Abstract
Objective
Kashin–Beck disease (KBD) is an endemic degenerative joint disease with a high disability rate. We retrospectively evaluated the 18-year clinical follow-up outcomes of adult patients with KBD who underwent arthroscopic debridement for knee osteoarthritis.
Methods
Thirty-one patients with KBD (31 knees) underwent arthroscopy for knee osteoarthritis. The visual analog scale (VAS) score, walking distance, knee mobility, and patients’ self-evaluated improvement in clinical symptoms were retrospectively evaluated before and 18 years after the operation.
Results
The patients’ self-evaluated clinical symptoms showed considerable improvement at 2, 6, and 8 years after surgery but deteriorated at 10 and 18 years after surgery. Knee mobility was greater after than before arthroscopy but decreased from 6 to 18 years postoperatively. The VAS score for knee pain was high before the operation, decreased at 2 years postoperatively, increased at 6 years postoperatively, and was significantly lower at 18 years postoperatively than before surgery. The walking distance was significantly longer at 2, 6, and 8 years postoperatively than preoperatively.
Conclusions
Arthroscopic treatment may be an effective therapy for adult patients with KBD who develop knee osteoarthritis. In this study, arthroscopy had a long-term effect on patients with KBD who had Kellgren–Lawrence grade <IV osteoarthritis.
Keywords: Kashin–Beck disease, arthroscopy, knee, osteoarthritis, debridement, pain, walking distance, mobility
Introduction
Kashin–Beck disease (KBD) is an endemic, chronic degenerative joint disease with a high disability rate. 1 Primary osteoarthritis and KBD are joint diseases that share the common feature of damage to the articular cartilage. 2 KBD is a special type of bone and joint disease, and its typical pathology involves damage to the epiphyseal cartilage and hyaline cartilage. 3 KBD mainly affects cartilage growth and development. 4 The clinical features of KBD in adult patients include joint pain, thickening, and deformation; restricted movement; and muscle atrophy. Patients with KBD who develop severe osteoarthritis exhibit a short stature, short finger/toe deformities, and staggering gait. 5 The weight-bearing joints, such as the knees, ankles, and hips, develop severe pain and dysfunction. Among these joints, KBD has a greater impact on the knee joint, causing joint stiffness, thickening, pain, and varus or valgus deformity 6 with consequent limitations in walking, squatting, and standing and even loss of knee joint activity, 7 seriously affecting patients’ quality of daily life. Therefore, prevention and control of KBD are very important in alleviating pain, improving quality of life, and promoting recovery of the labor force.
The treatments of knee arthritis in patients with KBD include medical8,9 and surgical strategies. 10 Medical treatment can relieve knee pain but cannot maintain long-term efficacy. Total knee arthroplasty (TKA) is the most effective therapy to relieve pain and improve knee function in patients with KBD who have severe knee osteoarthritis, 11 but the cost of TKA is high for patients. Because most patients with KBD live in remote mountainous and rural areas, they are often low-income people and cannot afford the cost of TKA. Arthroscopic debridement is an alternative surgical treatment for patients with KBD. Relative to TKA, arthroscopic debridement has several advantages such as minimal invasiveness, rapid recovery, and low cost. In terms of treatment costs, patients with KBD are more likely to accept arthroscopy.
Few reports have described the long-term outcomes of arthroscopic treatment for KBD-induced knee arthritis. As early as 2001, our research team began treating adult patients with KBD-induced knee pain by arthroscopic debridement.12,13 Eight-years of follow-up showed that arthroscopic surgery was effective for these patients. 14 The present study was performed to retrospectively analyze the 18-year follow-up outcomes of these adult patients with KBD who underwent knee arthroscopy in 2001.
