:
This work was supported by funding from the National Institute of Mental Health (K.J.D.A., R01MH108610; M.F.A., R01MH108610, R01MH112674; N.R.N., R01MH05379, R01MH108641, R01MH11682, R01MH10379; H.T.S., R01MH108610), the National Institute of Nursing Research (M.F.A. & H.T.S., R01NR014540), Veterans Affairs Health Services Research and Development (M.L.B, I01 HX002572), and the National Institute of General Medical Sciences (M.F.A. & H.T.S., U54GM115677).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest:
None.
Ethical standards:
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Ambiguous: 2102, 2215, 2280, 2305, 2385, 2396, 2411, 2440, 2480, 2516, 2840, 8312; negative: 2053, 2205, 2456, 2800, 2900, 3350, 6370, 6821, 9040, 9417, 9800, 9810; positive: 1340, 2045, 2075, 2091, 2209, 2550, 4614, 5470, 5831, 8190, 8200, 8470.
A total of n = 13 participants with outlier ESST data (e.g., above three standard deviations from mean values) were identified during data cleaning procedures. We conducted a sensitivity analysis by running regression models with and without these participants, which produced overall results that were comparable in terms of effect sizes of interest and consistent with our interpretations of the models presented here. We thus elected to report models including all subjects with complete data to increase statistical power of analyses and maximize generalizability of our results. Please see supplementary materials for analytic results after omitting participants with outlier ESST data.
References
- Aldao A, Gee DG, De Los Reyes A, & Seager I (2016). Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: Current and future directions. Developmental Psychopathology, 28(4pt1), 927–946. 10.1017/S0954579416000638 [DOI] [PubMed] [Google Scholar]
- Allen KJD, Bozzay ML, & Edenbaum ER (2019). Neurocognition and suicide risk in adults. Current Behavioral Neuroscience Reports, 6(4), 151–165. 10.1007/s40473-019-00189-y [DOI] [Google Scholar]
- Allen KJD, & Hooley JM (2015). Inhibitory control in people who self-injure: Evidence for impairment and enhancement. Psychiatry Research, 225(3), 631–637. 10.1016/j.psychres.2014.11.033 [DOI] [PubMed] [Google Scholar]
- Allen KJD, & Hooley JM (2019). Negative Emotional Action Termination (NEAT): Support for a cognitive mechanism underlying negative urgency in nonsuicidal self-injury. Behavior Therapy, 50(5), 924–937. 10.1016/j.beth.2019.02.001 [DOI] [PubMed] [Google Scholar]
- Allen KJD, Sammon MM, Fox KR, & Stewart JG (2020). Emotional response inhibition: A shared neurocognitive deficit in eating disorder symptoms and nonsuicidal self-injury. Brain Sciences, 10(2), 104. 10.3390/brainsci10020104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelakis I, Gillespie EL, & Panagioti M (2019). Childhood maltreatment and adult suicidality: A comprehensive systematic review with meta-analysis. Psychological Medicine, 49(7), 1057–1078. 10.1017/S0033291718003823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armey MF, Brick LAD, Schatten HT, Nugent NR, & Miller IW (2018). Ecologically assessed affect and suicidal ideation following psychiatric inpatient hospitalization. General Hospital Psychiatry, 63(2020), 89–96. 10.1016/j.genhosppsych.2018.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachmann S (2018). Epidemiology of suicide and the psychiatric perspective. International Journal of Environmental Research and Public Health, 15(7), 1425. 10.3390/ijerph15071425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, & Haines N (2019). Functionalist and constructionist perspectives on emotion dysregulation. In Beauchaine TP & Crowell SE (Eds.), The Oxford Handbook of Emotion Dysregulation. Oxford University Press. 10.1093/oxfordhb/9780190689285.013.1 [DOI] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, & Handelsman L (1997). Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child and Adolescent Psychiatry, 36(3), 340–348. 10.1097/00004583-199703000-00012 [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Zule W (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Berzenski SR (2018). Distinct emotion regulation skills explain psychopathology and problems in social relationships following childhood emotional abuse and neglect. Developmental Psychopathology, 31(02), 483–496. 10.1017/S0954579418000020 [DOI] [PubMed] [Google Scholar]
