Abstract
Aim
The long-term stress, anxiety and job burnout experienced by healthcare workers (HCWs) are important to consider as the novel coronavirus disease (COVID-19) pandemic stresses healthcare systems globally. The primary objective was to examine the changes in the proportion of HCWs reporting stress, anxiety, and job burnout over six months during the peak of the pandemic in Singapore. The secondary objective was to examine the extent that objective job characteristics, HCW-perceived job factors, and HCW personal resources were associated with stress, anxiety, and job burnout.
Method
A sample of HCWs (doctors, nurses, allied health professionals, administrative and operations staff; N = 2744) was recruited via invitation to participate in an online survey from four tertiary hospitals. Data were gathered between March-August 2020, which included a 2-month lockdown period. HCWs completed monthly web-based self-reported assessments of stress (Perceived Stress Scale-4), anxiety (Generalized Anxiety Disorder-7), and job burnout (Physician Work Life Scale).
Results
The majority of the sample consisted of female HCWs (81%) and nurses (60%). Using random-intercept logistic regression models, elevated perceived stress, anxiety and job burnout were reported by 33%, 13%, and 24% of the overall sample at baseline respectively. The proportion of HCWs reporting stress and job burnout increased by approximately 1·0% and 1·2% respectively per month. Anxiety did not significantly increase. Working long hours was associated with higher odds, while teamwork and feeling appreciated at work were associated with lower odds, of stress, anxiety, and job burnout.
Conclusions
Perceived stress and job burnout showed a mild increase over six months, even after exiting the lockdown. Teamwork and feeling appreciated at work were protective and are targets for developing organizational interventions to mitigate expected poor outcomes among frontline HCWs.
Introduction
The novel coronavirus disease (COVID-19) pandemic has caused a devastating global health crisis in 2020 that has seen more than 100 million infected and 2 million deaths worldwide [1]. In some countries, maximum-capacity ICU admissions and mounting death tolls have significantly stressed healthcare systems, which are sustained by healthcare workers (HCWs) working tirelessly on the frontlines. The long-term stress, anxiety and job burnout experienced by HCWs are thus important to investigate.
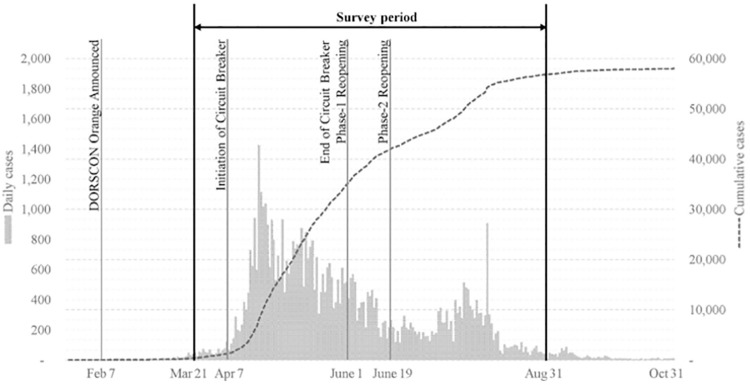
Singapore is a densely populated city state of 5·69 million residents. Between the six-month period of March 1 to August 31, 2020, confirmed cases of COVID-19 rose from 106 to 56,812 (Fig 1). The sharp rise in cases over the April-June period was largely attributed to several outbreak clusters in migrant worker dormitories, with 95% of the nation’s cases coming from these clusters [2]. A nationwide lockdown (called Circuit Breaker) was instituted between April 7-June 1 [3]. Although Singapore’s ICU capacity has not been compromised and the overall death rate of 0·05% is considered low [4], the country has been at the second highest alert level of the national 4-level Disease Outbreak Response System Condition since February 2020, and healthcare systems have introduced many new protocols to increase vigilance and precautionary measures [5].
Fig 1. Timeline of COVID-19 cases in Singapore and study survey period.
It is posited that being in such a state of stress and vigilance for a prolonged period of time will lead to negative psychological outcomes for HCWs. Early studies have reported elevated rates of chronic stress, anxiety states and job burnout among HCWs [6–8]. Reports of psychological morbidities appear to be widespread among frontline health workers, with a meta-analytic study suggesting that 41% of HCWs reported psychological distress during the COVID-19 period [9]. These results are unsurprising given the significant stressors facing frontline workers during the pandemic (e.g., personal safety and that of family and colleagues, long work hours, shortage of protective equipment) and highlight the importance of research focusing on those working on the frontlines. However, existing studies have mostly been cross-sectional in design and examined HCW outcomes only at specific time points in the pandemic.
