Abstract
Background
The COVID-19 global pandemic has had profound effects on mental health and wellbeing. The present study examined trends in distress and recovery in the aftermath of COVID-19 in China. Predictors that might increase risks or provide protections again distress were explored.
Method
Participants were recruited using social media during the COVID-19 pandemic to complete a baseline and 6-week follow-up survey (N = 241). The change patterns of PTSD symptoms from baseline to follow-up were characterized using latent class growth analysis (LCGA). A repeated-measures ANOVA was conducted to explore the differences in the depressive symptoms across trajectory groups. Multinominal logistic regression was performed to investigate potential predictors of the outcome trajectories.
Results
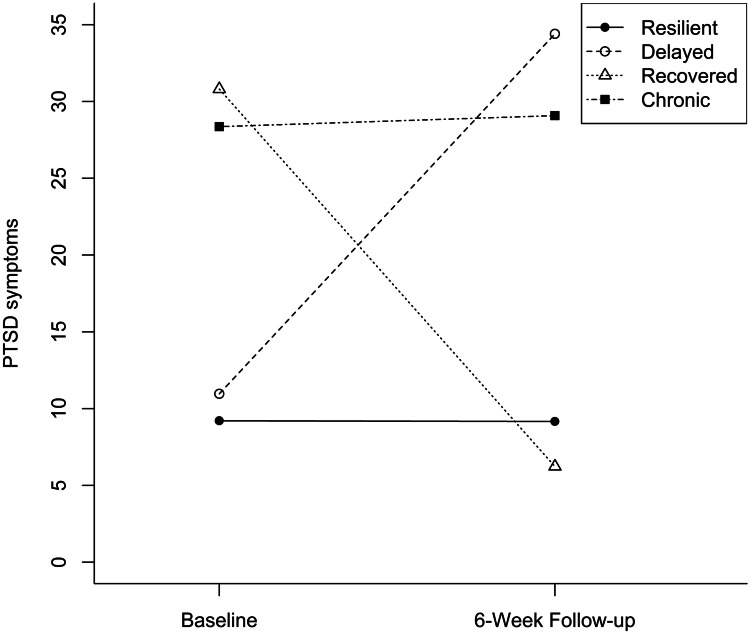
Four longitudinal outcome trajectories were identified: chronic (PTSD symptoms remained high; 14.9%), resilient (symptoms remained low; 43.2%), recovered (symptoms decreased from symptomatic levels to asymptomatic; 19.5%), and delayed (symptoms increased from asymptomatic levels to symptomatic; 22.4%). Hopelessness and maladaptive coping strategies were unique predictors of distress and resilience as well as longer-term trajectories.
Conclusion
Individuals evidenced four outcome trajectories of distress in the aftermath of COVID-19 in China. Despite the uncertainty and high levels of stress related to the pandemic, the majority of the sample demonstrated resilience and recovery. It is essential to identify individuals at risk for chronic and delayed distress in order to build resilience.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12529-021-10036-8.
Keywords: COVID-19, Trauma, Resilience, Distress, Hopelessness
Introduction
The global COVID-19 (SARS-CoV-2) pandemic has profoundly changed lives. As of August 2021, the World Health Organization reported more than 199 million confirmed cases across the globe [1]. After peaking in February 2020, China had drastic decreases in daily COVID-19 cases [1]. Individuals in the context of a global disaster may continue to be affected by ongoing post-disaster stressors, like the economic effects or concerns about worsening situations in other countries, which may add to COVID-19-related distress [2]. Conversely, surviving the pandemic may improve individuals’ resistance to later stressors and promote their resilience [3]. Researchers and clinicians have been calling for attention to not just physical health but also mental health during the pandemic as research on the high levels of distress is emerging [4–9]. Further, as China and other countries around the world are now seeing another rise in cases due to COVID-19 variants [1], chronic and acute stressors continue to be of concern as people may still be recovering from the initial quarantines while still facing even more restrictions in order to halt the spread of the Delta variant and high levels of uncertainty about the future. Given the protracted nature of the pandemic, longitudinal studies are necessary to understand trends in distress and recovery as well as long-term psychological adjustment [10].
Psychological Distress and Resilience
Research has demonstrated great heterogeneity in individuals’ responses to potentially traumatic events (PTEs) [11–15]. Although most people are exposed to at least one PTE or chronically aversive circumstance throughout their lifespans, the majority of people show resilience or may quickly recover from the initial traumatic distress [11]. Resilience reflects an individuals’ ability to keep distress low and to show psychological adjustment in the face of the adversity. In contrast to the resilience and recovery, some individuals develop chronic psychological problems such as posttraumatic stress disorder (PTSD) [16]. Epidemiologic research estimates that the lifetime PTSD prevalence is 8.3% [17]. However, previous taxonometric investigations suggest that PTSD may be better understood as psychological distress varying in severity and duration instead of a discrete clinical category suggesting that symptoms, not diagnoses, are important to study and further suggesting that the rates of distressing symptoms may be much higher than the rates of diagnoses [12, 13].
Four theoretical trajectories have been proposed to capture prototypical patterns of distress following a PTE: resilient, recovered, delayed, and chronic [11]. Resilient individuals are fairly stable with healthy levels of psychological and physical functioning in the face of a PTE; this is the most common outcome trajectory. Recovered individuals experience elevated psychological symptoms initially but gradually return to pre-trauma levels. In contrast, the delayed trajectory is characterized by initially moderate levels of psychological distress that increase across time. The chronic trajectory is indicated by consistently high levels of distress across time. The four trajectories were demonstrated and replicated in numerous studies on various types of PTEs (e.g., war, disease, injury, natural disaster, and sexual assault) and during previous pandemics, including Severe Acute Respiratory Syndrome (SARS) in 2003 and the H1N1 pandemic in 2009 [18–27].
