Abstract
Objective: This study aimed to emphasize facilitation training and strengthening of abdominal and core muscles in improving the inter-recti distance (IRD) and associated low back pain (LBP) among young postpartum females.
Materials and methods: A single-blinded randomized controlled trial, among forty young postpartum females, was conducted at a community health center. The females were divided into two equal groups through the envelope method where Group A received abdominal crunch training protocol whereas group B received double straight leg raise (DSLR) exercise protocol for 6 weeks and pre and post IRD and Oswestry disability index (ODI) scores were recorded.
Results: Group A showed improvement in IRD with a mean difference of 1.95±0.4 whereas in group B it was found to be 2.85±0.35 when assessed through finger palpation method. The mean difference of IRD, when measured through digital nylon caliper method in abdominal crunch and DSLR exercise group was 4.06±0.74 and 1.2±0.49 respectively. Moreover, ODI scores of group A were 2.70±1.05 whereas, group B scores were found to be 1.1±0.06 showing that LBP reduced in participants who performed abdominal crunch exercise.
Conclusion: This study reveals that 6 weeks of exercise protocol was observed to be effective in the management of DRA. Thus, abdominal crunch exercise seemed to produce promising results in a reduction of IRD and associated LBP.
Key Words: Rectus Abdominis, Low Back Pain, Physical Activity, Pelvic Floor, Postpartum Period, Pregnancy
Introduction
Globally, one of the most predominant health concerns that develop during pregnancy and early postpartum period accounts for diastasis rectus abdominis (DRA) that is experienced by females during the third trimester of pregnancy and nearly half of females come across it immediately post-delivery (1). DRA is a separation of the muscle flaps of the rectus abdominis muscle that happens as a consequence of sustained and prolonged stresses on linea alba (2). The two bellies of the rectus abdominis muscle are oriented anatomically in such a manner that they run parallel to each other and are connected by linea alba which is a connective tissue along the midline of the body (3). During the period of pregnancy, various hormonal changes occur followed by the softening and expansion of linea alba that accommodates the increasing weight of the growing fetus because of enlarged inter-recti distance (IRD) (4). The separation between the two muscle bellies is considered clinically significant if the distance between rectus abdominis muscles increases from greater than 2 finger-width or 2cm (5). Multiple factors were found to be evident behind the causes of DRA among females like pregnancy, old age, increased intra-abdominal pressure and weight lifting out of which increased abdominal pressure during pregnancy is the most common factor that affects 60% of women at 6 months of post-partum (6). As the pregnancy progresses, hormonal variations occur coupled with advancing stresses due to the weight of the fetus placed on abdominal muscles and soft tissue structures owing to their weakness resulting in stretching and in some cases lead to a slit on the linea alba leading to DRA (6). It poses several complications in females among which lower back pain is the most evident (5). Other complications include disturbed trunk stability and mobility, pelvic pain, disturbed posture, and pelvic floor dysfunction (5). This pain is believed to negatively impact the ADLs of these females rendering to minimal social life and traveling (5). The functional status of the patients with LBP can be identified using patient-reported questionnaires used to measure back-specific functional status (5). Oswestry disability index (ODI) is considered the gold standard for measuring disability and quality of life (QOL) for adults having low back pain (LBP) (7). DRA leads to several biomechanical constraints among which diminished mechanical control of the abdomen is considered to be a major problem (8). Along with this, females suffering from DRA also experience restrictions while performing trunk flexion, rotation as well as side bending (8). Such females also develop respiratory difficulty and disturbed support of abdominal viscera (5). The development of DRA causes the abdominal muscles to be found at a biomechanical disadvantage which successively diminishes the ability to stabilize the pelvis (9). The females are therefore prone to the progression of back pain on account of ligamentous laxity and supplementary load placed on the body (10). This causes the loss of integrity, and the mechanical control and functional strength of the abdominal wall are reduced, which eventually leads to DRA (10). This in turn worsens LBP and pelvic instability (11). DRA resolves spontaneously in the majority of females during the postpartum period whereas, strategies for DRA management comprise both conservative and surgical approaches but the widely used intervention strategy is exercise-based physical therapy intervention (12). Conservative treatment strategies involve daily functional activities and exercise regimes along with back care (12). Multiple physical therapies based interventional strategies and exercises are widely been used in physical therapy setups for the management of DRA (12). In the absence of efficacy of the conservative treatment, with high aesthetic and/or functional discomfort or the presence of a hernia, surgical intervention is often used (13). Abdominoplasty is a surgical procedure that has been used to treat severe cases of DRA that is a cosmetic procedure also referred commonly as a Tummy tuck (13). Physical therapy for the management of DRA includes several choices (14). The conventional management options include daily functional activities along with back care, corset or bracing; tupler technique, faradic electrical stimulation in conjunction with exercises (14). Exercises seem to offer numerous physical and psychological benefits to the body and help to maintain healthy body weight and avoid the accumulation of fat in the body (15). Abdominal exercises have proven to bring the left and right sides of the rectus abdominis muscle and diminish the load on the stomach or back (16). Moreover, double SLR exercise performed by gradually lifting the legs to 30ᴼ and then lowering extended legs back to plinth can improve abdominal strength without any detrimental effects (17). Hence, the present study is anticipated to show an early reduction of DRA through abdominal and core muscle exercises to reduce LBP in females during their post-partum period (17).
