Abstract
Purpose
Morphometric analysis of the patella and the patellar ligament is crucial in diagnosing and surgical corrections of knee injuries and patellofemoral joint disorders. Dimensions of the patella and the patellar ligament are frequently used in implant design and ACL reconstruction. This study aims to obtain detailed morphometric data on the patellar ligament and its localization based on gross anatomical dissections in the adult cadavers.
Methods
The present study consisted of 50 lower limbs from formalin-fixed male adult cadavers aged about 70 years (45–85) belonging to the South Indian population. Total length of the quadriceps tendon, patellar height, patellar ligament height, proximal width, distal width and thickness of the patellar ligament were measured meticulously. Mean, standard deviation, median scores of each parameter were computed for groups using SPSS 16.0. Level of significance was considered as p < 0.05. Wilcoxon signed-rank test was used to compare the various parameters on the right and left limbs. The relationships between all parameters were analyzed using Spearman’s rank correlation test.
Results
There was no statistically significant difference in the various measurements of the patella and patellar ligament between the right and left lower limbs. Patellar ligament length showed positive correlation with ligament thickness (r = 0.36; p = 0.078 for right limb and r = 0.33; p = 0.104 for left limb). Proximal width of ligament showed significant positive correlation with distal width (r = 0.41; p = 0.041 for right limb and r = 0.54; p = 0.006 for left limb).
Conclusion
This morphometric data and analysis might be fundamental in understanding various knee conditions in situ and necessary to orthopedic surgeons for successful planning and execution for ACL reconstruction using patellar ligament graft and other patellofemoral joint disorders.
Level of evidence
I
Keywords: Patella, Patellar tendon, Dimensions, Morphometric, Tendon graft
Introduction
The most common injury at the knee joint, especially in sportspeople, is a tear of the anterior cruciate ligament (ACL). The patellar ligament and quadriceps tendon are commonly used as grafts for ACL reconstruction, surgical revision, and multi-ligament surgery to restore functional stability. The patella is the largest sesamoid bone in the body that develops within the tendon of the quadriceps femoris muscle and is found on the anterior surface of the femoral condyles. It has two surfaces (anterior and posterior), three borders (superior, medial, and lateral), and an apex pointing inferiorly [31]. The patella, also called a knee cap, does not have morphological sex determination; nevertheless, it is one of the few bones in the human body that is resistant to post-mortem changes [25]. The extensor mechanism of the knee consists of the quadriceps muscle group and tendon, the patella, the patellar ligament, the tibial condyles, and the patellar retinaculum [11]. The patellar tendon (patellar ligament) is the central band of the tendon of the quadriceps femoris, which is continued distally from the patella to the tibial tuberosity. It is strong, flat, about 6 cm in length, and is attached proximally to the patellar apex and adjoining margins, while distally, it is attached to the tibial tuberosity [31]. This insertion is oblique and directed laterally. In the procedure of tibial osteotomy, the tibia is cut transversely just above the patellar tendon insertion. Failure to appreciate the obliquity of the tibial attachment of the tendon may lead to an unintended division of the tendon during this procedure, leading to unfortunate consequences [31].
Morphometric data from the studies on the patella and patellar ligament are crucial in the diagnosis and surgical corrections of knee-related injuries [21, 33] and patellofemoral joint disorders [2, 28]. Dimensions of the patella and patellar ligament are frequently utilized in implant design and specific surgical procedures such as patella resurfacing for total knee arthroplasty and the harvesting technique of patellar ligament grafts during the reconstruction of the anterior cruciate ligament [24, 26]. Determining the relationship between the patella and patellar ligament in different population groups is essential anthropologically and clinically. Understanding the pathogenesis of disorders involving the knee calls for detailed knowledge of the normal anatomy and biomechanics of the patella and the patellar ligament [9]. Previous studies have shown significant evidence-based racial differences in the morphometry of the knee joint, patellar ligament amongst the studied populations [8]. There are not any detailed studies dealing with the patella and patellar ligament morphometric measurements using cadavers belonging to the Indian population. The advantage of the measurements performed in a cadaveric approach is that they do not involve approximation and assumptions. Thus, in this study, we aimed to obtain detailed morphometric data on the patellar ligament and its localization based on gross anatomical dissections in the adult cadavers.
