Abstract
Vulnerable populations may be more vulnerable to mental health problems posed by the coronavirus disease 2019 (COVID-19) pandemic. A systematic review was performed to compare the mental health impact of COVID-19 between vulnerable and non-vulnerable groups. Five electronic databases were searched for observational studies reporting the psychological outcomes of both vulnerable populations and healthy controls during the COVID-19 era. The primary outcomes are the severity of depression and anxiety, and secondary outcomes include other aspects of mental health such as stress or sleep disturbance. Meta-analysis was performed for the severity of mental health symptoms, and the results were presented as standardized mean difference and 95% confidence intervals. A total of 25 studies were included. According to the findings, the elderly generally experienced significantly lower levels of psychological symptoms including depression, anxiety, and perceived stress. Pregnant women, patients with chronic diseases, and patients with pre-existing severe mental disorders showed mixed results according to each mental health outcome. The results indicate that vulnerable groups have been affected differently in the COVID-19 era. Though the insufficient number and heterogeneity of included studies leave the results inconclusive, our findings may contribute to identifying priorities of mental health needs among various vulnerable populations and allocating health resources with efficiency.
Keywords: mental health, COVID-19, coronavirus, pandemic, vulnerability
1. Introduction
The Coronavirus disease 2019 (COVID-19) pandemic has been posing a serious threat to people worldwide, not only due to its direct impact on physical health, but also due to its impact on psychological health. Overall, the primary therapeutic goal against the COVID-19 pandemic has mainly been focused on treatment for reducing mortality and prevention strategies, such as social distancing and quarantine [1], whereas mental health issues have not received much attention. However, as COVID-19 creates a huge impact on various aspects of people’s daily life, including separation from loved ones, uncertainty concerning the rapid spread of the pandemic, fear of being infected, feeling a loss of control and freedom, facing urgent socio-economic changes including job loss, financial issues, and changes in daily life style [2,3,4], one can easily assume that its negative psychological influences penetrate deeply into individuals’ daily life. Although psychological strain is difficult to notice and easily overlooked [5], considering its pervasive and accumulating effect on people compared to physical symptoms caused by the infection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [6,7], the psychological impacts of COVID-19 are an important issue. According to a systematic review of general populations affected by the mental health consequences of COVID-19, the prevalence of depression, anxiety, insomnia, posttraumatic stress disorder (PTSD), and psychological distress were 15.97%, 15.15%, 23.87%, 21.94%, and 13.29%, respectively [8]. Mental health experts have also continuously expressed concern over the negative long-term psychological impact of COVID-19 [9], referring to it as ‘new wave of pandemic’ and a ‘post-pandemic wave’ [10], which alarms the detrimental aftereffect of psychological consequences during this unprecedented pandemic era [11].
With respect to mental health resources, the data from the World Health Organization (WHO)’s Mental Health Atlas 2017 demonstrated the scarcity and disparities of the resources within/between countries [12]. This suggests the necessity of efficient utilization of mental health resources to meet needs. Meanwhile, vulnerable groups have been affected differently in other pandemics. During the 2003 severe acute respiratory syndrome (SARS) outbreak, pregnant women showed higher levels of anxiety than the pre-SARS control [13]. In addition, children are likely to develop fear and anxiety-related cognitive biases from threat information given by their parents during an influenza pandemic [14]. Additionally, in other natural disasters such as earthquakes, the elderly survivors were more susceptible to PTSD and general psychiatric morbidity than their younger counterparts [15]. As the elderly are reported to belong to fewer social networks, they may lack the social capital resources available during a disaster [16]. As such, different vulnerable groups may express dissimilar weaknesses, and evaluating the specific mental health vulnerabilities of certain groups could enable the efficient utilization of mental health resources on people most in need.
Psychological burden induced by COVID-19 pandemic disproportionately affects vulnerable populations, which calls for effective and fair support for those who are at the highest risk [17]. However, little is known about how COVID-19 has differently affected the mental health of each vulnerable population. To the best of our knowledge, there is no published article that comprehensively reviews and synthesizes data on mental health among vulnerable populations and compares the mental health impact of COVID-19 between vulnerable and non-vulnerable groups. Thus, we conducted a systematic review and meta-analysis to assess psychological and mental impact among vulnerable populations during the COVID-19 pandemic compared to healthy controls, through which the priorities of mental health needs can be identified.
2. Materials and Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [18] (Supplementary File S1). In addition, the protocol of this systematic review was registered in the Open Science Framework registries (osf.io/k8uy7). There were no amendments to the methodology after protocol registration.
2.1. Search Strategy
Two independent researchers (SH Nam and JH Nam) conducted a comprehensive search in following five electronic databases: Medline via PubMed, EMBASE via ovid, Cochrane library, PsycINFO, and Cumulative Index to Nursing & Allied Health Literature (CINAHL). The search strategy was reviewed by an experienced librarian (Supplementary File S2). There was no restriction on publication status (including gray literature), or publication country. The study search was conducted on 5 March 2021, and all studies published from declaration of the pandemic (11 March 2020) up to the search date (5 March 2021) were considered.
2.2. Eligibility Criteria
2.2.1. Types of Studies
Original cross-sectional or longitudinal studies reporting the psychological outcomes among vulnerable populations with healthy controls during COVID-19 were included. In the case of longitudinal studies, we included the first data measured right after the declaration of the pandemic. The following cases were excluded if they: (1) were not written in English, and (2) were abstracts, editorials, narrative reviews, opinions, perspectives, or letters.
2.2.2. Types of Participants
We defined our target populations (i.e., vulnerable populations) based on previous research considering vulnerability in the COVID-19 context [19,20]. People with chronic diseases, who are particularly suggested as vulnerable individuals in COVID-19 era by the Center for Disease Control and Prevention (CDC) [21], patients with serious mental illness, including schizophrenia, bipolar disorder, obsessive-compulsive disorder, major depressive disorder, generalized anxiety disorder, and panic disorder, those with a disability (disabled), elderly people over 60 years of age, youth/young people/children under 18 years of age and pregnant women are included as vulnerable populations. In the case of youth/young people/children under 18 years of age, although the risks of severe illness and mortality caused by COVID-19 are lower for young people, these populations may be vulnerable in terms of mental health due to other factors, including the loss of education [17] as well as a lack of psychological capital to preserve their mental health [22], as a result of school closures. In addition, child abuse/maltreatment, domestic violence [17], and the unemployment of their parents [23] may affect their mental health status. People with low socioeconomic status such as the unemployed, those with low income or precarious employment, homeless, single parents, racial/ethnic minorities, immigrants, refugee groups, and underinsured (uninsured patients or patients without health insurance) were included. There was no restriction on the severity of symptoms, gender, ethnicity, or race of patients. However, studies which did not present the participants’ information of age ranges or age criteria were excluded.
2.2.3. Types of Outcome
The primary outcomes are the severity of depression and anxiety diagnosed by clinicians or assessed using validated assessment tools as follows.
Depressive symptoms measured by validated tools such as Patient Health Questionnaire (PHQ-9) [24], Beck’s Depression Inventory II (BDI) [25], Center for Epidemiologic Studies Depression Scale (CES-D) [26], Depression subscale of the Depression, Anxiety, and Stress Scale-21 (DASS-21) [27], and Hospital Anxiety and Depression Scale (HADS) [28];
Anxiety symptoms measured by validated instruments such as Generalized Anxiety Disorder Scale-7 (GAD-7) [29], the State-Trait Anxiety Inventory (STAI) [30], Anxiety subscale of DASS-21 [27], and HADS [28].
Secondary outcomes included perceived stress measured by Perceived Stress Scale (PSS) [31], PTSD measured by the Impact of Event Scale (IES) [32], and Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) [33]; sleep quality was measured by validated assessment tools, such as the Insomnia Severity Index (ISI) [34], the Pittsburgh Sleep Quality Index (PSQI) [35], and the Leeds Sleep Evaluation Questionnaire (LSEQ) [36].
2.3. Study Selection
Two reviewers (SH Nam and JH Nam) independently performed a study selection to determine whether the searched studies met the inclusion/exclusion criteria. For the first inclusion, the titles and abstracts of the searched articles were assessed, and the full texts of all eligible studies were reviewed for their relevance. Disagreement regarding study selection was discussed by the two reviewers to resolve, and if the discrepancies were not resolved the corresponding author (CY Kwon) intervened.
2.4. Data Extraction
Data extraction was independently performed by two reviewers (SH Nam and JH Nam) using a standardized form in Microsoft Excel, 2016. The following information were extracted from included articles: first author’s name, year of publication, population (type of vulnerability), socio-demographic characteristics (country, gender proportion, age, ethnicity), study designs, total sample size, response rate, number of drop-outs, outcomes related to mental health, and the results. Disagreement regarding data extraction was discussed by the two reviewers to resolve, and if the discrepancies were not resolved the corresponding author (CY Kwon) intervened.
2.5. Assessment of Study Quality
The methodological quality of included studies was assessed by two independent reviewers (SH Nam and JH Nam) using the Joanna Briggs Institute (JBI) prevalence critical appraisal tool [37], which has been predominantly used in reviews on observational studies for reporting prevalence. This tool includes 9-items as follows: sample frame, sampling method, adequacy of sample size, description of the study settings and subjects, reliability and validity of measurements, appropriate statistical analysis, response rate and management of inadequate response rate. Each item was assessed and evaluated as being “yes”, “no”, “unclear”, or “not applicable” with reasons corresponding to the evaluation. Disagreement regarding the methodological quality assessment was discussed by the two reviewers to resolve, and if the discrepancies were not resolved the corresponding author (CY Kwon) intervened.
2.6. Data Analysis
In this review, quantitative synthesis was attempted according to mental health symptoms. Software Stata version 13.1 (StataCorp, College Station, TX, USA). and metan-code were used for the meta-analysis. A random-effect model was used, and the severity of mental health symptoms was presented as standardized mean difference (SMD) and 95% confidence intervals (CIs). I² statistic was used to estimate statistical heterogeneity, and I² values greater than 50% and 75% were interpreted as substantial and considerable heterogeneity, respectively. However, the heterogeneity of included studies, including the participants’ living environment, times from the COVID-19 outbreak, type of vulnerability, and potential comorbid diseases, were evident. Therefore, in this review, attention was paid to the values of data from individual study rather than pooled data in our meta-analyses.