Hence, this study aimed to identify the impact of a combination of exercise strategies in the management of DRA. Therefore, in this investigation emphasis is placed on facilitation training and abdominal and core muscle strengthening to discover effects on improvement of IRD in the postnatal population. Furthermore, long-term complications caused by the condition that includes trunk instability and limited mobility, LBP, disturbed posture, pelvic floor dysfunction, and pain leading to hernia in severe cases will be deterred and the functional status of the affected females will be improved.
Materials and methods
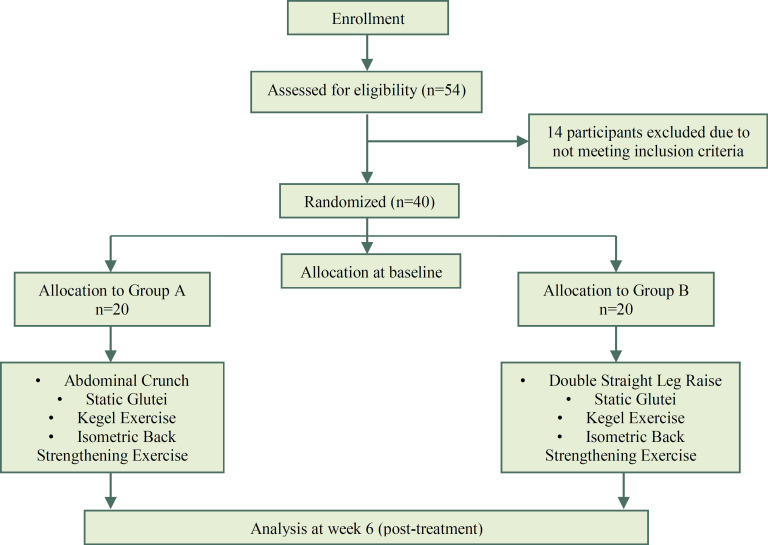
The ethical review committee of Ziauddin University had approved this study (med/sh/25/20). A randomized controlled trial was conducted at a community health care of an underprivileged area. Participants included were 3 months post-partum females who had vaginal or cesarean delivery with the presence of DRA >2 finger width and >2cm whereas, patients who had any pregnancy-induced condition like polyhydramnios, gestational hypertension, trauma to bowel or bladder, or any neurologic disease and its associated balance disorders, fetal microsomia and pelvic or abdominal surgery (except for a cesarean section) were considered as the exclusion criteria of this study. Forty participants were selected and the subjects were initially screened according to the standards formulated for this research. All of them were asked to fill a consent form after they were given a detailed explanation regarding the purpose of the study. The envelope technique was used for randomization and afterward exercise programs were administered by a trained Physical therapist. The details are illustrated in Figure 1.
Figure 1.
Framework of methodology as per the CONSORT Guidelines
Data was collected using the Finger palpation method, digital nylon calipers, and Oswestry Disability Index. Parameters of the exercise protocol were adapted from the American College of Sports Medicine. Training protocol includes 6 weeks of core strengthening exercises. The participants performed exercises on 3 alternate days for 6 weeks. Three sets with 10 repetitions of each exercise were performed in a training session. Participants in group A were asked to perform Abdominal crunches, Static glutei, Kegels, and Isometric back strengthening exercises while group B participants performed Double straight leg raise, Static glutei, Kegels, and Isometric back strengthening exercise. The initial readings of IRD were calculated through finger palpation and digital nylon caliper method at the beginning of the training program along with the values of ODI for the quantification of LBP.