Materials and methods
The study sample consisted of 50 lower limbs (25 right lower limbs and 25 left lower limbs) from formalin-fixed (10% formalin) male cadavers belonging to the South Indian population, procured from the Anatomy department of our college. The mean age of the cadavers was 75 years (45–85). Cadavers with osteoarthritic changes to the knee, visible surgical scars in the knee region, physical signs of deformity of the patella, or patellofemoral disease were excluded from the study. The incision was made on the medial sides of both knees of the cadaver, skin and facia lata were carefully removed to expose the quadriceps tendon, the patella, and the patellar ligament. The tendon of the quadriceps femoris and the patellar ligament was carefully freed from the underlying structures without causing any alteration to the desired structures. All measurements were performed while the patella and patellar ligament were in situ. The various morphometric measurements were measured using a calibrated rigid ruler (accuracy, 0.5 mm) and silk suture thread. All measurements were taken twice, in the same manner by the same investigator for all the limbs to avoid interobserver variability. Since there was no differences in the measurements, intra-observer reliability test was not performed. Total length of the quadriceps tendon, patellar height, patellar ligament height (patellar tendon length), proximal width, distal width and thickness of the patellar ligament were measured meticulously. The description of the measurements is shown in Table 1 and Fig. 1.
Table 1.
Description of measurements taken of the patella and patellar ligament
| Measurement | Abbreviation | Description |
|---|---|---|
| Total length | TL | The linear distance between the base of the patella and the attachment of the patellar ligament to the tibial tuberosity |
| Patella height | PH | The linear distance between the superior border and the apex of the patella |
| Patellar ligament height/patellar tendon length | PLH | The linear distance between the apex of the patella and the tibial tuberosity |
| Patellar ligament width (proximal end) | PW | Maximum width of the ligament just below the apex of the patella |
| Patellar ligament width (distal end) | DW | Maximum width of the ligament just above tibial tuberosity |
| Patellar ligament thickness | PT | The thickness of the ligament above its distal attachment |
Fig. 1.
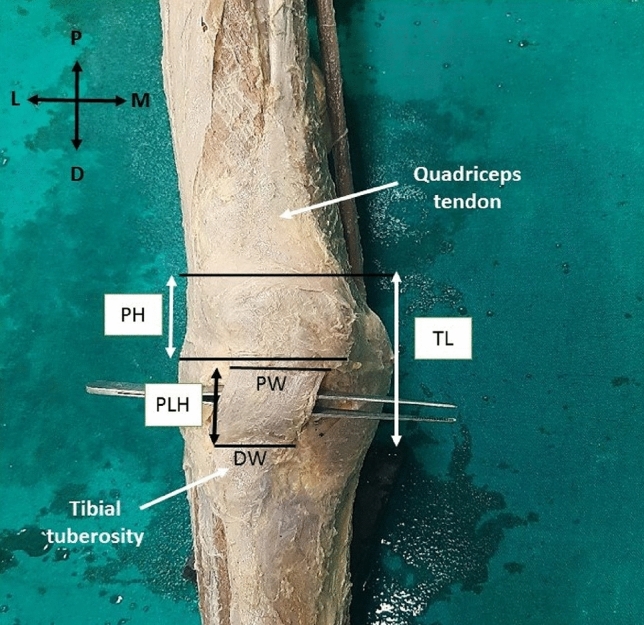
Figure showing the various measurements of the patella and patellar ligament. TL total length, PH patella height, PLH patellar ligament height, PW patellar ligament width (proximal end), DW patellar ligament width (distal end). Axis: P proximal, D distal, M medial, L lateral
The mean, standard deviation, median scores of each parameter were computed concerning groups using SPSS 16.0 statistical package (SPSS Inc, Chicago, IL). Level of significance (p-value) was set at 0.05. Wilcoxon signed-rank test was used to compare the various parameters on right and left limbs. The relationships between all parameters were analyzed using Spearman’s rank correlation test. To determine the statistical power, we performed power analysis for correlation in R version 3.6.3. The correlation power analysis estimated a power of 82.2% to determine the statistical power between the proximal width vs distal width in the left lower limb with a sample size of 25, level of significance of 5% and correlation coefficient of 0.54. Results were represented in relevant tables and graphs (Tables 2, 3, 4 and 5).
