Abstract
Objectives
Since 2020, COVID-19 has infected tens of millions and caused hundreds of thousands of fatalities in the United States. Infection waves lead to increased emergency department utilization and critical care admission for patients with respiratory distress. Although many individuals develop symptoms necessitating a ventilator, some patients with COVID-19 can remain at home to mitigate hospital overcrowding. Remote pulse-oximetry (pulse-ox) monitoring of moderately ill patients with COVID-19 can be used to monitor symptom escalation and trigger hospital visits, as needed.
Methods
We analyzed the cost-utility of remote pulse-ox monitoring using a Markov model with a 3-week time horizon and daily cycles from a US health sector perspective. Costs (US dollar 2020) and outcomes were derived from the University Hospitals’ real-world evidence and published literature. Costs and quality-adjusted life-years (QALYs) were used to determine the incremental cost-effectiveness ratio at a cost-effectiveness threshold of $100 000 per QALY. We assessed model uncertainty using univariate and probabilistic sensitivity analyses.
Results
Model results demonstrated that remote monitoring dominates current standard care, by reducing costs ($11 472 saved) and improving outcomes (0.013 QALYs gained). There were 87% fewer hospitalizations and 77% fewer deaths among patients with access to remote pulse-ox monitoring. The incremental cost-effectiveness ratio was not sensitive to uncertainty ranges in the model.
Conclusions
Patient with COVID-19 remote pulse-ox monitoring increases the specificity of those requiring follow-up care for escalating symptoms. We recommend remote monitoring adoption across health systems to economically manage COVID-19 volume surges, maintain patients’ comfort, reduce community infection spread, and carefully monitor needs of multiple individuals from one location by trained experts.
Keywords: COVID-19, critical care, emergency department, infectious disease, intensive care unit, pulse oximetry, telemedicine
Introduction
Since its discovery in December 2019, the severe acute respiratory syndrome (SARS)-coronavirus-2 has spread at a rapid rate to more than 190 countries. According to the World Health Organization (covid19.who.int, Geneva, Switzerland), COVID-19 has infected more than 180 million individuals and resulted in more than 4 million deaths worldwide as of July 16, 2021. The pandemic has had a severe impact on the United States in particular, which has led to >33 million confirmed cases and 603 000 deaths in the same time span.1 This unprecedented proliferation of positive cases in the United States has posed a significant burden on healthcare systems nationwide, depleting critical care resources and intensive care unit (ICU) beds that are necessary for in-hospital treatment of critically ill patients with COVID-19. For instance, California experienced an alarming exhaustion of critical care beds in January, 2021, decreasing the state’s ICU capacity to 2.1% and raising the statewide positivity rate to 11.3%.2 As of January 31, 2021, more than half of states reported that 70% to 100% of both inpatient and ICU beds are in use, with 2 states between 90% and 100% occupancy.3
Strategic management of ICU capacity and hospital resources is of utmost importance in mitigating future case surges, which are likely to continue to occur in waves in various communities depending on rates of immunization and COVID-19 variants. The resources necessary for treatment include mechanical ventilators for patients presenting acute respiratory distress syndrome (ARDS), personal protective equipment, critical care nurses and respiratory therapists, and ICU beds and adequate spacing and private rooms for symptomatic patients.4 Many of these resources are, at various times throughout the pandemic, in scarce supply. According to the Society of Critical Care Medicine, ICU capacity in the United States is 97 000 beds, or approximately 10% of all staffed hospital beds in the country,5 yet these ICU beds may themselves be understaffed—a 2015 American Hospital Association survey indicated that only 52% of hospital ICUs employed any intensivists.6 Considering these shortages of ICU capacity, resources, and staffing for critically ill patients, the United States could reach peak ICU occupancy levels in 2021.
Alternative healthcare delivery methods to manage capacity issues in ICUs would benefit all critically ill patients during this pandemic.7 Several studies indicate that most patients with COVID-19 who present with symptoms in the emergency department (ED) do not need immediate ICU care or mechanical ventilation. A February 2020 study from China reported that only 5% of symptomatic cases required critical care because of ARDS or other serious complication; most of these patients had preexisting chronic conditions, including cardiovascular disease.8 An April 2020 study on a cohort of hospitalized patients with COVID-19 from New York City reported that 14.2% of all cases required ICU treatment, whereas 12.2% of cases necessitated mechanical ventilation, with the median age for ICU admission at 68 years.9 These numbers suggest that most patients can be safely monitored for escalation from home without occupying hospital beds or depleting scarce medical resources.