Materials and methods
Inclusion and exclusion criteria
The inclusion criteria were KBD with knee pain, meniscus and cartilage injury, agreement to undergo primary arthroscopic debridement, Kellgren–Lawrence (K-L) grade <IV arthritis, and age of 18 to 70 years. The exclusion criteria were contraindications to arthroscopic debridement, post-traumatic arthritis or deformity, ongoing infection of the knee or other parts of the body, malignant tumors, diabetes, K-L grade >III osteoarthritis, and analgesic drugs taken within 1 month after surgery to the end of follow-up.
Study population
Thirty-one patients with KBD (31 knees) who underwent arthroscopy for knee osteoarthritis from February to April 2002 were retrospectively analyzed. All patients had been diagnosed with KBD according to the KBD diagnostic criteria (GB16003-1995), 15 and all were from a KBD-endemic area in Shaanxi Province, China. Written informed consent was obtained from all patients. The research protocol was approved by the Ethics Committee of Shaanxi Provincial People’s Hospital (approval number: 20190805) and was carried out in strict accordance with the Declaration of Helsinki. All patient details have been de-identified. The reporting of this study conforms to the STROBE guidelines. 16
Arthroscopic observation and surgical technique
The synovial morphology was observed under arthroscopy. The hyperplastic synovium was divided into four grades under arthroscopy as described by Ling et al.: 17 Grade 0, normal synovial villi are slender and almost translucent, and blood vessels are regularly distributed; grade I, slight synovial hyperemia and synovial edema are present; grade II, moderate synovial hyperemia, synovial edema, and synovial thickening are present; and grade III, severe synovial hyperemia, synovial hyperplasia, and synovial thickening are present, and some synovial villi resemble corals or sheep tails. Arthroscopic cartilage damage was graded using the Outerbridge classification.
The hyperplastic synovial membrane was removed. The torn meniscus and damaged cartilage were trimmed until their edges were smooth. The areas of full-thickness loss of cartilage and subchondral bone exposure were trimmed, and several holes were drilled with a 2.0-mm-diameter Kirschner wire. Loose bodies within the knee joint were found and removed.
Medication after surgery
For pain relief, ibuprofen was given to all patients within 3 days before surgery and was continued until 1 month after surgery. No oral medication for analgesia was given after 1 month postoperatively. No antibiotics were used to prevent knee infection after surgery.
In-hospital rehabilitation program for knee function
After the operation, the patients began to perform ankle pump exercises to prevent venous thrombosis of the lower extremities, and they exercised the function of the quadriceps femoris at the same time. They began to walk on the ground on the first day postoperatively, and the amount of activity gradually increased. On the third to seventh days after surgery, the patients were discharged from the hospital.
Outcome measures
Pain was measured using a visual analog scale (VAS). Knee function was assessed using the walking distance and knee mobility. Patients’ self-evaluated improvement in clinical symptoms and postoperative complications were also evaluated. Demographic data, clinical data, and follow-up outcomes were obtained preoperatively and at 2, 6, 8, 10, and 18 years postoperatively.
The walking distance was defined as the longest distance that a patient could continue to walk until joint pain or physical fatigue occurred. The improvement in clinical symptoms was evaluated by the patient according to his or her feelings. The patients’ self-evaluated improvement in clinical symptoms was graded as follows: considerable improvement (joint pain/swelling was significantly reduced or had disappeared), slight improvement (joint pain/swelling was slightly relieved), and deterioration (joint pain, swelling, and limited mobility persisted).
Statistical analysis
The data were analyzed using statistical software (IBM SPSS Statistics for Windows, Version 22.0; IBM Corp., Armonk, NY, USA). The results are expressed as mean ± standard deviation or absolute numbers. The chi-square test was used to compare categorical outcomes. The Bonferroni post hoc test was used to compare the outcomes between the preoperative and postoperative periods. A two-sided P-value of <0.05 was considered statistically significant.