Finger Palpation Method: The participants were advised to lie in a crook lying manner with the head and feet resting on the plinth along with a cushion positioned underneath. The subjects were asked to raise the head and shoulder off the plinth simultaneously touching the knees with the outstretched arm until the scapular spine cleared the surface. The therapist then palpated with the fingers on the participant’s linea alba horizontally. The finger-width fitted the distance between the internal borders of two rectus abdominal muscles.
The result was documented as per the number of fingers that could be placed between the muscle bellies. The center of the umbilicus was taken as a reference point; measurements were taken over the umbilicus, 2cm above and 2cm below the umbilicus. The procedure was repeated thrice and then the mean was recorded. As the process was completed, the subject was requested to return to her normal position. The readings were taken on weeks 0 and 6th.
Digital Nylon Caliper: IRD was measured through Digital Nylon Caliper and the subjects were instructed to acquire a crook-lying position. The head and feet of the subject are resting on the couch and a pillow is placed underneath whereas the arms were resting parallel to the body. The standard measurement locations were considered to be the umbilicus which served as the midpoint. Other desired measurement points included 4.5cm above and below the midpoint. The participants were then asked to perform partial curl up by raising the head while simultaneously crossing the arms over the chest and reaching forward towards the knees with outstretched arms. This position was maintained until the spine of the scapulae cleared the table surface. The subjects sustained the curl-up position meanwhile; medial borders of rectus abdominis muscles were palpated by the therapist. The measurement jaws of the digital nylon caliper were set perpendicular to the direction of muscles and eventually adjusted to perceive IRD width. The measurement locations were over, above, and below the umbilicus. Once the measurement was completed, the subjects were asked to return to resting position. The subjects were permitted to relax between measurements or at any point of fatigue. DRA is classified into four categories based on the distance between the two bellies of rectus abdominis muscle measured using a Digital Nylon caliper method, however the separation between the two bellies at or below the level of umbilicus if found to be less than 2.5cm, the patient was considered to be normal whereas, the values of the separation of the two bellies if found to be >2.5cm and <3.5cm condition was classified as mild and for moderate and severe conditions, the identified values were >3.5cm and <5cm and >5.0cm respectively (18).
ODI: For the quantification of LBP, an ODI questionnaire was used. The questionnaire is designed to be a self-reported survey, where patients suffering from LBP come across limitations in Activities of Daily Living (ADL’s) in several health constructs like personal care, lifting, walking, sitting, standing, sleeping, sexual life, social life, and traveling. The patients indicated the effect of pain on activities. The questions having a score range from 0 to 5, giving a maximum total score of 50.
The total score was then converted into a percentage by multiplying it by 2. Based on the collective responses, a score out of 100% was calculated, where a higher percentage equated to a greater level of disability. A score 0 to 20 equals a minimal level of disability, similarly, any score falling between 21 to 40 equals to moderate level of disability, 41 to 60 is for severe disability, 61 to 80 for crippling back pain and eventually scores between 81 to 100 will be for a bed-bound patient.
The data were analyzed using MedCalc Statistical Software version 19.0.5. The demographic details were illustrated using a frequency and percentage descriptive analysis. As the data was found to be normally distributed, paired t-test was run for within the group analyses and an independent t-test was run for between the group analyses. The level of significance was maintained at 0.05 at 95% of CI.
Results
Baseline Demographic Analysis: The baseline data shows a mean age of 29.8±4.1 in group A whereas 30.2±4.3 years in group B. Normal adults were found to be normal, BMI=23.4±2.5 whereas overweight population was found in group B= 26.8±3.5. Interestingly, only 12 out of 20 females were breastfeeding in group A whereas a lesser number of females were documented in group B (9 out of 20). The details of the demographic are represented in Table 1.
Table 1.
Demographic Characteristics of post-partum females with Diastasis Recti Abdominus
| Characteristic (Mean±SD) | Group-A | Group-B |
|---|---|---|
| No. of Participants | 20 | 20 |
| Age (year) | 29.8±4.1 | 30.2±4.3 |
| Weight (kg) | 65.2±5.8 | 63.2±7.2 |
| Height (cm) | 165.8±5.2 | 158.3±4.9 |
| BMI (kg/m2) | 23.4±2.5 | 26.8±3.5 |
| Time since delivery (days) | 88.4±56.2 | 68.43 ±37.20 |
| Breast feeding (n) | 12 | 9 |
| Physical Activity for at least 30 min, 3 times/week n (%) |
122 (68.7) | 65 (73.5) |
BMI: Body Mass Index
As the data is normally distributed therefore paired t test was run for both the intervention strategies.
