Abstract
Diabetic retinopathy (DR) is a complication of diabetes and one of the leading causes of vision loss worldwide. Despite extensive efforts to reduce visual impairment, the prevalence of DR is still increasing. The initial pathophysiology of DR includes damage to vascular endothelial cells and loss of pericytes. Ensuing hypoxic responses trigger the expression of vascular endothelial growth factor (VEGF) and other pro-angiogenic factors. At present, the most effective treatment for DR and diabetic macular edema (DME) is the control of blood glucose levels. More advanced cases require laser, anti-VEGF therapy, steroid, and vitrectomy. Pan-retinal photocoagulation for non-proliferative diabetic retinopathy (NPDR) is well established and has demonstrated promising outcomes for preventing the progressive stage of DR. Furthermore, the efficacy of laser therapies such as grid and subthreshold diode laser micropulse photocoagulation (SDM) for DME has been reported. Vitrectomy has been performed for vitreous hemorrhage and tractional retinal detachment for patients with PDR. In addition, anti-VEGF treatment has been widely used for DME, and recently its potential to prevent the progression of PDR has been remarked. Even with these treatments, many patients with DR lose their vision and suffer from potential side effects. Thus, we need alternative treatments to address these limitations. In recent years, the relationship between DR, lipid metabolism, and inflammation has been featured. Research in diabetic animal models points to peroxisome proliferator-activated receptor alpha (PPARα) activation in cellular metabolism and inflammation by oral fenofibrate and/or pemafibrate as a promising target for DR. In this paper, we review the status of existing therapies, summarize PPARα activation therapies for DR, and discuss their potentials as promising DR treatments.
Keywords: diabetic retinopathy, diabetic macula edema, anti-VEGF therapy, vitrectomy, laser photocoagulation, fenofibrate, pemafibrate
1. Introduction
Diabetic retinopathy (DR) is a severe complication of diabetes mellitus (DM) and is one of the leading causes of vision loss worldwide. The Vision Loss Expert Group (VLEG) reported that DR accounted for 1.25% of moderate to severe visual impairment and 1.07% of blindness [1]. A meta-analysis reviewed that the percentage of blindness caused by DR varied regionally from 2% in Oceania and East and Southeast Asia to 5.5% in Southern Latin America [2]. They also reported that DR caused blindness in regions with older populations, such as Eastern and Western Europe and Southern Latin America, compared to regions with relatively younger populations [2]. Regarding the type of DM, DR is observed in 42.1% of type 1 DM and 25.5% of type 2 DM [3]. Another study showed that type 1 DM patients were diagnosed with DR in 32.58% of cases, while type 2 DM patients were 23.04% of cases [4]. DR represents a dramatic socioeconomic cost for healthcare systems, and its prevalence has continuously increased in the aging society [5,6,7,8]. The public health burden of DR underlines the significance of searching for promising therapeutic approaches, as well as the advancement of current standards of DR care, including laser, anti-vascular endothelial growth factor (VEGF) therapy, steroid, and vitrectomy [9]. Although surgical or pharmacological therapeutic approaches in DR have been improved, the pathological mechanisms of DR have yet to be fully elucidated. In this study, we review the current proposed pathophysiology of DR and the status of existing surgical and/or pharmacological therapies. Furthermore, we summarize recent promising oral therapies in diabetes; fenofibrate and pemafibrate, well-known agonists of peroxisome proliferator-activated receptor alpha (PPARα) in treatments for dyslipidemia [10] and discuss their recent potentials as promising oral DR treatments.
2. Pathophysiology of DR
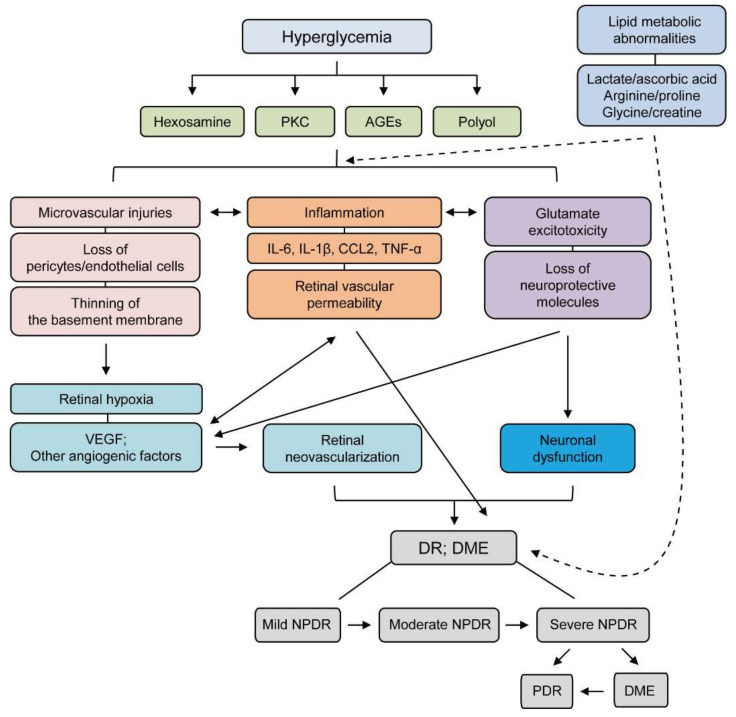
To date, there have been various insights into the pathophysiology of DR (Figure 1). Firstly, it was simply considered a microvascular disease [11], and hyperglycemia was thought to be the leading cause of retinal microvascular damage [12]. In this regard, pathological metabolic pathways such as accumulation of advanced glycation end products (AGEs) and induction of the protein kinase C (PKC), the polyol, and the hexosamine pathways have been implicated in retinal microvascular damage [13,14].
Figure 1.
A schematic illustration of the pathophysiology and stages of diabetic retinopathy (DR). Hyperglycemia evokes various pathological metabolic mechanisms such as accumulation of AGEs and induction of PKC, the polyol, and the hexosamine pathways. Microvascular injuries, inflammation, and glutamate excitotoxicity combine to damage the diabetic retina more severely after induction of these pathways. During these processes, representative features are highlighted: loss of pericytes/endothelial cells, thinning of the basement membrane, increases in IL-6, IL-1β, CCL-2, and TNF-α, retinal vascular permeability, and loss of neuroprotective molecules. These outcomes exacerbate neuronal dysfunction, retinal hypoxia, and increases in various angiogenic factors, including VEGF, which ultimately causes retinal neovascularization. All processes are inter-connected to the development and progression of DR. Furthermore, lipid metabolic abnormalities (changes in levels of lactate, ascorbic acid, arginine, proline, glycine, or creatine) in diabetes could aggravate the intensities of retinal injuries. The stages of DR depending on the severity of the disease: mild NPDR (microaneurysm), moderate NPDR (hemorrhage), severe NPDR (more severe hemorrhage, venous beading, and intraretinal microvascular abnormalities), PDR (new vessel formation, retinal detachment, and vitreous hemorrhage); DME (retinal detachment). Solid line; direct interaction, Dash line; indirect interaction. AGEs; advanced glycation end products, PKC; protein kinase C, CCL; Chemokine (C-C motif) ligand TNF; tumor Necrosis Factor, VEGF; vascular endothelial growth factor, DR; diabetic retinopathy, DME; diabetic macular edema, NPDR; non-proliferative diabetic retinopathy.
In the early stage of DR, loss of pericytes can lead to the eventual destruction of the microvasculature, as these cells physiologically enwrap the microvasculature and support endothelial cells [15]. Disturbing the interaction of pericytes with endothelial cells showed aggravation in diabetes-induced microvascular dysfunction [16]. Experimental studies showed that hyperglycemia caused the death of pericytes in vitro and in vivo [17,18]. Additionally, endothelial cell death and thinning of the basement membrane were also described in the early stage of DR [19,20]. Loss of pericytes and endothelial cells can cause capillary occlusion, which leads to retinal ischemic conditions.
Retinal ischemic conditions could lead to more severe stages in DR. Retinal ischemia induces increases in VEGF levels [21,22,23], and VEGF takes part in the mechanism that restores the blood supply to the ischemic retina. This process damages the retina more severely, termed neovascularization-induced retinal damages, and may cause the retina to wrinkle or detach [24,25]. The boundary between proliferative diabetic retinopathy (PDR) and non-PDR (NPDR) is determined by the condition of neovascularization (Figure 1). Neovascularization usually occurs at the vitreoretinal interface [26]. In some cases of NPDR, diabetic macular edema (DME) occurs as a complication. The macula in DME swells with fluid leaked from the damaged vasculature [27]. These conditions from PDR or DME are often related to the development of retinal detachment and vitreous hemorrhage leading to loss of vision in DR patients [27]. Accordingly, research scientists and clinicians have focused on controlling VEGF in DR experimentally and clinically, as they recognized the importance of its principle pathological role [21,23]. Several studies showed that upregulation of VEGF could be mediated by hypoxia-inducible factors (HIFs) [28]. Genes regulated by HIFs (angiogenin-2; ANGIO2, stromal-derived growth factor-1; SDF-1, and platelet-derived growth factor-B; PDGF-B) also play critical roles in retinal neovascularization [29,30]. Therefore, the regulation of HIFs with VEGF and other angiogenic genes has been targeted for the treatment of DR.
Retinal inflammation, as well as retinal degeneration, can be detected from the early stage to the chronic stage in DR. Elevation in various inflammatory cytokines and chemokines (monocyte chemoattractant protein 1/chemokine C-C motif ligand 2; MCP-1/CCL2, tumor necrosis factor-α; TNF-α, interleukin 1β; IL-1β, interleukin 6; IL-6) were described in the serum as well as the vitreous and aqueous humor of patients with DR [31,32,33,34,35,36,37,38,39,40]. Many experimental studies showed that increases in these cytokines and chemokines contributed to cell death of retinal neurons in DR [41,42]. Specifically, massive chronic inflammatory responses (such as infiltration of inflammatory cells to the retina, activation of retinal microglia, and retinal vascular permeability) consisting of numerous cytokines and chemokines are considered critical in the progression of DR, as opposed to individual inflammatory proteins. When it comes to retinal degeneration, increases in the expression of Bax and activation of caspase-3 were detected in retinal neuronal cells in experimental models of diabetes and humans [43,44,45]. Glutamate excitotoxicity with loss of neuroprotective molecules was also suggested to cause retinal neuronal cell death in the diabetic retina [9]. Taken together, there is no doubt that various factors, from microvascular abnormality to retinal cell death, are interconnected in their contributions to the development and progression of DR.
In addition to hyperglycemic dysregulation, lipid metabolic dysregulation has been implicated as a potential risk factor for the development and progression of DR. Clinical studies demonstrated there were strong associations between changes in plasma levels of high-density and low-density lipoproteins (HDL and LDL) and the development of severities of DR as well as diabetes [46,47,48,49,50,51,52]. Abnormal levels of lipids in the blood (termed dyslipidemia), including elevation of LDL, free fatty acids, and triglycerides, reduction of HDL, and inhibition of reverse cholesterol transport gene expressions, could be promoted under insulin-resistant conditions [53,54,55]. A higher frequency of retinal abnormalities was reported in diabetic subjects with dyslipidemia [56,57]. Even though more experimental evidence on lipid metabolic dysregulation with the development and progression of DR are needed, emerging evidence has shown that lipid-modifying drugs could exert possible protective effects in DR at the current stage [58,59].
Recently, several studies performed metabolomics with the vitreous humor in PDR patients. Metabolomics analysis of the vitreous humor could serve as a potential tool to identify new pathways associated with the development and progression of PDR. Barba et al. showed that lactate levels increased while ascorbic acid levels decreased in PDR patients compared to control patients [60]. Paris et al. showed that arginine and proline levels were upregulated in PDR patients [61]. Haines et al. demonstrated that the purine-related pathways were activated, and pyruvate levels increased in PDR patients [62]. Furthermore, our group showed that glycine levels increased, and creatine levels decreased in the vitreous humor of PDR patients [63]. Although research from new angles is underway, the pathophysiology of PDR has not yet been elucidated. More efforts are needed to elucidate the recent issue above.
3. Laser Treatment
3.1. Treatment for DR
The Diabetic Retinopathy Study (DRS) indicated four risk factors for vision loss in DR. These risk factors include the presence of vitreous or preretinal hemorrhage, the presence of new vessels, the location of new vessels on or near the optic disc, and finally, the severity of pathological conditions in new vessels [64]. According to this study, eyes with three or more risk factors are considered “at high risk” of vision loss in DR.