Results
Baseline characteristics of patients
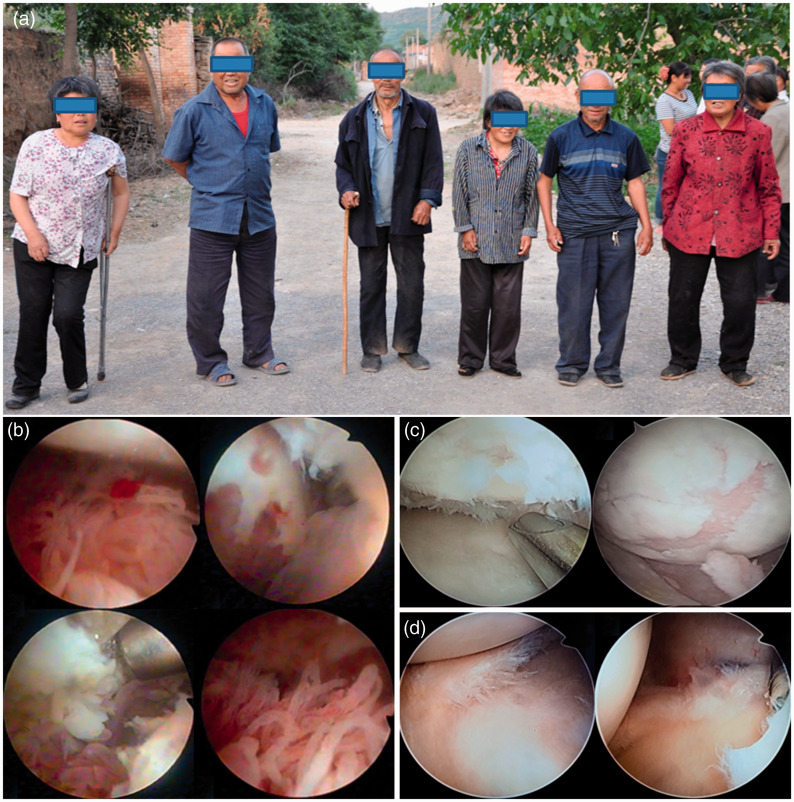
Thirty-one patients with KBD-induced knee arthritis underwent unilateral knee arthroscopic debridement. However, only 24 patients were followed up after the operation; the remaining 7 patients were lost to follow-up because of loss of contact. With the exception of one patient who underwent TKA, none of the patients underwent secondary operations on the ipsilateral or contralateral knee joints. No patients developed serious complications after surgery. The patients’ demographic and clinical characteristics are shown in Table 1, and their physical characteristics are shown in Figure 1(a).
Table 1.
Detailed demographic and clinical characteristics of 24 patients who were followed up.
| Demographic and clinical characteristics | Patients |
|---|---|
| Sex | |
| Male | 9 (37.5) |
| Female | 15 (62.5) |
| Age, years | 46.5 ± 18.7 |
| Side | |
| Right | 10 (41.7) |
| Left | 14 (58.3) |
| Varus/valgus deformities | |
| Varus | 21 (87.5) |
| Valgus | 3 (12.5) |
| Grade of knee osteoarthritis (Kellgren–Lawrence classification) | |
| Grade 0 | 0 (0.0) |
| Grade I | 2 (8.3) |
| Grade II | 16 (66.7) |
| Grade III | 6 (25.0) |
| Grade IV | 0 (0.0) |
| Surgery duration, minutes | 63.8 ± 11.8 |
Data are presented as n (%) or mean ± standard deviation.
Figure 1.
Physical characteristics of patients with Kashin–Beck disease and arthroscopic findings of synovial proliferation and cartilage and meniscus injuries. (a) The physical characteristics of adults with Kashin–Beck disease include short stature, varus or valgus knee deformity, lameness, restricted movement, and limited knee joint activity, which seriously affect patients’ daily life. (b) Synovial hyperplasia and synovial thickening were found under arthroscopy, and some villi resembled corals or sheep tails. (c) The cartilage showed full-thickness loss, and the subchondral bone was exposed. (d) The torn meniscus and damaged cartilage were trimmed.
