Abstract
Diabetic retinopathy (DR) complications can be prevented with regular screening and timely access to an ophthalmologist for treatment. But there are patient and health system barriers that can impact access to DR services. This study aims to identify enablers and barriers for accessing public DR eye care services in a low socio-economic urban area of Australia. We conducted a qualitative study using semi-structured interviews for patients with diabetes aged 35 years and older attending public ophthalmology services. Interviews were analyzed to identify themes and subthemes; and the COM-B framework was used to interpret the complex behavioral mechanisms, including capability, opportunity, and motivation factors, to explain adherence to DR eye care. Three main themes and 7 sub-themes relating to patient experiences of DR care were derived. Patients were found to be passive actors in their DR eye care, but patients trusted clinicians and were determined to maintain their vision and quality of life. The barriers and facilitators of care related to the health system (service availability and recall–reminder systems) and patient experiences (choices, knowledge, and fear). The findings of this study will guide patient-centered initiatives to target and improve access to DR care. Strategies should focus on improving communication between eye care providers, and communication with patients to empower them to become more active players in healthcare decisions.
Keywords: Diabetic retinopathy, patient experience, patient-centered health systems
Introduction
Diabetic retinopathy (DR) is an ocular complication affecting one-third of people with diabetes (1) and is responsible for 9% of vision loss in Australia (2). Regular eye examinations are recommended to detect disease (3), and prompt referral to specialists (ophthalmologists) for sight-saving treatment (3). In Australia, such examinations are available free of charge or at a subsidized cost for patients under the national health insurance scheme (Medicare Australia) (4). Despite this, there are gaps in the utilization of eye care among people with diabetes in Australia. In the 2015−2016 National Eye Health survey, 78% of non-Indigenous and 53% of Indigenous Australians with diabetes self-reported adherence to the recommended intervals for retinal examinations (5). However, a large cohort study examining Medicare Australia claims over 10 years (2006-2016), found that only half of the people with diabetes had accessed a biennial eye examination, and among those with diabetes for longer than 10 years only 20% were adherent to recommended screening intervals (6). Poor attendance at screening has been linked with worse health outcomes later on, with one study finding that patients requiring treatment for DR with laser coagulation were less likely to have attended an appointment with a general practitioner (GP) or specialist over the preceding 7-years, compared to those not receiving treatments (7).
Identifying patients who are non-adherent to eye examinations can guide initiatives to target and improve access to care. In one Australian study, it was found that patients non-adherent to screening were more likely to be born overseas, non-English speaking, or have higher body mass index, as well as higher education or income levels than those who adhered (6). In the current international literature, studies tend to focus on patient adherence to national DR screening programs which are delivered in primary care or hospital outpatient departments (8). Two recent systematic reviews (9,10) have identified barriers and facilitators of screening adherence. Barriers to obtaining services were found to include the patients’ fears of vision loss or treatments, or low DR health literacy; inaccessibility of services, such as clinic location, transport, costs, and convenience of appointment times; and health system factors, such as the use of referral and reminder systems, the availability of eye workforce, long wait-times and availability of appointments, and integration of DR screening with other services. In Australia, Lake et al (11) interviewed young adults with type 2 diabetes finding that the key facilitators to adherence were receiving a recommendation from a health professional followed by the patients’ beliefs about health negative consequences; while reported barriers were similar to those outlined above, specifically costs, life constraints, and low perception of risk. Glasson et al (12) have also assessed the experiences of Australian patients attending a remote telehealth DR screening program, finding that access was improved through the proximity of services to the patient, reduced travel costs, less time off work, and familiarity with local staff.
Despite DR being a progressive and chronic disease, few studies have investigated patient adherence for DR eye care beyond screening. One study from the United States assessed non-adherence at follow-up appointments, finding that one-third of DR patients missed or failed to reschedule their appointment within the recommended timeframes. Factors associated with non-adherence at follow-up (among patients with chronic eye disease) were found to be long wait times, difficulties rescheduling, financial barriers, taking time away from home or work duties, and having no escort to accompany them to an appointment (13). In Australia, gaps in the utilization of ophthalmologist services among patients referred for management of DR have also been reported (6,12,14). For example, a recent audit of public hospital records in western Sydney found that only 59% of patients newly referred for a DR consultation attended the first booked appointment, with 22% failing to reschedule or attend at all (14). However, across the literature, the reasons for non-adherence at DR services among patients requiring ongoing monitoring and treatments at the tertiary level have rarely been explored. Therefore, this study begins to fill this research gap by considering patient experiences and adherence to DR care along the care continuum (from screening to treatments) and aims to identify enablers and barriers for accessing public eye care services for DR care in a low socio-economic urban area of Australia.
Methods
Setting
This study was conducted in Western Sydney, a large metropolitan region in NSW Australia with a rate of diabetes mellitus that is 1.4 to 1.8 times higher than the national average (15). In Australia, guidelines recommend people with diabetes receive a comprehensive eye examination at least every 2-years or more frequently if they have higher risk factors (3,16). When DR is detected at (or above) a moderate level, patients should be seen by an ophthalmologist for management and sight-saving treatment (3). Patients can access examinations and some treatments for no cost in primary care (optometrist and GP) and public hospitals (ophthalmologists) (4). Patients may choose to attend private ophthalmology clinics, where costs are partially covered by Medicare Australia and the remainder paid by the patients. Additional costs are subject to the Medicare safety net which limits out-of-pocket costs for patients (17).
This study was conducted at several public-funded eye care services in the region where patients with DR were receiving free care under the guidance of an ophthalmologist. The services included:
One tertiary public hospital ophthalmology department.
- Two clinics providing services to hospital patients under a service agreement:
- A community-based optometry clinic delivering a collaborative model of care for low-grade DR through Medicare, with no out-of-pocket costs (18).
