Abstract
Early evidence of disproportionate COVID-19 infection and death rates in Native Hawaiian and Pacific Islander communities in the continental US raised concerns for similar disparities in Hawai‘i, where these communities make up 25% of the state's population. Representatives from more than 40 different government, academic, institutional and community-based organizations partnered to form the Hawai‘i Native Hawaiian and Pacific Islander COVID-19 Response, Recovery, and Resilience Team. The team consists of 5 committees including the Data & Research Committee. This committee is tasked with examining issues regarding the acquisition, quality, public reporting, and utilization of race/ethnicity-related health data used to inform priorities and guide resource allocation. Problems addressed by this committee include: inconsistency across agencies in the use of race identifiers, defaulting to the Office of Management and Budget standards which aggregated Native Hawaiian and Pacific Islanders, and methods of data collection and reporting by the Department of Health. Outcomes include: 2 forms with race categories that reflect the population of Hawai‘i; the reporting of disaggregated data by the Department of Health; and conversations with testing sites, laboratories, and health institutions urging a standardized form for race/ethnicity data collection. The collection and reporting of disaggregated race/ethnicity data is critical to guiding organizations in addressing underlying inequities in chronic disease and social determinants of health that can exacerbate the adverse effects of COVID-19. The Data and Research Committee's network offers a community-based model for collaborative work that honors culture and ensures Native Hawaiian, Pacific Islander, and other minority populations are recognized and counted.
Keywords: Native Hawaiian (NH), Pacific Islander (PI), data disaggregation, health disparities, COVID-19
Highlights
The COVID-19 pandemic highlighted the health disparities of NHPI populations.
Utilizing inclusive community-based collaborations ensure effective outcomes.
Disaggregation of race data is critical to informing NHPI disparity related policy.
Data collection processes need to be standardized.
Komo mai kau māpuna hoe.
“Dip your paddle in.”
(Everyone pitch in.)1
Introduction
The ‘ōlelo no‘eau (Native Hawaiian proverb) quoted above reflects the unprecedented response by Native Hawaiians and Pacific Islanders (NHPI) to work quickly and collaboratively to confront the staggering disparate impacts of COVID-19 on their communities. Nationally, NHPI communities are quite small (0.4% of the US population) and their issues frequently go unnoticed.2 However, early in the pandemic, concerns were raised by NHPI health advocates in the continental US that NHPI communities were being impacted disproportionately by COVID-19.3 Unfortunately, it was difficult to gain a clear understanding of the situation early in the pandemic, because most states did not disaggregate or even report NHPI COVID-19 data.3–6 The COVID-19 pandemic highlighted a range of data-related deficiencies with respect to how race/ethnicity data are collected, reported, and used, and the need for collaboration among government agencies, health care systems, and community leaders in Hawai‘i as well as nationally.
NHPI have long advocated for disaggregated racial data to best inform programmatic and policy efforts to effectively address health disparities.7 The COVID-19 pandemic further underscored the need for disaggregated race/ethnicity data to inform COVID-19 response and recovery efforts.4,5 The 1997 update to the Office of Management and Budget (OMB) federal race and ethnicity classification designated 5 basic racial groups, finally separating “Native Hawaiian or Other Pacific Islander” from the “Asian” category.8 Table 1 illustrates the revised OMB race and ethnicity classification standards.
Table 1.
Office of Budget and Management (OMB) Standards for the Classification of Federal Data on Race and Ethnicity (1997)
| Standards for Collection |
|---|
| Ethnic categories |
| Hispanic or Latino |
| Race categories |
| American Indian or Alaska Native |
| Asian |
| Black or African American |
| Native Hawaiian or Other Pacific Islander |
| White |
In the current paper, “Native Hawaiians” (NHs) refers to the original inhabitants of the Hawaiian archipelago, and “Pacific Islanders” (PIs) refers to the original inhabitants of the islands of Oceania. NHPI refers to a diverse group of peoples with distinct languages, cultures, and political affiliations with the US.
The minimum level of collection and reporting of race and ethnicity data to federal agencies must comply with the revised OMB Standards (1997). Although states can collect and report more granular categories for their own purposes, such categories must be rolled into the OMB classification categories when reporting data to federal agencies. The aggregation of such categories such as grouping NH with PI at both the federal and state level masks the differential social, political, economic, and health impacts that health crises, such as the COVID-19 pandemic, have on specific communities.
In Hawai‘i, NHs and a diverse community of PIs (eg, Samoan, Tongan, Chuukese, and Marshallese) make up more than 21% and 4% of the state's population, respectively. NHPI combined comprise 25% of the population of Hawai‘i and, depending on what agency is reporting, might encompass anywhere from 7 to more than 30 different PI groups.9–11 Thus, there is a need to further disaggregate NH and PI data to understand the unique needs of distinct PI populations.
