Abstract
Background
Dental caries in adolescents remains a significant public health problem with few oral health promotion interventions aimed at reducing dental caries in secondary school-aged students. Previous oral health and mobile health (mHealth) research has suggested the need for the development of a school-based behaviour change intervention incorporating a digital component. This study aimed to describe the development process of a behaviour change intervention to improve the oral health of students aged 11–16 years attending secondary schools in the UK.
Methods
A six-step process was used to develop the complex intervention informed by behaviour change theory and involving students, young people, parents and teachers in the process. The steps were: (1) identifying the target behaviours, namely tooth brushing with a fluoride toothpaste (2) identifying the theoretical basis and developing the causal model (3) reviewing the relevant literature and developing the logic model (4) designing the intervention with young people, parents and school staff (5) specifying the intervention content and (6) translating this content into features of the intervention and piloting.
Results
The resultant intervention included a quality-assured classroom-based session (CBS) (guided by a lesson plan and teaching resources), delivered by school teachers which was embedded within the school curriculum. This CBS was followed by a series of (Short Message Service) SMS texts delivered twice daily to student’s mobile telephones with the content, duration and timing of the messages informed by involvement of students and young people.
Conclusions
An intervention to improve the oral health of secondary school students through improved tooth brushing was rigorously developed based on behaviour change theory and work with young people, parents and school staff. Further research is needed to evaluate the outcomes and processes involved following the delivery of this intervention.
BRIGHT Trial Trial Registration ISRCTN12139369.
Keywords: Oral health, Behaviour change, Text messages, Young people
Background
Dental caries in adolescents remains a significant public health problem, particularly in social and economically deprived areas [1]. The current focus of community oral health promotion interventions in the UK is to reduce dental caries mainly with children under 11 years of age [2]. Few interventions are aimed at reducing dental caries in adolescents despite this being a critical stage where health practices are developed [3]. Examples of current oral health promotion interventions to improve the oral health of adolescents have been categorised into oral health education interventions and more complex interventions involving additional activities such as clinical prevention measures alongside the education component [4]. However, limitations of existing research include a lack of understanding of factors influencing the oral health behaviours of adolescents has been and little is known about adolescent’s receptiveness to interventions that seek to change these behaviours [5]. Previous research has looked at short-term changes in behaviour only [6] with further research recommended to develop interventions based on behaviour change theory including long term evaluation [4].
Mobile health (mHealth) interventions are increasingly being used to bring about health behaviour change. mHealth describes multimedia technologies that interface with health care delivery, most commonly through mobile phones. Short message service (SMS) interventions are the most widely studied mHealth intervention [7]. A recent systematic review of SMS found a small but statistically significant weighted mean effect size for the impact of SMS on preventive health behaviour change (d = 0.24) with positive effect of SMS interventions in 11 of the 35 included studies, with a further 13 studies having mixed effects [8]. Few mHealth interventions have been developed to improve the oral health of young patients or people.
A study of unemployed young people in New Zealand, called ‘Keep on Brushing (KOB)’ investigated a weekly SMS and free toothbrushes and toothpaste programme [9]. The intervention was underpinned by the Health Belief Model and aimed to improve tooth brushing frequency among those aged 18–24 years. The study found self-reported tooth brushing of twice or more per day increased from 51% at baseline to 70% at week three, 74% at week six, and 73% at week nine. No important differences were noted between age, gender, or ethnic groups, although attrition was relatively high with only 26% participating by week nine. The authors concluded that motivational text messaging improved the self-reported oral health of this hard-to-reach group and suggested a randomised control trial was needed including a longer intervention co-produced with the target group.
The BRIGHT Trial: Brushing RemInder 4 Good oral HealTh is a multi-centre, school-based, assessor-blinded, two-arm cluster-randomised control trial based on KOB [10]. BRIGHT aims to investigate the clinical and cost-effectiveness of a behaviour change intervention to improve the oral health of secondary school students (11–16 years) living in deprived areas of the UK. The BRIGHT trial also includes a process evaluation. The intervention is a multi-component, complex intervention with two parts; (1) a classroom-based session (CBS) embedded in the school curriculum and (2) a series of follow-up SMS text messages to student’s mobile telephones. BRIGHT includes around 40 schools with above the national average percentage of students eligible for free school meals. From these schools the trial has recruited over 4000 students aged 11–13 years. The primary outcome of the BRIGHT trial is the prevalence of obvious dental caries experience at 30 months.