- An ophthalmology practice delivering DR treatments (ie, anti-VEGF injections and laser treatment) through Medicare, with no out-of-pocket costs.
Participant Sampling and Recruitment
Patients were eligible to participate if they were attending a scheduled appointment in a DR clinic, including both new referrals and follow-up appointments; aged 35 years and older; and could read and converse in English. Participants were identified by reviewing clinic booking lists, or by nomination from the attending clinician. Eligible patients were approached in the clinic waiting room. Those providing written informed consent were given an option to complete the interview either face-to-face in a private area of the clinic while they waited or at the completion of their appointment, or over the phone later at a convenient time. Participants were recruited across eye care settings, with one researcher moving between the various DR clinics.
Data Collection
A semi-structured interview was designed to capture the patients’ eye care journey, starting with their diagnosis of diabetes, eye screening, up until the current appointment. Questions drew on patients’ current experiences, as well as their knowledge and broader perceptions about eye care. The interview schedule was informed by concepts arising in the published literature (Supplemental 1). Interviews were conducted by one researcher (BF) and audio recorded. Interviews were expected to last 15 to 30 min to ensure the patient was not inconvenienced, if longer, participants were asked if they were happy to continue. Interviews were conducted until thematic saturation was reached.
Reflexivity
The interviews were conducted at the clinics on the same day that the patients were receiving care, and the interviewer (BF) was a former employee of the hospital, not involved directly in patient care but occasionally during the interviews used a collective term of “we” to describe hospital staff or services. This context may have influenced participants comfort and willingness to respond openly, but they were regularly reminded that all responses, even if negative, were held in confidence and would not be shared with the attending clinicians. Additionally, the research team has a range of expertise including ophthalmology, optometry, health policy, and administration. None of the research team has a personal experience of living with DR. Thus, throughout data collection and analyses there was a need to reflect on the professional bias of the research team when attempting to understand the patient experience.
Analysis
Audio files from the initial 3 interviews were transcribed verbatim (by BF) and discussed amongst 3 researchers (BF, BA, HL) to further refine the interview questions and prompt to gain richer data in subsequent interviews. At the completion of data collection, the remaining audio files were transcribed verbatim by 3 researchers (BF, AD, SH) and uploaded into NVIVO 12 for analysis. An initial coding tree was developed based on existing literature relating to DR screening (Supplemental 2). Three researchers (BF, AD, SH) initially coded 2 interviews each, then discussed the coding framework and added additional codes informed by the interviews. The remaining transcripts were split evenly for coding, with a crossover of several transcripts for triangulation. As the first stage of analysis, themes and subthemes which emerged during the coding were documented during group discussions, and illustrative quotes were recorded.
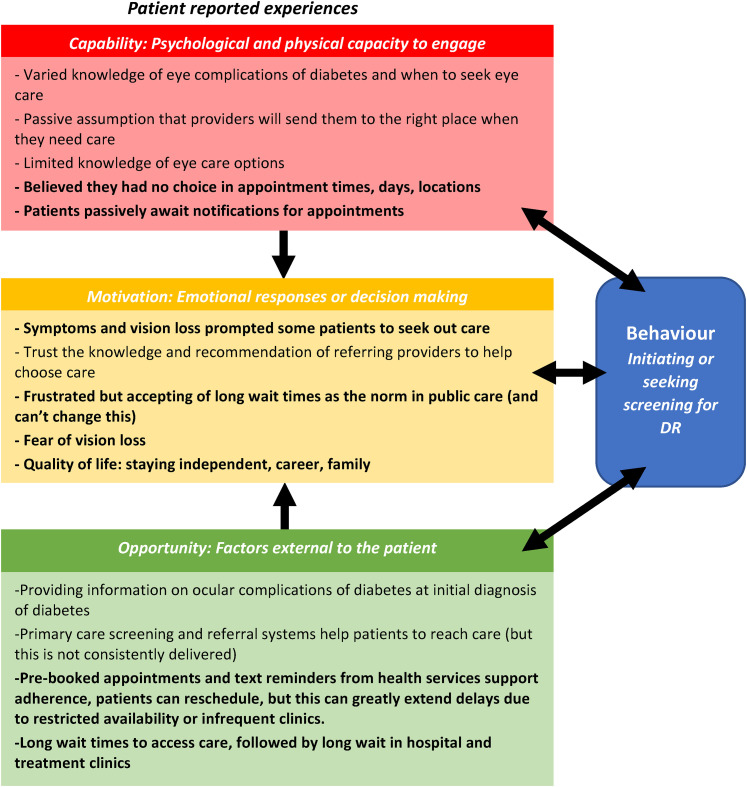
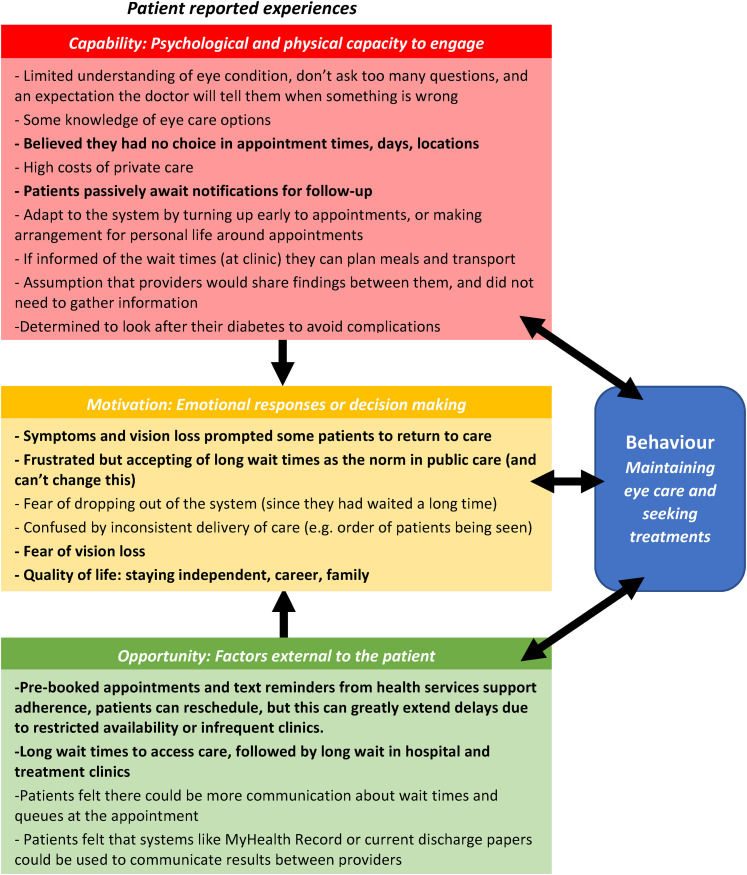
COM-B System Framework
At the second stage of analysis, the Michie et al (19) COM-B framework was adopted to identify and interpret the complex behavioral mechanisms involved in patients adherence to DR eye care. COM-B (19) suggests that health-seeking behaviors are influenced at the patient level through (i) psychological and physical capacity to engage with care (capability), (ii) emotional responses or decision making (motivation), or (iii) external factors (opportunity) which prompt or support patients to seek care (19). The themes and subthemes identified in the thematic analysis were reviewed to identify capability, opportunity, and motivation factors which were then mapped onto the COM-B diagram.
