Abstract
Objectives
: We examined the association between social frailty and depressive symptoms among community-dwelling older adults during the coronavirus disease 2019 pandemic. Additionally, we investigated whether home exercise habits moderated the impact of social frailty on depressive symptoms.
Methods
: This cross-sectional study included 1,103 community-dwelling older adults (54.0% female, mean age [standard deviation] = 81.1 [5.0] years) from a semi-urban area of Japan who completed a mailed questionnaire survey in October 2020. Social frailty status was categorized as non-social frailty, pre-social frailty, and social frailty, which was assessed by financial difficulties, living alone, lack of social activity, and contact with neighbors. Depressive symptoms were defined as a Kessler 6 score ≥5. We performed a multivariable logistic regression analysis to examine the association between social frailty and depressive symptoms, and also conducted stratified analysis of home exercise habits during the pandemic.
Results
: A total of 309 (28.0%) participants had depressive symptoms. Compared with non-social frailty, social frailty was associated with depressive symptoms (odds ratio [OR] = 1.80, 95% confidence interval [95%CI] = 1.16–2.79, p = 0.009). A similar relationship was observed in those who did not exercise at home (OR = 2.10, 95%CI = 1.14–3.84, p =0.017). However, no such relationship was observed in those who did exercise at home (OR = 1.50, 95%CI = 0.79–2.85, p =0.213).
Conclusions
: Social frailty was associated with a risk of depressive symptoms during the pandemic. In addition, our findings suggested that home exercise may buffer the association between social frailty and depressive symptoms.
Keywords: Social frailty, Japan, Older adults, COVID-19, Depressive symptoms, Home exercise
1. Introduction
Many people have been affected by the coronavirus disease 2019 (COVID-19) pandemic, both directly and indirectly. The World Health Organization declared a COVID-19 pandemic in March 2020 (World Health Organization, 2020). Owing to the insufficient establishment of effective pharmacological interventions, COVID-19 management depends on public health measures to mitigate its spread and flatten the pandemic curve. These measures include bans on public gatherings, stay-at-home policies, and physical distancing strategies(Hartley & Perencevich, 2020). In Japan, a state of emergency was issued by the government on April 7, 2020, calling for restrictions on interactions between citizens and refraining from social interactions (lifted on May 31, 2020) (Karako, Song, Chen, Tang, & Kokudo, 2021; Looi, 2020). Some prefectures declared a local prefectural-level state of emergency in late July 2020, corresponding to the second wave. This involved self-restraint when dining at restaurants at night (lifted in early September 2020) (Gifu Prefectural Office, 2020; Karako et al., 2021).
Although these strategies have helped to stop the spread of infectious diseases (Islam et al., 2020), there are concerns that they may have negative effects. For example, restricting social activities, such as going out and interacting with others, leads to a decrease in physical activity (PA) (Caputo & Reichert, 2020). Previous studies have shown that similar preventive measures applied during the COVID-19 pandemic led to an estimated 25% reduction of PA in the general population (Ammar et al., 2020; Malanchini et al., 2020; Yamada et al., 2020).
PA has a positive impact on mental health (Ku, Fox, & Chen, 2009). Previous studies have shown that confinement has a negative impact on general psychological health (Mihashi et al., 2009), which could lead to depression (Hull, 2005). Another study reported that a reduced level of PA during COVID-19 pandemic is associated with depression, which suggests that social behavioral limitations during the COVID-19 pandemic have worsened mental health (Puccinelli et al., 2021; Violant-Holz et al., 2020).
This decline in mental health may be more common among frail older adults. A meta-analysis of 23 studies reported an interaction between depression and frailty in older adults, with each condition being associated with an increased prevalence and incidence of the other disease, such as cognitive impairment (Soysal et al., 2017). Another 4-year follow-up study reported that, among the components of frailty, social frailty is more strongly associated with the occurrence of depressive symptoms among community-dwelling older adults than are physical frailty and cognitive frailty (Tsutsumimoto et al., 2018). Therefore, restricting social activities to counter infection may increase social frailty and consequently increase the incidence of depressive symptoms. A recent systematic review also suggested that as a sequela of the COVID-19 pandemic, the incidence of neuropsychiatric disorders such as depression could be expected to increase in direct proportion to social frailty (Lozupone et al., 2020). However, there have been an insufficient number of reports on the association between depressive symptoms and social frailty during the COVID-19 pandemic.