2.7. Publication Bias
When 10 or more studies were included in each meta-analysis, publication bias was evaluated through funnel plots.
3. Results
3.1. Study Selection
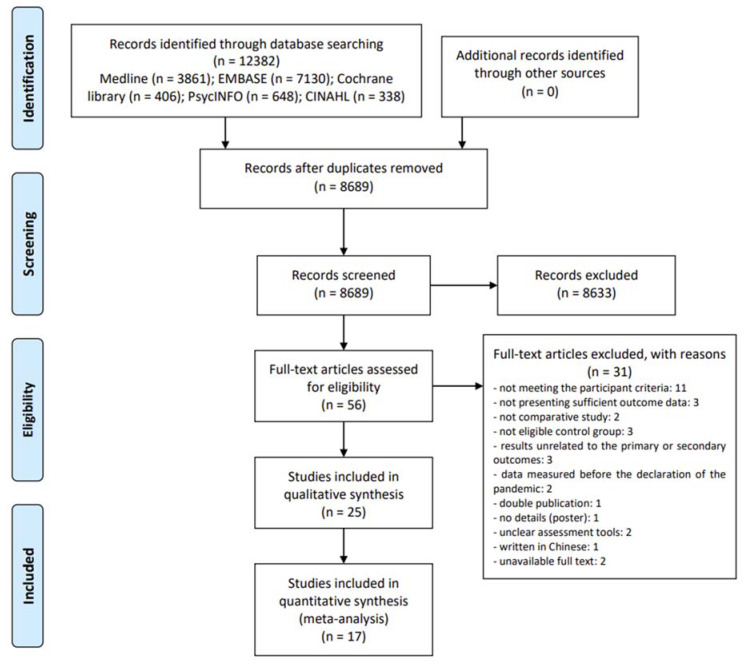
Among the searched 12,382 documents, titles and abstracts of 8689 studies were screened after excluding duplicate documents. The initial screening yielded a review of the full-texts of 56 potentially eligible studies, of which 31 studies that did not meet the inclusion criteria and were excluded (Supplementary File S3). Finally, 25 studies were included in this review [6,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. All of the included studies were written in English. Among them, 17 studies [38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55] were included in the meta-analysis (Figure 1).
Figure 1.
PRISMA Flow diagram.
3.2. Characteristics of Included Studies
Of the 25 studies included, 17 [6,39,40,43,44,45,46,48,49,50,51,53,54,55,56,57,58] were cross-sectional studies, and of the remaining studies, 6 [38,41,42,52,59,60] were case-control studies, and 2 [47,61] were longitudinal studies. Four studies [38,44,54,59] were conducted in Turkey, three in the United States [43,46,61], three in Spain [49,50,51] and Italy [53,55,58], two in Australia [40,48], China [39,56], and Iran [41,45], and one Germany [52], the Netherlands [60], Bangladesh [42], Israel [6], and Argentina [47], respectively. 22 studies [6,38,40,41,42,43,44,45,47,48,49,50,51,52,53,54,55,56,57,58,59,60] did not report the ethnicity of the participants. Otherwise, except for one study [39] involving only Chinese participants, the rest [46,61] were multi-ethnic studies. The subtypes of vulnerable populations among included studies were chronic disease patients in eleven studies [39,41,42,44,52,53,54,57,58,59,60], elderly [6,40,46,49,51] and SMI patients [43,48,50,55,61] in five studies, and pregnant women in four studies [38,45,47,56], respectively. The sample size ranged from 48 to 13,829. Except for three studies [6,40,58] that did not report participants’ ages, three studies reported median with interquartile range [41,44,46], and one study [53] reported range of age; all the remaining studies reported mean age. The most frequently used assessment tool was DASS-21 which was used in 7 studies [42,48,49,50,51,53,55] measuring depressive symptoms, anxiety, and stress. PHQ-9 was used in 5 studies [40,46,56,57,61] for assessing depressive symptoms, GAD-7 was used in 5 studies [40,46,56,57,61] for assessing anxiety, HADS was used in 5 studies [39,41,45,59,60] for assessing both depression and anxiety, and IES was used in 4 studies [46,49,50,51] for evaluating PTSD symptoms. There were only two studies [39,61] measuring sleep disturbance which used PSQI (Table 1).
Table 1.
Characteristics of included studies.
| Study | Study Design | Country | Ethnicity | Type of Vulnerability | Sample Size (M:F) | Mean Age (Year) | Outcomes | Results |
|---|---|---|---|---|---|---|---|---|
| Yassa 2020 | prospective CC | Turkey | NR | Pregnant | G1 (pregnant): 203 G2 (non-pregnant):101 |
G1: 27.4 ± 5.3 G2: 27.6 ± 4.1 |
1. STAI 20-item | 1-1. state anxiety: G1 > G2 + 1-2. trait anxiety: NS |
| García-Portilla 2020 | CS | Spain | NR | Elderly | G1 (60+): 1690 (831:859) G2 (59−): 13,363 (4308:9055) |
G1: 65.9 ± 5.1 G2: (male) 66.5 ± 5.4, (female) 64.4 ± 4.8 |
1. DASS-21 2. IES |
Female/Male 1-1. depression: G1 < G2 +/G1 < G2 + 1-2. anxiety: G1 < G2 +/G1 < G2 + 1-3. stress: G1 < G2 +/G1 < G2 + 2-1. intrusive thoughts: G1 < G2 +/G1 < G2 + 2-2. avoidant behavior: G1 < G2 +/G1 < G2 + |
| Cakiroglu 2020 | CS | Turkey | NR | Chronic disease | G1 (patients):15 G2 (healthy control): 33 |
G1: 15.80 ± 2.11 G2: 15.00 ± 2.5 |
1. STAI 20-item | 1-1. state anxiety: NS 1-2. trait anxiety: G1 > G2 + |
| González-Blanco 2020 | CS | Spain | NR | SMI | G1 (SMI): 125 (48:77) G2 (CMD): 250 (96:154) G3 (HC): 250 (96:154) |
G1: 43.25 ± 14.41 G2: 43.17 ± 14.27 G3: 43.27 ± 14.37 |
1. DASS-21 2. IES |
1-1. depression: G3 < G1 < G2 + 1-2. anxiety: G3 < G1 < G2 + 1-3. stress: G3 < G1 < G2 + 2-1. intrusive thoughts: G3 < G1 < G2 + 2-2. avoidant behavior: G1 < G3 < G2 + |
| Yocum 2021 | LS | United States | Multiethnicity | SMI | G1 (BD): 345 G2 (HC): 147 |
G1, G2: 49 | 1. PHQ-9 2. GAD-7 3. PSQI |
1. depression: G1 > G2 § 2. anxiety: G1 > G2 § 3. sleep: G1 > G2 § |
| Minahan 2020 | CS | United States | Multiethnicity | Elderly | G1 (18–39): 375 G2 (40–64): 542 G3 (65–92): 398 |
G1: 27.98 ± 5.18 G2: 55.44 ± 6.51 G3: 71.32 ± 5.10 |
1. PHQ-9 2. GAD-7 3. IES |
1. depression: G3 < G2 < G1 § 2. anxiety: G3 < G2 < G1 § 3. PTSD: G3 < G2 < G1 § |
| Pinkham 2021 | CS | United States | NR | SMI | G1 (SMI): 163 (64:99) G2 (HC): 27 (13:14) |
G1: 42.74 ± 11.26 G2: 38.41 ± 12.24 |
1. CES-D 2. PSS 3. PROMIS-anxiety |
1. depression: G1 > G2 § 2. stress: G1 > G2 § 3. anxiety: G1 > G2 § |
| Al-Sofiani 2020 | CS | Saudi Arabia | NR | Chronic disease | G1 (patients): 568 (242:326) G2 (HC): 1598 (632:966) |
NR | 1. PHQ-9 2. GAD-7 |
1. depression: G1 > G2 § 2. anxiety: G1 > G2 § |
| Senkalfa 2020 | CS | Turkey | NR | Chronic disease | G1 (patients): 45 (23:22) G2 (HC): 90 (46:44) |
Median (IQR) G1: 99.0 mo (63.3–139.5) G2: 106.7 mo (53.0–159.1) |
1. STAI-C | 1. anxiety: G1 < G2 § |
| Dadra 2020 | retrospective CC | Iran | NR | Chronic disease | G1 (patients): 42 (8:34) G2 (HC): 42 (13:29) |
Median (IQR) G1: 32 (24.5–47.75) G2: 37 (32–45.25) |
1. HADS | 1-1. anxiety: NS 1-2. depression: NS |
| Justo-Alonso 2020 | CS | Spain | NR | Elderly | G1 (18–25): 458 G2 (26–33): 729 G3 (34–45): 1358 G4 (46–60): 749 G5 (60−): 204 |
G1, G2: 39.24 ± 12.00 | 1. DASS-21 2. IES-R |
1-1. depression: G5 < G4 < G3 < G2 < G1 + 1-2. anxiety: G5 < G4 < G3 < G2 < G1 + 1-3. stress: G5 < G4 < G3 < G2 < G1 + 2. G5 < G4 < G3 < G2 < G1 + |
| Balci 2021 | retrospective CC | Turkey | NR | Chronic disease | G1 (patients): 45 (30:15) G2 (HC): 43 (24:19) |
Median (IQR) G1: 67 (60.00–73.50) G2: 66 (58.00–71.00) |
1. HADS | 1-1. depression: NS 1-2. anxiety: NS |
| Muro 2020 | CS | Italy | NR | Chronic disease | G1 (patients): 1113 G2 (HC): 1125 |
Range G1: 11–93 G2: 13–85 |
1. DASS-21 | 1-1. depression: G1 > G2 §
1-2. anxiety: G1 > G2 § 1-3. stress: G1 > G2 § |
| Xia 2020 | CS | China | single ethnicity | Chronic disease | G1 (patients): 119 (61:58) G2 (HC): 169 (76:93) |
G1: 61.18 ± 8.77 G2: 59.84 ± 8.15 |
1. HADS 2. PSQI |
1-1. depression: G1 > G2 +
1-2. anxiety: G1 > G2 * 2. G1 > G2 + |
| Karantonis 2021 | CS | Australia | NR | SMI | Group1 (BD): 43 (19:24) Group2 (HC): 24 (11:13) |
G1: 25.3 ± 11.14 G2: 22.79 ± 12.81 |
1. DASS-21 | 1-1. depression: G1 > G2 * 1-2. anxiety: G1 > G2 * 1-3. stress: G1 > G2 * |
| López-Morales 2020 | LS | Argentina | NR | Pregnant | Group1 (pregnant):102 Group2 (non-pregnant): 102 |
G1: 32.59 ± 4.73 G2: 32.54 ± 4.71 |
1. BDI –II 2. STAI |
1. depression: G1 > G2 § 2. anxiety: G1 > G2 § |
| Sayeed 2021 | prospective CC | Bangladesh | NR | Chronic disease | G1 (patients): 395 (305:90) G2 (HC): 395 (305:90) |
G1: 38.37 ± 12.92 G2: 36.17 ± 6.95 |
1. DASS-21 | 1-1. depression: G1 > G2 +
1-2. anxiety: G1 > G2 + 1-3. stress: G1 > G2 + |
| Stocker 2021 | CS | Australia | NR | Elderly | G1 (18–29): 1337 G2 (30–49): 5148 G3 (50–69): 5897 G 4(70+):1447 |
NR | 1. PHQ-9 2. GAD-7 |
1. depression: G4 < G3 < G2 < G1 § 2. anxiety: G4 < G3 < G2 < G1 § |
| Poll-Franse 2021 | retrospective CC | Netherland | NR | Chronic disease | G1 (patients): 4094 G2 (HC): 977 |
G1: 63.0 ± 11.1 G2: 62.3 ± 13.0 |
1. HADS | 1-1. depression: NS 1-2. anxiety: G1 > G2 + |
| Dobler 2020 | prospective CC | Germany | NR | Chronic disease | G1 (patients): 112 (25:87) G2 (HC): 52 (17:35) |
G1: 54.4 ± 14.0 G2: 52.3 ± 8.9 |
1. PHQ-4 | 1. depression: G1 < G2 + |
| Zach 2021 | CS | Israel | NR | Elderly | G1 (45–59): 645 (182:463) G2 (60–69): 393 (138:255) G3 (70+): 164 (60:103) |
NR | A questionnaire for measuring depressive moods | 1. depression: G1 > G2 > G3 + |
| Burrai 2020 | CS | Italy | NR | SMI | G1 (SMI): 77 (51:26) G2 (HC): 100 (50:50) |
G1: 46.61 ± 12.81 G2: 46.40 ± 11.52 |
1. DASS-21 | 1-1. depression: NS 1-2. anxiety: G1 > G2 * 1-3. stress: G1 < G2 * |