The health-seeking behaviors of interest in this study included:
initiation of eye care, for example, seeking DR screening in primary care, presentation at emergency departments, and initial referrals to tertiary care,
maintaining eye care, for example, routine attendance at screening, and review/treatment appointments for DR.
Ethics
This study received ethical approval from the South Eastern Sydney Local Health District Human Research Ethics Committee (reference 15/053-LNR/POWH/120) and site-specific approval by the WSLHD Research governance office (reference LNRSSA-15-WMEAD-225). The study was performed in accordance with the principles of the Declaration of Helsinki.
Results
Participants and Settings
Interviews were conducted with 15 patients attending the 3 eye services for the management of DR. The socio-demographic characteristics of participants are presented in Table 1. Most participants were male, overseas-born, and retired. Half spoke English as a primary language. The average age was 69 years, with a range of 37 to 80 years. Almost half were attending hospital clinics, with the remainder equally split between the collaborative care and treatment clinics.
Table 1.
Socio-Demographic Characteristics of Participants Attending Eye Services for Diabetic Retinopathy.
| Demographics | % | |
|---|---|---|
| Age | Median (range) | 69 (37-80 years) |
| Gender | Male | 73% |
| Ethnicity | Non-Indigenous | 27% |
| Other ethnicities (Armenian, Chinese, Croatian, English, Fijian, Indian, Singapore, South Korea, Sri Lanka, Ukraine, Vietnamese) | 73% | |
| Primary language spoken | English | 53% |
| English and another language (Fijian, Croatian, Hokien, Armenian) | 27% | |
| Another primary language (Singalet, Vietnamese, Korean) | 20% | |
| Level of education | None/primary school | 13% |
| High school | 40% | |
| Trade or certificate | 13% | |
| University | 33% | |
| Health insurance status | Private health insurance | 40% |
| No private health insurance | 60% | |
| Employment | Employed/self-employed | 27% |
| Retired | 67% | |
| Student | 7% | |
| Clinic type | Hospital | 46% |
| Private treatment clinic | 27% | |
| Community eye care clinic | 27% | |
Themes Relating to Patient Experiences of DR Eye Care
Three main themes and an additional 7 subthemes relating to the patient experience of DR care were derived (Table 2). Themes and subthemes are described below and supporting quotes are provided in Table 2.
-
The health system facilitates movement through the eye care pathway, patients passively accept this but are not in control.
The first theme and 3 subthemes suggest that free eye care, in this setting, has a top-down approach that guides patients through the various stages of eye care (eg, screening, referral). Patients were not in control, but were tolerant of long wait times and lengthy appointments since it was what they expected for public care and felt that they could not change this. (Table 2, Quote I.a.)- Existing systems promote patient access to care.At diagnosis of diabetes, several patients reported that they were prompted by their GP to undergo eye screening, but this was not always the case. Patients trusted that their GPs or optometrists would facilitate referral to specialists if (and when) additional care was needed. (Table 2, Quote I.a.)Participants also reported that the hospital/clinic used systems that reminded them to attend. For example, pre-booked appointments, letters, text messages, or options to reschedule if needed. Several patients had their own ways to remember, such as noting it on their personal calendar. However, patients passively awaited notifications for new or follow-up appointments. (Table 2, Quote I.a.)
- Patients have limited choice in appointments and limited knowledge of providers.Commonly, patients were not consulted or given a choice in the appointment times, days, or location; but were instructed by health services when they should attend. Sometimes they felt restricted by the availability of appointments or the frequency of specialist clinics. (Table 2, Quote I.b.)This meant that patients were waiting even longer if they needed to reschedule. However, some learned to adapt their routine to fit around the appointments. (Table 2, Quote I.b.)Additionally, many participants had limited knowledge of the different options that were available to them for DR eye care. Patients trusted that the referring GP/optometrists were well-informed and assumed that they would recommend an ophthalmologist/hospital with a good reputation. (Table 2, Quote I.b.)Other patients had previous experiences with private eye care services before switching to public care. These patients reported being uniformed and surprised by the costs of private care, with financial constraints were often cited as a key reason for changing. (Table 2, Quote I.b.)Patients had also waited a long time to access eye care appointments and feared being lost in the system if they did not attend. (Table 2, Quote I.b.)