Research during the COVID-19 pandemic supports this four-trajectory model [11]. Data from a nationally representative sample in Spain were categorized into four trajectories: resilient, delayed distress, recovered, and sustained distress based on absence/presence of distress at two assessment points (April and May 2020) [28]. Over half of the sample evinced resilience whereas around one-fourth experienced sustained distress [28]. In another longitudinal study of 21,938 adults in England (from March to July 2020) [29], four trajectories of depression and five of anxiety were identified using growth mixture modeling. Over 70% of the sample showed low levels of symptoms and around 10% showed severe or moderate levels of symptoms throughout the lockdown. Other studies have categorized individuals into high, normal, and low levels of resilience [30]. Low resilience individuals experienced increases in distress whereas high resilience individuals maintained a low level of distress [30]. These findings suggest that psychological responses to COVID-19 are heterogeneous and highlight the need to identify individuals who are at higher risk of high and chronic distress in order to target those at highest risk for prevention and intervention efforts [28, 30, 31].
Predictors of Psychological Resilience and Distress
Resilience and recovery are associated with various protective and risk factors. Trajectories of psychological distress after a PTE vary by factors such as pre-existing mental health conditions and demographics [25, 32, 33]. By characterizing different trajectories of psychological distress across different phases of the pandemic and examining predictors of membership in each trajectory, researchers can identify protective and risk factors that discretely predict resilience and recovery and help identify at-risk populations in order to improve resilience. Two key predictors of distress and resilience during PTEs are hopelessness and coping.
Hopelessness
Hopelessness has been found to predict PTSD symptoms in the aftermath of PTEs [34]; higher levels of hope are associated with greater reductions in PTSD and depressive symptoms [35]. The COVID-19 pandemic and resultant lockdowns may induce hopelessness about finances, careers, and future plans — as well as when and whether the pandemic will end. Research during the current pandemic has found that hopelessness is one of the strongest predictors of distress, internalizing symptoms, and anger and is negatively associated with resilience [36, 37]. Hope may be particularly important because it reflects an individual’s expectations about the longer-term effects of the pandemic, thereby affecting current-day behavioral and psychological responses. However, hope is not a static emotion and given the longstanding nature of the pandemic, it may wax and wane over time—as may distress levels.
Coping
Coping styles may be implicated in different trajectories of distress and there are clear associations between maladaptive coping and poor mental health outcomes. For example, avoidant coping is positively associated with psychological distress after trauma and negatively associated with resilience [11, 38]. Further, high reliance on avoidant coping strategies predicts more severe PTSD symptoms which, in turn, predicts greater use of avoidant coping [39]. However, the relationship between adaptive coping and psychological distress is less clear. In a 2007 meta-analysis [38], there was no association found between approach coping and distress. However, recent findings suggest that adaptive coping may be associated with resilience [40]. Given the high level of psychological distress caused by COVID-19, it is important to examine how different coping strategies may predict discrete trajectories of psychological distress. Adding to factors known to contribute to psychological distress and resilience, unique characteristics of pandemics such as fears of contagion and effects of quarantining may also affect individuals [14, 25, 41]. Additionally, health behaviors like substance use and pandemic-related worries may heighten stress and result in long-term negative mental health effects [25, 42].
This study aimed to investigate psychological distress and resilience in China during the COVID-19 pandemic using prospectively collected data collected at two timepoints. The first wave of data collection occurred in May 2020, with a 6-week follow-up. The first aim was to examine the trajectories of PTSD symptoms. We hypothesized that the trajectories during COVID-19 would be consistent with the four theoretical trajectories (resilient, recovered, delayed, and chronic) found in other research [11]. Next, this study aimed to explore potential predictors of the trajectories. Factors potentially associated with psychological distress and resilience, including hopelessness, coping, and individuals’ reactions to the pandemic, were tested.
Methods
Participants and Procedure
Participants were recruited using flyers distributed on social media sites (e.g., Zhihu) and through personal networks. The first wave of the survey was administered between May 3, 2020, and May 28, 2020. Six weeks later, participants who provided their email address for future follow-ups were sent an email to take part in the follow-up survey between June 18, 2020, and July 7, 2020. Full approval to this study has been given by Institutional Review Board. A total of 352 participants completed the first survey and provided their email address for future follow-ups. Of these, 241 participants responded to the follow-up survey, resulting in a sample of 241 participants. The mean age of participants was 20.15 (SD = 2.17; Median = 20; Range = 17–38). The sample primarily comprised men (70.1%), single (73.9%), and heterosexual individuals (78.8%; Table 1). Most participants resided in a small (40.7%) city, in Northwest China (24.5%), in a province with 500–599 confirmed cases (36.1%). No significant differences were found between the current sample and those who only completed the first survey in terms of PTSD symptoms, coping strategies, hopelessness, COVID-19 responses, and demographic variables.
Table 1.
Sample characteristics
| Demographic variables | n | Percent |
|---|---|---|
| Age (M, SD) | 20.15 (2.17) | |
| Gender | ||
| Women | 71 | 29.5% |
| Men | 169 | 70.1% |
| Sexual identity | ||
| Sexual minority | 49 | 20.3% |
| Only heterosexual | 190 | 78.8% |
| Relationship status | ||
| Single | 178 | 73.9% |
| In a committed relationship | 59 | 24.5% |
| Married | 2 | 0.8% |
| Place of residence | ||
| In a large city or a suburb near a large city | 57 | 23.7% |
| In a medium size city (50,000 to 250,000) | 50 | 20.7% |
| In a small city or town (under 50, 000) | 98 | 40.7% |
| In open country | 34 | 14.1% |
| Location | ||
| North China | 53 | 22.0% |
| Northeast China | 21 | 8.7% |
| East China | 28 | 11.6% |
| Central China | 19 | 7.9% |
| South China | 11 | 4.6% |
| Southwest of China | 49 | 20.3% |
| Northwest China | 59 | 24.5% |
| Local cases of COVID infection | ||
| 1000 or more | 27 | 11.2% |
| 500–999 | 87 | 36.1% |
| 100–499 | 82 | 34.0% |
| Less than 100 | 44 | 18.3% |
Some participants chose to not disclose their demographic information. Therefore, the number (percentage) of individuals in each category may add up to less than 241 (100%)
Measures
Participants were asked to report demographic information including gender, sexual identity, education, and relationship status as well as previous mental health diagnosis. The survey assessed participants’ responses to the COVID-19 pandemic (e.g., worries and protective behaviors), depressive and PTSD symptoms, hopelessness, and coping strategies at baseline. Depressive and PTSD symptoms, hopelessness, and coping strategies were measured again at follow-up. The survey instrument was adapted for a Chinese population from an international survey on COVID-19 and mental health [10].