Laser treatment for DR has been well established for several decades. Since pan-retinal photocoagulation (PRP) can reduce retinal neovascularization, it has been performed to reduce the high-risk development of PDR [65,66]. An analysis using a rabbit model of retinal ischemia showed that photocoagulation suppressed ischemia-induced VEGF, vascular permeability, and angiogenesis promoted by VEGF [67]. In addition, the level of VEGF was lower in eyes treated with PRP compared with that in untreated eyes [68]. For this reason, it is thought that destroying the retinal non-perfusion areas (NPAs) with a laser could reduce pathological angiogenesis from these areas. Therefore, PRP is considered an essential therapeutic tool in controlling DR activity. The optimal timing for PRP is between severe NPDR and early PDR, according to the Early Treatment Diabetic Retinopathy Study (ETDRS) [69]. Clinical trials have shown that PRP reduced the risk of severe vision loss by 50% or more in DR. Furthermore, only 1% of patients and 4% of eyes experienced severe vision loss in 5 years following photocoagulation [70,71]. This approach seemed promising to suppress the progression of DR. However, there were several problems reported in PRP therapies, such as peripheral visual field loss, delayed dark adaptation, and atrophic creep in long-term studies [72,73,74,75].
The pattern scan laser was developed in an attempt to solve these problems [76]. It has been reported that the decrease in the nerve fiber layer (which can be generally seen after PRP) was significantly improved after using the advanced laser. The degree of pain for the patient and the expansion of the coagulation zone were also reduced compared to those in the conventional laser. In addition, it has been reported that the amount of inflammatory cytokines induced following its treatment was lower than that of the conventional methods [77]. Finally, the operation time could be shortened, a significant point during the surgery [78,79]. Despite these benefits, the pattern scan laser has a narrow safety margin because of the short-pulse laser features and is easily influenced by hazy media such as vitreous hemorrhage. It is also known that the coagulation spot tends to shrink over time [80]. Besides, the pattern scan laser has been reported to lead to a higher frequency of retinal neovascularization, iris neovascularization, and neovascular glaucoma than the conventional PRP [81], which implies more investigations into conventional PRP and pattern scan laser therapies in DR may be needed.
Targeted retinal photocoagulation (TRP) has been used for patients with NPDR in some countries. This technique involves selective photocoagulation of the areas in retinal vascular occlusion. It has been reported that the progression rate of PDR could be slowed with selective photocoagulation in patients with multiple NPAs of one papillary diameter or more in NPDR [82]. In addition, a randomized clinical trial showed that extended TRP was effective in early PDR regression with fewer coagulation spots than the conventional PRP [83]. Recently, the navigated pattern laser (NAVILAS), a fundus camera-based photocoagulation system, has been developed. This system enables the delivery of navigated pattern PRP, selectively applied to NPAs [84]. However, in any of the described methods, fluorescence angiography (FA) is necessary to identify NPAs to determine the indication for photocoagulation. On the other hand, a recent randomized trial showed that combination therapy with ranibizumab and widefield FA-guided TRP did not improve visual acuity or reduce the number of anti-VEGF injections compared to ranibizumab alone in DME patients [85]. Therefore, further studies are needed.
3.2. Treatment for DME
The ETDRS showed that the focal/grid laser produced better outcomes than the natural course in patients with severe DME [86,87]. Severe macular edema is defined as retinal thickening that involves or threatens the macula’s center. The focal/grid laser is recommended especially for DME that does not include the fovea and does not require frequent visits to the hospital for treatment. However, large or dense coagulation near the macula may result in a paracentral dark spot. Furthermore, complications such as atrophic creep may occur in this chronic condition [88]. Based on these problems, the modified ETDRS laser was proposed in the Diabetic Retinopathy Clinical Research (DRCR) net in 2007 [89]. It is based on direct photocoagulation of capillary aneurysms with a minimally invasive setting and is becoming the standard.
Recently, subthreshold diode laser micropulse photocoagulation (SDM), invisible retinal phototherapy, has been developed to treat DME. It applies heat to the retinal pigment epithelium under conditions that do not cause cell death. The current indications for the SDM for DME are the localized edema outside the fovea and the mild macular edema, including the fovea. To date, several reports have shown a significant efficacy of SDM alone for DME [90,91,92]. Randomized controlled trials have also reported that the SDM is more effective than the modified ETDRS laser [91]. In general, this treatment alone is indicated for cases with relatively mild edema, and combined treatment with anti-VEGF therapy is indicated for severe DME [93].
4. Anti-VEGF Treatment
4.1. Treatment for DR
Protocol S reported that anti-VEGF treatment (ranibizumab) resulted in significantly better visual acuity than PRP treatment for PDR patients [94]. In addition, the anti-VEGF group had substantially less peripheral visual field loss, faced fewer cases of DME, and a decreased need for vitrectomy compared to those in the PRP group. Other studies have also shown improvements in Diabetic Retinopathy Severity Scale (DRSS) scores as well as a lower risk of vitrectomy and DME with intravitreal anti-VEGF treatment (ranibizumab), compared to PRP [95,96]. The Clinical Efficacy and Mechanistic Evaluation of Aflibercept for Proliferative Diabetic Retinopathy (CLARITY) trial was specifically designed to evaluate the efficacy of PRP versus aflibercept for patients with PDR without DME [97]. A study group showed that ranibizumab suppressed neovascularization and maintained better visual acuity than PRP treatment during the first 12 months of the PRIDE study, but it is not sustained after 24 months under real-world conditions [98,99]. Although these results suggest that anti-VEGF therapy could be more valuable for preventing the progression of DR than PRP, it should be noted that anti-VEGF treatment requires frequent follow-up, compared to general laser photocoagulation, which has a permanent effect on the operated eyes.
With regard to frequent follow-up in anti-VEGF treatment, there is a possibility of worsening retinopathy in patients who stop coming to the clinic. It is reported that anti-VEGF therapy alone has a worse prognosis than photocoagulation if a patient ceases the treatment [100]. Because anti-VEGF drugs are expensive and require multiple visits to the clinic, the management of PDR should be guided by both cost and patient-specific factors such as visit compliance.
4.2. Treatment for DME
A multicenter randomized clinical trial showed that anti-VEGF drugs had a therapeutic effect for DME that involves the central macula [101]. The RESTORE study showed that ranibizumab and laser therapy improved visual acuity more than focal/grid laser in patients with DME [102]. The RISE and RIDE study showed that ranibizumab improved visual acuity and macular edema in patients with DME [103]. On the other hand, the VISTA and VIVID studies showed that aflibercept had better visual improvement and more reduction in central retinal thickness than the focal/grid laser alone for DME involving the fovea [104,105]. In terms of the efficacy of bevacizumab, ranibizumab, and aflibercept for DME, it is controversial in randomized clinical trials. Although aflibercept was superior to bevacizumab and ranibizumab in eyes with visual acuity of 20/50 or worse at one year, aflibercept was no longer superior to ranibizumab at two years [106,107]. Another study showed that aflibercept could be more efficient in treating moderate or severe visual acuity loss cases, but aflibercept, bevacizumab, and ranibizumab had comparable effects for mild DME [108]. However, because of the short duration of the drug effect, multiple injections are required to maximize visual improvement. Thus, it is recommended that anti-VEGF therapy for DME involving the fovea may be combined with focal/grid laser therapies to reduce the number of injections [109].
Anti-VEGF injection may increase the risk of high intraocular pressure, infectious endophthalmitis, and cataract [110,111,112]. In addition, the intraocular injection may cause retinal damages or tractional retinal detachment. Furthermore, there is a possibility that anti-VEGF (which is intended to be injected into the vitreous) may unexpectedly diffuse to systemic circulation. The indication for the treatment and re-administration should be determined based on the patient’s general condition as well as their visual acuity and conditions of central retinal thickness.
5. Steroid Treatment
Treatment for DME
Steroid treatment is indicated when edema is diffuse throughout the macula. Steroids have an anti-inflammatory effect that helps to downregulate both pro-inflammatory and pro-angiogenic mediators, which are crucial for the development of DME. General steroid treatments have the possibility of multiple side effects, so topical corticosteroid treatments are preferable for DME. There are several options for administering steroids, such as intravitreal injection, subtenone injection, and dexamethasone intravitreal implant (DEX).
Intravitreal triamcinolone acetonide injection (IVTA) has played an essential role in treating DME for many years, especially prior to the approval of anti-VEGF injections [113,114]. Substantial improvements in macular thickness and visual acuity have been reported with IVTA [115]. Another group showed that a single IVTA injection to DME induced a significant improvement in macular thickness and visual acuity at three months after the treatment [116]. However, because of the short effective duration, multiple injections are required to maintain its efficacy. A clinical trial reported that there was no significant change between the bevacizumab vs. bevacizumab + IVTA groups in terms of best corrected visual acuity and central macular thickness changes, compared to the baseline at 24 weeks. Nonetheless, the bevacizumab + IVTA group showed earlier visual improvement [117]. Thus, combined therapy with anti-VEGF treatment may be recommended for the early visual improvement.
Subtenone triamcinolone acetonide injection (STTA) is also used to treat DME patients. Several studies have shown that STTA reduced retinal thickness and improved visual acuity [118,119]. However, it is still controversial regarding results for the DME treatment [118,119]. In addition, because it also has a short duration of effects, patients need multiple injections as they do with IVTA. To overcome this problem, STTA is often used in conjunction with anti-VEGF treatment. For example, a retrospective study compared the combination therapy of STTA and intravitreal anti-VEGF injection with anti-VEGF monotherapy to treat anti-VEGF-resistant DME. The thirty-eight eyes treated with the combination therapy showed significantly improved visual acuity and macular thickness after six months of treatment. Although STTA injection is less effective for short-term DME than IVTA injection, it has been shown that STTA resulted in less steroid-responsive intraocular pressure elevation than intravitreal steroids [120,121]. Another group showed that STTA treatment with bevacizumab improved morphological changes and reduced the frequency of bevacizumab treatments in DME patients [122]. Thus, STTA may be a useful adjunctive therapy in anti-VEGF-resistant DME in the case of existing concerns for steroid-induced glaucoma.
The DEX implant, an FDA-approved DME treatment, has become an alternative injection method to IVTA and STTA in several countries. It has provided a longer-term option for steroid therapy. Several retrospective studies have shown that in anti-VEGF-resistant eyes, a single DEX implant improved macular thickness and visual acuity [123,124,125,126]. Another group treated 16 eyes with a single DEX implant and reported significant improvements in macular thickness at one, two, and three months. However, the DRCR network showed that combination therapy of DEX implant and anti-VEGF did not improve visual acuity at twenty-four weeks more than anti-VEGF treatment alone [127]. Intravitreal fluocinolone acetonide is another implant with longer effective periods than the DEX implant. Multiple studies have shown that the intravitreal fluocinolone acetonide implant could be useful for treating anti-VEGF-resistant DME, with sustained beneficial visual acuity and macular thickness outcomes [128,129,130,131,132]. The systematic review included seven randomized clinical trials that suggested IVTA and surgical implantation of steroids may improve visual outcomes in eyes with refractory DME [133]. However, since each treatment can carry additional glaucoma and cataract progression risks, special care is needed to avoid these complications [134,135]. In addition, ophthalmologists need to be cautious of noninfectious endophthalmitis (NIE) in that ocular inflammation occurs after intravitreal injection of corticosteroids [136]. A recent study indicates that the incidence rate of NIE lies between 0.1% and 7.3% [137].
6. Surgical Treatment
6.1. Treatment for DR
PDR patients with dense and recurrent vitreous hemorrhage or tractional retinal detachment close to the retina or rhegmatogenous retinal detachment require surgical treatments. Vitrectomy refers to the surgery for retinal and vitreous diseases. During the surgery, surgeons remove the vitreous and replace it with another solution. Photocoagulation is needed to attach the retina if there is an NPA or retinal tear. In PDR patients, the longer a macular detachment occurs, the more difficult it becomes to restore vision due to the deterioration of macular photoreceptor function. In recent years, the development of small-incision vitrectomy such as the 23-, 25-, and 27-gauge and wide-angle viewing systems (for instance, Resight®) has contributed to the improvement of vitreoretinal surgery [138,139,140,141]. These techniques make vitrectomy less invasive and safer so that earlier vitrectomy, in cases with macula dragging due to fibrovascular tissue overlying the macula, may be indicated in patients with PDR [142]. Furthermore, these operations are shown to be safer following anti-VEGF pretreatment [143,144]. Thus, the indications of vitrectomy for the treatment of PDR have been expanded by the early intervention [145].
