Key Points
Question
What do the latest US data reveal about non–small cell lung cancer (NSCLC) epidemiology?
Findings
In this cross-sectional epidemiological analysis, NSCLC incidence decreased from 2010 to 2017 overall, but rose for patients with stage I disease. Prevalence of NSCLC has increased, and estimated 5-year survival was 26.4%; a high proportion of patients with stage IV disease aged 65 or older years were categorized as not treated.
Meaning
The increased incidence of stage I NSCLC at diagnosis likely reflects improved evaluation of incidental nodules; availability of more effective treatments may explain increased overall prevalence and increased 5-year survival, though patients aged 65 years or older with stage IV NSCLC may be undertreated.
This cross-sectional epidemiological analysis calculated the most recent epidemiological estimates of incidence, prevalence, and survival in patients with non–small cell lung cancer, and describes initial treatment overall and by stage in the US.
Abstract
Importance
Updated estimates of non–small cell lung cancer (NSCLC) in the US are needed.
Objective
To calculate the most recent epidemiologic estimates of NSCLC in the US.
Design, Setting, and Participants
This cross-sectional epidemiological analysis used the most recently released data from US cancer registries. The population-based US Cancer Statistics (USCS) database (2010-2017), comprised of the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries (NPCR) (collectively, SEER-NPCR) provided the NSCLC incidence estimate. The SEER-18 database provided data for incidence, prevalence, survival, and initial treatment by NSCLC stage. Adults aged 18 years or older diagnosed with NSCLC identified by International Classification of Diseases for Oncology, Third Edition, morphology codes were included.
Main Outcomes and Measures
Annual age-adjusted NSCLC incidence per 100 000 persons; annual prevalence per 100 000 persons; survival rate; initial treatment. Due to database release delays, incidence data were available through 2017, and other parameters through 2016. The analysis was conducted from June 2020 to July 2020.
Results
There were 1.28 million new NSCLC cases recorded during 2010 to 2017 in the US (SEER-NPCR: 53% male; 67% ≥ 65 years). From 2010 to 2017, NSCLC incidence per 100 000 decreased from 46.4 to 40.9 overall (age <65 years: 15.5 to 13.5; age ≥65 years: 259.9 to 230.0); the incidence of stage II, IIIA, and IIIB NSCLC was stable, and stage IV decreased slightly from 21.7 to 19.6, whereas stage I incidence increased from 10.8 to 13.2. From 2010 to 2016, NSCLC prevalence per 100 000 increased from 175.3 to 198.3 (nationwide projection of SEER-18); prevalence increased among younger patients (77.5 to 87.9) but decreased among older patients (825.1 to 812.4). Period survival analysis found that 26.4% of patients survived 5 years, which is higher than previously reported. The proportion of stage I NSCLC treated with radiation as single initial treatment rose markedly from 14.7% in 2010 to 25.7% in 2016. Patients with stage IV NSCLC aged 65 years or older were most likely to be untreated (38.3%).
Conclusions and Relevance
The findings of this cross-sectional epidemiological analysis suggest that the increased incidence of stage I NSCLC at diagnosis likely reflected improved evaluation of incidental nodules. A smaller proportion of patients aged 65 years or older with stage IV NSCLC were treated. Earlier detection and availability of effective treatments may underlie increased overall NSCLC prevalence, and higher than previously reported survival.
Introduction
Lung cancer is the leading cause of cancer-related deaths in men and women in the US and worldwide.1,2 Non–small cell lung cancer (NSCLC) represents approximately 84% of all lung cancers, whereas small-cell lung cancer (SCLC) represents approximately 13%.1 Historically, NSCLC has had a poor prognosis, particularly in later stages.3 However, treatment has changed markedly in the past decade with wider lung cancer screening, improved radiation techniques, and treatment advances.4,5 These changes have likely resulted in the reported decline in NSCLC mortality.6 Because treatment and prognosis differ by stage, updated epidemiological estimates by stage are of interest.
This cross-sectional epidemiological analysis calculated the most recent estimates of incidence, prevalence, and survival in patients with NSCLC, and describes initial treatment overall and by stage in the US.
Methods
Databases
The United States Cancer Statistics (USCS) database, and the Surveillance, Epidemiology, and End Results (SEER-18) database were used. Detailed descriptions are in eAppendix A in the Supplement. The analysis was conducted from June to July 2020.
Study Population
Our analysis was based on adults aged 18 years or older who were diagnosed with NSCLC starting in 2010 (the first year in which data were categorized by stage [SEER-18]). NSCLC was identified by International Classification of Diseases for Oncology, Third Edition (ICD-O-3) morphology codes (eAppendix B in the Supplement).7 The analysis included ICD-O-3 malignant histology/behavior and microscopically confirmed cases. Patient information in these databases is completely deidentified and publicly available, hence institutional review board approval was not needed per SEER/National Cancer Institute regulations.8,9
Study End Points and Statistical Analysis
Lung cancer subtype and histologic distribution were described. All NSCLC end points were reported for the overall population, as well as by age (<65 or ≥65 years), sex, and stage at diagnosis.
Incidence
Yearly incidence per 100 000 persons was age-adjusted to the 2000 US standard population.10 The total at-risk populations (denominators) were obtained from the USCS and SEER-18 databases. If the overall incidence from 2010 to 2017 was consistent between the SEER-NPCR (national level estimate) and SEER-18 databases, the SEER-18 incidence data was considered representative and was projected to a national level by stage.