Remote pulse oximetry (pulse-ox) telemonitoring is a convenient alternative to hospital admission. Remote pulse-ox has been tested to monitor oxygen saturation in patients with acute and chronic conditions, ranging from chronic-obstructive pulmonary disorder to congestive heart failure.10, 11, 12 During the COVID-19 pandemic, NorthShore University Health System evaluated the efficacy of at-home pulse-ox for COVID-19 positive patients, which relied on self-monitoring to determine whether returning to the hospital would be necessary based on oxygen saturation below 92%.13 The University Hospitals’ health system in Ohio has taken pulse-ox monitoring a step further by creating a clinical command center to monitor patients sent home from the ED with a commonly available, Bluetooth-enabled wearable pulse-ox monitor where data could be automatically transferred from the wearable device to the command center.14 Patients with worsening symptoms are then transported or called back into the hospital when levels worsen. The University Hospitals reported reductions in ED utilization, ICU admissions, and therefore reduced exposure risk for healthcare workers.15
International healthcare also made successful strides to manage COVID-19 volume surges using remote monitoring. In Saudi Arabia, patients with COVID-19 were sent home from the ED with remote monitoring devices that linked clinicians to continuous biometric and symptomatic data; patients with escalated criteria were connected to a physician for a phone or video consult.16 In United Kingdom, remote pulse-ox was also used to follow-up with ED patients discharged to home within 36 hours if their symptoms persisted or worsened.17 In The Netherlands, hospitalized patients with COVID-19 were eligible for early discharge with telemonitoring devices, which reduced length of stay and improved management of volume surges.18
To date, the value added by pulse-ox tele monitoring has largely focused on chronic health conditions.19 , 20 Given the extensive costs of treating patients with acute COVID-19 in ICUs, we sought to assess the cost-effectiveness of at-home monitoring with pulse-ox using data collected from the University Hospitals Cleveland Medical Center in Cleveland, Ohio.
Methods
Study Design
We developed a Markov model to estimate the cost-effectiveness of home-monitoring with pulse-ox among moderate to severely ill patients with COVID-19 presenting in the ED. Much of the cost and outcomes data for this model came from real-world evidence from the University Hospitals Cleveland Medical Center. We modeled patient care pathways from the ED back to home, with possible secondary ED visits and ICU admissions in 1-day cycles for a 3-week time horizon. The time horizon was chosen to reflect the average course of illness observed among patients in real-world data.21 The model exhibited a US healthcare sector perspective and did not incorporate a discount rate given the short time horizon. The results were interpreted based on the incremental cost-effectiveness ratio (ICER) and net monetary benefit (NMB) at a cost-effectiveness threshold of $100 000 per quality-adjusted life-year (QALY), in accordance with methodological recommendations from the US Panel on Cost-effectiveness in Health and Medicine.22
Model Structure
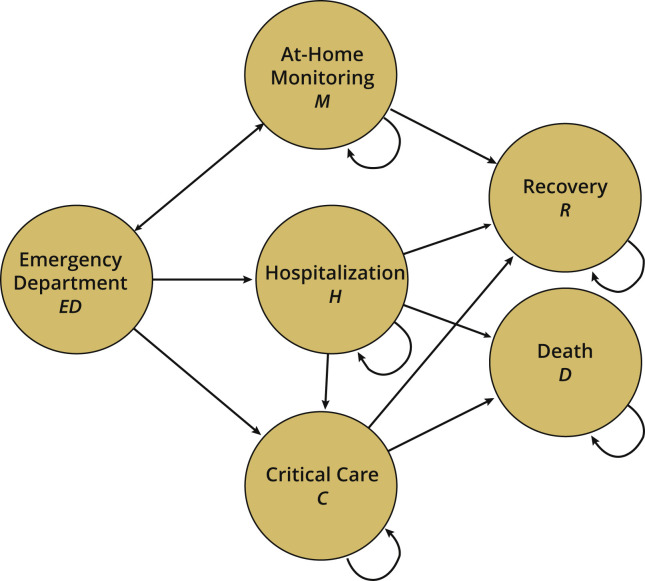
The Markov model consisted of 6 health states: ED visit, at-home monitoring with or without pulse-ox, COVID-19 recovery, hospitalization, ICU admission, and death (Fig. 1 ). Patient simulations began with presentation in the ED with respiratory symptoms because of COVID-19. From the ED, patients in the intervention group were hospitalized with concerning symptoms or were transitioned to at-home telemonitoring. Some individuals with home-monitoring returned to the ED within their first 5 days if they met a clinical threshold for follow-up. Those with severe symptoms were admitted to general hospital care or ICU care or allowed to return home. Patients in the control group did not have the option of at-home monitoring and were instead admitted to the hospital or ICU after their presentation to the ED because of a lack of sensitivity. From either comparator, patients moved through the course of treatment until they recovered or died.
