Abstract
Background
In the United States (US), barriers in access to later steps in the kidney transplantation process (i.e. waitlisting) have been well documented. Barriers in access to earlier steps (i.e. referral and evaluation) are less well described due to the lack of national surveillance data. In this review, we summarize the available literature on non-medical barriers in access to kidney transplant referral and evaluation.
Methods
Following PRISMA guidelines, we conducted a scoping review of the literature through June 3, 2021. We included all studies (quantitative and qualitative) reporting on barriers to kidney transplant referral and evaluation in the US published from 1990 onwards in English and among adult end-stage kidney disease (ESKD) patients (PROSPERO registration number: CRD42014015027). We narratively synthesized results across studies.
Results
We retrieved information from 33 studies published from 1990 to 2021 (reporting data between 1990 and 2018). Most studies (n=28, 85%) described barriers among patient populations, three (9%) among provider populations, and two (6%) included both patients and providers. Key barriers were identified across multiple levels and included patient- (e.g. socioeconomic, sociocultural, and knowledge), provider- (e.g. miscommunication, staff availability, provider perceptions and attitudes), and system- (e.g. geography, distance to care, healthcare logistics) level factors.
Conclusions
A multi-pronged approach (e.g. targeted and systemwide interventions, and policy change) implemented at multiple levels of the healthcare system will be necessary to reduce identified barriers in access to early kidney transplant steps. Collection of national surveillance data on these early kidney transplant steps is also needed to enhance our understanding of barriers to referral and evaluation.
Keywords: kidney transplantation, barriers, referral, evaluation
Introduction
For most of the 785,000 patients in the United States (US) living with end-stage kidney disease (ESKD),1 kidney transplantation remains the optimal treatment as it provides longer survival, better quality of life, and substantial cost savings as compared with remaining on dialysis.2 Despite this, only 13.5% of ESKD patients in 2018 were waitlisted for a kidney transplant.1
In the US, there are several complex steps to kidney transplantation that patients and clinical providers must navigate to ensure access to kidney transplantation. These steps, described previously3,4 and summarizedin Figure 1, vary by center but generally include: transplant education, referral for transplant evaluation, initiation of the transplant evaluation process by attending an education class and medical appointments, completing the evaluation process, including the multiple necessary tests and appointments, so that transplant clinicians can make a decision about transplant candidacy, approval and placement on the national deceased donor waiting list, and finally, receipt of a living or deceased donor transplant.
Figure 1.
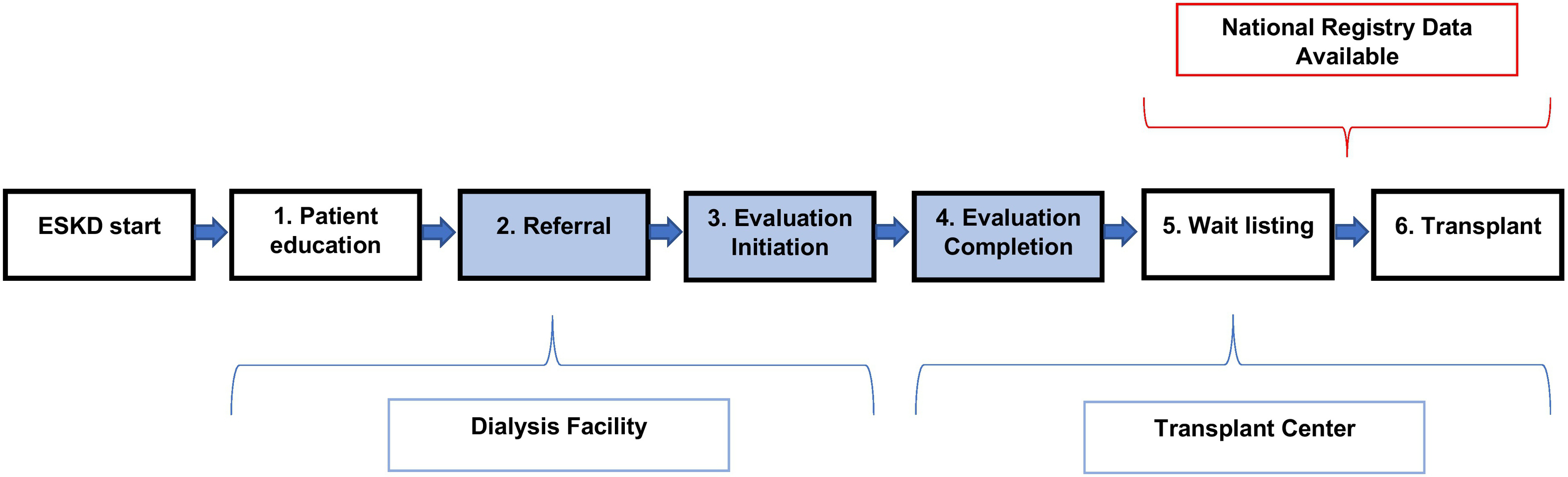
The Six Steps to Kidney Transplantation in the United States
A growing body of evidence has documented the multi-level (i.e. patient, provider, and system) barriers associated with later kidney transplant steps (i.e. waitlisting).5–7 For example, Black race,5 screening practices,6 and poor communication between care providers7 have all been associated with reduced waitlisting and kidney transplant rates. Whether these barriers also play a role in earlier steps of kidney transplantation (i.e. referral and evaluation) is less well known due to a lack of national surveillance data on these necessary critical steps. While a number of studies have examined these earlier outcomes, and two recent reviews have described these earlier outcomes in the context of racial disparities,8,9 there has been no scoping review summarizing all of the identified non-medical barriers to early kidney transplant steps. Understanding barriers at all steps in the kidney transplant process is important as some evidence suggests that factors associated with delays in later transplants steps are not always the same as factors associated with delays in earlier steps.10,11 For example, there is some evidence that Black ESKD patients in the Southeastern US have higher rates of referral for kidney transplantation, but lower evaluation rates,11 as compared with White ESKD patients, suggesting that interventions to reduce racial disparities in this region should be targeted to the step after referral, but before waitlisting.12 A comprehensive understanding of barriers at all steps in the kidney transplant process is essential to inform policy and formulate interventions to address specific barriers among targeted populations.
Therefore, in this scoping review we summarize the published literature reporting on non-medical barriers in access to early steps (i.e. referral, evaluation initiation, and evaluation completion) of kidney transplantation in the US.
Methods
This review adheres to the Preferring Reporting Items for Systematic Review and Meta-Analysis (PRISMA) extension for scoping reviews (PRISMA-ScR) guidelines,13 Supplementary Table 1. This review has been registered with the PROSPERO International Prospective Register of Systematic Reviews (registration number: CRD42020210587). A study protocol has not previously been published. As this is a review of existing studies, this study is exempt from Institutional Review Board approval.
Search strategy
A literature search was conducted with an experienced reference librarian (MSW) on May 14, 2020 to identify research articles published from 1990 onwards. Using a combination of controlled vocabulary and text words related to ESKD and kidney transplantation, searches were performed in PubMed, Cochrane Library, Embase, CINAHL, and Web of Science. In the broader subject search related to barriers to ESKD, and because of PubMed’s lack of proximity searching, it was deemed necessary to limit the text words used in the previous search strings, and broad concepts were searched. In addition, the search parameter “human” was not used in CINAHL, Web of Science, or Cochrane. Key search terms are described in detail in Supplementary Table 1. The search was updated on June 3, 2021 to identify any publications arising since May 14, 2020, and the reference lists of included studies were also screened for additional articles.
Eligibility criteria
We included all full-text research articles that reported only on non-medical barriers to referral, evaluation initiation, or evaluation completion among adult ESKD patients in the United States and published in English. We included both quantitative and qualitative research studies. To increase the generalizability of our findings to the broader adult ESKD population, we excluded studies that: 1) described kidney transplant access in pediatric populations; 2) described interventions to address barriers; 3) focused on barriers among donors; 4) focused on dual organ or re-transplantation; or 5) focused on non-general populations such as immigrants, previous donors, or other select populations.
Article selection
All identified articles were entered into Covidence, an online systematic review management program, for screening. Each article was title and abstract screened by any combination of two reviewers (JLH, AP, SR, KS, MU) and conflicts resolved by a third reviewer. Studies subsequently included in the full-text screen were also screened by two reviewers (JLH, AP, SR, KS, MU) and conflicts resolved by a third reviewer. In the event that conflicts could not be resolved by a third reviewer, a discussion by the full team was conducted until a final disposition was reached.
Data analysis and assessment of bias
Microsoft Excel was used to extract the following data from included articles: publication characteristics (i.e., year of publication, author names, PMID ID, journal, data source); study characteristics (i.e., study design (cohort, case-control, cross-sectional), study year), sample characteristics (i.e., sample size, description of the sample, age range); transplant outcome (i.e., referral, evaluation initiation, evaluation completion), barrier type (i.e., patient, provider, system), and findings (i.e. unadjusted, adjusted). Data extraction was performed by three authors (JLH, AP, KS) and discrepancies were discussed until a consensus was reached. Due to the heterogeneity of studies, a qualitative approach to data analyses was taken and data was synthesized narratively based on the key themes found in the research articles included in the review.