Prevalence
A crude estimate of yearly prevalence per 100 000 persons was defined as the yearly incidence plus all patients who were diagnosed with NSCLC in prior years (the earliest year was 2000 when SEER-18 was established). Yearly prevalence for 2010 to 2016 was estimated based on SEER-18 data and projected to a national level using the National Cancer Institute’s Projected Prevalence (ProjPrev) software.11
Survival
Survival time measures the time, in months, from the date of diagnosis to death. Period survival statistics provide an estimate of survival by piecing together the most recent conditional survival estimates from several cohorts, which are then used to generate relative estimates of 1-year, 2-year, 3-year, 4-year, and 5-year survival rates12,13 (eAppendix A in the Supplement).
Initial Treatment
First-course treatment (radiation, chemotherapy, and/or surgery) was summarized; other treatments (eg, immunotherapy) were not included in the database. Data were summarized in terms of no treatment, single treatment, or multiple treatments (various combinations of chemotherapy, radiation, and/or surgery).
Statistical Software
Data were analyzed with the SEER*Stat statistical software (version 8.3.6.1, April 29, 2020), provided by SEER and SAS statistical software (version 9.4, SAS Institute).
Results
Database Overview Including Lung Cancer by Type
In SEER-NPCR 2010 to 2017, there were over 1.5 million new lung cancer cases; of these, approximately 1.28 million were NSCLC (51% male; 70% aged ≥65 years). In SEER-18 over the same period, demographic distributions were similar in the NSCLC population (53% male; 68% aged ≥65 years; median [Q1-Q3] age at diagnosis was 70 [63-77] years). Overall, NSCLC accounted for most cases (82.9% in SEER-NPCR; 83.9% in SEER-18), followed by SCLC (13.9% in SEER-NPCR; 12.9% in SEER-18) (Figure 1, A and B).
Figure 1. Distribution of Lung Cancer by Histologic Findings and Distribution of NSCLC by Stage, Age, and Year.
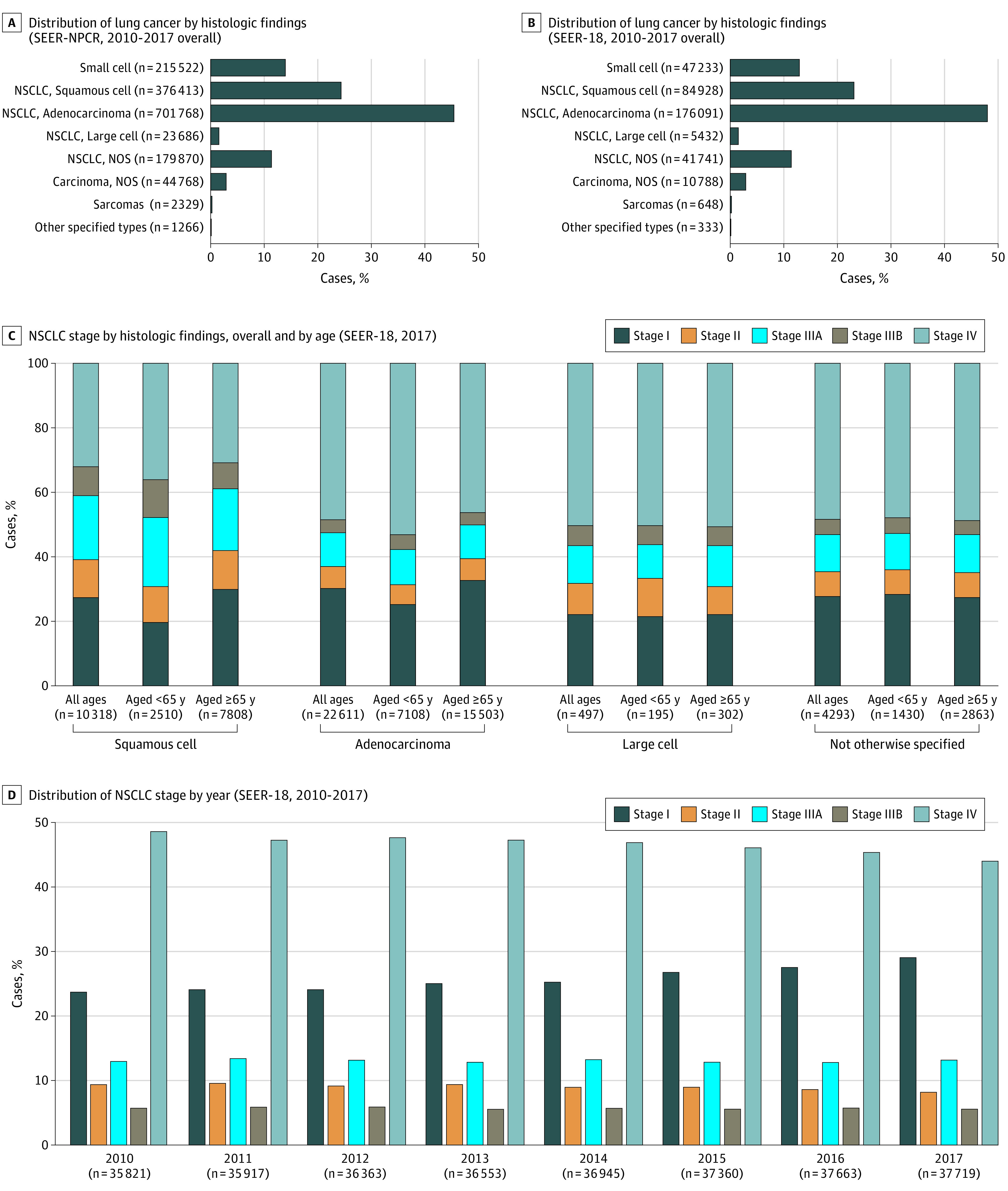
NOS indicates not otherwise specified; NSCLC, non–small cell lung cancer; SEER-18, Surveillance, Epidemiology, and End Results; NPCR, National Program of Cancer Registries. A, Distribution of lung cancer by histologic findings (SEER-NPCR, 2010-2017 overall). B, Distribution of lung cancer by histologic findings (SEER-18, 2010-2017 overall). C, NSCLC stage by histologic findings, overall and by age (SEER-18, 2017). D, Distribution of NSCLC stage by year (SEER-18, 2010-2017).