- Brown J, Cohen P, Johnson JG, & Smailes EM (1999). Childhood abuse and neglect: Specificity of effects on adolescent and young adult depression and suicidality. Journal of the American Academy of Child and Adolescent Psychiatry, 38(12), 1490–1496. 10.1097/00004583-199912000-00009 [DOI] [PubMed] [Google Scholar]
- Burke TA, Allen KJD, Carpenter RW, Siegel DM, Kautz MM, Liu RT, & Alloy LB (2021). Emotional response inhibition to self-harm stimuli interacts with momentary negative affect to predict nonsuicidal self-injury urges. Behaviour Research and Therapy. 10.1016/j.brat.2021.103865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cha CB, Najmi S Park JM, Finn CT, & Nock MK (2010). Attentional bias toward suicide-related stimuli predicts suicidal behavior. Journal of Abnormal Psychology, 119(3), 616. 10.1037/a0019710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capistrano CG, Bianco H, & Kim P (2016). Poverty and internalizing symptoms: The indirect effect of middle childhood poverty on internalizing symptoms via an emotional response inhibition pathway. Frontiers in Psychology, 7. 10.3389/fpsyg.2016.01242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & Johnson SL (2018). Impulsive reactivity to emotion and vulnerability to psychopathology. American Psychologist, 73(9), 1067–1078. 10.1037/amp0000387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, & Timpano KR (2017). Toward a functional view of the P Factor in psychopathology. Clinical Psychological Science, 5(5), 880–889. 10.1177/2167702617710037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chester DS, Lynam DR, Milich R, Powell DK, Andersen AH, & DeWall CN (2016). How do negative emotions impair self-control? A neural model of negative urgency. NeuroImage, 132, 43–50. 10.1016/j.neuroimage.2016.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1986). Statistical approaches to suicidal risk factor analysis. Annals of the New York Academy of Sciences, 487, 34–41. 10.1111/j.1749-6632.1986.tb27883.x [DOI] [PubMed] [Google Scholar]
- Comte M, Schön D, Coull JT, Reynaud E, Khalfa S, Belzeaux R, … Fakra E (2014). Dissociating bottom-up and top-down mechanisms in the cortico-limbic system during emotion processing. Cerebral Cortex, 26(1), 144–155. 10.1093/cercor/bhu185 [DOI] [PubMed] [Google Scholar]
- Crosby AE, Han B, Ortega LAG, Parks SE, & Gfroerer J (2011). Suicidal thoughts and behaviors among adults aged >18 Years – United States, 2008–2009. MMWR Surveillance Summaries, 60(13), 1–11. [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, … Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Friedman NP, Miyake A, Young SE, DeFries JC, Corley RP, & Hewitt JK (2008). Individual differences in executive functions are almost entirely genetic in origin. Journal of Experimental Psychology - General, 137(2), 201–225. 10.1037/0096-3445.137.2.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, & Janson S (2009). Burden and consequences of child maltreatment in high-income countries. The Lancet, 373(9657), 68–81. 10.1016/S0140-6736(08)61706-7 [DOI] [PubMed] [Google Scholar]
- Gollan JK, Hoxha D, Hunnicutt-Ferguson K, Norris CJ, Rosebrock L, Sankin L, & Cacioppo J (2016). Twice the negativity bias and half the positivity offset: Evaluative responses to emotional information in depression. Journal of Behavior Therapy and Experimental Psychiatry, 52, 166–170. 10.1016/j.jbtep.2015.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar M, & Quevedo K (2007). The neurobiology of stress and development. Annual Review of Psychology, 58(1), 145–173. 10.1146/annurev.psych.58.110405.085605 [DOI] [PubMed] [Google Scholar]