Current data collection methodologies and tools widely applied in Hawai‘i and elsewhere lack the needed specificity and validity to capture relevant data, including data that are critical to making important policy and resource-allocation decisions, especially during a public health crisis. A timeline of events showing data availability in 2020 for NHPI populations can be seen in Figure 1. This timeline illustrates how national problems in race/ethnicity-related data collection, such as the failure to look for and gather race/ethnicity-related data, led to a delay in recognizing the disparate impacts of COVID-19 on the NHPI community both nationally and locally.3,5–6,19–29
Figure 1.
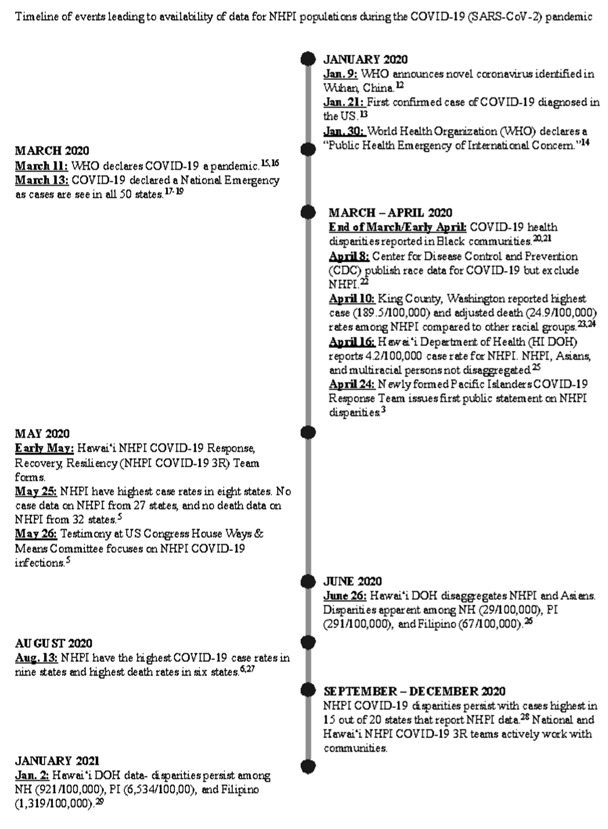
Timeline of Events Leading to Availability of Data for NHPI Populations During the COVID-19 (SARS-CoV-2) Pandemic
When the Centers for Disease Control and Prevention (CDC) first published race/ethnicity data regarding COVID-19 on April 8, 2020, NHPI data were not included.22 Hints of NHPI disparities started with reports in early April from Seattle, Washington, showing NHPI with the highest case rates of all racial/ethnic groups.23,24 By April 24, NHPI had the highest case rates in Washington, California, Utah, Oregon, and Hawai‘i.3 One month later, NHPI had the highest case rates in 8 of the 10 states that reported NHPI data.28 Unfortunately many states were not reporting NHPI data, and 2 reported NHPI data aggregated with Asians. By early June 2020, there were still 27 states that did not report NHPI COVID-19 case rate data.5
With many states not reporting race data for COVID-19, members of Congress and health care advocates rallied together to demand the reporting of race and ethnicity data for COVID-19 cases, hospitalizations, and deaths to fulfill “the need for comprehensive patient demographic data to better identify these racial and ethnic disparities, and to be able to respond with increased resources for prevention, testing, and treatment among populations experiencing those disparities.”5 By the first week of 2021, in 16 of the 21 states that reported NHPI data, NHPI had the highest per capita COVID-19 case rate of any racial/ethnic group.28,29
As of January 4, 2021, Hawai‘i, the only state to disaggregate NH from PI, reported the per capita cumulative case rate (unadjusted for age) for NHPI as 1 830 per 100 000 compared to 795 per 100 000 for non-NHPI. The NHPI population comprised 43% of COVID-19 cases. More specifically, PIs, who are 4% of the state population, comprised 25% of cases and had a cumulative case rate of 6 534/100 000 (Figure 1).29 At that time, 30% of the data were still missing due to a backlog at the State of Hawai‘i Department of Health, raising questions as to whether the disparity might be even worse than previously reported.29
NHPI suffer from disproportionately higher rates of comorbidities such as obesity, diabetes, cardiovascular disease, and asthma, which are known risk factors for severe COVID-19 related illness or death.30 Health and social determinants' disparities within the NHPI community, as with other marginalized communities in the US, place NHPI populations at greater risk for COVID-19 infections and adverse outcomes.30–34 The lack of a standard and culturally responsive protocol for data collection, management, and reporting make it difficult for health care organizations and government agencies to recognize and therefore adequately address and implement appropriate responses to not only COVID-19, but also to the underlying chronic conditions driving NHPI health and socioeconomic disparities.
Methodology: The Efforts of the Data and Research Committee
To address the adverse impact of COVID-19 on the social, cultural, economic, and health conditions of NHPI communities as well as the data deficiencies described earlier, the Hawai‘i Native Hawaiian and Pacific Islander COVID-19 Response, Recovery, and Resilience Team (NHPI 3R Team) was formed. This section describes the structure of the NHPI 3R Team, the specific role of the Data and Research Committee (DRC), and how the collaborative nature of this committee addressed the data deficiencies identified. The authors are all members of the DRC.