The current study prospectively examined changes in the proportion of HCWs reporting stress, anxiety, and job burnout over a period of six months encompassing the peak of the outbreak and lockdown in Singapore. We hypothesized that the rates of perceived stress, anxiety, and job burnout among HCWs would increase over time. We were also interested to know the extent objective job characteristics (occupation, managerial role, experience of severe acute respiratory syndrome [SARS] as a HCW, years of working experience, level of exposure to COVID-19, working nightshifts, long work hours), HCW-perceived job factors (perceived job risk, teamwork, COVID-19-related communication, job dedication, feeling appreciated at work), and personal resources (self-efficacy, emotional support) were associated with the psychological outcomes of interest controlling for demographic, self-reported health, and time factors. The Job Demands-Resources Model [10, 11] of employee well-being and suggests that job demands (e.g., burnout) may be offset by resources, which may be provided/cultivated at work (e.g., teamwork, positive work environment) or be intrinsic to the individual (e.g., self-efficacy). We hypothesized that HCW-perceived job factors and personal resources, which are malleable and may be targets of intervention, will be significantly associated with stress, anxiety, and job burnout. Understanding the risk or protective effect these factors have on the psychological outcomes of HCWs may be useful for developing targeted interventions or mitigating expected poor outcomes as the global pandemic continues.
Materials and methods
Study design
This study used the convenience sampling method to prospectively follow HCWs from four tertiary hospitals in Singapore that provided care to COVID-19 patients during the pandemic. Recruitment occurred throughout the duration of the study. The self-reported data were collected from 12 March—31 August 2020, which included the peak of the pandemic that year and the nationwide lockdown period that occurred between April 7-June 1, 2020.
Participants & data collection
Doctors, nurses, allied health professionals, administrative and operations staff from several institutions (Singapore General Hospital, KKH Women’s & Children’s Hospital, Changi General Hospital, Sengkang General Hospital) within the largest public healthcare group in Singapore were invited through work email and/or staff portals to participate. There were no exclusion criteria. Participation was voluntary and those who were interested accessed the study through a web link or QR code. Participants provided their consent online before completing the initial survey and monthly follow-ups which took 15 and 10 minutes to complete, respectively. Follow-up survey links were sent directly to participants’ email address, which served as a way to link the responses over time. No other personal identifying information was collected. Research assistants who managed the data collection on the Qualtrics platform were not involved in data analyses. The survey was administered in English. The study was approved by the National University of Singapore IRB (S-20-081) and exempted from review by the SingHealth Centralized IRB (2020/2160).
Measurements of study variables
Study outcomes
Stress was measured using the 4-item Perceived Stress Scale (PSS-4) [12]. A summed score ranging from 0–16 was calculated, and a median score threshold of ≥ 8 was used to indicate stress. Anxiety was measured using the 7-item Generalized Anxiety Disorder (GAD-7) scale [13]. A summed score ranging from 0–21 was calculated and the recommended threshold score of ≥ 10 was used. Job burnout was measured using a one-item burnout question from the Physician Work Life Scale where a score ≥ 3 indicated presence of job exhaustion [14]. The measure has been used with a range of HCWs including doctors, nurses, and administrative personnel [14]. Higher scores on all study outcomes indicated greater severity.
Objective job characteristics
Participants reported their number of working years in healthcare. The responses to the following questions were coded “yes”/ “no”: whether they had a supervisory role, experienced the 2003 SARS outbreak as a HCW, worked night-shifts in the past month and worked longer than usual hours in the past month. Exposure to COVID-19 was assessed by “How often does your job require you to come in contact with suspected/ confirmed COVID-19 patients/ specimens?” with the response options being “not at all”, “occasionally”, and “daily”.
HCW-perceived job factors
Perceived job risk was assessed using the item “I feel that my job puts me at great risk of exposure to COVID-19” where responses ranged from “strongly agree” to “strongly disagree” on a 6-point scale which was later recoded into a binary variable (high risk vs. low risk) [15]. Effective COVID-19 communication in the workplace was assessed using three items: availability/ timeliness of updates, trustworthiness of information, and clarity of policies and protocols. Teamwork was assessed via the statement “My work team has been working well together”. The response options were “yes”, “neutral”, and “no”. These workplace support questions were considered to have face validity and adapted from a previous SARS outbreak study [16]. Job dedication was measured using the subscale from the Utrecht Work Engagement Scale-9 [17], where a higher summed score indicated higher job dedication, which consisted of feelings of enthusiasm, inspiration and pride for one’s job. Feeling appreciated was assessed by the statement “I feel appreciated by my department/ hospital/ employer” where the responses were coded into a binary variable: “never”/ “rarely” vs. “sometimes”/ “always”.
Personal resources
The 4-item short forms of the Patient-Reported Outcomes Measurement Information System (PROMIS) [18] measures of emotional support [19] and general self-efficacy [20] were used. The Emotional Support scale assesses perceived feelings of being cared for and valued as a person, while the General Self-efficacy scale measures confidence in exerting control over one’s situation. Both measures were rated to on a 5-point scale, with higher scores indicating increase in the construct measured. Summed scores were converted into T-scores.
Self-reported health
Presence of a chronic health condition was assessed by the question “In your lifetime, have you ever been diagnosed by a physician as having a chronic disease or medical condition?” with the response options “yes”, “no” and “neutral”. Whether a participant had been quarantined during the duration of the study was coded as “yes”/ “no”.