Before the COVID-19 outbreak, some studies reported that regular PA could reduce symptoms of depression (Schuch et al., 2018). Thus, physical exercise was used during COVID-19 as a strategy to combat the psychological and physical consequences of confinement, and its practice has been widely recommended during this period (Polero et al., 2020). Therefore, it is important to clarify whether depression symptoms are reduced by approaches that increase PA, such as exercise at home, when social activity is limited.
In the present cross-sectional study, we examined the association between social frailty and depressive symptoms in community-dwelling older adults during the COVID-19 pandemic. Moreover, we investigated whether home exercise habits moderated the impact of social frailty on depressive symptoms.
2. Methods
2.1. Study population
In this cross-sectional study, we mailed a questionnaire survey to community-dwelling older adults living in Minokamo City, a semi-urban area in Japan. Surveys were conducted before and after two state of emergency declarations corresponding to the COVID-19 pandemic wave in the target municipalities (Japan's declaration of the emergency state mainly requested that individuals refrain from performing nonessential activities and maintain physical distancing, and avoidance of restaurants at night). The first survey was carried out between March 3 and March 16, 2020, just before the nationwide state of emergency declaration. The second survey was carried out between October 16 and October 30, 2020, after the state of emergency declaration had been made at the local prefecture-level in the target survey area (Gifu Prefectural Office, 2020). In the first survey, we randomly sampled non-institutionalized older adults aged ≥ 65 years and who were not eligible to receive public long-term care insurance (LTCI) benefits or with “support need levels” of 1 or 2 in the public LTCI system (the Japanese public LTCI system classifies frail older adults into 7 levels: “support need levels” 1 and 2, and “care need levels” 1 to 5, whereby higher numbers indicate an increased need) (Tsutsui & Muramatsu, 2005). The first survey invited 2000 older adults to participate, and 1350 individuals responded to the survey (response rate: 67.5%). Of these, 1106 individuals completed the second survey (follow-up rate: 81.9%). In this study, we cross-sectionally analyzed data from participation of the second survey. We excluded participants with missing age or sex information (n = 3). Data from a final total of 1103 participants were included in the analysis.
This study was reviewed and approved by the ethics committees of Seijoh University (No. 2020C0013) and the National Center for Geriatrics and Gerontology (No. 20TB4). The mailed questionnaire was accompanied by an explanation of the study purpose, and participants were informed that they could withdraw from the study at any point without facing any consequences. Informed consent was given when participants agreed to complete the questionnaire and returned the completed survey. All procedures conformed to the principles outlined in the Declaration of Helsinki.
2.2. Depressive symptoms
Depressive symptoms were measured using the Kessler 6 scale (K6) (Kessler et al., 2003), Japanese version (Furukawa et al., 2008), which consists of six items that assess how frequently respondents have experienced symptoms of psychological distress in the past 30 days. The response options range from 0 = none of the time to 4 = all of the time (possible total score range: 0–24). Thus, we defined depressive symptoms using the K6 scale score. One Canadian study showed that the K6 scale is a valid tool for assessing depressive symptoms (area under the curve and 95% confidence interval [95%CI] were 0.93 and 0.91–0.95, respectively) (Cairney, Veldhuizen, Wade, Kurdyak, & Streiner, 2007). Following this previous study (Cairney et al., 2007), we classified respondents with K6 scores ≥5 as having depressive symptoms. This cut-off point has been shown to have a sensitivity of 0.92 (95% CI, 0.88–0.95) and a specificity of 0.78 (95% CI, 0.77–0.79) for depressive symptoms.
2.3. Social Frailty Screening Index
The Social Frailty Screening Index includes items that assess general resources (financial difficulties), social resources (living alone), social behavior (lack of social activity), and the fulfillment of basic social needs (influential contact with neighbors). The measure was developed by Yamada et al.(Yamada & Arai, 2018) based on Bunt's social frailty concept (Bunt, Steverink, Olthof, van der Schans, & Hobbelen, 2017). The measure includes the four following questions: 1) “Are you satisfied with your economic condition?”. The response options are “very satisfied”, “satisfied”, “unsatisfied”, and “very unsatisfied”. “Poor general resources (1 point)” was operationally defined as an answer of “unsatisfied” or “very unsatisfied”; 2) “Do you live alone?”. “Poor social resources (1 point)” was defined as living alone; 3) “How often do you participate in the following groups: volunteer, sports, hobby, learning or cultural, nursing care prevention, senior citizens, or residents’ associations?”. The response options included “Four or more times a week”, “Two or three times a week”, “Once a week”, “One to three times a month”, “A few times in a year”, and “Never”. “Poor social behavior (1 point)” was defined as an answer of “Never” for all groups; 4) “How do you get along with your neighbors?”. The response options included “I have a neighbor who comes and goes to each house”, “I have a neighbor to chat with on the street”, “I have a neighbor to say hello to”, and “I do not communicate with neighbors”. “Poor fulfillment of basic social needs (1 point)” was defined as an answer of “I have a neighbor to say hello to” or “I do not communicate with neighbors”. We defined scores of 2 or more as social frailty, 1 as pre-social frailty, and 0 as non-social frailty based on previous research (Yamada & Arai, 2018).