Understanding the components of any complex intervention, their provenance and how they were derived has been recognised as being important in placing context around study findings and insight into their generalisabilty to other settings. It also allows potential users of the research to decide whether adaptations should be made for different circumstances. Yet reporting how complex interventions are developed and the theory underpinning them is often poor or even neglected [11, 12]. The aim of this paper is to describe the development process of a behaviour change intervention that is being used in the BRIGHT trial and the theory underlying its various components.
Method
Background to the intervention
The development of the intervention was informed by the guidance on the development of complex interventions [13] and behaviour change interventions [14] and designed with young people and other stakeholders. It is reported according to the GUIDED guideline for reporting of intervention development studies [12]. The intervention development framework employed was a combination approach, utilising both a theory and evidence-based approach, and a partnership approach [15].
Setting for the intervention
Secondary schools were chosen as an appropriate setting for the intervention as they provide an opportunity to reach large numbers of young people at low cost [16]. The modes of delivery, CBS and SMS were chosen to be practicable, acceptable, safe, affordable, sustainable and equitable as recommended for behaviour change interventions [17].
Intervention components
Classroom-based session (CBS)
The KOB study did not include any classroom activities so a bespoke lesson plan and teaching resources for the CBS were designed specifically for the BRIGHT trial. The CBS was developed to be delivered by teachers as part of the Personal Health and Social Education curriculum (England and Wales) and Health and Wellbeing (Scotland).
Short messaging service (SMS)
Key features of SMS health interventions include their duration and timing, tailoring them to the audience and linking SMS use with other activities, which in this case is the CBS [18]. However, limitations of using SMS include the restriction in the number of characters available, the need for basic literacy and limited access to mobile phones for some young people [19].
The results section will describe the six steps in the BRIGHT intervention development process:
Step 1 Identify target behaviours.
Step 2 Identify the theoretical base.
Step 3 Review relevant literature.
Step 4 Design the intervention with students, parents and school staff.
Step 5 Specify the intervention content.
Step 6 Translation of the intervention content into interventions features and piloting.
Results
The intervention was developed using the following six steps:
Step 1 Identify target behaviours.
The first step was to identify the target behaviour to reduce the prevalence of caries in permanent teeth. One of the most effective ways of reducing the prevalence of caries is twice-daily tooth brushing with fluoride toothpaste [20, 21]. Observational studies have shown the efficacy, frequency and duration of tooth brushing to be inadequate [22, 23] increasing the risk of caries [24, 25]. Behaviour change approaches are recommended to improve tooth brushing as a health behaviour [26]. The target behaviour was therefore improving the efficacy and frequency of tooth brushing with a fluoride toothpaste. Other behaviours to reduce dental caries related to diet were not targeted.
Step 2 Identify the theoretical base.
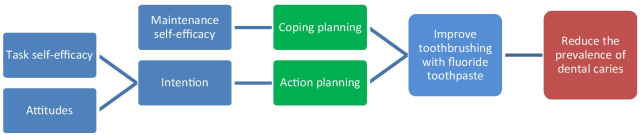
The intervention development drew on the Health Action Process Approach (HAPA) [27] as the causal model (Fig. 1) and was informed by the Behaviour Change Wheel [17].The main principles of the HAPA are that the health behaviour change process includes first a motivation phase (indicated in blue in Fig. 1) in which people develop their intentions, followed by a volitional phase. In the volitional phase action planning and coping planning (indicated in green) are needed to plan when, where, and how a behaviour will be conducted and for the anticipation of barriers to the behaviour.
Fig. 1.
Causal model for the intervention
Step 3 Review relevant literature.
In addition to the theoretical base, the literature from the fields of oral self-care in adolescents, SMS and teaching young people about health was reviewed.
Systematic literature searches were conducted via electronic databases MEDLINE via Ovid, PsycINFO, Scopus and Google Scholar. Multiple combinations of search terms included oral health, dental health, oral hygiene, oral self-care, tooth brushing, adolescents, children, behaviour change, intervention, and psychological. Additional articles were identified through hand searching of reference lists of relevant articles. The searches focused on children aged 11–16 years. An existing relevant systematic review was identified of psychosocial factors considered important for oral hygiene behaviour in young people aged 9–19 years [28], the following factors were found to be influential:
Motivational factors
Both maintenance- and task-self-efficacy refer to an individual’s belief in his or her ability to accomplish a task [29], such as effective tooth brushing.
Attitude refers to the extent to which an individual perceives a particular (oral health) behaviour as favourable or unfavourable [30] based on the outcome expectancy and risk perceptions.
Intention summarises an individual’s motivation to act [31].