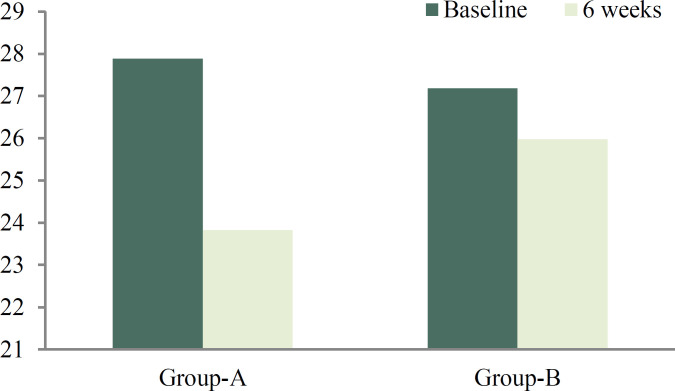
As observed, the mean score significantly improved in females performing both Abdominal Crunch as well as DSLR (FP: AC, inter-recti distance: pre= 3.05+0.22 post= 1.95+0.4 versus DSLR: pre: 3.00±0.01, post: 1.95±0.36). However, the mean difference was found to be highest in the AC Digital Caliper: 4.06 ± 0.74, whereas the FP showed higher mean difference 2.85±0.35 in the DSLR as shown in Table 2. The significant difference was observed in the inter-recti distance after 6 weeks of training using the digital nylon caliper represented in Figure 2.
Table 2.
The pre-post analysis of interrecti distance using Finger Palpation Method and Digital Nylon Caliper and low back pain measured through ODI among females with Diastasis Recti Abdominus
| N | Baseline | 6 Weeks | mean±SD | 95% of CI | P value (<0.05) | ||
|---|---|---|---|---|---|---|---|
| Finger Palpation Method | Group-A | 20 | 3.05±0.22 | 1.95±0.4 | 1.95±0.18 | -1.28 to -0.91 | *<0.001 |
| Group-B | 20 | 3.00±0.01 | 1.95±0.36 | 2.85±0.35 | -0.36 to 0.06 | 0.046 | |
| Digital Nylon Caliper | Group-A | 20 | 27.89±1.69 | 23.83±0.95 | 4.06±0.74 | -4.97 to -3.15 | *<0.001 |
| Group-B | 20 | 27.18±1.28 | 25.98±0.79 | 1.2±0.49 | -0.12 to 0.004 | *<0.001 | |
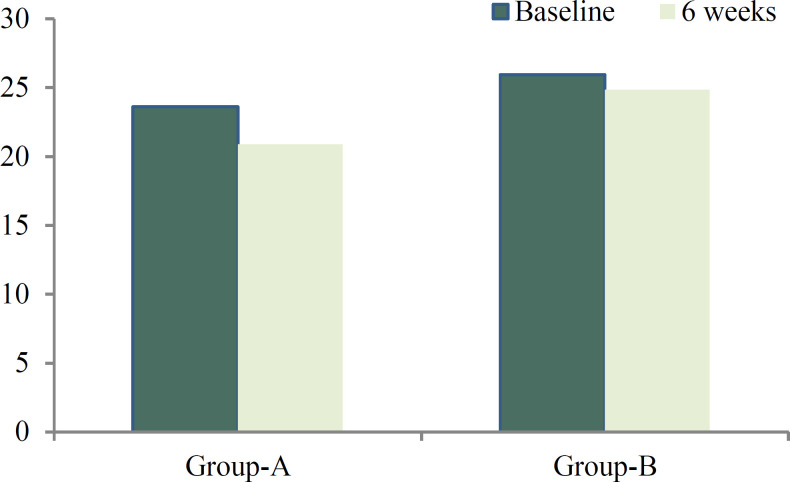
| Oswestry Disability Index | Group-A | 20 | 23.60±2.74 | 20.90±1.69 | 2.70±1.05 | -3.77 to -1.62 | *<0.001 |
| Group-B | 20 | 25.95±3.77 | 24.85±3.71 | 1.1±0.06 | -0.44 to 0.040 | *<0.001 |
The pre-post analysis of interrecti distance using Finger Palpation Method and Digital Nylon Caliper and low back pain measured through ODI among females with Diastasis Recti Abdominus,
Significant p-value<0.05.