Results were presented by patient-, provider-, and system-level barriers, as informed by a social determinants of health framework.14 Within these broad categories, key themes were grouped into subcategories as dictated by the findings of the review. For example, if a barrier was identified across several studies (e.g., race), a subcategory to describe those findings was generated. In other instances, where fewer studies reported on a specific factor, but multiple factors were deemed to be related, an umbrella term was created. For example, discrimination, mistrust of the medical system, and lack of social support was grouped under the heading sociocultural barriers. We focused on reporting barriers that were significantly associated with early kidney transplant access, and commented on other, non-significant barriers, deemed, in our professional opinion, to be important. Results were, largely, reported quantitively for quantitative studies, and qualitatively for qualitative studies.
The methodological quality of each study was critically appraised using a modified version of the Mixed Methods Appraisal Tool, which has previously demonstrated reliable quality scores for qualitative, quantitative, and mixed methods studies, Supplementary Table 2.15–17 Two authors (AP and MU) independently scored each study, and discrepancies were resolved by a third author (JLH).
Results
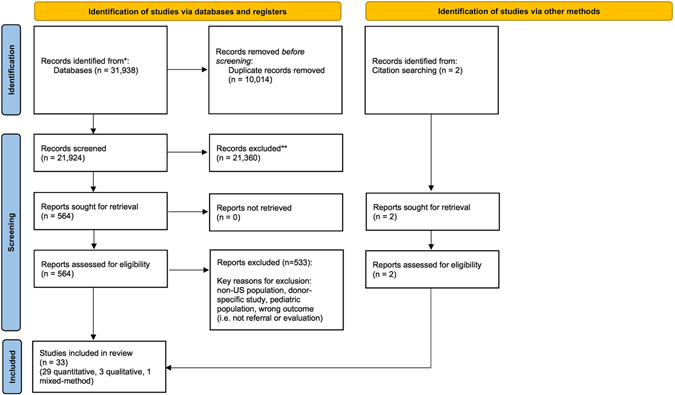
The original search yielded 31,935 records and three18–20 additional articles (total 31,398) were identified from the updated search in June 2021. A further two articles were identified from citation searching. After removing 10,014 duplicates, 21,924 articles were entered into Covidence for screening. At the conclusion of the review, 33 articles were included in the final sample (see Figure 2).
Figure 2.
PRISMA 2020 Flow Diagram of Literature Search for Scoping Review
The 33 articles included 29 quantitative, three qualitative, and one mixed-method study published from 1990–2021 and reporting on data between 1990 and 2018, Table 1. Eight (24%) studies reported on referral outcomes, 18 (55%) reported evaluation outcomes (initiation, completion, or both), six (18%) reported both referral and evaluation outcomes, and one (3%) reported on pre-emptive referral (i.e. referral prior to dialysis initiation). Though there are no national US studies on early steps to kidney transplantation, several states and regions were represented in this review: Alabama, Arizona, California, Colorado, Florida, Georgia, Hawaii, Illinois, New Mexico, New York, North Carolina, Michigan, Mid-Atlantic (Maryland, Virginia, District of Columbia), Missouri, Pennsylvania, South Carolina, and Washington.
Table 1.
Summary of studies included in a scoping review of barriers to early kidney transplant steps.
| First author (publication year) | Title | Study design | Study year | Population, setting | Sample size | Outcome | Barriers identified |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Ayanian [23] (1999) | The effect of patients’ preferences on racial differences in access to renal transplantation | Quantitative; cohort | 1996–1999 | Patients on dialysis; aged 18–54; Alabama, Southern California, Michigan, and the mid-Atlantic region | 1392 | Referral | Patient-level (Black racea) |
| Ayanian [51] (2004) | Physicians’ beliefs about racial differences in referral for renal transplantation | Quantitative; cross-sectional | 1999–2000 | Nephrologists; Alabama, Southern California, Michigan, and the mid-Atlantic region | 289 | Evaluation | Provider-level (patient-physician communication, perception of patient interest in transplant/ability to navigate transplant process, patient social and financial support, perceived ability of patient compliance after transplantationa) |
| Browne [44] (2011) | The relationship between social networks and pathways to kidney transplant parity: Evidence from Black Americans in Chicago | Quantitative; cross-sectional | 2004 | Black hemodialysis patients; aged 18–65; Chicago, Illinois | 228 | Evaluation | Patient-level (social network, incomea) Provider-level (information from dialysis teama) |
| Browne [52] (2016) | Kidney transplant referral practices in Southeastern dialysis units | Quantitative; cross-sectional | 2012 | Dialysis providers; Georgia, North Carolina, and South Carolina | 546 | Referral | Provider-level (delivery of transplant education, staff perception of patient interest and eligibility for transplantb) |
| Butler [20] (2021) | Thematic analysis of the medical records of patients evaluated for kidney transplant who did not receive a kidney | Qualitative chart review | 2008–2018 | ESKD patients who were referred, but did not get a transplant; Washington | 148 | Evaluation | Patient-level (uncertainty about evaluation process; psychological burdenb) Provider-level (local providers unclear about what the evaluation process might entail and requirements for transplantb) |
| Clark [24] (2008) | Promoting access to renal transplantation: the role of social support networks in completing pre-transplant evaluations | Quantitative; cohort | 1996–1997 | Patients on dialysis; aged 18–54; Alabama, Southern California, Michigan, and the mid-Atlantic region | 742 | Evaluation completion | Patient-level (Black race, older age, instrumental support networksa) Provider-level (physician recommends transplanta) System-level (geographic regiona) |
| Crenesse-Cozien [49] (2019) | Kidney transplant evaluation: inferences from qualitative interviews with African American patients and their providers | Qualitative; focus group | 2018 | African American patients listed or transplanted; transplant providers at a single center, Erie County, New York | 24 patients; 14 providers | Evaluation completion | Patient-level (inadequate transplant knowledge) Provider-level (staff inaccessibility and lacking support, miscommunication of transplant informationb) |
| Dageford [41] (2014) | Understanding patient barriers to kidney transplant evaluation | Quantitative; cross-sectional | 2012–2013 | Referred patients scheduled for an evaluation; single center (region not reported) | 104 | Evaluation initiation | Patient-level (health literacy, being able to afford the transplant operation and the medication post-transplant, concern about finding a living donor, being on dialysis, prior evaluation elsewhereb) |
| Epstein [25] (2000) | Racial disparities in access to renal transplantation - clinically appropriate or due to underuse or overuse? | Quantitative; cohort | 1996–1997 | Patients on dialysis; aged 18–54; Alabama, Southern California, Michigan, and the mid-Atlantic region | 1518 | Referral | Patient-level (Black race, low education, older age, patient preferencea) System-level (residence in Alabama, distance to transplant centera) |
| Gander [26] (2018) | Racial disparities in preemptive referral for kidney transplantation in Georgia | Quantitative; cohort | 2005–2015 | Adults referred for evaluation; Georgia | 7752 | Pre-emptive referral | Patient-level (Older age, Black race, male gender, no insurance coveragea) |
| Gillespie [47] (2017) | Hemodialysis clinic social networks, sex differences, and renal transplantation | Quantitative; cohort | 2012–2015 | Adult hemodialysis patients in a Mid-Atlantic region clinic | 46 | Referral and evaluation (initiation and completion) | Patient-level (social isolationa) |
| Grubbs [50] (2009) | Health literacy and access to kidney transplantation | Quantitative, cohort | 2007–2008 | Black and White hemodialysis patients; aged 18–75, San Francisco Bay, California | 62 | Referral | Patient-level (low health literacya) |
| Hamoda [46] (2020) | Association of sociocultural factors with initiation of the kidney transplant evaluation process | Quantitative; cohort | 2014–2016 | Black and White adults referred for evaluation; Georgia | 528 | Evaluation initiation | Patient-level (medical mistrust, experienced discrimination, perceived racisma) |
| Jones [27] (2018) | Racial/ethnic differences in barriers to kidney transplant evaluation among hemodialysis patients | Quantitative; cross-sectional | 2016 | Incident hemodialysis patients; Denver, Colorado | 167 | Evaluation | Patient-level (Black racea, lack of knowledge of transplant benefits and processb); |
| Kazley [42] (2012) | Barriers facing patients referred for kidney transplant cause loss to follow-up | Mixed-methods | 2009–2011 | Patients referred for transplant who did not follow-up with the workup; South Carolina | 83 | Evaluation completion | Patient-level (eligibility and financial concerns, scared of getting a transplant, concerns regarding transplant wait times and donor availability, lack of understanding of transplant benefits and processb) |
| Keddis [35] (2018) | Transplant center assessment of the inequity in the kidney transplant procees and outcomes for the Indigenous American patients | Quantitative; cross-sectional | 2012–2016 | Patients who had completed the transplant evaluation; Arizona | 900 | Time from referral to evaluation | Patient-level (Indigenous American race, dialysis durationa) System-level (distance to transplant centerb#) #distance to transplant center was not associated with time from referral to evaluation in multivariate analysis |
| Lockwood [28] (2017) | Patient-reported barriers to the pre-kidney transplant evaluation in an at-risk population in the United States | Quantitative; cohort | 2013–2014 | Adult ESKD patients who presented for evaluation; urban Midwestern transplant center (Illinois) | 100 | Evaluation initiation and completion | Patient-level (African American race, lower income, on dialysis, financial difficulty, transportation issues, psychosocial influences, perceived poor communication between patients and providers, access to careb); |
| McCauley [43] (1997) | Factors determining the rate of referral, transplantation, and survival on dialysis in women with ESRD | Quantitative; cohort | 1990–1992 | Females initiating dialysis; aged 18–55; Pennsylvania | 276 | Referral | Patient-level (older age, lower education level, unemploymenta) System-level (Alleghany county had higher rate of referral than Philadelphiaa) |
| McPherson [18] (2020) | Distance to kidney transplant center and access to early steps in the kidney transplantation process in the Southeastern United States | Quantitative; cohort | 2012–2017 | Adults initiating dialysis in Georgia, North Carolina, South Carolina | 27,250 | Referral and evaluation initiation | Patient-level (older age, female gender, White race, Medicare/Medicaid insurancea) System-level (increased distance from a transplant centerb#) #distance to transplant center was not associated with referral or evaluation in multivariate analysis |
