Abstract
Introduction
Lophomoniasis is caused by Lophomonas spp., a new emerging protozoan, which commonly affects the human lower respiratory tract. The Lophomonas parasite mostly lives commensally in the hindgut of cockroaches.
Case Presentation
We present the case of a 33-year-old woman, 30 weeks pregnant, who had severe COVID-19. She was intubated upon admission and began the routine COVID-19 treatment. To rule out possible super infection dual with COVID-19, microscopic examination of the patient's mini-bronchoalveolar lavage (mini-BAL) specimen, revealed L. blattarum, which was identified by the SSU rRNA-PCR and sequencing approaches (accession number: MZ093069). According to that, the patient was treated successfully with metronidazole.
Conclusion
To prevent serious complications, lophomoniasis should be listed in co-morbidity cases of COVID-19 infection during the COVID-19 pandemic worldwide. To the best of our knowledge, this is the first co-infection of Lophomonas blattarum and COVID-19 in the world which has been confirmed using a molecular approach.
Keywords: Lophomonas blattarum, COVID-19, Co-morbidity, PCR, Iran
Introduction
SARS-CoV-2 infection causes COVID-19, a disease with a wide range of clinical symptoms. While the majority of patients with COVID-19 experience only asymptomatic or moderate disease, at-risk patients can develop serious diseases that necessitate hospitalization and respiratory support. Older age, as well as underlying comorbidities like hypertension, cardiovascular disease, and diabetes, has been identified as risk factors for disabling conditions [1]. There is currently little known about SARS-CoV-2 infections in pregnancy. It is linked to an increased risk of preterm birth in pregnant women and, in some countries, a higher risk of maternal death [2]. Pregnancy may complicate the already complex management of infection with an emerging pathogen in the subset of pregnant women who develop severe or critical disease [3]. Lophomonas is a neglected and emerging protozoan which infects human lower (mostly) and upper respiratory tracts. It mostly lives as a commensal agent in the hindgut of cockroaches [4, 5]. For the last decades, lower and upper respiratory infections due to Lophomonas have been reported in some areas of the world, particularly in China and Iran. Iran has been known for the highest number of lophomoniasis cases reported in the world [6–11]. Moreover, Lophomonas blattarum (L. blattarum) has recently been isolated from the cockroaches in Mazandaran province, northern Iran [5].
To date, co-infections of lophomoniasis with other infectious diseases have been reported rarely all over the world. There is some evidence regarding co-morbidity of lophomoniasis with HIV and tuberculosis [4, 9, 12]. According to our knowledge, there have been no reports of lophomoniasis/COVID-19 co-infection. In this case study, we describe the diagnosis and treatment of a woman who was infected with Lophomonas and COVID-19 at the same time.
Case Presentation
A 33-year-old pregnant woman, at 30 weeks’ gestation, was admitted to the emergency unit on December 6, 2020. She suffered from hypertension, low back pain (LBP) with leg pain, fever, cough, shortness of breath and bilateral conjunctivitis. The patient had anemia (HG = 10.3), leukocytosis (20.4), neutrophilia (90.5%) and lymphopenia (6.1%) in the initial studies, with elevated ESR (100), CRP (53.7), and LDH (939), but all other parameters were normal.
Her chest was imaged using high-resolution computed tomography (HRCT) and revealed bilateral moultilobar patchy ground glass opacities, alveolar consolidations, and mild to moderate pleural effusion.
Due to the pandemic of COVID-19 and the patient’s suspicion of this infection, a sample was taken from the patient’s throat and larynx. The patient’s real-time reverse transcriptase–polymerase chain reaction (RT-PCR) test was positive, and she was admitted to the intensive care unit (ICU). Gradually, the patient’s shortness of breath increased, and the patient underwent intubation. Because of the risk of fetal death, the patient underwent cesarean section. The newborn was delivered from her mother with good health and negative RT-PCR results for COVID-19. The patient was treated with enoxaparin sodium, ticlopidine, remdesivir, amikacin, colomycin, methylprednisolone pulse therapy, magnesium sulfate and N-Acetylcystein (NAC). After 20 days, the patient was extubated from the mechanical ventilator. However, due to the persistence of cough and tracheal secretions, mini-BAL procedure, as less invasive, safe and quick approach, was performed by a sterile suction catheter of size 12 French. About 20 mL of sodium chloride 0.9% were instilled through the catheter and aspirate was collected in a sterile polypropylene tube by suction. After that, the endotracheal secretions at ambient condition were transported to the Iranian National Registry Center for Lophomoniasis (INRCL) at Imam Khomeini hospital, Mazandaran University of Medical Sciences, Sari, Iran, to rule out the lophomoniasis.