Volitional factors
Action planning involves moving beyond behavioural intentions because it includes the parameters of ‘when’, ‘where’ and ‘how’ [27] to practice oral hygiene behaviours. Explicitly specifying these parameters increases the likelihood that the behaviour will become habitual or automatic [32].
Coping planning is a self-regulatory strategy where individuals anticipate possible barriers to a behaviour (such as tooth brushing) and devise coping strategies to overcome them [27].
These were consistent with the HAPA model [27]. Scheerman and colleagues also acknowledged that there may be other influences on tooth brushing behaviour in adolescents that have not previously been researched, including ‘self-determination’, ‘anticipated regret’, ‘action control’ and ‘self-identity’ [28]. Further investigation of these additional influences suggested there was enough evidence for ‘self-determination’ to be included as a general approach incorporated into the intervention. Self-determination is the degree to which an individual's behaviour is self-motivated. For behaviours such as tooth brushing which may be an activity that young people are uninterested in, with intangible benefits, an intervention needs to encourage them to value the outcomes of tooth brushing, to take responsibility for it and be competent to facilitate self-motivation [33, 34]. These factors were built into the intervention development, particularly for the CBS lesson plan and teaching resources.
To create the lesson plan and teaching resources for the CBS, first the curricula for England, Scotland and Wales were analysed including: science key stage 3 (a) and 4 (b) [35, 36]; Personal, Social, Health and Economic study key stage 3 (PSHE 2014), the Scottish Curriculum for excellence experiences and outcomes for both science and health and wellbeing [37, 38]; and the Welsh Personal and Social Education framework [39]. The literature suggested the CBS must be based on dialogue, perceived to be relevant by students, be understandable, trustworthy and positive. Furthermore, adolescents want active teaching with opportunities to discuss questions about lifestyle with others [40].
For the SMS, a search for systematic reviews was conducted to establish the optimal duration, frequency and content. A recent systematic review of SMS found the length of interventions typically ranged from 1 to 66 weeks with a median duration of 12 weeks. There was some suggestion that interventions lasting 6–12 months were associated with greater effects than shorter interventions. The frequency of messages varied from five times per day to once a month depending on the expected frequency of the targeted behaviour [18]. Most studies used tailored messages based on participant characteristics including age, gender or location and some personalised the messages. However, SMS design needs to take into account the possibility of annoyance, boredom, content blindness and potentially purposeful avoidance and mitigate for these [41]. It has been recommended that future studies ensure the intervention, including the SMS, was developed rigorously, that the SMS messages were suitable for the target population, tailored to individuals’ key characteristics such as their age and used the participant’s name. A systematic review of SMS interventions in adolescents highlighted the importance for young people of personal choice and that SMS should be positive, relevant, short and use informal language [42]. These considerations were factored into subsequent steps.
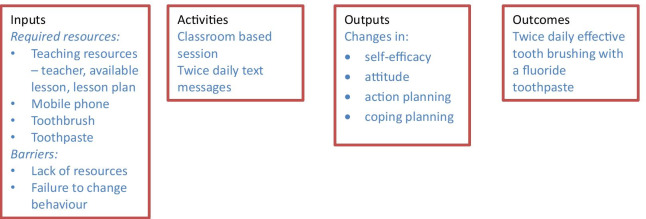
At the end of step 3 a logic model was developed (Fig. 2).
Fig. 2.
Intervention logic model
Step 4 Design the intervention with students, parents and school staff.
To build on step 3 and partner with school staff, students and parents to co-produce the intervention, workshops were held in schools in England, Wales and Scotland. Forty-five students attended the workshop and discussions were held with a further fifteen young people in the BRIGHT trial youth forum run by the youth empowerment charity Chilypep. A workshop was also held with 14 parents and discussions were held with three school teachers and a lecturer in secondary education.
Next, the results of the workshops with students and parents were used to decide on the best approach to engage students of this age. The outcome of these workshops was the decision that the lesson should contain a series of learning tasks and a case study for students to consider barriers to tooth brushing and help them identify solutions to coping with such challenges.
Students described the aspects of tooth brushing of interest to them namely wanting clean teeth and fresh breath. They described that showing the ‘disgusting’ or ‘scary’ consequences of poor oral health was likely to motivate them to brush their teeth more often. Students had excellent knowledge of the need to brush teeth twice daily but wanted to know more facts about what causes dental caries, the benefits of tooth brushing and the consequences of not brushing. The literature review suggested that while children are very aware that sugar causes dental caries they do not appreciate the role brushing with a fluoride toothpaste plays in the prevention of dental caries. The first section of the lesson plan therefore included a teacher-led description of:
The reasons tooth brushing with fluoride toothpaste is important.