However, there are many cases of poor prognosis in PDR following vitrectomy. Permanent vision loss may occur due to retinal detachment involved in the macula, glaucoma, or ischemic changes. Re-bleeding may occur after vitrectomy for vitreous hemorrhage, although a small incision vitrectomy reduces this recurrence [146,147]. Cataract formation should be considered after vitrectomy in patients with phakia. Although the incidence is low, it is also necessary to pay attention to postoperative endophthalmitis.
6.2. Treatment for DME
Vitrectomy has been reported to improve visual acuity for DME accompanied by an epiretinal membrane or thickened posterior vitreous cortex with vitreomacular traction [148,149,150]. Vitreoretinal surgery may also be considered a treatment option when the outcomes were not satisfactory from retinal photocoagulation and drug therapies such as anti-VEGF and steroids. Posterior vitreous detachment and peeling of the internal limiting membrane can be performed for DME. This is because the inner limiting membrane could become a scaffold for proliferative myofibroblasts [151], which may cause the recurrence of macular edema with the epiretinal membrane.
Long-term results showed improved visual acuity after vitrectomy for DME in 496 eyes, comparable to those shown in anti-VEGF therapy [152]. Vitrectomy caused a more significant central macular thickness reduction than IVTA 12 months after treatment, although it showed no statistically significant change in visual acuity [153]. It was reported that vitrectomy was morphologically effective after six months compared to the grid laser, but there was no significant difference in visual function. In addition, there was no significant difference in morphology or visual function after one year. On the other hand, it has been reported that the presence or absence of an internal limiting membrane detachment did not affect the prognosis of visual function in vitrectomy for DME without macular traction [154]. Recently, Imai et al. reported the effectiveness of cystotomy for long-term anatomical and functional improvements of refractory cystoid macular edema secondary to DR. However, it is necessary to accumulate many cases for the concrete conclusion of the effectiveness of cystotomy [155,156]. Overall, there is the possibility of the same risks as other vitrectomies, and care must be taken when choosing potential patients.
Importantly, all of these treatments are for advanced diseases. There is no safe and effective ophthalmic treatment other than controlling of blood glucose levels, even if the early stage of DR is observed. Thus, we need preventive treatments for DR.
7. Fenofibrate Therapy in DR
Fenofibrate is a well-known peroxisome proliferator-activated receptor alpha (PPARα) agonist. PPARα is one of the members in the nuclear receptor family of ligand-activated transcription factors [13]. Heterodimerization of PPARα with the retinoic X receptor regulates the transcription of genes involved in cellular metabolism [13]. Fenofibrate could reduce free fatty acids levels by upregulating the synthesis of molecules for fatty acid transport and β-oxidation through the activation of PPARα [13,157,158]. Furthermore, fenofibrate has the potential to induce an increase in the synthesis of apolipoproteins and high-density lipoprotein cholesterol [159,160,161]. In this regard, fenofibrate could be used as a therapeutic drug in metabolic syndrome. Fenofibrate has been effectively used in the US to manage patients with dyslipidemia since 1998 [162]. As metabolic syndrome is a common finding in patients with diabetes, the future use of fenofibrate in the management of patients with DR was also examined in the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study [163] and the Action to Control Cardiovascular Risk in Diabetes (ACCORD)-Eye study [164]. Based on the FIELD study, the fenofibrate-administered group showed a significant reduction of relative risk in need for laser treatment for DME and PDR. When it comes to the ACCORD-Eye study, the progression of DR was significantly reduced in the fenofibrate-statin-administered group compared to that in the only statin-administered group. Taken together, fenofibrate was suggested as a promising therapeutic for slowing the progression of DR.
Experimental animal studies also supported the notion that fenofibrate may have protection against DR [165,166,167]. Oral administration of fenofibric acid, the active metabolite of fenofibrate, reduced ganglion cell death and preserved amplitudes in oscillatory potentials and implicit time of b-wave in diabetic db/db mice [165]. Upregulated expressions of Il-6, Il-1β, P53, Bax, and Vegf and their protein expressions in the diabetic rat retina were reduced by oral administration of fenofibrate [166]. Similar effects of fenofibrate treatment were found in human retinal microvascular endothelial cells under high glucose stimulation [166]. Another study showed that oral administration of fenofibrate attenuated oxidative stress and neuroinflammation in the diabetic mouse retina via increasing expressions of a master regulator of antioxidative defense, nuclear factor erythroid 2–related factor 2 (Nrf2) and its target genes, including heme oxygenase 1 (Ho-1), and decreasing the formation of reactive oxygen species [167]. Taken together, fenofibrate appears viable for the treatment of DR.
Even though fenofibrate is a generally well-tolerated drug, its effects on increases in serum levels of creatinine were continuously reported [168,169,170]. This finding raised concerns regarding deleterious damages to renal function. Safety issues surrounding the use of fenofibrate are still debated. As such, fenofibrate is not highly recommended for use in patients with severe renal impairment. Along with this issue, researchers have been attempting to develop better therapeutics for PPARα activation.
8. Pemafibrate Therapy in DR
Pemafibrate is a new selective PPARα modulator, recently synthesized by Kowa Company, Ltd. as a more efficient and safer alternative to fenofibrate. Clinical studies in Japan demonstrated that pemafibrate showed superior effects on cellular metabolism compared to fenofibrate by improving liver function and increasing serum creatinine levels less likely or decreasing the estimated glomerular filtration rate [10,171,172]. One of the possible reasons is that pemafibrate is metabolized in the liver and excreted into the bile, while other fibrates, including fenofibrate, are predominantly excreted from the kidney. In this regard, pemafibrate could be a safer option in patients with severe renal impairment.
Experimental animal studies showed that pemafibrate could be used as a promising drug in diabetes and DR. In diabetic mice, oral administration of pemafibrate reduced plasma levels of triglycerides and vasoconstrictive eicosanoids [173]. Furthermore, impaired endothelial function in diabetic mice was attenuated by treatment with pemafibrate [173]. In high-fat diet mice with a femoral artery endothelial denudation injury, oral administration of pemafibrate increased serum levels of fibroblast growth factor 21 (FGF21) and decreased serum levels of insulin, attenuating neointima formation [174]. In our previous paper, long-term oral administration of pemafibrate improved blood glucose levels, modulated cellular metabolism, upregulated PPARα target genes in the liver (not in the retina), and increased serum levels of FGF21, to protect against diabetes-induced retinal dysfunction (amplitudes in oscillatory potentials) in mice [175]. Furthermore, we found that FGF21 could increase retinal protein expression of synaptophysin, one of the important molecules for maintaining oscillatory potentials [175]. Another study suggested that oral administration of pemafibrate directly inhibited retinal inflammation in diabetic rats by decreasing expressions of MCP-1 and VCAM-1 [176]. Furthermore, oral administration of pemafibrate inhibited diabetes-induced retinal vascular leukostasis by upregulating thrombomodulin expression [176]. Pemafibrate was recently suggested to protect against N-methyl-D-aspartate (NMDA) excitotoxicity-induced cell death in the rat retina (analyzed by TUNEL assay) [177]. This effect was associated with the inhibition of phosphorylated c-Jun, one of the possible links to the expression of apoptosis-related genes [177]. In terms of retinal neovascularization in DR, we previously demonstrated that oral administration of pemafibrate showed a significant reduction in retinal neovascularization in a murine model of oxygen-induced retinopathy [178]. Furthermore, a significant increase in serum levels of FGF21 and decreases in retinal HIF-1α immunostaining and Vegfa expression were found after oral administration of pemafibrate [178]. Taken together, pemafibrate therapy experimentally shows promise as a potential therapy for diabetes and DR.
Pemafibrate to Reduce cardiovascular OutcoMes by reducing triglycerides IN patiENts with diabeTes (PROMINENT), a phase 3 randomized clinical trial, has been ongoing (ClinicalTrials.gov Identifier: NCT03071692). Patients with dyslipidemia with type 2 diabetes were recruited in this study. Although DR had also been evaluated in the sub-analysis, because the number of recruited subjects for the DR study did not meet the criteria, it was suspended. However, if pemafibrate has therapeutic effects for metabolic syndromes, drug-repositioning of pemafibrate could be applied to treat retinal diseases, including DR, in the future.
9. Conclusions
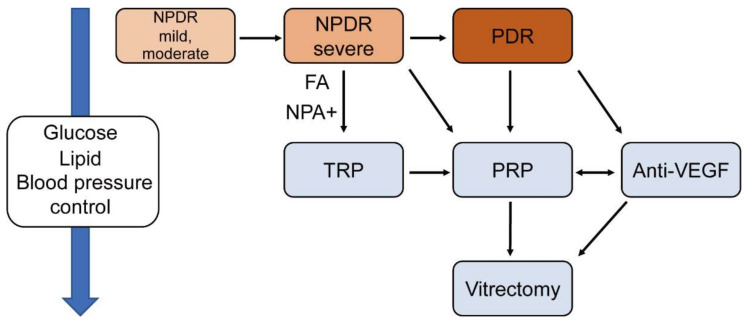
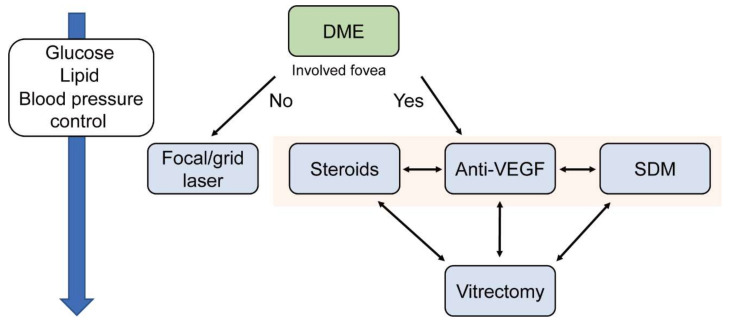
This study summarized current therapies such as laser, anti-VEGF, steroid, and surgery for DR and DME. Figure 2 and Figure 3 show suggested treatments for PDR and DME. Typically, patients with severe NPDR can be treated with PRP, however, if the NPA can be assessed in FA, then TRP can be a viable option as well. Patients with PDR need PRP or anti-VEGF therapy depending on the clinical and socioeconomic situation of the patients (Figure 2). The treatment of DME is divided according to whether the edema involves the fovea. If the edema does not include the fovea, patients could be treated by focal/ grid laser. If it includes the fovea, patients may be treated by anti-VEGF or steroid therapy. SDM is also an option, if available (Figure 3).
Figure 2.
A flowchart of suggested treatment for diabetic retinopathy (DR) without macular edema. DR is categorized as non-PDR (NPDR) and PDR. NPDR falls into three subcategories: mild, moderate, and severe. The control of glucose and lipid levels and blood pressure is crucial at any stage. NPDR; non-proliferative diabetic retinopathy, DME; diabetic macular edema, TRP; Targeted retinal photocoagulation, FA; Fluorescein angiography, NPA; non-perfusion area.
Figure 3.
A flowchart of suggested treatment for diabetic macular edema (DME). The strategy of treatment is decided by whether the edema includes the fovea or not. Controlling levels of glucose, lipid, and blood pressure is crucial at any stage. SDM; subthreshold diode laser micropulse photocoagulation, DME; diabetic macular edema.
Through every stage, the control of glucose and lipid levels is essential. However, all of these treatments can be applied for progressed diseases. Even if the early stage of DR is observed, clinicians can only contribute control of blood glucose levels, lipids, and hypertension [163,164,179,180,181]. It is also reported that controlling diabetic nephropathy, anemia, and sleep apnea is important for preventing DME [182]. This systemic medication is crucial to prevent and slow down the progression of DR. In addition, existing treatments are for vascular disorders, not for neurological disorders. Therefore, neuroprotection or preventive therapy for the early stage of DR needs to be developed as soon as possible. Future treatments may also be required with fewer side effects than the current therapies. At this point, many clinical studies with various therapeutic strategies are ongoing for slowing the progression of DR (searched in ClinicalTrials.gov).