- Patients wait around in clinics, but they do not fully understand why.Almost all participants in the hospital and treatment clinics felt that their appointments took too long. It was common to hear statements “several hours,” “all day,” or “until the cleaners came” in reference to experiences of appointments. Generally, the patients understood that the various tests, examinations, treatments, and interactions with multiple healthcare workers were needed. However, they felt there were unexplained delays and were confused by the processing of patient queues. For example, noticing that people with later appointments finished earlier, piles of medical files did not move, and patients with interpreters were fast-tracked. Patients were passively accepting of this since they could directly observe the high volume of patients in clinics. Some even tried to adapt to the system by arriving earlier or requesting earlier appointments, but they still waited. Many suggested that improved communication from the clinic around wait times and queues would improve their experience, by enabling them to take a walk, get food/coffee, or better arrange their transport with community services or family. (Table 2, Quote I.c.)
- A passive trust that healthcare providers will look after patients.
- Patients express limited understanding of eye conditions or eye care needsSeveral participants receiving treatments claimed that they had not been previously aware of DR until they developed acute visual symptoms, often presenting to the hospital emergency department when this happened. Other participants stated that their GP/optometrists had advised regular eye screening, but the patient had not actioned this until they had developed symptoms or other diabetes complications. Few participants had been undertaking routine DR screening since their initial diagnosis of diabetes.When prompted, most participants were uncertain or knew few details of their ocular diagnosis, mentioning they didn't ask too many questions or document these things, since they expected the specialist to tell them when something was wrong. (Table 2, Quote II.a.)Patients receiving collaborative care were satisfied with the information given by the optometrist, but also assumed the hospital would contact them when there was a problem.
- Patients expect providers to communicate about their care needs and health outcomesAlmost all participants believed that the various health/eye care providers (eg, ophthalmologists, GPs, optometrists) had two-way communication about their diagnosis and any treatments they had received. While some patients were unsure if their GPs needed all the details of the eye examination, including copies of OCTs or retinal photographs, most assumed that at least a summary report with a diagnosis should be shared. Some compared this expectation to experiences in other departments, including surgical wards or general diabetes clinics. The expectation of the two-way communication was so enshrined, that few participants had ever thought to question if this actually occurred. (Table 2, Quote II.b.)
- Patients place importance on looking after their health
- Patients are determined to maintain vision, independence, family responsibility, and quality of lifeThe vision was recognized as an important sense which enhanced the patient's quality of life and meant they could remain independent. Some participants valued vision as it allowed them to care for others (including grandchildren) or continue working. For others, vision gave independence which meant they could travel to and from appointments on their own, use public transport, taxis, or in some cases drive themselves. The fear of losing their vision encouraged patients to prioritize appointments. (Table 2, Quote III.a.)
- Patients feel a responsibility to manage all aspects of their diabetes.There was also a subtle theme whereby participants felt it was their responsibility to manage their diabetes. Some were confident in their actions to avoid complications, such as healthy eating, exercising, and maintaining blood glucose levels. Others felt they were less in control. Eye care was not always given the same importance as other aspects of diabetes care. (Table 2, Quote III.b.)
Table 2.
Overview of Themes and Sub-Themes Relating to Experiences of Eye Care for Diabetic Retinopathy.
| Theme | Sub-theme | Supporting quotes |
|---|---|---|
| I. The health system facilitates movement through the eye care pathway, patients passively accept but are not in control. | a. Existing systems promote patient access to care | “… and the waiting is not too bad, you know? I was expecting much longer wait time. Because I heard a lot of places where you go, you go you just sit there for a while … They say you know, that the public health care is sometimes taking longer”—D006—Male, 37 Years, hospital clinic “For some years now, I’ve been going to [the optometrist] as part of a diabetic care plan… initiated by my healthcare professional [doctor] … I had the sudden loss of vision, I went straight to [the optometrist] and from there this just kind of pursued onto that.”—D015—Male, 69 years, treatment clinic “They didn't think it was oedema, but they said they will give me an appointment for a couple of weeks time. That took more than a couple of weeks from memory, it dragged on.”—D015—Male, 69 years, treatment clinic |
| b. Patients have limited choice in appointments and limited knowledge of providers | “Oh, it's not easy to make an appointment for early morning … to see the doctor as early as possible …. The decision will be made by the system there. When the appointment we be coming. As a patient, I don't have any say.”—D008—Male, 57 years, hospital clinic “I didn't tell my boss for my day off … I forgot … I rescheduled, the last [appointment] … the ophthalmologist he only works for every Monday or once a month, something like this so that's why I had to wait until February [since December]”—D001—Female, 55 years, hospital clinic “I always chose my day off … to fit the appointment … My husband is not good at looking after my grandson [laughter]. So, I’m a bit worried that he's going to miss out lunch or this and that.”—D011—Female, 72 years, community clinic “Well, at least [my GP] knows who is the best place to go to get treatment … I’m in the dark. I don't even know where to go.”—D011—Female, 72 years, community clinic “[My optometrist] knows two Professors, one is in [another] hospital, but they didn't accept the referral … they did say waiting is way too long … I don't really know what the system is like. But if the person is more than qualified to look at your eyes, I don't really have any issues … And plus I don't have private hospital insurance, [the optometrist] said it would cost me a lot of money as well, if i do to private … but [the optometrist] said ‘let me see if I can refer you to one of the public hospitals and see how you go?’ And the public hospital is fine.”—D006—Male, 37 years, hospital clinic “They wanted me to see such and such person. First visit $800—what? Second visit—$800! I said nah, there's something wrong here. I talked to my GP, “Can I get out of this? A little bit cheaper?” That's why I came here.”—D013—Male, 61 years, treatment clinic “It is great to have a choice. But unfortunately… most of the time when you want to use your Medicare as a low cost, obviously I believe that there is no choice.”—D008—Male, 57 years, hospital clinic “the big problem for patients … once it goes beyond a set pathway, they’ve got no way of coping with it … again I must have missed an appointment, and they just drop you off. There's no follow up to say, ‘hey send him a letter’ and say, ‘where the hell are you?’ and for all I assume, they assume that I’m dead.”—D014—Male, 61 years, treatment clinic |