| Ciprandi 2020 | CS | Italy | NR | Chronic disease | G1 (patients): 712 (290:422) G2 (HC): 3560 (1450:2110) |
NS | 1. CPDI | 1. stress: G1 > G2 § |
| Mirzaei 2021 | CS | Iran | NR | Pregnant | G1 (pregnant): 200 G2 (non-pregnant):201 |
G1: 29.69 ± 5.85 G2: 32.59 ± 6.31 |
1. HADS | 1-1. depression: G1 > G2 +
1-2. anxiety: G1 > G2 + |
| Zhou 2020 | CS | China | NR | Pregnant | G1 (pregnant): 544 G2 (non-pregnant):315 |
G1: 31.1 ± 3.9 G2: 35.4 ± 5.7 |
1.PHQ-9 2. GAD-7 3. PCL-5 4. ISI |
1. depression: G1 < G2 + 2. anxiety: G1 < G2 + 2. PTSD: G1 < G2 + 3.sleep: NS |
Note. *, p < 0.05; +, p < 0.01; §, p-value was not reported. Abbreviations. BD, bipolar disorder; CC, case-control study; CES-D, Center for Epidemiologic Studies Depression Scale; CMD, common mental disorders; CS, cross-sectional study; DASS-21, Depression, Anxiety, and Stress Scale-21; G, group; GAD-7, Generalized Anxiety Disorder Scale-7; HADS, Hospital Anxiety and Depression Scale; HC, healthy controls; IES, Impact of Event Scale; IQR, interquartile range; ISI, insomnia severity index; LS, longitudinal study; NS, not significant; PCL-5, The Posttraumatic Stress Disorder Checklist for DSM-5; PHQ-9, Patient Health Questionnaire; PROMIS, Patient Reported Outcomes Measurement In-formation System; PSQI, Pittsburgh Sleep Quality Index; PSS, Perceived Stress Scale; PTSD, posttraumatic stress disorder; SMI, severe mental illness; STAI, State-Trait Anxiety Inventory; STAI-C, State-Trait Anxiety Inventory for Children.
3.3. Methodological Qualities of Included Studies
For question 1, “Was the sample frame appropriate to address the target population?”, 13 studies [6,40,42,43,46,47,49,50,51,56,57,58,60] that used online surveys spread through social media or websites using organizational and personal networks, and presented three or more sociodemographic characteristics or medical history of the participants, were evaluated as Y. Eight studies [38,39,41,44,52,54,55,61] that were conducted at a single institution (a hospital department, a clinical service, etc.) were evaluated as N, while four studies [45,48,53,59] that did not mention the sample frame were evaluated as U. For question 2, “Were study participants sampled in an appropriate way?”, no study was rated as Y as there were no studies that performed random sampling. Eighteen studies [6,39,40,41,42,43,44,45,46,47,49,50,51,52,56,57,58,61] that did not perform random sampling were evaluated as N, and seven studies [38,48,53,54,55,59,60] in which the sampling method was not mentioned were evaluated as U. For question 3, “Was the sample size adequate?”, 13 studies [6,40,42,45,46,49,50,51,53,56,57,58,60] for which sample size calculations were performed or with more than 500 participants were rated as Y based on previous study [62]. Nine studies [38,39,43,44,47,52,54,55,61] that did not clarify how the sample size was calculated were evaluated as U, while three studies [41,48,59] with less than 100 participants were rated as N. For question 4, “Were the study subjects and the setting described in detail?”, 24 studies [6,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,55,56,57,58,59,60,61] describing detailed sociodemographic characteristics of participants such as age, gender, marital status, income, and education were evaluated as Y. However, Cakiroglu et al. (2020) [54], in which sociodemographic characteristics of participants were collected but not presented in detail, was evaluated as U. For question 5, “Was the data analysis conducted with sufficient coverage of the identified sample?”, 19 studies [6,39,40,43,44,45,46,47,48,49,50,51,53,54,55,56,57,58,61] that did not present either the response rate or drop-out rate of subgroups were evaluated as U. Six studies [38,41,42,52,59,60] that used case-control design were rated as NA. For question 6, “Were valid methods used for the identification of the condition?”, all included studies [6,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61] used valid and reliable assessment tools mentioned in the Method section, and were evaluated as Y. For question 7, “Was the condition measured in a standard, reliable way for all participants?”, 19 studies [6,38,39,40,42,45,46,47,48,49,50,51,52,55,56,57,59,60,61] in which all participants answered the same questionnaire during the same period were evaluated as Y, while Ciprandi et al. (2020), in which two groups conducted surveys at a different time period [58], was evaluated as N. Five studies [41,43,44,53,54] that conducted verbal interviews without a detailed description of how reliability was ensured throughout the process (e.g., if the data collectors had undergone a standard training) were evaluated as U. Muro et al. (2020) was also rated as U, since it did not describe how the data were collected [53]. For question 8, “Was there appropriate statistical analysis?”, 24 studies [6,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,54,55,56,57,58,59,60,61] were rated as Y since they used appropriate statistical analysis, such as t-tests, one-way ANOVA, Mann–Whitney U tests, and Chi-Square tests, and presented means and standard deviations (SD). However, that of Muro et al. (2020) [53] was evaluated as N, since they did not present means and SD with appropriate statistical analysis but only presented the N(%) of the participants’ responses. For question 9, “Was the response rate adequate, and if not, was the low response rate managed appropriately?”, 19 studies [6,38,39,40,42,43,44,45,46,47,48,49,50,51,54,55,56,57,58] did not mention the response rate and were evaluated as U. Two studies [53,61] with more than 60% of the total response rate were evaluated as Y based on previous study [63]. Two studies [52,60] with less than 60% of the total response rate, and where non-response appeared to be related to the outcome measured as well as the characteristics of non-responders disparate to those who responded, were evaluated as N. Two studies [41,59] in which the participants were extracted through previous research were rated NA (Table 2).
Table 2.
The risk of bias of included studies.
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
|---|---|---|---|---|---|---|---|---|---|
| Yassa 2020 | N | U | U | Y | NA | Y | Y | Y | U |
| García-Portilla 2020 | Y | N | Y | Y | U | Y | Y | Y | U |
| Cakiroglu 2020 | N | U | U | U | U | Y | U | Y | U |
| González-Blanco 2020 | Y | N | Y | Y | U | Y | Y | Y | U |
| Yocum 2021 | N | N | U | Y | U | Y | Y | Y | Y |
| Minahan 2020 | Y | N | Y | Y | U | Y | Y | Y | U |
| Pinkham 2021 | Y | N | U | Y | U | Y | U | Y | U |
| Al-Sofiani 2020 | Y | N | Y | Y | U | Y | Y | Y | U |
| Senkalfa 2020 | N | N | U | Y | U | Y | U | Y | U |
| Dadra 2020 | N | N | N | Y | NA | Y | U | Y | NA |
| Justo-Alonso 2020 | Y | N | Y | Y | U | Y | Y | Y | U |
| Balci 2021 | U | U | N | Y | NA | Y | Y | Y | NA |
| Muro 2020 | U | U | Y | Y | U | Y | U | N | Y |
| Xia 2020 | N | N | U | Y | U | Y | Y | Y | U |
| Karantonis 2021 | U | U | N | Y | U | Y | Y | Y | U |
| López-Morales 2020 | Y | N | U | Y | U | Y | Y | Y | U |
| Sayeed 2021 | Y | N | Y | Y | NA | Y | Y | Y | U |
| Stocker 2021 | Y | N | Y | Y | U | Y | Y | Y | U |
| Poll-Franse 2021 | Y | U | Y | Y | NA | Y | Y | Y | N |
| Dobler 2020 | N | N | U | Y | NA | Y | Y | Y | N |
| Zach 2021 | Y | N | Y | Y | U | Y | Y | Y | U |
| Burrai 2020 | N | U | U | Y | U | Y | Y | Y | U |
| Ciprandi 2020 | Y | N | Y | Y | U | Y | N | Y | U |
| Mirzaei 2021 | U | N | Y | Y | U | Y | Y | Y | U |
| Zhou 2020 | Y | N | Y | Y | U | Y | Y | Y | U |
Note. Q1, Was the sample frame appropriate to address the target population?; Q2, Were study participants sampled in an appropriate way?; Q3, Was the sample size adequate?; Q4, Were the study subjects and the setting described in detail?; Q5, Was the data analysis conducted with sufficient coverage of the identified sample?; Q6, Were valid methods used for the identification of the condition?; Q7, Was the condition measured in a standard, reliable way for all participants?; Q8, Was there appropriate statistical analysis?; Q9, Was the response rate adequate, and if not, was the low response rate managed appropriately? Abbreviations. N, No; NA, not applicable; U, unclear; Y, yes.