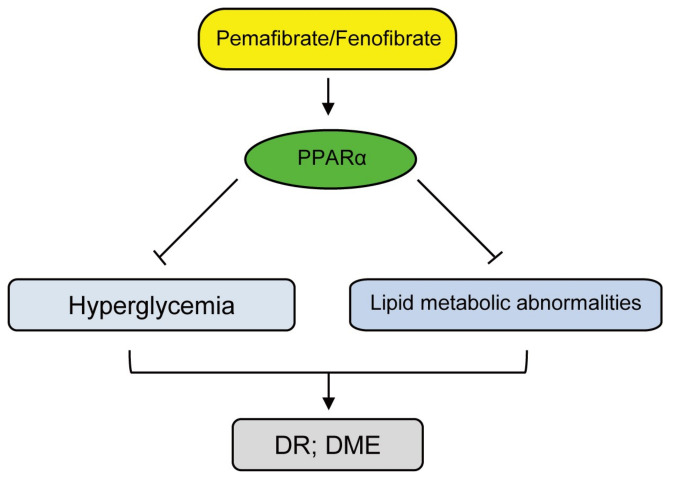
Based on the outcomes summarized in this review, oral non-invasive PPARα agonists (fenofibrate and pemafibrate) treatments could be one of the promising therapeutics to prevent the development and/or the progression of DR (Figure 4). Even though more investigations are needed, we hope that ophthalmologists can prevent DR with these drugs.
Figure 4.
A flowchart of promising treatments for diabetic retinopathy (DR) and diabetic macular edema (DME). PPARα activation by pemafibrate/fenofibrate is associated with modulating energy homeostasis in hyperglycemia and lipid metabolic abnormalities through the regulation of both lipid and glucose levels. Continuous control of levels of glucose and lipid is available with this promising treatment. DR; diabetic retinopathy, DME; diabetic macular edema.
Acknowledgments
We are grateful to W. Allen at Boston Children’s Hospital for critical discussions.
Author Contributions
T.K. provided technical and funding assistance; Y.T., D.L. and T.K. designed the study; Y.T. and D.L. wrote the manuscript; T.K., K.N. and K.T. reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported by Grants-in-Aid for Scientific Research (KAKENHI, number 15K10881, and 18K09424) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT) to T.K. and Manpei Suzuki Diabetes Foundation, Alcon Research Institute, and Bert M. Glaser MD Award to Y.T.
Conflicts of Interest
Kazuo Tsubota is CEO in Tsubota Laboratory, Inc. The remaining authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bourne R.R.A., Flaxman S.R., Braithwaite T., Cicinelli M.V., Das A., Jonas J.B., Keeffe J., Kempen J.H., Leasher J., Limburg H., et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: A systematic review and meta-analysis. Lancet Glob. Health. 2017;5:e888–e897. doi: 10.1016/S2214-109X(17)30293-0. [DOI] [PubMed] [Google Scholar]
- 2.Leasher J.L., Bourne R.R., Flaxman S.R., Jonas J.B., Keeffe J., Naidoo K., Pesudovs K., Price H., White R.A., Wong T.Y., et al. Global Estimates on the Number of People Blind or Visually Impaired by Diabetic Retinopathy: A Meta-analysis from 1990 to 2010. Diabetes Care. 2016;39:1643–1649. doi: 10.2337/dc15-2171. [DOI] [PubMed] [Google Scholar]
- 3.Zietz B., Kasparbauer A., Ottmann S., Spiegel D., Palitzsch K.D. Diabetic retinopathy and associated risk factors in type-1 and type-2 diabetics in the Upper Palatinate. Dtsch. Med. Wochenschr. 2000;125:783–788. doi: 10.1055/s-2007-1024518. [DOI] [PubMed] [Google Scholar]
- 4.Matuszewski W., Baranowska-Jurkun A., Stefanowicz-Rutkowska M.M., Modzelewski R., Pieczynski J., Bandurska-Stankiewicz E. Prevalence of Diabetic Retinopathy in Type 1 and Type 2 Diabetes Mellitus Patients in North-East Poland. Medicine. 2020;56:164. doi: 10.3390/medicina56040164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stewart M.W. Socioeconomic Cost of Diabetic Retinopathy and Therapy. In: Stewart M.W., editor. Diabetic Retinopathy: Current Pharmacologic Treatment and Emerging Strategies. Springer; Singapore: 2017. pp. 257–268. [DOI] [Google Scholar]
- 6.Orji A., Rani P.K., Narayanan R., Sahoo N.K., Das T. The economic burden of diabetic retinopathy care at a tertiary eye care center in South India. Indian J. Ophthalmol. 2021;69:666. doi: 10.4103/ijo.IJO_1538_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang X., Low S., Kumari N., Wang J., Ang K., Yeo D., Yip C.C., Tavintharan S., Sum C.F., Lim S.C. Direct medical cost associated with diabetic retinopathy severity in type 2 diabetes in Singapore. PLoS ONE. 2017;12:e0180949. doi: 10.1371/journal.pone.0180949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Avidor D., Loewenstein A., Waisbourd M., Nutman A. Cost-effectiveness of diabetic retinopathy screening programs using telemedicine: A systematic review. Cost Eff. Resour. Alloc. 2020;18:16. doi: 10.1186/s12962-020-00211-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simó R., Hernández C. Neurodegeneration in the diabetic eye: New insights and therapeutic perspectives. Trends Endocrinol. Metab. Tem. 2014;25:23–33. doi: 10.1016/j.tem.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Yamashita S., Masuda D., Matsuzawa Y. Pemafibrate, a New Selective PPARα Modulator: Drug Concept and Its Clinical Applications for Dyslipidemia and Metabolic Diseases. Curr. Atheroscler. Rep. 2020;22:5. doi: 10.1007/s11883-020-0823-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barot M., Gokulgandhi M.R., Patel S., Mitra A.K. Microvascular complications and diabetic retinopathy: Recent advances and future implications. Future Med. Chem. 2013;5:301–314. doi: 10.4155/fmc.12.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lutty G.A. Effects of diabetes on the eye. Investig. Ophthalmol. Vis. Sci. 2013;54:ORSF81. doi: 10.1167/iovs.13-12979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tomita Y., Lee D., Tsubota K., Kurihara T. PPARα Agonist Oral Therapy in Diabetic Retinopathy. Biomedicines. 2020;8:433. doi: 10.3390/biomedicines8100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang W., Lo A.C.Y. Diabetic Retinopathy: Pathophysiology and Treatments. Int. J. Mol. Sci. 2018;19:1816. doi: 10.3390/ijms19061816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bergers G., Song S. The role of pericytes in blood-vessel formation and maintenance. Neuro-Oncology. 2005;7:452–464. doi: 10.1215/S1152851705000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu C., Ge H.M., Liu B.H., Dong R., Shan K., Chen X., Yao M.D., Li X.M., Yao J., Zhou R.M., et al. Targeting pericyte-endothelial cell crosstalk by circular RNA-cPWWP2A inhibition aggravates diabetes-induced microvascular dysfunction. Proc. Natl. Acad. Sci. USA. 2019;116:7455–7464. doi: 10.1073/pnas.1814874116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naruse K., Nakamura J., Hamada Y., Nakayama M., Chaya S., Komori T., Kato K., Kasuya Y., Miwa K., Hotta N. Aldose reductase inhibition prevents glucose-induced apoptosis in cultured bovine retinal microvascular pericytes. Exp. Eye Res. 2000;71:309–315. doi: 10.1006/exer.2000.0882. [DOI] [PubMed] [Google Scholar]
- 18.Romeo G., Liu W.H., Asnaghi V., Kern T.S., Lorenzi M. Activation of nuclear factor-kappaB induced by diabetes and high glucose regulates a proapoptotic program in retinal pericytes. Diabetes. 2002;51:2241–2248. doi: 10.2337/diabetes.51.7.2241. [DOI] [PubMed] [Google Scholar]
- 19.Beltramo E., Porta M. Pericyte loss in diabetic retinopathy: Mechanisms and consequences. Curr. Med. Chem. 2013;20:3218–3225. doi: 10.2174/09298673113209990022. [DOI] [PubMed] [Google Scholar]
- 20.Bianchi E., Ripandelli G., Taurone S., Feher J., Plateroti R., Kovacs I., Magliulo G., Orlando M.P., Micera A., Battaglione E., et al. Age and diabetes related changes of the retinal capillaries: An ultrastructural and immunohistochemical study. Int. J. Immunopathol. Pharm. 2016;29:40–53. doi: 10.1177/0394632015615592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aiello L.P., Wong J.-S. Role of vascular endothelial growth factor in diabetic vascular complications. Kidney Int. 2000;58:S113–S119. doi: 10.1046/j.1523-1755.2000.07718.x. [DOI] [PubMed] [Google Scholar]
- 22.Selim K.M., Sahan D., Muhittin T., Osman C., Mustafa O. Increased levels of vascular endothelial growth factor in the aqueous humor of patients with diabetic retinopathy. Indian J. Ophthalmol. 2010;58:375. doi: 10.4103/0301-4738.67042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao Y., Singh R.P. The role of anti-vascular endothelial growth factor (anti-VEGF) in the management of proliferative diabetic retinopathy. Drugs Context. 2018;7:212532. doi: 10.7573/dic.212532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta N., Mansoor S., Sharma A., Sapkal A., Sheth J., Falatoonzadeh P., Kuppermann B., Kenney M. Diabetic retinopathy and VEGF. Open Ophthalmol. J. 2013;7:4–10. doi: 10.2174/1874364101307010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy S., Amin S., Roy S. Retinal fibrosis in diabetic retinopathy. Exp. Eye Res. 2016;142:71–75. doi: 10.1016/j.exer.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ishibazawa A., Nagaoka T., Yokota H., Takahashi A., Omae T., Song Y.S., Takahashi T., Yoshida A. Characteristics of Retinal Neovascularization in Proliferative Diabetic Retinopathy Imaged by Optical Coherence Tomography Angiography. Investig. Ophthalmol. Vis. Sci. 2016;57:6247–6255. doi: 10.1167/iovs.16-20210. [DOI] [PubMed] [Google Scholar]
- 27.Cohen S.R., Gardner T.W. Diabetic Retinopathy and Diabetic Macular Edema. Dev. Ophthalmol. 2016;55:137–146. doi: 10.1159/000438970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang H., He J., Johnson D., Wei Y., Liu Y., Wang S., Lutty G.A., Duh E.J., Semba R.D. Deletion of placental growth factor prevents diabetic retinopathy and is associated with Akt activation and HIF1α-VEGF pathway inhibition. Diabetes. 2015;64:200–212. doi: 10.2337/db14-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campochiaro P.A. Molecular pathogenesis of retinal and choroidal vascular diseases. Prog. Retin. Eye Res. 2015;49:67–81. doi: 10.1016/j.preteyeres.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelly B.D., Hackett S.F., Hirota K., Oshima Y., Cai Z., Berg-Dixon S., Rowan A., Yan Z., Campochiaro P.A., Semenza G.L. Cell type-specific regulation of angiogenic growth factor gene expression and induction of angiogenesis in nonischemic tissue by a constitutively active form of hypoxia-inducible factor 1. Circ. Res. 2003;93:1074–1081. doi: 10.1161/01.RES.0000102937.50486.1B. [DOI] [PubMed] [Google Scholar]
- 31.Kim M., Kim Y., Lee S.J. Comparison of aqueous concentrations of angiogenic and inflammatory cytokines based on optical coherence tomography patterns of diabetic macular edema. Indian J. Ophthalmol. 2015;63:312–317. doi: 10.1530/endoabs.41.GP87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vujosevic S., Micera A., Bini S., Berton M., Esposito G., Midena E. Proteome analysis of retinal glia cells-related inflammatory cytokines in the aqueous humour of diabetic patients. Acta Ophthalmol. 2016;94:56–64. doi: 10.1111/aos.12812. [DOI] [PubMed] [Google Scholar]
- 33.Boss J.D., Singh P.K., Pandya H.K., Tosi J., Kim C., Tewari A., Juzych M.S., Abrams G.W., Kumar A. Assessment of neurotrophins and inflammatory mediators in vitreous of patients with diabetic retinopathy. Investig. Ophthalmol. Vis. Sci. 2017;58:5594–5603. doi: 10.1167/iovs.17-21973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adamiec-Mroczek J., Oficjalska-Młyńczak J., Misiuk-Hojło M. Proliferative diabetic retinopathy-The influence of diabetes control on the activation of the intraocular molecule system. Diabetes Res. Clin. Pract. 2009;84:46–50. doi: 10.1016/j.diabres.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 35.Bromberg-White J.L., Glazer L., Downer R., Furge K., Boguslawski E., Duesbery N.S. Identification of VEGF-independent cytokines in proliferative diabetic retinopathy vitreous. Investig. Ophthalmol. Vis. Sci. 2013;54:6472–6480. doi: 10.1167/iovs.13-12518. [DOI] [PubMed] [Google Scholar]
