To the Editor:
COVID-19 has led to significant global changes in clinical practice with several health care providers transitioning to virtual health care (VHC); however, the impact of VHC on patients with neuropituitary tumors remains unclear. We sought to assess the impact of VHC on referral patterns of neuropituitary tumors at our center.
The Halifax Neuropituitary Program is the sole tertiary care referral center for patients with neuropituitary disorders in Atlantic Canada and maintains a comprehensive provincial database of all neuropituitary tumors in the province of Nova Scotia. In response to the COVID-19 pandemic, Nova Scotia went into a strict lockdown in March 2020, and all nonemergency provincial health care was abruptly transitioned to VHC, which was mainly conducted through telephone monitoring.
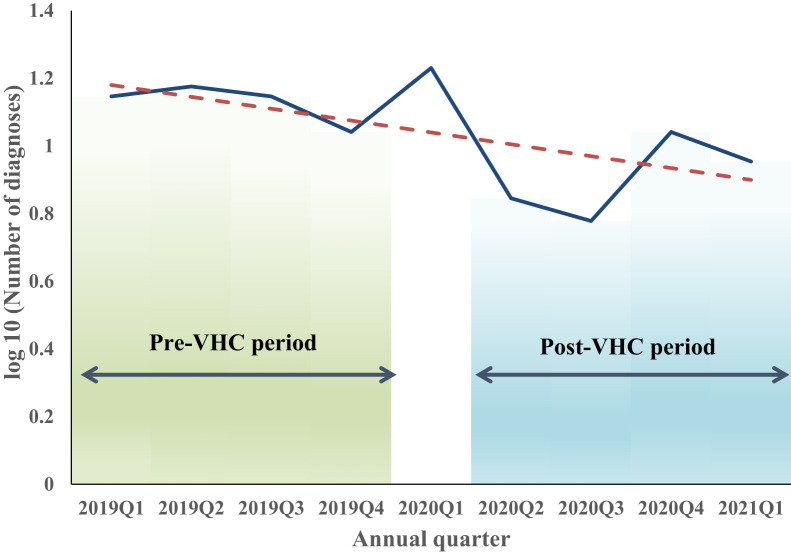
We retrospectively reviewed data on new referrals to the Halifax Neuropituitary Program from January 2019 to April 2021. To examine the effect of COVID-19–related VHC, data for each year were divided into annual quarters. We assumed 2019Q1 to 2019Q4 to be the pre-VHC period and 2020Q2 to 2021Q1 as the post-VHC period. The number of new diagnoses for nonfunctioning pituitary adenoma, prolactinoma, adrenocorticotropic hormone–producing adenoma, growth hormone–producing adenoma (acromegaly), Rathke cleft cyst, craniopharyngioma, and sellar meningioma were quantified and compared between the pre- and post-VHC periods (Fig.).
Fig.
Decreasing trend in the overall neuropituitary diagnoses at the Halifax Neuropituitary Program. A provincial state of emergency was declared on March 22, 2020, during which all nonemergency health care was transitioned to VHC. We assumed 2019Q1 to 2019Q4 as the pre-VHC period and 2020Q2 to 2021Q1 as the post-VHC period. VHC = virtual health care.
There was a significant decrease in new neuropituitary referrals from the pre– to post–COVID-19 period (54 vs 33, respectively; P = .03). Fewer referrals were received among all categories of neuropituitary tumors; furthermore, no new cases of acromegaly were diagnosed in the post-VHC period, despite a steady prior annual incidence in the preceding 2 years. There was 1 Cushing syndrome diagnosis in the pre-VHC period but none in the post-VHC period.
Although the observed 39% decrease in overall neuropituitary diagnoses is significant, the complete absence of acromegaly diagnosis is alarming, especially where significant delays in the diagnosis of acromegaly have already been reported; an Italian endocrinology unit observed a 50% decrease in new acromegaly diagnoses and a 33% reduction in on-site evaluations of patients with acromegaly between 2019 and 2020.1
This observed decreasing trend in neuropituitary diagnoses is probably multifactorial. Many patients avoided or delayed access to medical care during the pandemic owing to widespread lockdown and fear of infection.2 Access to laboratory and imaging services was significantly limited during the first half of 2020 in our province, which may also have contributed to this trend. However, despite full restoration of services during the past 12 months, this trend has remained unchanged. The absence of acromegaly diagnosis may be due to the concealment of facial features by face masks during face-to-face medical appointments or nonvideo telephone consultations.
Although telemedicine and VHC offer a convenient solution to breaking the barriers of time and distance for remote patients and offering social distancing during the pandemic, missed or delayed diagnoses will likely occur when relying largely on patients’ descriptions of symptoms and lack of physical examination. If telephone-based VHC becomes a significant component of patient care, we should anticipate further delays or missed diagnoses of neuropituitary disorders, which may lead to an increased risk of comorbidities due to uncontrolled hormonal dysfunction in patients.
Although there has been an uptake of VHC by the private sector in Canada, its use in the publicly funded system varies across different health jurisdictions.3 The percentage of VHC in the province of Ontario, Canada, increased from 1.3% in 2019 to 29.2% in 2020; however, video-assisted VHC accounted for only 8.8% of all virtual visits.4 Further studies are required to assess our observed trend in centers in which video consultation platforms are available to allow visualization of physical changes. Our data suggest that the role of VHC must be critically assessed as it may not be an effective alternative to face-to-face care for neuropituitary disorders.
Disclosure
The authors have no multiplicity of interest to disclose.
References
- 1.Gatto F., Khorrami K., Nista F., Corica G., Ferone D. Acromegaly management in a tertiary referral center after 1 year of the coronavirus 2019 pandemic: a double challenge. Endocr Pract. 2021;27(8):856–857. doi: 10.1016/j.eprac.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubin R. COVID-19’s crushing effects on medical practices, some of which might not survive. JAMA. 2020;324(4):321–323. doi: 10.1001/jama.2020.11254. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Medical Association Virtual Care in Canada: Discussion Paper. https://www.cma.ca/sites/default/files/pdf/News/Virtual_Care_discussionpaper_v2EN.pdf Accessed September 18, 2021.
- 4.Bhatia R.S., Chu C., Pang A., Tadrous M., Stamenova V., Cram P. Virtual care use before and during the COVID-19 pandemic: a repeated cross-sectional study. CMAJ Open. 2021;9(1):E107–E114. doi: 10.9778/cmajo.20200311. [DOI] [PMC free article] [PubMed] [Google Scholar]