Table 2.
Table showing the various morphometric measurements of the patella and patellar ligament
| Variables | Right lower limb | Left lower limb | ||
|---|---|---|---|---|
| Median | Mean ± SD (cm) | Median (range) | Mean ± SD (cm) | |
| Total length (TL) | 10 | 9.96 ± 0.84 | 10 | 9.88 ± 0.88 |
| Patellar height (PH) | 5 | 5.08 ± 0.64 | 5 | 5.2 ± 0.78 |
| Patellar ligament height (PLH) | 5 | 4.88 ± 0.65 | 5 | 4.68 ± 0.91 |
| Proximal width (PW) | 3.5 | 3.56 ± 0.43 | 4 | 3.50 ± 0.44 |
| Distal width (DW) | 2.5 | 2.62 ± 0.49 | 2.5 | 2.48 ± 0.45 |
| Patellar ligament thickness (PT) | 6 | 5.92 ± 0.62 | 6 | 5.80 ± 0.74 |
Table 3.
Table showing the result for Wilcoxon signed-rank test to compare the level of significance between the studied variables in the right and left limbs
| Wilcoxon Signed rank test | |
|---|---|
| Variables | p-value (between right and left limbs) |
| Total length (TL) | 0.664 |
| Patellar height (PH) | 0.322 |
| Patellar ligament height (PLH) | 0.368 |
| Proximal width (PW) | 0.551 |
| Distal width (DW) | 0.3137 |
| Patellar ligament thickness (PT) | 0.4437 |
Table 4.
Table showing the correlation between the length of the patellar ligament and ligament thickness in the right and left lower limbs
| Length of patellar ligament vs ligament thickness | Spearman’s rank correlation coefficients | p-value |
|---|---|---|
| Right lower limb | 0.36 | 0.078 |
| Left lower limb | 0.33 | 0.104 |
Table 5.
Table showing the correlation between proximal and distal width of the patellar ligament in the right and left lower limbs
| Proximal width vs distal width of the patellar ligament | Spearman’s rank correlation coefficients | p-value |
|---|---|---|
| Right lower limb | 0.41 | 0.041* |
| Left lower limb | 0.54 | 0.006* |
*At 5% level of significance
Results
Side differences
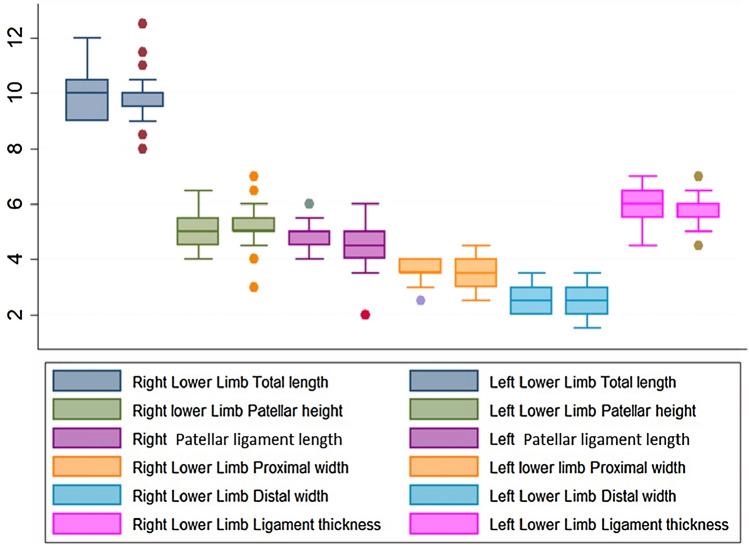
A Wilcoxon signed-rank test showed that there was no statistically significant difference in the various measurements of the patella and patellar ligament between the right and left lower limbs (p > 0.05) (Fig. 2, Table 3). The average length of the patellar ligament was 4.8 cm on the right limb and 4.6 cm on the left limb. The shortest ligament was about 2 cm (range 3–6 cm) was observed in the left limb with no obvious pathology. Patellar height was almost the same in both limbs (5.03 cm) (Table 3).