Arthroscopic observation of knee during surgery
Three patients had grade I arthroscopic synovial hyperplasia, 5 patients had grade II, and 23 patients had grade III (Figure 1(b)). All patients had Outerbridge grade IV cartilage damage (Figure 1(c)). Cartilage injuries were distributed on the articular surfaces of the patella, femoral notch, femoral condyle, medial tibial plateau, and lateral tibial plateau. Twenty-three patients had osteophytes, and the osteophytes were distributed on the femoral condyles, intercondylar fossa, and upper and lower poles of the patella. Twenty-four patients had vertical longitudinal, oblique, and horizontal tears in the meniscus; two patients had a radial meniscus tear; and five patients had no meniscus tears (Figure 1(d)). Eight patients had loose bodies in the knee joints.
Patients’ self-evaluated improvement in clinical symptoms after surgery
The patients’ self-evaluations of clinical symptoms revealed improvement after surgery. However, the total self-evaluated improvement rates thereafter gradually decreased until they reached 91.67% at 10 years and 79.17% at 18 years after surgery (Table 2).
Table 2.
Outcome measures after operation in patients with Kashin–Beck disease.
| Time | Patients’ self-evaluation of clinical symptom improvement |
Improvement of knee mobility | Improvement of knee pain | Improvement of walking distance |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Considerable improvement | Slight improvement | Deterioration | Total improvement rate | <1 km | 1–5 km | >5 km | |||
| Preoperatively | 131.6 ± 14.7 | 6.9 ± 1.5b | 12 (50.0) | 9 (37.5) | 3 (12.5) | ||||
| 2 years | 23 (95.8) | 1 (4.2) | 0 (0.0) | 100% | 134.3 ± 13.1a | 1.7 ± 1.3b | 2 (8.3) | 12 (50.0) | 10 (41.7)b |
| 6 years | 17 (70.8) | 7 (29.2) | 0 (0.0) | 100% | 132.3 ± 14.5a | 3.4 ± 2.9b | 3 (12.5) | 11 (45.8) | 10 (41.7)b |
| 8 years | 21 (87.5) | 3 (12.5) | 0 (0.0) | 100% | 125.0 ± 8.1a | 3.3 ± 2.2b | 6 (25.0) | 9 (37.5) | 9 (37.5)b |
| 10 years | 14 (58.3) | 8 (33.3) | 2 (8.3) | 91.67% | 117.8 ± 15.3b | 3.4 ± 1.3b | 6 (25.0) | 12 (50.0) | 6 (25.0)a |
| 18 years | 9 (37.5) | 10 (41.7) | 5 (20.8) | 79.17% | 114.5 ± 17.5b | 3.7 ± 1.3b | 7 (29.2) | 13 (54.2) | 4 (16.7)a |
Data are presented as n (%) or mean ± standard deviation.
aCompared with before surgery, P > 0.05.
bCompared with before surgery, P < 0.05.
Improvement of knee mobility after arthroscopy
The knee mobility after arthroscopy was higher than that before surgery, but the difference was not statistically significant. The knee mobility gradually decreased from 6 to 8 years postoperatively. It then further decreased at 10 and 18 years after surgery, at which time it was significantly lower than that before surgery (Table 2).
Improvement of knee pain after arthroscopy
The VAS score for knee pain was high preoperatively, after which it rapidly decreased and reached a nadir at 2 years postoperatively. However, the VAS score for knee pain was higher at 6 and 8 years postoperatively than at 2 years postoperatively, and it continued to increase at 10 and 18 years postoperatively. The VAS score for knee pain at 2, 6, 8, 10, and 18 years postoperatively was significantly lower than that before surgery (Table 2).