NSCLC Histology and Staging
Adenocarcinoma was the most common histologic finding (54.7%) followed by squamous cell (29.4%) in the SEER-NPCR database (57.1% and 27.6%, respectively, in SEER-18) (eAppendix C, eTable 1 in the Supplement). The frequency distribution of NSCLC stages by histologic analysis at initial diagnosis (SEER-18, 2017) is shown in Figure 1C; the proportion of stage I at diagnosis was higher among older patients, whereas the proportion of stage IV was higher among younger patients. From 2010 to 2017 (SEER-18), the proportion of stage I at diagnosis increased from 24% to 29%, whereas the proportion of stage IV decreased from 48% to 44.1% (Figure 1D).
Incidence of NSCLC (SEER-NPCR and SEER-18)
In SEER-NPCR, the incidence of NSCLC decreased from 46.4 to 40.9 per 100 000 from 2010 to 2017 (Figure 2A) (eAppendix C, eTable 2 in the Supplement). The incidence was markedly higher among older than younger patients and decreased from 2010 to 2017 in both age groups: for patients younger than 65 years, the incidence decreased from 15.5 to 13.5 per 100 000; for patients aged 65 years or older, the incidence decreased from 259.9 to 230.0. Of 163 716 incident cases of NSCLC in 2017, 50 795 (31%) were younger than 65 years, and 112 921 (69%) were aged 65 years or older. The incidence of NSCLC was consistently higher for men than for women, and decreased from 2010 to 2017 in both sexes: for men, the incidence decreased from 56 to 46.5 per 100 000; for women, the incidence per 100 000 decreased from 39.1 to 36.6.
Figure 2. Annual Incidence of NSCLC (2010-2017) Overall and by Age and Stage.
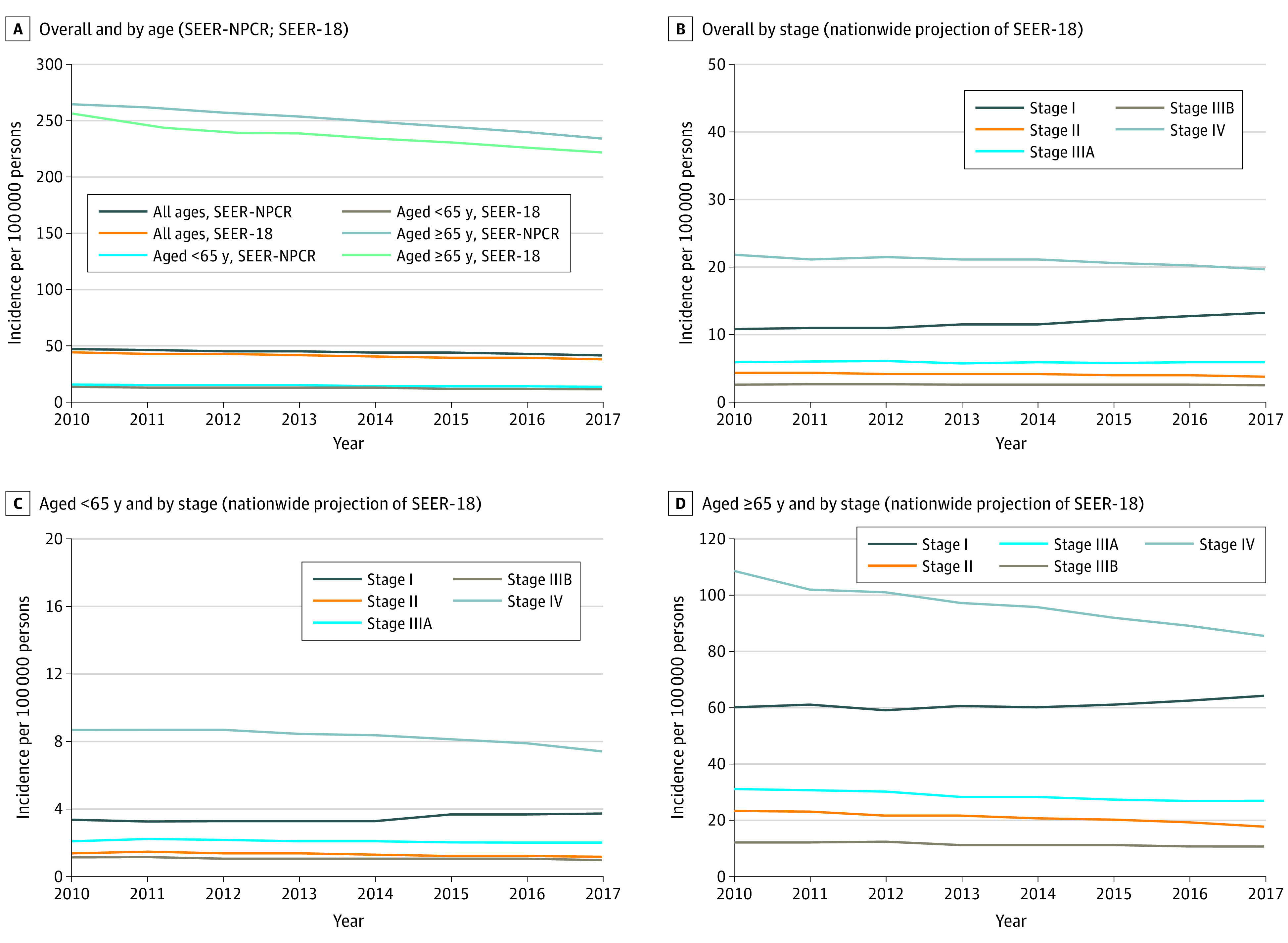
NSCLC indicates non–small cell lung cancer; SEER-18, Surveillance, Epidemiology, and End Results; NPCR, National Program of Cancer Registries. A, NSCLC incidence overall and by age (SEER-NPCR; SEER-18). B, Overall incidence by stage (nationwide projection of SEER-18). C, Incidence among those younger than 65 years by age and stage (nationwide projection of SEER-18). D, Incidence among those aged 65 years or older by stage (nationwide projection of SEER-18). Maximum values of vertical axes vary based on range of data shown. Overall incidence data (ie, not broken out by stage) are from SEER-NPCR and SEER-18. All other data are SEER-18 projected to a national level.