3.4. Mental Health Impact of COVID-19 on Vulnerable Groups
3.4.1. Depressive Symptoms: Primary Outcome
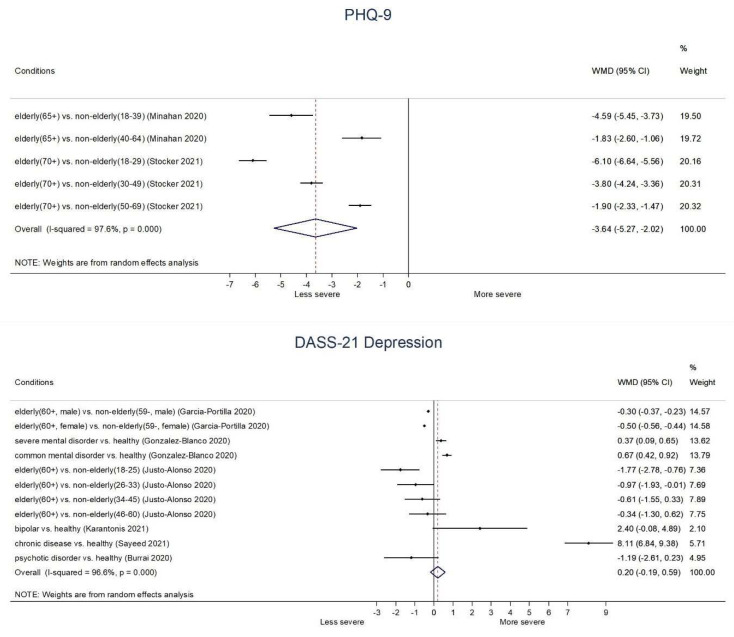
Elderly: In the context of COVID-19, elderly (65+ or 70+) groups generally showed significantly lower depressive symptoms than non-elderly groups on PHQ-9 (WMD −4.59, 95% CI: −5.45 to −3.73 (65+ vs. 18–39 age); −1.84, −2.60 to −1.06 (65+ vs. 40–64 age); −6.10, −6.64 to −5.56 (70+ vs. 18–29 age); −3.80, −4.24 to −3.36 (70+ vs. 30–49 age); −1.90, −2.33 to −1.47 (70+ vs. 50–69 age)) as well as DASS-21 Depression score (−1.77, −2.78 to −0.76 (60+ vs. 18–25 age)); (−0.97, −1.93 to −0.01 (60+ vs. 26–33 age)). In addition, there was borderline significance between elderly (60+) group and 34–45 age group (−0.61, −1.55 to 0.33) or 46–60 age group (−0.34, −1.30 to 0.62) on DASS-21 Depression score. Moreover, both male elderly (60+) (−0.30, −0.37 to −0.23) and female elderly (60+) (−0.50, −0.56 to −0.44) showed significantly lower DASS-21 Depression score than male non-elderly (59−) and female non-elderly (59−), respectively (Figure 2).
Chronic disease: Patients with pulmonary hypertension patients (PHQ-4: 2.30, 1.58 to 3.02), patients with chronic disease (DASS-21 Depression: 8.11, 6.84 to 9.38), and patients with Parkinson’s disease (HADS-Depression: 1.07, 0.13 to 2.01) showed significantly higher depressive symptoms than healthy control. However, there was no significant difference between patients taking immune suppressants compared to healthy control in the HADS-Depression score (−0.22, −1.98 to 1.54) (Figure 2, Supplementary File S4).
Severe mental illness: Patients with SMI (CES-D: 7.71, 5.70 to 9.72; DASS-21 Depression: 0.37, 0.09 to 0.65) and patients with common mental disorder (DASS-21 Depression: 0.67, 0.42 to 0.92) showed significantly higher depressive symptoms than healthy control. In addition, there was borderline significance between patients with bipolar disorder and healthy control (DASS-21 Depression score: 2.40, −0.08 to 4.89), and patients with psychotic disorder and healthy control (DASS-21 Depression score: −1.19, −2.61 to 0.23) (Figure 2).
Pregnant: Pregnant women showed significantly higher depressive symptoms than non-pregnant women on DASS-21 Depression (1.47, 0.78 to 2.16), but not on BDI-II (0.79, −0.68 to 2.26) (Supplementary File S4).
Figure 2.
Depressive symptoms in vulnerable groups during COVID-19. Abbreviations. DASS-21, Depression, Anxiety, and Stress Scale-21; PHQ-9, Patient Health Questionnaire.
3.4.2. Anxiety: Primary Outcome
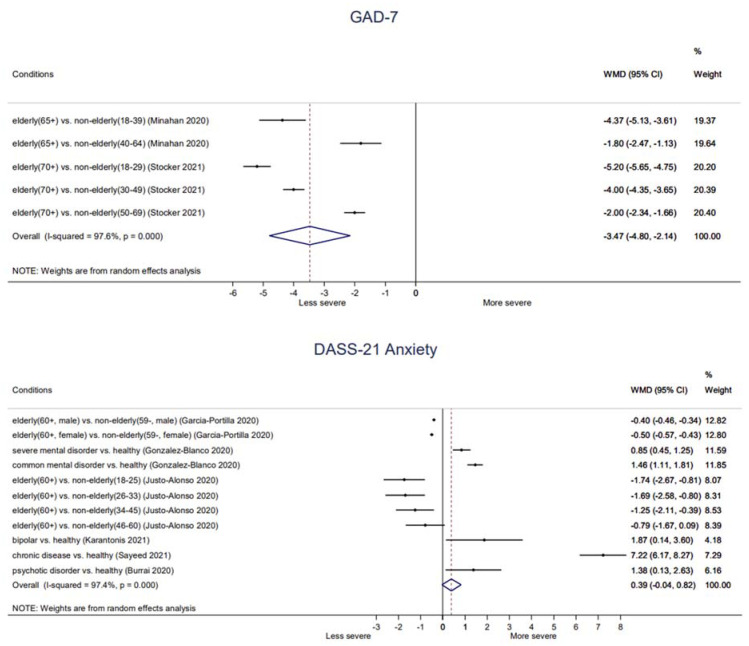
Elderly: Elderly (65+ or 70+) groups generally showed significantly lower anxiety symptoms than non-elderly groups on GAD-7 (−4.37, −5.13 to −3.61 (65+ vs. 18–39 age); −1.80, −2.47 to −1.13 (65+ vs. 40–64 age); −5.20, −5.65 to −4.75 (70+ vs. 18–29 age); −4.00, −4.35 to −3.65 (70+ vs. 30–49 age); −2.00, −2.34 to −1.66 (70+ vs. 50–69 age)) as well as on DASS-21 Anxiety score (−1.74, −2.67 to −0.81 (60+ vs. 18–25 age); −1.69; −2.58 to −0.80 (60+ vs. 26–33 age); −1.25; −2.11 to −0.39 (60+ vs. 34–45 age)). In addition, there was borderline significance between elderly (60+) group and 40–60 age group (−0.79, −1.67 to 0.09) on DASS-21 Anxiety score. Moreover, both male elderly (60+) (−0.40, −0.46 to −0.34) and female elderly (60+) (−0.50, −0.57 to −0.43) showed significantly lower DASS-21 Anxiety score than male non-elderly (59−) and female non-elderly (59−), respectively (Figure 3).
Chronic diseases: There were no significant differences between patients taking immune suppressants (1.38, −0.31 to 3.07) or patients with Parkinson’s disease (0.27, −0.62 to 1.16) compared to healthy control on HADS-Anxiety score. In addition, children with chronic illness (STAI-S: −2.64, −7.90 to 2.62) or children with cystic fibrosis (STAI-S: −1.00, −5.79 to 3.79) did not show significantly different state anxiety compared to healthy peers. However, children with chronic illness showed significantly higher trait anxiety (STAI-T: 6.23, 0.55 to 11.91) than that of healthy peers. Patients with chronic disease showed significantly higher anxiety symptoms (DASS-21 Anxiety: 7.22, 6.17 to 8.27) than that of healthy control (Figure 3, Supplementary File S4).
Severe mental illness: Patients with SMI (Patient Reported Outcomes Measurement Information System Anxiety: 3.71, 2.34 to 5.08; DASS-21 Anxiety: 0.85, 0.45 to 1.25), patients with bipolar disorder (DASS-21 Anxiety: 1.87, 0.14 to 3.60), patients with psychotic disorder (DASS-21 Anxiety: 1.38, 0.13 to 2.63), and patients with common mental disorder (DASS-21 Anxiety: 1.46, 1.11 to 1.81) showed significantly higher anxiety symptoms than healthy control (Figure 3).
Pregnant: There were two conflicting results on state anxiety between pregnant and non-pregnant participants, that one found that that of pregnant women was significantly lower than that of non-pregnant women (STAI-S: −4.66; −7.32 to −2.00), while the other one found no significant difference (STAI-S: 1.15; −1.31 to 3.61). Otherwise, trait anxiety (STAI-T: −3.46, −6.12 to −0.80) and anxiety symptoms (HADS-Anxiety: 0.80, 0.09 to 1.51) of pregnant women were significantly lower than those of non-pregnant women (Supplementary File S4).
Figure 3.
Anxiety symptoms in vulnerable groups during COVID-19. Abbreviations. DASS-21, Depression, Anxiety, and Stress Scale-21; GAD-7, Generalized Anxiety Disorder Scale-7.