Data analysis
A random-intercept logistic regression model, which is robust when missingness depends only on observed data (i.e., missing at random [MAR]), was used to investigate two questions: (1) whether rates of stress, anxiety, and job burnout among HCWs were increasing over time, and (2) what were the predictors of stress, anxiety, and job burnout among HCWs. To address the first question, we regressed the psychological outcomes of interest on calendar month. Calendar months were initially specified as a categorical variable to visualize trends, and later as a continuous variable to test for any statistically significant linear or quadratic trends.
To address the second question, we regressed the psychological outcomes of interest on potential predictors, while controlling for calendar month, demographic factors (age, gender, marital status, presence of a chronic health condition and living with children, elderly, or vulnerable persons), and placement on quarantine related to COVID-19. Predictors considered include objective job characteristics, HCW-perceived job factors and personal resources which were described earlier. Regression models omitting HCW-perceived job factors and personal resources were also estimated to investigate how predictive objective job characteristics are of the outcomes in the absence of information on subjective factors. Analyses were conducted using Stata version 15·1 [21] and statistical inference was based on cluster-robust standard errors (SEs) at the individual level [22] and the 5% significance level.
Results
A total of 2744 HCWs participated in the survey. The study had a rolling admission and proportions of the sample completing their initial survey were 34% in March, 38% in April, 24% in May, 3% in June and 1% in July. Participants responded an average of two surveys. The majority of the sample were nurses (60%), female (81%), and lived with others considered vulnerable (children, elderly, or immunocompromised individuals; 57%). A small proportion reported being put on quarantine due to COVID-19 at some point during the study period (9%). The HCWs in this sample reported daily, occasional, and no contact with suspected/ confirmed COVID-19 cases at rates of 20%, 48% and 33% respectively. Refer to Table 1 for breakdown by occupation and further details.
Table 1. Healthcare worker characteristics (N = 2744).
| All | Doctors | Nurses | Allied health professionals | Others | |
|---|---|---|---|---|---|
| (N = 2744) | (n = 383) | (n = 1637) | (n = 409) | (n = 315) | |
| Mean (SD) or Frequency (%) | |||||
| Demographics | |||||
| Female | 2227 | 201 | 1473 | 316 | 237 |
| (81%) | (52%) | (90%) | (77%) | (75%) | |
| Male | 517 | 182 | 164 | 93 | 78 |
| (19%) | (48%) | (10%) | (23%) | (25%) | |
| Age | 38·86 | 37·80 | 34·75 | 35·36 | 39·95 |
| (10·59) | (9·95) | (10·31) | (10·10) | (11·99) | |
| Marital status | |||||
| Single | 1214 | 152 | 729 | 217 | 116 |
| (44%) | (40%) | (45%) | (53%) | (37%) | |
| Married | 1445 | 223 | 857 | 184 | 181 |
| (53%) | (58%) | (52%) | (45%) | (58%) | |
| Divorced/Separated | 68 | 8 | 43 | 5 | 12 |
| (3%) | (2%) | (3%) | (1%) | (4%) | |
| Widowed | 17 | 0 | 8 | 3 | 6 |
| (1%) | (0%) | (1%) | (1%) | (2%) | |
| Self-reported Health | |||||
| Living with vulnerable household members | 1558 | 225 | 890 | 251 | 192 |
| (57%) | (59%) | (54%) | (61%) | (61%) | |
| Have chronic medical condition | 567 | 73 | 331 | 80 | 83 |
| (21%) | (19%) | (20%) | (20%) | (26%) | |
| Been on quarantine due to COVID-19 | 233 | 30 | 133 | 53 | 17 |
| (9%) | (8%) | (9%) | (14%) | (6%) | |
| Job Characteristics | |||||
| Work experience as HCW | |||||
| <5 years | 624 | 81 | 314 | 119 | 110 |
| (23%) | (21%) | (19%) | (29%) | (35%) | |
| 5–9 years | 725 | 89 | 449 | 102 | 85 |
| (27%) | (23%) | (28%) | (25%) | (27%) | |
| 10–14 years | 651 | 75 | 439 | 89 | 48 |
| (24%) | (20%) | (27%) | (22%) | (15%) | |
| 15+ years | 727 | 137 | 428 | 94 | 68 |
| (27%) | (36%) | (26%) | (23%) | (22%) | |
| Managerial/Supervisory role | 771 | 194 | 344 | 155 | 78 |
| (28%) | (51%) | (21%) | (38%) | (25%) | |
| Experienced SARS as HCW | 589 | 91 | 358 | 75 | 65 |
| (22%) | (24%) | (22%) | (18%) | (21%) | |
| Contact with COVID-19 cases | |||||
| No contact | 900 | 67 | 366 | 240 | 227 |
| (33%) | (18%) | (22%) | (59%) | (72%) | |
| Occasional contact | 1306 | 254 | 866 | 124 | 62 |
| (48%) | (66%) | (53%) | (30%) | (20%) | |
| Daily contact | 537 | 62 | 404 | 45 | 26 |
| (20%) | (16%) | (25%) | (11%) | (8%) | |
| Long work hours | 1045 | 144 | 675 | 126 | 100 |
| (40%) | (40%) | (43%) | (33%) | (34%) | |
| Worked night shifts | 1394 | 183 | 1107 | 65 | 39 |
| (53%) | (50%) | (71%) | (17%) | (13%) |
|
Note. Frequencies may not add up to total sample size due to missing responses.