2.4. Exercise at home
Frequency of exercise at home was assessed by a single question, “How often have you exercised at home during (April to August 2020) the outbreak of the coronavirus infection?” The response options included “Four or more times a week”, “Two or three times a week”, “Once a week”, “One to three times a month”, “A few times in a year”, and “Never”. Participants were dichotomized into “exercise” (once or more times a week) and “non-exercise” (less than once a week) groups.
2.5. Covariates
The covariates included age, sex, basic activities of daily living (BADL), instrumental ADL (IADL), educational attainment, present illness, and PA. BADL was assessed using a single question, “Do you need someone's care or assistance in your daily life?”, and responses were dichotomized into “no difficulty” (response: “no need for care or assistance”) or “difficulty” (response: “need some care or assistance, but do not currently receive any” or “currently receive some care”). IADL was measured using a 5-item subscale, as in a previous study (Koyano, Shibata, Nakazato, Haga, & Suyama, 1991), and categorized participants who had difficulty with at least 1 item as “difficulty” and the others as “no difficulty”. Comorbidity referred to whether the following diseases were currently being treated or were sequelae: hypertension, stroke, heart disease, diabetes, hyperlipidemia, cancer, skeletal muscle disease, depression, and dementia. Those who confirmed the presence of at least one of these conditions were classified as “Yes,” and the rest were classified as “No.” Self-rated health was dichotomized into “poor” or “good”. Educational attainment was dichotomized as “low” (<10 years) or “middle/high” (≥10 years). PA was measured using 3-item subscale (Inoue et al., 2008) and the total METs/day score was calculated, as in a previous study, and classified into tertiles according to the total METs/days (“high”, “middle”, and “low”).
2.6. Statistical analysis
First, descriptive statistics and differences in each variable according to the level of social frailty were assessed using an ANOVA for continuous variables and chi-square test for categorical variables. Post-hoc analysis of ANOVA results was carried out using the Bonferroni's multiple comparison test. Second, multivariable logistic regression analysis was used to examine the association between social frailty and depressive symptoms, and the odds ratios (ORs) and 95% CIs for depressive symptoms were estimated. Two analytical models were created with the crude and adjusted models, including all covariates. Finally, we estimated the association between depressive symptoms and the level of social frailty stratified by exercise at home after adjusting for all covariates.
To mitigate the potential bias caused by missing information, we used the multiple imputation approach under the missing at random assumption (i.e., the missing data mechanism depends only on observed variables). We generated 20 imputed datasets using the multiple imputation by chained equations procedure and pooled the results using Rubin's rules (White, Royston, & Wood, 2011). Furthermore, for the sensitivity analysis, we performed a complete case analysis.
We used SPSS version 24 (IBM, Armonk, NY, USA) for all analyses, with a two-tailed significance level set at 5%.
3. Results
Data from a total of 1103 participants were analyzed. Table 1 shows the participants’ characteristics according to the level of social frailty. The mean age of participants was 81.1 years (standard deviation = 5.0), and 596 (54.0%) participants were female. The prevalence of each component determining social frailty (general resources, social resources, social behavior, the fulfillment of basic social needs) was 19.6%, 14.5%, 20.2%, and 18.0%, respectively. Regarding the participants’ level of social frailty, 460 (41.7%), 359 (32.5%), and 169 (15.3%) had non-social frailty, social pre-frailty, and social frailty, respectively. Those with social frailty were likely to be older, to have difficulty in BADL and IADL, to be less educated, to have low PA, and to exercise less at home. In total, 309 (28.0%) participants had depressive symptoms. Depressive symptoms were more common in those with social frailty (non-social frailty 22.2%, social pre-frailty 32.0%, and social frailty 46.2%).
Table 1.