| McPherson [19] (2021) | Dialysis facility profit status and early steps in kidney transplantation in the Southeastern United States | Quantitative; cohort | 2012–2017 | Adults initiating dialysis in Georgia, North Carolina, South Carolina | 33,651 | Referral and evaluation initiation | System-level (For-profit dialysis centera#) #For profit status was associated with referral, but not evaluation initiation |
| Monson [29] (2015) | Disparities in completion rates of the medical prerenal transplant evaluation by race or ethnicity and gender | Quantitative; cohort | 2009–2010 | Adult patients presenting for initial evaluation, Chicago, Illinois | 256 | 12-month evaluation completion | Patient-level (Black race, Hispanic ethnicity, longer dialysis durationa) |
| Nonterah [36] (2020) | Pre-transplant evaluation completion for Black/African American renal patients: two theoretical frameworks | Qualitative; focus group | 2014–2015 | Transplant providers from 9 transplant centers in the Mid-Atlantic, Mid-Western, and Southeast; and African American (AA) patients at a single safety-net hospital in the mid-Atlantic region | 30 patients; 23 providers | Evaluation completion | Patient-level (socioeconomic impediments, belief systems, personality characteristics, informational/educational gapsb) Provider-level (miscommunicationb) Systems-level (healthcare logisticsb) |
| Patzer [30] (2012) | The role of race and poverty on steps to kidney transplantation in the Southeastern United States | Quantitative; cohort | 2005–2010 | Adult ESKD patients referred for evaluation, Georgia | 2291 | Evaluation (initiation and completion) |
Evaluation initiation Patient-level (Black race, public insurance, low education, unemploymentb) System-level (neighborhood-level poverty, distance to transplant center, ruralityb) Evaluation completion Patient-level (Black race, public insuranceb) |
| Patzer [10] (2015) | Variation in dialysis facility referral for kidney transplantation among patients with end-stage renal disease in Georgia | Quantitative; cohort | 2005–2012 | Incident adult ESKD patients; aged 18–69, Georgia | 15,279 | 12-month referral | Patient-level (older age, White race, female gender, lower utilization of pre-ESKD nephrology care, Medicaid/Medicare insurancea) |
| Patzer [11] (2020) | Dialysis facility referral and start of evaluation for kidney transplantation among patients treated with dialysis in the Southeastern United States | Quantitative; cohort | 2012–2018 | Incident adult ESKD patients; aged 18–79; Georgia, North Carolina, and South Carolina | 34,857 | 12-month referral and 6-month evaluation initiation | System-level (dialysis facility profit status, patient-social worker ratio, neighborhood povertya) 12-month referral: Patient-level (older age, female gender, White race, Medicare or Medicaid insurance, pre-ESKD nephrology carea) System-level (dialysis facility profit status#, patient-social worker ratio, neighborhood povertya) 6-month evaluation (from referral date): Patient-level (older age, female gender, Black race, Medicare or Medicaid insurance, pre-ESKD nephrology carea System-level (dialysis facility profit status#, patient-social worker ratio, neighborhood povertya) #not significant in adjusted models |
| Paul [37] (2018) | Standardized transplantation referral ratio to assess performance of transplant referral among dialysis facilities | Quantitative; cohort | 2008–2012 | Incident ESKD patients, Georgia | 8308 | Referral (ratio) and evaluation | Patient-level (older age, non-Black race, female gender, Medicare insurancea) System-level (dialysis facilitya) |
| Plantinga [48] (2017) | Referral for kidney transplantation and indicators of quality of dialysis care: a cross-sectional study | Quantitative; cross-sectional | 2005–2012 | Incident ESKD patients; aged 18–69; Georgia | 12,926 | 12-month Referral | Patient-level (pre-ESKD nephrology care, transplant education, initiating dialysis with permanent accessa) System-level (high transplant ratio, high waitlist rate, and high catheter use at 90 daysa) |
| Schold [40] (2011) | Barriers to evaluation and waitlisting for kidney transplantation | Quantitative; cohort | 2003–2008 | Referred adult ESKD patients; Florida | 3029 | Evaluation | Patient-level (older age, lower income, non-commercial insurancea) |
| Sequist [34] (2004) | Access to renal transplantation among American Indians and Hispanics | Quantitative; cohort | 1994–1999 | Dialysis patients; aged 20–59; Arizona and New Mexico | 1335 | Referral and evaluation (initiation and completion) |
Referral: Patient-level (White race, older age, low education, longer dialysis duration, use of peritoneal dialysisa) Evaluation Initiation: Patient-level (Hispanic ethnicitya) Evaluation Completion: Patient-level (American Indian racea) |
| Tandon [55] (2016) | Nephrologists likelihood of referring patients for kidney transplant based on hypothetical scenarios | Quantitative; cross-sectional | Not reported | Nephrologists, Eastern US | 216 | Referral | Patient-level (older age rural residencea) Provider-level (no academic affiliation, being >10 years from fellowshipa) |
| Waterman [31] (2013) | Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant | Quantitative; cohort | 2004–2010 | Referred Black and White ESKD patients, Missouri | 695 | Evaluation completion within 1 year | Patient-level (Black race, low trust in hospitals, less comprehensive insurance coverage, lower willingness to be on the waiting list or to pursue living donor kidney transplant, lower access to transplant education resources, lower transplant knowledgea) |
| Weng [32] (2005) | Rates of completion of the medical evaluation for renal transplantation | Quantitative; cohort | 2002–2003 | Patients evaluated for transplant, Pennsylvania | 175 | Time to evaluation completion | Patient-level (Black race, never married status, not enquiring about living donor kidney, Medicare insurance, source of transplant information was not a physician or nursea) |
| Wong [33] (2009) | Racial disparities in Pacific Islanders undergoing renal transplant evaluation | Quantitative; cohort | 2005–2007 | Patients referred for evaluation, Hawaii | 207 | Time to attending evaluation initiation and completion | Patient-level (Pacific Islander raceb) |
Multivariate Adjusted.
Unadjusted.
Table 1 details the studies included in this review and the key kidney transplant barriers identified in each study. Below, we summarize these findings in the context of patient, provider, and system-level barriers to transplant, but acknowledge that these multi-level factors are not always mutually exclusive.
Quality assessment of included studies
The quality of these studies is reported in Supplementary Table 3. Overall, we deemed all studies to have sufficient quality to be included in the review with only seven (21%) studies having just one quality criterion listed as “No” or “Can’t Tell”. All other quality criterions were categorized as “Yes”.
Patient-level Barriers
In total, 30 (91%) studies identified patient-level barriers to referral or evaluation. These can largely be categorized into race, gender, health insurance, sociocultural, and knowledge-based barriers.
Race
It is well known that racial and ethnic minorities experience reduced access to later kidney transplant steps (i.e. waitlisting).21 Race and ethnicity, in the context considered here, serves as a social construct and a proxy for racism that operates at multiple levels (e.g., interpersonal or structural).22 In this review of barriers to early kidney transplant steps, 16 studies collectively show that Black,11,23–32 Pacific Islander,33 Hispanic,29,34 and Indigenous Americans34,35 are more likely to have reduced access to transplant referral and evaluation as compared with White Americans. The majority of the evidence related to racial disparities in early kidney transplant steps describes differences between Black and White ESKD patients. Surprisingly, most studies in this review showed that Black race was associated with a reduced likelihood of evaluation initiation or completion, but not referral. In fact, in studies where both referral and evaluation outcomes were assessed, Black (vs. White) ESKD patients were ~22% more likely to be referred, but ~7% less likely to be evaluated.18,34,36,37 The exception to this was two studies that reported Black (vs. White) race was associated with reduced referral rates, though these were both older studies conducted in the late 1990s.23,25 In contrast, in a study in Georgia, Black (vs. White) ESKD patients were 37% less likely to be pre-emptively referred,26 suggesting that racial disparities observed at later kidney transplant steps (i.e. waitlisting) may be partially explained by a lack of adequate healthcare or pre-dialysis care by a nephrologist, which disproportionately impacts Black Americans.1
Gender
Overall, fewer studies reported gender as a barrier to early kidney transplant steps, despite female gender being a well-documented barrier to later transplant steps.38 Of the five studies reporting gender as a barrier, largely studies from Georgia, South Carolina, and North Carolina, women were ~14% less likely to be referred and ~6% less likely to be evaluated as compared with men,10,11,18,37 yet 16% more likely to be pre-emptively referred after adjustment for several other factors including socioeconomic characteristics.26 Reasons for these gender disparities remain elusive, even for later transplant steps. However, commonly cited reasons include a lower probability of discussing kidney transplantation as a treatment option with women, fewer women completing the clinical workup needed for kidney transplantation, and gender discrimination (e.g. physicians may assess a woman’s health differently).39 It has also been reported that women are more likely to have health-related and psychosocial concerns about transplantation and have more personal concerns in asking for potential living-related donation as compared with men.39
Health Insurance status
Despite Medicare generally being available to patients with ESKD, health insurance status may still be a barrier to kidney transplant referral and evaluation. In this review, public or no insurance (vs. private insurance), was reported to be associated with reduced rates of referral and evaluation in ten studies across several US regions.10,11,18,26,30–32,36,37,40 Financial concerns related to the cost of the kidney transplant operation and the medication post-transplant are cited as key barriers to early transplant access.28,36,41,42 Racial disparities in access to early kidney transplant steps may be explained, in part, by insurance coverage as Black Americans are less likely to have private insurance when compared to White Americans.30 Further, a lack of insurance may be driven by, or compounded, by low (vs. high) education,25,30,34,43 unemployment (vs. employed),30,43 and low (vs. high) income28,36,40,44 which were identified as barriers to referral and evaluation in eight studies included in this review.