Figure 1.
A Markov model simulating treatment of moderate-to-severe patients with COVID-19 using telehealth monitoring with pulse oximetry compared with hospitalization.
C indicates critical care; D, death; ED, emergency department; H, hospitalization; M, at-home monitoring; R, recovery.
With at-home monitoring, patients remained at home with a pulse-ox transmitting vital signs to a hospital command center for 5 days. With hospitalization, patients were assumed to be under observation at the hospital for 7 days based on the upper-bound length of stay reported for US patients with COVID-19 who were discharged from the hospital to home or self-care.23 Within the 7 days of hospitalization, the patient could transition to critical care if symptoms escalated. With critical care, patients were assumed to be on ventilators in the ICU for 10 days. From hospitalization and critical care, patients transitioned to recovery or death. Patient mortality only occurred in the hospital or critical care health states because of complications from pneumonia or septic shock.24
Model Parameters
Probabilities
Data on rates of transition between the ED and home and hospital care and ICU admissions were collected from administrative data at the University Hospitals Cleveland before and after rollout of the pulse-ox intervention (Table 1 14 , 25, 26, 27, 28, 29, 30, 31, 32, 33). These data are validated by a clinical command center that employs at least 1 physician (MD) or registered nurse (RN) 24 hours per day, 7 days per week. Data collection from this pilot has been ongoing since its inception in March 2020.
Table 1.
Model parameters.
| Parameter | Range for sensitivity analysis |
||||
|---|---|---|---|---|---|
| Deterministic value | Lower bound | Upper bound | Distribution | Source | |
| Transition probabilities | |||||
| With M | |||||
| ED to M (first visit) | 0.930 | 0.740 | 1.000 | Beta | 14 |
| ED to M (second visit) | 0.170 | 0.130 | 0.200 | Beta | 14 |
| ED to H (second visit) | 0.600 | 0.480 | 0.710 | Beta | 14 |
| ED to C (first visit) | 0.070 | 0.060 | 0.080 | Beta | 14 |
| ED to C (second visit) | 0.240 | 0.190 | 0.290 | Beta | 14 |
| M to ED | 0.050 | 0.040 | 0.060 | Beta | 14 |
| M to R | 0.950 | 0.760 | 1.000 | Beta | 14 |
| H to C | 0.115 | 0.090 | 0.140 | Beta | 25 |
| H to R | 0.974 | 0.780 | 1.000 | Beta | 25 |
| H to D | 0.026 | 0.020 | 0.030 | Beta | 25 |
| C to R | 0.974 | 0.780 | 1.000 | Beta | 25 |
| C to D | 0.026 | 0.020 | 0.030 | Beta | 25 |
| R to R | 1.000 | 0.800 | 1.000 | Beta | — |
| D to D | 1.000 | 0.800 | 1.000 | Beta | — |
| Without M | |||||
| ED to C | 0.070 | 0.050 | 0.084 | Beta | 14 |
| ED to H | 0.930 | 0.740 | 1.000 | Beta | 14 |
| H to C | 0.115 | 0.092 | 0.138 | Beta | 25 |
| H to R | 0.974 | 0.779 | 1.000 | Beta | 25 |
| H to D | 0.026 | 0.021 | 0.031 | Beta | 25 |
| C to R | 0.974 | 0.7792 | 1.000 | Beta | 25 |
| C to D | 0.026 | 0.021 | 0.031 | Beta | 25 |
| R to R | 1.000 | 0.800 | 1.000 | Beta | — |
| D to D | 1.000 | 0.800 | 1.000 | Beta | — |
| Costs per episode (USD 2020) | |||||
| ED Costs | $26 095 | $17 913 | $40 801 | Log-normal | 26, 27 |
| M Costs | $114 | $91 | $137 | Log-normal | 14, 28, 29, 30, 31, 32 |
| H Costs | $43 917 | $35 134 | $52 701 | Log-normal | 14 |
| C Costs | $21 040 | $16 832 | $25 249 | Log-normal | 14 |
| R Costs | $0.00 | $0.00 | $0.00 | Log-normal | — |
| D Costs | $0.00 | $0.00 | $0.00 | Log-normal | — |
| Utilities (QALYs) | |||||
| Utility of ED | 0.50 | 0.40 | 0.60 | Beta | 30 |
| Utility of M | 0.50 | 0.40 | 0.60 | Beta | 30 |
| Utility of H | 0.25 | 0.20 | 0.30 | Beta | 30 |
| Utility C | 0.05 | 0.04 | 0.06 | Beta | 30 |
| Utility R | 0.76 | 0.61 | 0.91 | Beta | 33 |
| Utility of D | 0.00 | 0.00 | 0.00 | Beta | — |
C indicates critical care; D, death; ED, emergency department; H, hospitalization; M, at-home monitoring; QALY, quality-adjusted life-year; R, recovery; USD, US dollar.