The consequences of not tooth brushing.
The students were then asked to identify for themselves the benefits of tooth brushing and the consequences of not brushing their teeth. The students in the workshops were able to identify the barriers that stopped them brushing, particularly in the evening. The principle barrier for students without parental control at bedtime was being ‘too busy’ to brush their teeth, particularly playing games or chatting to friends online. Other barriers at bed time included being too tired (and falling asleep or forgetting to brush) and being on a sleepover. In the morning, the main barrier was not wanting to get out of bed to brush their teeth.
Feedback from school stakeholders suggested the CBS should be developed so it could be delivered by teachers with no training required and all necessary resources, including a lesson plan, provided.
The outputs of the workshop were also used as the basis of the SMS. Students expressed a preference for simple messages, which did not come across as ‘nagging’, did not attempt at humour, were personalised and that were written in full text rather than ‘textspeak’. They requested some choice over the timing of the messages that would arrive in the morning and at night, including later choice of timing at weekends plus the ability to stop the messages if they became annoying.
Parents were positive about the intervention in terms of the potential for reducing dental caries and improving tooth brushing. Parents felt a CBS may be more effective at improving tooth brushing than their efforts at home. Parents suggested the wording of the SMS would be important for their effectiveness and wanted assurance of security of the telephone numbers.
Step 5 Specify the intervention content.
Based on steps 2, 3 and 4 the components of the intervention were brought together. The behaviour change technique taxonomy (with associated codes provided in brackets) [43] was applied to select behaviour change technqiues based on the psychological determinants of tooth brushing behaviour (Table 1) and related to the causal model. This work predated the Theory and Technique Tool [44], but the behaviour change techniques selected are broadly supported by the links with mechanisms of action [45] constructs that relate to the determinants found in the causal model for this intervention (Table 1).
Table 1.
Behaviour change techniques and description
| Technique | Description |
|---|---|
| Information about health consequences (5.1) |
The CBS explained the effectiveness of fluoride toothpaste at improving oral health based on concerns of students i.e. appearance, social reasons, health reasons including reducing dental caries This information was reinforced with the SMS |
| Goal setting (1.1) | The CBS encouraged the students to decide to improve their brushing (intention development) through a personalised brushing plan |
| Problem solving (1.2, 1.4) | The CBS helped students identify barriers and facilitators to tooth brushing and to develop personalised brushing plans (action and coping planning) |
| Instruction on how to perform a behaviour (4.1) | The CBS included a video clip and factsheet to show students how to brush effectively.This is re-enforced through the SMS to develop self-efficacy |
| Action planning (1.4) | The CBS involved detailed planning of what the student will do, including a definition of the behaviour, specifying twice daily tooth brushing for 2 min in terms of where, when and how |
| Prompts/cues (7.1) | The CBS taught students to identify cues (associated with times of day and transitionary spaces) that can be used to remind them to brush their teeth |
The behaviour change technique codes are provided in brackets
Step 6 Translation of the intervention content into interventions features and piloting.
The final step involved integrating the content through discussions between members of the research team, external experts and further refinement work with the BRIGHT youth forum, parents, school nurses and teachers.
Development of the CBS
This first section of the CBS aimed to develop student’s motivation to brush their teeth and stimulate sufficient reason for them to want to change their behaviour [46]. This content of the CBS was consistent with the motivational factors of the HAPA, which were further developed in the second section of the CBS, which focused on self-efficacy.
The second section focused on self-efficacy in terms of how to brush teeth well. The workshop stimulated several key questions students wanted to know including how to physically brush teeth well and a video clip was incorporated into the lesson plan to address this. Several questions arose from the workshops that students were interested in having answers to, these were incorporated into a Frequently Asked Questions (FAQ) fact sheet. The FAQ fact sheet was designed and produced by the BRIGHT youth forum.
The third section of the CBS focused on action planning, coping planning and peer support. Students in the workshops were able to identify the barriers that stopped them from tooth brushing but they found it more difficult to derive their own practical solutions that would be appropriate for the BRIGHT intervention. This finding led to the inclusion of a case study approach involving a character who students could relate to; ‘Charlie’ was faced with the kinds of barriers identified in the workshops. This persona work allowed the teacher to provide examples of the solutions that might work for Charlie. Following this group activity individual students were encouraged to identify their own barriers and solutions.
The lesson plan and resources were then quality assured by two teacher educators. Using this feedback, minor amendments were made. The lesson was then delivered as a pilot to a class of students aged 12–13 years of age. This opportunity allowed refinement of the resources and lesson plan. The teachers delivering the lesson confirmed all necessary materials were available for it to be delivered without the need for specific training.