3.4.3. Stress—Secondary Outcome
Elderly: Elderly (60+) group showed significantly lower stress symptoms than non-elderly groups on DASS-21 Stress score (−3.37, −4.67 to −2.07 (60+ vs. 18–25 age); −2.97, −4.23 to −1.71 (60+ vs. 26–33 age), −2.65, −3.87 to −1.43 (60+ vs. 34–45 age), −1.54, −2.78 to −0.30 (60+ vs. 46–60 age)). In addition, both male elderly (60+) (−1.00, −1.11 to −0.89) and female elderly (60+) (−1.40, −1.52 to −1.28) showed significantly lower DASS-21 Stress score than male non-elderly (59−) and female non-elderly (59−), respectively (Supplementary File S4).
Chronic disease: Patients with chronic disease showed significantly higher stress symptoms than healthy control on DASS-21 Stress score (8.72, 7.47 to 9.97) (Supplementary File S4).
Severe mental illness: Patients with SMI (PSS: 1.84, 0.68 to 3.00; DASS-21 Stress: 0.42, 0.94 to 0.10) and patients with bipolar disorder (DASS-21 Stress: 2.91, 0.31 to 5.50) showed significantly higher stress symptoms than healthy control. However, patients with psychotic disorder showed significantly lower stress symptoms than healthy control on DASS-21 Stress (1.98, 3.50 to −0.46). Meanwhile, there was no significant difference in common mental disorder patients compared to healthy control in the DASS-21 Stress (0.19, −0.29 to 0.67) (Supplementary File S4).
3.4.4. PTSD—Secondary Outcome
Elderly: Elderly (60+ or 65+) groups generally showed significantly lower PTSD symptoms than non-elderly groups on IES Total score (−0.38, −0.48 to −0.28 (65+ vs. 18–39 age); −0.16, −0.25 to −0.07 (65+ vs. 40–64 age)), IES-R Total score (−5.18, −8.39 to −1.97 (60+ vs. 18–25 age); −5.02, −8.17 to −1.87 (60+ vs. 26–33 age); −4.07, −7.16 to −0.98 (60+ vs. 34–45 age)), IES-R Hyperactivation score (−1.88, −2.86 to −0.90 (60+ vs. 18–39 age); −1.81, −2.77 to −0.85 (60+ vs. 26–33 age); −1.53, −2.47 to −0.59 (60+ vs. 34–45 age)), IES-R Evitation score (−2.10, −3.37 to −0.83 (60+ vs. 18–25 age); −1.48, −2.72 to −0.24 (60+ vs. 26–33 age)), and IES-R Intrusions score (−1.73, −3.15, −0.31 (60+ vs. 26–33 age); 1.37, −2.76 to 0.02 (60+ vs. 34–45 age)). Moreover, both male (60+) and female elderly (60+) showed significantly lower PTSD symptoms than their non-elderly counterparts (IES-Intrusive thoughts: −0.30, −0.41 to −0.19 (male 60+ vs. male 59−); −0.40, −0.52 to −0.28 (female 60+ vs. female 59−); IES-Avoidant Behavior: −0.20, 0.34 to −0.06 (male 60+ vs. male 59−); 0.60, −0.73 to −0.47 (female 60+ vs. female 59−)). A borderline significant difference was found between elderly (60+) and 34–45 age group (−1.17, −2.39 to 0.05) on IES-R Evitation. However, no significant difference was found between elderly (60+) and 46–60 age group (IES-R Total: −1.70, −4.85 to 1.45; IES-R Hyperactivation: 0.90, −1.85 to 0.05; IES-R Intrusions: −0.64, −2.05 to 0.77; IES-R Evitation: −0.15, −1.39 to 1.09). IES-R Intrusions score of elderly (60+) compared to that of 18–25 age group was also not significant (−1.21, −2.66 to 0.24) (Supplementary File S4).
Severe mental illness: Patients with common mental disorder showed significantly higher intrusive thoughts and avoidant behavior than healthy control on IES-Intrusive thoughts (1.06, 0.62 to 1.50) and IES-Avoidant Behavior score (0.96, 0.52 to 1.40), respectively. In addition, there was borderline significance between SMD patients and healthy control on IES-Intrusive thoughts (0.44, −0.04 to 0.92). However, patients with SMI showed significantly lower avoidant behavior than healthy control (IES-Avoidant Behavior: −0.82, −1.32 to −0.32) (Supplementary File S4).
3.4.5. Sleep—Secondary Outcome
Chronic disease: Patients with Parkinson’s disease showed significantly higher sleep disturbance than healthy control (PSQI Global Score: 92.77, 1.85 to 3.69) (Supplementary File S4).
3.4.6. Positive/Negative Affect—Secondary Outcome
Pregnant: No significant difference was found between pregnant women compared with non-pregnant women on positive nor negative affect (PANAS: −0.34, −1.67 to 0.99; 0.14, −1.68, 1.98) (Supplementary File S4).
3.5. Publication Bias
There was no meta-analysis result including 10 or more studies, therefore, publication bias through funnel plots could not be evaluated.
4. Discussion
4.1. The Findings
To the best of our knowledge, there was no systematic review and meta-analysis comparing the mental health impact of COVID-19 between the vulnerable and non-vulnerable groups. In this current study, we analyzed psychological impacts of the COVID-19 pandemic among vulnerable populations compared to healthy controls.
Among the 17 studies included in the meta-analysis, 4 studies were on the elderly, 3 on pregnant women, 6 on patients with chronic diseases, and 4 on patients with SMI. In general, the elderly experienced significantly lower severities of several psychological symptoms including depression, anxiety, and perceived stress compared to non-elderly groups. Severity of PTSD symptoms also tended to be significantly lower in the elderly, although several results were non-significant according to the age of comparison groups. Other vulnerable populations including pregnant women, patients with chronic diseases, and SMI showed mixed results according to each mental health outcome. Specifically, the perceived stress level of patients with chronic diseases was significantly higher than that of the control group, whereas depressive symptoms and anxiety were not significant between the two groups. Pregnant women showed mixed results in depressive symptoms and anxiety results, and insignificant results in positive/negative affect. Patients with pre-existing SMI experienced significantly higher levels of anxiety and sleep disturbance compared to the general public, while showing mixed results on depressive symptoms, perceived stress and PTSD symptoms (Table 3). In general, the included studies did not perform random sampling but used convenience sampling, leaving the results susceptible to selection bias. In addition, in most of the included studies, the response rate or drop-out rate of both the total participants and subgroups was not reported, thus it is unclear whether the studies’ validity was appropriately managed.
Table 3.
Summary of results of included studies.
| Outcomes (Compared to Control Group) |
Elderly | Chronic Disease |
Pregnant | SMI |
|---|---|---|---|---|
| Mental health outcomes | ||||
| Depressive symptoms | ↓ * | Mixed (↑ *, NS) | Mixed (↑ *, NS) | Mixed (↑ *, ↓ *) |
| Anxiety | ↓ * | Mixed (↑ *, NS) | Mixed (↓ *,↑ *, NS) | ↑ * |
| Stress | ↓ * | ↑ * | - | Mixed (↓ *,↑ *) |
| PTSD symptoms | Mixed (↓ *, NS) | - | - | Mixed † (↑ *,↓ *) |
| Sleep disturbance | - | ↑ * | - | - |
| Positive affect | - | - | NS | - |
| Negative affect | - | - | NS | - |
Note. ↑ or ↓, The symptom severity was significantly higher or lower than that of control group; *, p < 0.05; †, the results differed between SMI (bipolar disorder and psychotic disorders) and CMD (depression and anxiety) classified by Gonzalez-Blanco (2020). Abbreviations. CMD, common mental disorder; NS, not significant; PTSD, posttraumatic stress disorder; SMI, severe mental illness.
4.2. Clinical Interpretation
Vulnerable populations are known to be affected by pandemic-induced mental impacts to a greater extent than general populations [64]. The pandemic could exacerbate health disparities and increase susceptibility to stress among vulnerable groups [65], which could eventually make them suffer from more depression, anxiety, distress, and post-traumatic stress [39,42,43,47,48,61,66]. Understanding the psychological impact of COVID-19 on different populations would provide clinical implications for the identification of high-risk groups and designing interventions, as well as policies for better mental health care systems, which is of critical importance in the context of public health at a global level.
Previous studies reported that elderly and patients with pre-existing chronic health conditions are not only at a higher risk of infection and mortality from COVID-19, but are also more likely to experience negative psychological consequences [42,48,52,61]. Interestingly, however, the elderly showed fewer symptoms of poor mental health during the COVID-19 epidemic in several included studies. The results of the studies on the elderly could reflect that older people may already have been living alone with few social contacts or may have been relatively free from economic activities before COVID-19, whereas the younger generation may suffer more from the increased psychological impact of economic restrictions or instability—such as lay-offs—caused by the pandemic [51]. Unlike other natural disasters in which social capital is of great importance [16], COVID-19 discourages social contact, so the limited social network of the elderly may have buffered them against the negative impact of COVID-19 on mental health. In addition, relatively high resilience in old age and low levels of psychological well-being in younger ages could be significant factors regarding better mental health outcomes among the elderly [46]. It is consistent with a previous study which found that, compared to younger populations, elderly, more resilient, and risk-averse people experience less anxiety during COVID-19 [67]. Young people adopt acute changes to their learning methods and make use of online-based technologies and devices, which could aggravate psychological distress [68]. Since sudden loss of income and job insecurity due to COVID-19 have been reported to lead to poorer health outcomes [17], the increased financial instability of an economic crisis may result in negative psychological outcomes among young people. These results are consistent with previous research conducted during different pandemics: the influenza outbreak and SARS, during which decreased distress among the elderly was found [69,70]. Further, during mandated “stay-at-home” periods, social distancing increases family time spent at home, which may act as a positive factor for the elderly who had been spending most of their time at home long before the outbreak.
Meanwhile, individuals with chronic health conditions were found to have suffered from more distress compared to healthy controls. Sayeed (2021) found that the perceived stress of chronic disease patients was higher than that of the healthy control. Strict social distancing, quarantine policy, and fear of infections made it difficult for patients with chronic diseases to utilize consistent medical care, particularly in countries where there is a shortage of medical and human resources [42]. Among Parkinson’s disease patients, higher levels of sleep disturbances were found compared to the healthy controls [39]. Difficulties completing ongoing treatments and making the regular visits to health care services that Parkinson’s disease patients need may contribute to the lack of medical consultation and the sleep state of Parkinson’s disease patients. In addition, the incidence of insomnia, anxiety disorders, and depressive disorders may depend on an individual’s pre-existent health conditions—particularly the presence of autoimmune diseases—rather than their profession [71]. Therefore, people with chronic disease during the pandemic require social and clinical support for their psychological well-being and stress reduction.