- 36.Mao C., Yan H. Roles of elevated intravitreal IL-1β and IL-10 levels in proliferative diabetic retinopathy. Indian J. Ophthalmol. 2014;62:699. doi: 10.4103/0301-4738.136220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ghodasra D.H., Fante R., Gardner T.W., Langue M., Niziol L.M., Besirli C., Cohen S.R., Dedania V.S., Demirci H., Jain N., et al. Safety and Feasibility of Quantitative Multiplexed Cytokine Analysis From Office-Based Vitreous Aspiration. Investig. Ophthalmol. Vis. Sci. 2016;57:3017–3023. doi: 10.1167/iovs.15-18721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu H., Hwang D.K., Song X., Tao Y. Association between Aqueous Cytokines and Diabetic Retinopathy Stage. J. Ophthalmol. 2017;2017:9402198. doi: 10.1155/2017/9402198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Funatsu H., Yamashita H., Sakata K., Noma H., Mimura T., Suzuki M., Eguchi S., Hori S. Vitreous levels of vascular endothelial growth factor and intercellular adhesion molecule 1 are related to diabetic macular edema. Ophthalmology. 2005;112:806–816. doi: 10.1016/j.ophtha.2004.11.045. [DOI] [PubMed] [Google Scholar]
- 40.Vujosevic S., Micera A., Bini S., Berton M., Esposito G., Midena E. Aqueous Humor Biomarkers of Müller Cell Activation in Diabetic Eyes. Investig. Ophthalmol. Vis. Sci. 2015;56:3913–3918. doi: 10.1167/iovs.15-16554. [DOI] [PubMed] [Google Scholar]
- 41.Feenstra D.J., Yego E.C., Mohr S. Modes of Retinal Cell Death in Diabetic Retinopathy. J. Clin. Exp. Ophthalmol. 2013;4:298. doi: 10.4172/2155-9570.1000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rübsam A., Parikh S., Fort P.E. Role of Inflammation in Diabetic Retinopathy. Int. J. Mol. Sci. 2018;19:942. doi: 10.3390/ijms19040942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mohr S., Xi X., Tang J., Kern T.S. Caspase Activation in Retinas of Diabetic and Galactosemic Mice and Diabetic Patients. Diabetes. 2002;51:1172. doi: 10.2337/diabetes.51.4.1172. [DOI] [PubMed] [Google Scholar]
- 44.Podestà F., Romeo G., Liu W.-H., Krajewski S., Reed J.C., Gerhardinger C., Lorenzi M. Bax Is Increased in the Retina of Diabetic Subjects and Is Associated with Pericyte Apoptosis in Vivo and in Vitro. Am. J. Pathol. 2000;156:1025–1032. doi: 10.1016/S0002-9440(10)64970-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kowluru R.A., Koppolu P. Diabetes-induced Activation of Caspase-3 in Retina: Effect of Antioxidant Therapy. Free Radic. Res. 2002;36:993–999. doi: 10.1080/1071576021000006572. [DOI] [PubMed] [Google Scholar]
- 46.Dornan T.L., Carter R.D., Bron A.J., Turner R.C., Mann J.I. Low density lipoprotein cholesterol: An association with the severity of diabetic retinopathy. Diabetologia. 1982;22:167–170. doi: 10.1007/BF00283746. [DOI] [PubMed] [Google Scholar]
- 47.Kissebah A.H., Kohner E.M., Lewis B., Siddiq Y.K., Lowy C., Fraser T.R. Plasma-lipids and glucose/insulin relationship in non-insulin-requiring diabetics with and without retinopathy. Lancet. 1975;1:1104–1108. doi: 10.1016/S0140-6736(75)92497-6. [DOI] [PubMed] [Google Scholar]
- 48.Eckel R.H., McLean E., Albers J.J., Cheung M.C., Bierman E.L. Plasma lipids and microangiopathy in insulin-dependent diabetes mellitus. Diabetes Care. 1981;4:447–453. doi: 10.2337/diacare.4.4.447. [DOI] [PubMed] [Google Scholar]
- 49.Mohan R., Mohan V., Susheela L., Ramachandran A., Viswanathan M. Increased LDL cholesterol in non-insulin-dependent diabetics with maculopathy. Acta Diabetol. Lat. 1984;21:85–89. [PubMed] [Google Scholar]
- 50.Chakraborty A., Mondal P.R., Kundu S.C., Batabyal S.K. Serum lipids and lipoproteins in diabetic retinopathy. J. Assoc. Physicians India. 1986;34:631–632. [PubMed] [Google Scholar]
- 51.Chew E.Y., Klein M.L., Ferris F.L., III, Remaley N.A., Murphy R.P., Chantry K., Hoogwerf B.J., Miller D. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study (ETDRS) Report 22. Arch. Ophthalmol. 1996;114:1079–1084. doi: 10.1001/archopht.1996.01100140281004. [DOI] [PubMed] [Google Scholar]
- 52.Sasongko M.B., Wong T.Y., Nguyen T.T., Kawasaki R., Jenkins A., Shaw J., Wang J.J. Serum apolipoprotein AI and B are stronger biomarkers of diabetic retinopathy than traditional lipids. Diabetes Care. 2011;34:474–479. doi: 10.2337/dc10-0793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Reaven G.M., Chen Y.D. Role of insulin in regulation of lipoprotein metabolism in diabetes. Diabetes/Metab. Rev. 1988;4:639–652. doi: 10.1002/dmr.5610040703. [DOI] [PubMed] [Google Scholar]
- 54.Goff D.C., Jr., D’Agostino R.B., Jr., Haffner S.M., Otvos J.D. Insulin resistance and adiposity influence lipoprotein size and subclass concentrations. Results from the Insulin Resistance Atherosclerosis Study. Metab. Clin. Exp. 2005;54:264–270. doi: 10.1016/j.metabol.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 55.Ginsberg H.N., Zhang Y.L., Hernandez-Ono A. Regulation of plasma triglycerides in insulin resistance and diabetes. Arch. Med. Res. 2005;36:232–240. doi: 10.1016/j.arcmed.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 56.Sacks F.M., Hermans M.P., Fioretto P., Valensi P., Davis T., Horton E., Wanner C., Al-Rubeaan K., Aronson R., Barzon I., et al. Association between plasma triglycerides and high-density lipoprotein cholesterol and microvascular kidney disease and retinopathy in type 2 diabetes mellitus: A global case-control study in 13 countries. Circulation. 2014;129:999–1008. doi: 10.1161/CIRCULATIONAHA.113.002529. [DOI] [PubMed] [Google Scholar]
- 57.Cetin E.N., Bulgu Y., Ozdemir S., Topsakal S., Akın F., Aybek H., Yıldırım C. Association of serum lipid levels with diabetic retinopathy. Int. J. Ophthalmol. 2013;6:346–349. doi: 10.3980/j.issn.2222-3959.2013.03.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hammer S.S., Busik J.V. The role of dyslipidemia in diabetic retinopathy. Vis. Res. 2017;139:228–236. doi: 10.1016/j.visres.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chang Y.-C., Wu W.-C. Dyslipidemia and diabetic retinopathy. Rev. Diabet. Stud. 2013;10:121–132. doi: 10.1900/RDS.2013.10.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barba I., Garcia-Ramirez M., Hernandez C., Alonso M.A., Masmiquel L., Garcia-Dorado D., Simo R. Metabolic fingerprints of proliferative diabetic retinopathy: An 1H-NMR-based metabonomic approach using vitreous humor. Investig. Ophthalmol. Vis. Sci. 2010;51:4416–4421. doi: 10.1167/iovs.10-5348. [DOI] [PubMed] [Google Scholar]
- 61.Paris L.P., Johnson C.H., Aguilar E., Usui Y., Cho K., Hoang L.T., Feitelberg D., Benton H.P., Westenskow P.D., Kurihara T., et al. Global metabolomics reveals metabolic dysregulation in ischemic retinopathy. Metabolomics. 2016;12:15. doi: 10.1007/s11306-015-0877-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Haines N.R., Manoharan N., Olson J.L., D’Alessandro A., Reisz J.A. Metabolomics Analysis of Human Vitreous in Diabetic Retinopathy and Rhegmatogenous Retinal Detachment. J. Proteome Res. 2018;17:2421–2427. doi: 10.1021/acs.jproteome.8b00169. [DOI] [PubMed] [Google Scholar]
- 63.Tomita Y., Cagnone G., Fu Z., Cakir B., Kotoda Y., Asakage M., Wakabayashi Y., Hellstrom A., Joyal J.S., Talukdar S., et al. Vitreous metabolomics profiling of proliferative diabetic retinopathy. Diabetologia. 2021;64:70–82. doi: 10.1007/s00125-020-05309-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Diabetic Retinopathy Study Research Group Four risk factors for severe visual loss in diabetic retinopathy. The third report from the Diabetic Retinopathy Study. The Diabetic Retinopathy Study Research Group. Arch. Ophthalmol. 1979;97:654–655. doi: 10.1001/archopht.1979.01020010310003. [DOI] [PubMed] [Google Scholar]
- 65.Diabetic Retinopathy Study Research Group Indications for photocoagulation treatment of diabetic retinopathy: Diabetic Retinopathy Study Report no. 14. The Diabetic Retinopathy Study Research Group. Int. Ophthalmol. Clin. 1987;27:239–253. doi: 10.1097/00004397-198702740-00004. [DOI] [PubMed] [Google Scholar]
- 66.Early Treatment Diabetic Retinopathy Study Research Group Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report no. 3. The Early Treatment Diabetic Retinopathy Study Research Group. Int. Ophthalmol. Clin. 1987;27:254–264. doi: 10.1097/00004397-198702740-00005. [DOI] [PubMed] [Google Scholar]
- 67.Gozawa M., Takamura Y., Miyake S., Matsumura T., Morioka M., Yamada Y., Inatani M. Photocoagulation of the Retinal Nonperfusion Area Prevents the Expression of the Vascular Endothelial Growth Factor in an Animal Model. Investig. Ophthalmol. Vis. Sci. 2017;58:5946–5953. doi: 10.1167/iovs.17-22739. [DOI] [PubMed] [Google Scholar]
- 68.Aiello L.P., Avery R.L., Arrigg P.G., Keyt B.A., Jampel H.D., Shah S.T., Pasquale L.R., Thieme H., Iwamoto M.A., Park J.E., et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N. Engl. J. Med. 1994;331:1480–1487. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 69.Early Treatment Diabetic Retinopathy Study Research Group Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. ETDRS report number 7. Ophthalmology. 1991;98:741–756. doi: 10.1016/s0161-6420(13)38009-9. [DOI] [PubMed] [Google Scholar]
- 70.Chew E.Y., Ferris F.L., III, Csaky K.G., Murphy R.P., Agron E., Thompson D.J., Reed G.F., Schachat A.P. The long-term effects of laser photocoagulation treatment in patients with diabetic retinopathy: The early treatment diabetic retinopathy follow-up study. Ophthalmology. 2003;110:1683–1689. doi: 10.1016/S0161-6420(03)00579-7. [DOI] [PubMed] [Google Scholar]
- 71.Diabetic Retinopathy Study Research Group Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology. 1981;88:583–600. [PubMed] [Google Scholar]
- 72.Striph G.G., Hart W.M., Jr., Olk R.J. Modified grid laser photocoagulation for diabetic macular edema. The effect on the central visual field. Ophthalmology. 1988;95:1673–1679. doi: 10.1016/S0161-6420(88)32957-X. [DOI] [PubMed] [Google Scholar]
- 73.Sims L.M., Stoessel K., Thompson J.T., Hirsch J. Assessment of visual-field changes before and after focal photocoagulation for clinically significant diabetic macular edema. Ophthalmologica. 1990;200:133–141. doi: 10.1159/000310094. [DOI] [PubMed] [Google Scholar]
- 74.Seiberth V., Alexandridis E., Feng W. Function of the diabetic retina after panretinal argon laser coagulation. Graefes. Arch. Clin. Exp. Ophthalmol. 1987;225:385–390. doi: 10.1007/BF02334163. [DOI] [PubMed] [Google Scholar]