The NHPI 3R Team, a collective of more than 40 organizations that directly serves NHPI communities, was formed in May 2020 to address NHPI COVID-19 related disparities. The NHPI 3R Team has 4 Co-Leads (2 NHs and 2 PIs) and 5 committees: (1) Testing, Contact Tracing and Isolation, (2) Policy, (3) Social Supports and Recovery, (4) Communication, and (5) Data and Research. Partners include government agencies, academic groups, and community groups (both nonprofit and grassroots). The organizational structure of the 3R Team can be seen in Figure 2.
Figure 2.
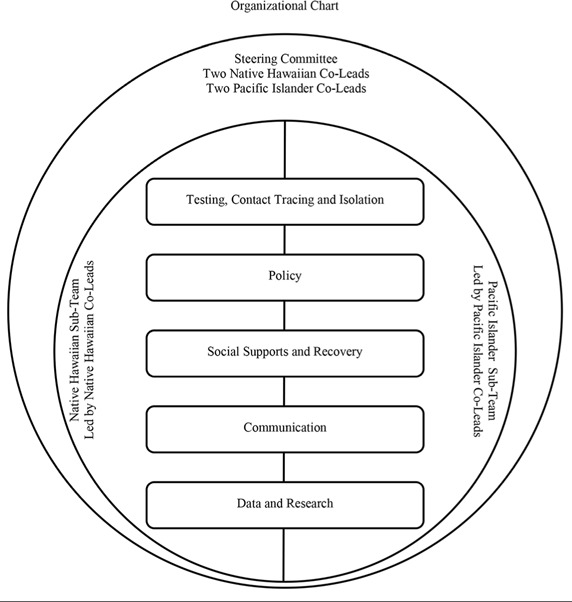
The Hawai‘i Native Hawaiian Pacific Islander Response, Recovery, and Resiliency Team (NHPI 3R Team)
When the NHPI 3R team was formed in May 2020, there were significant gaps in data needed to accurately assess the impact of COVID-19 on NHPI in Hawai‘i, including insufficient, inconsistent, untimely, and inaccessible data across various state and county departments and health care organizations. The Data and Research Committee (DRC) of the NHPI 3R team was formed to address these issues. Soon after, the Kūkākūkā Data Disaggregation Hui sponsored by the Office of Hawaiian Affairs (OHA), a group with similar interests in addressing issues around NHPI data, merged with the DRC.
NHPI 3R Team's Data and Research Committee (DRC) was designed to be a flexible and fluid network consisting of various organizations and governmental agencies with shared core values and a passion for eliminating NHPI health disparities as spotlighted by the COVID-19 pandemic. Current DRC members, which include the authors, belong to a wide range of organizations, which are summarized in Table 2.
Table 2.
Members of the Data and Research Committee
| Organization | Type |
|---|---|
| Office of Hawaiian Affairs | Government |
| Hawai‘i State Department of Health | Government |
| Department of Hawaiian Homelands | Government |
| Papa Ola Lokahi | Non-profit |
| ‘Ahahui o na Kauka (Assn of NH Physicians) | Non-profit |
| Hawai‘i Pacific Health | Healthcare facility/system |
| Kokua Kalihi Valley | Healthcare facility/system |
| The Queen's Health systems | Healthcare facility/system |
| Waimanalo Health Center | Healthcare facility/system |
| Hawai‘i Pacific University | Academia |
| The University of Hawai‘i at Mānoa, John A. Burns School of Medicine, Department of Native Hawaiian Health | Academia |
| The University of Hawai‘i at Mānoa, Myron B. Thompson School of Social Work, Center on Aging, Pacific Health Analytics Collaborative | Academia |
The collective work of the NHPI 3R team is guided by NHPI core values. These core values were agreed upon at the formation of the NHPI 3R team by its members and include: pono (equity, just, virtuous), aloha (love, compassion), kuleana (right, privilege and responsibility), ‘ohana (family, relations), laulima (cooperation, joint action), and imua (movement forward, to advance). Also, cultural protocols and practices are at the forefront and woven into the work that is done to remind all team members of the importance of the work and to draw strength and guidance from ancestral and spiritual relations.
The purpose of the DRC is to ensure that NHPI data are disaggregated and to identify data and research gaps, develop a course of action to address these gaps, and provide recommendations. Important goals include ensuring that data on health disparities across racial/ethnic groups are no longer invisible so that needed policies and interventions can be created and resources can be allocated where most needed. More specifically, the DRC's goals are to:
-
(1)
Identify priorities and strategies to address the immediate data and research issues to better understand the COVID-19 impact on NHPI communities.
-
(2)
Establish long-term priorities for systemic change regarding data governance policies and procedures.
-
(3)
Build and strengthen a network of NHPI serving organizations, government agencies, and other community organizations to inform and support these goals.