Figure 2.
representing the pre and post inter-recti difference among post-partum females with DRA
Between the group analysis was performed using Independent t test revealing a significant difference in reducing low back pain p <0.05 (at 95% of CI, t= 4.31 p<0.001) as represented in Table 3.
Table 3.
Post-Mean Comparison of Group-A and B for inter-recti distance and low back pain among post-partum females
| Variables | n | mean±SD | Test t |
P value
(<0.05) |
| Finger Palpation Method | 20 | 1.95±0.4 | 7.48 | *<0.001 |
| Digital Nylon Caliper | 20 | 2.85±0.36 | 7.77 | *<0.001 |
| Oswestry Disability Index | 20 | 3.95±2.02 | 4.31 | *0.001 |
Significant p-value<0.05.
The bar graph shows a significant improvement in group A ODI pre: 23.60±2.74; post 20.90±1.69; where is group B ODI pre: 25.95±3.77; post 24.85±3.71 (Figure 3) with a mean difference of 3.95±2.02 where level of significance is p<0.05.
Figure 3.
Illustrating the graphical representation of Oswestry Disability Index of group A and group B
Discussion
DRA, a prevalent condition that occurs mostly in post-partum females causing major health concerns if not treated properly. LBP and disturbed QOL are among the primary consequences triggered by DRA. The main purpose of this research was to highlight the impact of a specially designed 6-week exercise training protocol. The outcome measures for this study included IRD measurement through Finger palpation and the Digital Nylon Caliper method. LBP was quantified and its effects were assessed through a questionnaire termed as Oswestry Disability Index (ODI). A research was conducted in 2016 in which the author worked on DRA evaluation through finger palpation and digital nylon caliper method (16). Khandale et al. in a study used two different techniques for evaluation of diastasis recti consisting of finger palpation and digital caliper method (18). Mota et al. 2016 in their study affirm that finger palpation has sufficient reliability to be used in clinical practice and subsequently, in 2013, a researcher stated that digital nylon caliper is a reliable and valid tool for measuring IRD (19).
Abdominal crunches performed by participants in our study produced significant results. The mechanism of these exercises that lead to the correction of muscular defect has been explained that abdominal contraction increases pressure and converts the abdomen into a rigid cylinder that increases the stability of the spine, improves abdominal strength, and decreases abdominal separation (20). Abdominal muscle facilitation, stabilization, and concentric activation were followed by these exercises (20). The objective of our study is to incorporate abdominal exercises as they can escort the two flaps of the rectus abdominis muscle together and minimize the additional stress on the trunk or back. Therefore, strengthening exercises for abdominals are suggested to be followed during the postnatal period, predominantly to lessen IRD. Another literature shows that posterior pelvic tilt exercise did not produce abdominal bulging when performed (21). Similarly, this study also made use of the aforementioned outcome measures due to their reliability and validity. Digital nylon calipers are also used to measure IRD. According to Chiarello et al., it is a reliable and valid tool for measuring IRD (13). This equipment has adequate intra-rater reliability having an intraclass correlation coefficient (ICC) of 0.78-0.97 (22). Whereas; ODI shows good construct validity and has been used as the standard of comparison for other outcome measures assessing LBP-induced disability. Internal consistency is acceptable as Cronbach α ranges from 0.741 to 0.87. Test-retest reliability is high as the values range from r = 0.83 to 0.99 and vary according to the time interval between measurements. ICC values range from 0.84 to 0.94 (23-27).
In our study, isometric back strengthening exercise was performed by the participants that in turn caused posterior pelvic tilting and hence, resulted in reduced LBP without causing muscular separation of abdominals. Similarly, DSLR exercise was performed by participants in group B in which the lower leg is slowly lifted to 30ᴼ and subsequently extended to bed (16). The results of the study performed by Khandale et al revealed that DSLR can increase abdominal strength without any harmful effects (18). Similar to this finding, the results seemed to be significant and the closure of DRA was evident upon assessment through the nylon caliper method after 6 weeks of training received by group B. Whereas, IRD decreased in group A subjects who performed abdominal crunch exercise, which suggests that abdominal strengthening exercise contributes to the narrowing of IRD in postpartum women. Additionally, LBP seemed to decrease in group A and B females when pre and post ODI scores were compared on week 0 and 6.