- 75.Golden M.P., Russell B.P., Ingersoll G.M., Gray D.L., Hummer K.M. Management of diabetes mellitus in children younger than 5 years of age. Am. J. Dis. Child. 1985;139:448–452. doi: 10.1001/archpedi.1985.02140070022019. [DOI] [PubMed] [Google Scholar]
- 76.Blumenkranz M.S., Yellachich D., Andersen D.E., Wiltberger M.W., Mordaunt D., Marcellino G.R., Palanker D. Semiautomated patterned scanning laser for retinal photocoagulation. Retina. 2006;26:370–376. doi: 10.1097/00006982-200603000-00024. [DOI] [PubMed] [Google Scholar]
- 77.Takamura Y., Arimura S., Miyake S., Matsumura T., Gozawa M., Iwasaki K., Inatani M. Panretinal Photocoagulation Using Short-Pulse Laser Induces Less Inflammation and Macular Thickening in Patients with Diabetic Retinopathy. J. Ophthalmol. 2017;2017:8530261. doi: 10.1155/2017/8530261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Iwase T., Ueno Y., Ra E., Ito Y., Terasaki H. Changes in choriocapillaris and retinal morphology after laser photocoagulation by OCT angiography: A case report. Medicine. 2018;97:e13278. doi: 10.1097/MD.0000000000013278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sanghvi C., McLauchlan R., Delgado C., Young L., Charles S.J., Marcellino G., Stanga P.E. Initial experience with the Pascal photocoagulator: A pilot study of 75 procedures. Br. J. Ophthalmol. 2008;92:1061–1064. doi: 10.1136/bjo.2008.139568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lavinsky D., Cardillo J.A., Mandel Y., Huie P., Melo L.A., Farah M.E., Belfort R., Palanker D. Restoration of retinal morphology and residual scarring after photocoagulation. Acta Ophthalmol. 2013;91:e315–e323. doi: 10.1111/aos.12045. [DOI] [PubMed] [Google Scholar]
- 81.Chappelow A.V., Tan K., Waheed N.K., Kaiser P.K. Panretinal photocoagulation for proliferative diabetic retinopathy: Pattern scan laser versus argon laser. Am. J. Ophthalmol. 2012;153:137–142.e132. doi: 10.1016/j.ajo.2011.05.035. [DOI] [PubMed] [Google Scholar]
- 82.Japanese Society of Ophthalmic Diabetology, Subcommittee on the Study of Diabetic Retinopathy Treatment. Sato Y., Kojimahara N., Kitano S., Kato S., Ando N., Yamaguchi N., Hori S. Multicenter randomized clinical trial of retinal photocoagulation for preproliferative diabetic retinopathy. JPN J. Ophthalmol. 2012;56:52–59. doi: 10.1007/s10384-011-0095-2. [DOI] [PubMed] [Google Scholar]
- 83.Nikkhah H., Ghazi H., Razzaghi M.R., Karimi S., Ramezani A., Soheilian M. Extended targeted retinal photocoagulation versus conventional pan-retinal photocoagulation for proliferative diabetic retinopathy in a randomized clinical trial. Int. Ophthalmol. 2018;38:313–321. doi: 10.1007/s10792-017-0469-7. [DOI] [PubMed] [Google Scholar]
- 84.Chhablani J., Mathai A., Rani P., Gupta V., Arevalo J.F., Kozak I. Comparison of conventional pattern and novel navigated panretinal photocoagulation in proliferative diabetic retinopathy. Investig. Ophthalmol. Vis. Sci. 2014;55:3432–3438. doi: 10.1167/iovs.14-13936. [DOI] [PubMed] [Google Scholar]
- 85.Brown D.M., Ou W.C., Wong T.P., Kim R.Y., Croft D.E., Wykoff C.C., DAVE Study Group Targeted Retinal Photocoagulation for Diabetic Macular Edema with Peripheral Retinal Nonperfusion: Three-Year Randomized DAVE Trial. Ophthalmology. 2018;125:683–690. doi: 10.1016/j.ophtha.2017.11.026. [DOI] [PubMed] [Google Scholar]
- 86.Early Treatment Diabetic Retinopathy Study Research Group Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch. Ophthalmol. 1985;103:1796–1806. [PubMed] [Google Scholar]
- 87.Early Treatment Diabetic Retinopathy Study Research Group Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1987;94:761–774. doi: 10.1016/s0161-6420(87)33527-4. [DOI] [PubMed] [Google Scholar]
- 88.Fong D.S., Segal P.P., Myers F., Ferris F.L., Hubbard L.D., Davis M.D. Subretinal fibrosis in diabetic macular edema. ETDRS report 23. Early Treatment Diabetic Retinopathy Study Research Group. Arch. Ophthalmol. 1997;115:873–877. doi: 10.1001/archopht.1997.01100160043006. [DOI] [PubMed] [Google Scholar]
- 89.Writing Committee for the Diabetic Retinopathy Clinical Research Network. Fong D.S., Strauber S.F., Aiello L.P., Beck R.W., Callanan D.G., Danis R.P., Davis M.D., Feman S.S., Ferris F., et al. Comparison of the modified Early Treatment Diabetic Retinopathy Study and mild macular grid laser photocoagulation strategies for diabetic macular edema. Arch. Ophthalmol. 2007;125:469–480. doi: 10.1001/archopht.125.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ohkoshi K., Yamaguchi T. Subthreshold micropulse diode laser photocoagulation for diabetic macular edema in Japanese patients. Am. J. Ophthalmol. 2010;149:133–139. doi: 10.1016/j.ajo.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 91.Lavinsky D., Cardillo J.A., Melo L.A., Jr., Dare A., Farah M.E., Belfort R., Jr. Randomized clinical trial evaluating mETDRS versus normal or high-density micropulse photocoagulation for diabetic macular edema. Investig. Ophthalmol. Vis. Sci. 2011;52:4314–4323. doi: 10.1167/iovs.10-6828. [DOI] [PubMed] [Google Scholar]
- 92.Qiao G., Guo H.K., Dai Y., Wang X.L., Meng Q.L., Li H., Chen X.H., Chen Z.L. Sub-threshold micro-pulse diode laser treatment in diabetic macular edema: A Meta-analysis of randomized controlled trials. Int. J. Ophthalmol. 2016;9:1020–1027. doi: 10.18240/ijo.2016.07.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Inagaki K., Hamada M., Ohkoshi K. Minimally invasive laser treatment combined with intravitreal injection of anti-vascular endothelial growth factor for diabetic macular oedema. Sci. Rep. 2019;9:7585. doi: 10.1038/s41598-019-44130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sun J.K., Glassman A.R., Beaulieu W.T., Stockdale C.R., Bressler N.M., Flaxel C., Gross J.G., Shami M., Jampol L.M., Diabetic Retinopathy Clinical Research Network Rationale and Application of the Protocol S Anti-Vascular Endothelial Growth Factor Algorithm for Proliferative Diabetic Retinopathy. Ophthalmology. 2019;126:87–95. doi: 10.1016/j.ophtha.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gross J.G., Glassman A.R., Liu D., Sun J.K., Antoszyk A.N., Baker C.W., Bressler N.M., Elman M.J., Ferris F.L., III, Gardner T.W., et al. Five-Year Outcomes of Panretinal Photocoagulation vs Intravitreous Ranibizumab for Proliferative Diabetic Retinopathy: A Randomized Clinical Trial. JAMA Ophthalmol. 2018;136:1138–1148. doi: 10.1001/jamaophthalmol.2018.3255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Writing Committee for the Diabetic Retinopathy Clinical Research Network. Gross J.G., Glassman A.R., Jampol L.M., Inusah S., Aiello L.P., Antoszyk A.N., Baker C.W., Berger B.B., Bressler N.M., et al. Panretinal Photocoagulation vs Intravitreous Ranibizumab for Proliferative Diabetic Retinopathy: A Randomized Clinical Trial. JAMA. 2015;314:2137–2146. doi: 10.1001/jama.2015.15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sivaprasad S., Prevost A.T., Vasconcelos J.C., Riddell A., Murphy C., Kelly J., Bainbridge J., Tudor-Edwards R., Hopkins D., Hykin P., et al. Clinical efficacy of intravitreal aflibercept versus panretinal photocoagulation for best corrected visual acuity in patients with proliferative diabetic retinopathy at 52 weeks (CLARITY): A multicentre, single-blinded, randomised, controlled, phase 2b, non-inferiority trial. Lancet. 2017;389:2193–2203. doi: 10.1016/S0140-6736(17)31193-5. [DOI] [PubMed] [Google Scholar]
- 98.Lang G.E., Stahl A., Voegeler J., Quiering C., Lorenz K., Spital G., Liakopoulos S. Efficacy and safety of ranibizumab with or without panretinal laser photocoagulation versus laser photocoagulation alone in proliferative diabetic retinopathy—The PRIDE study. Acta Ophthalmol. 2019;98:e530–e539. doi: 10.1111/aos.14312. [DOI] [PubMed] [Google Scholar]
- 99.Lang G.E., Stahl A., Voegeler J., Quiering C., Zaremba L., Lorenz K., Spital G., Liakopoulos S. Observational outcomes in proliferative diabetic retinopathy patients following treatment with ranibizumab, panretinal laser photocoagulation or combination therapy—The non-interventional second year follow-up to the PRIDE study. Acta Ophthalmol. 2021 doi: 10.1111/aos.14907. [DOI] [PubMed] [Google Scholar]
- 100.Obeid A., Su D., Patel S.N., Uhr J.H., Borkar D., Gao X., Fineman M.S., Regillo C.D., Maguire J.I., Garg S.J., et al. Outcomes of Eyes Lost to Follow-up with Proliferative Diabetic Retinopathy That Received Panretinal Photocoagulation versus Intravitreal Anti-Vascular Endothelial Growth Factor. Ophthalmology. 2019;126:407–413. doi: 10.1016/j.ophtha.2018.07.027. [DOI] [PubMed] [Google Scholar]
- 101.Diabetic Retinopathy Clinical Research Network. Elman M.J., Aiello L.P., Beck R.W., Bressler N.M., Bressler S.B., Edwards A.R., Ferris F.L., III, Friedman S.M., Glassman A.R., et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117:1064–1077.e35. doi: 10.1016/j.ophtha.2010.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mitchell P., Bandello F., Schmidt-Erfurth U., Lang G.E., Massin P., Schlingemann R.O., Sutter F., Simader C., Burian G., Gerstner O., et al. The RESTORE study: Ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–625. doi: 10.1016/j.ophtha.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 103.Nguyen Q.D., Brown D.M., Marcus D.M., Boyer D.S., Patel S., Feiner L., Gibson A., Sy J., Rundle A.C., Hopkins J.J., et al. Ranibizumab for diabetic macular edema: Results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119:789–801. doi: 10.1016/j.ophtha.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 104.Korobelnik J.F., Do D.V., Schmidt-Erfurth U., Boyer D.S., Holz F.G., Heier J.S., Midena E., Kaiser P.K., Terasaki H., Marcus D.M., et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121:2247–2254. doi: 10.1016/j.ophtha.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 105.Brown D.M., Schmidt-Erfurth U., Do D.V., Holz F.G., Boyer D.S., Midena E., Heier J.S., Terasaki H., Kaiser P.K., Marcus D.M., et al. Intravitreal Aflibercept for Diabetic Macular Edema: 100-Week Results From the VISTA and VIVID Studies. Ophthalmology. 2015;122:2044–2052. doi: 10.1016/j.ophtha.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 106.Diabetic Retinopathy Clinical Research Network. Wells J.A., Glassman A.R., Ayala A.R., Jampol L.M., Aiello L.P., Antoszyk A.N., Arnold-Bush B., Baker C.W., Bressler N.M., et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N. Engl. J. Med. 2015;372:1193–1203. doi: 10.1056/NEJMoa1414264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wells J.A., Glassman A.R., Ayala A.R., Jampol L.M., Bressler N.M., Bressler S.B., Brucker A.J., Ferris F.L., Hampton G.R., Jhaveri C., et al. Aflibercept, Bevacizumab, or Ranibizumab for Diabetic Macular Edema: Two-Year Results from a Comparative Effectiveness Randomized Clinical Trial. Ophthalmology. 2016;123:1351–1359. doi: 10.1016/j.ophtha.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cai S., Bressler N.M. Aflibercept, bevacizumab or ranibizumab for diabetic macular oedema: Recent clinically relevant findings from DRCR.net Protocol T. Curr. Opin. Ophthalmol. 2017;28:636–643. doi: 10.1097/ICU.0000000000000424. [DOI] [PubMed] [Google Scholar]
