Highlights
-
•
Among HICs, uniform declines in premature death from CVD and cancer were observed.
-
•
Cancer mortality exceeded CVD in 9 of 10 HICs in 2000 and in all 10 by 2019.
-
•
CVD mortality exceeded cancer in all MICs in 2000, and in 8 countries by 2019.
-
•
Less than half of the studied countries are predicted to meet the SDG 3.4 target.
-
•
Evidence-based, prioritized, costed and financed programmes are needed to accelerate progress.
Keywords: Cancer, Cardiovascular disease, Premature mortality, SDGs, Epidemiology
Abstract
With the 2030 Sustainable Development Goals (SDG) target of a one-third reduction in noncommunicable diseases (NCDs) less than a decade away, it is timely to assess national progress in reducing premature deaths from the two leading causes of mortality worldwide. We examine trends in the probability of dying ages 30–70 from cardiovascular disease (CVD) and cancer 2000–19 in 10 middle-income (MICs) and 10 high-income (HICs) countries with high quality data. We then predict whether the SDG target will be met in each country for CVD, cancer and for the four main NCDs combined. Downward trends were more evident in HICs relative to the MICs, and for CVD relative to cancer. CVD and cancer declines ranged from 30–60% and 20–30% in HICs over the 20-year period, but progress was less uniform among the MICs. Premature deaths from cancer exceeded CVD in nine of the 10 HICs by 2000 and in all 10 by 2019; in contrast, CVD mortality exceeded cancer in all 10 MICs in 2000 and remained the leading cause in eight countries by 2019. Two of the 10 MICs (Colombia and Kazakhstan) and seven of the HICs (Australia, Chile, Italy, New Zealand, Norway, Slovakia, and the U.K.) are predicted to meet the SDG NCDs target. Whether countries are on course to meet the target by 2030 reflects changing risk factor profiles and the extent to which effective preventative and medical care interventions have been implemented. In addition, lessons can be learned given people living with NCDs are more susceptible to severe COVID-19 illness and death.
Introduction
Twenty years have passed since governments adopted the UN Political Declaration on Noncommunicable diseases (NCDs) and committed to action to combat premature mortality from NCDs. Cardiovascular diseases (CVD), cancer, diabetes and chronic lung disease dominate the premature mortality landscape. These and all other NCDs have been estimated to be responsible for over three-quarters (77.0%) of the 20.4 million deaths at ages 30 to 70 worldwide in 2019 [1], and the burden is expected to rise over the next decades as populations’ age, communicable diseases are progressively controlled, and the prevalence of key risk factors for NCDs increases. The inclusion of the target of a one-third reduction in premature mortality (ages 30–70) from the four major NCDs, as part of the UN 2030 Sustainable Development Goals (SDG target 3.4 [2]), thus reflects the global importance of chronic diseases and the health, social, and economic benefits of their control.
In the 25 most populated countries of the world, a recent Lancet report highlighted that the NCDs target is likely to be met upon a modest acceleration in the recently declining premature mortality trends [3]. A study of 52 countries primarily in high- and upper-middle-income countries indicated a 30% reduction in NCDs was feasible by 2030 [4]. On the other hand, the most recent study by the NCD Countdown 2030 collaborators projected that the rate of change in premature mortality was too slow to achieve SDG 3.4, with only women in 17 countries and men in 15 countries on track to meet the target [5].
Given CVD and cancer are responsible for over two-thirds of all premature deaths from NCDs and are also the two leading causes of premature mortality worldwide, there is clear utility in understanding how the national trajectories of these specific diseases differ, given distinct as well as intersecting interventions are effective for their prevention and control [6], [7], [8]. The focus of this study is thus the assessment of trends in the probability of death of the two diseases over the period 2000–19 in a subset of countries with robust mortality data, but varying levels of income. The primary aim is to assess national trajectories 2000–19 and their likely impact on SDG target 3.4 by the year 2030, assuming a baseline year of 2015.
Data and methods
We selected 20 geographically and economically diverse countries spanning five continents where the mortality data series from civil and vital registration systems (CRVS) were of reasonable quality [9], and for which CVD (ICD-10 I00-I99) and cancer (ICD-10 C00-C97) were the two leading causes of death in 2019. Countries were partitioned into two income groups according to current World Bank definitions based on gross national income (GNI) per capita [10]. The middle-income countries group (MICs) comprised the Philippines, Ukraine and Uzbekistan (classified as lower-middle income economies with a GNI per capita between $1,036 and $4,045) and Brazil, Bulgaria, Costa Rica, Colombia, Kazakhstan, Mauritius, Mexico (upper-middle income economies with a GNI per capita between $4,046 and $12,535). The high-income countries group (HICs with a GNI per capita of $12,536 or more) comprised Australia, Chile, France, Italy, Japan, New Zealand, Norway, Slovakia, the UK, and the U.S.
To assess recent trends in the 20 countries, we extracted the unconditional probabilities of dying between ages 30 and 70 years from CVD, cancer, diabetes (ICD-10 E10-E14) and chronic respiratory diseases (ICD-10 J30-J98) for the years 2000–19 in both sexes combined from CVD, cancer and for the four major NCDs combined, CVD, cancer, as well as from the WHO’s Global Health Estimates (GHE) [1]. To assess the change in these trends set against the SDG target 3.4, we calculated the percentage change in the probability of dying from CVD, cancer, and the four NCDs combined for each country 2000–19. A linear extrapolation of this trend was then used to predict the corresponding year when the national target of a one-third reduction would likely be met for each of the three disease groups, relative to the baseline of 2015, the year in which the United Nations Member States set the health-related targets.
Results
Trends in CVD and cancer 2000–19
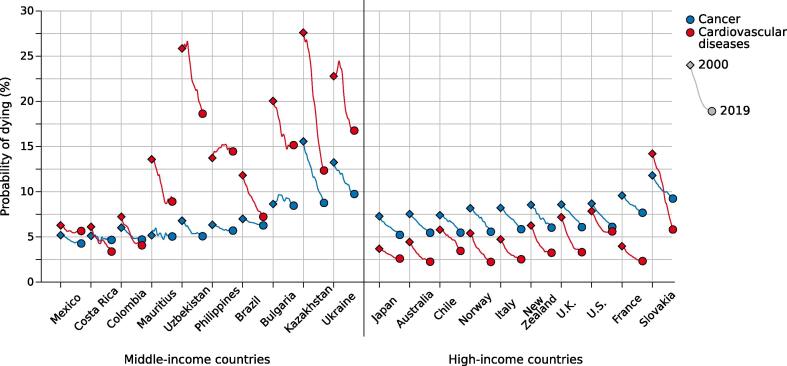
Fig. 1 portrays the trends in the probability of premature death from cancer and CVD annually in both sexes combined over the 20-year period, 2000–19. Countries are shown in ascending order of their magnitude in 2019 within the two income levels. The probability of death from both diseases was much higher in the majority of MICs relative to the 10 HICs at the start of the study period, with an up to 10-fold and 2.5-fold variation in CVD and cancer respectively among the former in 2000. This disparity tended to narrow over the 20 years, though the steady declines in both diseases in all HICs contrasted with the fluctuations in the direction and magnitude of the trends in CVD and cancer among the MICs. The corresponding trends in males and females are provided in the Appendix (Fig. A1, Fig. A2, respectively).