The remaining transition probabilities, including transition probabilities to and from critical care, were obtained from the US Centers for Disease Control and Prevention.34 According to these US Centers for Disease Control and Prevention data, we assumed equal probabilities of transitioning from hospitalization to critical care (2.6%) or from hospitalization to death (11.5%) in both the standard care and telehealth comparators, because the University Hospitals pilot did not observe differences that would have implied varying these values between comparators.
Costs
Microcosting was used to aggregate the University Hospitals’ COVID-19–related costs and information from a targeted literature review to supply data for model health states. The University Hospitals administrative data from Cleveland and Ahuja facilities provided average cost per patient with COVID-19 episode in general hospital care based on average medical-surgical costs and ICU costs. As costs per episode, the model applied a fixed cost of care while a patient remained in a particular health state (eg, hospitalization, critical care). We assumed that 50% of patients in the hospitalization state and the critical care state required an invasive procedure (eg, tracheostomy for mechanical ventilation, revascularization for acute limb ischemia).35 , 36
Given that the cost-effectiveness was modeled from the healthcare sector perspective, societal costs, such as patient time, were not included. ED out-of-pocket costs for patients with COVID-19 observed among 12 major cities were averaged and assumed to be 11% of the total per-patient cost in the ED from a hospital perspective.26 , 27
The costs of at-home monitoring consisted of the pulse-ox device, the amount of clinician-time required per case at the command center (ie, 1 full-time RN per 40 patients with COVID-19 per day), and hourly wages for RNs at general medical or surgical hospitals ($38.20 2019 US dollar) converted to 2020 US dollar using the medical consumer price index.28 , 29 We assumed 2 factors regarding these costs: (1) that costs for operating the command center should be explicit costs rather than sunk costs, because it is unlikely for health systems to have an existing setup to avoid an upfront investment in this infrastructure; and (2) that there were no costs associated with death and recovery states.
Health state utilities
As of this study, there were no published QALY estimates for COVID-19. Therefore, QALY values for health states involving infection with COVID-19 (ie, ED, home-monitoring, hospitalization, and critical care) were assumed to be equal to the lower bound QALY estimates for SARS as estimated from a Canadian study using the Health Utilities Index-3.30 These values were selected based on their inclusion of ARDS symptoms and social isolation if infected.
Sensitivity Analyses
We conducted univariate 1-way and probabilistic sensitivity analyses to evaluate the model’s uncertainty with respect to parameter values. In the 1-way sensitivity analyses, we varied parameters to their upper and lower bound values, which were 95% confidence intervals reported in literature or ±20% of their mean if confidence intervals were not reported. We estimated the sensitivity of the ICER and NMB to these values at a cost-effectiveness threshold of $100 000 per QALY. We conducted a probabilistic sensitivity analysis with 1000 Monte Carlo simulations, which are independent simulations from the study observations, tallying more than 800 standard care patients and over 100 telehealth patients who were readmitted.31 Utility and transition probabilities were fit to beta-distributions and costs were fit to log-normal distributions.
Results
Coronavirus Outcomes
Health outcomes improved and utilization decreased with the implementation of at-home pulse-ox telemonitoring during the 3-week time horizon. The mortality rate with at-home monitoring was approximately 6 per 1000 patients with COVID-19, whereas the mortality rate was 26 per 1000 without at-home monitoring, which is consistent with most outcomes nationally.32 Within the time horizon, 131 patients with at-home monitoring were admitted to the ICU, whereas 177 patients were admitted to the ICU without at-home monitoring arm. Finally, hospitalizations between the 2 arms varied widely, with 104 patients hospitalized after at-home monitoring, and 823 patients hospitalized in the absence of at-home monitoring. Overall, these data reflect lower specificity for tertiary care utilization in the absence of pulse-ox data.
Base Case Results
With substantially reduced costs and improved effectiveness, at-home monitoring dominated standard care for severe patients with COVID-19 (Table 2 ). At-home monitoring presented a cost-savings of approximately $11 472 per patient, at a gain of 0.013 QALYs per patient on average. The incremental NMB per patient at a cost-effectiveness threshold of $100 000 per QALY was $12 809 (Table 2).