The majority (71%) of HCWs perceived their job to put them at high risk of exposure to COVID-19. The majority perceived COVID-19-related communication to be timely (82%), trustworthy (82%) and clear (63%); that their team worked well together (76%); and that they felt appreciated at work (80%). Elevated perceived stress, anxiety, and job burnout were reported by 33%, 13% and 24% of the overall sample at baseline, respectively; nurses reported the highest rates across all study outcomes. Refer to Table 2 for further details.
Table 2. Healthcare worker-perceived job factors, personal resources, and study outcomes at initial survey (N = 2744).
| All | Doctor | Nurse | Allied health | Others | |
|---|---|---|---|---|---|
| (n = 2744) | (n = 383) | (n = 1637) | (n = 409) | (n = 315) | |
| Mean (SD) or Frequency (%) | |||||
| Perceived job factors | |||||
| Job risk | |||||
| High | 1882 | 263 | 1264 | 208 | 147 |
| (71%) | (71%) | (80%) | (53%) | (49%) | |
| Low | 758 | 106 | 318 | 180 | 154 |
| (29%) | (29%) | (20%) | (46%) | (51%) | |
| Effective COVID-19 communication | |||||
| Available/timely updates (Yes) | 2100 | 296 | 1253 | 313 | 238 |
| (82%) | (82%) | (81%) | (83%) | (82%) | |
| Trustworthy information (Yes) | 2110 | 317 | 1242 | 319 | 232 |
| (82%) | (88%) | (80%) | (85%) | (80%) | |
| Clear protocols and policies (Yes) | 1617 | 197 | 977 | 239 | 204 |
| (63%) | (55%) | (63%) | (64%) | (70%) | |
| Teamwork | |||||
| Yes | 1948 | 311 | 1137 | 283 | 217 |
| (76%) | (86%) | (73%) | (76%) | (75%) | |
| Neutral | 580 | 42 | 393 | 80 | 65 |
| (23%) | (12%) | (25%) | (21%) | (22%) | |
| No | 33 | 4 | 15 | 10 | 4 |
| (1%) | (1%) | (1%) | (3%) | (1%) | |
| Not applicable | 17 | 4 | 6 | 2 | 5 |
| (1%) | (1%) | (0·5%) | (1%) | (2%) | |
| Feel appreciated at work | |||||
| Never/Rarely | 507 | 60 | 303 | 80 | 64 |
| (20%) | (17%) | (20%) | (21%) | (22%) | |
| Sometimes/Always | 2071 | 301 | 1248 | 295 | 227 |
| (80%) | 83%) | (80%) | (79%) | (78%) | |
| Job dedication | 12·52 | 13·52 | 12·36 | 12·42 | 12·33 |
| (3·35) | (3·07) | (3·39) | (3·12) | (3·54) | |
| Personal resources | |||||
| Self-efficacy | 44·87 | 46·96 | 44·56 | 44·30 | 44·64 |
| (7·90) | (7·63) | (7·77) | (8·00) | (8·40) | |
| Emotional Support | 50·40 | 52·08 | 50·22 | 50·45 | 49·21 |
| (8·46) | (7·63) | (8·55) | (8·42) | (8·74) | |
| Study outcomes | |||||
| Stress (PSS-4) | 6·10 (2·61) | 5·74 (2·50) | 6·21 (2·64) | 6·05 (2·49) | 5·98 (2·66) |
| score ≥ 8 | 33% | 26% | 36% | 29% | 28% |
| Anxiety (GAD-7) | 4·96 (4·47) | 4·58 (4·20) | 5·07 (4·58) | 4·94 (4·12) | 4·91 (4·59) |
| score ≥10 | 13% | 11% | 14% | 12% | 13% |
| Job burnout (PWLS-1) | 2·12 (0·79) | 1·99 (0·70) | 2·18 (0·81) | 2·13 (0·73) | 1·95 (0·77) |
| score ≥3 | 24% | 17% | 27% | 22% | 16% |
Note. Frequencies may not add up to total sample size due to missing responses.
Change over time
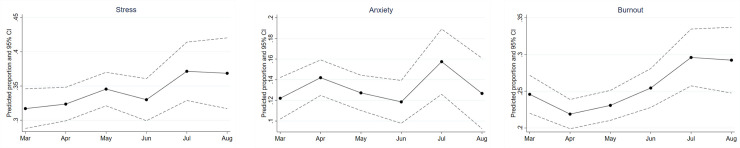
Fig 2 plots predicted the proportion of HCWs reporting stress, anxiety, and job burnout by calendar months, accounting only for random individual effects. Fig 2(a) and 2(c) show that the proportion of HCWs reporting stress and job burnout were trending upwards over the period of March to August. In particular, there was an increase in proportion of HCWs reporting job burnout in July and August relative to April, which was when the lockdown was implemented and when hospital services were cut back (p = ·001). While the proportion reporting anxiety did not exhibit a clear increasing trend, the timing of its fluctuations upwards appeared to coincide with the implementation of the lockdown in April/ May and resumption of full hospital services in July.