Fig. 1.
Trends in the unconditional probability of dying between ages 30 and 70 years from cardiovascular diseases and cancer 2000–19 in middle-income (left panel) and high-income countries (right panel). Both sexes. Countries within income group are ordered in terms of increasing probability of dying from cancer in 2019. Source: WHO Global Health Estimates [1].
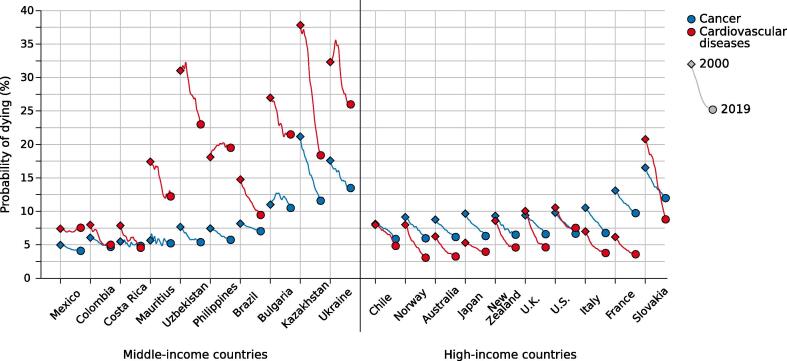
Fig. A1.
Trends in the unconditional probability of dying between ages 30 and 70 years from cardiovascular diseases and cancer 2000–19 in middle-income (left panel) and high-income countries (right panel). Males. Countries within income group are ordered in terms of increasing probability of dying from cancer in 2019. Source: WHO Global Health Estimates [1].
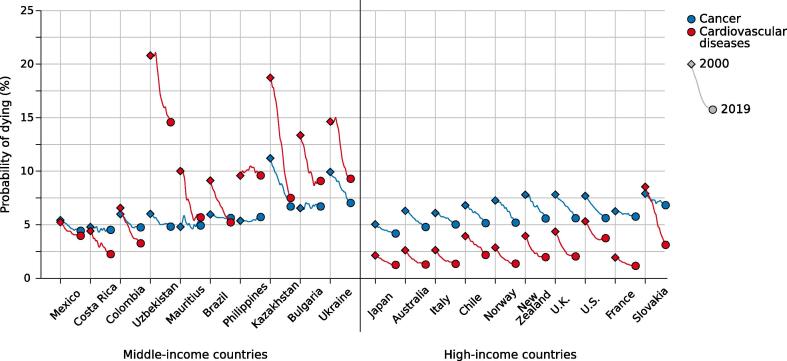
Fig. A2.
Trends in the unconditional probability of dying between ages 30 and 70 years from cardiovascular diseases and cancer 2000–19 in middle-income (left panel) and high-income countries (right panel). Females. Countries within income group are ordered in terms of increasing probability of dying from cancer in 2019. Source: WHO Global Health Estimates [1].
The absolute percentage change in the magnitude of the probabilities of death in 2000–19 is quantified in Table 1. The declines tended to be larger in HICs relative to MICs, and for CVD relative to cancer. Five of the 10 MICs, and eight of the 10 HICs, saw declines in CVD mortality of greater than 30% from 2000 to 2019. For cancer, Kazakhstan was an outlier, being the only MIC where the corresponding decline was of the same order of magnitude, while in the HICs, the magnitude of the trends was more homogenous, with declines in the range of 20–30% observed over the two decades. The corresponding yearly percentage change in diabetes and respiratory disease 2000–19 is provided in the Appendix (Table A).
Table 1.
Change in cumulative risk of premature mortality (ages 30–69) from CVD, cancer and the four major NCDS combined (CVD, cancer, COPD and diabetes) between 2000 and 2019 (with 95% confidence intervals), plus the predicted year that the SDG 3.4 will be met from the baseline year of 2015.
| Income level/ Country1 |
CVD 2000–19: % change (95 %CI)2 |
Predicted year SDG target met3 |
Cancer 2000–19: % change (95 %CI)2 |
Predicted year SDG target met3 |
Four major NCDS 2000–19: % change (95 %CI)2 |
Predicted year SDG target met3 |
|---|---|---|---|---|---|---|
| Middle-Income | ||||||
| Brazil | −38.8 (-48.4 to −25.2) | 2028 | −10.3 (-26.1 to 10.5) | 2073 | −28.4 (-40.2 to −12.2) | 2034 |
| Bulgaria | −24.3 (-50.8 to 11.9) | 2040 | −2.1 (-43.4 to 56.6) | – | −15.1 (-45.7 to 25.7) | 2055 |
| Colombia | −43.7 (-64.3 to −11.0) | 2026 | −21.8 (-53.9 to 30.3) | 2041 | −35.7 (-61.0 to 3.9) | 2029 |
| Costa Rica | −44.8 (-65.7 to −12.2) | 2025 | −8.9 (-49.1 to 60.3) | 2079 | −26.0 (-57.3 to 25.8) | 2037 |
| Kazakhstan | −55.3 (-70.4 to −35.5) | 2023 | −43.7 (-63.9 to −12.5) | 2026 | −45.9 (-63.9 to –22.2) | 2025 |
| Mauritius | −34.4 (-56.5 to −3.6) | 2031 | −2.4 (-42.9 to 65.3) | – | −20.3 (-49.0 to 21.8) | 2044 |
| Mexico | −9.9 (-31.6 to 17.8) | 2078 | −17.8 (-39.5 to 13.6) | 2047 | −6.9 (–32.3 to 27.2) | – |
| Philippines | +5.3 (–32.0 to 53.9) | – | −10.2 (-43.1 to 42.3) | 2074 | +6.0 (-31.2 to 57.4) | – |
| Ukraine | −26.4 (-48.4 to 3.5) | 2036 | −26.4 (-54.2 to 14.7) | 2036 | −26.5 (-49.0 to 4.2) | 2036 |
| Uzbekistan | −27.9 (-46.3 to −5.0) | 2033 | −25.3 (-54.3 to 15.8) | 2036 | −26.1 (-46.8 to 1.4) | 2035 |
| High-Income | ||||||
| Australia | −49.3 (-63.5 to −30.2) | 2024 | −27.5 (-50.1 to 4.7) | 2034 | –33.7 (-53.7 to −5.6) | 2030 |
| Chile | −40.5 (-57.7 to −16.4) | 2024 | −26.0 (-50.5 to 11.4) | 2033 | −29.9 (-52.8 to 3.6) | 2030 |
| France | −41.5 (-59.6 to −15.2) | 2027 | −19.9 (-45.0 to 16.8) | 2043 | −24.9 (-48.1 to 9.6) | 2037 |
| Italy | −46.7 (-55.5 to −34.0) | 2025 | −28.8 (-40.9 to −14.3) | 2032 | –33.9 (-45.6 to −19.6) | 2030 |
| Japan | −29.3 (-39.8 to −15.9) | 2034 | −28.2 (-38.4 to −16.6) | 2033 | −27.6 (-39.1 to −13.5) | 2035 |
| New Zealand | −48.1 (-61.2 to −31.1) | 2026 | −29.4 (-50.9 to 0.8) | 2032 | −35.6 (-53.8 to −10.5) | 2030 |
| Norway | −58.7 (-65.6 to −49.9) | 2022 | −31.7 (-45.4 to −14.2) | 2031 | −39.2 (-51.6 to −24.1) | 2027 |
| Slovakia | −59.0 (-74.6 to −36.2) | 2021 | −21.7 (-55.3 to 32.9) | 2040 | −39.0 (-63.5 to −2.7) | 2027 |
| U.K. | −53.8 (-59.6 to −47.7) | 2024 | −29.2 (-38.3 to −18.1) | 2031 | −37.4 (-46.2 to −27.7) | 2028 |
| U.S. | −28.7 (-39.7 to −16.6) | 2036 | −29.6 (-38.4 to −17.9) | 2032 | −24.9 (-36.0 to −12.3) | 2038 |
1. Based on the World Bank classification
2. % change in probability of death at ages 30–69 from 2000 to 2019
3. Year predicted from a linear interpolation of the % change 2000–19 e.g. assuming these trends continue into the future, using the year 2015 as baseline “-“ denotes SDG target predicted to not be met over the course of the 21st century
Trends in MICs
Among the MICs, the probability of death from CVD was consistently higher than that of cancer in the year 2000 (Fig. 1, left panel), as was the magnitude of the decline in subsequent years (Table 1). The rate of CVD decline varied considerably, from 10% in Mexico were to 39–55% in Brazil, Colombia, Costa Rica and Kazakhstan; the Philippines was an exception, where an increase in CVD of 5% was observed. As well as Kazakhstan (a 44% decrease in the probability of death), the largest declines in cancer were seen in Ukraine and Uzbekistan (around 25%). In contrast, the cancer declines were rather minor, around 2% over the two decades, in Bulgaria and Mauritius.