In SEER-18, the incidence of NSCLC decreased from 43.6 to 37.5 per 100 000 from 2010 to 2017 (Figure 2A) (eAppendix C, eTable 2 in the Supplement). The incidence per 100 000 decreased from 2010 to 2017 in both age strata: for patients younger than 65 years, incidence decreased from 13.5 to 11.4; for patients aged 65 years or older, incidence decreased from 251.8 to 217.9. Of 39 220 incident cases in 2017, 11 641 (30%) were younger than 65 years, and 27 579 (70%) were aged 65 years or older. The incidence was higher for men than for women, and decreased from 2010 to 2017 in both sexes: for men, the incidence decreased from 52.6 to 42.4 per 100 000; for women, the incidence decreased from 36.8 to 33.8. The incidence and general patterns of incidence were consistent between the SEER-NPCR and SEER-18 databases (eAppendix C, eTable 2 in the Supplement).
Incidence of NSCLC by Stage (Nationwide Projection of SEER-18)
From 2010 to 2017, the incidence of stage II, IIIA, and IIIB NSCLC was stable, and stage IV decreased slightly from 21.7 to 19.6 per 100 000, whereas stage I increased from 10.8 to 13.2 per 100 000 (Figure 2B) (eAppendix C, eTable 3 in the Supplement). The absolute increase in stage I incidence was more pronounced among patients aged 65 years or older (60.3 to 64.2 per 100 000 vs 3.32 to 3.72 per 100 000 in the aged <65 years cohort) though the relative increases in stage I incidence were greater among patients younger than 65 years (12% vs 6.6% for those aged ≥65 years, Figure 2, C and D; eAppendix C, eTable 3 in the Supplement). The greatest absolute and relative reductions in incidence from 2010 to 2017 were observed among patients aged 65 years or older with stage IV NSCLC (108.6 to 85.5 per 100 000, a change of −27%) compared with the younger than 65 years cohort (8.7 to 7.4 per 100 000, a change of −17.6%).
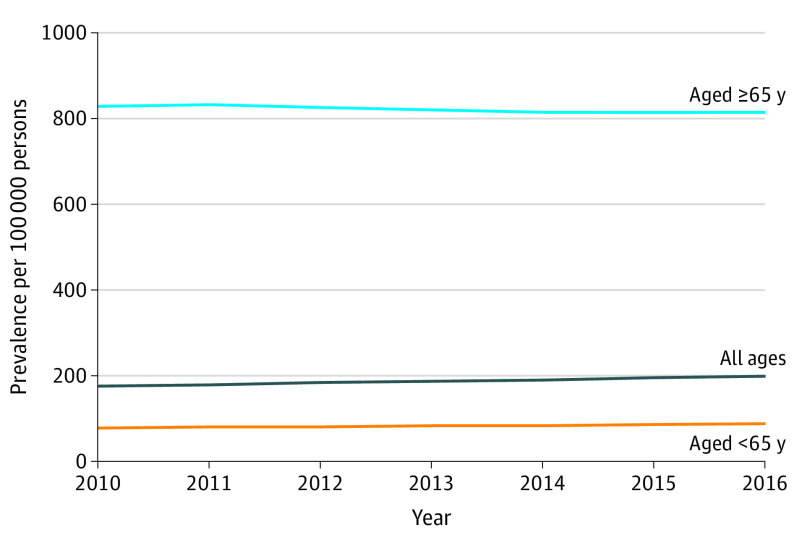
Prevalence of NSCLC (Nationwide Projection of SEER-18)
The prevalence of NSCLC increased from 175.3 to 198.3 per 100 000 persons from 2010 to 2016 (Figure 3) (eAppendix C, eTable 4 in the Supplement). This trend was observed in both men and women over the same time frame; women had a higher prevalence than men in each year assessed (eg, in 2016: 185.8 per 100 000 persons for men vs 210.3 per 100 000 persons for women). Whereas prevalence from 2010 to 2016 generally rose among patients younger than 65 years, it decreased among those aged 65 years or older. The prevalence in patients aged 65 years or older was consistently 9 times higher than that in patients younger than 65 years (eg, in 2016: 812.4 vs 87.9 per 100 000 persons) (Figure 3).
Figure 3. Annual Prevalence of NSCLC (2010-2016, Nationwide Projection of SEER-18) Overall and by Age.
NSCLC indicates non–small cell lung cancer; SEER-18, Surveillance, Epidemiology, and End Results. Prevalence data are from SEER-18 projected to a national level.
Survival After Diagnosis of NSCLC (SEER-18)
Estimates of survival based on SEER-18 are summarized in the Table. The 1-year survival for patients with NSCLC was 55.1% whereas the 5-year survival was 26.4%. Period survival estimates were lower for men vs women (5-year estimate: 21.9% vs 31.3%), and slightly lower for patients aged 65 years or older vs those younger than 65 years (5-year estimate: 25.5% vs 27.9%). For stage IV patients, the 5-year survival estimate was 5.8% (4.6% for age ≥65 years; 7.5% for age <65 years).