COVID-19 Responses
COVID Worries
Participants were asked whether they had been exposed to the coronavirus on a 5-point scale (1 = Definitely Not, 5 = Definitely Yes) and to rate how worried they felt about 8 pandemic-related factors on a scale of 0 (not worried at all) to 100 (extremely worried), for example, how worried are you about: (1) being exposed to COVID-19; (2) becoming infected in the next 3 months; and (3) running out of money (see full list in Supplemental Table 1). The 8-item scale demonstrated excellent internal consistency (α = 0.909).
COVID Protective Actions
Participants were asked to indicate whether they had used each of the 10 recommended protective actions to help prevent the spread of coronavirus in the past 2 weeks (e.g., wearing masks; Supplemental Table 1). An index score was created to reflect the total number of protective actions taken by participants (range = 0–10).
COVID Severity
Severity of the COVID-19 pandemic in each participant’s province was indicated by the cumulative number of COVID-19 positive cases [1].
Health Behaviors
Participants were asked whether they had ever consumed alcohol. If yes, they were asked if they had consumed any alcohol over the past 7 days. Participants were also asked how healthy they felt their eating was on a 5-point scale (1 = Poor, 5 = Excellent).
Mental Health
PTSD Symptoms
The Impact of Event Scale (IES) is a 15-item questionnaire measuring subjective distress related to a specific event [43]. Seven of the 15 items measure intrusive symptoms, and 8 items measure avoidance symptoms. The scale was adapted to measure acute peritraumatic stress (i.e., the tense of all items was changed from the past to present to examine PTSD symptoms at the time of the PTE). Participants were specifically asked to rate their levels of stress related to COVID-19 (e.g., I have dreams about [COVID-19]) in the past 7 days on a 4-point scale (ranging from 0 = not at all to 3 = often). The IES has been used to screen for PTSD in clinical and research settings [44–46]. Previous literature has reported strong criterion validity and convergent validity of IES. The internal consistency of the overall IES scores based on the modified version among the current sample at the first assessment was excellent (α = 0.942).
Depressive Symptoms
The Center for Epidemiologic Studies Depression (CES-D) scale is a self-report scale with strong internal consistency and high specificity [47]. This study used an 11-item version of the CES-D with comparable psychometric properties to the original version to reduce participant burden [48]. Participants were asked to indicate how often they have experienced each of the 11 items (e.g., felt depressed) during the past week from 0 (rarely or none of the time) to 3 (most of the time). The internal consistency based on the current sample at the first wave of assessment was 0.850.
Hopelessness
The Beck Hopelessness Scale (BHS) is a 20-item self-report scale measuring negative attitudes about the future. Individuals were asked to indicate whether each item was true or false for them (e.g., My future seems dark to me) [49]. Each item response was assigned a score of 0 or 1. Total scores ranged from 0 to 20 with higher scores reflecting higher levels of hopelessness. The scale had fair reliability in this study (0.719).
Coping
The Brief-COPE is a 28-item self-report questionnaire assessing coping strategies. Participants were asked to rate each item on a 4-point Likert scale (0 = I haven’t been doing this at all; 3 = I’ve been doing this a lot) [50]. Items are categorized into adaptive coping and maladaptive coping [51]. Adaptive coping consists of 8 subscales (active coping, planning, positive reframing, acceptance, humor, religion, emotional support, and instrumental support). Maladaptive coping consists of 6 subscales (denial, venting, substance use, behavioral disengagement, self-distraction, and self-blame). The internal consistency for adaptive coping and maladaptive coping for this sample were 0.890 and 0.837, respectively.
Data Analysis
A heatmap of missing values was drawn to visualize the patterns of missing values in order to examine the randomization of the missing values. Missing values were replaced with the median value of the item. Sensitivity analyses were conducted to compare the participants who completed both waves of survey (N = 241) to those who only completed the first survey (n = 111). Specifically, t-tests and chi-square tests were performed to compare the two groups in terms of mental health outcomes, COVID-19 responses, and demographical variables.
An unconditional latent class growth analysis (LCGA) was performed to examine the trajectories of PTSD symptoms using Mplus 8.3 [52]. The LCGA began with a single-class model and then added one class each time until none of the likelihood tests was significant. The conceptual rationale and statistical model fit of all models were compared to select the best fitting model. The model fit indices include Akaike’s Information Criterion (AIC) and Bayesian Information Criterion (BIC), sample-size adjusted Bayesian information criterion (ssBIC), and VLMR LRT = Vuong–Lo–Mendell–Rubin likelihood ratio test (VLMR LRT) [53].
After the best model was selected, a repeated-measures ANOVA, with a within-subject factor Time (baseline, follow-up) and a between-subject factor Trajectory, was performed to explore the differences in the depressive symptoms across trajectory groups. Additionally, to explore factors potentially associated with trajectories, one-way ANOVAs with Bonferroni post hoc pairwise comparisons and Chi-square tests were conducted to compare the trajectories on demographics, COVID-19-related worries and actions, and other mental and behavioral health variables measured at the first wave of assessment. The Benjamini–Hochberg Procedure with a false discovery rate (FDR) of 15% was performed to control the FDR. Finally, predictors that significantly differed across trajectories groups were entered into a multinomial logistic regression simultaneously to examine their associations with trajectories. These analyses were performed by using SPSS version 26.0 [54].