Table 2.
Expected base case results per patient.
| Alternatives | Clinical findings (per 1000) |
Economic findings |
|||||
|---|---|---|---|---|---|---|---|
| Hospital admissions | Deaths | Cost, $ | Δ cost, $ | QALY | ΔQALY | ICER, $ per QALY | |
| Standard care: no remote monitoring | 823 | 26 | 51 183 | 0.019 | Dominated | ||
| Telehealth: with pulse oximetry monitoring at home | 104 | 6 | 39 711 | −11 471 | 0.032 | 0.013 | |
Δ indicates Difference in Cost or QALY; ICER, incremental-cost-effectiveness ratio; QALY, quality-adjusted life-year.
Sensitivity Analyses
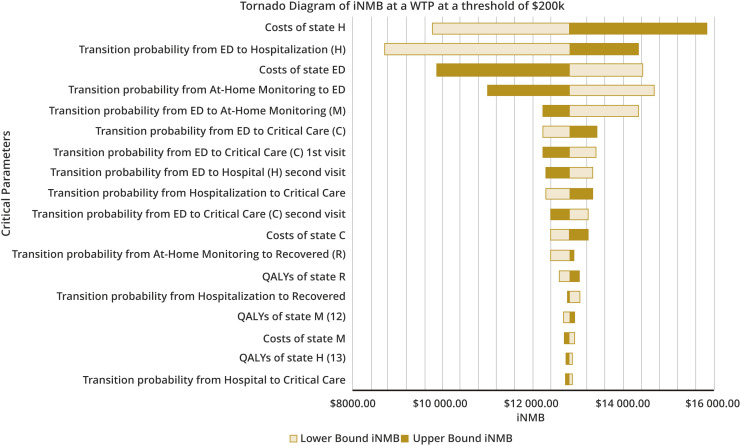
Univariate sensitivity analyses yielded no change in model results. The costs of hospitalization, the transition probability from the ED to a hospitalization, the transition probability from ED to at-home monitoring, and the transition probability from at-home monitoring back to the ED were associated with the greatest variability in reported NMB of at-home monitoring for the observation of severe patients with coronavirus (Fig. 2 ).
Figure 2.
Tornado diagram of univariate sensitivity analysis. Each parameter was varied by reported 95% confidence interval or ±20% if a reported confidence interval was not reported. Results are presented in terms of iNMB range. Black bars represent upper-bound estimates of the parameter, and white bars represent lower bound estimates.
C indicates critical care; ED, emergency department; H, hospitalization; iNMB, incremental net monetary benefit; K, thousand; M, at-home monitoring; QALY, quality-adjusted life-year; R, recovery; WTP, willingness-to-pay.
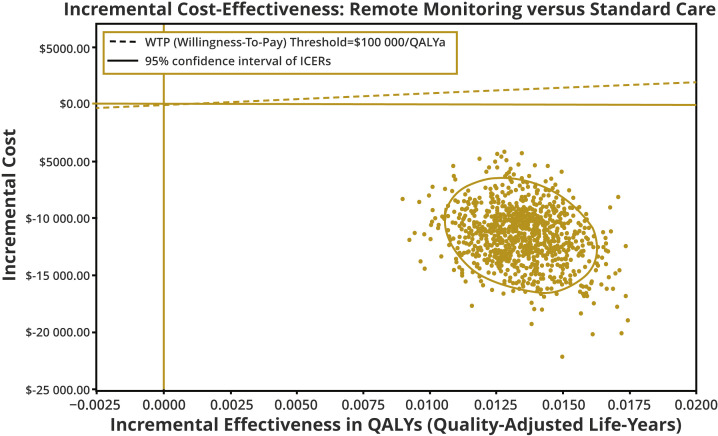
Multivariate probabilistic sensitivity analysis with 1000 Monte Carlo simulations at a cost-effectiveness threshold of $100 000 per QALY indicated that our findings were robust to variations in current model parameter uncertainty. These simulations were distinct from the >800 observed patients at the University Hospitals with or without telehealth. At-home telemonitoring maintained its dominance over standard care in 100% of simulations (Fig. 3 ).
Figure 3.
Probabilistic sensitivity analysis. ICER scatterplot of 1000 Monte Carlo simulations.
ICER indicates incremental cost-effectiveness ratio; QALY, quality-adjusted life-year; WTP, willingness-to-pay.