|
| c. Patients wait around at appointments but do not fully understand why | “… they overbook, there's too many people. What can you do? (laughter) … they’ve been sitting there all day … other ones come in before ‘em and they’re seen before … what's there to argue about, you’re not going to be seen any quicker, you’ve just got to sit and wait you know.”—D003, Male, 69 years, hospital clinic “By the time I leave here, it's dark out there. And if I don't have transport, and I can't drive of course, because I can't see. So, um, you walk up to the station, and your eyes are like big footballs, and the lights are shining, and you’ve got no idea. It's a bit hard to look at the screen to see if you're catching the right train or not.”—D016, Male, 79 years, treatment clinic |
|
| II. A passive trust that healthcare providers will look after patients | a. Patients express limited understanding of eye conditions or eye care needs | “I said, you’re my god, you do whatever you want. I go with whatever she [ophthalmologist] says.”—D013, Male, 61 years, treatment clinic |
| b. Patients expect providers to communicate about their care needs and health outcomes | “from my understanding, that's what they normally do, like [doctors name] will send results straight to my GP, because my GP referral letter is there, they wrote my referral letter.”—D001, Female, 55 years, hospital clinic | |
| III. Patients place importance on looking after their health | c. Patients are determined to maintain vision, independence, family responsibility, and quality of life | “the fear over the years, is that the anxiety, the reason was because my right eye was or bad compared to left eye… because if your eyes not working, you can't see this world, you can't see your future, you can't see your grandchildren or anybody tomorrow.”—D008, Male, 57 years, hospital clinic |
| d. Patients feel a responsibility to manage all aspects of their diabetes | “I haven't gone out of my way to look for eye care because once I was diagnosed with type 2 diabetes, I knew I had to start watching the bloods. Which I do, I mean I try very hard and occasionally I get a gold star my doctors says because my Hb1ac (sic), whatever it is, is down.”—D015, Male, 69 years, treatment clinic “I don't think it's something the eye clinic can do. More the patient themselves. I’m really bad at doing that. I’m too busy at work, and I just eat whatever. But I should start doing it.”—D006, Male, 37 years, public hospital |
COM-B Framework
Themes were mapped to the COM-B Framework to provide insights into processes for initiation (Figure 1) and maintenance (Figure 2) of eye care. These configurations depict the interface between the patient (capability and motivation) and the health system (opportunity) for adherence to eye care. Generally, the motivations related to fear of vision loss and the broad impacts this would have on their life. At the initiation stage, patient decisions were guided through the trust of healthcare providers, whereas at the maintenance stage, patients became fearful of dropping out. For all stages of care, patients tended to engage as passive recipients of eye care; but there is evidence that as their care was maintained, patients became more engaged by adapting to the system. Choice, health literacy, and being informed of eye care options were some of the key features identified by the patients which would help to empower them. Current mechanisms used by the health system were identified as being opportunities that supported health-seeking behavior, but long waits/waiting times negatively impacted on the patient experience. The results also highlight that the health system could re-orient toward patient-centered care and improve communication during the maintenance stages of care.
Figure 1.
Patient-reported factors that influence the initiation of eye care for diabetic retinopathy, an adaptation of the COM-B framework (19). *Text in bold are common features across Figures 1 and 2.
Figure 2.
Patient-reported factors that influence the maintenance of eye care and seeking treatments for diabetic retinopathy, an adaptation of the COM-B framework (19). *Text in bold are common features across Figures 1 and 2.
Discussion
This study provides new insight into the experiences of patients who are using a range of publicly funded DR eye care services in a low socio-economic urban area of Australia. Informed by the patient perspective and synthesis with the COM-B system (Figures 1 and 2), this study has identified factors that influence health-seeking behaviors for DR eye screening and ongoing maintenance and treatment. The findings have highlighted an interface existing between the patients’ involvement in seeking care (capabilities and motivations) and the support of the health system that surrounds them (opportunity).
A consistent finding across the study themes was the notion that patients were often passive actors when it came to seeking and maintaining DR eye care. They were highly reliant on the health system to facilitate their care and placed a large amount of trust in their healthcare providers to guide them (Table 2). A recent systematic review of qualitative studies examining patient experiences of DR screening identified that a lack of referral and follow-up systems is a common barrier for adherence to screening (8). However, 2 studies conducted in similar settings to the current study have evaluated the experiences of patients attending for cataract surgery and glaucoma management, finding that patients’ trust in providers was a key influencing factor when deciding where to go for ophthalmic care (20,21). More broadly, evidence suggests that trust in healthcare providers can have a positive influence on health-seeking behaviors for patients with chronic diseases, such as influencing their uptake of referral to allied health for diabetes management (eg, optometry, podiatry) (22), and adherence to diabetes care plans or attendance at follow-up appointments (22,23). Trust in health providers can also result in better clinical outcomes for chronic diseases, with one survey (23) showing that when patients with chronic diseases (including diabetes) scored highly on a health provider relationship scale, there was a strong association with medication adherence and psychosocial outcomes. However, in the current study, trust in healthcare providers existed in a context where patients were not always equipped with the knowledge and information needed to independently guide their choices about DR care. For example, several participants did not seek out DR examinations until vision loss had occurred. Patients also reported that there was little transparency of the costs for attending private care. Therefore, improved communication between the patient and provider, particularly in the early stages of a diabetes diagnosis, may empower the patient to seek out early interventions (8,24). Emphasis should be placed on the consequences of non-adherence, and also the eye care options available at different stages of disease. Primary care providers are well placed to provide ongoing messaging about DR eye care throughout the lifespan (25), and patient-centered approaches which allow patients to actively participate in their eye care by asking questions should be adopted since this can lead to better adherence, improved safety and improved clinical outcomes (26).