Irrespective of the temporal developments, the probability of death from CVD remained higher than that of cancer in 8 of the 10 MICs by 2019. The exceptions were Colombia and Costa Rica, where cancer surpassed CVD because of a larger decline in CVD relative to cancer (Table 1). An outlier was the Philippines, in which the gaps in premature death appeared to widen, given the opposing trends in CVD and cancer.
Trends in HICs
Among the HICs, a downward trend in the probability of death from both diseases was observed in all countries 2000–19; for CVD the declines ranged from less than 30% in Japan and the U.S., to over 50% in Norway, Slovakia and the U.K. For cancer, the declines ranged from 20–22% in France and Slovakia to 29–31% in New Zealand, Norway, the U.K. and the U.S. (Table 1).
In stark contrast to the relative positioning of CVD and cancer in MICs, the probability of premature death from cancer among the HICs already exceeded CVD in 9 of the 10 studied countries by 2000 (Fig. 1, right panel). With the uniformly downward mortality trends observed for both CVD and cancer, the ranking remained unchanged over the subsequent two decades. Slovakia was the only nation with a higher probability of premature death from CVD than cancer in 2000 among HICs, but this ranking reversed over subsequent years because of the relatively greater CVD mortality decline. Thus, in all 10 HICs studied, cancer was the leading cause of premature death by 2019. An interesting, but preliminary observation was the possible deceleration or stabilisation in the CVD trends within the five most recent years, notably among HICs, including Australia, Italy, New Zealand, the U.K. and the U.S.
Trends in the four major NCDs 2000–19
The percentage change in the probability of death from the four major NCDs is included in Table 1. The probability of death from the four major NCDs fell in all 20 countries from 2000 to 2019, with the exception of the Philippines. There was considerable variation in the magnitude of the decline, particularly among the MICs that ranged from 7% in Mexico to over 35% in Colombia and Kazakhstan. The declines were more uniform in the HICs, ranging from a 25% drop in the U.S. over the 20-year period to over 35% in New Zealand, Norway, Slovakia and the U.K.
Will the SDG target 3.4 be met by 2030?
The predicted year that a one-third reduction in premature death from the four major NCDs relative to the baseline of 2015 is given in Table 1. Two of the 10 MICs (Colombia and Kazakhstan) and seven of the HICs (Australia, Chile, Italy, New Zealand, Norway, Slovakia and the U.K.) are predicted to meet the one-third reduction by 2030, assuming past trends continue into the future (Table 1). A further four MICs (Brazil, Costa Rica, Ukraine and Uzbekistan) and the remaining three HICs (France, Japan and the U.S.) will meet the target between the years 2031 and 2040. According to the predictions, Bulgaria and Mauritius will reach the target in 2044 and 2055 respectively, while Mexico and the Philippines will not meet the target in this century.
Discussion
CVD and cancer rank as the first and second leading premature causes of death in almost 130 countries worldwide, and are within the top three causes in close to 180 countries [11]. Our analysis of premature mortality in 20 diverse countries with robust data makes it clear that while progress has been made, there remains marked diversity in the underlying risk profiles at the national level. Some of the factors contributing to the CVD and cancer burden are shared and are indeed critical in developing prevention strategies for NCDs overall, including tobacco and alcohol consumption, physical inactivity and obesity. Time trends thus reflect ongoing shifts in the prevalence of these determinants, and whether policies for control are effectively implemented [12], [13], [14]. Looking into the determinants and the respective degree of progress in combatting CVD and cancer in more depth, three key messages can be highlighted.
Firstly, among the 10 HICs under study, declines in premature death from CVD and cancer were observed in this millennium, a reduction ranging from around 30–60% and 20–30% from 2000 to 2019, respectively. The declining trends in CVD in each of 10 HICs mirror the trajectories of mortality rates from coronary heart disease and stroke reported across numerous countries in the industrialized world that began in the 1960s, in North America, North and Western Europe, Asia (Japan) and Oceania (Australia and New Zealand) [15], [16], [17], [18]. They stem from technical proficiencies in the prevention of CVD including a lowering of serum cholesterol and blood pressure (linked to improvements in diet), as well as medical and surgical interventions. These include the control and treatment of hypertension, the increased use of statins to lower cholesterol in the blood, and use of thrombolysis and stents in acute coronary syndrome to prevent infarction [15]. With reductions in smoking prevalence and salt intake also possible explanatory factors, there have been considerable efforts to assess the relative contribution of primordial versus primary prevention [19], [20], [21]. There are however considerable variations reported between countries, in part dependant on the indicator used [22] Moreover, a rising prevalence of obesity, physical inactivity and alcohol consumption has been reported in many countries that, without further intervention, may change the CVD landscape in future decades.
A notable but still speculative finding in our study is the possible deceleration or stabilisation in very recent CVD trends in a number of countries, including Australia, Italy, New Zealand, the U.K. and the U.S. This finding has already been highlighted in the latter country [23], while Ezzati and Leon have, in noting the broad declines in CVD mortality and their contribution to increasing life expectancy [18], also highlighted that progress may be compromised in the wake of the continuing epidemic of obesity and rising levels of diabetes, The recent stagnation in the U.S. rate of decline in CVD mortality from 2011 – among men and women and among blacks and whites – as well as the flattening out of trends among younger age groups, has been linked to these adiposity-related factors, including uncontrolled levels of blood pressure [24]. Such trends are also postulated as the main reason that increasing U.S. life expectancy has come to a halt [25]. More broadly, Adair and Lopez have recently reported a deceleration in CVD mortality rates declines at ages 35–74 in a number of countries, and some evidence of increasing rates [26].
