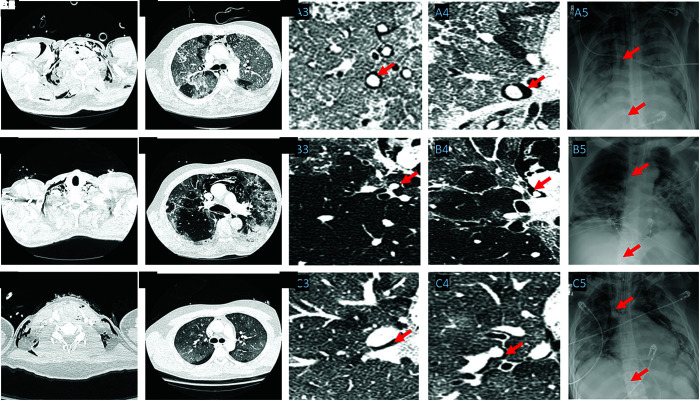
Three healthy adult males (age 48, Figure 1A; age 61, Figure 1B; and age 35, Figure 1C) presented with spontaneous pneumomediastinum from coronavirus disease (COVID-19) before the institution of positive pressure ventilation. Chest computed tomography confirmed pneumomediastinum and air tracking along the pulmonary vasculature. Each patient underwent venovenous extracorporeal membrane oxygenation (VV-ECMO) for optimal lung-protective ventilation to mitigate exacerbation of pneumomediastinum from mechanical ventilation after clinical deterioration. Patients B and C have been liberated from VV-ECMO and discharged, whereas patient A remains on VV-ECMO.
Figure 1.
Chest computed tomography axial slices of the three separate patients with coronavirus disease (COVID-19) presenting with spontaneous pneumomediastinum. The figure is arranged in panels representing each patient (A, B, and C). A1, B1, and C1 demonstrate subcutaneous emphysema, and A2, B2, and C2 show evidence of pneumomediastinum in each patient. A3 and A4, B3 and B4, and C3 and C4 show air tracking along the pulmonary vasculature (shown with red arrows) in magnified chest computed tomography axial slices. A5, B5, and C5 demonstrate the positioning of the cannulas (located in the superior vena cava and inferior vena cava) for venovenous extracorporeal membrane oxygenation (shown with red arrows) on portable chest radiography.
Cases of pneumomediastinum have been described in COVID-19 (1); however, persistent questions remain as to the underlying mechanisms and optimal management strategy. The Macklin effect is a pathophysiologic process initiated by alveolar basement membrane destruction, rupture, interstitial emphysema, and dissecting air along the pulmonary vasculature into the mediastinum (2). The pulmonary pathophysiology of COVID-19 is recognized to be attributed to a widespread inflammation and destruction of the alveolar–capillary unit (3). The Macklin effect, with cyclical rapid changes in transpulmonary pressure during respiration, could account for COVID-19–associated spontaneous pneumomediastinum and represent severe compromise in pulmonary mechanics, culminating in patient self-inflicted lung injury (4). In such cases, the use of VV-ECMO could be considered to provide lung-protective respiratory support.
Footnotes
Originally Published in Press as DOI: 10.1164/rccm.202105-1179IM on August 17, 2021
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Mart MF, Norfolk SG, Flemmons LN, Stokes JW, Bacchetta MD, Trindade AJ, et al. Pneumomediastinum in acute respiratory distress syndrome from COVID-19. Am J Respir Crit Care Med. 2021;203:237–238. doi: 10.1164/rccm.202008-3376IM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Macklin CC. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: clinical implications. Arch Intern Med (Chic) 1939;64:913–926. [Google Scholar]
- 3. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438–442. doi: 10.1164/rccm.201605-1081CP. [DOI] [PubMed] [Google Scholar]