Greater anxiety responses in SMI patients than general populations indicate that SMI patients carry an intrinsically increased psychological burden [43]. Restricted opportunities due to poor social networks also make it difficult for individuals with SMI to obtain emotional and substantial support from family members or neighbors [72].
Mixed results may have been found owing to different characteristics of participants and study settings. Specifically, the characteristics of the participants could be dissimilar, depending on whether the patient of SMI or chronic disease is an inpatient, an outpatient, or a patient in residential rehabilitation. Patients in rehabilitation communities may perceive more freedom and security compared to those who are in a hospital setting, but may also get more ongoing social support from staff, medical professionals, and peers [55]. Patients with chronic diseases also tend to use more protective actions, including wearing masks, washing hands, and avoiding crowded public areas [41]. In addition, pregnant women have been reported to show different mental health outcomes depending on factors such as age, marital status, and support from their spouse/family members [73].
Mixed results could also be attributed to the different capacity of each country to cope with mental health problems. According to the WHO, there are significant differences between the coping capacities of each country toward mental health problems [74]. Following the discontinuation of face-to-face services, large differences in the acceptance rates of psychiatric interventions adopting telemedicine or teletherapy were reported between high- and low-income countries. The allocation of resources for maintaining core mental health services also varies from country to country. Specifically, 89% of countries from the survey reported that mental health and psychosocial support were part of their country’s COVID-19 coping plans, but only 17% of these countries possessed additional funds to address these issues. Sociocultural factors are also related to mental health problems caused by COVID-19. Cultural background with social values, individualism, avoidant tendency towards uncertainty, and power balance were pointed out to be associated with disparate behavioral responses and mental health [75].
Furthermore, mixed results may depend on different epidemic stages, or when the lockdown policies were enforced in each country, as well as when mental health was measured in each individual study. Previous research with repeated measures reported that while it was not significant for 2–4 days after formal declaration of social isolation, as time passed (after 47 days) depression and anxiety significantly increased among pregnant women [47]. Different mental effects were also found according to the stage of the epidemic: whether it is in its initial stages with a surge of cases and mortality, or in its alleviating stages with an increasing number of cured patients and formal/obvious information/guidelines on COVID-19 [76]. In sum, mental health outcomes were measured at a different time among the included studies, with differences in the timing and duration of lockdown by country.
4.3. Strengths and Limitations
There are significant public and clinical implications to the present study. As mental health becomes an increasingly important issue in the era of the COVID-19, identifying the priorities of mental health problems according to each psychological symptom in vulnerable populations may enable efficient use of medical resources. In addition, a comprehensive review of the mental health of the vulnerable in the pandemic will help to develop strategies to preemptively protect the mental health of the vulnerable in a similar pandemic in the future. Taking into account the vulnerability of the subject, the results in this study could be used to develop psycho-social interventions at both clinical and community levels in order to effectively address the threat to mental health posed by COVID-19. Considering the fact that vulnerable groups often lack acceptability and proactive use of medical resources [77], the mental health improvement strategy for the vulnerable group is essential in the area of welfare, and the findings in this systematic review will be helpful in developing welfare strategies for improving national mental health.
There are also certain limitations to the present study. First, since we used the first-measured value after the declaration of the pandemic, several results may not have reflected a significant difference throughout time. However, the changing mental health effects over time in the COVID-19 era have been documented in several studies [61,76]. Second, our results cannot confirm the prevalence of diagnosed psychiatric disorders, since the included research did not use clinicians’ standardized interviews but only depended on self-reported measures. Given that mental health assessed by self-reported measures may be overestimated compared to mental health assessed by mental health professionals [78], the psychiatric symptoms in both vulnerable and non-vulnerable groups in our findings may have been exaggerated. Third, due to the insufficient number and heterogeneity of included studies, we could not obtain the results of a meta-analysis based on a sufficient number of studies on specific psychiatric symptoms in specific vulnerable groups. Therefore, most of the mental health effects were based on observational studies, which could potentially affect the credibility of our findings. Fourth, the methodological quality of the included studies was not the best overall. In particular, as most studies did not perform random sampling, the findings of this review may be susceptible to selection bias. This limitation suggests that our findings may be significantly affected by the results published in later high-quality, large-scale observational studies. Fifth, the different sociocultural settings of the included studies may have led to the mixed results since this study did not include a sufficient number of studies to analyze cultural factors. The way to respond to disasters and maintain psychological well-being may differ according to one’s cultural background [79], implying that people are affected differently by the COVID-19 pandemic depending on the culture to which they belong. Sixth, the geographical location of the participants was not taken into account in our study. However, participants in different geographic areas may have experienced a disparate mental health impact from the pandemic, depending on the severity of COVID-19 exposure in their area. For example, a recent study found that differences of geographical regions and population density may affect the magnitude of negative consequences on mental health outcomes during the COVID-19 pandemic [80]. Seventh, we only included comparative studies on ‘a vulnerable population versus a healthy control’ which has left us with large variations in the participants’ age, times from the COVID-19 outbreak, type of vulnerability, and potential comorbid diseases between collected studies. Therefore, in this review, attention was paid to the values of data from individual study rather than pooled data in our meta-analyses. Nonetheless, the variations among included studies could not be eliminated, particularly in terms of age variations in two vulnerable groups—chronic disease patients and SMI patients. Finally, despite our detailed search for various vulnerable groups, such as children, those with a disability (disabled), unemployed, low income or in precarious employment, homeless, single parents, racial/ethnic minorities, immigrants, refugee groups, and underinsured (uninsured patient or patients without health insurance), only four vulnerable groups—the elderly, pregnant women, chronic disease patients, SMI patients—were included in the quantitative analysis. Therefore, the mental health impact of COVID-19 on some vulnerable populations could not be assessed. In the future studies the mental health impact of COVID-19 on other vulnerable populations should be examined. Although excluded because they did not meet the inclusion criteria for this review there are also recent studies investigating the mental health of other vulnerable populations, such as racial/ethnic minorities [81] and people with physical disabilities [82]. In the future, in the context of COVID-19, the mental health of these vulnerable populations needs to be investigated more specifically through comparison with an ethnically mainstream or physically healthy control group.
4.4. Suggestion of Future Studies
Suggestion for future studies can be made based on the limitations. First, future study may wish to examine longitudinal studies on how the mental health of a vulnerable group has changed throughout the COVID-19 era. For example, recently protocols of studies investigating the longitudinal impact of COVID-19 on the mental health of people with disabilities, the elderly [83], and pregnant women and their children [84] have been published. Second, the use of clinicians’ standardized assessments other than self-reported measures can be suggested for future studies, by which the prevalence of diagnosed psychiatric disorders can be better confirmed. However, it should be taken into account that face-to-face evaluation is limited in the COVID-19 era. In this context, in Australia, there are ongoing community mental health services, using telehealth modalities such as video conference, online forums, and mobile apps to manage mental health problems [85], which could suggest alternative strategies for clinicians when evaluating mental health in the face of the pandemic. Third, as more studies on mental health problems in vulnerable populations become available, future systematic reviews and meta-analyses may be better performed in terms of homogeneity, high methodological quality, and including a sufficient number studies. Regarding mental health issues in the COVID-19 era, there have been many studies investigating the mental health of the general population [86], frontline health care workers [87], and COVID-19 patients [88], but few studies on vulnerable groups. However, given that COVID-19 is disproportionately affecting the physical and mental health of the vulnerable [89], future research which illuminates mental health problems of vulnerable groups should be better supported. Fourth, further studies can also be suggested to examine how cultural/geographic factors and the pandemic interact to affect the mental health of each vulnerable group. Since coping strategies and emotional responses to stress situations have been reported to vary among different cultures [90], further studies to confirm the cultural differences in mental health impacts of COVID-19 can be suggested. Fifth, future studies may attempt to control the age range of their included studies, or perform subgroup analysis in terms of age, in order to prevent large age variations in the synthesized data of each vulnerable group. In particular, the better mental health of the elderly found in our study could be clarified in further study, through conducting qualitative interviews of the population. Finally, we encourage future studies to continue to consider the mental health impact of COVID-19 on other vulnerable populations besides the four vulnerable groups that we examined. To facilitate these studies, consensus may be needed to define ‘mentally vulnerable groups’ in the context of COVID-19.
5. Conclusions
Overall, our findings indicate that vulnerable groups have been affected differently in the COVID-19 era. By investigating a wide range of vulnerable groups rather than focusing on a specific vulnerable group, we were able to evaluate whether certain mental health problems were more likely to occur (or be prevalent) in certain vulnerable groups. Although the insufficient number and heterogeneity of included studies leave the results inconclusive, our findings may contribute to identifying the priorities of mental health needs among various vulnerable populations and to allocating health resources efficiently in the present and the future.
Acknowledgments
Thanks to experienced librarian Eun-sun Park at Seoul National University Medical Library for reviewing the search strategy of this review.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph182010830/s1, Supplementary File S1. PRISMA 2020 checklists; Supplementary File S2. Search terms used in each database; Supplementary File S3. Excluded studies after full-text review; Supplementary File S4. The results of meta-analysis in this review.
Author Contributions
Conceptualization, S.-H.N. and J.-H.N.; methodology, S.-H.N., J.-H.N. and C.-Y.K.; formal analysis, S.-H.N., J.-H.N. and C.-Y.K.; data curation, S.-H.N. and J.-H.N.; writing—original draft preparation, S.-H.N. and J.-H.N.; writing—review and editing, S.-H.N., J.-H.N. and C.-Y.K.; visualization, S.-H.N. and J.-H.N.; supervision, C.-Y.K.; project administration, C.-Y.K.; funding acquisition, C.-Y.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: HF20C0079).
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to this study is a systematic literature review targeting previously published studies.
Informed Consent Statement
Patient consent was waived due to this study is a systematic literature review targeting previously published studies.
Data Availability Statement
This data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors have no conflict of interest to declare.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Silva Junior F., Sales J., Monteiro C.F.S., Costa A.P.C., Campos L.R.B., Miranda P.I.G., Monteiro T.A.S., Lima R.A.G., Lopes-Junior L.C. Impact of COVID-19 pandemic on mental health of young people and adults: A systematic review protocol of observational studies. BMJ Open. 2020;10:e039426. doi: 10.1136/bmjopen-2020-039426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simonetti G., Iosco C., Taruschio G. Mental Health and COVID-19: An Action Plan. 2020. [(accessed on 21 March 2021)]. Available online: https://www.preprints.org/manuscript/202004.0197/v1.