Participant characteristics.
| The level of social frailty |
p-value | ||||
|---|---|---|---|---|---|
| Non-social frailty | Social pre-frailty | Social frailty | |||
| n = 460 | n = 359 | n = 169 | |||
| Age (years), mean (SD) | 80.52 (4.52) | 80.93 (5.02) | 82.01 (5.63) †, ⁎ | 0.003 | |
| Sex, n (%) | Men | 233 (50.7) | 165 (46.0) | 70 (41.4) | 0.097 |
| Women | 227 (49.3) | 194 (54.0) | 99 (58.6) | ||
| BADL, n (%) | No difficulty | 418 (90.9) | 302 (84.1) | 121 (71.6) | <0.001 |
| Difficulty | 38 (8.3) | 55 (15.3) | 47 (27.8) | ||
| Missing | 4 (0.9) | 2 (0.6) | 1 (0.6) | ||
| IADL, n (%) | No difficulty | 426 (92.6) | 304 (84.7) | 162 (71.6) | <0.001 |
| Difficulty | 24 (5.2) | 49 (13.6) | 44 (26.0) | ||
| Missing | 10 (2.2) | 6 (1.7) | 4 (2.4) | ||
| Comorbidity, n (%) | No | 330 (71.7) | 283 (78.8) | 139 (82.2) | 0.018 |
| Yes | 97 (21.1) | 63 (17.5) | 20 (11.8) | ||
| Missing | 33 (7.2) | 13 (3.6) | 10 (5.9) | ||
| Educational attainment, n (%) | Middle/high | 318 (69.1) | 239 (66.6) | 103 (60.9) | 0.231 |
| Low | 141 (30.7) | 119 (33.1) | 63 (37.3) | ||
| Missing | 1 (0.2) | 1 (0.3) | 3 (1.8) | ||
| Physical activity, n (%) | High | 139(30.2) | 82 (22.8) | 23 (13.6) | <0.001 |
| Middle | 184 (40.0) | 117 (32.6) | 43 (25.4) | ||
| Low | 95 (20.7) | 122 (34.0) | 90 (53.3) | ||
| Missing | 42 (9.1) | 38 (10.6) | 13 (7.7) | ||
| Exercise at home | Exercise | 254 (55.2) | 171 (47.6) | 64 (37.9) | <0.001 |
| Non-exercise | 152 (33.0) | 142 (39.6) | 88 (52.1) | ||
| Missing | 54 (11.7) | 46 (12.8) | 17 (10.1) | ||
| Depressive symptoms, n (%) | No | 301 (65.4) | 208 (57.9) | 76 (45.0) | <0.001 |
| Yes | 102 (22.2) | 115 (32.0) | 78 (46.2) | ||
| Missing | 57 (12.4) | 36 (10.0) | 15 (8.9) | ||
Significant differences compared with the social robust groups, post-hoc analysis using Bonferroni's multiple comparison test (p < 0.05). Group differences were examined using an ANOVA or χ2-test. BADL, basic activities of daily living; IADL, instrumental activities of daily living; SD, standard deviation
Missing data, n = 115 for the level of social frailty
Table 2 presents the association between social frailty and depressive symptoms. Multivariable logistic regression analysis revealed that, compared with non-social frailty, social frailty was significantly associated with depressive symptoms after adjusting for all covariates using the multiple imputation approach; the ORs (95% CIs) for depressive symptoms were 1.80 (1.16–2.79) for social frailty (p =0.009) and 1.29 (0.93–1.78) for social pre-frailty (p =0.128).
Table 2.
Association between social frailty and depressive symptoms during the COVID-19 pandemic, multivariable logistic regression analysis with multiple imputation approach.
| Crude model |
Adjusted model |
|||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| The level of social frailty | ||||
| Non-social frailty | 1.00 (reference) | 1.00 (reference) | ||
| Social pre-frailty | 1.60 (1.18–2.17) | 0.003 | 1.29 (0.93–1.78) | 0.128 |
| Social frailty | 2.94 (2.00–4.31) | <0.001 | 1.80 (1.16–2.79) | 0.009 |
| Age (per 1 year) | 1.02 (0.99–1.05) | 0.152 | ||
| Women (ref: men) | 1.32 (0.99–1.76) | 0.062 | ||
| BADL difficulty (ref: no difficulty) | 3.14 (2.00–4.92) | <0.001 | ||
| IADL difficulty (ref: no difficulty) | 2.25 (1.44–3.54) | <0.001 | ||
| Comorbidity (ref: no) | 1.21 (0.83–1.75) | 0.325 | ||
| Low educational (ref: middle/high) | 1.15 (0.86–1.55) | 0.343 | ||
| Physical activity | ||||
| Middle (ref: high) | 1.23 (0.84–1.77) | 0.291 | ||
| Low (ref: high) | 1.33 (0.91–1.97) | 0.144 | ||
| Exercise at home (ref: Non-exercise) | 0.93 (0.69–1.27) | 0.654 | ||
BADL, basic activities of daily living; CI, confidence interval; IADL, instrumental activities of daily living; OR, odds ratio
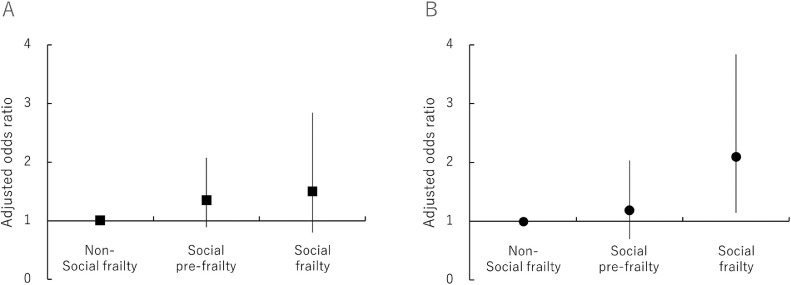
Fig. 1 shows the ORs and 95% CIs for depressive symptoms for each level of social frailty stratified by exercise at home, adjusted for all covariates. In participants who had not exercised at home, the ORs of social frailty with depressive symptoms were slightly increased (OR: 2.10, 95% CIs: 1.14–3.84, p =0.017). On the other hand, in participants who had exercised at home, social frailty was moderately associated with depressive symptoms (OR: 1.50, 95% CI: 0.79–2.85, p =0.213). However, the ‘social frailty’ × exercise at home (exercise at home was coded as 0 for non-exercise or 1 for exercise) interaction was not significantly associated (p =0.299), although the OR was in the expected direction (OR: 0.65, 95% CI: 0.29–1.46).