Fig. 2.
Comparison of morphometric measurements between right and left lower limbs
Descriptive analyses
The mean, standard deviation, and median scores for the measurements of the patella and the patellar ligament are presented in Table 2.
Analyses of correlation
Spearman’s correlation analysis was performed.
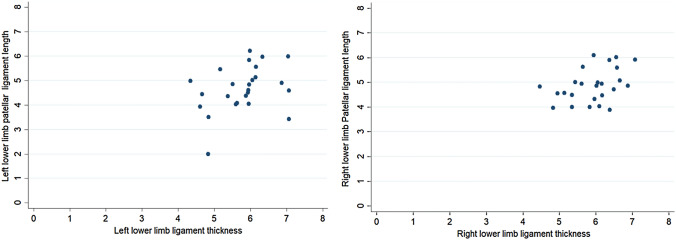
Patellar ligament length showed low correlation with ligament thickness (r = 0.36; p = 0.078 for right limb and r = 0.33; p = 0.104 for left limb) (Table 4, Fig. 3). Proximal width of ligament showed significant positive correlation with distal width (r = 0.41; p = 0.041 for right limb and r = 0.54; p = 0.006 for left limb) (Table 5, Fig. 4). There was a negative (r = − 0.18) statistically non-significant (p value = 0.38) relationship between patella height and patellar tendon length (PLH) in the right lower limb. However, in the left lower limb, there was a negative (r = − 0.47) statistically significant moderate (p value = 0.02) relationship between patella height and patellar tendon length (PLH) in the right lower limb (Fig. 5). This indicates that, as the patellar height increases, the patellar tendon length decreases.
Fig. 3.
Correlation between lengths of patellar ligament vs. ligament thickness in right and left lower limbs
Fig. 4.
Correlation between Proximal width vs. distal width of the patellar ligament between the right and left lower limbs
Fig. 5.
Correlation between patellar height vs. length after patella (patellar ligament height) of the right and left lower limbs
Discussion
A relevant anatomical knowledge regarding musculoskeletal structure with its associated relationships has always been essential to orthopedic surgeons. Although many studies focus on the geometry of patella and patellar tendon, these studies are mainly radiological, intraoperative measurements, and biomechanical studies. There are very few cadaveric studies dealing with the actual in situ measurements of the patella and patellar ligament to the authors' knowledge. Thus, this study was aimed to provide the whole integrated morphometry of the patella and patellar ligament using anatomical dissection. Although the anatomical methods have the disadvantage of limited clinical material for substantial clinical research, the data obtained from these studies are beneficial for adapting to modern surgical procedures.
Morphometric measurements of the patella are important anthropologically as they can be used in forensic science for sex determination with the highest accuracy rate. In the present study mean height of the patella was approx. 5 cm on both limbs. This finding is similar to the study of Schlenzka et al., wherein the mean patellar height was 5.4 cm in 50 fresh cadaveric patellae studied by them [28]. In previous studies, the mean patellar height was found to be 44.6 mm which was MRI study [33], 39.9 mm in a study on CT scans from 40 Chinese volunteers [30], 42.96 mm in a study using dry patella [4], 38.07 mm in a study on dry patella of Indian population [20], and 43.7 mm in cadaveric patellae of European ancestry [23]. Although the reasons for variations in patellar height cannot be validated, the differences may be due to the difference in methods of measuring, age, sexes, study group, ethnicity, and stature [23]. It is known that morphometric variations are often observed in measurements even within the same population group and that the variation could be more striking across different ethnic groups.
Dimensions and classification of patellae are important for anthropologists and surgeons for the determination of the size of a patellar implant [18]. A disproportional implant of the patellofemoral joint would result in ineffective lever support, limitation of motion, excessive wear, and patella instability with associated knee pain [14].