Table. Period Survival (SEER-18).
| Characteristic | Period survival rate, % | ||||
|---|---|---|---|---|---|
| 1-year | 2-year | 3-year | 4-year | 5-year | |
| Overall | 55.1 | 41.0 | 33.8 | 29.5 | 26.4 |
| Age, y | |||||
| <65 | 57.7 | 42.7 | 35.2 | 30.8 | 27.9 |
| ≥65 | 53.7 | 40.1 | 33.1 | 28.8 | 25.5 |
| Men | 50.4 | 35.6 | 28.6 | 24.6 | 21.9 |
| Women | 60.3 | 46.9 | 39.5 | 34.8 | 31.3 |
| Stage | |||||
| I | 92.8 | 85.2 | 78.2 | 73.1 | 68.4 |
| II | 78.7 | 64.3 | 55.3 | 49.2 | 45.1 |
| IIIA | 66.5 | 47.3 | 37.2 | 30.6 | 26.2 |
| IIIB | 54.3 | 34.3 | 25.4 | 20.5 | 17.3 |
| IV | 31.3 | 16.6 | 10.6 | 7.5 | 5.8 |
| Age <65 y | |||||
| Stage | |||||
| I | 94.6 | 88.9 | 83.2 | 78.7 | 74.9 |
| II | 86.7 | 73.5 | 64.9 | 59.0 | 55.3 |
| IIIA | 73.5 | 54.4 | 43.7 | 37.0 | 32.0 |
| IIIB | 59.2 | 37.8 | 28.9 | 23.5 | 20.4 |
| IV | 36.5 | 20.2 | 13.1 | 9.6 | 7.5 |
| Age ≥65 y | |||||
| Stage | |||||
| I | 92.0 | 83.6 | 76.0 | 70.6 | 65.3 |
| II | 75.1 | 60.2 | 50.9 | 44.7 | 40.0 |
| IIIA | 62.8 | 43.4 | 33.7 | 27.1 | 22.9 |
| IIIB | 51.0 | 31.9 | 23.0 | 18.2 | 15.1 |
| IV | 28.0 | 14.3 | 9.0 | 6.2 | 4.6 |
Abbreviation: SEER, Surveillance, Epidemiology, and End Results.
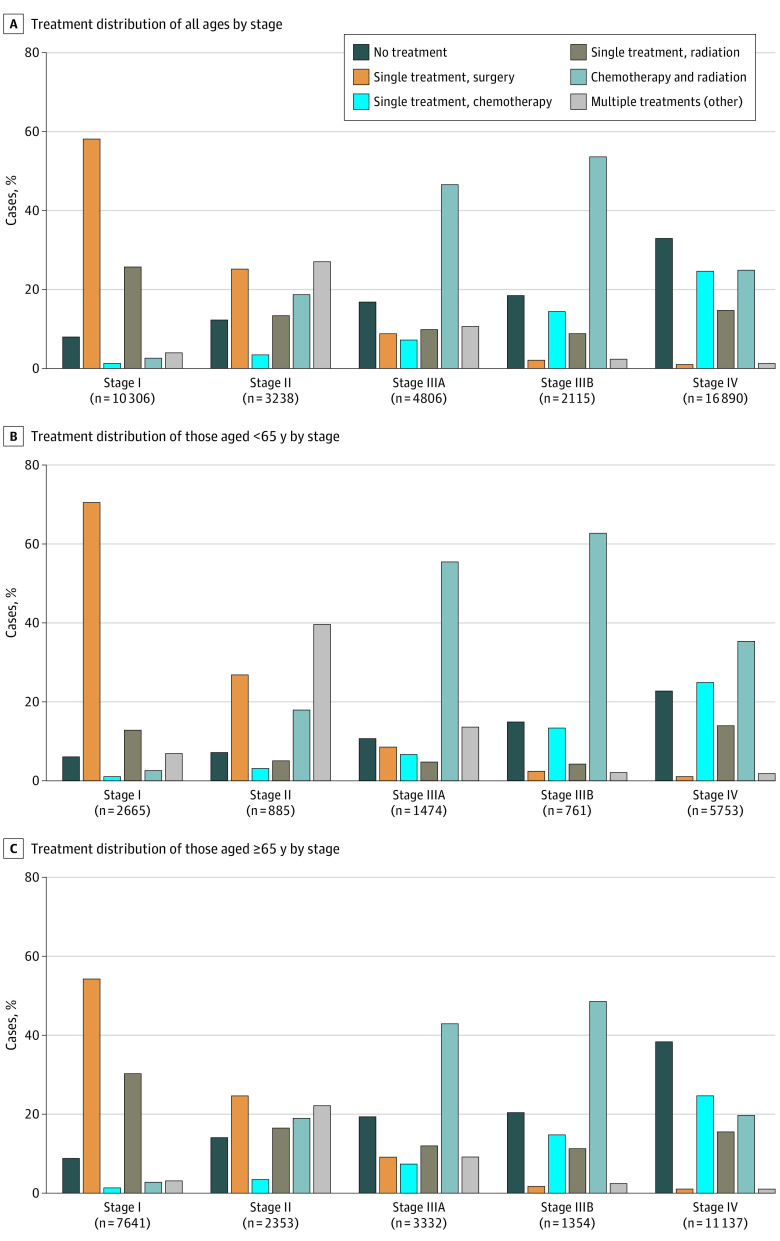
Initial Treatment for NSCLC (SEER-18)
In 2016, approximately 23% of all NSCLC patients were categorized as receiving no treatment, almost half (49.5%) received a single modality treatment (ie, surgery, chemotherapy, or radiation), and 27.7% received multiple treatments initially; this distribution was similar in all years assessed (eAppendix C, eTable 5 in the Supplement). The remainder of this section will primarily focus on 2016 (most recent year with data available). Of patients who received no treatment, most were aged 65 years or older (77.5%). Receiving no treatment was more common in patients aged 65 years or older vs those younger than 65 years (25.4% vs 16.7%), and in patients with stage IV vs stages I to IIIB NSCLC (33.1% vs 11.8%) (eAppendix C, eTables 5 and 6 in the Supplement). Treatment patterns in the overall population were generally consistent for men and women. A higher proportion of older patients (aged ≥65 years) received initial treatment with a single modality than those younger than 65 years (51.3% vs 45.6%); whereas a lower proportion of older than younger patients received multiple treatments (23.3% vs 37.7%).