Fig 2.
(a)-(c). Proportion of healthcare workers reporting stress, anxiety and job burnout. (a). Proportion of healthcare workers reporting stress between March-August 2021. (b). Proportion of healthcare workers reporting anxiety between March-August 2021. (c). Proportion of healthcare workers reporting job burnout between March-August 2021. Note. Predicted proportions estimated from a random intercept model without additional controls.
Specifying calendar months as a continuous variable, we used the same regression model (controlling only for random individual effects) to test for linear and quadratic trends. We found statistically significant positive linear trends for stress (OR = 1·08, SE = 0·04, p < ·05) and job burnout (OR = 1·16, SE = 0·05, p < ·01), implying that the proportion of HCWs who reported being stressed and burnt out increased by approximately 1·0% and 1·2% respectively per month over the study period. The quadratic term for calendar months was significant only for job burnout (p < ·05).
Predictors of stress, anxiety, and job burnout
For each outcome, we estimated two models (Table 3). Model 1 examined the association between outcomes of interest and objective job characteristics only while controlling for demographic, self-reported health, and time factors. Working long hours was significantly associated with stress, anxiety, and job burnout. Occupation was also related to the study outcomes. Compared to doctors, nurses were more likely to report higher stress, AHPs more likely to report job burnout, and other HCWs were more likely to report anxiety. Compared to HCWs with the least work experience, HCWs worked 5–9 years were more likely to report job burnout. Being in a managerial/supervisory role was associated with lower stress.
Table 3. Predictors of stress, anxiety, and job burnout.
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Stress | Anxiety | Job Burnout | Stress | Anxiety | Job Burnout | |
| Objective Job Characteristics: | ||||||
| Doctor | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Nurse | 1·79** | 1·43 | 1·63† | 1·11 | 0·88 | 1·02 |
| (0·36) | (0·43) | (0·43) | (0·21) | (0·26) | (0·26) | |
| Allied Health | 1·25 | 1·39 | 1·85* | 0·82 | 0·91 | 1·35 |
| (0·31) | (0·49) | (0·58) | (0·19) | (0·32) | (0·40) | |
| Others | 1·22 | 2·21* | 1·17 | 0·71 | 1·29 | 0·75 |
| (0·34) | (0·86) | (0·42) | (0·19) | (0·51) | (0·26) | |
| Managerial/Supervisory role | 0·72* | 0·76 | 1·01 | 0·88 | 0·99 | 1·24 |
| (0·12) | (0·17) | (0·21) | (0·13) | (0·23) | (0·24) | |
| Experienced SARS as HCW | 0·68 | 1·22 | 0·83 | 0·73 | 1·40 | 0·98 |
| (0·18) | (0·48) | (0·30) | (0·18) | (0·53) | (0·33) | |
| < 5 years’ experience | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| 5–9 years’ experience | 1·12 | 0·97 | 1·72* | 0·97 | 0·78 | 1·44† |
| (0·21) | (0·25) | (0·40) | (0·18) | (0·21) | (0·31) | |
| 10–14 years’ experience | 0·87 | 0·73 | 1·33 | 0·83 | 0·67 | 1·37 |
| (0·21) | (0·25) | (0·39) | (0·19) | (0·23) | (0·38) | |
| 15+ years’ experience | 1·18 | 1·17 | 1·14 | 1·03 | 0·10 | 1·19 |
| (0·37) | (0·55) | (0·46) | (0·31) | (0·47) | (0·45) | |
| No COVID-19 contact | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Occasional COVID-19 contact | 1·19 | 1·04 | 1·37† | 1·06 | 0·89 | 1·41* |
| (0·17) | (0·20) | (0·23) | (0·14) | (0·18) | (0·23) | |
| Daily COVID-19 contact | 1·25 | 1·28 | 1·11 | 1·37† | 1·19 | 1·46† |
| (0·22) | (0·31) | (0·24) | (0·23) | (0·29) | (0·30) | |
| Work night shift | 0·95 | 1·11 | 1·30 | 1·06 | 1·25 | 1·48* |
| (0·13) | (0·22) | (0·23) | (0·15) | (0·25) | (0·26) | |
| Long work hours | 1·95** | 2·85** | 4·12** | 1·63** | 2·27** | 3·36** |
| (0·22) | (0·46) | (0·58) | (0·18) | (0·38) | (0·46) | |
| HCW-Perceived Job Factors: | ||||||
| Team work well together | - | - | - | 0·59** | 0·69* | 0·55** |
| (0·08) | (0·13) | (0·08) | ||||
| Effective COVID-19 communication | - | - | - | 0·90* (0·05) | 0·91 (0·07) | 0·94 (0·06) |
| Job dedication | - | - | - | 0·87** | 0·85** | 0·76** |
| (0·02) | (0·03) | (0·02) | ||||
| Perceived job risk | - | - | - | 1·29** | 1·80** | 1·11 |
| (0·11) | (0·24) | (0·12) | ||||
| Feel appreciated at work (Sometimes/Always) | - | - | - | 0·65** (0·09) | 0·41** (0·08) | 0·34** (0·05) |
| Personal Resources: | ||||||
| Emotional support | - | - | - | 0·95** | 0·97** | 0·98* |
| (0·01) | (0·01) | (0·01) | ||||
| Self-efficacy | - | - | - | 0·92** | 0·94** | 0·96** |
| (0·01) | (0·01) | (0·01) | ||||
| Observations | 4857 | 4857 | 4858 | 4758 | 4758 | 4759 |
SARS = Severe Acute Respiratory Syndrome; HCW = healthcare worker
Coefficients represent odds ratios. Cluster-robust standard errors at the individual level are reported in parentheses. Additional controls not reported in the table include calendar month dummies, age, gender, marital status, presence of chronic health condition and living with children, elderly, or vulnerable persons), and placement on quarantine related to COVID-19. Statistical significance denoted by † p<0·10 * p<0·05, ** p<0·01.