Discussion
At-home telemonitoring with pulse-ox devices presents a cost-effective solution to handle surges of patients presenting with COVID-19 symptoms in the ED by monitoring patients from the safety of their home rather than using costly inpatient hospital services. Although these patients have rightful concerns about their symptoms for COVID-19, their status may not necessitate immediate use of limited health system resources during surges such as hospital beds of mechanical ventilators. Monitoring them from the comfort and safety of their home for signs of escalating symptoms for ARDS associated with oxygen depletion presents an option for population health management that could save upward of $11 000 per-patient costs and stabilize clinical benefits compared with other alternatives. Given the 2020 rate of COVID-19 incidence, this represents a budget impact of $11 in savings per person per month in the United States. Thus, these findings regarding the use of remote pulse-ox monitoring could benefit not only patients with COVID-19 but other patients presenting with ARDS symptoms such as influenza and future outbreaks of coronavirus variants (eg, SARS-coronavirus-2, Middle East respiratory syndrome-coronavirus-2).
As the United States continues to vaccinate its population to address COVID-19 using preventive means, the possibility of future surges has not dissipated. COVID-19 variants that are not responsive to the vaccines and other future viruses that cause ARDS present a clear and present danger to health systems that have been continually overwhelmed since early 2020. Having a plan in place that includes leveraging new technology such as pulse-ox monitoring to manage population health and limited health system resources ensures that a bed and mechanical ventilator will be available for those who need it most.
Decision makers who weigh the value of this telehealth model should seriously consider models for reimbursing health systems who invest in pulse-ox monitoring at-home. Such a system not only manages volume surges but limits charges passed onto payers for high-cost hospitalizations. The upfront cost to establish this critical infrastructure for population health management may be nontrivial given that thousands of pulse-ox monitors, overhead space, and full-time equivalents of clinical staff are needed to maintain the system. Payers should work with health systems in a reimbursement structure that rewards reductions in health system utilization with lower-cost technology for continuous monitoring.
Pulse-ox technology, in particular, has never been more accessible to individual patients. This technology, which was once limited to hospital beds, is now marketed directly to consumers. By leveraging a technology that is easily accessible to consumers, there are few barriers for any community health system to initiate a plan for COVID-19 management. The fact that telehealth systems can facilitate remote monitoring of pulse-ox technology adds to a growing field of telehealth that has transformed the delivery of healthcare during the COVID-19 pandemic. Although hope springs eternal that the COVID-19 pandemic soon comes to an end, the opportunity for remote pulse-ox monitoring of other patient cohorts with similar issues, such as those with congestive heart failure, chronic-obstructive pulmonary disorder, or chronic asthma, may gain similar clinical benefits of this system.
This study has a number of limitations. First, the results of the study are based on early-trial evidence in the Cleveland community. Rollout of remote monitoring systems for COVID-19 would benefit in terms of generalizability to other types of communities, including rural medicine and dense urban areas and international communities. Second, Cleveland faced concerning surges for COVID-19, but perhaps not the degree of surge experienced in locations such as New York City. Understanding the limitations of this mechanism in health systems exceeding a critical mass is important. Third, some of the additional parameters such as QALYs are extrapolated from other patient cohorts with ARDS symptoms, such as SARS; COVID-19–specific QALYs would be preferred. Fourth, the model lacks data to provide insights on value for different subgroups, particularly relating to age, sex, race, or ethnicity. It would be helpful to better understand the value of this system to such subgroups, although the population tested in Cleveland reflected a diverse population within a small-sized cohort. Fifth, although we assumed equal probabilities from hospitalization to critical care and to death between comparators, it is likely that critical care admission and mortality rates are greater in the standard care arm. Given that we did not have exact data to support this hypothesis, we maintained equal rates to support a conservative estimate of the ICER for this study. Sixth, the time horizon of this model is relatively short in comparison with recommendations from the US Panel on Cost-effectiveness in Health and Medicine, which recommends horizons to examine short- and long-term value. Given the acute nature of COVID-19, the value of this technology was highlighted on a short-term horizon to illustrate to medical directors that costs could be recouped relatively quickly.
Sixth, the generalizability of this study is further limited to communities that have the proper technological infrastructure to rollout remote pulse-ox monitoring devices. Communities that wish to implement this cost-effective solution need several high-cost resources: (1) volumes of disposable wearable devices with Bluetooth-enabled pulse-ox monitoring that can be linked to a command center, (2) a command center that can track multiple patients’ statuses at once, (3) clinical experts that can monitor patients from a command center, and (4) an internet network that spans from a community health system to patients’ homes. Without these elements, implementing this proposed intervention may not be feasible and remains challenging for global health settings.