The development of the patellar ligament in the fetal period is important as the pathologic conditions of the patellar ligament in adulthood may be associated with fetal development [5, 19]. Patellar ligament plays a vital role in the extensor mechanism of knees, and patellar tendinitis, partial or complete ligament tears, can result in loss of ligament function. It is opined that complete patellar ligament tears are primarily seen in athletes, volleyball, and basketball players [10]. Ligament tear will result in restricted activity levels, thereby decreasing quality of life [16]. Hence knowledge regarding the exact anatomy of the patellar ligament is important to understand its functional mechanism and aid in its surgical reconstruction. Another common ligament injury seen nowadays is the tear of the anterior cruciate ligament (ACL). ACL is an intracapsular ligament of the knee joint. The area of origin and insertion of the ACL is reported to average 113 and 136 mm2, respectively. The cross-sectional area at midsubstance varies between 36 and 44 mm2, while the length of the anterior and posterior aspect of the ligament is reported to vary between 22 and 41 mm [7, 12]. With varying techniques employed by surgeons, the source of the graft tissue to replace the damaged ACL is of critical importance to ensure the best outcome. The most commonly used grafts for ACL reconstruction are those of the patellar ligament and the hamstrings (semitendinosus or gracilis), to a lesser extent, the fascia lata and quadriceps tendon [27]. Although there are numerous options available, there is no agreement in the literature on the most suitable choice for the graft source [1, 17, 22]. Many factors need to be considered in selecting a graft material like, it should be easily accessible, should rapidly ligamentize once implanted, and be comparable to the strength of ACL [13]. Therefore, the patellar ligament is the most favored choice for graft as it has greater tensile strength, it may be vascular, and can have some bony part with it providing better chances for successful graft [3]. Both the quadriceps tendons and patellar ligaments have been tested for strength and load-bearing capacity and are comparable in this regard [15]. The patellar ligament is stronger and more rigid than the quadriceps tendon [29]. Patellar tendon bone grafts should be used for young patients and high demand athletes who prefer early return to high-level activities, while hamstring tendons are advantageous when a large skin incision or anterior knee pain should be avoided [6]. The length of the patellar tendon is a major concern in ACL reconstruction surgery with a patellar tendon graft. The bone peg harvested from the inferior pole of the patella is usually placed at the femoral tunnel, and that from tibial tuberosity at the tibial tunnel, and the ligament substance between the bong pegs acts as the reconstructed ACL [33].
We found in our study that the length of the patellar ligament on the right limb was slightly more when compared to the left limb, and a slight positive correlation was observed between the ligament length and ligament thickness in both the limbs (r = 0.36 for right limb and r = 0.33 for left limb). Even though we could not give exact justification for these observations, we assume that factors such as predominant use of one limb, posture, physique, etc., might produce better muscle tone on one side, thereby directly affecting the length and thickness of the patella and patellar ligament. A positive correlation was also observed between the proximal and distal width of the patellar ligament in both limbs (r = 0.41 for right limb and r = 0.54 for left limb). The patellar ligament was wider proximally than distally, which was following a previous study [32]. The authors opine that this difference is because the tendon fascicles tend to converge toward the midline before their attachment to the tibia. Although the measurements performed in a cadaveric approach is advantageous as they do not involve approximation and assumptions, the measurements obtained from images are more accurate and repeatable. A single technique is unlikely to be optimal in all circumstances. Therefore, we suggest that morphometric measurements from the cadaveric method and radiological methods could be integrated to provide optimum accuracy and desired reproducibility in clinical settings.
Limitations of the present study include the use of embalmed cadavers; the gender-wise difference could not be calculated due to the non-availability of female cadavers and the absence of data such as height or BMI of the cadavers. Although we found a correlation between patellar ligament length and thickness, we could not find detailed studies in the literature to correlate our findings and assumptions. Another limitation of the study was that, as two or more observers could not do the morphometric measurements, the inter-observer error of measurement could not be performed. Therefore the accuracy of measurements could not be reinforced.
Conclusion
The present cadaveric study is beneficial for local anthropological records and provides an essential reference guide for designing patellar prosthetic implants for the South Indian population. This morphometric data might be fundamental in understanding various knee conditions in situ and necessary to orthopedic surgeons for successful planning and execution for ACL reconstruction using patellar ligament graft and other patellofemoral joint disorders.
Author contributions
Protocol/project development: AAP, NK. Data collection: AAP, NK. Data analysis: MGL, VCS. Manuscript writing/editing: AAP, NK. All authors have read and approved the final version of the manuscript.
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal. Nil.