Model 2 examined the contribution of HCW-perceived job factors and personal resources to the earlier model. Perceived high job risk was associated with increased stress and anxiety. Effective COVID-19 communication was associated with lower stress. As expected, perceived teamwork, job dedication, feeling appreciated at work, self-efficacy and emotional support were significantly and negatively associated with lower stress, anxiety, and job burnout. Most objective job characteristics that were predictive of psychological outcomes in Model 1 (i.e., occupation, years of working experience, and holding a managerial role) were no longer statistically significant with the inclusion of subjective factors (i.e., HCW-perceived job factors and personal resources) in Model 2. Only long work hours, working night shifts and frequency of COVID-19 contact remained significant in Model 2.
Discussion
Our data show changes in the proportion of HCWs who reported stress, anxiety, and job burnout at the peak of the COVID-19 pandemic in Singapore. Prospective data collection was made possible by online, electronic surveys that allowed fast, efficient data collection with wide reach. The proportion of HCWs reporting stress and job burnout rose an average of 1·0% and 1·2% per month respectively over the study period, with indications of a U-shaped trend for rates of job burnout. These findings are consistent with our hypotheses and corroborate reports in the news worldwide that HCWs are feeling the brunt of the pandemic as it wears on. The generally mild increase over time found in the study may reflect the relative stability we see in Singapore, and the healthcare system’s ability to effectively respond to the outbreak, i.e., low community transmissions, wide-spread testing efforts, minimal COVID-19 transmissions to healthcare workers within the work setting, etc.
We found fluctuations in the proportion of HCWs reporting anxiety that potentially reflect pandemic-response events such as entering and exiting the lockdown. Given that anxiety may be viewed as a sequelae of maladaptive coping to stress, one would expect stress and anxiety to have similar trajectories. Instead, the proportion of HCWs reporting anxiety did not continue to increase after the lockdown (in contrast to stress), suggesting that HCWs are resilient and had ways to cope that allowed their anxiety to return to earlier levels after pandemic-response events.
The trajectory of job burnout is one that appears to reflect how busy workload was for the majority of HCWs during the study period. We see that rate of job burnout decreased during the lockdown when many elective services/ procedures in the hospital were temporarily halted and split-team arrangements were implemented, which then progressively increased as hospitals resumed services, dealt with the backlog of cases, and had an increased number of patients who were admitted for suspected COVID-19 (e.g., patients with community-acquired pneumonia). Additionally, HCWs had to adjust to newly-implemented infection control protocols and audits, while dealing with patients and families that were also adjusting to new hospital policies such as mandatory swabs, restricted visitations, etc. The rates of job burnout in July and August were significantly higher than March pre-lockdown, however it is unclear whether they are significantly different than pre-COVID-19 rates as we do not have the data for comparison. However, our early rate of job burnout (ie, 25% in March) corresponds to that of palliative care HCWs in Singapore pre-COVID-19 that indicated 26% of their respondents reported emotional exhaustion (an aspect of burnout which is similar to what we measured) [23].
HCW-perceived job factors and personal resources, as compared to objective job characteristics, were found to be significantly associated with stress, anxiety, and job burnout. Although the frequency of COVID-19 contact and night shifts were significantly associated with job burnout, only reports of working longer hours than usual appeared to be strongly and consistently associated with stress, anxiety, and job burnout. The effects of long work hours is compounded by not having time-off to rest and recharge. Anecdotal reports indicate HCWs taking minimal time off in the last year, partly due to increased workload post-lockdown and partly due to international travel restrictions. Future studies may want to consider residential status of healthcare workers, especially when a substantial proportion of the healthcare workforce consists of HCWs who are non-residents or with families overseas.