Based on microscopic and specific PCR techniques which are described below, lophomoniasis was confirmed. Thus, metronidazole 500 mg three times daily for two weeks was added to COVID-19 treatment to treat Lophomonas infection. The patient was discharged from the hospital after 27 days with complete recovery. This study was reviewed and approved by the research ethics committee of Mazandaran University of Medical Sciences (IR.MAZUMS.REC. 1399.255).
Laboratory Approaches and Findings to Rule Out Lophomoniasis
Microscopic Examination
A mini-BAL specimen (about 20 mL) was centrifuged at 2000 × g for 5 min. Then, the sediment was observed under (× 40) magnification light microscope. Motile trophozoite of Lophomonas was detected in a direct wet-mount examination, which was confirmed by Giemsa staining technique (see Fig. 1).
Fig. 1.
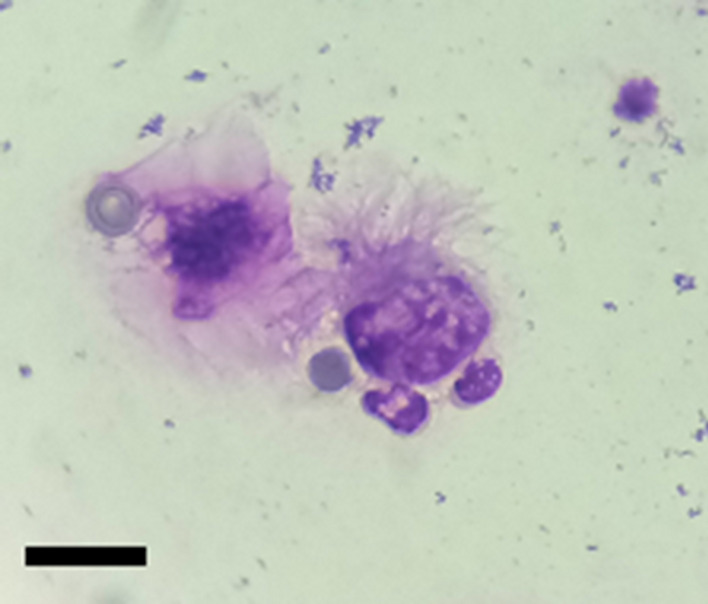
Giemsa stained smear showing a trophozoite of Lophomonas blattarum in mini-BAL specimen (× 1000). Bar = 10 μm
Molecular Identification
DNA Extraction
The sediment of the mini-BAL specimen was submitted to DNA extraction using the 200 μL of the specimen was homogenized in 200 μL of digestive buffer containing 50 mM Tris–HCl (pH 7.6), 1 mM EDTA and 1% Tween 20, to which 20 μL of the proteinase K solution (20 mg enzyme/mL) was added. The homogenized solution was then incubated overnight at 45 °C. The subsequent homogenate was then given 200 μL of phenol:chloroform:isoamyl alcohol (25:24:1) solution. The solution was centrifuged at 14,000 g for 15 min after being vigorously shaken. The supernatant was put into a new microtube, which was then filled with 400 mL of cold 100% ethanol and maintained at − 20 °C for 2 h. Following that, 200 μL of 70% ethanol were added to the sediment, centrifuged, and the precipitate was suspended in 50 μL of double-distilled water and kept at 4 °C until use.