Sociocultural Barriers
Sociocultural factors, the values, beliefs, and customs of a population, and the interpersonal relationships and societal structures that shape them, have been associated with several health outcomes.45 Here, the sociocultural barriers to early kidney transplant steps identified in this review include perceived discrimination, mistrust of the medical system, and lack of social support.
In a 2020 study, Hamoda et al. examined sociocultural factors that may explain racial disparities in evaluation initiation.46 In this study of 528 adult ESKD patients referred for evaluation in Georgia, the proportion of Black patients initiating evaluation was less than that of Whites (49.6% vs 57.9%), although this difference did not reach statistical significance (p=0.11). In multivariable models, medical mistrust, experienced discrimination, and perceived racism were associated with a 41%, 38%, and 39% decrease in rates of evaluation initiation, respectively. Interestingly, these associations were not significantly modified by race in this majority Black sample of patients, despite the prevalence of these factors being reportedly higher in Black vs. White patients.. Medical mistrust was similarly identified as a barrier to evaluation completion in a Missouri study, 31 and in a qualitative study of Black ESKD patients from a single center in the Mid-Atlantic.36 Hamoda et al.46 conclude that racism and its sociocultural correlates, rather than race alone, play a critical role in perpetuating racial disparities in kidney transplant access, and highlight the limited nature of using race alone to measure underlying sociocultural barriers to kidney transplant access.46
Low levels of social support was identified as a barrier to early transplant steps in five studies included in this review.24,32,36,44,47 Using a social network theory approach, Browne44 demonstrated that Black hemodialysis patients who had people in their social network with information about kidney transplant were 76% more likely to be evaluated for a kidney transplant, but were not more likely to have the correct information about how to get a kidney transplant. In a multi-regional study including over 700 ESKD patients, those with low levels of instrumental support were less likely to have complete kidney transplant evaluations as compared with those with high levels (25% vs. 46%, respectively).24 In a smaller study of 46 hemodialysis patients, those that formed a social network within their dialysis facility completed a median of two additional steps toward kidney transplantation as compared with socially isolated patients.47 In focus groups, Black ESKD patients also identified having a strong social network as a motivator to completing kidney transplant evaluation.36 Finally, in a surprising finding from a Pennsylvania study, those who were never married completed the kidney transplant evaluation more rapidly than those who were married.32 The authors of this study hypothesized these patients may have strong social networks despite never being married, or may have other unmeasured characteristics that are associated with timely completion of the transplant evaluation process.32
Other sociocultural factors associated with early kidney transplant access identified in this review included patient belief systems, personality characteristics, perceived burden, fear of having a transplant, and willingness to ask friends or family to be a kidney donor.20,31,36,42 For example, in focus groups among Black ESKD patients, patients’ religious beliefs, faith or spirituality were identified as motivators to completing transplant evaluation.36 Patients desire to get off dialysis and have a better quality of life was similarly identified as a motivator for evaluation completion, while fears about losing health insurance benefits after transplant or feeling overwhelmed were identified as barriers to completing the evaluation.36 In a South Carolina mixed-methods study, one of the most commonly cited barriers to completing kidney transplant evaluation was being scared of getting a transplant,42 which may result from misinformation, misperceptions related to transplant surgery, or limited health literacy/health decision-making capacity. This same study found that almost 10% of study participants did not believe anyone would serve as a donor for them.42 In a large study examining racial disparities in kidney transplant access, Black ESKD patients were less willing to allow a living donor to volunteer as compared with White ESKD patients (21.0% vs. 39.5%, respectively), and this was associated with substantially reduced odds of evaluation completion, even after adjustment for several other factors.31 Finally, psychological burden, in particular expressions of guilt and remorse about health factors and behaviours, was identified as a key barrier from clinical chart review of ESKD patients who had been referred, but not transplanted.20
Knowledge-based Barriers
Inadequate transplant knowledge, including a lack of pre-ESKD nephrology care, continues to be a significant barrier to kidney transplant access, and has been shown to reduce referral11,48 and evaluation20,27,31,36,42,49 rates in multiple study populations across several US regions. Though transplant knowledge is considered here as a patient-level factor, the causes of inadequate transplant knowledge are typically upstream and thus solutions are likely to be needed at both system and provider levels, rather than at the patient-level alone.
Inadequate transplant knowledge, coupled with low health-related literacy,41,50 are commonly perceived as key barriers to early steps of kidney transplantation, particularly among racial and ethnic minority groups. For example, in a Colorado study among 167 haemodialysis patients, a lack of understanding of the benefits of kidney transplant was shown to be disproportionately higher among Black (43%) and Hispanic (42%) adults as compared with non-Hispanic Whites (10%).27 Similar results were found for understanding the kidney transplant process in this same study,27 and was identified as a key barrier to evaluation in a thematic analysis of 143 ESKD patients in Washington who were referred, but never transplanted.20 Lower access to kidney transplant education resources has also been cited as a key barrier among Black ESKD patients31 for which culturally appropriate educational interventions may serve as successful strategies to reduce racial disparities in kidney transplant access.
Provider-level Barriers
In total, 9 (27%) studies reported on provider-level barriers to referral or evaluation. These can largely be categorized into barriers related to miscommunication, provider perceptions and attitudes, and staff availability and experience.
Miscommunication
The most common provider-level barrier reported was miscommunication between patients and providers. In a study of 278 nephrologists, 38% believed that patient-physician communication was a very or moderately important reason for the observed racial differences in access to early steps of kidney transplant, though this was as high as 46% and 51% in Black and Asian/Pacific Islander physicians, respectively.51 In a purposive sample of 228 Black dialysis patients in Chicago, patients who get (vs. do not get) informational social support from their dialysis team were 63% (95%CI: 18%−25%) more likely to be seen at a kidney transplant center.44 In two qualitative studies, the importance of consistent patient-provider communication was emphasized by both patients and providers. Patients accessing the waitlist emphasized consistent communication as an enabling factor to timely kidney transplant access.36,49
Provider perceptions and attitudes
Three studies in our review described provider perception and attitudes as potential barriers to kidney transplant referral or evaluation. In 2016, the Southeastern Kidney Transplant Coalition, a multidisciplinary collaborative that advocates for increased access to kidney transplant in Georgia, North Carolina, and South Carolina, developed a survey to identify dialysis staff-reported barriers to transplant.52 In this survey of over 500 dialysis facility staff (primarily nurse managers and social workers), only 23% of staff perceived that >50% of their patients were eligible for a kidney transplant,52 despite previous research showing that less than 15% of patients have absolute medical contraindications to transplant.32,53 This same survey reported that even fewer (19%) providers perceived that patients were interested in a kidney transplant,52 though other studies have shown that more than 70% of ESKD patients are interested in a kidney transplant.54
In a survey among nephrologists in four US regions, physicians were less likely to believe kidney transplantation improves survival for Black patients than for White patients (69% vs. 89%, p=0.001), were similarly likely to believe it improves quality of life for each group (84% vs. 86%) as compared with dialysis therapy. Black physicians were non-significantly more likely than White or Asian/Pacific Islander physicians to believe kidney transplantation improves survival for Black patients.51 This study also showed that physicians viewed patients’ preferences and availability of living donors as the most important reasons why Black patients are less likely than White patients to be evaluated for kidney transplantation.51 Physician attitudes and beliefs, coupled with conscious or unconscious bias, are likely to directly influence the likelihood that they will (or will not) refer patients for transplant.