The uniform declines in premature cancer death among HICs are seen more recently than for CVD, with the peak and decline in corresponding cancer mortality first observed in the early-1990s in the U.S. [27], [28] and in several Northern and Western European countries [29], [30]. Prior to the downturn, deliberations on the perceived lack of progress against cancer and the relative capability of different strategies to control the disease was a mainstay in the literature [31]. Certainly, interpreting overall cancer mortality trends is complex, given they comprise a multiple number of cancer types and subtypes for which numerous risk factors and specific primary, secondary and tertiary interventions have all potentially contributed to their direction and magnitude [28]. The present gap can however be considered at least partially the result of a limited investment in early diagnosis and treatment of cancer [65]. Further, several major cancers associated with a poor prognosis – including cancers of the (non-cardia) stomach and liver cancer– are infectious in origin. A number of “unplanned” primary prevention measures have served to reduce rates of the former subtype for many decades [32], while the introduction of HBV vaccination from the 1980s is likely to have a long-term impact on reducing hepatocellular carcinoma rates [33].
Nevertheless it is noteworthy that just four cancers (lung, colorectum, female breast and pancreas), each linked to one or more key risk factors for CVD – tobacco, alcohol and obesity – explain around half of the premature cancer burden in the 10 HICs included in this study. Lung cancer explains about 1 in 5 premature deaths, and while the disease is the most common cancer caused by cigarette smoking, at least 19 other cancer sites or subsites are causally related to smoking, including colorectal and pancreatic cancer [34], [35]. The current patterns and trends in premature cancer death thus partly reflect the maturity of the tobacco epidemic and sex-specific differentials in historic tobacco exposure, for which prevalence has diminished in the 10 HICs under study over the last decades, although there is considerable temporal variability in the proportion of adult smokers by country and sex [36]. In women, for instance, smoking prevalence has halved from 2000 to 2015 to about 14% in Australia and New Zealand, while it is stable at around 27% in France and increasing in Slovakia, with national smoking prevalence estimated at 27% by 2015 [36].
Advances in therapy and the adoption of best practices in cancer diagnosis and management are likely important explanatory factors for the colorectal cancer trends observed in the HICs [37], although survival differentials still exist [38]. While population-based screening have had an impact in some settings, programmes are quite recent and only fully implemented in a handful of countries [39]. Established risk factors for colorectal cancer include the consumption of alcohol, a high intake of red and processed meat, obesity and sedentary lifestyle [40]. Although incidence declines have been linked to healthier lifestyles, such as diets rich in fibre, the increases in incidence rates among recent generations in several high-income populations aged under 50 years is a concern [41]. Similarly, female breast mortality rates have been in decline in most high-income countries, despite a rising or stable incidence trend. The former have been attributed to multiple factors including early detection through mammography and a number of breakthroughs in treatment [42]. A study from Norway estimated 20% and 23% reductions in breast cancer mortality as a result of screening invitations and treatment improvements, respectively, among women aged over 50 years [43] – although the relative contributions of these factors must certainly vary by countries. The downward trends in incidence rates in a number of high-income countries, following a reduction in the use of post-menopausal hormonal therapy during the 2000 s [44], [45], [46] may have also had some knock-on effect on the probability of premature death. Lastly, it is worth noting that relative to the successes in prevention of the aforementioned cancers – which are amenable to one or more effective preventative or curative interventions – pancreatic cancer has become a leading cause of premature death by virtue of its consistently poor prognosis. Trends are difficult to decipher, and to-date, the aetiology is not well understood, with about one in five of all pancreatic cancer deaths attributed to tobacco smoking, with alcohol and obesity also likely playing a role. While pre-existing type 2 diabetes is associated with higher risk, there remains the prospect of reverse causation, whereby pancreatic cancer can induce diabetes [47]. Irrespective of the underlying causes, the disease is predicted to become a leading cause of cancer death in the European Union by 2025 [48].
Secondly, and in contrast to the HICs, progress is less uniform among MICs. On the positive side, there are evidently major recent successes in CVD control, where reductions of between 30% and 60%, within the range of the HICs, were observed in half of the MICs under study. In Brazil, where CVD and cancer are the causes of over half the deaths among adults, declining death rates at ages 45–64 in ischaemic disease (IHD) and stroke, as well as other cardiovascular diseases have been reported [49], as they have for IHD and stroke in Ukraine and Kazakhstan at ages 25–64 [50]. Yet high mortality rates in MICs persist with rates two to seven times higher than those of the 10 HICs studied here. The recent PURE study reported that 70% of CVD cases could be attributed to a few amenable risk factors, with hypertension and tobacco use being the dominant global determinants, whereas high cholesterol and low education were more important in HICs and MICs, respectively [51]. Ukraine and Kazakhstan both have a high prevalence of smoking and hypertension [50], while the EUROASPIRE V survey reported the majority of high-risk CVD patients in 24 countries – predominantly in Southern and Eastern Europe, and including Bulgaria, Kazakhstan and Ukraine – had failed to attain lifestyle, blood pressure, lipid and glycaemic targets [52]. Despite recent declines in CVD mortality, alongside declines in smoking and hypertension, concomitant rises in obesity and type II diabetes have been reported in Kazakhstan and Ukraine [50]. In supporting health system reforms and tackling NCDs in Kazakhstan, WHO EURO has provided a cost-benefit analysis that sets implementation costs against health gains, identifying national policies that would provide optimal returns on investment [53].
Population-based interventions including those targeting reduced salt intake and tobacco consumption have been shown to be highly cost-effective in low- and middle-income settings, with a potential to generate economic gains that can be reinvested. The exceptional increasing trend in CVD premature mortality rates observed in the Philippines has been noted previously [17], with one estimate indicating that over 18,000 premature deaths could be averted upon the introduction of a tax on sweetened beverages [54], increasingly seen as a cost-effective measure to drive down NCDs [55]. A recent report has revealed that an investment in the prevention and control of NCDs in the country could prevent over 350,000 premature deaths 2015–30 [56].
While challenges in implementation remain [57], the recent PolyIran and the International Polycap Study (TIPS-3) trials [58], [59] have revealed the promise of the polypill approach to prevention, reporting 5-year outcomes of a fixed-dose combination therapy of a formulation of statins, blood pressure-lowering drugs, and aspirin. In the Iranian trial, the polypill group had a 34% lower risk of major cardiovascular events than those receiving usual care [58], while in the multi-centre TIPS-3 study, the polypill group had a 31% lower risk than those randomly assigned to receive double placebo [59]. Such findings aligns with the WHO ‘best buys’ package for reducing total CVD risk that supports the inclusion of multidrug therapy for cardiovascular disease prevention, including the treatment of new cases of acute myocardial infarction with acetylsalicylic acid [12]. The approach is also highly-cost effective, with Bertram et al reporting that investment in preventative interventions of an additional $1·50 per capita per year could avert 15 million deaths, as well as 8 and 13 million incident cases of stroke and ischaemic heart disease in 20 countries over the period 2015–2030 [60].