Development of the content of SMS
The previous steps allowed a list of 50 candidate SMS messages to be drafted. These messages were reviewed by fifteen young people with each message rated on a 3-point scale (bad, OK, good). Only the messages that were considered OK or good by the majority of the young people were selected for piloting by the BRIGHT youth forum who received twice daily messages for two weeks and they were asked to identify which messages they preferred. Additionally, the youth forum suggested which times should be offered for morning text and evening texts during the weekday and weekends. A final schedule of 28 messages (2 per day over 14 days) was developed to be repeated until the student requested these to stop.
Discussion
This paper has described the process through which a behaviour change intervention was developed using a theory and evidence-based approach, and a partnership approach [15] with the aim of improving the oral health of students aged 11–16 years attending secondary schools in the UK. The resultant intervention includes a CBS, delivered by school teachers which is re-enforced by a series of SMS messages delivered twice daily to student’s mobile telephones. The intervention development has been reported according to relevant guidelines [12].
The intervention was required to address the paucity of oral health promotion interventions for secondary school aged students (Public Health England, 2014) and attempted to integrate a traditional classroom-based delivery method complemented by a more novel mHealth technological solution. The strength of the intervention was its rigorous development based on behaviour change theory and designed with young people, parents and school staff. The CBS was developed to be embedded in the school curriculum which helped schools see the relevance of the topic and will facilitate future implementation. The SMS component was developed based on recommendations from previous studies on the need for the SMS to be appropriate for the target population, including diversity of messages to avoid annoyance, boredom and potentially content blindness [41].
However, as an intervention specifically designed to reduce dental caries, it has some limitations. First, the intervention was developed solely to focus on tooth brushing with a fluoride toothpaste and did not attempt to change other behaviours to reduce dental caries, specifically reduction of sugar consumption. This approach was chosen as the determinants of tooth brushing behaviours in young people are different to those related to diet and so the behaviour change techniques required are different. Further work is needed to develop effective, theory-driven oral health promotion programmes aimed at adolescents more generally.
Second, as stated in the logic model, the intervention requires students to have a mobile phone, a toothbrush and fluoride toothpaste. Providing toothpaste or toothbrushes as part of the intervention may be possible in some areas but would significantly influence the cost, particularly as the students would need regular supplies. One partial solution was letting students know, as part of the FAQ fact sheet, that cheap supermarket own brand oral hygiene products were available and as effective as branded products. While some students have limited access to mobile phones [19], there is also some research that suggests children with low socio-economic status have better mobile phone access than their more affluent peers [47].
The intervention is currently being evaluated through the BRIGHT randomised control trial which includes evaluation of (self-report and clinical) oral health outcomes and a mixed-methods process evaluation. The process evaluation plays an essential part in this trial, ensuring implementation, mechanisms of impact and context are assessed (Moore et al. 2015). Implementation will be explored in terms of the process through which the intervention (CBS and SMS) is delivered, what is delivered in different schools, the fidelity (consistency of delivery), dose (quantity of intervention delivered), reach (extent to which participants come into contact with intervention) and adaptations (alterations made to intervention for better contextual fit). The mechanisms of impact will be examined for how the intervention activities and student’s interactions with them trigger change in tooth brushing behaviours, self-efficacy, social norms, action and coping planning, self-determination and any unintended effects. Finally, context will be explored through examining the broader school culture and how it may have influenced and interacted with the delivery and functioning of the intervention and its outcomes. This includes external factors such as school structure and any changes to the curriculum. As a result of the outcome and process evaluation, further refinement of the intervention may be required.
Conclusion
In conclusion, this intervention to improve the oral health of secondary school students through tooth brushing, was rigorously developed based on behaviour change theory and work with young people, parents and school staff. Further research is needed to evaluate the outcomes and processes involved following the delivery of this intervention.
Acknowledgements
We would like to acknowledge the help received from the students, parents, schools involved and support from Alicia Ridout (mHabitat), Chilypep staff member https://www.chilypep.org.uk/ of the BRIGHT youth forum, trial staff from York Trials Unit and David Cooper (Headteacher of Batley Girls’ High School). Two of the authors of this paper (Peter Day and Zoe Marshman) are supported by the NIHR Applied Research Collaborations Yorkshire and Humber (NIHR ARC YH) NIHR200166 www.arc-yh.nihr.ac.uk. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR, the NHS or the Department of Health and Social Care.