- Hadland SE, Wood E, Dong H, Marshall BDL, Kerr T, Montaner JS, & DeBeck K (2015). Suicide attempts and childhood maltreatment among street youth: A prospective cohort study. Pediatrics, 136(3), 440–449. 10.1542/peds.2015-1108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handley TE, Kay-Lambkin FJ, Baker AL, Lewin TJ, Kelly BJ, Inder KJ, … Kavanagh DJ (2016). Investigation of a suicide ideation risk profile in people with co-occurring depression and substance use disorder. The Journal of Nervous and Mental Disease, 204(11), 820–826. 10.1097/NMD.00000000000000473 [DOI] [PubMed] [Google Scholar]
- Heleniak C, Jenness JL, Vander Stoep A, McCauley E, & McLaughlin KA (2015). Childhood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognitive Therapy and Research, 40(3), 394–415. 10.1007/s10608-015-9735-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson AJ, & Tottenham N (2015). Regulatory skill as a resilience factor for adults with a history of foster care: A pilot study. Developmental Psychobiology, 57(1), 1–16. 10.1002/dev.21227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jollant F, Lawrence NL, Olié E, Guillaume S, & Courtet P (2011). The suicidal mind and brain: A review of neuropsychological and neuroimaging studies. The World Journal of Biological Psychiatry, 12(5), 319–339. 10.3109/15622975.2011.556200 [DOI] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010.) Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, 51(6), 706–716. 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, & May AM (2015). The Three-Step Theory (3ST): A new theory of suicide rooted in the “Ideation-to-Action” framework. International Journal of Cognitive Therapy, 8(2), 114–129. 10.1521/ijct.2015.8.2.114 [DOI] [Google Scholar]
- Lang PJ, Bradley MM, & Cuthbert BN (2008). International Affective Picture System (IAPS): Affective ratings of pictures and instruction manual. Technical Report A-8. University of Florida. [Google Scholar]
- Loman MM, Johnson AE, Westerlund A, Pollak SD, Nelson CA, & Gunnar MR (2013). The effect of early deprivation on executive attention in middle childhood: Early deprivation and executive attention. Journal of Child Psychology and Psychiatry, 54(1), 37–45. 10.1111/j.1469-7610.2012.02602.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan A, & Cicchetti D (2002). Impact of child maltreatment and interadult violence on children’s emotion regulation abilities and socioemotional adjustment. Child Development, 73(5), 1525–1542. 10.1111/1467-8624.00488 [DOI] [PubMed] [Google Scholar]
- McCrory EJ, & Viding E (2015). The theory of latent vulnerability: Reconceptualizing the link between childhood maltreatment and psychiatric disorder. Developmental Psychopathology, 27(2), 493–505. 10.1017/S0954579415000115 [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, & Lambert HK (2017). Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Current Opinion in Psychology, 14, 29–34. 10.1016/j.copsyc.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller IW, Camargo CA, Arias SA, Sullivan AF, Allen MH, Goldstein AB, … & ED-SAFE Investigators. (2017). Suicide prevention in an emergency department population: the ED-SAFE study. JAMA Psychiatry, 74(6), 563–570. 10.1001/jamapsychiatry.2017.0678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy FC, Sahakian BJ, Rubinsztein JS, Michael A, Rogers RD, Robbins TW, & Paykel ES (1999). Emotional bias and inhibitory control processes in mania and depression. Psychological Medicine, 29(6), 1307–1321. 10.1017/s0033291799001233 [DOI] [PubMed] [Google Scholar]
- Pollak SD, Nelson CA, Schlaak MF, Roeber BJ, Wewerka SS, Wiik KL, … Gunnar MR (2010). Neurodevelopmental effects of early deprivation in postinstitutionalized children. Child Development, 81(1), 224–236. 10.1111/j.1467-8624.2009.01391.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, … Mann J (2008). Columbia-Suicide Severity Rating Scale (C-SSRS). Columbia University Medical Center. [Google Scholar]