Our study shows that abdominal crunch and DSLR exercise proved beneficial in reducing IRD after 6 weeks of intervention (p<0.001). Statistical comparison was performed to evaluate the efficiency of Abdominal crunch and DSLR exercise which highlighted the fact that abdominal crunch exercise produced better results than DSLR exercise based on outcome measures. The mean difference of IRD on finger palpation method in an abdominal crunch and DSLR exercise group was 1.95±0.18 and 2.85±0.35 whereas, the mean difference of IRD when measured through nylon caliper method in an abdominal crunch and DSLR exercise group was 4.06±0.74 and 1.2±0.49 respectively which affirms the finding. Moreover, ODI scores of group A were 2.70±1.05 whereas, group B scores were found to be 1.1±0.06 showing that LBP reduced at a better rate in participants who performed abdominal crunch exercise. The findings of our study were significant but a few delimitations still exist. The sample size of this study was small (n=40) due to which the results may not be generalized. The parity of females was not fixed as the development of DRA is more likely to occur in multiparous women whereas, in nulliparous females, the incidence is comparatively less.
This study will prove beneficial to the post-partum female population to follow the guidelines of exercise as imparted through this research. The research is innovative particularly for the Asian population as other literature of similar nature has not compared abdominal crunch and DSLR exercises. Moreover, clinicians will pay more attention to the condition, its assessment and will refer the patients for physical therapy management of the said condition.
The basic findings of this study may be used in the future with a large sample size for validation of results. Along with this, the follow-up period of the study may also be included to better understand the long-term influence of the exercise regime. Additionally, further researches should as well aim at producing prolonged effects of abdominal exercises in postpartum females alongside biofeedback or muscular stimulation may be utilized. To carry out advanced studies on DRA, innovative exercise protocols may be integrated to observe and compare the effects on post-natal women.
Conclusion
This 6-week long randomized controlled study determined significant relationships between DRA measurement, LBP, and ODI scores. Generally, better results were shown by females in group A who performed abdominal crunch exercise as compared to group B females who performed DSLR exercise.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interests
Authors have no conflict of interests.
Notes:
Citation: Saleem Z, Khan AA, Farooqui SI, Yasmeen R, Rizvi J. Effect of Exercise on Inter-Recti Distance and Associated Low Back Pain Among Post-Partum Females: A Randomized Controlled Trial. J Family Reprod Health 2021; 15(3): 202-9.
References
- 1.Benjamin D, van de Water A, Peiris C. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014;100:1–8. doi: 10.1016/j.physio.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Gunnarsson U, Stark B, Dahlstrand U, Strigård K. Correlation between Abdominal Rectus Diastasis Width and Abdominal Muscle Strength. Dig Surg. 2015;32:112–6. doi: 10.1159/000371859. [DOI] [PubMed] [Google Scholar]
- 3.Mommers E, Ponten J, Al Omar A, de Vries Reilingh T, Bouvy N, Nienhuijs S. The general surgeon’s perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc. 2017;31:4934–49. doi: 10.1007/s00464-017-5607-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Köckerling F, Botsinis M, Rohde C, Reinpold W. Endoscopic-Assisted Linea Alba Reconstruction plus Mesh Augmentation for Treatment of Umbilical and/or Epigastric Hernias and Rectus Abdominis Diastasis – Early Results. Front Surg. 2016:3. doi: 10.3389/fsurg.2016.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benjamin D, Frawley H, Shields N, van de Water A, Taylor N. Relationship between diastasis of the rectus abdominis muscle (DRAM) and musculoskeletal dysfunctions, pain and quality of life: a systematic review. Physiotherapy. 2019;105:24–34. doi: 10.1016/j.physio.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Acharry N, Kutty R. Abdominal Exercise with Bracing, A Therapeutic Efficacy in Reducing Diastasis-Recti Among Postpartal Females. Int J Physiother. 2015;3:999–1005. [Google Scholar]