Conclusions
The remote pulse-ox monitoring system trialed in Cleveland presents a cost-effective alternative to handling COVID-19 surges. Health systems with a limited number of open hospital beds and mechanical ventilators caused by the COVID-19 pandemic can use pulse-ox monitors to manage volumes of patients with COVID-19 symptoms who are not critically ill from the comfort and safety of their homes. Doing so maintains their connectivity to clinical experts who can determine whether medical follow-up is necessary and minimizes exposure of patients with COVID-19 to other noninfectious patients in hospitals. We recommend that all health systems explore a COVID-19 population management system that includes the use of remote pulse-ox monitors for those patients who could be susceptible to ARDS symptoms.
Article and Author Information
Author Contributions: Concept and design: Padula, Pronovost
Acquisition of data: Miano, Hughes, Grosso, Pronovost
Analysis and interpretation of data: Padula, Kelley, Crawford, Choy, Pronovost
Drafting of manuscript: Padula, Kelley, Crawford, Choy
Critical Revision of the paper for important intellectual content: Padula, Miano, Kelley, Crawford, Choy, Hughes, Grosso, Pronovost
Statistical Analysis: Padula, Miano, Kelley, Crawford, Choy, Hughes, Grosso
Provision of study materials or patients: Miano, Hughes, Grosso
ObtainingFunding: Padula
Administrative andTechnical Support: Kelley, Crawford, Choy
Supervision: Padula, Pronovost
Conflict of Interest Disclosure: Dr Padula reported receiving grants from the National Institutes of Health paid to the University of Southern California during the conduct of the study and consulting fees from Monument Analytics and Masimo Corp outside of the submitted work. Dr Padula is an Editor for Value in Health and had no role in the peer-review process of this article. No other disclosures were reported.
Funding Support: Dr Padula is supported by an unrestricted grant from the US National Institutes of Health (NIH/OER KL2 TR001854).
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.COVID-19 map Baltimore: Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/
- 2.Tracking COVID-19 in CA. California State Government. https://covid19.ca.gov/
- 3.HHS protect public data hub: state representative estimates for hospital utilization. US Department of Health and Human Services. https://protect-public.hhs.gov/
- 4.Murthy S., Gomersall C.D., Fowler R.A. Care for critically ill patients with COVID-19. JAMA. 2020;323(15):1499–1500. doi: 10.1001/jama.2020.3633. [DOI] [PubMed] [Google Scholar]
- 5.2020 AHA hospital statistics. American Hospital Association. https://www.aha.org/system/files/media/file/2020/01/2020-aha-hospital-fast-facts-new-Jan-2020.pdf
- 6.Halpern N.A., Tan K.S., DeWitt M., Pastores S.M. Intensivists in U.S. acute care hospitals. Crit Care Med. 2019;47(4):517–525. doi: 10.1097/CCM.0000000000003615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Llanes J.M., Castro Delgado R., Pederson M.G., Meneghini M., Arcos González P. Surging critical care capacity for COVID-19: key now and in the future. Prog Disaster Sci. 2020;8 doi: 10.1016/j.pdisas.2020.100136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 9.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area [published correction appears in JAMA. 2020;323(20):2098] JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jubran A. Pulse oximetry. Crit Care. 2015;19(1):272. doi: 10.1186/s13054-015-0984-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Field M.J., Grigsby J. Telemedicine and remote patient monitoring. JAMA. 2002;288(4):423–425. doi: 10.1001/jama.288.4.423. [DOI] [PubMed] [Google Scholar]
- 12.Tang J., Mandrusiak A., Russell T. The feasibility and validity of a remote pulse oximetry system for pulmonary rehabilitation: a pilot study. Int J Telemed Appl. 2012;2012 doi: 10.1155/2012/798791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah S., Majmudar K., Stein A., et al. Novel use of home pulse oximetry monitoring in COVID-19 patients discharged from the emergency department identifies need for hospitalization. Acad Emerg Med. 2020;27(8):681–692. doi: 10.1111/acem.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pronovost PJ. To make progress against Covid-19, processes must serve people, not a ‘labyrinth of bureacratic rules.’ STAT News, June 30, 2020. https://www.statnews.com/2020/06/30/to-make-progress-against-covid-19-processes-must-serve-people-not-a-labyrinth-of-bureaucratic-rules/. Accessed on May 2, 2021