Fig. 1.
ORs and CIs for depressive symptoms for the level of social frailty with or without exercise at home. (A) With exercise at home; (B) without exercise at home.
The error bars indicate 95% confidence intervals. The values were imputed using the multiple imputation approach and adjusted for all covariates.
We also confirmed that the ORs of social frailty for depressive symptoms were approximately similar to those obtained in the complete analysis (Supplementary Table 1, Supplementary Figure 1).
4. Discussion
The present cross-sectional study demonstrated the association between social frailty and depressive symptoms in older adults during the COVID-19 pandemic. We found that social frailty was associated with depressive symptoms during the pandemic, and exercise at home may buffer this relationship. Our findings suggested that those with social frailty had poorer mental health during the COVID-19 pandemic and that forming exercise habits at home maintained a healthy mental health status.
Previous studies have reported a prevalence of social frailty of approximately 8% to 18% in community-dwelling older adults according to each social frailty index (Garre-Olmo, Calvó-Perxas, López-Pousa, de Gracia Blanco, & Vilalta-Franch, 2013; Lee, Chon, Kim, Ki, & Yun, 2020; Teo, Gao, Nyunt, Wee, & Ng, 2017). Using the same index, Yamada et al. found that 18.0% had social frailty (Yamada & Arai, 2018). The current study found a prevalence of social frailty of 15.3%, which is consistent with previous findings. However, the present study could not clarify the change in the rate of social frailty before and after the COVID-19 outbreak.
Our results indicate that those with social frailty had a high risk of depressive symptoms during the COVID-19 pandemic. Several longitudinal studies have suggested that social frailty may be a predictor of depressive symptoms (Chen et al., 2021; Tsutsumimoto et al., 2018). Moreover, social frailty has been reported to be more strongly associated with depressive symptoms than the physical and cognitive components of frailty (Tsutsumimoto et al., 2018). Both social frailty and depressive symptoms were expected to increase during the pandemic, as they result from limiting social behaviors to counter the spread of coronavirus (Lozupone et al., 2020). However, there has been a lack of empirical evidence of these associations during the COVID-19 pandemic. Although the present study is a cross-sectional study, and it is not clear whether social frailty is more likely to result in depressive symptoms during the COVID-19 pandemic, those with social frailty had a higher proportion of depressive symptoms than those with non-social frailty, which indicates the need for preventive measures.
Previous studies have shown that exercise is an effective measure that is often recommended to prevent depression in older adults (Knapen, Vancampfort, Moriën, & Marchal, 2015; Seo & Chao, 2018). Therefore, we examined whether exercise at home, which can be done during the COVID-19 pandemic, reduced depressive symptoms. Our results showed that there was no significant interaction effect between level of social frailty × exercise at home; however, the stratified analysis showed that home exercise habits alleviated depressive symptoms in individuals with social frailty. One possible reason for this is the biochemical or physiological mechanisms associated with increased PA (Daley, 2008; Deslandes et al., 2009). However, our results showed a moderating effect of home-based exercise, even when considering physical activities. Another study showed that regular exercise had a positive impact on personal and psychological parameters, and exercise was a preferred method by which to enhance self-efficacy, self-esteem, and physical awareness (Tikac, Unal, & Altug, 2021), which suggests that those who exercised at home had fewer depressive symptoms.