- 7.Yates M, Shastri-Hurst N. The Oswestry Disability Index. Occup Med (Chic Ill) 2017;67:241–2. [Google Scholar]
- 8.Thabet A, Alshehri M. Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: a randomised controlled trial. J Musculoskelet Neuronal Interact. 2019;19:62–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Sperstad J, Tennfjord M, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50:1092–6. doi: 10.1136/bjsports-2016-096065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kato S, Murakami H, Demura S, Yoshioka K, Shinmura K, Yokogawa N, et al. Abdominal trunk muscle weakness and its association with chronic low back pain and risk of falling in older women. BMC Musculoskelet Disord. 2019;20:273. doi: 10.1186/s12891-019-2655-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Capitano S. Laparoscopic transabdominal preperitoneal approach for umbilical hernia with rectus diastasis. Asian J Endosc Surg. 2017;10:334–5. doi: 10.1111/ases.12365. [DOI] [PubMed] [Google Scholar]
- 12.Nahabedian M. Management Strategies for Diastasis Recti. Semin Plast Surg. 2018;32:147–154. doi: 10.1055/s-0038-1661380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giridharan G. Effectiveness of Exercise in Treating Rectus Abdominis Diastasis. Biomedicine (Taipei) 2019;38 [Google Scholar]
- 14.Nahabedian M, Nahabedian A. Closing the gap for patients with rectus abdominis diastasis. Nursing. 2018;48:49–52. doi: 10.1097/01.NURSE.0000527601.09592.14. [DOI] [PubMed] [Google Scholar]
- 15.Michalska A, Rokita W, Wolder D, Pogorzelska J, Kaczmarczyk K. Diastasis recti abdominis - a review of treatment methods. Ginekol Pol. 2018;89:97–101. doi: 10.5603/GP.a2018.0016. [DOI] [PubMed] [Google Scholar]
- 16.Lalingkar R, Gosavi P, Jagtap V, Yadav T. Effect of Electrical Stimulation Followed by Exercises in Postnatal Diastasis Recti Abdominis. IJHSR. 2019;9:88–92. [Google Scholar]
- 17.Kamel D, Yousif A. Neuromuscular Electrical Stimulation and Strength Recovery of Postnatal Diastasis Recti Abdominis Muscles. Ann Rehabil Med. 2017;41:465. doi: 10.5535/arm.2017.41.3.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khandale S, Hande D. Effects of Abdominal Exercises on Reduction of Diastasis Recti in Postnatal Women. IJHSR. 2016;6:182–91. [Google Scholar]
- 19.Mota P, Pascoal AG, Sancho F, Carita AI, Bø K. Reliability of the inter-rectus distance measured by palpation. Comparison of palpation and ultrasound measurements. Man Ther. 2013;18:294–8. doi: 10.1016/j.math.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 20.Reinpold W, Köckerling F, Bittner R, Conze J, Fortelny R, Koch A, et al. Classification of Rectus Diastasis-A Proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS) Front Surg. 2019:6. doi: 10.3389/fsurg.2019.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chiarello C, McAuley J. Concurrent Validity of Calipers and Ultrasound Imaging to Measure Interrecti Distance. J Orthop Sports Phys Ther. 2013;43:495–503. doi: 10.2519/jospt.2013.4449. [DOI] [PubMed] [Google Scholar]
- 22.Van de Water A, Benjamin D. Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM): A systematic review of their measurement properties and meta-analytic reliability generalisation. Man Ther. 2016;21:41–53. doi: 10.1016/j.math.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 23.Kim E, Lee H. The Effects of Deep Abdominal Muscle Strengthening Exercises on Respiratory Function and Lumbar Stability. J Phys Ther Sci. 2013;25:663–5. doi: 10.1589/jpts.25.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Werner L, Dayan M. Diastasis Recti Abdominis-diagnosis, Risk Factors, Effect on Musculoskeletal Function, Framework for Treatment and Implications for the Pelvic Floor. Current Women’s Health Reviews. 2019;15:86–101. [Google Scholar]
- 25.Denteneer L, Van Daele U, Truijen S, Hertogh W, Meirte J, Deckers K et al. The Modified Low Back Pain Disability Questionnaire. Spine (Phila Pa 1976) 2018;43:E292–E298. doi: 10.1097/BRS.0000000000002304. [DOI] [PubMed] [Google Scholar]
- 26.Fairbank J, Pynsent P. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940–53. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 27.Davidson M, Keating J. A Comparison of Five Low Back Disability Questionnaires: Reliability and Responsiveness. Phys Ther. 2002;82:8–24. doi: 10.1093/ptj/82.1.8. [DOI] [PubMed] [Google Scholar]