Previously published studies on HCW well-being during the COVID-19 pandemic have reported various job risk factors, notably that nurses and those with a higher degree of exposure to suspected/ confirmed cases have poorer outcomes [7, 8, 24]. Our data indicate that there are factors beyond objective job characteristics that are important to consider, e.g., perceiving one’s job to be high risk increased the odds of stress and anxiety by 29% and 80% respectively. Our findings are consistent with prior studies examining the role of perceived risk [25, 26] and highlight the opportunities leaders in positions of authority have to shape and influence these perceptions of risks, especially in the context where there may be fear among HCWs due to misinformation, e.g. over-inflation of the transmissibility of the virus or its sequelae.
A number of protective factors emerged, with the two most important ones being teamwork and feeling appreciated at work. HCWs who reported that their team(s) worked well together and that they felt appreciated at work sometimes or always had 31–45% and 35–66% respectively lower odds of being stressed, anxious, and burnt out. Being able to trust and depend on one another and feeling valued are intuitively important in times like this, and our data substantiates this. There have been countless efforts around the world to show appreciation to various groups of frontline workers throughout the pandemic, and indeed, they are important morale boosters. A less well-publicized strategy relates to efforts to improve or maintain camaraderie and teamwork among HCWs. This may be particularly important for those on the frontlines who are exhausted, crave human connection, yet have been told to minimize contact with one another for safety purposes. Readers who are further interested about psychological principles that can improve teamwork in medical settings during crisis are referred to Traylor et al.’s review [27]. Consistent with findings in prior literature, other protective factors that were associated with mitigation of stress, anxiety, and job burnout include job dedication (i.e., feelings of enthusiasm, inspiration and pride for one’s job), emotional support (i.e., having others to confide in), and self-efficacy (i.e., feeling confident in one’s ability to cope) [28–30]. These resources are potentially important to build and nurture at the workplace, and will help the healthcare workforce be psychologically resilient during challenging times.
Study limitations
We did not measure previous mental health history; this was a conscious decision made to respect HCW privacy. We did not have pre-COVID-19 data to compare prior rates of stress, anxiety, and job burnout; thus, our interpretation of the data is only within the study time frame. We had considerable dropouts where approximately half of our sample contributed one data point; this was dealt by using a random-intercept model. Our model assumes that data missingness depends only on observed data (ie, MAR); in the worst case scenario, we are underestimating rates of stress, anxiety, and job burnout as those who dropped out had higher odds of being stressed at their initial survey.
Conclusions
Our prospective investigation found that during the six-month peak of the pandemic in Singapore, stress and job burnout increased mildly over time, while anxiety fluctuated according to pandemic-response events. We found that there are a number of protective work-related and personal resources that may be modifiable through initiatives and interventions to ameliorate HCW stress, anxiety, and job burnout, two of which are teamwork and feeling appreciated at work. Every country or hospital setting has its own unique features and challenges, and our hope is that the findings presented can be helpful in any way to others as we continue the ongoing worldwide battle.
Data Availability
Data cannot be shared publicly because of the sensitive nature of mental health information of healthcare workers. Data is owned by SingHealth and may be made available for researchers who meet the criteria for access to confidential data by contacting the SingHealth Data Protection Office at pdpa@singhealth.com.sg.
Funding Statement
The authors acknowledge the support of the Pandemic Impact and Resilience Fund by the Musim Mas Group, through the Singapore General Health Hospital Development Fund (grant no. FRGR01PNDM20 to TKH, https://www.giving.sg/web/sghhdf). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Worldometer [Internet]. COVID-19 Coronavirus Pandemic. [cited 2021 Jan 26]. Available from: https://www.worldometers.info/coronavirus/.
- 2.Ministry of Health Singapore [Internet]. Measures to Contain the COVID-19 Outbreak in Migrant Worker Dormitories. Singapore 2020. Available from: https://www.moh.gov.sg/news-highlights/details/measures-to-contain-the-covid-19-outbreak-in-migrant-worker-dormitories
- 3.Ministry of Health Singapore [Internet]. Circuit Breaker to Minimize Further Spread of COVID-19 Singapore 2020 [cited 2020 February 12]. Available from: https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19.
- 4.Geddie J, Aravindan A. Why is Singapore’s COVID-19 death rate the world’s lowest. Reuters. 2020. Sept 17; Sect. APAC. [Google Scholar]
- 5.Ministry of Health Singapore [Internet]. Risk Assessment Raised to DORSCON Orange Singapore 2020 [cited 2020 February 12]. Available from: https://www.moh.gov.sg/news-highlights/details/risk-assessment-raised-to-dorscon-orange.