There were some perceived strengths of the current DR public eye care system. As observed in themes emerging from previous qualitative studies (8), top-down mechanisms employed by the health system, such as referral, pre-booked appointments, and reminders (letters and text messages) were reported by all participants as supporting their attendance (Figure 1, Table 2). These findings are in agreement with existing literature for DR screening which showed that contact from the healthcare provider/institution is an enabler for adherence (9,10,27) since it removes the need for patients to be proactive in seeking care (9). This current study adds further to this, demonstrating that these mechanisms also support adherence to ongoing care (Figure 2). However, the patients were reliant on the health service and passively awaited a notification, which might also be a weakness of these mechanisms. Several patients feared being dropped out of the system if they unknowingly missed an appointment. Thus a nationally coordinated patient-centered recall and reminder system, such as KeepSight (28) which actively prompts patients to seek DR screening, may add value to these existing systems. In this study, the lack of choice in the timings of appointments also meant that some patients needed to make compromises to attend, such as taking time off work, lost income, or making alternative carer or transport arrangements. While rescheduling was possible, it could come with extended waits. Such uncertainties have been reported elsewhere as barriers (8,9) which can weigh on the patients as a negative of their experience and lead to non-attendance. Furthermore, in this study, the majority of participants were retired (67%) and were able to be flexible, but since half the people with diabetes in Australia are of working age (29) many may not be willing or able to make these trade-offs.
The patients in this study shared several negatives experiences, such as the long wait to reach an appointment or the long waiting time in the clinic. But despite these shortcomings, they were generally complacent. This may have been partly influenced by a fear of vision loss and a sense of urgency to attend, but many also felt that they lacked any other choice when seeking care in the public sector (Figures 1 and 2). Patient experiences provide a unique perspective that can inform the redesign of services or the development of new models of care (30). Based on these accounts, strategies that seek to shorten wait times and choices in this setting will likely improve the patient experience. Collaborative care schemes are one approach which has been shown to significantly shorten hospital wait times for patients with low risk or stable DR (18). Such schemes might also offer a better patient experience by delivering care in more acceptable locations, with greater access to transport or reduced travel times (27). Another benefit of these schemes is that they offer enhanced communication between referring providers, which is often a shortcoming in hospital care (8,31). In the current study, patients held a firm expectation that this was already happening, which might be attributed to their passive trust that the healthcare providers act in their best interest to guide them to appropriate care. Thus, patients have identified that improvements to DR eye care could focus on ways to strengthen communication between providers, such as summary outcome letters, or upscaling of existing e-health portals to share health information online, such as My Health Record (32). In contrast, one Welsh study used a discrete choice experiment to elicit patient preferences for DR screening, finding that patients were willing to wait longer to get a screening appointment if offered an explanation of their results by a healthcare professional rather than by letter (33). Patients in our study also offered novel solutions which may improve their in-clinic waiting experience, such as enhanced communication about queue times through the use of notice boards, or queuing pager systems similar to those used in restaurants. Some suggested that access to queuing information might provide them with improved choices while they were waiting, such as seeking food or taking a walk.
Strengths and Limitations
This study was able to capture a broad perspective of patient adherence to DR eye care across the eye care continuum, extending beyond screening to include those attending for ongoing monitoring and treatment. It has also provided an opportunity for patients to assess the quality of care and inform future directions to better meet their DR eye care needs (24). One of the main drawbacks of this study is that the perspectives of patients who are not adhering to DR eye care, for various reasons, were not captured. However, it may be difficult to find these patients if they are avoidant of eye care services, uninformed, or face other access barriers. Another limitation is that the study sample was restricted to one large urban area of Australia (western Sydney) which has access to a public hospital ophthalmology department. The experiences in this setting may differ greatly to other places, particularly rural and remote areas where public eye care services are less available. Furthermore, the study was set in a low-socioeconomic region, with high costs noted as being a major deterrent in seeking private care. Therefore it does not capture the perspectives of patients who are willing to paying for eye care in the private sector.
Conclusions
In the public eye care setting in western Sydney, healthcare providers and existing recall and reminder mechanisms help to facilitate adherence to DR eye care. However, patients are mostly passive and place a large amount of trust in the provider and the health services to guide them. Patient adherence is often driven by fear (of vision loss, or falling through the gaps), but they often have limited choices when it comes to DR eye care in public settings. The findings of this study may be used to inform improvements in DR eye care. For example, one strategy might be to strengthen communication with the patient and also between their healthcare providers (30). Two-way communication between patients and their providers may help patients become more informed about the disease, its consequences, and their options when seeking DR care. This would empower them to become more active players. Other strategies may seek to provide services that are more accommodating for patients with conflicting priorities, particularly those of working age, or at risk of non-adherence. When seeking to improve experiences of eye care, health systems should adopt patient-centered approaches which emphasize the patients’ preferences (26) and actively involve the patient in setting health policy and research agendas (24) or when redesigning services to ensure the needs of patients are met (30).