Operationally, the weekly group meetings are conducted remotely and administratively supported by Papa Ola Lōkahi, also known as the Native Hawaiian Health Board. Table 3 shows the DRC data gaps and research needs identified, the activities conducted to address these needs, and the results of these efforts to date.
Table 3.
Responses to Data and Research Issues
| Data Issues | Responses/Activity | Result |
|---|---|---|
| Collection | ||
| Inconsistent collection of race/ethnicity identifiers across testing organizations including hospitals. | Reliance on OMB 15 Federal standards that aggregate Native Hawaiians and Pacific Islanders. | Ongoing advocacy for change with testing sites, labs, health institutions. |
| Management | ||
| Develop a data collection form that appropriately captures the racial and ethnic populations served by Hawai‘i hospitals and medical records. | Research project planned with two main hospital systems assessing the consistency of data entry, methods, forms, ease of use. | Race and ethnicity data collection. Long and Short forms developed. |
| Inconsistent data entry. The decision to initially focus on the backlog of NHPI race data entry at DOH. | Recruit individuals to follow up on missing race data and assist with data entry. | DRC partners recruited two staff members. Missing race data reduced from 52% to 19%. |
| Reporting | ||
| Lack of timely sharing of disaggregated NHPI data. | Develop a collaborative relationship with DOH/DOCD advocating for timely sharing. |
|
| Race data collected for positive cases but was not reported by disaggregated race and ethnicity categories. | Advocate for reporting by disaggregated race and ethnicity. | NHPI and Asians are disaggregated in COVID-19 reporting. |
| No disaggregated data reported for hospitalizations, deaths, and negative cases. | Support DOH efforts through a collaborative relationship. | Disaggregated data by race and ethnicity for hospitalization and deaths reported. |
| Limited understanding of the distribution of negative cases among NHPI. | Sub-team developed to consider accessing databases of negative cases from Hawai‘i Pacific Health and Queen's Health Systems hospitals. | Collaborative partnership with Hawai‘i Pacific Health and Queens Health Systems. Goals:
|
Achievements
In addition to the results summarized in Table 3, the following 3 primary activities illustrate the work of the DRC around COVID-19.
1. Development of a Race & Ethnicity Data Collection Form
Realizing that uniformity in the documentation of race was needed, the DRC created data collection forms to best represent the unique racial/ethnic demographics of Hawai‘i. Particularly, addressing the mixed-race category was important because 24.2% of Hawai‘i's population identifies as multiracial.35 Although the Department of Health (DOH) has a prioritization algorithm method for identifying primary race when reporting data,36 the DRC felt that allowing the respondents to self-identify their primary race would collect a more accurate reflection of their true racial/ethnic identity and any influences this may have on epidemiological outcomes. Building upon work started by the OHA Kūkākūkā Data Disaggregation Hui, a recommended list of 29 race/ethnicity categories was developed that included all known PI categories (Appendix 1). A shorter list with 12 race categories was also developed to address concerns about the length and time required to complete the form (Appendix 2). The DRC continues to look for opportunities to strongly advocate for the use of these forms.
2. Department of Health (DOH) Collaboration with the DRC
Early in the pandemic, as the first wave of COVID-19 cases were identified in Hawai‘i, race and ethnicity data were not routinely reported by the DOH despite the agency having these data.37 The first public release of race/ethnicity data by the DOH in mid-April, covering 450 confirmed cases, showed that persons identifying as white and NHPI were disproportionately more likely to be diagnosed with COVID-19.26 This crude stratification of the race/ethnicity data relied on the standard federally defined OMB categories. Also, NHPI numbers only reflected single race, not mixed-race, categories. The insufficiency of the existing federal race classification for predominantly Asian and Pacific Islander populations of Hawai‘i has been previously documented.38 However, several barriers prevented further disaggregation, including:
-
(1)
lack of access to disaggregated population reference data needed to detect disparities;
-
(2)
lack of consistent standardized methodology for persons of mixed-race; for example, some data collection protocols place mixed-race NHs into a “mixed-race” category or “other” category, which makes NHs invisible and does not reflect their actual ethnic identity; and
-
(3)
lack of appreciation for the importance of data disaggregation in informing appropriate COVID-19 policy and response efforts.
The DOH's partnership with the DRC was instrumental in helping the DOH's Disease Outbreak Control Division (DOCD) navigate data disaggregation challenges. From June 2020, epidemiologists from DOCD joined the DRC and attended weekly meetings to promote information sharing and discuss data challenges and related resources. As a result of this collaboration, there has been a change in the way that race/ethnicity data are reported. Table 4 shows the racial/ethnic categories reported by the DOH DOCD in April 2020 compared to when the agency started reporting disaggregated NHPI data in July 2020. Notably, as seen in Figure 3, disaggregation of the COVID-19 race/ethnic data in Hawai‘i revealed that the disparity observed among NHPI was concentrated in PI communities.29
Table 4.