- 3.Rubin G.J., Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 4.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zach S., Zeev A., Ophir M., Eilat-Adar S. Physical activity, resilience, emotions, moods, and weight control of older adults during the COVID-19 global crisis. Eur. Rev. Aging Phys. Act. 2021;18:5. doi: 10.1186/s11556-021-00258-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murata S., Rezeppa T., Thoma B., Marengo L., Krancevich K., Chiyka E., Hayes B., Goodfriend E., Deal M., Zhong Y., et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress. Anxiety. 2021;38:233–246. doi: 10.1002/da.23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Dalexis R.D., Goulet M.A., Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021;295:113599. doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pfefferbaum B., North C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 10.APA One Year Later, a New Wave of Pandemic Health Concerns. [(accessed on 21 March 2021)]. Available online: https://www.apa.org/news/press/releases/stress/2021/one-year-pandemic-stress.
- 11.Clemente-Suárez V.J., Navarro-Jiménez E., Jimenez M., Hormeño-Holgado A., Martinez-Gonzalez M.B., Benitez-Agudelo J.C., Perez-Palencia N., Laborde-Cárdenas C.C., Tornero-Aguilera J.F. Impact of COVID-19 pandemic in public mental health: An extensive narrative review. Sustainability. 2021;13:3221. doi: 10.3390/su13063221. [DOI] [Google Scholar]
- 12.Mental Health ATLAS 2017. [(accessed on 21 August 2021)]. Available online: https://www.who.int/publications-detail-redirect/9789241514019.
- 13.Lee D.T., Sahota D., Leung T.N., Yip A.S., Lee F.F., Chung T.K. Psychological responses of pregnant women to an infectious outbreak: A case-control study of the 2003 SARS outbreak in Hong Kong. J. Psychosom. Res. 2006;61:707–713. doi: 10.1016/j.jpsychores.2006.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Remmerswaal D., Muris P. Children’s fear reactions to the 2009 Swine Flu pandemic: The role of threat information as provided by parents. J. Anxiety Disord. 2011;25:444–449. doi: 10.1016/j.janxdis.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 15.Jia Z., Tian W., Liu W., Cao Y., Yan J., Shun Z. Are the elderly more vulnerable to psychological impact of natural disaster? A population-based survey of adult survivors of the 2008 Sichuan earthquake. BMC Public Health. 2010;10:172. doi: 10.1186/1471-2458-10-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer M.A. Elderly Perceptions of Social Capital and Age-Related Disaster Vulnerability. Disaster. Med. Public Health Prep. 2017;11:48–55. doi: 10.1017/dmp.2016.139. [DOI] [PubMed] [Google Scholar]
- 17.Lancet T. Redefining vulnerability in the era of COVID-19. Lancet. 2020;395:1089. doi: 10.1016/S0140-6736(20)30757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open Med. 2009;3:e123–e130. [PMC free article] [PubMed] [Google Scholar]
- 19.Kuy S., Tsai R., Bhatt J., Chu Q.D., Gandhi P., Gupta R., Gupta R., Hole M.K., Hsu B.S., Hughes L.S., et al. Focusing on Vulnerable Populations During COVID-19. Acad. Med. 2020;95:e2–e3. doi: 10.1097/ACM.0000000000003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsai J., Wilson M. COVID-19: A potential public health problem for homeless populations. Lancet Public Health. 2020;5:e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.CDC People with Certain Medical Conditions. [(accessed on 29 April 2021)]; Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
- 22.de Miranda D.M., da Silva Athanasio B., de Sena Oliveira A.C., Silva A.C.S. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduct. 2020:101845. doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health. 2020;14:1–11. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beck A.T., Ward C.H., Mendelson M., Mock J., Erbaugh J. An inventory for measuring depression. Arch. Gen. Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 25.Beck A.T., Steer R.A., Brown G.K. Beck Depression Inventory: BDI-II: Manual. Springer; Dordrecht, The Netherlands: 1987. [Google Scholar]
- 26.Radloff L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 27.Lovibond S.H., Lovibond P.F. Manual for the Depression Anxiety Stress Scales. Psychology Foundation of Australia; Sydney, Australia: 1996. [Google Scholar]
- 28.Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 29.Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 30.Marteau T.M., Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) Br. J. Clin. Psychol. 1992;31:301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 31.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 32.Horowitz M., Wilner N., Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosom. Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Cameron R.P., Gusman D. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Prim. Care Psychiatry. 2003;9:9–14. [Google Scholar]
- 34.Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 35.Buysse D.J., Reynolds C.F., III, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 36.Parrott A.C., Hindmarch I. The Leeds Sleep Evaluation Questionnaire in psychopharmacological investigations—A review. Psychopharmacology. 1980;71:173–179. doi: 10.1007/BF00434408. [DOI] [PubMed] [Google Scholar]
- 37.Joanna Briggs Institute . The Systematic Review of Prevalence and Incidence Data. Joanna Briggs Institute; Adelaide, Australia: 2014. [Google Scholar]
- 38.Yassa M., Yassa A., Yirmibes C., Birol P., Unlu U.G., Tekin A.B., Sandal K., Mutlu M.A., Cavusoglu G., Tug N. Anxiety levels and obsessive compulsion symptoms of pregnant women during the COVID-19 pandemic. Turk. J. Obs. Gynecol. 2020;17:155–160. doi: 10.4274/tjod.galenos.2020.91455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xia Y., Kou L., Zhang G., Han C., Hu J., Wan F., Yin S., Sun Y., Wu J., Li Y., et al. Investigation on sleep and mental health of patients with Parkinson’s disease during the Coronavirus disease 2019 pandemic. Sleep Med. 2020;75:428–433. doi: 10.1016/j.sleep.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stocker R., Tran T., Hammarberg K., Nguyen H., Rowe H., Fisher J. Patient Health Questionnaire 9 (PHQ-9) and General Anxiety Disorder 7 (GAD-7) data contributed by 13,829 respondents to a national survey about COVID-19 restrictions in Australia. Psychiatry Res. 2021;298:113792. doi: 10.1016/j.psychres.2021.113792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shahidi Dadras M., Ahmadzadeh Z., Younespour S., Abdollahimajd F. Evaluation of anxiety and depression in patients with morphea taking immunosuppressive drugs during the COVID-19 pandemic. J. Dermatol. Treat. 2020:1–7. doi: 10.1080/09546634.2020.1819528. [DOI] [PubMed] [Google Scholar]
- 42.Sayeed A., Kundu S., Al Banna M.H., Christopher E., Hasan M.T., Begum M.R., Chowdhury S., Khan M.S.I. Mental Health Outcomes of Adults with Comorbidity and Chronic Diseases during the COVID-19 Pandemic: A Matched Case-Control Study. Psychiatr. Danub. 2020;32:491–498. doi: 10.24869/psyd.2020.491. [DOI] [PubMed] [Google Scholar]
- 43.Pinkham A.E., Ackerman R.A., Depp C.A., Harvey P.D., Moore R.C. COVID-19-related psychological distress and engagement in preventative behaviors among individuals with severe mental illnesses. npj Schizophr. 2021;7:7. doi: 10.1038/s41537-021-00136-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pinar Senkalfa B., Sismanlar Eyuboglu T., Aslan A.T., Ramasli Gursoy T., Soysal A.S., Yapar D., Ilhan M.N. Effect of the COVID-19 pandemic on anxiety among children with cystic fibrosis and their mothers. Pediatr. Pulmonol. 2020;55:2128–2134. doi: 10.1002/ppul.24900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mirzaei N., Jahanian Sadatmahalleh S., Bahri Khomami M., Moini A., Kazemnejad A. Sexual function, mental health, and quality of life under strain of COVID-19 pandemic in Iranian pregnant and lactating women: A comparative cross-sectional study. Health Qual. Life Outcomes. 2021;19:66. doi: 10.1186/s12955-021-01720-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Minahan J., Falzarano F., Yazdani N., Siedlecki K.L. The COVID-19 Pandemic and Psychosocial Outcomes Across Age Through the Stress and Coping Framework. Gerontologist. 2021;61:228–239. doi: 10.1093/geront/gnaa205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.López-Morales H., Del Valle M.V., Canet-Juric L., Andrés M.L., Galli J.I., Poó F., Urquijo S. Mental health of pregnant women during the COVID-19 pandemic: A longitudinal study. Psychiatry Res. 2021;295:113567. doi: 10.1016/j.psychres.2020.113567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Karantonis J.A., Rossell S.L., Berk M., Van Rheenen T.E. The mental health and lifestyle impacts of COVID-19 on bipolar disorder. J. Affect. Disord. 2021;282:442–447. doi: 10.1016/j.jad.2020.12.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Justo-Alonso A., Garcia-Dantas A., Gonzalez-Vazquez A.I., Sanchez-Martin M., Del Rio-Casanova L. How did Different Generations Cope with the COVID-19 Pandemic? Early Stages of the Pandemic in Spain. Psicothema. 2020;32:490–500. doi: 10.7334/psicothema2020.168. [DOI] [PubMed] [Google Scholar]
- 50.González-Blanco L., Dal Santo F., García-Álvarez L., de la Fuente-Tomás L., Moya Lacasa C., Paniagua G., Sáiz P.A., García-Portilla M.P., Bobes J. COVID-19 lockdown in people with severe mental disorders in Spain: Do they have a specific psychological reaction compared with other mental disorders and healthy controls? Schizophr. Res. 2020;223:192–198. doi: 10.1016/j.schres.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garcia-Portilla P., de la Fuente Tomas L., Bobes-Bascaran T., Jimenez Trevino L., Zurron Madera P., Suarez Alvarez M., Menendez Miranda I., Garcia Alvarez L., Saiz Martinez P.A., Bobes J. Are older adults also at higher psychological risk from COVID-19? Aging Ment. Health. 2021;25:1297–1304. doi: 10.1080/13607863.2020.1805723. [DOI] [PubMed] [Google Scholar]