Abbreviations
- mHealth
Mobile health
- CBS
Classroom-based session
- SMS
Short message service
- KOB
Keep on brushing
- HAPA
Health action process approach
- PSHE
Personal, social, health and economic
- FAQ
Frequently asked questions
- BRIGHT
Brushing reminder 4 good oral health
Authors' contributions
ZM was one of the co-PIs on the BRIGHT Trial, led the design of the intervention, prepared the original draft and refined the paper. SE led the literature review, liaised with the youth forum and contributed to refining the paper. IK was a co-applicant on the BRIGHT Trial and provided expertise in behaviour change throughout the development of the intervention and refinement of the paper. DD was a co-applicant on the BRIGHT Trial and provided expertise in education throughout the development of the intervention and refinement of the paper. MR led the school workshops in Scotland, was involved in the design of the intervention and refinement of the paper. IC was a co-applicant on the BRIGHT Trial, involved in the school workshops in Wales, brought expertise in caries prevention school-based programmes and refinement of the paper. SP and PD were co-applicants on the BRIGHT Trial, involved in the school workshops in England and refinement of the paper. MA was involved in the literature review and refinement of the paper. NI was one of the co-PIs on the BRIGHT Trial, was involved throughout the intervention development and refined the paper. All authors have read and approved the final manuscript.
Funding
This study has been funded by the National Institute for Health Research (NIHR), Health Technology Assessment (HTA) Programme. Project No. 15/166/08 Interventions to Improve Oral Health in Deprived Young People. The funding body influenced the design of the study.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available as permission was not sought but are available from the corresponding author on reasonable request. The intervention is currently undergoing evaluation and the resources may require further refinement before they are finalised. The current drafts are available from the corresponding author.
Declarations
Ethics approval and consent to participate
The intervention development was conducted as Patient and Public Involvement work prior to the start of data collection for the BRIGHT trial (registration number ISRCTN12139369, 10/05/2017). The East of Scotland Research Ethics Committee provided ethical approval for the BRIGHT trial (REC reference: 17/ES/0096). Informed consent was obtained from students, parents and the youth forum members. Details of the trial can be found at: BRIGHT: Brushing reminder 4 good oral health—Trials and Statistics, University of York. We confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jürgensen N, Petersen PE. Promoting oral health of children through schools–results from a WHO global survey 2012. Community Dent Health. 2013;30(4):204–218. [PubMed] [Google Scholar]
- 2.Public Health England 2014. Improving oral health: an evidence-informed toolkit for local authorities. PHE. London PSHE Association. 2014. PSHE Education programme of study (key stage 3) [Online]. Available: https://www.psheassociation.org.uk/system/files/PSHE%20Education%20Programme%20of%20Study%20%28Key%20stage%201-5%29%20Jan%202017_2.pdf. Accessed 9 Oct 2019.
- 3.American Academy of Pediatric dentistry Guideline on adolescent oral health care. Pediatr Dent. 2015;37:151–158. [PubMed] [Google Scholar]
- 4.Tsai C, Raphael S, Agnew C, McDonald G, Irving M. Health promotion interventions to improve oral health of adolescents: a systematic review and meta-analysis. Commun Dent Oral Epidemiol. 2020;48(6):549–560. doi: 10.1111/cdoe.12567. [DOI] [PubMed] [Google Scholar]
- 5.Calderon SJ, Mallory C. A systematic review of oral health behavior research in American adolescents. J Sch Nurs. 2014;30(6):396–403. doi: 10.1177/1059840514544034. [DOI] [PubMed] [Google Scholar]
- 6.Tolvanen M, Lahti S, Poutanen R, Seppä L, Hausen H. Children’s oral health-related behaviors: individual stability and stage transitions. Commun Dent Oral Epidemiol. 2010;38(5):445–452. doi: 10.1111/j.1600-0528.2010.00549.x. [DOI] [PubMed] [Google Scholar]
- 7.Marcolino MS, Oliveira JAQ, D'Agostino M, Ribeiro AL, Alkmim MBM, Novillo-Ortiz D. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018;6(1):e23. doi: 10.2196/mhealth.8873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armanasco AA, Miller YD, Fjeldsoe BS, Marshall AL. Preventive health behavior change text message interventions: a meta-analysis. Am J Prev Med. 2017;52(3):391–402. doi: 10.1016/j.amepre.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 9.Schluter P, Lee M, Hamilton G, Coe G, Messer-Perkins H, Smith B. Keep on brushing: a longitudinal study of motivational text messaging in young adults aged 18–24 years receiving work and income support. J Public Health Dent. 2015;75(2):118–125. doi: 10.1111/jphd.12079. [DOI] [PubMed] [Google Scholar]