Comparison of Race Categories from Hawaii DOH DOCD Case Report Forms April 2020 vs July 2020
| April 2020 Hawaii Case Report Form race categories | July 2020 Hawaii Revised Case Report Form race categories |
|---|---|
| Black | White |
| White | Native Hawaiian |
| Asian | Pacific Islander, specify: |
| American Indian/Alaska Native | Japanese |
| Native Hawaiian/Other Pacific Islander | Filipino |
| Unknown | Chinese |
| Other, specify: | Other Asian, specify: |
| Black | |
| Other, specify: |
Adapted from Centers for Disease Control and Prevention
Figure 3.
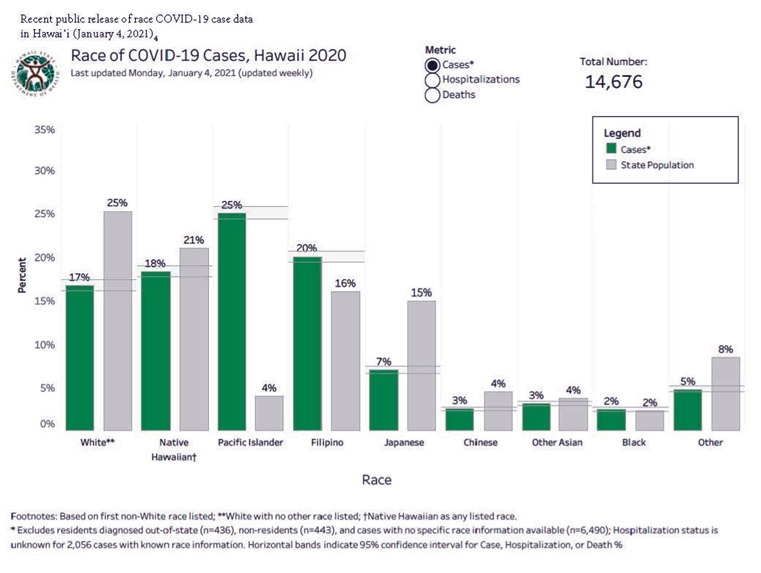
Race of COVID-19 Cases. Hawai‘i 2020
The collaboration also:
-
(1)
enabled DOH DOCD to receive input on the most effective, accurate, and culturally respectful way to publicly share more detailed COVID-19 race/ethnicity data;
-
(2)
provided guidance and mentorship to a DOH student researcher who began retrospectively collecting specific race/ethnicity data for disaggregation;
-
(3)
facilitated meetings with community stakeholders to present updated results;
-
(4)
enabled a partner to provide additional staff to help process the backlog of testing data; and
-
(5)
provided an opportunity for the team to work on a joint report detailing the race/ethnicity disparities in the state's COVID-19 data.
Additional collaborative efforts with the DOH Chronic Disease Prevention and Health Promotion Division, the Hawai‘i Health Data Warehouse, and the University of Hawa‘i at Mānoa Office of Public Health Studies allowed for sharing of information and the adoption of consistent data reporting standards across state programs.
The importance of interdepartmental and community partnerships and collaboration cannot be overstated. Without economic incentives (eg, federal grants) or local statutes in place to require data disaggregation, DOCD relied on a broad base of assistance to overcome significant barriers to disaggregation during a public health emergency. This assistance allowed DOCD to provide critical data needed to detect emerging COVID-19 disparities in Hawai‘i.
3. Hawai‘i Pacific Health and The Queen's Medical Center Collaboration with the DRC
There are gaps in data on COVID-19 testing in Hawai‘i because the DOH DOCD receives and reports on information only from patients with positive COVID-19 test results. The DRC has offered the opportunity for committee members with ties to 2 of the major health care systems in Hawai‘i, Hawai‘i Pacific Health and The Queen's Medical Center, to collaborate in discussions on how to utilize their electronic medical record databases to fill some of these gaps. The DOH DOCD contact tracing allows for additional detailed disaggregated race and ethnicity data collection from patients testing positive, but not for those who test negative. Hawai‘i Pacific Health and The Queen's Health Systems comprise the largest medical systems in the state of Hawai‘i and are responsible for a significant amount of COVID-19 testing, including testing symptomatic and exposed individuals as well as individuals requiring clearance for procedures, travel, or hospital admissions. Comprehensive review of electronic medical record data on sociodemographic characteristics such as race, age, gender, and place of residence from all patients who received COVID-19 testing regardless of test results could provide insight into how these factors may influence access and utilization of COVID-19 testing and testing sites.
Although race and ethnicity demographic information is part of patients' electronic medical records, these data may be incomplete or inconsistently documented. For example, some demographic categories within the medical record aggregate NH and PI into a single NHPI category, which makes it difficult to study differences between these 2 populations through medical chart review.