Among Black and White ESKD patients in Alabama, Southern California, Michigan and the mid-Atlantic region, having a physician who recommended kidney transplant (vs. not recommending transplant) was associated with a 119% (95%CI: 21% to 260%) increased odds of evaluation completion after adjustment for several patient and provider-level characteristics.24
Staff availability and experience
In a survey among 252 nephrologists, those with an academic affiliation had a 64% (95%CI: 34%−100%) higher likelihood of referral for kidney transplant among 19 hypothetical patients, while being more than ten years from fellowship was associated with a 36% (95%CI: 47%−22%) decreased likelihood of transplant recommendation in multivariate models.55 Attendance at national nephrology meetings, and urbanicity of provider practice were not associated with kidney transplant referral in the same study. In focus groups, perceived inaccessibility to staff was deemed a critical barrier to kidney transplant access by patients.49 In the broader landscape of patient care, lack of knowledge of the kidney transplant process by local patient care providers (i.e. general practitioners) has also been identified as a barrier to completing the evaluation process, with local providers often relying on their patients to inform them about the complex process.20
System-level Barriers
In total, 13 (39%) studies identified system-level barriers to referral or evaluation. These can largely be categorized into barriers related to dialysis facility, geography, distance to care, healthcare logistics, and neighborhood-level factors.
Dialysis Facility Factors
A 2021 study by McPherson et al.19 reported that dialysis patients in the Southeastern US were 16% less likely to be referred within 12-months of dialysis initiation (Hazard Ratio: 0.87, 95%CI: 0.80–0.88) if they were treated at a for-profit dialysis facility as compared with a non-profit dialysis facility after adjustment for multiple factors. However, once referred, there were no significant differences in initiating evaluation with 6-months (HR: 0.92, 95%CI: 0.83–1.03).19 Using the same data, Patzer et al.11 similarly concluded that dialysis facility for-profit status was associated with lower rates of referral, but not evaluation, and additionally reported that a lower patient to social worker ratio in dialysis facilities was associated with lower rates of referral and evaluation.
Among 241 dialysis facilities in Georgia, Plantinga et al.48 explored several dialysis-facility factors associated with patient referral for kidney transplantation within one year of dialysis initiation between 2005 and 2011. In fully adjusted models, high (vs. low) standardized kidney transplant ratio, high (vs. low) waitlisting rate, and high (vs. low) catheter use at 90 days were associated with increased odds of referral.48 Other dialysis facility factors (e.g. standardized mortality and hospital admission ratios, percent vaccinated, and urea reduction ratio) were not associated with referral rates.48
Using similar Georgia referral data from over 8,000 patients with ESKD, Paul et al. calculated a standardized transplantation referral ratio (STReR), a ratio of observed to expected kidney transplant referrals.37 The STReR ratio demonstrated significant variation in dialysis facility referral performance across Georgia, even after adjustment for differences in baseline patient characteristics (e.g. demographic and clinical factors), suggesting that a large part of the observed variance in facility performance is due to dialysis facility-level factors, such as for-profit status or patient-social worker ratio, rather than variation in the patient pool.37
Geography
Four studies in this review explored the relationship between geography and completion of referral25,43 and evaluation24,30 steps. Using data from five states and the District of Colombia (DC) between 1996 and 1997, Epstein et al. reported that living in Alabama, as compared to Michigan, Southern California, and Mid-Atlantic (Maryland, Virginia, DC) was a predictor of referral among people deemed appropriate kidney transplant candidates.25 In contrast, residence in Michigan and Alabama was a predictor of referral in those classified as inappropriate kidney transplant candidates.25 In the same cohort, residents of Alabama, Michigan, and Southern California had a 46%, 55%, and 51% reduced odds of completing evaluation, respectively, as compared with residents of Mid-Atlantic States in fully adjusted models.24 In Pennsylvania, dialysis patients living in Philadelphia County were 56% less likely to be referred compared with those in Allegheny County (Odds Ratio: 0.44, 95%CI: 0.21–0.90, p=0.024) in multivariable adjusted analyses.43 Finally, data from a single urban transplant center in Georgia demonstrated that degree of rurality was associated with a reduced odds of evaluation initiation, but not evaluation completion.30
Distance to Care
Distance to care, particularly among those in rural areas, may be a possible barrier to early kidney transplant steps. For example, there is some indication that the 262 US adult kidney transplant centers may not be as geographically widespread as the >7,000 dialysis facilities, and thus, they may be less accessible to referred patients on dialysis.1 Four studies in our review reported distance to a kidney transplant center as a possible barrier to referral and evaluation. Two studies reported that increased distance to a transplant center was associated with an increased odds of referral21,25 in unadjusted analyses. A 2020 study by McPherson et al.18 among almost 30,000 dialysis patients in Georgia, North Carolina, and South Carolina, reported that distance to a kidney transplant center was associated with referral or evaluation in unadjusted, but not adjusted, models similar to findings from a 2018 study among dialysis patients at a single kidney transplant center in Arizona.35 Collectively, these results, suggest that distance is unlikely to be the primary driving force in accessing these early steps in the kidney transplant process. It is likely that other unmeasured factors, such as travel time or transportation as reported in some studies in this review,28,36,42 may have a larger effect.
Healthcare Logistics
In one qualitative study of 30 patients and 23 providers, provider-identified barriers to evaluation at the institutional level included healthcare logistics (e.g. difficult finding a doctor’s office, finding parking) and kidney transplant-specific problems (e.g. scheduling difficulties, delayed referral, long wait time, limited access to transplant coordinators).36 These same barriers were identified by patients.
Neighborhood-level Factors
Dialysis patients residing in neighbourhoods with a higher (vs. lower) proportion of people living in poverty has been associated with reduced referral10,11 and evaluation11,30 after adjustment for several confounders, in multiple studies using data from the Southeastern US (Georgia, North Carolina, and South Carolina). This association is yet to be demonstrated in other US regions or for other neighborhood level factors.
Discussion
This is the first scoping review to summarize the available evidence on all non-medical barriers to kidney transplant referral and evaluation in the United States. A major limitation to a comprehensive assessment of the barriers to early kidney transplant steps remains the lack of national surveillance data on referral and evaluation rendering our reliance on published studies to inform our understanding. Despite this, among the 33 studies included in this review, we identified several barriers operating at multiple levels. Figure 312 is a pictorial representation of the interconnectedness of these patient, provider, and system-level factors, and demonstrates the importance of targeting multiple levels of the healthcare system to improve access to early steps to kidney transplantation. We acknowledge that these multi-level factors are not always mutually exclusive and that many barriers have upstream causes for which solutions should also be upstream. For example, though race is identified as a patient-level factor, systemic racism operating at multiple levels upstream of kidney transplant referral and evaluation contributes to the observed racial disparities we observe in kidney transplant access. Further, we acknowledge that this review convers a relatively large period, i.e., 1990 to 2018, in which nephrology and transplant practices, as well as national transplant access policies may have changed. Despite this, we believe the non-medical barriers considered in this review such as race and socioeconomic status, have remained relatively consisted over time and barriers reported in earlier years are likely to be still relevant today. Below, we discuss several possible interventions and policy-based solutions to improve referral and evaluation rates for kidney transplantation.
Figure 3.