There are sharp contrasts between MICs and HICs in terms of the cancer trends; the declines in MICs range from the relative outlier of Kazakhstan with a 44% decrease from over the 20-year period, to 15–25% in a further four countries, through to 2–10% elsewhere. Such divergent trends provide a snapshot of the current “cancer divide” and the need for a concerted global effort to deliver effective preventative and curative cancer interventions in transitioning economies as a means to close it [61]. In a global review of national cancer planning, four-fifths of countries had cancer-related policies by 2015, an improvement from 2000, with those with national cancer control plans (NCCPs) addressing the elements of cancer control more comprehensively than those countries with NCD plans alone [62]. In many MICs however, there remains an overwhelming need for evidence-based programmes to be appropriately costed and financed, and made operational according to level of resource and the local cancer profile [62]. Guidance to policy makers comes from the WHO package of best buys for cancer [12] and an essential package of potentially cost-effective cancer measures from the third edition of Disease Control Priorities [63]. In addition a checklist of core elements of NCCPs has been developed that seek to facilitate governments in the processes of formulating, implementing and evaluating cancer plans in diverse settings [64]. The WHO Cancer Report on Cancer sets as a priority the early diagnosis and treatment of curable cancers, which will be a critical driver to national progress in meeting the premature mortality target [65]. A complementary launch of three WHO initiatives aims to support the commitments of WHO Member States to strengthen and scale-up services to tackle the inequitable cervical [66], breast [67] and childhood cancer [68] burden and outcomes worldwide.
Thirdly, less than half of high- and middle-income nations are predicted to meet the SDG 3.4 target of a one-third reduction in premature mortality from the four major NCDs by 2030 – in two of the ten MICs and in seven of the HICs. This is broadly in line with other studies showing the pace of decline varies substantially, even within world area [3], [69], with HICs in regions within the Asia-Pacific, North America, Northern and Western Europe more likely to be on track to attain the NCD target by 2030 than MICs. The stratified analyses for CVD and cancer suggest a somewhat more complex picture, with declines in the probability of death greater for CVD than cancer.
This paper has several strengths as well as weaknesses. We selected countries across five continents where underlying mortality data were considered of reasonable quality and for which CVD and cancer ranked as leading causes of premature death. In that sense the study is sufficiently comprehensive to provide insight into the relative progress in controlling the two diseases in geographically- and income-diverse settings, and in tracking whether countries are on course to meet the SDG NCD target as a result. The trade-off in having such a focus is the inevitable exclusion of countries and subpopulations for which the mortality profile and trends may radically differ. A major limitation was thus our inability to include an equivalent situation analysis of countries classified as low-income countries, stemming from a paucity of data available; WHO have reported that one-third of Member States (MS) have no primary data on over half of the 18 relevant indicators required for monitoring the SDGs [70], with cause-of-death data complete and of high quality in only one-quarter of MS [71]. The completeness of mortality data in the WHO African region, for example, is 6%, the very region where estimates of the probability of dying from NCDs is greatest [69]. While the global dominance of NCDs is clear, the extent of epidemiologic transition towards the major types including CVD and cancer depends on national trajectories of social and economic development. The trends in both diseases are unfavourable in low-income settings [69], with many countries now faced with a double burden of deaths from NCDs and infectious diseases [72], as well as syndemics involving NCDs [8].
Another limitation was the specific focus on monitoring CVD and cancer trends pertinent to the SDG target 3.4. In so doing we discounted the complex patterns and trends in mortality according to disease or demographic subgroups. Populations above the age of 70 years are not studied here, yet this group represents a considerable and growing proportion of the risk of mortality from NCDs. Patterns and trends by cancer and CVD stratified by sex, age, and socioeconomic group reveal major differences [69], [73]. Further, differentials in the trends in coronary heart disease and stroke – collectively explaining 80% of CVD premature deaths – are well-established [15], [17]. Cancer-specific trends are equally diffuse, given cancer is a collective of multiple diseases – 15 cancer types explain the equivalent 80% global burden – with many determinants and interventions across the cancer continuum [74]. Clearly further elucidation and tracking in subgroups is highly relevant but could not be afforded within this study.
In response to the growing NCD burden, governments have committed to the scale-up of efforts to prevent and treat NCDs in line with the UN Agenda for Sustainable Development and Universal Health Coverage. Given the direct link between well-functioning CRVS and improved health outcomes [75], it is perhaps not surprising that the HICs studied here fare relatively better, with respect to meeting the NCD target by 2030. A global analysis suggests the majority of countries will fail to meet it however [76], despite the demonstration of a high return from their investment in NCD control to countries at all income levels [77]. Noting this, the WHO Independent High-Level Commission on NCDs recommended political leadership in multi-sectoral engagement, sustainable financing and a prioritisation of selected investments that would serve as a driver to further actions needed to reach the target. Investing in CVD prevention has been shown to be vital in attaining SDG 3.4 [60]. Reducing the prevalence of risk factors amenable to prevention (and included among WHO's best buys for NCD control) – tobacco use, harmful alcohol consumption, obesity as well as raised blood pressure – was projected to reduce premature mortality from CVD by 34% by 2025 from 2010 levels, if the specific WHO “25 by 25” risk factor targets met [7]. Yet the overall reduction for cancer was just 7%, owing to its extended latency, the relative delay in the benefits of specific interventions, as well as the greater heterogeneity in risk factors - relative to CVD and other NCDs, signalling the need for governments to adapt and integrate national cancer control plans tailored to the local cancer profile [6].
The extrapolation of the national trends to predict the year in which countries may reach the SDG 3.4 target does not account for the impact of the COVID-19 pandemic. Yet a recent WHO review highlighted the role of NCDs and the underlying risk factors in increasing susceptibility to COVID-19 infection and the likelihood of poorer outcomes [78]. A survey conducted from March to June 2020 revealed that every country had had disruption of health services, and for NCDs, diagnosis and treatment were affected in 69% of countries surveyed [78], [79]. Evidently, there are lessons to be learned as the world ‘builds back better’, given people living with NCDs are at high risk of severe COVID illness and death.
In summary, in a group of 20 of high- and middle-income nations, uniform declines in premature death from CVD and cancer were observed in this millennium in HICs, whereas progress was more mixed among MICs, with greater success evident in the control of CVD. The SDG target for NCDs is likely to be attained in seven of the ten HICs and two of the MICs studied by 2030, thus revealing both advances and inequities in progress in the two leading causes of premature mortality, responsible for 1 in 2 premature deaths worldwide. This study seeks to inform countries how to invest in effective and cost-effective measures to curb early deaths from NCDs among its citizens, and thus reap the associated public health and economic benefits. It serves to reiterate the need for evidence-based, prioritized, costed and financed programmes to accelerate the achievement of SDG 3.4 in this decade.
Funding
None.
Disclaimer
Where authors are identified as personnel of the International Agency for Research on Cancer / World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer / World Health Organization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix. A
See Fig. A1, Fig. A2 and Table A.
Table A.