Treatment Trends by Stage
Through years 2010 to 2016, notable shifts in initial treatment trends were observed in all NSCLC stages except stage IV. Generally, the proportions of patients with stages I to IIIA receiving surgery alone as initial therapy decreased, whereas the proportions with stages I to II receiving radiation alone as initial therapy increased; the proportion of patients with stage IIIB disease receiving radiation alone decreased (eAppendix C, eTable 6 in the Supplement). Among patients with stage I disease, the increase in single treatment radiation from 2010 to 2016 was more pronounced in patients aged 65 years or older (17.4% to 30.2%) than those younger than 65 years (7.7% to 12.8%).
The approximate proportions of patients with stage IV disease receiving no treatment, single treatment, and multiple treatments were 31% to 33%, 40% to 41%, and 26% to 28%, respectively, without notable variation through the years. A higher proportion of patients with stage IV disease aged 65 years or older received no treatment compared with those younger than 65 years (38.3% vs 22.8%), whereas a lower proportion received multiple treatment modalities as their first line of treatment than those younger than 65 years (20.8% vs 37.3%). The proportions of patients with stage IV disease receiving single treatments, and trends in the distribution of single treatments, were comparable between age groups.
Treatment trends by age and stage in 2016 are summarized in Figure 4. The proportion of patients categorized as having no treatment increased with increasing stage: 8%, 12.2%, 16.8%, 18.5%, and 33.1% of patients in stages I, II, IIIA, IIIB, and IV, respectively (Figure 4A). Regardless of stage, a greater proportion of patients aged 65 years or older received no initial treatment compared with those younger than 65 years (Figure 4, B and C).
Figure 4. Distribution of Initial Treatment by NSCLC Stage (SEER-18, 2016) .
NSCLC indicates non–small cell lung cancer; SEER-18, Surveillance, Epidemiology, and End Results. A, for all ages; B, for those younger than 65 years; and C, those aged 65 years or older. Multiple treatments (other) indicates various combinations of chemotherapy, radiation, and/or surgery (excluding chemotherapy + radiation).
Discussion
Overall, in this study, the incidence of NSCLC decreased slightly from 2010 to 2017; however, when examined by stage, the incidence of patients initially diagnosed with stage IV disease decreased, whereas that of stage I NSCLC increased. The incidence of stages II to III was relatively stable. One possible explanation for the increase in patients diagnosed with stage I NSCLC may be the increase in screening after publication of the National Lung Screening Trial (NSLT) in 2011 and US Preventive Services Task Force in 2013.14,15 Although the CMS National Coverage Decision was implemented in 2015, it is possible that awareness of the benefits of lung cancer screening after the publication of the NLST results in 2011 may have led to better follow-up of patients identified as having incidental pulmonary nodules and therefore diagnosed with lung cancer at an earlier stage. However, our data, though supportive, cannot completely attribute the stage shift to better follow-up of patients with these incidental pulmonary findings, given the overall limited uptake of lung cancer screening to date. Among patients aged 65 years or older, an increase in stage I NSCLC accompanied by a decrease in stage IV NSCLC at diagnosis is most likely associated with increased screening in this age group, and should be used to promote the establishment of lung cancer screening programs. This interpretation is supported by comparing changes in incidence for each stage among patients aged 65 years or older with the percentage of Medicare Part B patients receiving low-dose CT scans for lung cancer screening (HCPCS code G0297). Figure 2B shows that the incidence of stage I NSCLC in this population was relatively flat until 2015, at which point it began to increase. The first column of eAppendix C and eTable 7 in the Supplement provides detail behind Figure 2B, showing the year-to-year percentage changes in stage I NSCLC incidence from 2010 to 2017 (calculated using the results in eTable 3 in the Supplement). Columns 2 to 4 of eTable 7 in the Supplement are the number of Medicare Part B patients receiving low-dose CT scans for lung cancer screening, the total number of Medicare Part B patients, and the percent receiving low-dose CT scans for lung cancer screening. There were no CT scans from 2010 to 2014 since funding for them started in 2015.16 Year-on-year stage I incidence increased by 1.99%, 2.03%, and 3.03% from 2015 to 2017, coincident with increases in the percent of Medicare Part B patients receiving CT scans.
The incidence of NSCLC decreased across sex and age subgroups. These findings are consistent with a prior SEER-based comprehensive overview17 of lung cancer over the past 4 decades, which reported decreases in lung cancer incidence among both men and women in the past decade, and largely attributed these trends to tobacco control programs. The decrease in NSCLC incidence among women was smaller than that in men; this is consistent with a North American Association of Central Cancer Registries (NAACCR)-based report18 in which lung cancer incidence decreased in both men and women from 1995–2015, but the magnitude of decrease was greater in men.