- 109.Hirano T., Toriyama Y., Iesato Y., Imai A., Hirabayashi K., Nagaoka T., Takamura Y., Sugimoto M., Murata T. Effect of leaking perifoveal microaneurysms on resolution of diabetic macular edema treated by combination therapy using anti-vascular endothelial growth factor and short pulse focal/grid laser photocoagulation. JPN J. Ophthalmol. 2017;61:51–60. doi: 10.1007/s10384-016-0483-8. [DOI] [PubMed] [Google Scholar]
- 110.Fintak D.R., Shah G.K., Blinder K.J., Regillo C.D., Pollack J., Heier J.S., Hollands H., Sharma S. Incidence of endophthalmitis related to intravitreal injection of bevacizumab and ranibizumab. Retina. 2008;28:1395–1399. doi: 10.1097/IAE.0b013e3181884fd2. [DOI] [PubMed] [Google Scholar]
- 111.Hernandez-Pastor L.J., Ortega A., Garcia-Layana A., Giraldez J. Ranibizumab for neovascular age-related macular degeneration. Am. J. Health Syst. Pharm. 2008;65:1805–1814. doi: 10.2146/ajhp070342. [DOI] [PubMed] [Google Scholar]
- 112.Pearson P.A., Comstock T.L., Ip M., Callanan D., Morse L.S., Ashton P., Levy B., Mann E.S., Eliott D. Fluocinolone acetonide intravitreal implant for diabetic macular edema: A 3-year multicenter, randomized, controlled clinical trial. Ophthalmology. 2011;118:1580–1587. doi: 10.1016/j.ophtha.2011.02.048. [DOI] [PubMed] [Google Scholar]
- 113.Martidis A., Duker J.S., Greenberg P.B., Rogers A.H., Puliafito C.A., Reichel E., Baumal C. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002;109:920–927. doi: 10.1016/S0161-6420(02)00975-2. [DOI] [PubMed] [Google Scholar]
- 114.Jonas J.B., Sofker A., Hayler J., Degenring R.F. Intravitreal crystalline triamcinolone acetonide as an additional tool in pars plana vitrectomy for complicated proliferative vitreoretinopathy? Acta Ophthalmol. Scand. 2003;81:663–665. doi: 10.1046/j.1395-3907.2003.0108.x. [DOI] [PubMed] [Google Scholar]
- 115.Jeon S., Lee W.K. Effect of intravitreal triamcinolone in diabetic macular edema unresponsive to intravitreal bevacizumab. Retina. 2014;34:1606–1611. doi: 10.1097/IAE.0000000000000109. [DOI] [PubMed] [Google Scholar]
- 116.Kim J.H., Lee T.G., Lew Y.J. Short-term efficacy of intravitreal triamcinolone acetonide for bevacizumab-resistant diabetic macular oedema. Acta Ophthalmol. 2015;93:e178–e179. doi: 10.1111/aos.12504. [DOI] [PubMed] [Google Scholar]
- 117.Ahmadieh H., Ramezani A., Shoeibi N., Bijanzadeh B., Tabatabaei A., Azarmina M., Soheilian M., Keshavarzi G., Mohebbi M.R. Intravitreal bevacizumab with or without triamcinolone for refractory diabetic macular edema; a placebo-controlled, randomized clinical trial. Graefes. Arch. Clin. Exp. Ophthalmol. 2008;246:483–489. doi: 10.1007/s00417-007-0688-0. [DOI] [PubMed] [Google Scholar]
- 118.Entezari M., Ahmadieh H., Dehghan M.H., Ramezani A., Bassirnia N., Anissian A. Posterior sub-tenon triamcinolone for refractory diabetic macular edema: A randomized clinical trial. Eur. J. Ophthalmol. 2005;15:746–750. doi: 10.1177/112067210501500614. [DOI] [PubMed] [Google Scholar]
- 119.Bakri S.J., Kaiser P.K. Posterior subtenon triamcinolone acetonide for refractory diabetic macular edema. Am. J. Ophthalmol. 2005;139:290–294. doi: 10.1016/j.ajo.2004.09.038. [DOI] [PubMed] [Google Scholar]
- 120.Choi Y.J., Oh I.K., Oh J.R., Huh K. Intravitreal versus posterior subtenon injection of triamcinolone acetonide for diabetic macular edema. Korean J. Ophthalmol. 2006;20:205–209. doi: 10.3341/kjo.2006.20.4.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Qi H.P., Bi S., Wei S.Q., Cui H., Zhao J.B. Intravitreal versus subtenon triamcinolone acetonide injection for diabetic macular edema: A systematic review and meta-analysis. Curr. Eye Res. 2012;37:1136–1147. doi: 10.3109/02713683.2012.705412. [DOI] [PubMed] [Google Scholar]
- 122.Shimura M., Yasuda K., Minezaki T., Noma H. Reduction in the frequency of intravitreal bevacizumab administrations achieved by posterior subtenon injection of triamcinolone acetonide in patients with diffuse diabetic macular edema. JPN J. Ophthalmol. 2016;60:401–407. doi: 10.1007/s10384-016-0458-9. [DOI] [PubMed] [Google Scholar]
- 123.Rishi P., Rishi E., Attiku Y., Dhami A., Iyer V. Real-world experience with pro re nata dosing of intravitreal dexamethasone implant for eyes with refractory diabetic macular edema. GMS Ophthalmol. Cases. 2020;10:Doc21. doi: 10.3205/oc000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bansal P., Gupta V., Gupta A., Dogra M.R., Ram J. Efficacy of Ozurdex implant in recalcitrant diabetic macular edema—A single-center experience. Int. Ophthalmol. 2016;36:207–216. doi: 10.1007/s10792-015-0103-5. [DOI] [PubMed] [Google Scholar]
- 125.Totan Y., Guler E., Guragac F.B. Dexamethasone Intravitreal Implant for Chronic Diabetic Macular Edema Resistant to Intravitreal Bevacizumab Treatment. Curr. Eye Res. 2016;41:107–113. doi: 10.3109/02713683.2014.1002048. [DOI] [PubMed] [Google Scholar]
- 126.Shah A.R., Xi M., Abbey A.M., Yonekawa Y., Faia L.J., Hassan T.S., Ruby A.J., Wolfe J.D. Short-term Efficacy of Intravitreal Dexamethasone Implant in Vitrectomized Eyes with Recalcitrant Diabetic Macular Edema and Prior Anti-VEGF Therapy. J. Ophthalmic. Vis. Res. 2016;11:183–187. doi: 10.4103/2008-322X.183928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Maturi R.K., Glassman A.R., Liu D., Beck R.W., Bhavsar A.R., Bressler N.M., Jampol L.M., Melia M., Punjabi O.S., Salehi-Had H., et al. Effect of Adding Dexamethasone to Continued Ranibizumab Treatment in Patients With Persistent Diabetic Macular Edema: A DRCR Network Phase 2 Randomized Clinical Trial. JAMA Ophthalmol. 2018;136:29–38. doi: 10.1001/jamaophthalmol.2017.4914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Coney J.M. Fluocinolone acetonide 0.19 mg intravitreal implant improves foveal thickness and reduces treatment burden for up to 1 year in eyes with persistent diabetic macular edema. Int. Med. Case Rep. J. 2019;12:161–169. doi: 10.2147/IMCRJ.S192524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chronopoulos A., Chronopoulos P., Ashurov A., Korb C., Pfeiffer N., Hattenbach L.O. Switching to intravitreal fluocinolone acetonide implant for refractory diabetic macular edema: 12- and 24-month results. Eur. J. Ophthalmol. 2021:1120672121992982. doi: 10.1177/1120672121992982. [DOI] [PubMed] [Google Scholar]
- 130.McCluskey J.D., Kaufman P.L., Wynne K., Lewis G. Early adoption of the fluocinolone acetonide (FAc) intravitreal implant in patients with persistent or recurrent diabetic macular edema (DME) Int. Med. Case Rep. J. 2019;12:93–102. doi: 10.2147/IMCRJ.S191171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Pessoa B., Coelho J., Correia N., Ferreira N., Beirao M., Meireles A. Fluocinolone Acetonide Intravitreal Implant 190 mug (ILUVIEN(R)) in Vitrectomized versus Nonvitrectomized Eyes for the Treatment of Chronic Diabetic Macular Edema. Ophthalmic Res. 2018;59:68–75. doi: 10.1159/000484091. [DOI] [PubMed] [Google Scholar]
- 132.Massin P., Erginay A., Dupas B., Couturier A., Tadayoni R. Efficacy and safety of sustained-delivery fluocinolone acetonide intravitreal implant in patients with chronic diabetic macular edema insufficiently responsive to available therapies: A real-life study. Clin. Ophthalmol. 2016;10:1257–1264. doi: 10.2147/OPTH.S105385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Grover D., Li T.J., Chong C.C. Intravitreal steroids for macular edema in diabetes. Cochrane Database Syst. Rev. 2008:CD005656. doi: 10.1002/14651858.CD005656.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kocabora M.S., Yilmazli C., Taskapili M., Gulkilik G., Durmaz S. Development of ocular hypertension and persistent glaucoma after intravitreal injection of triamcinolone. Clin. Ophthalmol. 2008;2:167–171. doi: 10.2147/OPTH.S2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cekic O., Chang S., Tseng J.J., Akar Y., Barile G.R., Schiff W.M. Cataract progression after intravitreal triamcinolone injection. Am. J. Ophthalmol. 2005;139:993–998. doi: 10.1016/j.ajo.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 136.Jonisch J., Lai J.C., Deramo V.A., Flug A.J., Fastenberg D.M. Increased incidence of sterile endophthalmitis following intravitreal preserved triamcinolone acetonide. Br. J. Ophthalmol. 2008;92:1051–1054. doi: 10.1136/bjo.2007.136069. [DOI] [PubMed] [Google Scholar]
- 137.Mason R.H., Ballios B.G., Yan P. Noninfectious endophthalmitis following intravitreal triamcinolone acetonide: Clinical case and literature review. Can. J. Ophthalmol. 2020;55:471–479. doi: 10.1016/j.jcjo.2020.06.002. [DOI] [PubMed] [Google Scholar]
- 138.Eckardt C. Transconjunctival sutureless 23-gauge vitrectomy. Retina. 2005;25:208–211. doi: 10.1097/00006982-200502000-00015. [DOI] [PubMed] [Google Scholar]
- 139.Tomita Y., Kurihara T., Uchida A., Nagai N., Shinoda H., Tsubota K., Ozawa Y. Wide-Angle Viewing System versus Conventional Indirect Ophthalmoscopy for Scleral Buckling. Sci. Rep. 2015;5:13256. doi: 10.1038/srep13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Fujii G.Y., De Juan E., Jr., Humayun M.S., Pieramici D.J., Chang T.S., Awh C., Ng E., Barnes A., Wu S.L., Sommerville D.N. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109:1807–1812. doi: 10.1016/S0161-6420(02)01179-X. [DOI] [PubMed] [Google Scholar]
- 141.Inoue M. Wide-angle viewing system. Dev. Ophthalmol. 2014;54:87–91. doi: 10.1159/000360453. [DOI] [PubMed] [Google Scholar]
- 142.Oellers P., Mahmoud T.H. Surgery for Proliferative Diabetic Retinopathy: New Tips and Tricks. J. Ophthalmic Vis. Res. 2016;11:93–99. doi: 10.4103/2008-322X.180697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zhang Z.H., Liu H.Y., Hernandez-Da Mota S.E., Romano M.R., Falavarjani K.G., Ahmadieh H., Xu X., Liu K. Vitrectomy with or without preoperative intravitreal bevacizumab for proliferative diabetic retinopathy: A meta-analysis of randomized controlled trials. Am. J. Ophthalmol. 2013;156:106–115.e102. doi: 10.1016/j.ajo.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 144.Zhao X.Y., Xia S., Chen Y.X. Antivascular endothelial growth factor agents pretreatment before vitrectomy for complicated proliferative diabetic retinopathy: A meta-analysis of randomised controlled trials. Br. J. Ophthalmol. 2018;102:1077–1085. doi: 10.1136/bjophthalmol-2017-311344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Berrocal M.H., Acaba L.A., Acaba A. Surgery for Diabetic Eye Complications. Curr. Diab. Rep. 2016;16:99. doi: 10.1007/s11892-016-0787-6. [DOI] [PubMed] [Google Scholar]