Change in cumulative risk of premature mortality (ages 30–69) from diabetes and respiratory diseases between 2000 and 2019 (with 95% confidence intervals).
| Income level/ Country1 |
Diabetes 2000–19: % change (95 %CI)2 |
Respiratory diseases 2000–19: % change (95 %CI)2 |
|---|---|---|
| Middle-Income | ||
| Brazil | −24.4 (-43.2 to 1.1) | −47.0 (-56.9 to −29.1) |
| Bulgaria | −38.6 (-67.7 to 12.3) | 49.7 (-14.7 to 160.0) |
| Colombia | −56.8 (-77.7 to −19.1) | −49.5 (-71.4 to −2.8) |
| Costa Rica | 13.1 (-48.9 to 136.8) | −49.9 (-74.5 to 2.2) |
| Kazakhstan | −17.3 (-52.8 to 41.8) | –32.6 (-63.5 to 23.9) |
| Mauritius | −14.2 (-49.9 to 44.3) | −28.1 (-63.6 to 41.3) |
| Mexico | 12.9 (-26.4 to 68.5) | –33.1 (-56.4 to 2.3) |
| Philippines | 101.6 (4.4 to 261.1) | −15.2 (-46.4 to 38.7) |
| Ukraine | −38.0 (-63.3 to 2.4) | −71.2 (-82.8 to −45.5) |
| Uzbekistan | 7.0 (-37.1 to 75.6) | −69.7 (-84.1 to −28.4) |
| High-Income | ||
| Australia | −20.4 (-47.1 to 18.5) | −30.5 (-55.5 to 9.9) |
| Chile | −21.0 (-56.4 to 39.5) | −17.6 (-56.4 to 53.2) |
| France | −30.5 (-55.4 to 6.0) | −14.1 (-53.3 to 54.0) |
| Italy | −29.3 (-43.7 to −11.4) | −30.9 (-56.2 to 6.8) |
| Japan | −35.3 (-61.2 to 8.6) | −16.6 (-50.9 to 42.0) |
| New Zealand | −34.2 (-59.1 to 4.5) | –32.0 (-54.3 to 5.1) |
| Norway | −17.3 (-36.4 to 7.4) | −19.2 (-51.3 to 28.1) |
| Slovakia | −15.7 (-59.1 to 65.7) | −20.5 (-64.8 to 48.5) |
| U.K. | −36.7 (-48.8 to −21.3) | −18.3 (-42.7 to 11.3) |
| U.S. | −6.3 (-27.7 to 20.2) | −5.4 (-28.8 to 20.3) |
1. Based on the World Bank classification
2. % change in probability of death at ages 30–69 from 2000 to 2019
References
- 1.World Health Organization. Global Health Estimates 2019: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2019. (https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates), World Health Organization, Geneva, 2020.
- 2.United Nations. Sustainable Development Goals Knowledge Platform. Sustainable Development Goal 3. Ensure healthy lives and promote well-being for all at all ages. , 2020. https://sustainabledevelopment.un.org/sdg3. (Accessed 1 April 2021).
- 3.Norheim O.F., Jha P., Admasu K., Godal T., Hum R.J., Kruk M.E. Avoiding 40% of the premature deaths in each country, 2010–30: review of national mortality trends to help quantify the UN sustainable development goal for health. Lancet. 2015;385(9964):239–252. doi: 10.1016/S0140-6736(14)61591-9. [DOI] [PubMed] [Google Scholar]
- 4.Cao B., Bray F., Ilbawi A., Soerjomataram I. Effect on longevity of one-third reduction in premature mortality from non-communicable diseases by 2030: a global analysis of the Sustainable Development Goal health target. Lancet Glob Health. 2018;6(12):e1288–e1296. doi: 10.1016/S2214-109X(18)30411-X. [DOI] [PubMed] [Google Scholar]
- 5.NCD Countdown collaborators. NCD Countdown 2030: pathways to achieving Sustainable Development Goal target 3.4, Lancet 396(10255) (2020) 918-934. [DOI] [PMC free article] [PubMed]
- 6.Wild C.P., Bray F., Forman D., Franceschi S., Sankaranarayanan R., Straif K. Cancer in the 25x25 non-communicable disease targets. Lancet. 2014;384(9953):1502–1503. doi: 10.1016/S0140-6736(14)61918-8. [DOI] [PubMed] [Google Scholar]
- 7.Kontis V., Mathers C.D., Rehm J., Stevens G.A., Shield K.D., Bonita R. Contribution of six risk factors to achieving the 25x25 non-communicable disease mortality reduction target: a modelling study. Lancet. 2014;384(9941):427–437. doi: 10.1016/S0140-6736(14)60616-4. [DOI] [PubMed] [Google Scholar]
- 8.Mendenhall E., Kohrt B.A., Norris S.A., Ndetei D., Prabhakaran D. Non-communicable disease syndemics: poverty, depression, and diabetes among low-income populations. Lancet. 2017;389(10072):951–963. doi: 10.1016/S0140-6736(17)30402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. World Health Organization. World health statistics 2019: monitoring health for the SDGs, sustainable development goals, World Health Organization, Geneva, 2019.
- 10.World Bank. World Bank Country and Lending Groups - Country Classification, 2020. . https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. (Accessed 30 September 2020).
- 11.Bray F, Laversanne M, Weiderpass E, Soerjomataram I. The ever-increasing importance of cancer as a leading cause of premature death worldwide, Cancer, in press. [DOI] [PubMed]
- 12.World Health Organization. ‘Best buys’ and other recommended interventions for the prevention and control of noncommunicable diseases: Updated Appendix 3 of the global action plan for the prevention and control of noncommunicable diseases 2013-2020., 2017. https://www.who.int/ncds/management/WHO_Appendix_BestBuys.pdf. (Accessed 1 September 2021).
- 13.Ezzati M., Riboli E. Can noncommunicable diseases be prevented? Lessons from studies of populations and individuals, Science. 2012;337(6101):1482–1487. doi: 10.1126/science.1227001. [DOI] [PubMed] [Google Scholar]
- 14.Koene R.J., Prizment A.E., Blaes A., Konety S.H. Shared Risk Factors in Cardiovascular Disease and Cancer. Circulation. 2016;133(11):1104–1114. doi: 10.1161/CIRCULATIONAHA.115.020406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mensah G.A., Wei G.S., Sorlie P.D., Fine L.J., Rosenberg Y., Kaufmann P.G. Decline in Cardiovascular Mortality: Possible Causes and Implications. Circ Res. 2017;120(2):366–380. doi: 10.1161/CIRCRESAHA.116.309115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones D.S., Greene J.A. The decline and rise of coronary heart disease: understanding public health catastrophism. Am J Public Health. 2013;103(7):1207–1218. doi: 10.2105/AJPH.2013.301226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roth G.A., Johnson C., Abajobir A., Abd-Allah F., Abera S.F., Abyu G. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ezzati M., Obermeyer Z., Tzoulaki I., Mayosi B.M., Elliott P., Leon D.A. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol. 2015;12(9):508–530. doi: 10.1038/nrcardio.2015.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Capewell S., Beaglehole R., Seddon M., McMurray J. Explanation for the decline in coronary heart disease mortality rates in Auckland, New Zealand, between 1982 and 1993. Circulation. 2000;102(13):1511–1516. doi: 10.1161/01.cir.102.13.1511. [DOI] [PubMed] [Google Scholar]
- 20.Ford E.S., Ajani U.A., Croft J.B., Critchley J.A., Labarthe D.R., Kottke T.E. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. The New England journal of medicine. 2007;356(23):2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 21.Laatikainen T., Critchley J., Vartiainen E., Salomaa V., Ketonen M., Capewell S. Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am J Epidemiol. 2005;162(8):764–773. doi: 10.1093/aje/kwi274. [DOI] [PubMed] [Google Scholar]