SSU rRNA-PCR and Sequencing
Molecular detection of Lophomonas was performed by genus-specific small subunit ribosomal RNA (SSU rRNA) PCR. The initial pairs used were forward (F) 5′-GAG AAG GCG CCT GAG AGA T-3′ and reverse (R) 5′-ATG GGA GCA AAC TCG CAG A-3′ as described by Fakhar et al. [10], amplifying a region of 214 base pairs (bp) (Fakhar et al. 2019). The amplified operations used a total volume of 25 μL, which included 12.5 μL Master Mix (Fermentas, Inc.), 1 μL of each primer, 5 μL of extracted DNA, and 5.5 μL of distilled water. In a thermocycler (Corbett Research, Sydney, Australia), 35 cycles were done, with an initial denaturation at 94 °C for 2 min, followed by 40 cycles of 94 °C for 1 min, 57 °C for 1 min, and 94 °C for 1 min.
The PCR products were then electrophoresed on a 1.5 percent (w/v) agarose gel in Tris–borate-EDTA (TBE) buffer for 6 μL. After staining with SafeViewTM DNA Stains, a 214-bp band was identified using UV transillumination (Applied Biological Materials, Inc.). Then, to species identification, the PCR product was sequenced using Sanger sequencing technology and then edited with BioEdit software (v.7.2). Next, the sequence result of the isolate was deposited in the GenBank by BanKit (Accession Numbers: MZ093069). The identity of this isolate in comparison with others available L. blattarum that was reported from Iran (Accession Numbers: MZ093070-78 and MN: 243135.1), were 98.5% and 99–100%, respectively.
Discussion
According to a systematic study, the most frequent clinical symptoms of COVID-19 in pregnant women are fever and cough, with sore throat and diarrhea being less common. Elevated neutrophil ratios and reduced lymphocyte ratios are typical at laboratory demonstrations. The majority of births result in a cesarean operation, which is far higher than the WHO's prescription for vaginal delivery, which may be considered by a gynecologist to avoid maternal respiratory distress during pregnancy. It is one of the most common obstetrical complications and the leading cause of neonatal morbidity and mortality. They would have chronic long-term health problems if they survived [13, 14]. The cords of affected mothers should be removed as soon as possible, and their newborns should be isolated and tested as soon as possible [15].
Lophomonas is a neglected parasite reported from a few countries which still remains unknown to many medical scientists [16]. Lophomoniasis is endemic in several areas of Iran [5–11]. About the fact that this condition is commonly seen in patients with immunodeficiency in other countries [17], it is often reported in patients with immunocompetent in Iran [6–11]. Lophomoniasis symptoms such as cough, fever and dyspnea are common in other respiratory infections. As a result, diagnosing and treating this infection is challenging [18]. Metronidazole is considered as the first-line therapeutic choice for lophomoniasis treatment [18]. Recent studies have revealed that metronidazole reduces the levels of inflammatory factors such as IL8, IL6, IL1B, TNFα, IL12, and IFNγ, as well as the levels of CRP and neutrophil count, which were increased during COVID-19 infection. Additionally, metronidazole has the potential to increase the number of circulatory lymphocytes [19]. Prescribing this drug, in addition to eliminating the Lophomonas infection, may have accelerated the patient's response to treatment for COVID-19 infection.
In several reports, L. blattarum was considered an opportunistic infection in patients with kidney and liver allograft transplantation, under corticosteroid therapy, HIV infection, and tuberculosis [4]. SARS-CoV-2 infection impairs the immune system, making individuals more susceptible to other infections and reactivating latent infections [20]. According to a meta-analysis study, patients with chronic pulmonary disease who have underlying lung scratches are at risk of developing severe cases of COVID-19 [21]. Many problems which occur from co-infection in a pregnant woman with COVID-19, which may be due to complications of COVID-19 itself that are caused by another infection. All infections may intensify each other's complications, or drug reactions between medications used to treat certain infections [13].
Lophomonas parasite appears to be involved in the severity of COVID-19 disease and can be considered as a risk factor. Hence, managing and diagnosing co-infections is critical in clinical practice. Since lophomoniasis is prevalent in several areas of the world such as Iran [6–11], consequently, it should be listed in co-morbidity cases of COVID-19 infection through the COVID-19 pandemic worldwide.