Supplemental Material
Supplemental material, sj-docx-1-jpx-10.1177_23743735211049652 for Experiences of Patients With Diabetes Attending a Publicly Funded Eye Care Pathway in Western Sydney: A Qualitative Study by Belinda K Ford, Blake Angell, Andrew JR White, Annita Duong, Saya Hiidome and Lisa Keay in Journal of Patient Experience
Supplemental material, sj-docx-2-jpx-10.1177_23743735211049652 for Experiences of Patients With Diabetes Attending a Publicly Funded Eye Care Pathway in Western Sydney: A Qualitative Study by Belinda K Ford, Blake Angell, Andrew JR White, Annita Duong, Saya Hiidome and Lisa Keay in Journal of Patient Experience
Acknowledgments
The authors acknowledge the valuable contribution of the patients who participated in this study and thank staff at each of the clinics for supporting recruitment. Acknowledgment is also extended to Dr Hueiming Liu for her guidance during the early stages of interviews to improve the quality of responses.
Footnotes
Author Contributions: Belinda K Ford designed the study, collected the data, and made a substantial contribution to the analysis and interpretation of findings, and prepared the first draft of the manuscript. BA and AW contributed to the study design and interpretation of findings and revised the manuscript. SH and AD made substantial contributions to the analysis and interpretation of findings and revised the manuscript. LK made substantial contributions to the study conception, interpretation of findings and revised the final manuscript. All authors read and approved the final manuscript.
Availability of Data and Material: The authors can provide de-identified data upon reasonable request however, further use would be subject to additional ethical review.
Consent to Participate: All eligible subjects were participants were provided a written participant information statement and had the study explained to them by one of the researchers, and all participating subjects provided written informed consent.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: This study received ethical approval from the South Eastern Sydney Local Health District Human Research Ethics Committee (reference 15/053-LNR/POWH/120) and site-specific approval by the WSLHD Research governance office (reference LNRSSA-15-WMEAD-225).
Funding: The lead author (BF) of this manuscript was supported by an Australian Research Training Program PhD scholarship. No additional funding was received for this study.
ORCID iDs: Belinda K Ford https://orcid.org/0000-0003-4416-2389
Blake Angell https://orcid.org/0000-0002-7188-7740
Statement of Human and Animal Rights: All procedures in this study were conducted in accordance with the South Eastern Sydney Local Health District Human Research Ethics Committee (reference 15/053-LNR/POWH/120) approved protocols. The study was performed in accordance with the principles of the Declaration of Helsinki.
This article does not contain any animal subjects.
Statement of Informed Consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Yau JWY, Rogers SL, Kawasaki R, Lamoureaux EL, Kowalsaki JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556-64. doi: 10.2337/dc11-1909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keel S, Xie J, Foreman J, Van Wijngaarden P, Taylor HR, Dirani M. The prevalence of diabetic retinopathy in Australian adults with self-reported diabetes: the national eye health survey. Ophthalmology. 2017;124(7):977-84. doi: 10.1016/j.ophtha.2017.02.004 [DOI] [PubMed] [Google Scholar]
- 3.Mitchell P, Foran S, Wong TY, Chua B, Patel E, Ojaimi E, et al. Guidelines on the management of diabetic retinopathy National health and Medical Research Council. 2008
- 4.Australian Government Department of Health, Medicare. MBS Online-Medicare Benefits Schedule. 2020. [cited 2020 25th September]; Available from: http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Home.
- 5.Foreman J, et al. Adherence to diabetic eye examination guidelines in Australia: the national eye health survey. Medical Journal of Australia. 2017;206(9):402-6. [DOI] [PubMed] [Google Scholar]
- 6.Gibson AA, Humphries J, Gillies M, Nassar N, Colagiuri S. Adherence to eye examination guidelines among individuals with diabetes: an analysis of linked health data. Clinical and Experimental Ophthalmology. 2020;48(9):1229-38. doi: 10.1111/ceo.13830 [DOI] [PubMed] [Google Scholar]
- 7.Orr N, Boyages SC. Patterns of care as a risk factor for the development of vision-threatening diabetic retinopathy: a population-based matched case-control study using insurance claims (Medicare) data. Diabetic Medicine. 2005;22(8):1083-90. doi: 10.1111/j.1464-5491.2005.01663.x [DOI] [PubMed] [Google Scholar]
- 8.Egunsola O, Dowsett LE, Diaz R, Brent M, Rac V, Clement FM. Diabetic retinopathy screening: a systematic review of qualitative literature. Canadian Journal of Diabetes. 2021;45(7). doi: 10.1016/j.jcjd.2021.01.014 [DOI] [PubMed] [Google Scholar]
- 9.Graham–Rowe E, Lorencatto F, Lawrenson JG, Burr JM, Grimshaw JM, Ivers NM, et al. Barriers to and enablers of diabetic retinopathy screening attendance: a systematic review of published and grey literature. Diabetic Medicine. 2018;35(10):1308-19. doi: 10.1111/dme.13686 [DOI] [PubMed] [Google Scholar]
- 10.Piyasena MMPN, Murthy GVS, Yip JL, Gilbert C, Zuurmond M, Peto T, et al. Systematic review on barriers and enablers for access to diabetic retinopathy screening services in different income settings. PLOS One. 2019;14(4):e0198979. doi: 10.1371/journal.pone.0198979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lake AJ, Browne JL, Rees G, Speight J. What factors influence uptake of retinal screening among young adults with type 2 diabetes? A qualitative study informed by the theoretical domains framework. Diabetes and its Complications. 2017;31(6):997-1006. doi: 10.1016/j.jdiacomp.2017.02.020 [DOI] [PubMed] [Google Scholar]
- 12.Glasson NM, Larkins SL, Crossland LJ. What do patients with diabetes and providers think of an innovative Australian model of remote diabetic retinopathy screening? A qualitative study. BMC Health Services Research. 2017;17(1):1–16. https://link.springer.com/article/10.1186/s12913-017-2045-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson AC, Thompson MO, Young DL, Lin RC, Sansilo SR, Moshfeghi DM, et al. Barriers to follow-up and strategies to improve adherence to appointments for care of chronic eye diseases. Investigative ophthalmology & visual science. 2015;56(8):4324-31. doi: 10.1167/iovs.15-16444 [DOI] [PubMed] [Google Scholar]
- 14.Ford BK, Keay L, Angell B, Hyams S, Mitchell P, Liew G, et al. An audit of referrals for diabetic retinopathy in a public hospital ophthalmology service in western Sydney, Australia. Aust J Prim Health. 2020;26(4):293-99. doi: 10.1071/PY20084 [DOI] [PubMed] [Google Scholar]
- 15.Astell-Burt T, Feng X, Kolt GS, McLean M, Maberly G. Understanding geographical inequities in diabetes: multilevel evidence from 114,755 adults in Sydney, Australia. Diabetes research and clinical practice. 2014;106(3):e68-73. doi: 10.1016/j.diabres.2014.09.033 [DOI] [PubMed] [Google Scholar]
- 16.Hanna S. Optometry Australia - Guidelines on the examination and management of patients with diabetes. Clinical and experimental optometry. 2016;99(2):120-6. doi: 10.1111/cxo.12340 [DOI] [PubMed] [Google Scholar]
- 17.Medicare Australia. Medicare safety nets: what are the thresholds. 2020. [cited 2020 14th November]; Available from: https://www.servicesaustralia.gov.au/individuals/services/medicare/medicare-safety-nets/what-are-thresholds.