Availability of data and material
Data from human cadavers were used for the study.
Code availability
Not applicable.
Declarations
Conflict of interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Anderson AF, Snyder RB, Lipscomb AB. Anterior cruciate ligament reconstruction: a prospective randomized study of three surgical methods. Am J Sport Med. 2001;29:272–279. doi: 10.1177/03635465010290030201. [DOI] [PubMed] [Google Scholar]
- 2.Andrikoula S, Tokis A, Vasiliadis HS, Georgoulis A. The extensor mechanism of the knee joint: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2006;14:214–220. doi: 10.1007/s00167-005-0680-3. [DOI] [PubMed] [Google Scholar]
- 3.Butler DL, Grood ES, Noyes FR, Sodd AN. On the interpretation of our anterior cruciate ligament data. Clin Orthop Relat Res. 1985;196:26–36. [PubMed] [Google Scholar]
- 4.Chhaparwal R, Hiware S, Chhaparwal P, Chhaparwal N. Morphometric study of knee cap (patella) Ann Int Med Dent Res. 2018;4(6):AT05–AT09. [Google Scholar]
- 5.Chung CB, Skaf A, Roger B, Campos J, Stump X, Resnick D. Patellar tendon lateral femoral condyle friction syndrome: MR imaging in 42 patients. Skelet Radiol. 2001;30(12):694–697. doi: 10.1007/s002560100409. [DOI] [PubMed] [Google Scholar]
- 6.Dargel J, Gotter M, Mader K, Pennig D, Koebke J, Schmidt-Wiethoff R. Biomechanics of the anterior cruciate ligament and implications for surgical reconstruction. Strateg Trauma Limb Reconstr. 2007;2(1):1–12. doi: 10.1007/s11751-007-0016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duthon VB, Barea C, Abrassart S, et al. Anatomy of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14:204–213. doi: 10.1007/s00167-005-0679-9. [DOI] [PubMed] [Google Scholar]
- 8.Faraj AA, Nevelos AB. Ethnic factors in Perthes disease: a retrospective study among white and Asian population living in the same environment. Acta Orthop Belg. 2000;66(3):255–258. [PubMed] [Google Scholar]
- 9.Fox AJS, Wanivenhaus F, Rodeo SA. The basic science of the patella: structure, composition, and function. J Knee Surg. 2012;25(2):127–141. doi: 10.1055/s-0032-1313741. [DOI] [PubMed] [Google Scholar]
- 10.Garau G, Rittweger J, Mallarias P, Longo UG, Maffulli N. Traumatic patellar tendinopathy. Disabil Rehabil. 2008;30(20–22):1616–1620. doi: 10.1080/09638280701786096. [DOI] [PubMed] [Google Scholar]
- 11.Grelsamer RP, Weinstein CH. Applied biomechanics of the patella. Clin Orthop Relat Res. 2001;389:9–14. doi: 10.1097/00003086-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Harner CD, Baek GH, Vogrin TM, et al. Quantitative analysis of anterior cruciate ligament insertions. Arthroscopy. 1999;15:741–749. doi: 10.1016/S0749-8063(99)70006-X. [DOI] [PubMed] [Google Scholar]
- 13.Hijazi MM, Khan MA, Altaf FMN, Ahmed MR, Alkhushi AG, Sakran AMEA. Quadriceps tendon and patellar ligament; a morphometric study. Prof Med J. 2015;22(9):1192–1195. [Google Scholar]
- 14.Iranpour F, Merican AM, Cobb JP, Amis AA. The width: thickness ratio of the patella: an aid in knee arthroplasty. Clin Orthop Relat Res. 2008;466:1198–1203. doi: 10.1007/s11999-008-0130-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones KG. Reconstruction of the ACL using the central one-third of the patellar ligaments. A follow up reports. J Bone Jt Surg (Am) 1970;52A:1362–1368. [Google Scholar]
- 16.Kadir D, Necdet K, Levent E, Hasan O. Morphometry of the patellar ligament in human fetuses. SDU Typ Fak Derg. 2014;21(2):35–40. [Google Scholar]