The 5-year period survival estimate for the NSCLC population was 26.4%—higher than previously published period estimates of 23.3% (2014)19 and 24.6% (2015).20 This increase is consistent with a trend of increasing 5-year survival in a SEER-based analysis of lung cancer, and can be explained by improvements in treatment and/or earlier treatment associated with earlier diagnosis, though the possibility of lead time bias (longer recorded survival postcancer diagnosis resulting from earlier detection of cancer) cannot be completely excluded.17,21,22 The 5-year survival estimate was lowest for patients with stage IV NSCLC, especially among those aged 65 years or older (4.6%), but still higher than previously reported.3 Period survival estimates were lower for men than women, and only slightly lower for older than for younger patients.
In contrast to the overall decline in incidence, but consistent with the improvement in survival, the overall prevalence of NSCLC increased from 2010 to 2016, suggesting that patients are generally living longer after diagnosis. Whereas NSCLC prevalence increased among younger patients, it decreased among those aged 65 years or older. The overall prevalence trend was driven by the majority of the US population being younger (ie, the US population [denominator] was mostly aged <65 years), although older patients represented approximately two-thirds of NSCLC patients (ie, NSCLC cases [numerator] were mostly aged ≥65 years; eAppendix C, eTable 4 in the Supplement).
Although surgery remains the predominant initial treatment for stage I NSCLC, there has been a rise in the use of radiation over the past decade. This is likely due to increasing data on the efficacy of stereotactic body radiation in early-stage NSCLC.23,24 Despite availability of more effective treatments for NSCLC, a substantial proportion of patients (approximately 23% in 2016) may be undertreated. This potentially undertreated proportion was higher among patients aged 65 years or older vs those younger than 65 years (25.4% vs 16.7%) and could be a factor underlying the decreased NSCLC prevalence in the older subgroup. Patients with stage IV NSCLC aged 65 years or older had the highest proportion with no treatment. Although concerning, these findings are not surprising, as previous studies in early-stage disease have shown that older individuals are not offered adjuvant chemotherapy after surgical resection, even though the magnitude of benefit with such treatment was the same as in younger adults.25 However, these data should be interpreted with caution since the SEER-18 database only includes first-course radiation, chemotherapy, and surgery but not other treatments (eg, immunotherapy). Thus, some of the patients categorized as having no treatment may have received other treatments not included in the database. However, the guidelines do not differentiate between treatment modalities based on age, and treatments should not be excluded simply based on age26; thus, this relative undertreatment of older adults needs further investigation. Reasons for not treating older patients may include comorbid conditions that preclude aggressive therapy, reluctance of older patients to receive treatments, and therapeutic nihilism on the part of the practitioner.27 Of note, immunotherapy for NSCLC was not available as a first-line option prior to November 2016, and thus would not affect the most recently released registry data that form the basis of our report. Future estimates may reflect the improved survival seen in clinical trials with immunotherapy agents.
Limitations
Limitations of this analysis include its retrospective nature and use of registries that do not necessarily classify treatments as clinicians do. Also, due to natural lag in cancer registry data collection/release, certain data in the SEER-18 registry were only available through 2016. Another potential limitation is that the SEER-18 database does not include a nationwide sample.
These limitations notwithstanding, the SEER-NPCR database offered the advantage of directly providing nationally representative incidence data. After establishing consistency between SEER-NPCR and SEER-18 in terms of NSCLC incidence, we projected the more detailed prevalence and incidence information with staging data available in SEER-18 to a national level. Thus, our report provides an important and comprehensive update of epidemiologic information for NSCLC.
Conclusions
In this study, the incidence of NSCLC decreased from 2010 to 2017, and across age and sex subgroups. A rise in the incidence of stage I NSCLC at diagnosis likely reflects increased screening in the past decade. Increased overall prevalence of NSCLC and higher 5-year survival than reported previously may be associated with earlier detection of NSCLC and introduction of more effective treatments. Despite availability of effective treatments, patients aged 65 years or older with stage IV NSCLC have the lowest 5-year survival, which may be at least partly due to undertreatment. The reasons for this should be studied further.
eMethods
eTable 1. Incidence of NSCLC in the US by Histology 2010-2017
eTable 2. Incidence of NSCLC in the US, 2010-2017
eTable 3. Incidence of NSCLC in the US by Stage (Overall and Age Stratified), 2010-2017
eTable 4. Prevalence of NSCLC in the US, 2010-2016 (Unadjusted)
eTable 5. Initial Treatment for NSCLC (SEER-18, 2016)
eTable 6. Initial treatment by stage and by age
eTable 7. Incidence of Stage I NSCLC in patients ≥65 years of age and Medicare Part B CT scan proportions
References