The COVID-19 pandemic has not only affected physical health, but also mental health (Fiorillo & Gorwood, 2020). Despite differences in the epidemic situation between countries, previous study indicated that continuing even exercise at home during the COVID-19 pandemic may reduce the side effects of COVID-19 on mental health after the pandemic (Hu, Tucker, Wu, & Yang, 2020). Our study suggested that forming exercise habits to maintain a healthy mental health status during the pandemic may be helpful, especially in older adults with social frailty.
This study has several limitations. First, this study was cross-sectional study, and so we were unable to determine causal relationships. However, this is the first study to clarify the relationship between social frailty and depressive symptoms during the COVID-19 pandemic. In the future, longitudinal research should be conducted to investigate causal relationships. Second, this study used a questionnaire, and so misclassification might have occurred in the assessment of depressive symptoms. Moreover, we were unable to determine which type of exercise was more strongly associated with reduced depression. Nonetheless, it is meaningful to suggest an approach that can reduce depressive symptoms in those with social frailty. Third, it was necessary to evaluate not only social frailty but also physical and cognitive frailty and examine their relationships. However, because it was a questionnaire survey, we could not evaluate grip strength, walking speed, or MMSE because this may have caused residual confounding. Therefore, these factors could have caused residual confounding. Finally, our study participants were slightly older than typical community-dwelling older adults, and our survey was conducted in a semi-urban area in Japan. This may reduce the generalizability of our results; thus, further nationwide research is needed.
5. Conclusions
In conclusion, the present results indicate that social frailty was associated with depressive symptoms during the COVID-19 pandemic. However, even in participants with social frailty, this relationship was mitigated in those who exercised at home. Our findings indicated that depressive symptoms in socially frail older adults need to be addressed and that exercise at home may help these individuals to maintain their mental health.
CRediT authorship contribution statement
Takahiro Hayashi: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Visualization, Writing – original draft. Taiji Noguchi: Data curation, Funding acquisition, Writing – review & editing. Yuta Kubo: Data curation, Funding acquisition, Writing – review & editing. Naoki Tomiyama: Data curation, Funding acquisition, Writing – review & editing. Akira Ochi: Data curation, Funding acquisition, Writing – review & editing. Hiroyuki Hayashi: Data curation, Funding acquisition, Writing – review & editing.
Declaration of competing interest
None
Acknowledgments
Acknowledgments
We offer our sincere thanks to the staff of the Minokamo City office. We would also like to thank all the study participants.
Funding Statement
This study was supported by JSPS KAKENHI (Grant-in-Aid for Scientific Research [C]: 19K02200, and Grant-in-Aid for Young Scientists: No. 21K17322). The authors also received a research grant from the Health Science Center Foundation (2019-2020), the Japan Full-hap Survey Research Grant (2020) from the Japan Small Business Welfare Foundation.
Data statement
All datasets have ethical or legal restrictions for public deposition because of the inclusion of sensitive information about the human participants.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.archger.2021.104555.