- 15.Motta L.P., Silva P.P.F.D., Borguezan B.M., et al. An emergency system for monitoring pulse oximetry, peak expiratory flow and body temperature of patients with COVID-19 at home: development and preliminary application. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0247635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aalam A.A., Hood C., Donelan C., Rutenberg A., Kane E.M., Sikka N. Remote patient monitoring for ED discharges in the COVID-19 pandemic. Emerg Med J. 2021;38(3):229–231. doi: 10.1136/emermed-2020-210022. [DOI] [PubMed] [Google Scholar]
- 17.Bell L.C., Norris-Grey C., Luintel A., et al. Implementation and evaluation of a COVID-19 rapid follow-up service for patients discharged from the emergency department. Clin Med (Lond) 2021;21(1):e57–e62. doi: 10.7861/clinmed.2020-0816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grutters L.A., Majoor K.I., Mattern E.S.K., Hardeman J.A., van Swol C.F.P., Vorselaars A.D.M. Home telemonitoring makes early hospital discharge of COVID-19 patients possible. J Am Med Inform Assoc. 2020;27(11):1825–1827. doi: 10.1093/jamia/ocaa168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cowie M.R., Simon M., Klein L., Thokala P. The cost-effectiveness of real-time pulmonary artery pressure monitoring in heart failure patients: a European perspective. Eur J Heart Fail. 2017;19(5):661–669. doi: 10.1002/ejhf.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grustam A.S., Severens J.L., De Massari D., Buyukkaramikli N., Koymans R., Vrijhoef H.J.M. Cost-effectiveness analysis in telehealth: A comparison between home telemonitoring, nurse telephone support, and usual care in chronic heart failure management. Value Health. 2018;21(7):772–782. doi: 10.1016/j.jval.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 21.Liu X., Zhou H., Zhou Y., et al. Risk factors associated with disease severity and length of hospital stay in COVID-19 patients. J Infect. 2020;81(1):e95–e97. doi: 10.1016/j.jinf.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neumann P.J., Cohen J.T., Weinstein M.C. Updating cost-effectiveness -- the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–797. doi: 10.1056/NEJMp1405158. [DOI] [PubMed] [Google Scholar]
- 23.Lavery A.M., Preston L.E., Ko J.Y., et al. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission - United States, March-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1695–1699. doi: 10.15585/mmwr.mm6945e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cascella M., Rajnik M., Cuomo A., et al. StatPearls. StatPearls Publishing Pearls Publishing LLC; Treasure Island, FL: 2020. Features, evaluation and treatment coronavirus (COVID 19) [PubMed] [Google Scholar]
- 25.COVID-19. Centers for Disease Control and Prevention (CDC) www.cdc.gov/coronavirus/2019-ncov
- 26.Health system tracker: out-of-pocket spending. The Peterson Center on Healthcare, Kaiser Family Foundation (KFF) https://www.healthsystemtracker.org/indicator/access-affordability/out-of-pocket-spending/
- 27.The Costs of COVID-19: how much does it really cost to seek care? Castlight health. https://www.castlighthealth.com/wp-content/uploads/2020/03/Costs-of-COVID-19.pdf
- 28.Occupational employment and wages. US Bureau of Labor Statistics (BLS) https://www.bls.gov/oes/current/oes291141.htm
- 29.Consumer price index for all urban consumers: medical care in U.S. City average. Federal Reserve Bank of St. Louis. https://fred.stlouisfed.org/series/CPIMEDSL
- 30.Khan K., Muennig P., Gardam M., Zivin J.G. Managing febrile respiratory illnesses during a hypothetical SARS outbreak. Emerg Infect Dis. 2005;11(2):191–200. doi: 10.3201/eid1102.040524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Briggs A.H. Handling uncertainty in cost-effectiveness models. Pharmacoeconomics. 2000;17(5):479–500. doi: 10.2165/00019053-200017050-00006. [DOI] [PubMed] [Google Scholar]
- 32.Baud D., Qi X., Nielsen-Saines K., Musso D., Pomar L., Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. 2020;20(7):773. doi: 10.1016/S1473-3099(20)30195-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sullivan P.W., Ghushchyan V. Preference-Based EQ-5D index scores for chronic conditions in the United States. Med Decis Making. 2006;26(4):410–420. doi: 10.1177/0272989X06290495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.CDC COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chao T.N., Harbison S.P., Braslow B.M., et al. Outcomes after tracheostomy in COVID-19 patients. Ann Surg. 2020;272(3):e181–e186. doi: 10.1097/SLA.0000000000004166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bellosta R., Luzzani L., Natalini G., et al. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg. 2020;72(6):1864–1872. doi: 10.1016/j.jvs.2020.04.483. [DOI] [PMC free article] [PubMed] [Google Scholar]