- 18.Tahhan N, Ford BK, Angell BA, Liew G, Nazarian J, Mitchell P, et al. Evaluating the cost and wait-times of a task-sharing model of care for diabetic eye care: a case study from Australia. BMJ Open. 2020;10(10):e036842. doi: 10.1136/bmjopen-2020-036842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions . Implementation Science. 2011;6(1):42. doi: 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilbert C, Keay L, Palagyi A, Do VQ, McClusky P, White A, et al. Investigation of attributes which guide choice in cataract surgery services in urban Sydney, Australia. Clinical and Experimental Optometry. 2018;101(3):363-71. doi: 10.1111/cxo.12653 [DOI] [PubMed] [Google Scholar]
- 21.Lu TC, Semsarian CR, White AJR, Dunn H, Angell B, Ford B, et al. Journey to glaucoma care–trusting but uncertain and uninformed: a qualitative study. Clinical and experimental optometry. 2020;103(4):484-9. doi: 10.1111/cxo.12955 [DOI] [PubMed] [Google Scholar]
- 22.Messina J, Campbell S, Rebecca M, Eyles E, Sanders C. A narrative systematic review of factors affecting diabetes prevention in primary care settings. PLoS One. 2017;12(5):e0177699. doi: 10.1371/journal.pone.0177699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eton DT, Ridgeway JL, Linzer M, Boehm DH, Rogers EA, Yost J, et al. Healthcare provider relational quality is associated with better self-management and less treatment burden in people with multiple chronic conditions. Patient preference and patient adherence. 2017;11:1635. doi: 10.2147/PPA.S145942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dean S, Mathers JM, Calvert M, Kyte DG, Conroy D, Folkard A, et al. “The patient is speaking”: discovering the patient voice in ophthalmology. British Journal of Ophthalmology. 2017;101(6):700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McDonald J, Jayasuriya R, & Harris MF. The influence of power dynamics and trust on multidisciplinary collaboration: a qualitative case study of type 2 diabetes mellitus. BMC Health Services Research. 2012;12(1):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Delaney LJJC. Patient-centred care as an approach to improving health care in Australia. Collegian. 2018;25(1):119-23. doi: 10.1016/j.colegn.2017.02.005 [DOI] [Google Scholar]
- 27.O’Connor PM, Harper CA, Brunton CL, Clews SJ, Haymes SA, Keefe JE. Shared care for chronic eye diseases: perspectives of ophthalmologists, optometrists and patients. Medical Journal of Australia. 2012;196(10):646-50. [DOI] [PubMed] [Google Scholar]
- 28.Diabetes Australia. Keepsight – about KeepSight. 2020. [cited 2020 24th November]; Available from: https://www.keepsight.org.au/about.
- 29.Australian Institute of Health and Welfare. Diabetes. AIHW: Canberra. 2020.
- 30.Kitson A, Marshall A, Bassett K, Zeitz K. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. Journal of Advanced Nursing. 2013;69(1):4-15. doi: 10.1111/j.1365-2648.2012.06064.x [DOI] [PubMed] [Google Scholar]
- 31.Long JC, Blakely B, Mahmoud Z, Ly A, Zangerl B, Kalloniatis M, et al. Evaluation of a hospital-based integrated model of eye care for diabetic retinopathy assessment: a multimethod study. BMJ Open. 2020;10(4):e034699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Australian Digital Health Agency. My health record – for healthcare professionals. 2020. [cited 2020 24th November]; Available from: https://www.myhealthrecord.gov.au/for-healthcare-professionals.
- 33.Yeo ST, et al. Preferences of people with diabetes for diabetic retinopathy screening: a discrete choice experiment. 2012; 29(7):869-77. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpx-10.1177_23743735211049652 for Experiences of Patients With Diabetes Attending a Publicly Funded Eye Care Pathway in Western Sydney: A Qualitative Study by Belinda K Ford, Blake Angell, Andrew JR White, Annita Duong, Saya Hiidome and Lisa Keay in Journal of Patient Experience
Supplemental material, sj-docx-2-jpx-10.1177_23743735211049652 for Experiences of Patients With Diabetes Attending a Publicly Funded Eye Care Pathway in Western Sydney: A Qualitative Study by Belinda K Ford, Blake Angell, Andrew JR White, Annita Duong, Saya Hiidome and Lisa Keay in Journal of Patient Experience