- 6.Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020. Apr 1;7(4):e15–e6. doi: 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA network open. 2020. Mar 23;3(3):e203976–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naldi A, Vallelonga F, Di Liberto A, Cavallo R, Agnesone M, Gonella M, et al. COVID-19 pandemic-related anxiety, distress and burnout: prevalence and associated factors in healthcare workers of North-West Italy. BJPsych Open. 2021. Jan 7;7(1). doi: 10.1192/bjo.2020.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry research. 2020. Nov;293:113382. doi: 10.1016/j.psychres.2020.113382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bakker AB, Demerouti E. The Job Demands-Resources model: State of the art. Journal of Managerial Psychology. 2007;22(3):19. doi: 10.1108/02683940710733115 [DOI] [Google Scholar]
- 11.Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. Journal of Applied psychology. 2001. July;86(3):499. [PubMed] [Google Scholar]
- 12.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983. Dec:385–96. [PubMed] [Google Scholar]
- 13.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of internal medicine. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 14.Dolan ED, Mohr D, Lempa M, Joos S, Fihn SD, Nelson KM, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30(5):582–7. Epub 2014/12/03. doi: 10.1007/s11606-014-3112-6 ; PubMed Central PMCID: PMC4395610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koh D, Lim MK, Chia SE, Ko SM, Qian F, Ng V, et al. Risk Perception and Impact of Severe Acute Respiratory Syndrome (SARS) on Work and Personal Lives of Healthcare Workers in Singapore What Can We Learn? Medical Care. 2005. July:676–82. doi: 10.1097/01.mlr.0000167181.36730.cc [DOI] [PubMed] [Google Scholar]
- 16.Shiao JS, Koh D, Lo LH, Lim MK, Guo YL. Factors predicting nurses’ consideration of leaving their job during the SARS outbreak. Nurs Ethics. 2007. Jan 1;14(1):5–17. Epub 2007/03/06. doi: 10.1177/0969733007071350 . [DOI] [PubMed] [Google Scholar]
- 17.Schaufeli WB, Bakker AB, Salanova M. The Measurement of Work Engagement With a Short Questionnaire: A Cross-National Study. Educ Psychol Meas. 2006. Aug 1;66(4):701–16. doi: 10.1177/0013164405282471 [DOI] [Google Scholar]
- 18.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of clinical epidemiology. 2010. Nov;63(11):1179–94. doi: 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shensa A, Sidani JE, yi Lin L, Bowman ND, Primack BA. Social media use and perceived emotional support among US young adults. Journal of community health. 2016. Jun;41(3):541–9. doi: 10.1007/s10900-015-0128-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salsman JM, Schalet BD, Merluzzi TV, Park CL, Hahn EA, Snyder MA, et al. Calibration and initial validation of a general self-efficacy item bank and short form for the NIH PROMIS®. Quality of Life Research. 2019. Sep;28(9):2513–23. doi: 10.1007/s11136-019-02198-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooperation S. Stata 15. Stata Cooperation, College Station, TX. 2017. [Google Scholar]
- 22.Cameron AC, Miller DL. A practitioner’s guide to cluster-robust inference. Journal of human resources. 2015. Mar;50(2):317–72. [Google Scholar]
- 23.Koh MYH, Chong PH, Neo PSH, Ong YJ, Yong WC, Ong WY, et al. Burnout, psychological morbidity and use of coping mechanisms among palliative care practitioners: A multi-centre cross-sectional study. Palliative medicine. 2015. Mar;29(7):633–42. [DOI] [PubMed] [Google Scholar]
- 24.Lu W. ea. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research. 2020. Epub 4 Apil 2020. doi: 10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lam SC, Arora T, Grey I, Suen LKP, Huang EY-z, Li D, et al. Perceived risk and protection from infection and depressive symptoms among healthcare workers in mainland China and Hong Kong during COVID-19. Frontiers in psychiatry. 2020. July 15;11:686. doi: 10.3389/fpsyt.2020.00686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yıldırım M, Arslan G, Özaslan A. Perceived Risk and Mental Health Problems among Healthcare Professionals during COVID-19 Pandemic: Exploring the Mediating Effects of Resilience and Coronavirus Fear. International Journal of Mental Health and Addiction 2020. Nov 16:1–11. doi: 10.1007/s11469-020-00424-8 ; PMCID: PMC7668285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Traylor AM, Tannenbaum SI, Thomas EJ, Salas E. Helping healthcare teams save lives during COVID-19: Insights and countermeasures from team science. Am Psychol. 2021. Jan;76(1):1–13. doi: 10.1037/amp0000750 Epub 2020 Oct 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vagni M, Maiorano T, Giostra V, Pajardi D. Coping with COVID-19: emergency stress, secondary trauma and self-efficacy in healthcare and emergency workers in Italy. Frontiers in Psychology. 2020. Sep 3;11:566912. doi: 10.3389/fpsyg.2020.566912 ; PMCID: PMC7494735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. General hospital psychiatry. 2020. Nov-Dec;67:144–145. doi: 10.1016/j.genhosppsych.2020.03.011 Epub 2020 Apr 3. ; PMCID: PMC7194721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiong H, Yi S, Lin Y. The Psychological Status and Self-Efficacy of Nurses During COVID-19 Outbreak: A Cross-Sectional Survey. Inquiry: A Journal of Medical Care Organization, Provision and Financing. 2020. Sep 8;57. doi: 10.1177/0046958020957114 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data cannot be shared publicly because of the sensitive nature of mental health information of healthcare workers. Data is owned by SingHealth and may be made available for researchers who meet the criteria for access to confidential data by contacting the SingHealth Data Protection Office at pdpa@singhealth.com.sg.