- 146.Khuthaila M.K., Hsu J., Chiang A., DeCroos F.C., Milder E.A., Setlur V., Garg S.J., Spirn M.J. Postoperative vitreous hemorrhage after diabetic 23-gauge pars plana vitrectomy. Am. J. Ophthalmol. 2013;155:757–763.e2. doi: 10.1016/j.ajo.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 147.Park D.H., Shin J.P., Kim S.Y. Comparison of clinical outcomes between 23-gauge and 20-gauge vitrectomy in patients with proliferative diabetic retinopathy. Retina. 2010;30:1662–1670. doi: 10.1097/IAE.0b013e3181d95261. [DOI] [PubMed] [Google Scholar]
- 148.Tachi N., Ogino N. Vitrectomy for diffuse macular edema in cases of diabetic retinopathy. Am. J. Ophthalmol. 1996;122:258–260. doi: 10.1016/S0002-9394(14)72018-5. [DOI] [PubMed] [Google Scholar]
- 149.Yamamoto T., Hitani K., Tsukahara I., Yamamoto S., Kawasaki R., Yamashita H., Takeuchi S. Early postoperative retinal thickness changes and complications after vitrectomy for diabetic macular edema. Am. J. Ophthalmol. 2003;135:14–19. doi: 10.1016/S0002-9394(02)01819-6. [DOI] [PubMed] [Google Scholar]
- 150.Lewis H., Abrams G.W., Blumenkranz M.S., Campo R.V. Vitrectomy for diabetic macular traction and edema associated with posterior hyaloidal traction. Ophthalmology. 1992;99:753–759. doi: 10.1016/S0161-6420(92)31901-3. [DOI] [PubMed] [Google Scholar]
- 151.Park D.W., Dugel P.U., Garda J., Sipperley J.O., Thach A., Sneed S.R., Blaisdell J. Macular pucker removal with and without internal limiting membrane peeling: Pilot study. Ophthalmology. 2003;110:62–64. doi: 10.1016/S0161-6420(02)01440-9. [DOI] [PubMed] [Google Scholar]
- 152.Kumagai K., Furukawa M., Ogino N., Larson E., Iwaki M., Tachi N. Long-term follow-up of vitrectomy for diffuse nontractional diabetic macular edema. Retina. 2009;29:464–472. doi: 10.1097/IAE.0b013e31819c632f. [DOI] [PubMed] [Google Scholar]
- 153.Doi N., Sakamoto T., Sonoda Y., Yasuda M., Yonemoto K., Arimura N., Uchino E., Ishibashi T. Comparative study of vitrectomy versus intravitreous triamcinolone for diabetic macular edema on randomized paired-eyes. Graefes Arch. Clin. Exp. Ophthalmol. 2012;250:71–78. doi: 10.1007/s00417-011-1777-7. [DOI] [PubMed] [Google Scholar]
- 154.Kumagai K., Hangai M., Ogino N., Larson E. Effect of Internal Limiting Membrane Peeling on Long-Term Visual Outcomes for Diabetic Macular Edema. Retina. 2015;35:1422–1428. doi: 10.1097/IAE.0000000000000497. [DOI] [PubMed] [Google Scholar]
- 155.Simunovic M.P., Hunyor A.P., Ho I.V. Vitrectomy for diabetic macular edema: A systematic review and meta-analysis. Can. J. Ophthalmol. 2014;49:188–195. doi: 10.1016/j.jcjo.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 156.Imai H., Tetsumoto A., Yamada H., Hayashida M., Otsuka K., Miki A., Kusuhara S., Nakamura M. Long-Term Effect of Cystotomy with or without the Fibrinogen Clot Removal for Refractory Cystoid Macular Edema Secondary to Diabetic Retinopathy. Retina. 2021;41:844–851. doi: 10.1097/IAE.0000000000002921. [DOI] [PubMed] [Google Scholar]
- 157.Oosterveer M.H., Grefhorst A., van Dijk T.H., Havinga R., Staels B., Kuipers F., Groen A.K., Reijngoud D.-J. Fenofibrate simultaneously induces hepatic fatty acid oxidation, synthesis, and elongation in mice. J. Biol. Chem. 2009;284:34036–34044. doi: 10.1074/jbc.M109.051052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Arai T., Kim H.-J., Chiba H., Matsumoto A. Interaction of Fenofibrate and Fish Oil in Relation to Lipid Metabolism in Mice. J. Atheroscler. Thromb. 2009;16:283–291. doi: 10.5551/jat.E463. [DOI] [PubMed] [Google Scholar]
- 159.Sasaki J., Yamamoto K., Ageta M. Effects of fenofibrate on high-density lipoprotein particle size in patients with hyperlipidemia: A randomized, double-blind, placebo-controlled, multicenter, crossover study. Clin. Ther. 2002;24:1614–1626. doi: 10.1016/S0149-2918(02)80064-9. [DOI] [PubMed] [Google Scholar]
- 160.Mellies M.J., Stein E.A., Khoury P., Lamkin G., Glueck C.J. Effects of fenofibrate on lipids, lipoproteins, and apolipoproteins in 33 subjects with primary hypercholesterolemia. Atherosclerosis. 1987;63:57–64. doi: 10.1016/0021-9150(87)90082-7. [DOI] [PubMed] [Google Scholar]
- 161.Sharma R., Mahajan M., Singh B., Bal B.S., Kant R. Apolipoprotein modifying effects of statins and fibrate in various age groups of coronary artery disease patients. J. Indian Med. Assoc. 2006;104:492–494, 496, 498. [PubMed] [Google Scholar]
- 162.Guay D.R. Micronized fenofibrate: A new fibric acid hypolipidemic agent. Ann. Pharmacother. 1999;33:1083–1103. doi: 10.1345/aph.18432. [DOI] [PubMed] [Google Scholar]
- 163.Keech A., Simes R.J., Barter P., Best J., Scott R., Taskinen M.R., Forder P., Pillai A., Davis T., Glasziou P., et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): Randomised controlled trial. Lancet. 2005;366:1849–1861. doi: 10.1016/S1567-5688(06)81349-8. [DOI] [PubMed] [Google Scholar]
- 164.ACCORD Study Group. ACCORD Eye Study Group. Chew E.Y., Ambrosius W.T., Davis M.D., Danis R.P., Gangaputra S., Greven C.M., Hubbard L., Esser B.A., et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. N. Engl. J. Med. 2010;363:233–244. doi: 10.1056/NEJMoa1001288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Bogdanov P., Hernández C., Corraliza L., Carvalho A.R., Simó R. Effect of fenofibrate on retinal neurodegeneration in an experimental model of type 2 diabetes. Acta Diabetol. 2015;52:113–122. doi: 10.1007/s00592-014-0610-2. [DOI] [PubMed] [Google Scholar]
- 166.Wang N., Zou C., Zhao S., Wang Y., Han C., Zheng Z. Fenofibrate Exerts Protective Effects in Diabetic Retinopathy via Inhibition of the ANGPTL3 Pathway. Investig. Ophthalmol. Vis. Sci. 2018;59:4210–4217. doi: 10.1167/iovs.18-24155. [DOI] [PubMed] [Google Scholar]
- 167.Liu Q., Zhang F., Zhang X., Cheng R., Ma J.-X., Yi J., Li J. Fenofibrate ameliorates diabetic retinopathy by modulating Nrf2 signaling and NLRP3 inflammasome activation. Mol. Cell. Biochem. 2018;445:105–115. doi: 10.1007/s11010-017-3256-x. [DOI] [PubMed] [Google Scholar]
- 168.Kostapanos M.S., Florentin M., Elisaf M.S. Fenofibrate and the kidney: An overview. Eur. J. Clin. Investig. 2013;43:522–531. doi: 10.1111/eci.12068. [DOI] [PubMed] [Google Scholar]
- 169.Jun M., Zhu B., Tonelli M., Jardine M.J., Patel A., Neal B., Liyanage T., Keech A., Cass A., Perkovic V. Effects of Fibrates in Kidney Disease: A Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2012;60:2061–2071. doi: 10.1016/j.jacc.2012.07.049. [DOI] [PubMed] [Google Scholar]
- 170.Kim S., Ko K., Park S., Lee D.R., Lee J. Effect of Fenofibrate Medication on Renal Function. Korean J. Fam. Med. 2017;38:192–198. doi: 10.4082/kjfm.2017.38.4.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ida S., Kaneko R., Murata K. Efficacy and safety of pemafibrate administration in patients with dyslipidemia: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2019;18:38. doi: 10.1186/s12933-019-0845-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Fruchart J.-C. Pemafibrate (K-877), a novel selective peroxisome proliferator-activated receptor alpha modulator for management of atherogenic dyslipidaemia. Cardiovasc. Diabetol. 2017;16:124. doi: 10.1186/s12933-017-0602-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Suto K., Fukuda D., Shinohara M., Ganbaatar B., Yagi S., Kusunose K., Yamada H., Soeki T., Hirata K.-I., Sata M. Pemafibrate, A Novel Selective Peroxisome Proliferator-Activated Receptor α Modulator, Reduces Plasma Eicosanoid Levels and Ameliorates Endothelial Dysfunction in Diabetic Mice. J. Atheroscler. Thromb. 2021:61101. doi: 10.5551/jat.61101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Horikawa T., Kawanami T., Hamaguchi Y., Tanaka Y., Kita S., Ryorin R., Takashi Y., Takahashi H., Tanabe M., Yanase T., et al. Pemafibrate, a PPAR alpha agonist, attenuates neointima formation after vascular injury in mice fed normal chow and a high-fat diet. Heliyon. 2020;6:e05431. doi: 10.1016/j.heliyon.2020.e05431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tomita Y., Lee D., Miwa Y., Jiang X., Ohta M., Tsubota K., Kurihara T. Pemafibrate Protects Against Retinal Dysfunction in a Murine Model of Diabetic Retinopathy. Int. J. Mol. Sci. 2020;21:6243. doi: 10.3390/ijms21176243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Shiono A., Sasaki H., Sekine R., Abe Y., Matsumura Y., Inagaki T., Tanaka T., Kodama T., Aburatani H., Sakai J., et al. PPARα activation directly upregulates thrombomodulin in the diabetic retina. Sci. Rep. 2020;10:10837. doi: 10.1038/s41598-020-67579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Fujita N., Sase K., Tsukahara C., Arizono I., Takagi H., Kitaoka Y. Pemafibrate prevents retinal neuronal cell death in NMDA-induced excitotoxicity via inhibition of p-c-Jun expression. Mol. Biol. Rep. 2021;48:195–202. doi: 10.1007/s11033-020-06032-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Tomita Y., Ozawa N., Miwa Y., Ishida A., Ohta M., Tsubota K., Kurihara T. Pemafibrate Prevents Retinal Pathological Neovascularization by Increasing FGF21 Level in a Murine Oxygen-Induced Retinopathy Model. Int. J. Mol. Sci. 2019;20:5878. doi: 10.3390/ijms20235878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Klein R., Klein B.E., Moss S.E., Davis M.D., DeMets D.L. The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch. Ophthalmol. 1984;102:520–526. doi: 10.1001/archopht.1984.01040030398010. [DOI] [PubMed] [Google Scholar]
- 180.Nielsen N.V. Diabetic retinopathy I. The course of retinopathy in insulin-treated diabetics. A one year epidemiological cohort study of diabetes mellitus. The Island of Falster, Denmark. Acta Ophthalmol. 1984;62:256–265. doi: 10.1111/j.1755-3768.1984.tb08402.x. [DOI] [PubMed] [Google Scholar]
- 181.Kawasaki R., Tanaka S., Tanaka S., Yamamoto T., Sone H., Ohashi Y., Akanuma Y., Yamada N., Yamashita H., Japan Diabetes Complications Study Group Incidence and progression of diabetic retinopathy in Japanese adults with type 2 diabetes: 8 year follow-up study of the Japan Diabetes Complications Study (JDCS) Diabetologia. 2011;54:2288–2294. doi: 10.1007/s00125-011-2199-0. [DOI] [PubMed] [Google Scholar]
- 182.Diep T.M., Tsui I. Risk factors associated with diabetic macular edema. Diabetes Res. Clin. Pract. 2013;100:298–305. doi: 10.1016/j.diabres.2013.01.011. [DOI] [PubMed] [Google Scholar]