- 52.Dobler C.L., Krüger B., Strahler J., Weyh C., Gebhardt K., Tello K., Ghofrani H.A., Sommer N., Gall H., Richter M.J., et al. Physical Activity and Mental Health of Patients with Pulmonary Hypertension during the COVID-19 Pandemic. J. Clin. Med. 2020;9:4023. doi: 10.3390/jcm9124023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.De Muro M., Amadori S., Ardu N.R., Cerchiara E., De Fabritiis P., Niscola P., Dante S., Schittone V., Tesei C., Trawinska M.M., et al. Impact on Mental Health, Disease Management and Socioeconomic Modifications in Hematological Patients during COVID-19 Pandemia in Italy. Blood. 2020;136:35–37. doi: 10.1182/blood-2020-141599. [DOI] [Google Scholar]
- 54.Cakiroglu S., Yeltekin C., Fisgin T., Oner O.B., Aksoy B.A., Bozkurt C. Are the anxiety levels of pediatric hematology-oncology patients different from healthy peers during the COVID-19 outbreak? J. Pediatric Hematol. Oncol. 2020;43:e608–e612. doi: 10.1097/MPH.0000000000001924. [DOI] [PubMed] [Google Scholar]
- 55.Burrai J., Roma P., Barchielli B., Biondi S., Cordellieri P., Fraschetti A., Pizzimenti A., Mazza C., Ferracuti S., Giannini A.M. Psychological and Emotional Impact of Patients Living in Psychiatric Treatment Communities during Covid-19 Lockdown in Italy. J. Clin. Med. 2020;9:3787. doi: 10.3390/jcm9113787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhou Y., Shi H., Liu Z., Peng S., Wang R., Qi L., Li Z., Yang J., Ren Y., Song X., et al. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl. Psychiatry. 2020;10:319. doi: 10.1038/s41398-020-01006-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Al-Sofiani M.E., Albunyan S., Alguwaihes A.M., Kalyani R.R., Golden S.H., Alfadda A. Determinants of mental health outcomes among people with and without diabetes during the COVID-19 outbreak in the Arab Gulf Region. J. Diabetes. 2021;13:339–352. doi: 10.1111/1753-0407.13149. [DOI] [PubMed] [Google Scholar]
- 58.Ciprandi R., Bonati M., Campi R., Pescini R., Castellani C. Psychological distress in adults with and without cystic fibrosis during the COVID-19 lockdown. J. Cyst. Fibros. 2021;20:198–204. doi: 10.1016/j.jcf.2020.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Balci B., Aktar B., Buran S., Tas M., Donmez Colakoglu B. Impact of the COVID-19 pandemic on physical activity, anxiety, and depression in patients with Parkinson’s disease. Int. J. Rehabil. Res. 2021;44:173–176. doi: 10.1097/MRR.0000000000000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.van de Poll-Franse L.V., de Rooij B.H., Horevoorts N.J.E., May A.M., Vink G.R., Koopman M., van Laarhoven H.W.M., Besselink M.G., Oerlemans S., Husson O., et al. Perceived Care and Well-being of Patients with Cancer and Matched Norm Participants in the COVID-19 Crisis: Results of a Survey of Participants in the Dutch PROFILES Registry. JAMA Oncol. 2021;7:279–284. doi: 10.1001/jamaoncol.2020.6093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yocum A.K., Zhai Y., McInnis M.G., Han P. Covid-19 pandemic and lockdown impacts: A description in a longitudinal study of bipolar disorder. J. Affect. Disord. 2021;282:1226–1233. doi: 10.1016/j.jad.2021.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bujang M.A., Sa’at N., Bakar T.M.I.T.A. Sample size guidelines for logistic regression from observational studies with large population: Emphasis on the accuracy between statistics and parameters based on real life clinical data. Malays. J. Med. Sci. 2018;25:122. doi: 10.21315/mjms2018.25.4.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fincham J.E. Response rates and responsiveness for surveys, standards, and the Journal. Am. J. Pharm. Educ. 2008;72:43. doi: 10.5688/aj720243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.De Sousa A., Mohandas E., Javed A. Psychological interventions during COVID-19: Challenges for low and middle income countries. Asian J. Psychiatr. 2020;51:102128. doi: 10.1016/j.ajp.2020.102128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Santo F., González-Blanco L., García-Álvarez L., la Fuente-Tomás L., Moya-Lacasa C., Paniagua G., Valtueña-García M., Martín-Gil E., Álvarez-Vázquez C., Sáiz P.P. 859COVID-19 lockdown in people with severe mental disorders in Spain: Do they have a specific psychological reaction? Eur. Neuropsychopharmacol. 2020;40:S475–S476. doi: 10.1016/j.euroneuro.2020.09.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McCleskey J., Gruda D. Risk-taking, resilience, and state anxiety during the COVID-19 pandemic: A coming of (old) age story. Personal. Individ. Differ. 2021;170:110485. doi: 10.1016/j.paid.2020.110485. [DOI] [Google Scholar]
- 68.Al-Kumaim N.H., Alhazmi A.K., Mohammed F., Gazem N.A., Shabbir M.S., Fazea Y. Exploring the impact of the COVID-19 pandemic on university students’ learning life: An integrated conceptual motivational model for sustainable and healthy online learning. Sustainability. 2021;13:2546. doi: 10.3390/su13052546. [DOI] [Google Scholar]
- 69.Taylor M.R., Agho K.E., Stevens G.J., Raphael B. Factors influencing psychological distress during a disease epidemic: Data from Australia’s first outbreak of equine influenza. BMC Public Health. 2008;8:347. doi: 10.1186/1471-2458-8-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ko C.H., Yen C.F., Yen J.Y., Yang M.J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin. Neurosci. 2006;60:397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- 71.Wańkowicz P., Szylińska A., Rotter I. Insomnia, Anxiety, and Depression Symptoms during the COVID-19 Pandemic May Depend on the Pre-Existent Health Status Rather than the Profession. Brain Sci. 2021;11:1001. doi: 10.3390/brainsci11081001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Druss B.G. Addressing the COVID-19 Pandemic in Populations with Serious Mental Illness. JAMA Psychiatry. 2020;77:891–892. doi: 10.1001/jamapsychiatry.2020.0894. [DOI] [PubMed] [Google Scholar]
- 73.Alipour Z., Kheirabadi G.R., Kazemi A., Fooladi M. The most important risk factors affecting mental health during pregnancy: A systematic review. East. Mediterr. Health J. 2018;24:549–559. doi: 10.26719/2018.24.6.549. [DOI] [PubMed] [Google Scholar]
- 74.Brunier A., Drysdale C. COVID-19 Disrupting Mental Health Services in Most Countries, WHO Survey. WHO; Geneva, Switzerland: 2020. [Google Scholar]
- 75.Furlong Y., Finnie T. Culture counts: The diverse effects of culture and society on mental health amidst COVID-19 outbreak in Australia. Ir. J. Psychol. Med. 2020;37:237–242. doi: 10.1017/ipm.2020.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gibson B.A., Ghosh D., Morano J.P., Altice F.L. Accessibility and utilization patterns of a mobile medical clinic among vulnerable populations. Health Place. 2014;28:153–166. doi: 10.1016/j.healthplace.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dorz S., Borgherini G., Conforti D., Scarso C., Magni G. Comparison of self-rated and clinician-rated measures of depressive symptoms: A naturalistic study. Psychol. Psychother. Theory Res. Pract. 2004;77:353–361. doi: 10.1348/1476083041839349. [DOI] [PubMed] [Google Scholar]
- 79.Jogia J., Kulatunga U., Yates G., Wedawatta G. Culture and the psychological impacts of natural disasters: Implications for disaster management and disaster mental health. Built. Hum. Environ. Rev. 2014;7:1. [Google Scholar]
- 80.Hennein R., Mew E.J., Lowe S.R. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS ONE. 2021;16:e0246602. doi: 10.1371/journal.pone.0246602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Goldmann E., Hagen D., El Khoury E., Owens M., Misra S., Thrul J. An examination of racial and ethnic disparities in mental health during the Covid-19 pandemic in the US South. J. Affect. Disord. 2021;295:471–478. doi: 10.1016/j.jad.2021.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lebrasseur A., Fortin-Bédard N., Lettre J., Bussières E.-L., Best K., Boucher N., Hotton M., Beaulieu-Bonneau S., Mercier C., Lamontagne M.-E. Impact of COVID-19 on people with physical disabilities: A rapid review. Disabil. Health J. 2020;14:101014. doi: 10.1016/j.dhjo.2020.101014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Reid H., Miller W.C., Esfandiari E., Mohammadi S., Rash I., Tao G., Simpson E., Leong K., Matharu P., Sakakibara B. The Impact of COVID-19–Related Restrictions on Social and Daily Activities of Parents, People with Disabilities, and Older Adults: Protocol for a Longitudinal, Mixed Methods Study. JMIR Res. Protoc. 2021;10:e28337. doi: 10.2196/28337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Giesbrecht G.F., Bagshawe M., van Sloten M., MacKinnon A.L., Dhillon A., van de Wouw M., Vaghef-Mehrabany E., Rojas L., Cattani D., Lebel C. Protocol for the Pregnancy During the COVID-19 Pandemic (PdP) Study: A Longitudinal Cohort Study of Mental Health Among Pregnant Canadians During the COVID-19 Pandemic and Developmental Outcomes in Their Children. JMIR Res. Protoc. 2021;10:e25407. doi: 10.2196/25407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhou X., Snoswell C.L., Harding L.E., Bambling M., Edirippulige S., Bai X., Smith A.C. The role of telehealth in reducing the mental health burden from COVID-19. Telemed. e-Health. 2020;26:377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 86.Xiong J., Lipsitz O., Nasri F., Lui L.M., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vizheh M., Qorbani M., Arzaghi S.M., Muhidin S., Javanmard Z., Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 2020;19:1967–1978. doi: 10.1007/s40200-020-00643-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhao Q., Hu C., Feng R., Yang Y. Investigation of the Mental Health of Patients with Novel Coronavirus Pneumonia. Chin. J. Neurol. 2020;12:E003. [Google Scholar]
- 89.Egede L.E., Ruggiero K.J., Frueh B.C. Ensuring mental health access for vulnerable populations in COVID era. J. Psychiatr. Res. 2020;129:147. doi: 10.1016/j.jpsychires.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tweed R.G., White K., Lehman D.R. Culture, stress, and coping: Internally-and externally-targeted control strategies of European Canadians, East Asian Canadians, and Japanese. J. Cross Cult. Psychol. 2004;35:652–668. doi: 10.1177/0022022104270109. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This data used to support the findings of this study are included within the article.