Results
Trajectory Memberships
The model fit for one- to five-class models improved significantly from one to four classes (Supplemental Table 2). Although the five-class model showed slightly better model fit indices than the four-class model, the improvement was minimal and insignificant. Going from the four-class model, the five-class model separated one class into two classes that shared similar patterns; thus, it was at higher risk of overextraction of classes and model instability. The four-class model was more parsimonious and aligned with the four theoretical trajectories of traumatic distress. Thus, we chose the four-class solution for further analyses.
Figure 1 depicts the four trajectories of individuals’ symptom changes during the pandemic. The majority of the sample fit into the resilient trajectory (n = 104, 43.2%), characterized by absence of PTSD symptoms at both timepoints. The delayed group, accounting for 22.4% (n = 54) of the sample, showed low levels of PTSD symptoms at baseline and high levels of PTSD symptoms at follow-up. In contrast, the recovered group (n = 47, 19.5%) initially reported high levels of PTSD symptoms at baseline and low levels of PTSD symptoms at follow-up, suggesting recovery. Finally, a minority of individuals (n = 36, 14.9%) reported high levels of PTSD symptoms at both baseline and follow-up.
Fig. 1.
Outcome trajectories in the aftermath of the COVID-19
Although the main effect of time was not significant, F(1, 237) = 1.44, p = 0.232, η2 = 0.006, suggesting no changes in depressive symptoms from baseline to follow-up for the whole sample, the repeated-measures of ANOVA demonstrated a significant main effect of trajectory group, F(3, 237) = 30.84, p < 0.001, η2 = 0.281 and a significant interaction between trajectory and time, F(3, 237) = 3.75, p = 0.012, η2 = 0.045. Bonferroni post hoc tests suggest that the recovered and resilient groups reported significantly higher levels of depressive symptoms than the chronic and delayed groups (all p values < 0.001). Further, the recovered and resilient groups reported lower levels of depressive symptoms at follow-up than at baseline whereas the delayed and chronic groups evidenced the opposite change pattern.
Baseline Predictors of Trajectory Membership
The differences among the four theoretical trajectories in demographic variables, responses to COVID-19, and mental and behavioral health outcomes measured at the first wave of assessment are summarized in Supplemental Table 3. There were significant differences in hopelessness, coping strategies, and past 7-day alcohol use. To examine whether these variables uniquely predicted discrete theoretical trajectories after controlling for other variables, all potential predictors were examined simultaneously in multinomial logistic regressions. Table 2 shows the odds ratios (ORs) for each variable in predicting resilient, recovered, and delayed versus chronic, recovered and delayed versus resilient, and delayed versus recovered group (comparisons were chosen to be conceptually meaningful). Individuals’ hopelessness and maladaptive coping were found to be unique and consistent predictors of the four trajectories.
Table 2.
Multinomial logistic regression predicting trajectories using baseline variables
| Chronic (ref.) vs | Resilient (ref.) vs | Recovered (ref.) vs | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resilient | Recovered | Delayed | Recovered | Delayed | Delayed | |||||||
| Outcome measure | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| COVID worries | 0.98 | 0.96–1.00 | 1.00 | 0.96–1.02 | 1.00 | 0.98–1.02 | 1.02 | 0.99–1.04 | 1.02 | 1.00–1.04 | 1.00 | 0.98–1.03 |
| Hopelessness | 0.78 | 0.64–0.95 | 0.74 | 0.58–0.93 | 1.00 | 0.83–1.20 | 0.94 | 0.78–1.19 | 1.28 | 1.09–1.51 | 1.36 | 1.08–1.71 |
| Maladaptive coping | 0.03 | 0.01–0.15 | 1.91 | 0.50–7.27 | 0.06 | 0.12–0.28 | 60.29 | 13.54–268.38 | 1.80 | 0.42–7.64 | 0.03 | 0.01–0.15 |
| Adaptive coping | 1.50 | 0.34–6.54 | 1.76 | 0.34–6.54 | 2.63 | 0.56–12.45 | 1.17 | 0.27–5.00 | 1.75 | 0.54–5.69 | 1.50 | 0.31–7.37 |
| Alcohol use | ||||||||||||
| Yes | 0.52 | 0.16–1.68 | 0.48 | 0.16–1.68 | 1.29 | 0.42–3.96 | 0.94 | 0.25–3.50 | 2.49 | 0.94–6.64 | 2.66 | 0.73–9.64 |
| No | — | — | — | — | — | — | — | — | — | — | — | — |
Significant (p < .05) odd ratios indicated in boldface
Chronic Versus Other Groups
Compared to the chronic group, individuals who were more hopeless (p = 0.015) and used more maladaptive coping strategies (p < 0.001) were less likely to be in the resilient compared to the chronic trajectory. Also, membership in the recovered trajectory was less likely among individuals with higher levels of hopelessness (p = 0.011). Individuals who used more maladaptive coping strategies were more likely to remain in the chronic than the delayed trajectory (p < 0.001).
Resilient Versus Recovered and Delayed
Compared to the resilient group, individuals who were more hopeless were more likely to develop delayed distress (p = 0.003). The probability of being in the recovered trajectory versus the resilient trajectory was significantly higher among those who used more maladaptive coping strategies (p < 0.001).
Recovered Versus Delayed
Compared to the recovered group, individuals who had higher levels of hopelessness and used fewer maladaptive coping strategies were more likely to belong to the delayed rather than the recovered trajectory.