- 10.Marshman Z, Ainsworth H, Chestnutt IG, Day P, Dey D, El Yousfi S, Fairhurst C, Gilchrist F, Hewitt C, Jones C, et al. Brushing reminder 4 good oral health (BRIGHT) trial: does an SMS behaviour change programme with a classroom-based session improve the oral health of young people living in deprived areas? A study protocol of a randomised controlled trial. Trials. 2019;20(1):452. doi: 10.1186/s13063-019-3538-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoddinott P. A new era for intervention development studies. Pilot Feasibility Stud. 2015;1(1):36. doi: 10.1186/s40814-015-0032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duncan E, O'Cathain A, Rousseau N, Croot L, Sworn K, Turner KM, Yardley L, Hoddinott P. Guidance for reporting intervention development studies in health research (GUIDED): an evidence-based consensus study. BMJ Open. 2020;10(4):e033516. doi: 10.1136/bmjopen-2019-033516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, Yardley L, Hoddinott P. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):e029954. doi: 10.1136/bmjopen-2019-029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Public Health England . Achieving behaviour change. London: Public Health England; 2020. [Google Scholar]
- 15.O’Cathain A, Croot L, Sworn K, Duncan E, Rousseau N, Turner K, Yardley L, Hoddinott P. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud. 2019;5(1):41. doi: 10.1186/s40814-019-0425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: an opportunity for oral health promotion. Bull World Health Organ. 2005;83(9):677–685. [PMC free article] [PubMed] [Google Scholar]
- 17.Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. London: Silverback Publishing; 2014. [Google Scholar]
- 18.Armanasco AA, Miller YD, Fjeldsoe BS, Marshall AL. Preventive health behavior change text message interventions: a meta-analysis. Am J Prevent Med. 2017;52:391–402. doi: 10.1016/j.amepre.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 19.L’Engle KL, Mangone ER, Parcesepe AM, Agarwal S, Ippoliti NB. Mobile phone interventions for adolescent sexual and reproductive health: a systematic review. Pediatrics. 2016;138:e20160884. doi: 10.1542/peds.2016-0884. [DOI] [PubMed] [Google Scholar]
- 20.Yaacob M, Worthington HV, Deacon SA, Deery C, Walmsley AD, Robinson PG, Glenny AM. Powered versus manual toothbrushing for oral health. Cochrane Library. 2014. [DOI] [PMC free article] [PubMed]
- 21.Marinho V, Higgins J, Logan S, Sheiham A. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Libr. 2003;203:CD002278. doi: 10.1002/14651858.CD002278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White D, Chadwick B, Nuttall N, Chestnutt I, Steele J. Oral health habits amongst children in the United Kingdom in 2003. Br Dent J. 2006;200(9):487–491. doi: 10.1038/sj.bdj.4813523. [DOI] [PubMed] [Google Scholar]
- 23.Zeedyk M, Longbottom C, Pitts N. Tooth-brushing practices of parents and toddlers: a study of home-based videotaped sessions. Caries Res. 2005;39(1):27–33. doi: 10.1159/000081653. [DOI] [PubMed] [Google Scholar]
- 24.Pine CM, Adair PM, Nicoll AD, Burnside G, Petersen PE, Beighton D, Gillett A, Anderson R, Anwar S, Brailsford S. International comparisons of health inequalities in childhood dental caries. Community Dent Health. 2004;21(1 Suppl):121–130. [PubMed] [Google Scholar]
- 25.Verrips G, Kalsbeek H, Van Woerkum C, Koelen M, Kok-Weimar T. Correlates of toothbrushing in preschool children by their parents in four ethnic groups in The Netherlands. Community Dent Health. 1994;11(4):233–239. [PubMed] [Google Scholar]
- 26.Gray-Burrows K, Day P, Marshman Z, Aliakbari E, Prady S, McEachan R. Using intervention mapping to develop a home-based parental-supervised toothbrushing intervention for young children. Implement Sci. 2016;11(1):61. doi: 10.1186/s13012-016-0416-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. 2008;57(1):1–29. doi: 10.1111/j.1464-0597.2007.00325.x. [DOI] [Google Scholar]
- 28.Scheerman JF, Loveren C, Meijel B, Dusseldorp E, Wartewig E, Verrips GH, Ket JC, Empelen P. Psychosocial correlates of oral hygiene behaviour in people aged 9 to 19—a systematic review with meta-analysis. Commun Dent Oral Epidemiol. 2016;44(4):331–341. doi: 10.1111/cdoe.12224. [DOI] [PubMed] [Google Scholar]
- 29.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- 30.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 31.Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006;132(2):249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- 32.Wieber F, Thürmer JL, Gollwitzer PM. Promoting the translation of intentions into action by implementation intentions: behavioral effects and physiological correlates. Front Hum Neurosci. 2015;9:395. doi: 10.3389/fnhum.2015.00395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Halvari AEM, Halvari H, Bjørnebekk G, Deci EL. Self-determined motivational predictors of increases in dental behaviors, decreases in dental plaque, and improvement in oral health: a randomized clinical trial. Health Psychol. 2012;31(6):777. doi: 10.1037/a0027062. [DOI] [PubMed] [Google Scholar]
- 34.Deci EL, Eghrari H, Patrick BC, Leone DR. Facilitating internalization: the self-determination theory perspective. J Pers. 1994;62(1):119–142. doi: 10.1111/j.1467-6494.1994.tb00797.x. [DOI] [PubMed] [Google Scholar]
- 35.Department of Education. Science programmes of study: Key stage 3, National curriculum in England [Online]. 2014a. Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/335174/SECONDARY_national_curriculum_-_Science_220714.pdf. Accessed 29 Jun 2017.