- Rodman AM, Jenness JL, Weissman DG, Pine DS, & McLaughlin KA (2020). Neurobiological markers of resilience to depression following childhood maltreatment: The role of neural circuits supporting cognitive control of emotion. Biological Psychiatry, 86(6), 464–473. 10.1016/j.biopsych.2019.04.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochat L, Billieux J, Gagnon J, & Van der Linden M (2018). A multifactorial and integrative approach to impulsivity in neuropsychology: Insights from the UPPS model of impulsivity. Journal of Clinical and Experimental Neuropsychology, 40(1), 45–61. 10.1080/13803395.2017.1313393 [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Dackis MN, & Cicchetti D (2011). Child maltreatment and allostatic load: Consequences for physical and mental health in children from low-income families. Developmental Psychopathology, 23(4), 1107–1124. 10.1017/S0954579411000587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz K, Fan J, Magidina O, Marks D, Hahn B, & Halperin J, 2007. Does the emotional go/no-go task really measure behavioral inhibition? Convergence with measures on a non-emotional analog. Archives of Clinical Neuropsychology, 22(2), 151–160. 10.1016/j.acn.2006.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz KP, Clerkin SM, Halperin JM, Newcorn JH, Tang CY, & Fan J (2009). Dissociable neural effects of stimulus valence and preceding context during the inhibition of responses to emotional faces. Human Brain Mapping, 30(9), 2821–2833. 10.1002/hbm.20706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Samson JA, Anderson CM, & Ohashi K (2016). The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews: Neuroscience, 17(10), 652–666. 10.1038/nrn.2016.111 [DOI] [PubMed] [Google Scholar]
- Tottenham N, Hare TA, Quinn BT, Mccarry TW, Nurse M, Gilhooly T, … Casey B (2010). Prolonged institutional rearing is associated with atypically large amygdala volume and difficulties in emotion regulation. Developmental Science, 13(1), 46–61. 10.1111/j.1467-7687.2009.00852.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turecki G, Ernst C, Jollant F, Labonté B, & Mechawar N (2012). The neurodevelopmental origins of suicidal behavior. Trends in Neuroscience, 35(1), 14–23. 10.1016/j.tins.2011.11.008 [DOI] [PubMed] [Google Scholar]
- Van Heeringen K, Bijttebier S, Desmyter S, Vervaet M, & Baeken C (2014). Is there a neuroanatomical basis of the vulnerability to suicidal behavior? A coordinate-based meta-analysis of structural and functional MRI studies. Frontiers in Human Neuroscience, 8. 10.3389/fnhum.2014.00824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaseen ZS, Kopeykina I, Gutkovich Z, Bassirnia A, Cohen LJ, &. Galynker II (2014). Predictive validity of the Suicide Trigger Scale (STS-3) for post-discharge suicide attempt in high-risk psychiatric inpatients. PLoS One, 9(1), e86768. 10.1371/journal.pone.0086768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman DG, Bitran D, Miller AB, Schaefer JD, Sheridan MA, & McLaughlin KA (2019). Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Developmental Psychopathology, 31(3), 899–915. 10.1017/S0954579419000348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildeman C, Emanuel N, Leventhal JM, Putnam-Hornstein E, Waldfogel J, & Lee H (2014). The prevalence of confirmed maltreatment among US children, 2004 to 2011. JAMA Pediatrics, 168(8), 706–713. 10.1001/jamapediatrics.2014.410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (n.d.). Suicide data. http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/ (accessed August 27, 2020).
- Zatti C, Rosa V, Barros A, Valdivia L, Calegaro VC, Freitas LH, … Schuch FB (2017). Childhood trauma and suicide attempt: A meta-analysis of longitudinal studies from the last decade. Psychiatry Research, 256, 353–358. 10.1016/j.psychres.2017.06.082 [DOI] [PubMed] [Google Scholar]
- Zhang H, Chen Z, Jia Z, & Gong Q (2014). Dysfunction of neural circuitry in depressive patients with suicidal behaviors: A review of structural and functional neuroimaging studies. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 53, 61–66. 10.1016/j.pnpbp.2014.03.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