Discussion
This study provides a preliminary understanding of trajectories of psychological distress and resilience in the aftermath of the COVID-19 pandemic. Four change patterns of traumatic distress were identified: resilient (PTSD symptoms remained low); chronic (symptoms remained high); recovered (symptoms decreased from symptomatic levels to asymptomatic); and delayed (level of severity gradually increased from asymptomatic to symptomatic). These patterns were consistent with the prototypical trajectories following PTEs [11], thus validating previous research that suggests heterogeneity in individuals’ distress and resilience during PTEs like the COVID-19 global pandemic. Furthermore, the chronic and delayed groups demonstrated higher levels of depressive symptoms, which increased over time, whereas the resilient and recovered groups evidenced lower levels of depressive symptoms, which decreased over time. These findings suggest that depression may be associated with, and affected by, traumatic distress, both chronic and delayed.
Our data suggest key predictors of psychological resilience and distress as the crisis of the pandemic wanes. Membership in the resilient and recovered trajectory groups was associated with lower levels of hopelessness. Those in the resilient group also reported using fewer maladaptive coping strategies during the pandemic. Our findings suggest that for individuals who have initially high levels of distress, those with lower levels of hopelessness may be more likely to recover. Hopelessness was also a significant predictor of delayed distress. The identification of these predictors may help us understand how resilience and recovery were achieved and in turn, pertinent precautions can be taken for distressed individuals to reduce their distress.
Chronic and Delayed Distress
Although there were no reported cases of COVID-19 in the sample, nearly 40% of individuals showed chronic and delayed distress and about 20% experienced acute distress initially and then recovered. This suggests that the pandemic has likely caused severe psychological distress that varies in onset and duration. Notably, the current proportion of those in the delayed group (22.4%) was higher than the range (5–10%) typically observed in the aftermath of a PTE (5–10%) [11]. This may be because, in contrast to typical PTEs, pandemics are more prolonged and cause additional stressors (e.g., financial hardships), potentially leading to anticipatory anxiety and hopelessness for life after the pandemic. Further, the COVID-19 pandemic is more widespread and prolonged than other modern pandemics, thus potentially affecting people’s ability to find hope.
Despite the decreasing daily new cases in China at the time of data collection, it remained unclear when the pandemic would end, and the risk of a future outbreak remained high. Indeed, hopelessness was prevalent in this sample and was a consistent predictor of distress, both chronic and delayed. Although hopelessness is a typical response to extreme adversity, it may lead to deteriorated functioning [55] due to worries about long-term negative implications for the future [56], which may then culminate in psychological distress [56]. Hopeless individuals may be less motivated to actively cope with the destructive effects of the pandemic and less likely to show healthy adjustment [57], thereby potentially maintaining distress and even resulting in a delayed onset of distress. Given the current global concerns about the variants (e.g., Delta) and new restrictions being put in place in China and elsewhere, we would anticipate that hopelessness might be even more prevalent today. Our data suggests that this is a sizable risk factor for poor mental health and that prevention and intervention efforts are needed.
Resilience and Recovery
Despite the severity and prolonged nature of the pandemic, the resilient trajectory was the most common outcome with over 40% of the sample showing minimal levels of distress and roughly 20% recovering from the initial distress in the aftermath of COVID-19. As with those in the more distressed trajectories, hope seems to be implicated in resilience and recovery. Both recovered and resilient individuals had lower hopelessness than chronic individuals, indicating that hope may not only be a buffer against acute distress but may also facilitate recovery. Given the protracted nature of the pandemic, it is challenging—and yet imperative—to retain some hope to avoid unremitting distress.
Coping plays an important role in the psychological adjustment after a PTE [38]. Individuals who used fewer maladaptive coping strategies (e.g., denial and repression) were more likely to remain resilient. These maladaptive coping strategies serve as avoidance which may provide short-term relief from stressors but may, in the long-term, drain the amount of energy devoted to coping and hinder effective adjustment [38]. Our data suggest that avoidant coping strategies led to decrements in mental health during the COVID-19 lockdown [58]. Conversely, adaptive coping strategies were not associated with trajectories of distress, which is consistent with a previous meta-analysis [38]. In the face of such a significant and widespread PTE like a global pandemic, it may be hard to consistently use adaptive coping. Coping strategies that were previously effective may not work in current pandemic due to its uncontrollability and high levels of uncertainty [35]. Notably, this study only covered a relatively short timespan; the long-term positive effects of adaptive coping strategies may not have been captured. One reason for this may be that specific strategies may be more or less effective. Recent research showed that socially supportive coping was associated with a faster decrease in anxiety and depressive symptoms whereas problem- and emotion-focused coping strategies [58], which are typically considered to be adaptive strategies, were not. More research is needed to help us understand the effects of different coping strategies and which are important for alleviating distress during the current pandemic as well as future public crises.
Comparing the currents trajectories to those identified in other countries and regions may facilitate our understanding of resilience and distress associated with major public health disasters. It is noteworthy that the current study identified lower rates of the resilient and recovered groups and higher rates of the delayed and chronic groups than other trajectory studies during the pandemic. This may be because the current sample primarily comprised young adults, who have been found to be at higher risk of psychological distress than older people [59]. Additionally, this study specifically examined the trajectories of PTSD symptoms whereas other studies have included negative emotions like depression and anxiety in their trajectories. Although these symptoms often co-occur [16], changes in PTSD symptoms may be more similar to the theoretical trajectories of traumatic distress. Although different methods have been used to examine mental health trajectories during the pandemic, our study and others have consistently demonstrated that individuals develop heterogenous patterns of distress and resilience. This finding highlights the need to take into account longer-term mental health trajectories in prevention and intervention efforts.
Implications
At the time of the study, China had entered a post-peak COVID-19 era and the long-term psychological effects of the pandemic, along with the effects of socially mediated events and containment efforts (e.g., grief and loss, mandatory quarantining, and reduced access to leisure activities) had begun to emerge. Currently, we are experiencing recent surges due to the COVID-19 variants and low vaccination rates globally, which has resulted in containment efforts in some areas, including portions of China. Unfortunately, this means we continue to need long-term follow-up to understand how the variants and low rates of vaccination worldwide — as well as the reinstitution of containment efforts — may be affecting mental health. Our findings that hope plays an important role in protecting against distress amplify the need to understand the impacts of potentially feeling hopeful due to a sense that the pandemic is over, and then the impacts of possible declines in hope/increases in hopelessness during the resurgences and in determining what the “new normal” is for the world.