Appendix. Supplementary materials
References
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6):1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunt S., Steverink N., Olthof J., van der Schans C.P., Hobbelen J.S.M. Social frailty in older adults: A scoping review. European Journal of Ageing. 2017;14(3):323–334. doi: 10.1007/s10433-017-0414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairney J., Veldhuizen S., Wade T.J., Kurdyak P., Streiner D.L. Evaluation of 2 measures of psychological distress as screeners for depression in the general population. Canadian Journal of Psychiatry. 2007;52(2):111–120. doi: 10.1177/070674370705200209. [DOI] [PubMed] [Google Scholar]
- Caputo E.L., Reichert F.F. Studies of physical activity and COVID-19 during the pandemic: A scoping review. Journal of Physical Activity & Health. 2020;17(12):1275–1284. doi: 10.1123/jpah.2020-0406. [DOI] [PubMed] [Google Scholar]
- Chen Z., Jiang X., Shi G., Wang Y., Chu X., Wang Z., et al. Social frailty and longitudinal risk of depressive symptoms in a Chinese population: The Rugao longevity and aging study. Psychogeriatrics. 2021;21(4):483–490. doi: 10.1111/psyg.12696. [DOI] [PubMed] [Google Scholar]
- Daley A. Exercise and depression: A review of reviews. Journal of Clinical Psychology in Medical Settings. 2008;15(2):140–147. doi: 10.1007/s10880-008-9105-z. [DOI] [PubMed] [Google Scholar]
- Deslandes A., Moraes H., Ferreira C., Veiga H., Silveira H., Mouta R., et al. Exercise and mental health: Many reasons to move. Neuropsychobiology. 2009;59(4):191–198. doi: 10.1159/000223730. [DOI] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. European Psychiatry. 2020;63(1):e32. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa T.A., Kawakami N., Saitoh M., Ono Y., Nakane Y., Nakamura Y., et al. The performance of the Japanese version of the K6 and K10 in the world mental health survey Japan. International Journal of Methods in Psychiatric Research. 2008;17(3):152–158. doi: 10.1002/mpr.257. 10.1002/mpr.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garre-Olmo J., Calvó-Perxas L., López-Pousa S., de Gracia Blanco M., Vilalta-Franch J. Prevalence of frailty phenotypes and risk of mortality in a community-dwelling elderly cohort. Age and Ageing. 2013;42(1):46–51. doi: 10.1093/ageing/afs047. [DOI] [PubMed] [Google Scholar]
- Gifu Prefectural Office Information on a new type of coronavirus infection in Gifu Prefecture. “Emergency Measures for "second wave emergency” (Governor’s Message) 2020 https://www.pref.gifu.lg.jp/site/covid19/62123.html Retrieved from. Accessed April 7, 2021. [Google Scholar]
- Hartley D.M., Perencevich E.N. Public Health Interventions for COVID-19: Emerging Evidence and Implications for an Evolving Public Health Crisis. JAMA. 2020;323(19):1908–1909. doi: 10.1001/jama.2020.5910. [DOI] [PubMed] [Google Scholar]
- Hu S., Tucker L., Wu C., Yang L. Beneficial effects of exercise on depression and anxiety during the Covid-19 pandemic: A narrative review. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.587557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull H.F. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases. 2005;11(2):354–355. doi: 10.3201/eid1102.040760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoue M., Yamamoto S., Kurahashi N., Iwasaki M., Sasazuki S., Tsugane S. Daily total physical activity level and total cancer risk in men and women: Results from a large-scale population-based cohort study in Japan. American Journal of Epidemiology. 2008;168(4):391–403. doi: 10.1093/aje/kwn146. [DOI] [PubMed] [Google Scholar]
- Islam N., Sharp S.J., Chowell G., Shabnam S., Kawachi I., Lacey B., et al. Physical distancing interventions and incidence of coronavirus disease 2019: Natural experiment in 149 countries. BMJ. 2020;370 doi: 10.1136/bmj.m2743. m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karako K., Song P., Chen Y., Tang W., Kokudo N. Overview of the characteristics of and responses to the three waves of COVID-19 in Japan during 2020-2021. Bioscience Trends. 2021;15(1):1–8. doi: 10.5582/bst.2021.01019. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., et al. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Knapen J., Vancampfort D., Moriën Y., Marchal Y. Exercise therapy improves both mental and physical health in patients with major depression. Disability and Rehabilitation. 2015;37(16):1490–1495. doi: 10.3109/09638288.2014.972579. [DOI] [PubMed] [Google Scholar]
- Koyano W., Shibata H., Nakazato K., Haga H., Suyama Y. Measurement of competence: Reliability and validity of the TMIG index of competence. Archives of Gerontology and Geriatrics. 1991;13(2):103–116. doi: 10.1016/0167-4943(91)90053-s. [DOI] [PubMed] [Google Scholar]
- Ku P.W., Fox K.R., Chen L.J. Physical activity and depressive symptoms in Taiwanese older adults: A seven-year follow-up study. Preventive Medicine. 2009;48(3):250–255. doi: 10.1016/j.ypmed.2009.01.006. [DOI] [PubMed] [Google Scholar]