- 22.Gouda H.N., Critchley J., Powles J., Capewell S. Why choice of metric matters in public health analyses: a case study of the attribution of credit for the decline in coronary heart disease mortality in the US and other populations. BMC public health. 2012;12:88. doi: 10.1186/1471-2458-12-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Y., Freedman N.D., Albert P.S., Huxley R.R., Shiels M.S., Withrow D.R. Association of Cardiovascular Disease With Premature Mortality in the United States. JAMA Cardiol. 2019;4(12):1230. doi: 10.1001/jamacardio.2019.3891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ritchey M.D., Wall H.K., George M.G., Wright J.S. US trends in premature heart disease mortality over the past 50 years: Where do we go from here? Trends Cardiovasc Med. 2020;30(6):364–374. doi: 10.1016/j.tcm.2019.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mehta N.K., Abrams L.R., Myrskylä M. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proc Natl Acad Sci U S A. 2020;117(13):6998–7000. doi: 10.1073/pnas.1920391117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lopez A.D., Adair T. Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics, Int J Epidemiol. 2019;48(6):1815–1823. doi: 10.1093/ije/dyz143. [DOI] [PubMed] [Google Scholar]
- 27.Wingo P.A., Cardinez C.J., Landis S.H., Greenlee R.T., Ries L.A.G., Anderson R.N. Long-term trends in cancer mortality in the United States, 1930–1998. Cancer. 2003;97(S12):3133–3275. doi: 10.1002/cncr.11380. [DOI] [PubMed] [Google Scholar]
- 28.Jemal A., Ward E., Thun M., Miranda J.J. Declining death rates reflect progress against cancer. PLoS ONE. 2010;5(3):e9584. doi: 10.1371/journal.pone.0009584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doll R., Boreham J. Recent trends in cancer mortality in the UK. Br J Cancer. 2005;92(7):1329–1335. doi: 10.1038/sj.bjc.6602450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levi F, Lucchini F, Negri E, Boyle P, La Vecchia C. Cancer mortality in Europe, 1990-1994, and an overview of trends from 1955 to 1994, European journal of cancer (Oxford, England : 1990) 1999; 35(10): 1477-516. [DOI] [PubMed]
- 31.Bailar J.C., 3rd, Gornik H.L. Cancer undefeated. The New England journal of medicine. 1997;336(22):1569–1574. doi: 10.1056/NEJM199705293362206. [DOI] [PubMed] [Google Scholar]
- 32.Howson C.P., Hiyama T., Wynder E.L. The decline in gastric cancer: epidemiology of an unplanned triumph. Epidemiol Rev. 1986;8:1–27. doi: 10.1093/oxfordjournals.epirev.a036288. [DOI] [PubMed] [Google Scholar]
- 33.Zanetti A.R., Van Damme P., Shouval D. The global impact of vaccination against hepatitis B: a historical overview. Vaccine. 2008;26(49):6266–6273. doi: 10.1016/j.vaccine.2008.09.056. [DOI] [PubMed] [Google Scholar]
- 34.Thun M. In: The Cancer Atlas. Jemal A., Torre L., Soerjomataram I., Bray F., editors. American Cancer Society; Atlanta, Georgia: 2019. Risks of tobacco. [Google Scholar]
- 35.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Volume 83: Tobacco Smoke and Involuntary Smoking. Available at: https://monographs.iarc.fr/wp-content/uploads/2018/06/mono83.pdf, 2004. [PMC free article] [PubMed]
- 36.World Health Organization . WHO; Geneva: 2015. WHO global report on trends in prevalence of tobacco smoking. [Google Scholar]
- 37.Araghi M., Soerjomataram I., Jenkins M., Brierley J., Morris E., Bray F. Global trends in colorectal cancer mortality: projections to the year 2035. Int J Cancer. 2019;144(12):2992–3000. doi: 10.1002/ijc.32055. [DOI] [PubMed] [Google Scholar]
- 38.Arnold M., Rutherford M.J., Bardot A., Ferlay J., Andersson T.M., Myklebust T.A. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995–2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol. 2019;20(11):1493–1505. doi: 10.1016/S1470-2045(19)30456-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.International Agency for Research on Cancer. Colorectal cancer screening. IARC Handb Cancer Prev. 17:1–300. Available from: http://publications.iarc.fr/573., 2019. [PubMed]
- 40.Arnold M., Abnet C.C., Neale R.E., Vignat J., Giovannucci E.L., McGlynn K.A. Global Burden of 5 Major Types Of Gastrointestinal Cancer. Gastroenterology. 2020;159(1):335–349.e15. doi: 10.1053/j.gastro.2020.02.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Araghi M., Soerjomataram I., Bardot A., Ferlay J., Cabasag C.J., Morrison D.S. Changes in colorectal cancer incidence in seven high-income countries: a population-based study. Lancet Gastroenterol Hepatol. 2019;4(7):511–518. doi: 10.1016/S2468-1253(19)30147-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DeSantis C.E., Bray F., Ferlay J., Lortet-Tieulent J., Anderson B.O., Jemal A. International Variation in Female Breast Cancer Incidence and Mortality Rates. Cancer Epidemiol Biomarkers Prev. 2015;24(10):1495–1506. doi: 10.1158/1055-9965.EPI-15-0535. [DOI] [PubMed] [Google Scholar]
- 43.Sebuodegard S, Botteri E, Hofvind S. Breast cancer mortality after implementation of organized population-based breast cancer screening in Norway, J Natl Cancer Inst 2019. [DOI] [PubMed]
- 44.Ravdin P.M., Cronin K.A., Howlader N., Berg C.D., Chlebowski R.T., Feuer E.J. The decrease in breast-cancer incidence in 2003 in the United States. The New England journal of medicine. 2007;356(16):1670–1674. doi: 10.1056/NEJMsr070105. [DOI] [PubMed] [Google Scholar]
- 45.Parkin D.M. Is the recent fall in incidence of post-menopausal breast cancer in UK related to changes in use of hormone replacement therapy? European journal of cancer (Oxford, England : 1990) 2009;45(9):1649–1653. doi: 10.1016/j.ejca.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 46.Canfell K., Banks E., Moa A.M., Beral V. Decrease in breast cancer incidence following a rapid fall in use of hormone replacement therapy in Australia. The Medical journal of Australia. 2008;188(11):641–644. doi: 10.5694/j.1326-5377.2008.tb01821.x. [DOI] [PubMed] [Google Scholar]
- 47.Harding J.L., Shaw J.E., Peeters A., Cartensen B., Magliano D.J. Cancer risk among people with type 1 and type 2 diabetes: disentangling true associations, detection bias, and reverse causation. Diabetes Care. 2015;38(2):264–270. doi: 10.2337/dc14-1996. [DOI] [PubMed] [Google Scholar]
- 48.Ferlay J., Partensky C., Bray F. More deaths from pancreatic cancer than breast cancer in the EU by 2017. Acta oncologica (Stockholm, Sweden) 2016;55(9-10):1158–1160. doi: 10.1080/0284186X.2016.1197419. [DOI] [PubMed] [Google Scholar]
- 49.Lotufo P.A. Trends in cardiovascular diseases and heart disease death rates among adults aged 45–64: Brazil, 2000–2017. Sao Paulo Med J. 2019;137(3):213–215. doi: 10.1590/1516-3180.2019.1373.220719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nowbar A.N., Gitto M., Howard J.P., Francis D.P., Al-Lamee R. Mortality From Ischemic Heart Disease. Circ Cardiovasc Qual Outcomes. 2019;12(6) doi: 10.1161/CIRCOUTCOMES.118.005375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yusuf S., Joseph P., Rangarajan S., Islam S., Mente A., Hystad P. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395(10226):795–808. doi: 10.1016/S0140-6736(19)32008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kotseva K., Wood D., De Bacquer D., De Backer G., Ryden L., Jennings C. A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries, Eur. J Prev Cardiol. 2016;23(6):636–648. doi: 10.1177/2047487315569401. [DOI] [PubMed] [Google Scholar]
- 53.WHO Regional Office for Europe. Prevention and control of noncommunicable diseases in Kazakhstan. The case for investment., 2019. https://www.euro.who.int/en/countries/kazakhstan/publications/prevention-and-control-of-noncommunicable-diseases-in-kazakhstan.-the-case-for-investment-2019. (Accessed 30 August 2021).