Our findings have several implications specifically for researchers, public health officials, and healthcare practitioners. First, our data suggest that reactions to a public mental health crisis can be accurately reflected by the four theoretical trajectories of distress following PTEs. This suggests that a one-size-fits-all policy may fail to address the complexities of people’s experiences. Practitioners and policy makers should be aware that there may not be one simple universal solution to protect at-risk populations and that both universal and tailored prevention and intervention efforts are needed. Access to supports such as counseling and community-based support groups should be promoted at the policy and population levels [60]. Published guidelines should also consider discrete intervention strategies tailored to the different subgroups of the population who may be at the highest risk. Secondly, hopelessness and coping appear to play key roles in responses to the pandemic and may provide important intervention targets in order to reduce maladaptive coping and help people find hope in highly stressful and uncertain situations. Providing accurate information about the pandemic may also help reduce fears and worries. More research is needed to determine specifically what brings hope for people during the pandemic. Further, clear and accessible education on the virus, mitigation and prevention efforts, and risk factors are needed to help dispel myths and unfounded worries. Finally, given that young adults have been found to be most affected by the pandemic, our findings may have unique implications for facilitating young adults’ adjustment.
Limitations and Future Directions
Despite multiple strengths—including a prospective design and robust validated measures—this study has several limitations. First, there were few demographic differences as the majority of participants were college students and thus largely homogenous. Despite this, we found that heterogeneity in responses to the pandemic in a relatively homogenous group is important. Future research should recruit participants with more diverse demographic and socio-economic backgrounds. Second, the current study examined trajectories based on two waves of data across 6 weeks. Although the LCGA can be used for exploring trajectories of two-point data and can minimize the risk of arbitrary and artificial manipulation that commonly occurs in the manual categorization of trajectories [61], it implicitly assumes a linear change pattern. Ideal designs should examine individuals’ longer-term changes in distress and resilience with multiple waves of data—including after the end of the pandemic to explore nonlinear change patterns.
Third, this study aimed to examine how individuals adapted to the pandemic and how reactions during the pandemic might predict resilience and distress. Although the longitudinal design allowed us to investigate the change patterns and explore predictors for change, it is unknown whether some predictors measured at baseline (e.g., eating and use of alcohol) were reactions to the pandemic that may change over time or if they were pre-pandemic traits/behaviors/coping strategies. Prospective studies that measure mental health prior to the pandemic may control for the confounding effects and support the determining of causal associations [19]. Future studies could also investigate whether interventions addressing the identified predictors could effectively change individuals’ distress trajectories. Additionally, some predictors in the current study (e.g., eating behavior) were not assessed using validated scales but with a single item intended to capture perceptions of behavioral change. Objective measures, along with subjective self-report measures, should be used to increase external validity. Despite these limitations, as the pandemic is likely to last for months or even years globally, this study provides vital information for understanding its longer-term effects on individuals’ behavioral and mental health.
Conclusion
In conclusion, the current study presents data on psychological distress and resilience in the face of a global pandemic. Individuals evidenced four theoretical trajectories of distress in the context of COVID-19: chronic, delayed, recovered, and resilient. Key factors associated with distress and resilience over time were coping strategies and hopelessness. Being hopeful and using fewer maladaptive strategies can promote resilience and recovery. Nevertheless, more research is needed to understand the underlying processes that contribute to resilience and distress. Notably, a not insignificant proportion of this sample appeared to be fairly resilient and able to maintain some sense of hope despite the uncertainty and high levels of stress related to this pandemic.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank Jeffrey Cornell for his careful review and edits of the manuscript, and gratitude for his support.
Funding
Dr. Zhang’s work was supported by the National Natural Science Fund of China [grant number 72002008]. The National Social Science Fund of China [grant number 18ZDA056]; The National Natural Science Fund of China [grant number 72072008]; Humanities and Social Sciences Fund of Ministry of Education of China [grant number 19YJC630217]; and The Fundamental Research Funds for the Central Universities [grant number PT2017]. Dr. Veldhuis’ work on this manuscript was supported by an NIH/NIAAA Pathway to Independence Award (K99AA028049; C.B. Veldhuis, Principal Investigator).
Declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statement Regarding Informed Consent
Informed consent was obtained from all participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tao Lin, Email: tl860218@ohio.edu.
Zhihui Yi, Email: zyi7@uic.edu.
Sixue Zhang, Email: zhangsixuess@163.com, Email: sz@mail.buct.edu.cn.
Cindy B. Veldhuis, Email: c.veldhuis@columbia.edu
References
- 1.John Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [Internet]. 2021. Available from: https://coronavirus.jhu.edu/map.html.