Improvement of walking distance after arthroscopy
The walking distance at 2, 6, and 8 years postoperatively was significantly longer than that preoperatively (P < 0.05), and it then decreased at 10 and 18 years postoperatively. Although more patients had a walking distance of 1 to 5 km and >5 km at 10 and 18 years postoperatively, this finding was not significantly different from that before the operation (Table 2).
Discussion
This study is the first to reveal the 18-year follow-up outcomes of patients with KBD who underwent arthroscopic treatment for knee osteoarthritis. Our results demonstrate that arthroscopic treatment is an effective therapy for adult patients with KBD-induced knee osteoarthritis and that it has a long-term effect on patients with less severe joint deformities (K-L grade <IV).
KBD in children is currently controlled in China 18 ; however, 527,338 adults with KBD remained in endemic areas of China in 2018, 19 and they were plagued by knee pain. Therefore, relieving and treating the knee joint pain of adults with KBD have become important parts of the prevention and treatment of KBD. Any surgical procedure that improves physical function and relieves pain can be used as an adjunct or alternative to the treatment of KBD. 20 However, few data are available on the effectiveness of arthroscopic debridement for knee arthritis in patients with KBD because only a few patients with KBD can afford the cost of surgery. Because of the financial difficulties faced by most patients with KBD, they are more willing to bear the cost of arthroscopy that of other surgical treatments such as TKA and high tibial osteotomy. Therefore, it is important to evaluate the long-term efficacy of knee arthroscopy for the treatment of knee osteoarthritis in patients with KBD.
In this study, 31 adult patients with KBD underwent arthroscopy, but only 24 patients could be continuously followed up after surgery; the remaining patients were lost to follow-up. The patients’ self-evaluated improvements in clinical symptoms, knee mobility, and knee pain revealed good outcomes both in the early postoperative period and at the 8-year follow-up. Fond et al. 21 reported that 32 of 36 patients who underwent arthroscopy achieved good results at the 2-year follow-up. Additionally, 25 of the 36 patients were very satisfied with the results at the 5-year follow-up. Surprisingly, our study showed that 19 of the 24 patients who underwent arthroscopy had satisfactory results during the 18-year follow-up. Figueroa et al. 22 reported that most patients with unstable cartilage or meniscus injuries had good and excellent results at short- and medium-term follow-up after arthroscopy.
The walking distance of the patients with KBD in the present study was significantly longer within 6 years postoperatively than that preoperatively, indicating that arthroscopy improved the daily living ability or range of activities in patients with KBD. The 10- and 18-year follow-up outcomes showed that the patients’ self-evaluated improvements in clinical symptoms, knee mobility, knee pain, and walking distance began to gradually decline. Three possible reasons for these findings can be considered. First, severe pathological changes are present in the knees of patients with KBD. Second, arthroscopic surgery can only remove some of the osteophytes, damaged cartilage, and proliferative synovium, and the repair of the damaged meniscus and cartilage is thus incomplete. Third, as the patients get older, the articular cartilage ages and degenerates, and the contracture of muscles and ligaments results in further decline of joint function.
Aaron et al. 23 proposed that it is important to divide patients into various subgroups based on age, severity of osteoarthritis, and severity of cartilage injury when assessing the efficacy of arthroscopy. These variables may affect postoperative outcomes. In the present study, however, the small sample size was not sufficient for a subgroup analysis, which is a limitation of our study. Most patients with KBD live in remote mountain areas, and their families have a poor economic status. Relatively few patients with KBD can afford arthroscopic surgery. Therefore, it was difficult to expand the sample size of this study.
Although all patients with KBD in this study had cartilage damage, these patients had mild deformities (K-L grade <IV). This is also one of the main reasons for maintenance of the long-term effects after arthroscopic surgery. Therefore, patients with KBD who develop knee arthritis should be selected according to the severity of their knee arthritis to ensure that they have good long-term efficacy after arthroscopic debridement surgery. Arthroscopic surgery cannot significantly reduce joint pain, and it is difficult to increase knee joint mobility for patients with advanced KBD who have extensive cartilage damage, subchondral bone sclerosis, and severe knee deformity (K-L grade >III).