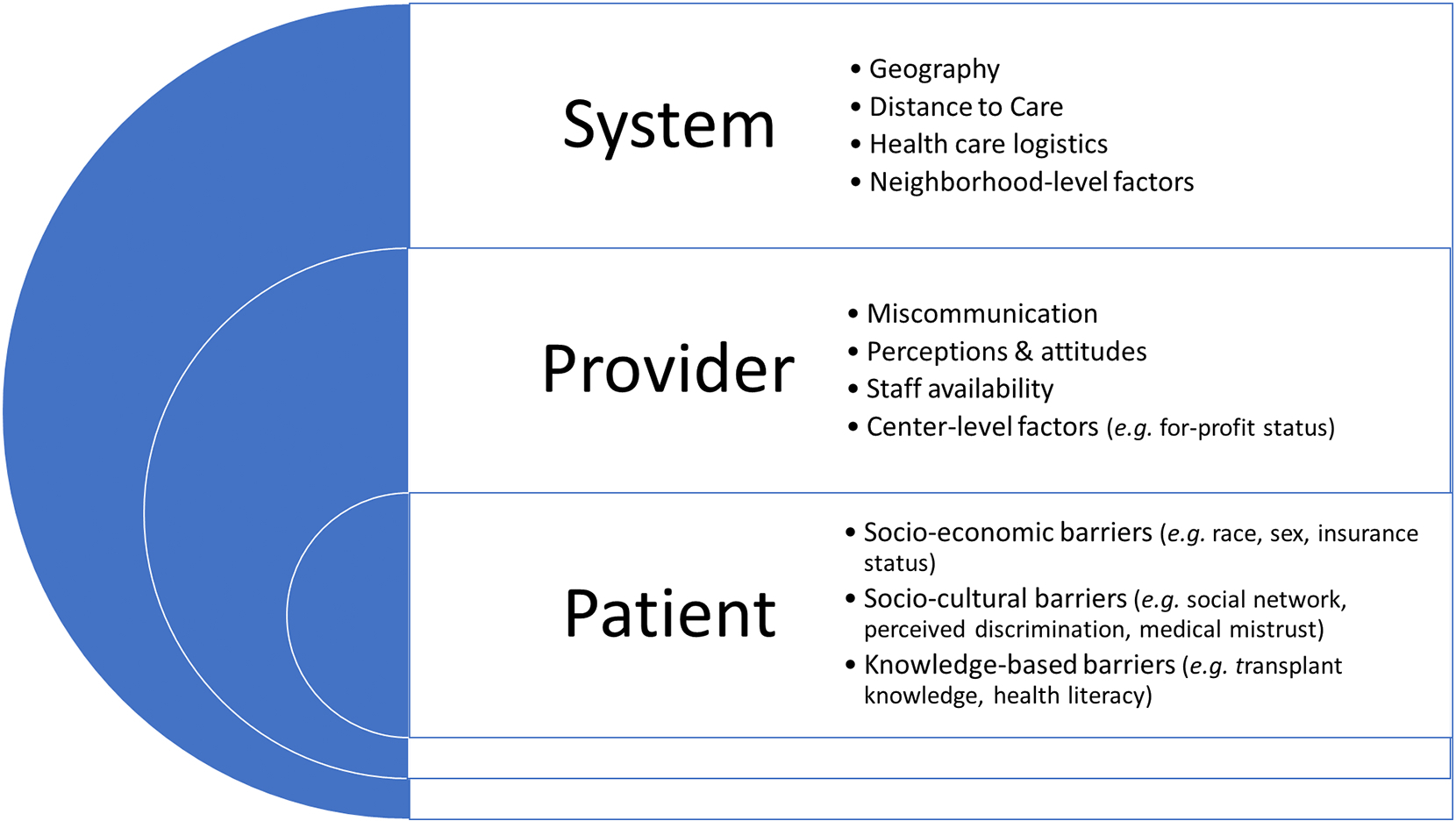
A summary of the key multi-level barriers identified to kidney transplant referral and evaluation in this review
Interventions
There are several targeted and system-wide interventions that may increase rates of referral and evaluation. First, regular screening of high-risk patients (e.g., patients with CKD) for kidney failure is needed and should be followed by referral of all patients to a nephrologist as early in the course of disease as possible. To reduce disparities in referral rates, screening tools for kidney failure should also no longer adjust for race.56 Removal (vs. inclusion) of race in eGFR has been associated with an increase in the proportion of Black adults diagnosed with chronic kidney disease (CKD) and later stages of CKD, which in turn leads to a higher rate of referral to specialist care and increased access to kidney disease education, including transplantation.56 Perhaps most importantly, removal of race from eGFR estimates is an important step in addressing historical misuse of race as a biological variable to further racism.56
Early access to education and information about kidney transplantation, including living donor transplantation, as early as possible in the transplant process (e.g. late-stage CKD patients) is also needed. Targeted interventions, specifically among Black patients, are being tested in practice,57,58 but systems-wide implementation is needed. Accumulating evidence has shown that multi-component education and quality improvement interventions at the kidney transplant program and dialysis facility-level can improve transplant access and reduce disparities in referral,59,60 waitlisting, and living donor transplant.61,62 For example, in a randomized, dialysis facility-based controlled trial involving more than 9000 patients across Georgia, Patzer et al. found that dialysis facilities receiving a kidney transplant education and engagement intervention were 75% more likely to refer patients for transplant within 12 months of dialysis initiation compared to facilities not receiving the intervention.60 Despite these promising findings, interventions have not been implemented nationally, and it is unclear how sustainable these interventions are in practice, though some short-term studies (~12 months) demonstrate sustainability and feasibility for dissemination across ESRD networks.59
Last, we need to increase awareness among referring healthcare providers that patient-centered educational information should be culturally tailored to patients’ needs. There is a pressing need for organizational culture and leadership to reflect these standards. For example, nephrology providers and dialysis organizations should have clear standards for kidney transplant education content, discussion, and timing.63 This may be facilitated by better capture of education provision on the medical evidence form (CMS2728) that is completed within 45 days of a patient beginning dialysis.
Policies
In recent years, several polices have aimed to increase access to kidney transplantation, discussed in detail by Patzer et al.64 For example, the Centers for Medicare and Medicaid Services (CMS) initiated a targeted goal to increase the number of waitlisted patients to 30% by 2023,65 and the July 2019 Advancing American Kidney Health Initiative Executive Order aims to double the number of kidney transplants by 2030 in part through new payment models to financially reward nephrologists and dialysis facilities for transplants.66 In December 2020, the US Congress passed the Immuno Bill to extend Medicare coverage of immunosuppressive medications for kidney transplant patients indefinitely,67 which is anticipated to improve transplant access as those who previously did not pursue transplant as a treatment option due to concerns about losing Medicare coverage may now be more likely to pursue a transplant.68 A mandatory CMS ESKD Treatment Choices model began in January 2021 and further incentivizes waitlisting through a modality performance score, which may lead to increased referrals for kidney transplantation.69 Finally, preliminary evidence suggests that Medicaid Expansion under the Affordable Care Act, introduced in 2010, is associated with an increase in the proportion of new pre-emptive listings for kidney transplantation with Medicaid coverage with greater benefit seen in racial and ethnic minority groups.70 While the impact of these collective policies is not yet clear, there is a potential that these could influence access to kidney transplantation. Future research will be essential to determine how these policies affect kidney transplant access at all steps, especially among underrepresented minority groups.
Second, quality metrics that focus on kidney transplant referral have been developed for both dialysis facilities37 and transplant centers,71 and national efforts through CMS72 and the Health Resources and Services Administration are actively focusing on developing new quality measures that could incentivize early transplant access. Quality metrics related to patient transplant education were also proposed by the ESRD Access to Kidney Transplant Expert Panel in 2015.73 These tools, that measure and compare transplant access between dialysis facilities and transplant centers against a national average, are a potentially valid and reliable metric that could be used as a clinical performance metric to evaluate early kidney transplant access. However, national data on referrals is needed to implement these quality metrics to ensure equitability in transplant access. In addition to quality metrics, standardized criteria for referral and evaluation across dialysis and transplant centers is needed. The current lack of transparency in patient evaluation and selection (e.g., a patient may be eligible at one center but not another) is likely a barrier to patients completing the earlier steps to kidney transplant.20
Finally, some members of the kidney transplant community have also advocated for an “Opt-Out” model for transplant referral.74 In this proposed system, patients are automatically referred to a transplant center for evaluation if they meet basic eligibility criteria developed by the transplant community. Patients would be systematically referred unless they opt out explicitly.74 Advocates for this model suggest that creating the default as “transplant referral” stands to improve access to information about the procedure though whether this approach would reduce barriers before or after referral is not clear.75
Conclusion
This review highlights several patient, provider, and system-level factors associated with lower rates of kidney transplant referral and evaluation in the United States. A multi-pronged approach (e.g. targeted and systemwide interventions, and policy change) implemented at multiple levels of the healthcare system will be necessary to improve equitable access to early transplant steps. Collection of national surveillance data on early kidney transplant steps, as well as routinely captured data on upstream social determinants of health, including the measurement of racism rather than race, will also be necessary to enhance our understanding of barriers to kidney transplant referral and evaluation.
Supplementary Material
Highlights.
Non-medical barriers to kidney transplant exist at referral and evaluation steps
Barriers are multi-level, operating at individual, provider, and system-levels
A multi-pronged approach is needed to improve equitable access to early transplant steps
Funding
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities grants U01MD010611 and R01DK122701. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of interest
Kylie Snow is currently employed by Booz Allen Hamilton.
‘Declarations of interest: none’.