- 17.Keays SL, Bullock-Saxton J, Keays AC, Newcombe P. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendinosus and gracilis. Knee. 2001;8:229–234. doi: 10.1016/S0968-0160(01)00099-0. [DOI] [PubMed] [Google Scholar]
- 18.Koyuncu E, Cankara N, Sulak O, Ozguner G, Albay S. The morphometry of patella and patellar ligament during the fetal period. Clin Anat. 2011;24:225–231. doi: 10.1002/ca.21075. [DOI] [PubMed] [Google Scholar]
- 19.Lee D, Bouffard JA. Ultrasound of the knee. Eur J Ultrasound. 2001;14(1):57–71. doi: 10.1016/S0929-8266(01)00146-X. [DOI] [PubMed] [Google Scholar]
- 20.Murugan M, Ambika S, Nim VK. Knee cap: a morphometric study. Int J Anat Res. 2017;5(1):3556–3559. doi: 10.16965/ijar.2016.451. [DOI] [Google Scholar]
- 21.Miller TT, Staron RB, Feldman F. Patellar height on sagittal MR imaging of the knee. AJR Am J Roentgenol. 1996;167:339–341. doi: 10.2214/ajr.167.2.8686598. [DOI] [PubMed] [Google Scholar]
- 22.Mologne TS, Friedman MJ. Graft options for ACL reconstruction. Am J Orthop. 2000;29:845–853. [PubMed] [Google Scholar]
- 23.Olateju OL, Philander I, Bidmos MA. Morphometric analysis of the patella and patellar ligament of South Africans of European ancestry. S Afr J Sci. 2013;109(9/10):1–5. doi: 10.1590/sajs.2013/20130069. [DOI] [Google Scholar]
- 24.Philips CL, Silver DAT, Schranz PJ, Mandalia V. The measurement of patellar height: a review of the methods of imaging. J Bone Jt Surg Br. 2010;92B:1045–1053. doi: 10.1302/0301-620X.92B8.23794. [DOI] [PubMed] [Google Scholar]
- 25.Phoophalee P, Prasitwattanaseree S, Riengrojpitak S, Mahakkanukrauh P (2012) Sex determination by patella measurement in Thais. In: Proceedings of the 1st ASEAN plus three graduate research congress, pp 472–477
- 26.Portner O, Pakzad H. The evaluation of patellar height: a simple method. J Bone Jt Surg Am. 2011;93:73–80. doi: 10.2106/JBJS.I.01689. [DOI] [PubMed] [Google Scholar]
- 27.Potage D, Duparc F, D’Utruy A, Courage O, Roussignol X. Mapping the quadriceps tendon: an anatomic and morphometric study to guide tendon harvesting. Surg Radiol Anat. 2015;37(9):1063–1067. doi: 10.1007/s00276-015-1486-8. [DOI] [PubMed] [Google Scholar]
- 28.Schlenzka D, Schwesinger G. The height of the patella: an anatomical study. Eur J Radiol. 1990;11:19–21. doi: 10.1016/0720-048X(90)90097-U. [DOI] [PubMed] [Google Scholar]
- 29.Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB. A prospective randomized comparison of patellar tendon verses semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:214–220. doi: 10.1177/03635465020300021201. [DOI] [PubMed] [Google Scholar]
- 30.Shang P, Zhang L, Hou Z, Bai X, Ye X, Xu Z, Huang X. Morphometric measurement of the patella on 3D model reconstructed from CT scan images for the southern Chinese population. Chin Med J. 2014;127:96–101. [PubMed] [Google Scholar]
- 31.Standring S (2008) Upper arm. In: Gray’s anatomy, 40th edn. Elsevier Churchill Livingstone, Edinburgh, pp 1394–1396
- 32.Toumi H, Higashiyama I, Suzuki D, Kumai T, Bydder G, McGonagle D, Emery P, Fairclough J, Benjamin M. Regional variations in human patellar trabecular architecture and the structure of the proximal patellar tendon enthesis. J Anat. 2006;208(1):47–57. doi: 10.1111/j.1469-7580.2006.00501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yoo JH, Yi SR, Kim JH. The geometry of patella and patellar tendon measured on knee MRI. Surg Radiol Anat. 2007;29(8):623–628. doi: 10.1007/s00276-007-0261-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data from human cadavers were used for the study.
Not applicable.