Institutional-level partnerships regarding shared patient data across health care systems in the past have been challenging due to competing financial priorities and regulations on sharing patient health information. However, health care institutions hold a wealth of patient clinical data that cannot be obtained reliably from self-report measures. With the need to address pandemic-related challenges including access to testing for NHPI populations, the DRC offered a valuable forum to: (1) bring together invested participants from these 2 health systems, (2) build a foundation of trust, and (3) discuss the potential for a future research project utilizing electronic medical records to further understand testing access and potential data gaps. The results of this research project collaboration would provide a rich source of information that could be utilized and shared with the DRC committee to aid that committee and others within the NHPI 3R team in identifying target areas to improve equitable health outcomes across NHPI communities.
Table 5 provides a summary of recommendations from the DRC regarding data governance and best practices for collaborating with NHPI communities.
Table 5.
DRC Recommendations
| Data Governance |
| Advocate for more accurate data collection, transparent data management, and disaggregated reporting across State departments and health institutions. |
| Promote the use of the categories in the DRC short form across departments in collecting race data. |
| Promote the importance of communication and transparency between all collaborators in partnerships with health institutions to obtain trust for managing sensitive patient data while respecting stakeholders' need for data ownership and independent analysis of data. |
| Advocate for OMB to eliminate the use of the “2 or more” category for multiple race classifications and replace it with a reporting schema similar to the Census Bureau reporting categories alone and in combination with one or more races. |
| Advocate for States to adopt data collection strategies that accurately reflect their populations by expanding the race categories available for selection and/or including the identification of a primary category as an additional question. |
| Advocate for States to create a minimum level of standardization across departments for the collection, management, and reporting of race data. |
| Promote and engage in solution-oriented discussions regarding the challenges of counting small populations (e.g. confidentiality). |
| Collaborating with Community |
| Collectively align goals and strategies across multiple stakeholders and institutions. |
| Collectively establish shared values to guide the work and partner relationships. |
| Identify stakeholders and additional collaborators across multiple institutions to aid in obtaining administrative, technological, and other resource funding. |
| Post-pandemic, government agencies need to continue to engage the NHPI community (e.g., advisory committees, stakeholder feedback sessions, etc.) with a particular emphasis on their inclusion to address health and social determinants of health inequities. |
Discussion
Although the membership is large and diverse, the success of the NHPI 3R Team and the DRC lies in the shared core values of pono, aloha, kuleana, ‘ohana, laulima, and imua that inspire the DRC to work for the betterment of Hawai‘i communities. The DRC's collaborative efforts have resulted in the creation and sharing of documents that list specific race/ethnicity categories for data collection that reflect the diverse population of Hawai‘i; a partnership with the DOH in reporting COVID-19 outcomes according to disaggregated NH, PI, and Asian race groups; and advocacy for accurate racial/ethnic data collection with partners conducting COVID-19 testing. Also, the DRC is actively identifying research needs to address data gaps and continuing to establish valuable cross-sector partnerships at the local, state, and national levels.
The DRC continues to meet regularly as the need remains for data collection and research pertinent to NHPI communities. As COVID vaccine efforts across the state continue, future efforts may include investigating the attitudes and perspectives of NHPI around COVID-19 vaccination and vaccine hesitancy to ensure vaccination equity in these communities.39 The DRC is also considering the continuation of the group to explore other issues that continue to impact NHPI physical and mental health, such as unexpected complications (eg, multisystem inflammatory syndrome in children) and long-term sequelae of COVID-19 (eg, long COVID-19) and their impact on socio-economic conditions and vice versa.40,41 Health disparities experienced by NHPI and other minority populations are masked by the aggregation of data for these groups, effectively eliminating visibility and acknowledgment of specific health needs. Health agencies, institutions, and organizations must collect accurate, meaningful data, including race data to better guide resource and policy decisions toward health equity.
Practical Implications
Obtaining disaggregated racial/ethnic data is paramount to understanding and developing effective policies addressing health inequities in chronic health conditions and other underlying risk factors that lead to disparities in COVID-19 outcomes.
Researchers and policymakers must actively engage with stakeholders within the NHPI community to ensure that accurate data are reported in a meaningful way that benefits NHPI communities and does not further stigmatize already marginalized NHPI populations.
A collaborative model that bridges key stakeholders across government, non-profit, academic, and community organizations while also adhering to cultural NHPI values can lead to more effective partnerships and utilization of combined resources.
This collaborative model creates opportunities for research and policy-setting in investigating other chronic disease disparities in the NHPI community.
Acknowledgments
Mahalo to Ignatius Bau for providing data references and review and to the DRC partners for their support.