Conclusions
In this study, we evaluated the long-term postoperative outcomes of arthroscopic debridement in patients with KBD who had knee osteoarthritis. The results demonstrated that arthroscopic surgery may be effective for the treatment of knee osteoarthritis in adult patients with KBD and that it has a long-term effect on patients with mild joint deformity (K-L grade <IV).
Footnotes
Author contributions: All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted. Xiang-Hui Dong, Zhan-Kui Jin, and Ming Ling participated in the design of the study and the analysis and interpretation of the data. Cui-Xiang Xu, Ming Chen, Zhi Yi, Shi-Zhang Liu, Xue-Yuan Wu, Zheng-Ming Sun, and Yan-Hai Chang collected the clinical data. Xiang-Hui Dong, Zhan-Kui Jin, Cui-Xiang Xu, and Ming Ling participated in the analysis and interpretation of the data and the manuscript preparation. Zhan-Kui Jin and Xiang-Hui Dong had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was supported by the Key Scientific Research Project of Shaanxi Provincial Department of Education (21JS039), Talent Support Program of Shaanxi Provincial People’s Hospital (2021BJ-04), Shaanxi Provincial People’s Hospital Technology Development Incubation Fund, Shaanxi Province Key R&D Program (2020SF-303, 2018ZDXM-SF-054), Shaanxi Provincial Health Research Fund Project (2018E012), and Special Project for Guiding the Transformation of Major Scientific and Technological Achievements of Shaanxi Province (2013KTCG01-12).
ORCID iD: Ming Ling https://orcid.org/0000-0001-9578-0860
References
- 1.Wang K, Yu J, Liu H, et al. Endemic Kashin-Beck disease: a food-sourced osteoarthropathy. Semin Arthritis Rheum 2020; 50: 366–372. DOI: 10.1016/j.semarthrit.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 2.Duan C, Guo X, Zhang XD, et al. Comparative analysis of gene expression profiles between primary knee osteoarthritis and an osteoarthritis endemic to northwestern China, Kashin-Beck disease. Arthritis Rheum 2010; 62: 771–780. DOI: 10.1002/art.27282. [DOI] [PubMed] [Google Scholar]
- 3.Wu SX, Wang WZ, Zhang F, et al. Expression profiles of genes involved in apoptosis and selenium metabolism in articular cartilage of patients with Kashin-Beck osteoarthritis. Gene 2014; 535: 124–130. DOI: 10.1016/j.gene.2013.11.050. [DOI] [PubMed] [Google Scholar]
- 4.Hu J, Wang YM, Wang WY, et al. Perturbations in amino acid metabolism in children with Kaschin-Beck disease: a study of urinary target metabolomics. Biomed Environ Sci 2019; 32: 34–37. DOI: 10.3967/bes2019.004. [DOI] [PubMed] [Google Scholar]
- 5.Li Y, Zhou Z, Shen B, et al. Clinical features of Kashin-Beck disease in adults younger than 50 years of age during a low incidence period: severe elbow and knee lesions. Clin Rheumatol 2013; 32: 317–324. DOI: 10.1007/s10067-012-2115-0. [DOI] [PubMed] [Google Scholar]
- 6.Mathieu F, Begaux F, Suetens C, et al. Anthropometry and clinical features of Kashin-Beck disease in central Tibet. Int Orthop 2001; 25: 138–141. DOI: 10.1007/s002640000192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mathieu F, Begaux F, Lan ZY, et al. Clinical manifestations of Kashin-Beck disease in Nyemo Valley, Tibet. Int Orthop 1997; 21: 151–156. DOI: 10.1007/s002640050139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luo R, Liu G, Liu W, et al. Efficacy of celecoxib, meloxicam and paracetamol in elderly Kashin-Beck disease (KBD) patients. Int Orthop 2011; 35: 1409–1414. DOI: 10.1007/s00264-010-1062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang X, Pei FX, Zhou ZK, et al. A randomized, single-blind comparison of the efficacy and tolerability of hyaluronate acid and meloxicam in adult patients with Kashin-Beck disease of the knee. Clin Rheumatol 2012; 31: 1079–1086. DOI: 10.1007/s10067-012-1979-3. [DOI] [PubMed] [Google Scholar]