Conclusion
To the best of our knowledge, for the first time, co-occurrence of COVID-19 and lophomoniasis is reported in this paper. Many febrile infections can look like COVID-19, and SARS-CoV-2 infection can help spread or reactivate infectious diseases. We must not overlook other infectious diseases with related clinical manifestations in the midst of the COVID-19 pandemic. We recommend that healthcare systems be vigilant to enable early identification of co‐infections such as Lophomonas with COVID‐19. All symptomatic COVID‐19 cases with similar symptoms should be investigated for other common infections in endemic regions, especially in pregnant women to avoid complications.
Acknowledgements
The authors would like to express their appreciation to all hospital nurses who worked tirelessly during the COVID-19 pandemic.
Funding
Financial support for this study was received from the INRCL at Mazandaran University of Medical Sciences, Sari, Iran (No: 7712).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mahdi Fakhar, Email: mahdif53@yahoo.com.
Ali Sharifpour, Email: asharifpour0209@yahoo.com.
References
- 1.Gebrecherkos T, Gessesse Z, KebedeY, Gebreegzabher A, Tassew G, Abdulkader M, Ebuy H, Desta A, Hailu A, Harris V (2021) Effect of co-infection with parasites on severity of COVID-19. medRxiv PPR277525. 10.1101/2021.02.02.21250995
- 2.Lorenz C, Azevedo TS, Chiaravalloti-Neto F. COVID-19 and dengue fever: a dangerous combination for the health system in Brazil. Travel Med Infect Dis. 2020;35:1–2. doi: 10.1016/j.tmaid.2020.101659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kucirka LM, Norton A, Sheffield JS. Severity of COVID-19 in pregnancy: a review of current evidence. Am J Reprod Immunol. 2020;84:e13332. doi: 10.1111/aji.13332. [DOI] [PubMed] [Google Scholar]
- 4.Li R, Gao ZC. Lophomonas blattarum infection or just the movement of ciliated epithelial cells? Chin Med J. 2016;129:739–742. doi: 10.4103/0366-6999.178025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Motevalli-Haghi SF, Shemshadian A, Nakhaei M, Faridnia R, Dehghan O, Shafaroudi MM, Kelarijani MN, Nikookar SH, Kalani H, Fakhar M. First report of Lophomonas spp. in German cockroaches (Blattella Germanica) trapped in hospitals, northern Iran. J Parasit Dis. 2021 doi: 10.1007/s12639-021-01381-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berenji F, Fata A, Vakili V, Sayedi SJ, Abdollahi B, Imanfar H, Nakhaei M, Parian M, Khorasani SR. Unexpected high rate of Lophomonas blattarum in resistant upper and lower respiratory infection. Health Sci. 2016;5:74–80. doi: 10.1003/0326-6039.108011. [DOI] [Google Scholar]
- 7.Mirzazadeh F, Berenji F, Amini M, Salehi M, Shamsian A, Fata A, Parian M, Nakhaei M, Ghofraniha L. Lophomonas blattarum in asthmatic patients and control group. J Res Med Dental Sci. 2017;5:1–5. doi: 10.24896/jrmds.2017551. [DOI] [Google Scholar]
- 8.Ghafarian N, Bakhtiari E, Berenji F, Nakhaei M, Nakhaei B, Jamali-Behnam F, Sayedi J. The study of Lophomonas blattarum infection in children with respiratory symptoms: a descriptive clinical study in north east of Iran. Int J Pediatr. 2018;6:7797–7802. doi: 10.22038/ijp.2018.29199.2555. [DOI] [Google Scholar]
- 9.Talebian M, Berenji F, Amini M, Sayedi SJ, Shamsian A, Afzalaghaee M, Fata A, Parian M, Nakhaei M. A study about clinical symptoms and laboratory signs of adult and pediatric patients with Lophomonas blattarum. J Res Med Dental Sci. 2018;6:312–317. doi: 10.24896/jrmds.20186151. [DOI] [Google Scholar]