Abbreviations
- CDC
Centers for Disease Control and Prevention
- COVID-19
coronavirus disease 2019 virus
- DOH
Department of Health
- DOCD
Disease Outbreak Control Division
- DRC
Data and Research Committee
- NH
Native Hawaiian
- NHPI
Native Hawaiian and Pacific Islander
- NHPI 3R Team
Hawai‘i Native Hawaiian and Pacific Islander COVID-19 Response, Recovery, and Resilience Team
- OHA
Office of Hawaiian Affairs
- OMB
Office of Management and Budget
- PI
Pacific Islander
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- US
United States
- WHO
World Health Organization
Appendix 1. Race/Ethnicity Data Collection Long Form
-
What is your race/ethnicity? (Check all that apply)
White or Caucasian
Black or African American
American Indian
Alaska Native
Asian Indian
Chinese
Filipino
Japanese
Korean
Vietnamese
Other Asian (please specify ______________)
Native Hawaiian
Chamorro
Samoan
Tongan
Fijian
Tahitian
Marshallese
Chuukese
Kosraean
Pohnpeian
Yapese
Palauan/Belauan
Nauruan
Kiribati
Other Pacific Islander (please specify ______________)
Other (please specify ______________)
Unknown
Refused/Prefer not to answer
-
Pick ONLY ONE of these groups which best represents your race and ethnicity.
-
a.
White or Caucasian
-
b.
Black or African American
-
c.
American Indian
-
d.
Alaska Native
-
e.
Asian Indian
-
f.
Chinese
-
g.
Filipino
-
h.
Japanese
-
i.
Korean
-
j.
Vietnamese
-
k.
Other Asian (please specify ______________)
-
l.
Native Hawaiian
-
m.
Chamorro
-
n.
Samoan
-
o.
Tongan
-
p.
Fijian
-
q.
Tahitian
-
r.
Marshallese
-
s.
Chuukese
-
t.
Kosraean
-
u.
Pohnpeian
-
v.
Yapese
-
w.
Palauan/Belauan
-
x.
Nauruan
-
y.
Kiribati
-
z.
Other Pacific Islander (please specify ______________)
-
aa.
Other (please specify ______________)
-
bb.
Unknown
-
cc.
Refused/Prefer not to answer
-
a.
What language do you prefer to use when discussing your health care? (fillable)_____________________________________________________
-
Interpreter needed?
Yes
No
Don't Know
Appendix 2. Race/Ethnicity Data Collection Short Form
-
What is your race/ethnicity? (Check all that apply)
White or Caucasian
Black or African American
American Indian or Alaska Native
Chinese
Filipino
Japanese
Other Asian (please specify ______________)
Native Hawaiian
Other Pacific Islander (please specify ______________)
Other (please specify ______________)
Unknown
Refused/Prefer not to answer
-
Pick ONLY ONE of these groups which best represents your race and ethnicity.
White or Caucasian
Black or African American
American Indian or Alaska Native
Chinese
Filipino
Japanese
Other Asian (please specify ______________)
Native Hawaiian
Other Pacific Islander (please specify ______________)
Other (please specify ______________)
Unknown
Refused/Prefer not to answer
What language do you prefer to use when discussing your health care? (fillable)_____________________________________________________
-
Interpreter needed?
Yes
No
Don't Know
Conflict of Interest
None of the authors identify any conflicts of interest.
References
- 1.Pukui MK, editor. ‘Olelo No‘eau: Hawaiian Proverbs & Poetical Sayings. Bishop Museum Press; 1983. [Google Scholar]
- 2.Native Hawaiian/Other Pacific Islander - The Office of Minority Health. Accessed April 8, 2021. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=65.
- 3.Pacific Islander Center of Primary Care Excellence, author. Devastating COVID-19 rate disparities ripping through Pacific Islander Communities in the U.S. Published online April 24, 2020. Accessed January 1, 2021. https://mk0picopce2kx432grq5.kinstacdn.com/wp-content/uploads/2020_0424-PICOPCE-COVID19-Press-Release.pdf.
- 4.National Council of Asian Pacific Islander Physicians, author. Recommendations for Comprehensive Patient Demographic Data Collection and Reporting for COVID-19 Testing and Treatment April 2020. Published online April 20, 2020. Accessed April 8, 2021. https://mcusercontent.com/d7f02dd24377959c916d14de6/files/52d07c5c-2317-433c-ab3a-a7639cb8ed21/NCAPIP_Recommendations_for_Patient_Demographic_Data_Related_to_COVID_19_April_2020.pdf.
- 5.National Council of Asian Pacific Islander Physicians, author. Disproportionate Impact of COVID-19 on Communities of Color: Hearings before the Senate Ways and Means Committee, US House of Representatives. 116th Congress. Published online June 9, 2020. Accessed January 1, 2021. https://waysandmeans.house.gov/sites/democrats.waysandmeans.house.gov/files/documents/NCAPIP%20Statement%20on%20COVID-19%20Disparities.pdf.
- 6.UCLA Center for Health Policy and Research, author. NHPI COVID-19 Data Policy Lab Dashboard. Tableau Software. Accessed August 13, 2020. https://healthpolicy.ucla.edu/health-profiles/Pages/NHPI-COVID-19-Dashboard.aspx.