- 2.Smid GE, Van Der Velden PG, Lensvelt-Mulders GJLM, Knipscheer JW, Gersons BPR, Kleber RJ. Stress sensitization following a disaster: a prospective study. Psychol Med. 2012;42:1675–1686. doi: 10.1017/S0033291711002765. [DOI] [PubMed] [Google Scholar]
- 3.Höltge J, Mc Gee SL, Maercker A, Thoma MV. A salutogenic perspective on adverse experiences. Eur J Heal Psychol. 2018;25:53–69. doi: 10.1027/2512-8442/a000011. [DOI] [Google Scholar]
- 4.Dalton L, Rapa E, Stein A. Protecting the psychological health of children through effective communication about COVID-19. Lancet Child Adolesc Heal Elsevier. 2020;4:346–347. doi: 10.1016/S2352-4642(20)30097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry Elsevier. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McIntyre RS, Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020;19:250–251. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holingue C, Kalb LG, Rieham KE, Bennett D, Kapteyn A, Veldhuis CB, et al. Mental distress in the United States at the beginning of the COVID-19 pandemic. Am J Public Health. 2020;e1–7. [DOI] [PMC free article] [PubMed]
- 8.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen psychiatry. Shanghai Mental Health Center; 2020;33. [DOI] [PMC free article] [PubMed]
- 9.Ran L, Wang W, Ai M, Kong Y, Chen J, Kuang L. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: a study of the general population in China at the peak of its epidemic. Soc Sci Med. Elsevier Ltd; 2020;262:113261. [DOI] [PMC free article] [PubMed]
- 10.Veldhuis CB, Nesoff ED, McKowen ALW, Rice DR, Ghoneima H, Wootton AR, et al. Addressing the critical need for long-term mental health data during the COVID-19 pandemic: changes in mental health from April to September 2020. Prev Med (Baltim) [Internet]. Elsevier Inc.; 2021;146:106465. Available from: 10.1016/j.ypmed.2021.106465. [DOI] [PMC free article] [PubMed]
- 11.Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 12.Bonanno GA, Mancini AD. Beyond resilience and PTSD: mapping the heterogeneity of responses to potential trauma. Psychol Trauma Theory, Res Pract Policy. 2012;4:74–83. doi: 10.1037/a0017829. [DOI] [Google Scholar]
- 13.Galatzer-Levy IR, Bryant RA. 636,120 ways to have posttraumatic stress disorder. Perspect Psychol Sci. 2013;8:651–662. doi: 10.1177/1745691613504115. [DOI] [PubMed] [Google Scholar]
- 14.Hobfoll SE, Mancini AD, Hall BJ, Canetti D, Bonanno GA. The limits of resilience: distress following chronic political violence among Palestinians. Soc Sci Med [Internet]. Elsevier Ltd; 2011;72:1400–8. Available from: 10.1016/j.socscimed.2011.02.022. [DOI] [PMC free article] [PubMed]
- 15.Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Soc Sci Med [Internet]. Elsevier Ltd; 2009;68:2190–8. Available from: 10.1016/j.socscimed.2009.03.043. [DOI] [PubMed]
- 16.Ahmed AS. Post-traumatic stress disorder, resilience and vulnerability. Adv Psychiatr Treat. 2007;13:369–375. doi: 10.1192/apt.bp.106.003236. [DOI] [Google Scholar]
- 17.Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. 2007;20:251–62. [DOI] [PMC free article] [PubMed]
- 18.Lam WWT, Bonanno GA, Mancini AD, Ho S, Chan M, Hung WK, et al. Trajectories of psychological distress among Chinese women diagnosed with breast cancer. Psychooncology. 2010;19:1044–1051. doi: 10.1002/pon.1658. [DOI] [PubMed] [Google Scholar]
- 19.Galatzer-Levy IR, Huang SH, Bonanno GA. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin Psychol Rev [Internet]. Elsevier; 2018;63:41–55. Available from: 10.1016/j.cpr.2018.05.008. [DOI] [PubMed]
- 20.Dikmen-Yildiz P, Ayers S, Phillips L. Longitudinal trajectories of post-traumatic stress disorder (PTSD) after birth and associated risk factors. J Affect Disord [Internet]. Elsevier B.V.; 2018;229:377–85. Available from: 10.1016/j.jad.2017.12.074. [DOI] [PubMed]
- 21.Bonanno GA, Mancini AD, Horton JL, Powell TM, LeardMann CA, Boyko EJ, et al. Trajectories of trauma symptoms and resilience in deployed US military service members: prospective cohort study. Br J Psychiatry. 2012;200:317–323. doi: 10.1192/bjp.bp.111.096552. [DOI] [PubMed] [Google Scholar]
- 22.Galatzer-Levy IR, Brown AD, Henn-Haase C, Metzler TJ, Neylan TC, Marmar CR. Positive and negative emotion prospectively predict trajectories of resilience and distress among high-exposure police officers. Emotion. 2013;13:545–553. doi: 10.1037/a0031314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong SB, Youssef GJ, Song SH, Choi NH, Ryu J, McDermott B, et al. Different clinical courses of children exposed to a single incident of psychological trauma: a 30-month prospective follow-up study. J Child Psychol Psychiatry Allied Discip. 2014;55:1226–1233. doi: 10.1111/jcpp.12241. [DOI] [PubMed] [Google Scholar]
- 24.Zhu Z, Galatzer-Levy IR, Bonanno GA. Heterogeneous depression responses to chronic pain onset among middle-aged adults: a prospective study. Psychiatry Res. 2014;217:60–66. doi: 10.1016/j.psychres.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bonanno GA, Ho SMY, Chan JCK, Kwong RSY, Cheung CKY, Wong CPY, et al. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: a latent class approach. Heal Psychol. 2008;27:659–667. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- 26.Wheaton MG, Abramowitz JS, Berman NC, Fabricant LE, Olatunji BO. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognit Ther Res Springer. 2012;36:210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- 27.Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry Elsevier. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valiente C, Vázquez C, Contreras A, Peinado V, Trucharte A. A symptom-based definition of resilience in times of pandemics: patterns of psychological responses over time and their predictors. Eur J Psychotraumatol [Internet]. Taylor & Francis; 2021;12. Available from: 10.1080/20008198.2020.1871555. [DOI] [PMC free article] [PubMed]
- 29.Saunders R, Buckman JEJ, Fonagy P, Fancourt D. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol Med. 2020; [DOI] [PMC free article] [PubMed]
- 30.Riehm KE, Brenneke SG, Adams LB, Gilan D, Lieb K, Kunzler AM, et al. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J Affect Disord [Internet]. Elsevier B.V.; 2021;282:381–5. Available from: 10.1016/j.jad.2020.12.071. [DOI] [PMC free article] [PubMed]
- 31.Zhang L, Wang L, Liu Y, Zhang J, Zhang X, Zhao J. Resilience predicts the trajectories of college students’ daily emotions during COVID-19: a latent growth mixture model. Front Psychol. 2021;12. [DOI] [PMC free article] [PubMed]
- 32.Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J Consult Clin Psychol. 2007;75:671–682. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- 33.Holingue C, Badillo-Goicoechea E, Riehm KE, Veldhuis CB, Thrul J, Johnson RM, et al. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: findings from American trend panel survey. Prev Med (Baltim) [Internet]. Elsevier; 2020;139:106231. Available from: 10.1016/j.ypmed.2020.106231. [DOI] [PMC free article] [PubMed]
- 34.Ozdemir O, Boysan M, Guzel Ozdemir P, Yilmaz E. Relationships between posttraumatic stress disorder (PTSD), dissociation, quality of life, hopelessness, and suicidal ideation among earthquake survivors. Psychiatry Res Elsevier Ireland Ltd. 2015;228:598–605. doi: 10.1016/j.psychres.2015.05.045. [DOI] [PubMed] [Google Scholar]
- 35.Glass K, Flory K. Are coping strategies, social support, and hope associated with psychological distress among Hurricane Katrina survivors? 2009;28:779–95.