- 10.Fakhar M, Nakhaei M, SharifpourA KH, Banimostafavi ES, Abedi S, Safanavaei S, Aliyali M. First molecular diagnosis of Lophomoniasis: the end of a controversial story. Acta Parasitol. 2019;64:390–393. doi: 10.2478/s11686-019-00084-2. [DOI] [PubMed] [Google Scholar]
- 11.Fakhar M, Nakhaei M, Sharifpour A, Safanavaei S, Abedi S, Tabaripour R, Aliyali M, Modanloo M, Saberi R, Kalani H, Banimostafav ES. Morphological and molecular identification of emerged Lophomonas blattarum infection in Mazandaran Province, northern Iran: first registry-based study. Acta Parasitol. 2021 doi: 10.1007/s11686-021-00422-3. [DOI] [PubMed] [Google Scholar]
- 12.VermaS VG, Singh DV, Mokta J, Negi RS, Jhobta A, Kanga A. Dual infection with pulmonary tuberculosis and Lophomonas blattarum in India. Int J Tuberc Lung Dis. 2015;19:368–369. doi: 10.5588/ijtld.14.0513. [DOI] [PubMed] [Google Scholar]
- 13.Abbas AM, Salah S, Fathy SK, Rashad A, AboBakr A, Yousof EA, Saeed A, Youssef EN, Shaltout AS, Ahmed OA. Role of co-infection in the immunopathology of COVID-19 in pregnancy. Arch Health Sci. 2020;4:1–6. doi: 10.31829/2641-7456/ahs2020-4(1)-117. [DOI] [Google Scholar]
- 14.Hassanipour S, Faradonbeh SB, Momeni K, Heidarifard Z, Khosousi M-J, Khosousi L, Ameri H, Arab-Zozani M. A systematic review and meta-analysis of pregnancy and COVID-19: signs and symptoms, laboratory tests, and perinatal outcomes. Int J Reprod Biomed. 2020;18:1005–1018. doi: 10.18502/ijrm.v18i12.8022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asadi L, Tabatabaei RS, Safinejad H, Mohammadi M. New corona virus (COVID-19) management in pregnancy and childbirth. Arch Clin Infect Dis. 2020;15:e102938. doi: 10.5812/archcid.102938. [DOI] [Google Scholar]
- 16.Keighobadi M, Nakhaei M, Sharifpour A, Khasseh AA, Safanavaei S, Tabaripour R, Aliyali M, Abedi S, Mehravaran H, Banimostafavi ES. A bibliometric analysis of global research on Lophomonas sp. in scopus (1933–2019) Infect Disord Drug Targets. 2020;21:230–237. doi: 10.2174/1871526520666200727153142. [DOI] [PubMed] [Google Scholar]
- 17.XueJ LYL, Yu X-M, Li D-K, Liu M-F, Qiu J-F, Xue J-J. Bronchopulmonary infection of Lophomonas blattarum: a case and literature review. Korean J Parasitol. 2014;52:521–525. doi: 10.3347/kjp.2014.52.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martinez-Girón R, van Woerden HC. Lophomonas blattarum and bronchopulmonary disease. J Med Microbiol. 2013;62:1641–1648. doi: 10.1099/jmm.0.059311-0. [DOI] [PubMed] [Google Scholar]
- 19.Gharebaghi R, Heidary F, Moradi M, Parvizi M. Metronidazole; a potential novel addition to the COVID-19 treatment regimen. Arch Acad Emerg Med. 2020;8:e40. doi: 10.1139/aaem.1.559332-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen X, Liao B, Cheng L, Peng X, Xu X, Li Y, Hu T, Li J, Zhou X, Ren B. The microbial coinfection in COVID-19. Appl Microbiol Biotechnol. 2020;104:7777–7785. doi: 10.1007/s00253-020-10814-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu H, Chen S, Liu M, Nie H, Lu H. Comorbid chronic diseases are strongly correlated with disease severity among COVID-19 patients: a systematic review and meta-analysis. Aging Dis. 2020;11:668–678. doi: 10.14336/AD.2020.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]