Data availability
Not applicable
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.United States Renal Data System. USRDS Annual Data Report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2020. [Google Scholar]
- 2.Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 2011;11(10):2093–109. doi: 10.1111/j.1600-6143.2011.03686.x [published Online First: 2011/09/03] [DOI] [PubMed] [Google Scholar]
- 3.Alexander GC, Sehgal AR. Barriers to cadaveric renal transplantation among blacks, women, and the poor. JAMA 1998;280(13):1148–52. doi: 10.1001/jama.280.13.1148 [published Online First: 1998/10/20] [DOI] [PubMed] [Google Scholar]
- 4.Alexander GC, Sehgal AR, Transplant Task Force of The Renal Network I. Variation in access to kidney transplantation across dialysis facilities: using process of care measures for quality improvement. Am J Kidney Dis 2002;40(4):824–31. doi: 10.1053/ajkd.2002.35695 [published Online First: 2002/09/27] [DOI] [PubMed] [Google Scholar]
- 5.Patzer RE, Amaral S, Wasse H, et al. Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol 2009;20(6):1333–40. doi: 10.1681/ASN.2008030335 [published Online First: 2009/04/03] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tong A, Hanson CS, Chapman JR, et al. The preferences and perspectives of nephrologists on patients’ access to kidney transplantation: a systematic review. Transplantation 2014;98(7):682–91. doi: 10.1097/TP.0000000000000336 [published Online First: 2014/08/15] [DOI] [PubMed] [Google Scholar]
- 7.Navaneethan SD, Aloudat S, Singh S. A systematic review of patient and health system characteristics associated with late referral in chronic kidney disease. BMC Nephrol 2008;9:3. doi: 10.1186/1471-2369-9-3 [published Online First: 2008/02/27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harding JLPA, Patzer RE. Non-Medical Barriers to Early Steps in Kidney Transplantation Among Underrepresented Groups in the United States. Current Opinions in Organ Transplantation 2021;[In Press] [DOI] [PubMed] [Google Scholar]
- 9.Lockwood MB, Bidwell JT, Werner DA, et al. Non-Biological Barriers to Referral and the Pre-Kidney Transplant Evaluation Among African Americans in the United States: A Systematic Review. Nephrol Nurs J 2016;43(3):225–38; quiz 39. [published Online First: 2016/08/10] [PubMed] [Google Scholar]
- 10.Patzer RE, Plantinga LC, Paul S, et al. Variation in Dialysis Facility Referral for Kidney Transplantation Among Patients With End-Stage Renal Disease in Georgia. JAMA 2015;314(6):582–94. doi: 10.1001/jama.2015.8897 [published Online First: 2015/08/12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patzer RE, McPherson L, Wang Z, et al. Dialysis facility referral and start of evaluation for kidney transplantation among patients treated with dialysis in the Southeastern United States. Am J Transplant 2020;20(8):2113–25. doi: 10.1111/ajt.15791 [published Online First: 2020/01/26] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patzer RE, Gander J, Sauls L, et al. The RaDIANT community study protocol: community-based participatory research for reducing disparities in access to kidney transplantation. BMC Nephrol 2014;15:171. doi: 10.1186/1471-2369-15-171 [published Online First: 2014/10/29] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018;169(7):467–73. doi: 10.7326/M18-0850 [published Online First: 2018/09/05] [DOI] [PubMed] [Google Scholar]
- 14.National Institute on Minority Health and Health Disparities. NIMHD Research Framework. 2017. [Available from: https://www.nimhd.nih.gov/about/overview/research-framework.html accessed 16 September 2021. [Google Scholar]
- 15.Pace R, Pluye P, Bartlett G, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012;49(1):47–53. doi: 10.1016/j.ijnurstu.2011.07.002 [published Online First: 2011/08/13] [DOI] [PubMed] [Google Scholar]
- 16.Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health 2014;35:29–45. doi: 10.1146/annurev-publhealth-032013-182440 [published Online First: 2013/11/06] [DOI] [PubMed] [Google Scholar]
- 17.Hong QNPP, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O’Cathain A, Rousseau M-C, Vedel I. Mixed Methods Appraisal Tool (MMAT). Registration of Copyright (#1148552), Canadian Intellectual Property Office, Industry Canada, 2018. [Google Scholar]
- 18.McPherson LJ, Barry V, Yackley J, et al. Distance to Kidney Transplant Center and Access to Early Steps in the Kidney Transplantation Process in the Southeastern United States. Clin J Am Soc Nephrol 2020;15(4):539–49. doi: 10.2215/CJN.08530719 [published Online First: 2020/03/27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McPherson LJ, Walker ER, Lee YH, et al. Dialysis Facility Profit Status and Early Steps in Kidney Transplantation in the Southeastern United States. Clin J Am Soc Nephrol 2021. doi: 10.2215/CJN.17691120 [published Online First: 2021/05/28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Butler CR, Taylor JS, Reese PP, et al. Thematic analysis of the medical records of patients evaluated for kidney transplant who did not receive a kidney. BMC Nephrol 2020;21(1):300. doi: 10.1186/s12882-020-01951-1 [published Online First: 2020/07/28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patzer RE, McClellan WM. Influence of race, ethnicity and socioeconomic status on kidney disease. Nat Rev Nephrol 2012;8(9):533–41. doi: 10.1038/nrneph.2012.117 [published Online First: 2012/06/28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Comstock RD, Castillo EM, Lindsay SP. Four-year review of the use of race and ethnicity in epidemiologic and public health research. Am J Epidemiol 2004;159(6):611–9. doi: 10.1093/aje/kwh084 [published Online First: 2004/03/09] [DOI] [PubMed] [Google Scholar]
- 23.Ayanian JZ, Cleary PD, Weissman JS, et al. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med 1999;341(22):1661–9. doi: 10.1056/NEJM199911253412206 [published Online First: 1999/11/26] [DOI] [PubMed] [Google Scholar]
- 24.Clark CR, Hicks LS, Keogh JH, et al. Promoting access to renal transplantation: the role of social support networks in completing pre-transplant evaluations. J Gen Intern Med 2008;23(8):1187–93. doi: 10.1007/s11606-008-0628-7 [published Online First: 2008/05/15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation--clinically appropriate or due to underuse or overuse? N Engl J Med 2000;343(21):1537–44, 2 p preceding 37. doi: 10.1056/NEJM200011233432106 [published Online First: 2000/11/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gander JC, Zhang X, Plantinga L, et al. Racial disparities in preemptive referral for kidney transplantation in Georgia. Clin Transplant 2018;32(9):e13380. doi: 10.1111/ctr.13380 [published Online First: 2018/08/14] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones D, You Z, Kendrick JB. Racial/Ethnic Differences in Barriers to Kidney Transplant Evaluation among Hemodialysis Patients. Am J Nephrol 2018;47(1):1–7. doi: 10.1159/000484484 [published Online First: 2017/12/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lockwood MB, Saunders MR, Nass R, et al. Patient-Reported Barriers to the Prekidney Transplant Evaluation in an At-Risk Population in the United States. Prog Transplant 2017;27(2):131–38. doi: 10.1177/1526924817699957 [published Online First: 2017/06/16] [DOI] [PubMed] [Google Scholar]
- 29.Monson RS, Kemerley P, Walczak D, et al. Disparities in completion rates of the medical prerenal transplant evaluation by race or ethnicity and gender. Transplantation 2015;99(1):236–42. doi: 10.1097/TP.0000000000000271 [published Online First: 2014/12/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patzer RE, Perryman JP, Schrager JD, et al. The role of race and poverty on steps to kidney transplantation in the Southeastern United States. Am J Transplant 2012;12(2):358–68. doi: 10.1111/j.1600-6143.2011.03927.x [published Online First: 2012/01/12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Waterman AD, Peipert JD, Hyland SS, et al. Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol 2013;8(6):995–1002. doi: 10.2215/CJN.08880812 [published Online First: 2013/03/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weng FL, Joffe MM, Feldman HI, et al. Rates of completion of the medical evaluation for renal transplantation. Am J Kidney Dis 2005;46(4):734–45. doi: 10.1053/j.ajkd.2005.06.011 [published Online First: 2005/09/27] [DOI] [PubMed] [Google Scholar]
- 33.Wong LL, Kindle K, Limm B. Racial disparities in Pacific Islanders undergoing renal transplant evaluation. Hawaii Med J 2009;68(2):30–3. [published Online First: 2009/04/24] [PubMed] [Google Scholar]
- 34.Sequist TD, Narva AS, Stiles SK, et al. Access to renal transplantation among American Indians and Hispanics. Am J Kidney Dis 2004;44(2):344–52. doi: 10.1053/j.ajkd.2004.04.039 [published Online First: 2004/07/21] [DOI] [PubMed] [Google Scholar]
- 35.Keddis MT, Sharma A, Ilyas M, et al. Transplant center assessment of the inequity in the kidney transplant process and outcomes for the Indigenous American patients. PLoS One 2018;13(11):e0207819. doi: 10.1371/journal.pone.0207819 [published Online First: 2018/11/22] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nonterah CW, Gardiner HM. Pre-transplant evaluation completion for Black/African American renal patients: Two theoretical frameworks. Patient Educ Couns 2020;103(5):988–98. doi: 10.1016/j.pec.2019.11.005 [published Online First: 2019/11/18] [DOI] [PubMed] [Google Scholar]
- 37.Paul S, Plantinga LC, Pastan SO, et al. Standardized Transplantation Referral Ratio to Assess Performance of Transplant Referral among Dialysis Facilities. Clin J Am Soc Nephrol 2018;13(2):282–89. doi: 10.2215/CJN.04690417 [published Online First: 2018/01/27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Segev DL, Kucirka LM, Oberai PC, et al. Age and comorbidities are effect modifiers of gender disparities in renal transplantation. J Am Soc Nephrol 2009;20(3):621–8. doi: 10.1681/ASN.2008060591 [published Online First: 2009/01/09] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melk A, Babitsch B, Borchert-Morlins B, et al. Equally Interchangeable? How Sex and Gender Affect Transplantation. Transplantation 2019;103(6):1094–110. doi: 10.1097/TP.0000000000002655 [published Online First: 2019/02/13] [DOI] [PubMed] [Google Scholar]