- 1.American Cancer Society . Facts & Figures 2019. Accessed June 13, 2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 3.Cetin K, Ettinger DS, Hei YJ, O’Malley CD. Survival by histologic subtype in stage IV nonsmall cell lung cancer based on data from the Surveillance, Epidemiology and End Results Program. Clin Epidemiol. 2011;3:139-148. doi: 10.2147/CLEP.S17191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diwanji TP, Mohindra P, Vyfhuis M, et al. Advances in radiotherapy techniques and delivery for non-small cell lung cancer: benefits of intensity-modulated radiation therapy, proton therapy, and stereotactic body radiation therapy. Transl Lung Cancer Res. 2017;6(2):131-147. doi: 10.21037/tlcr.2017.04.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones GS, Baldwin DR. Recent advances in the management of lung cancer. Clin Med (Lond). 2018;18(suppl 2):s41-s46. doi: 10.7861/clinmedicine.18-2-s41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howlader N, Forjaz G, Mooradian MJ, et al. The effect of advances in lung-cancer treatment on population mortality. N Engl J Med. 2020;383(7):640-649. doi: 10.1056/NEJMoa1916623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fritz A, Percy C, Jack A, et al. , eds. International Classification of Diseases for Oncology. 3rd edition. Geneva, Switzerland: World Health Organization; 2000. Accessed September 25, 2020. https://apps.who.int/iris/bitstream/handle/10665/96612/9789241548496_eng.pdf;jsessionid=9F6F5CB6C762D10A185888244FDA8B18?sequence=1 [Google Scholar]
- 8.NPCR and SEER – US Cancer statistics public use database. Accessed June 8, 2020. https://www.cdc.gov/cancer/uscs/public-use/pdf/uscs-public-use-database-fact-sheet-508.pdf
- 9.National Cancer Institute SEER-Medicare linked database—IRB approval & HIPAA regulations. Accessed Sept 30, 2021. https://healthcaredelivery.cancer.gov/seermedicare/privacy/hipaa.html
- 10.National Cancer Institute . Surveillance, Epidemiology, and End Results Program. Standard Population – 19 Age Groups. Accessed July 18, 2020. https://seer.cancer.gov/stdpopulations/stdpop.19ages.html
- 11.National Cancer Institute . Surveillance Research Program. Projected Prevalence (ProjPrev) software. Accessed June 21, 2021. https://surveillance.cancer.gov/projprev/
- 12.Brenner H, Hakulinen T. Advanced detection of time trends in long-term cancer patient survival: experience from 50 years of cancer registration in Finland. Am J Epidemiol. 2002;156(6):566-577. doi: 10.1093/aje/kwf071 [DOI] [PubMed] [Google Scholar]
- 13.National Cancer Institute . Division of Cancer Control and Population Sciences. Surveillance Research Program. Accessed June 21, 2021. https://surveillance.cancer.gov/survival/cohort.html
- 14.Aberle DR, Adams AM, Berg CD, et al. ; National Lung Screening Trial Research Team . Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409. doi: 10.1056/NEJMoa1102873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Screening for Lung Cancer . U.S. Preventive Services Task Force Final Recommendation. December, 2013. Accessed September 21, 2021. www.uspreventiveservicestaskforce.org/home/getfilebytoken/KsRfT_uSd7J6WeXmbvbkav
- 16.Centers for Medicare and Medicaid Services . Medicare Coverage of Screening for Lung Cancer with Low Dose Computed Tomography (LDCT). MLN Matters Number: MM9246. October 15, 2015. Accessed September 21, 2021. www.lungcancerscreeningguide.org/wp-content/uploads/2018/10/MLM-MattersMedicareCoverageof-Screening.-pdf.pdf
- 17.Lu T, Yang X, Huang Y, et al. Trends in the incidence, treatment, and survival of patients with lung cancer in the last four decades. Cancer Manag Res. 2019;11:943-953. doi: 10.2147/CMAR.S187317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jemal A, Miller KD, Ma J, et al. Higher lung cancer incidence in young women than young men in the United States. N Engl J Med. 2018;378(21):1999-2009. doi: 10.1056/NEJMoa1715907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noone AM, Howlader N, Krapcho M, et al. , eds. SEER Cancer Statistics Review, 1975–2015, National Cancer Institute. Bethesda, MD. Based on November 2017 SEER data submission, posted to the SEER web site, April 2018. Accessed September 21, 2021. https://seer.cancer.gov/csr/1975_2015/
- 20.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2016, National Cancer Institute. Bethesda, MD. Based on November 2018 SEER data submission, posted to the SEER web site, April 2019. Accessed September 21, 2021. https://seer.cancer.gov/csr/1975_2016/
- 21.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128-2137. doi: 10.1056/NEJMsa1010705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersson TM-L, Rutherford MJ, Humphreys K. Assessment of lead-time bias in estimates of relative survival for breast cancer. Cancer Epidemiol. 2017;46:50-56. doi: 10.1016/j.canep.2016.12.004 [DOI] [PubMed] [Google Scholar]
- 23.Timmerman RD, Paulus R, Pass HI, et al. Stereotactic body radiation therapy for operable early-stage lung cancer: findings from the NRG Oncology RTOG 0618 Trial. JAMA Oncol. 2018;4(9):1263-1266. doi: 10.1001/jamaoncol.2018.1251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abel S, Hasan S, Horne ZD, Colonias A, Wegner RE. Stereotactic body radiation therapy in early-stage NSCLC: historical review, contemporary evidence and future implications. Lung Cancer Manag. 2019;8(1):LMT09. doi: 10.2217/lmt-2018-0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ganti AK, Williams CD, Gajra A, Kelley MJ. Effect of age on the efficacy of adjuvant chemotherapy for resected non-small cell lung cancer. Cancer. 2015;121(15):2578-2585. doi: 10.1002/cncr.29360 [DOI] [PubMed] [Google Scholar]
- 26.Ganti AK, deShazo M, Weir AB III, Hurria A. Treatment of non-small cell lung cancer in the older patient. J Natl Compr Canc Netw. 2012;10(2):230-239. doi: 10.6004/jnccn.2012.0021 [DOI] [PubMed] [Google Scholar]
- 27.Blanco R, Maestu I, de la Torre MG, Cassinello A, Nuñez I. A review of the management of elderly patients with non-small-cell lung cancer. Ann Oncol. 2015;26(3):451-463. doi: 10.1093/annonc/mdu268 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eTable 1. Incidence of NSCLC in the US by Histology 2010-2017
eTable 2. Incidence of NSCLC in the US, 2010-2017
eTable 3. Incidence of NSCLC in the US by Stage (Overall and Age Stratified), 2010-2017
eTable 4. Prevalence of NSCLC in the US, 2010-2016 (Unadjusted)
eTable 5. Initial Treatment for NSCLC (SEER-18, 2016)
eTable 6. Initial treatment by stage and by age
eTable 7. Incidence of Stage I NSCLC in patients ≥65 years of age and Medicare Part B CT scan proportions