- 54.Saxena A., Koon A.D., Lagrada-Rombaua L., Angeles-Agdeppa I., Johns B., Capanzana M. Modelling the impact of a tax on sweetened beverages in the Philippines: an extended cost-effectiveness analysis. Bull World Health Organ. 2019;97(2):97–107. doi: 10.2471/BLT.18.219980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sassi F., Belloni A., Mirelman A.J., Suhrcke M., Thomas A., Salti N. Equity impacts of price policies to promote healthy behaviours. Lancet. 2018;391(10134):2059–2070. doi: 10.1016/S0140-6736(18)30531-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Republic of the Philippines Department of Health. Investment In Non-Communicable Diseases Prevention And Control Will Save Lives And Contribute To The Philippines Saving Up To 4.8% Of Annual GDP. , 2019. https://doh.gov.ph/press-release/investment-in-non-communicable-diseases-prevention-and-control-will-save-lives-and-contribute-to-the-Philippines-saving-up-to-4.8%25-of-annual-GDP. (Accessed 1 September 2021).
- 57.Huffman M.D., Salam A., Patel A. Implementation Strategies for Cardiovascular Polypills. JAMA. 2019;322(23):2279–2280. doi: 10.1001/jama.2019.18102. [DOI] [PubMed] [Google Scholar]
- 58.Roshandel G., Khoshnia M., Poustchi H., Hemming K., Kamangar F., Gharavi A. Effectiveness of polypill for primary and secondary prevention of cardiovascular diseases (PolyIran): a pragmatic, cluster-randomised trial. Lancet. 2019;394(10199):672–683. doi: 10.1016/S0140-6736(19)31791-X. [DOI] [PubMed] [Google Scholar]
- 59.Yusuf S., Joseph P., Dans A., Gao P., Teo K., Xavier D. Polypill with or without Aspirin in Persons without Cardiovascular Disease. The New England journal of medicine. 2021;384(3):216–228. doi: 10.1056/NEJMoa2028220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bertram M.Y., Sweeny K., Lauer J.A., Chisholm D., Sheehan P., Rasmussen B. Investing in non-communicable diseases: an estimation of the return on investment for prevention and treatment services. Lancet. 2018;391(10134):2071–2078. doi: 10.1016/S0140-6736(18)30665-2. [DOI] [PubMed] [Google Scholar]
- 61.Knaul F.M., Arreola-Ornelas H., Rodriguez N.M., Mendez-Carniado O., Kwete X.J., Puentes-Rosas E. Avoidable Mortality: The Core of the Global Cancer Divide. J Glob Oncol. 2018;4:1–12. doi: 10.1200/JGO.17.00190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Romero Y., Trapani D., Johnson S., Tittenbrun Z., Given L., Hohman K. National cancer control plans: a global analysis. Lancet Oncol. 2018;19(10):e546–e555. doi: 10.1016/S1470-2045(18)30681-8. [DOI] [PubMed] [Google Scholar]
- 63.Gelband H., Sankaranarayanan R., Gauvreau C.L., Horton S., Anderson B.O., Bray F. Disease Control Priorities-3 Cancer Author, Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: key messages from Disease Control Priorities. Lancet. 2016;387(10033):2133–2144. doi: 10.1016/S0140-6736(15)00755-2. [DOI] [PubMed] [Google Scholar]
- 64.Oar A., Moraes F.Y., Romero Y., Ilbawi A., Yap M.L. Core elements of national cancer control plans: a tool to support plan development and review. Lancet Oncol. 2019;20(11):e645–e652. doi: 10.1016/S1470-2045(19)30404-8. [DOI] [PubMed] [Google Scholar]
- 65.World Health Organization . WHO; Geneva: 2015. WHO report on cancer: setting priorities, investing wisely and providing care for all. [Google Scholar]
- 66.World Health Organization. Cervical Cancer Elimination Initiative, 2021. https://www.who.int/initiatives/cervical-cancer-elimination-initiative. (Accessed 2 September 2021).
- 67.World Health Organization. New global breast cancer initiative highlights renewed commitment to improve survival, 2021. https://www.who.int/news/item/08-03-2021-new-global-breast-cancer-initiative-highlights-renewed-commitment-to-improve-survival. (Accessed 2 September 2021).
- 68.World Health Organization. Global initiative for childhood cancer, 2021. https://www.who.int/publications/m/item/global-initiative-for-childhood-cancer. (Accessed 2 September 2021).
- 69.NCD Countdown collaborators. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4, Lancet 392(10152) (2018) 1072-1088. [DOI] [PubMed]
- 70.World Health Organization . World Health Organization; Geneva: 2019. World health statistics 2019: monitoring health for the SDGs, sustainable development goals. [Google Scholar]
- 71.World Health Organization . World Health Organization; Geneva: 2018. World health statistics 2018: monitoring health for the SDGs, sustainable development goals. [Google Scholar]
- 72.Bygbjerg I.C. Double burden of noncommunicable and infectious diseases in developing countries. Science. 2012;337(6101):1499–1501. doi: 10.1126/science.1223466. [DOI] [PubMed] [Google Scholar]
- 73.Niessen L.W., Mohan D., Akuoku J.K., Mirelman A.J., Ahmed S., Koehlmoos T.P. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet. 2018;391(10134):2036–2046. doi: 10.1016/S0140-6736(18)30482-3. [DOI] [PubMed] [Google Scholar]
- 74.International Agency for Research on Cancer. World Cancer Report: Cancer Research for Cancer Prevention. Available from: http://publications.iarc.fr/586, International Agency for Research on Cancer, Lyon, France, 2020.
- 75.Phillips D.E., AbouZahr C., Lopez A.D., Mikkelsen L., de Savigny D., Lozano R. Are well functioning civil registration and vital statistics systems associated with better health outcomes? Lancet. 2015;386(10001):1386–1394. doi: 10.1016/S0140-6736(15)60172-6. [DOI] [PubMed] [Google Scholar]
- 76.GBD Sdg Collaborators Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):2091–2138. doi: 10.1016/S0140-6736(18)32281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nugent R., Bertram M.Y., Jan S., Niessen L.W., Sassi F., Jamison D.T. Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. Lancet. 2018;391(10134):2029–2035. doi: 10.1016/S0140-6736(18)30667-6. [DOI] [PubMed] [Google Scholar]
- 78.World Health Organization. Responding to noncommunicable diseases during and beyond the COVID-19 pandemic: a rapid review, 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-Non-communicable_diseases-Evidence-2020.1. (Accessed 16 August 2021).
- 79.World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020., 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1. (Accessed 28 February 2021).