- 10.Tang X, Zhou ZK, Shen B, et al. Total knee arthroplasty in elderly patients with severe Kashin-Beck disease of the knee. Int Orthop 2014; 38: 753–759. DOI: 10.1007/s00264-013-2171-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jin ZK, Yang Y, Xu CX, et al. Outcomes of total knee arthroplasty in the adult Kashin-Beck disease with severe osteoarthritis. Int Orthop 2019; 43: 323–331. DOI: 10.1007/s00264-018-4029-1. [DOI] [PubMed] [Google Scholar]
- 12.Yi Z, Ling M, Luo Z. Observation on treatment result of arthroscopic knee clearing and reconstructing operation in Kaschin-Beck disease. China Journal of Endoscopy 2006; 12: 937–939. DOI: 10.3969/j.issn.1007-1989.2006.09.014. [Google Scholar]
- 13.Ling M, Huang X, Yi Z. Evaluation of long term effects of arthroscopic knee debridement and reconstructing for treating osteoarthritis in patients with Kaschin-Beck disease. Chinese Journal of Endemiology 2010; 29: 559–561. DOI: 10.3760/cma.j.issn.1000-4955.2010.05.026. [Google Scholar]
- 14.Ling M, Sun Z, Yi Z, et al. Long-term efficacy of arthroscopic debridement on knee osteoarthritis in patients with Kashin-Beck disease. Cell Biochem Biophys 2015; 73: 125–128. DOI: 10.1007/s12013-015-0635-3. [DOI] [PubMed] [Google Scholar]
- 15.Disease CODC. Diagnostic criteria of Kaschh-Beck disease. Chinese Journal of Endemiology 1994: 309. [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573–577. DOI: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 17.Ling M, Yi Z, Wang Y. . Morphological observation of knee joint arthroscope. Chinese Journal of Endoscopy 2001; 7: 41–42. DOI: 10.3969/j.issn.1007-1989.2001.06.018. [Google Scholar]
- 18.Liu YQ. Reviewing focus of prevention and treatment of Kashin-Beck disease. Chinese Journal of Endemiology 2008; 27: 473–474. DOI: 10.3760/cma.j.issn.1000-4955.2008.05.001. [Google Scholar]
- 19.Committee CHAF. 2018 China Health Statistics Yearbook. Beijing: China Union Medical University Press, 2018, p.274. [Google Scholar]
- 20.Yu FF, Xia CT, Fang H, et al. Evaluation of the therapeutic effect of treatment with intra-articular hyaluronic acid in knees for Kashin-Beck disease: a meta-analysis. Osteoarthritis Cartilage 2014; 22: 718–725. DOI: 10.1016/j.joca.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 21.Fond J, Rodin D, Ahmad S, et al. Arthroscopic debridement for the treatment of osteoarthritis of the knee: 2- and 5-year results. Arthroscopy 2002; 18: 829–834. DOI: 10.1053/jars.2002.36225. [DOI] [PubMed] [Google Scholar]
- 22.Figueroa D, Calvo R, Villalon IE, et al. Clinical outcomes after arthroscopic treatment of knee osteoarthritis. Knee 2013; 20: 591–594. DOI: 10.1016/j.knee.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Aaron RK, Skolnick AH, Reinert SE, et al. Arthroscopic debridement for osteoarthritis of the knee. J Bone Joint Surg Am 2006; 88: 936–943. DOI: 10.2106/JBJS.D.02671. [DOI] [PubMed] [Google Scholar]