- Lee Y., Chon D., Kim J., Ki S., Yun J. The predictive value of social frailty on adverse outcomes in older adults living in the community. Journal of the American Medical Directors Association. 2020;21(10) doi: 10.1016/j.jamda.2020.03.010. 1464–1469.e1462. [DOI] [PubMed] [Google Scholar]
- Looi M.K. Covid-19: Japan declares state of emergency as Tokyo cases soar. BMJ. 2020;369 doi: 10.1136/bmj.m1447. m1447. [DOI] [PubMed] [Google Scholar]
- Lozupone M., La Montagna M., Di Gioia I., Sardone R., Resta E., Daniele A., et al. Social frailty in the COVID-19 pandemic era. Frontiers in psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.577113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malanchini G., Malacrida M., Ferrari P., Leidi C., Ferrari G., Racheli M., et al. Impact of the coronavirus disease-19 outbreak on physical activity of patients with implantable cardioverter defibrillators. Journal of Cardiac Failure. 2020;26(10):898–899. doi: 10.1016/j.cardfail.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihashi M., Otsubo Y., Yinjuan X., Nagatomi K., Hoshiko M., Ishitake T. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychology. 2009;28(1):91–100. doi: 10.1037/a0013674. [DOI] [PubMed] [Google Scholar]
- Polero P., Rebollo-Seco C., Adsuar J.C., Pérez-Gómez J., Rojo-Ramos J., Manzano-Redondo F., et al. Physical activity recommendations during COVID-19: Narrative review. International Journal of Environmental Reseach and Public Health. 2020;18 doi: 10.3390/ijerph18010065. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puccinelli P.J., da Costa T.S., Seffrin A., de Lira C.A.B., Vancini R.L., Nikolaidis P.T., et al. Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: An internet-based survey. BMC Public Health. 2021;21(1):425. doi: 10.1186/s12889-021-10470-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch F.B., Vancampfort D., Firth J., Rosenbaum S., Ward P.B., Silva E.S., et al. Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. The American Journal of Psychiatry. 2018;175(7):631–648. doi: 10.1176/appi.ajp.2018.17111194. [DOI] [PubMed] [Google Scholar]
- Seo J.Y., Chao Y.Y. Effects of exercise interventions on depressive symptoms among community-dwelling older adults in the United States: A systematic review. Journal of Gerontological Nursing. 2018;44(3):31–38. doi: 10.3928/00989134-20171024-01. [DOI] [PubMed] [Google Scholar]
- Soysal P., Veronese N., Thompson T., Kahl K.G., Fernandes B.S., Prina A.M., et al. Relationship between depression and frailty in older adults: A systematic review and meta-analysis. Ageing Research Reviews. 2017;36:78–87. doi: 10.1016/j.arr.2017.03.005. [DOI] [PubMed] [Google Scholar]
- Teo N., Gao Q., Nyunt M.S.Z., Wee S.L., Ng T.P. Social frailty and functional disability: Findings from the singapore longitudinal ageing studies. Journal of the American Medical Directors Association. 2017;18(7):637.e613–637.e619. doi: 10.1016/j.jamda.2017.04.015. [DOI] [PubMed] [Google Scholar]
- Tikac G., Unal A., Altug F. Regular exercise improves the levels of self-efficacy, self-esteem and body awareness of young adults. The Journal of Sports Medicine and Physical Fitness. 2021 doi: 10.23736/s0022-4707.21.12143-7. [DOI] [PubMed] [Google Scholar]
- Tsutsui T., Muramatsu N. Care-needs certification in the long-term care insurance system of Japan. Journal of the American Geriatrics Society. 2005;53(3):522–527. doi: 10.1111/j.1532-5415.2005.53175.x. [DOI] [PubMed] [Google Scholar]
- Tsutsumimoto K., Doi T., Makizako H., Hotta R., Nakakubo S., Kim M., et al. Social frailty has a stronger impact on the onset of depressive symptoms than physical frailty or cognitive impairment: A 4-year follow-up longitudinal cohort study. Journal of the American Medical Directors Association. 2018;19(6):504–510. doi: 10.1016/j.jamda.2018.02.008. [DOI] [PubMed] [Google Scholar]
- Violant-Holz V., Gallego-Jiménez M.G., González-González C.S., Muñoz-Violant S., Rodríguez M.J., Sansano-Nadal O., et al. Psychological health and physical activity levels during the COVID-19 pandemic: A systematic review. International Journal of Environmental Reseach and Public Health. 2020;(24):17. doi: 10.3390/ijerph17249419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White I.R., Royston P., Wood A.M. Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine. 2011;30(4):377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2020. Archived: WHO Timeline - COVID-19. Retrieved from https://www.who.int/news/item/27-04-2020-who-timeline—covid-19. Accessed April 7, 2021. [Google Scholar]
- Yamada M., Arai H. Social frailty predicts incident disability and mortality among community-dwelling japanese older adults. Journal of the American Medical Directors Association. 2018;19(12):1099–1103. doi: 10.1016/j.jamda.2018.09.013. [DOI] [PubMed] [Google Scholar]
- Yamada M., Kimura Y., Ishiyama D., Otobe Y., Suzuki M., Koyama S., et al. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: A cross-sectional online survey. The Journal of Nutrition, Health & Aging. 2020;24(9):948–950. doi: 10.1007/s12603-020-1424-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.