- 36.Shanahan L, Steinhoff A, Bechtiger L, Murray AL, Nivette A, Hepp U, et al. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. 2020. [DOI] [PMC free article] [PubMed]
- 37.Gambaro E, Mastrangelo M, Sarchiapone M, Marangon D, Gramaglia C, Vecchi C, et al. Resilience, trauma, and hopelessness: protective or triggering factor for the development of psychopathology among migrants? BMC Psychiatry BMC Psychiatry. 2020;20:1–15. doi: 10.1186/s12888-019-2374-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Littleton H, Horsley S, John S, Nelson DV. Trauma coping strategies and psychological distress: a meta-analysis. 2007;20:977–988. doi: 10.1002/jts.20276. [DOI] [PubMed] [Google Scholar]
- 39.Badour CL, Blonigen DM, Boden MT, Feldner MT, Bonn-Miller MO. A longitudinal test of the bi-directional relations between avoidance coping and PTSD severity during and after PTSD treatment. Behav Res Ther [Internet]. Elsevier Ltd; 2012;50:610–6. Available from: 10.1016/j.brat.2012.06.006. [DOI] [PMC free article] [PubMed]
- 40.Karstoft KI, Armour C, Elklit A, Solomon Z. The role of locus of control and coping style in predicting longitudinal PTSD-trajectories after combat exposure. J Anxiety Disord [Internet]. Elsevier Ltd; 2015;32:89–94. Available from: 10.1016/j.janxdis.2015.03.007. [DOI] [PubMed]
- 41.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet [Internet]. Elsevier Ltd; 2020;395:912–20. Available from: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed]
- 42.Rogers AH, Shepherd JM, Garey L, Zvolensky MJ. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res. Elsevier Ireland Ltd; 2020;293:113407. [DOI] [PMC free article] [PubMed]
- 43.Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Rash CJ, Coffey SF, Baschnagel JS, Drobes DJ, Saladin ME. Psychometric properties of the IES-R in traumatized substance dependent individuals with and without PTSD. Addict Behav. 2008;33:1039–1047. doi: 10.1016/j.addbeh.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hosey MM, Leoutsakos JMS, Li X, Dinglas VD, Bienvenu OJ, Parker AM, et al. Screening for posttraumatic stress disorder in ARDS survivors: validation of the impact of event Scale-6 (IES-6) Crit Care Critical Care. 2020;24:1–7. doi: 10.1186/s13054-020-2759-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coffey SF, Gudmundsdottir B, Beck JG, Palyo SA, Miller L. Screening for PTSD in Motor vehicle accident survivors using the PSS-SR and IES. J Trauma Stress. 2006;19:119–128. doi: 10.1002/jts.20106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. Sage Publications Sage CA: Thousand Oaks, CA; 1977;1:385–401.
- 48.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D depression symptoms index. J Aging Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 49.Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 50.Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 51.Moore BC, Biegel DE, Mcmahon TJ. Maladaptive coping as a mediator of family stress. J Soc Work Pract Addict. 2011;11:17–39. doi: 10.1080/1533256X.2011.544600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Muthén & Muthén; 2019.
- 53.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model. 2007;14:535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- 54.IBM Corp. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp; 2020.
- 55.Liu SR, Kia-Keating M, Modir S. Hope and adjustment to college in the context of collective trauma. J Am Coll Heal. 2017;65:323–330. doi: 10.1080/07448481.2017.1312412. [DOI] [PubMed] [Google Scholar]
- 56.Scher CD, Resick PA. Hopelessness as a risk factor for post-traumatic stress disorder symptoms among interpersonal violence survivors. Cogn Behav Ther Taylor & Francis. 2005;34:99–107. doi: 10.1080/16506070510008434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bonanno GA, Diminich ED. Annual research review: positive adjustment to adversity - trajectories of minimal-impact resilience and emergent resilience. J Child Psychol Psychiatry Allied Discip. 2013;54:378–401. doi: 10.1111/jcpp.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fluharty M, Bu F, Steptoe A, Fancourt D. Coping strategies and mental health trajectories during the first 21 weeks of COVID-19 lockdown in the United Kingdom. Soc Sci Med [Internet]. Elsevier Ltd; 2021;279:113958. Available from: 10.1016/j.socscimed.2021.113958. [DOI] [PMC free article] [PubMed]
- 59.Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L, et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. 2020;6:1–9. doi: 10.1192/bjo.2020.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Veldhuis CB, Stuart E, Fallin MD. Five urgent public health policies to combat the mental health effects of COVID-19. Heal Aff blog [Internet]. 2021 Jan; Available from: 10.1377/hblog20210122.959001/full/.
- 61.Duncan TE, Duncan SC, Strycker LA. An introduction to latent variable growth curve modeling: concepts, issues, and application. 2. New York: Taylor & Francis Group; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.