- 36.Department of Education. Science programmes of study: Key stage 4, National curriculum in England [Online]. 2014b. Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/381380/Science_KS4_PoS_7_November_2014.pdf. Accessed 29 Jun 2017.
- 37.Learning and Teaching Scotland. Curriculum for excellence, Health and wellbeing: experiences and outcomes [Online]. 2009a. Available: https://www.education.gov.scot/Documents/health-and-wellbeing-eo.pdf. Accessed 29 Jun 2017.
- 38.Learning and Teaching Scotland. Curriculum for excellence, Science: experiences and outcomes [Online]. 2009b. Available: https://www.education.gov.scot/Documents/sciences-eo.pdf. Accessed 29 Jun 2017.
- 39.Welsh Assembly Government. Personal and social education framework for 7-19 year olds in Wales [Online]. 2008. Available: https://hwb.gov.wales/curriculum-for-wales-2008/key-stages-2-to-4/personal-and-social-education-framework-for-7-to-19-year-olds-in-wales. Accessed 9 Oct 2019.
- 40.Hedman E, Gabre P, Riis U. Adolescents’ attitudes towards tobacco use and oral health: four “portraits”. Int J Qual Stud Health Well Being. 2008;3(4):248–255. doi: 10.1080/17482620802267431. [DOI] [Google Scholar]
- 41.Kocielnik R, Hsieh G. Send me a different message: utilizing cognitive space to create engaging message triggers. In: Proceedings of the 2017 ACM conference on computer supported cooperative work and social computing. portland, Oregon, USA: Association for Computing Machinery, 2017, pp. 2193–2207.
- 42.Loescher LJ, Rains SA, Kramer SS, Akers C, Moussa R. A systematic review of interventions to enhance healthy lifestyle behaviors in adolescents delivered via mobile phone text messaging. Am J Health Promot. 2018;32(4):865–879. doi: 10.1177/0890117116675785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, Eccles MP, Cane J, Wood CE. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 44.Johnston M, Carey RN, Connell Bohlen LE, Johnston DW, Rothman AJ, de Bruin M, Kelly MP, Groarke H, Michie S. Development of an online tool for linking behavior change techniques and mechanisms of action based on triangulation of findings from literature synthesis and expert consensus) Transl Behav Med. 2020;11:1049–1065. doi: 10.1093/tbm/ibaa050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carey RN, Connell LE, Johnston M, Rothman AJ, de Bruin M, Kelly MP, Michie S. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med. 2019;53(8):693–707. doi: 10.1093/abm/kay078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stokes E, Ashcroft A, Platt M. Determining liverpool adolescents' beliefs and attitudes in relation to oral health. Health Educ Res. 2006;21(2):192–205. doi: 10.1093/her/cyh055. [DOI] [PubMed] [Google Scholar]
- 47.Militello LK, Kelly SA, Melnyk BM. Systematic review of text-messaging interventions to promote healthy behaviors in pediatric and adolescent populations: implications for clinical practice and research. Worldviews Evid Based Nurs. 2012;9(2):66–77. doi: 10.1111/j.1741-6787.2011.00239.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available as permission was not sought but are available from the corresponding author on reasonable request. The intervention is currently undergoing evaluation and the resources may require further refinement before they are finalised. The current drafts are available from the corresponding author.