- 40.Schold JD, Gregg JA, Harman JS, et al. Barriers to evaluation and wait listing for kidney transplantation. Clin J Am Soc Nephrol 2011;6(7):1760–7. doi: 10.2215/CJN.08620910 [published Online First: 2011/05/21] [DOI] [PubMed] [Google Scholar]
- 41.Dageforde LA, Box A, Feurer ID, et al. Understanding Patient Barriers to Kidney Transplant Evaluation. Transplantation 2015;99(7):1463–9. doi: 10.1097/TP.0000000000000543 [published Online First: 2015/01/22] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kazley AS, Simpson KN, Chavin KD, et al. Barriers facing patients referred for kidney transplant cause loss to follow-up. Kidney Int 2012;82(9):1018–23. doi: 10.1038/ki.2012.255 [published Online First: 2012/07/27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCauley J, Irish W, Thompson L, et al. Factors determining the rate of referral, transplantation, and survival on dialysis in women with ESRD. Am J Kidney Dis 1997;30(6):739–48. doi: 10.1016/s0272-6386(97)90077-9 [published Online First: 1997/12/16] [DOI] [PubMed] [Google Scholar]
- 44.Browne T. The relationship between social networks and pathways to kidney transplant parity: evidence from black Americans in Chicago. Soc Sci Med 2011;73(5):663–7. doi: 10.1016/j.socscimed.2011.06.031 [published Online First: 2011/08/02] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Institute of Medicine (US) Committee on Assessing Interactions Among Social B, and Genetic Factors in Health,. The Impact of Social and Cultural Environment on Health. In: Hernandez LMBD, ed. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. Washington (DC): National Academies Press (US) 2006. [PubMed] [Google Scholar]
- 46.Hamoda RE, McPherson LJ, Lipford K, et al. Association of sociocultural factors with initiation of the kidney transplant evaluation process. Am J Transplant 2020;20(1):190–203. doi: 10.1111/ajt.15526 [published Online First: 2019/07/07] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gillespie A, Fink EL, Traino HM, et al. Hemodialysis Clinic Social Networks, Sex Differences, and Renal Transplantation. Am J Transplant 2017;17(9):2400–09. doi: 10.1111/ajt.14273 [published Online First: 2017/03/21] [DOI] [PubMed] [Google Scholar]
- 48.Plantinga LC, Pastan SO, Wilk AS, et al. Referral for Kidney Transplantation and Indicators of Quality of Dialysis Care: A Cross-sectional Study. Am J Kidney Dis 2017;69(2):257–65. doi: 10.1053/j.ajkd.2016.08.038 [published Online First: 2016/11/25] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Crenesse-Cozien N, Dolph B, Said M, et al. Kidney Transplant Evaluation: Inferences from Qualitative Interviews with African American Patients and their Providers. J Racial Ethn Health Disparities 2019;6(5):917–25. doi: 10.1007/s40615-019-00592-x [published Online First: 2019/04/26] [DOI] [PubMed] [Google Scholar]
- 50.Grubbs V, Gregorich SE, Perez-Stable EJ, et al. Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol 2009;4(1):195–200. doi: 10.2215/CJN.03290708 [published Online First: 2008/12/06] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ayanian JZ, Cleary PD, Keogh JH, et al. Physicians’ beliefs about racial differences in referral for renal transplantation. Am J Kidney Dis 2004;43(2):350–7. doi: 10.1053/j.ajkd.2003.10.022 [published Online First: 2004/01/30] [DOI] [PubMed] [Google Scholar]
- 52.Browne T, Patzer RE, Gander J, et al. Kidney transplant referral practices in southeastern dialysis units. Clin Transplant 2016;30(4):365–71. doi: 10.1111/ctr.12693 [published Online First: 2016/01/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kianda MN, Wissing KM, Broeders NE, et al. Ineligibility for renal transplantation: prevalence, causes and survival in a consecutive cohort of 445 patients. Clin Transplant 2011;25(4):576–83. doi: 10.1111/j.1399-0012.2010.01317.x [published Online First: 2010/08/20] [DOI] [PubMed] [Google Scholar]
- 54.Browne T, Amamoo A, Patzer RE, et al. Everybody needs a cheerleader to get a kidney transplant: a qualitative study of the patient barriers and facilitators to kidney transplantation in the Southeastern United States. BMC Nephrol 2016;17(1):108. doi: 10.1186/s12882-016-0326-3 [published Online First: 2016/08/01] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tandon A, Wang M, Roe KC, et al. Nephrologists’ likelihood of referring patients for kidney transplant based on hypothetical patient scenarios. Clin Kidney J 2016;9(4):611–5. doi: 10.1093/ckj/sfw031 [published Online First: 2016/08/02] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Diao JA, Wu GJ, Taylor HA, et al. Clinical Implications of Removing Race From Estimates of Kidney Function. JAMA 2021;325(2):184–86. doi: 10.1001/jama.2020.22124 [published Online First: 2020/12/03] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cabacungan AN, Diamantidis CJ, St Clair Russell J, et al. Development of a Telehealth Intervention to Improve Access to Live Donor Kidney Transplantation. Transplant Proc 2019;51(3):665–75. doi: 10.1016/j.transproceed.2018.12.032 [published Online First: 2019/04/14] [DOI] [PubMed] [Google Scholar]
- 58.Patzer RE, McPherson L, Redmond N, et al. A Culturally Sensitive Web-based Intervention to Improve Living Donor Kidney Transplant Among African Americans. Kidney Int Rep 2019;4(9):1285–95. doi: 10.1016/j.ekir.2019.05.771 [published Online First: 2019/09/14] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hamoda RE, Gander JC, McPherson LJ, et al. Process evaluation of the RaDIANT community study: a dialysis facility-level intervention to increase referral for kidney transplantation. BMC Nephrol 2018;19(1):13. doi: 10.1186/s12882-017-0807-z [published Online First: 2018/01/18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Patzer RE, Paul S, Plantinga L, et al. A Randomized Trial to Reduce Disparities in Referral for Transplant Evaluation. J Am Soc Nephrol 2017;28(3):935–42. doi: 10.1681/ASN.2016030320 [published Online First: 2016/10/16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Waterman AD, Peipert JD, Cui Y, et al. Your Path to Transplant: A randomized controlled trial of a tailored expert system intervention to increase knowledge, attitudes, and pursuit of kidney transplant. Am J Transplant 2021;21(3):1186–96. doi: 10.1111/ajt.16262 [published Online First: 2020/11/28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Weng FL, Davis LA, Ohman-Strickland PA, et al. Destination Transplant: Protocol for a Parallel-group Randomized Trial of an Educational Intervention to Increase Kidney Transplant Among Black People on the Transplant Waiting List. Transplant Direct 2021;7(4):e683. doi: 10.1097/TXD.0000000000001136 [published Online First: 2021/03/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Koch-Weser S, Porteny T, Rifkin DE, et al. Patient Education for Kidney Failure Treatment: A Mixed-Methods Study. Am J Kidney Dis 2021. doi: 10.1053/j.ajkd.2021.02.334 [published Online First: 2021/04/25] [DOI] [PubMed] [Google Scholar]
- 64.Patzer RE, Pastan SO. Policies to promote timely referral for kidney transplantation. Semin Dial 2020;33(1):58–67. doi: 10.1111/sdi.12860 [published Online First: 2020/01/21] [DOI] [PubMed] [Google Scholar]
- 65.IPRO. 2018. CMS statement of work for ESRD networks 2018 [Available from: https://esrd.ipro.org/wp-content/uploads/2017/11/2017-10-30-Statement-of-Work.pdf accessed 24 June 2021.
- 66.Hippen BE, Reed AI, Ketchersid T, et al. Implications of the Advancing American Kidney Health Initiative for kidney transplant centers. Am J Transplant 2020;20(5):1244–50. doi: 10.1111/ajt.15619 [published Online First: 2019/09/29] [DOI] [PubMed] [Google Scholar]
- 67.American Society of Transplantation. Immuno Bill passes after 20 years 2020. [Available from: https://www.myast.org/about-ast/presidents-blog/immuno-bill-passes-after-20-years# accessed 24 June 2021.
- 68.Grubbs V, Plantinga LC, Vittinghoff E, et al. Medicare immunosuppressant coverage and access to kidney transplantation: a retrospective national cohort study. BMC Health Serv Res 2012;12:254. doi: 10.1186/1472-6963-12-254 [published Online First: 2012/08/17] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Centers for Medicare & Medicaid Services. End-Stage Renal Disease Treatment Choices (ETC) model fact sheet 2020. [Available from: https://www.cms.gov/newsroom/fact-sheets/endstage-renal-disease-treatment-choices-etc-model-fact-sheet. accessed 24 June 2021.
- 70.Harhay MN, McKenna RM, Boyle SM, et al. Association between Medicaid Expansion under the Affordable Care Act and Preemptive Listings for Kidney Transplantation. Clin J Am Soc Nephrol 2018;13(7):1069–78. doi: 10.2215/CJN.00100118 [published Online First: 2018/06/23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Paul S, Melanson T, Mohan S, et al. Kidney transplant program waitlisting rate as a metric to assess transplant access. Am J Transplant 2021;21(1):314–21. doi: 10.1111/ajt.16277 [published Online First: 2020/08/19] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Centers for Medicare and Medicaid Services. Technical Expert Panel Charter: Practitioner Level Measurement of Effective Access to Kidney Transplantation 2020. [Available from: https://www.cms.gov/files/document/measurement-effective-access-kidney-transplantation-practitioner-level-tep-charter.pdf accessed 24 June 2021.
- 73.CMS Technical Expert Panel. Access to kidney transplantation TEP summary report 2015. [Available from: https://www.dialysisdata.org/sites/default/files/content/ESRD_Measures/Access_To_Kidney_Transplantation_TEP_Summary_Report.pdf accessed 1 July 2021.
- 74.Huml AM, Sedor JR, Poggio E, et al. An opt-out model for kidney transplant referral: The time has come. Am J Transplant 2021;21(1):32–36. doi: 10.1111/ajt.16129 [published Online First: 2020/06/11] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Davidai S, Gilovich T, Ross LD. The meaning of default options for potential organ donors. Proc Natl Acad Sci U S A 2012;109(38):15201–5. doi: 10.1073/pnas.1211695109 [published Online First: 2012/09/06] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.