- 7.Kaholokula JK, Yee BWK, Okamoto SK. Special issue introduction: Advancing Native Hawaiian and Other Pacific Islander health. Asian American Journal of Psychology. 2019;10((3)):197–205. [Google Scholar]
- 8.Office of Management and Budget, author. Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity, 62 FR 58782. Accessed January 2, 2021. https://www.govinfo.gov/app/details/FR-1997-10-30/97-28653.
- 9.State of Hawaii Department of Business, Economic Development and Tourism, author. State of Hawaii Data Book 2019. Published online 2019. Accessed January 5, 2021. https://files.hawaii.gov/dbedt/economic/databook/db2019/section01.pdf.
- 10.Nguyen D-H, Florentina S. Hawaii Behavioral Risk Factor Surveillance System 2014 Results. Published online 2015. Accessed April 7, 2021. https://health.hawaii.gov/brfss/files/2015/08/HBRFSS_2014_results.pdf.
- 11.Hawaii Health Data Warehouse, author. Hawaii Health Data Warehouse Race-Ethnicity Documentation. Published online August 2011. Accessed April 7, 2021. http://www.hhdw.org/wp-content/uploads/HHDW-Race-Ethnicity-Documentation-Report.pdf.
- 12.World Health Organization, author. WHO Statement Regarding Cluster of Pneumonia Cases in Wuhan, China. Published January 2, 2020. Accessed January 1, 2021. https://www.who.int/china/news/detail/09-01-2020-who-statement-regarding-cluster-of-pneumonia-cases-in-wuhan-china.
- 13.Harcourt J, Tamin A, Lu X, et al. Severe acute respiratory syndrome Coronavirus 2 from patient with Coronavirus disease, United States. Emerg Infect Dis. 2020;26((6)):1266–1273. doi: 10.3201/eid2606.200516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization, author. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) Published January 30, 2020. Accessed November 27, 2020. https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 15.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91((1)):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Journal of Managed Care Staff, author. A timeline of COVID-19 developments in 2020. AJMC. Published January 1, 2021. Accessed April 8, 2021. https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020.
- 17.US Department of Health & Human Services, author. Determination that a public health emergency exists. Published January 31, 2020. Accessed January 7, 2021. https://www.phe.gov/emergency/news/healthactions/phe/Pages/2019-nCoV.aspx.
- 18.Executive Office of the President, author. Declaring a national emergency concerning the novel Coronavirus Disease (COVID-19) outbreak. Federal Register. Published March 18, 2020. Accessed January 1, 2021. https://www.federalregister.gov/documents/2020/03/18/2020-05794/declaring-a-national-emergency-concerning-the-novel-coronavirus-disease-covid-19-outbreak.
- 19.CDC COVID-19 Response Team, author. Geographic differences in COVID-19 cases, deaths, and incidence - United States, February 12-April 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69((15)):465–471. doi: 10.15585/mmwr.mm6915e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kendi I. The Coronavirus is exposing our racial divides. The Atlantic. https://www.theatlantic.com/ideas/archive/2020/04/coronavirus-exposing-our-racial-divides/609526/. Published April 6, 2020. Accessed January 7, 2021.
- 21.Thebault R, Tran AB, Williams V. The coronavirus is infecting and killing black Americans at an alarmingly high rate. Washington Post. https://www.washingtonpost.com/nation/2020/04/07/coronavirus-is-infecting-killing-black-americans-an-alarmingly-high-rate-post-analysis-shows/. Published April 7, 2020. Accessed January 7, 2021.
- 22.News ABC, author. CDC releases new data as debate grows over racial disparities in coronavirus deaths. ABC News. Accessed April 8, 2021. https://abcnews.go.com/Politics/cdc-releases-data-debate-grows-racial-disparities-coronavirus/story?id=70041803.
- 23.Manahan LM., (DOH) COVID-19 Morbidity and Mortality by Race, Ethnicity and Language in Washington State. Washington State Department of Health; Published online July 2, 2020:9. [Google Scholar]
- 24.Summary of race & ethnicity among confirmed COVID-19 cases in King County, WA. Published online April 10, 2020. Accessed December 15, 2020. https://kingcounty.gov/depts/health/communicablediseases/disease-control/novel-coronavirus/%7E/media/depts/health/communicablediseases/documents/C19/COVID-19-cases-race-ethnicity.ashx.
- 25.Hawaii State Department of Health, author. Hawaii COVID-19 Data. Published April 16, 2020. Accessed April 16, 2020. https://health.hawaii.gov/coronavirusdisease2019/what-you-should-know/current-situation-in-hawaii/
- 26.Hofschneider A. COVID-19 cases among Pacific Islanders surge in Hawaii. Honolulu Civil Beat. Published June 29, 2020. Accessed January 2, 2021. https://www.civilbeat.org/2020/06/covid-19-cases-among-pacific-islanders-surge-in-hawaii/
- 27.UCLA Health, author. COVID-19 exposes how Native Hawaiians and Pacific Islanders face stark health care disparities - UCLA Health - Los Angeles, CA. Published August 25, 2020. Accessed January 1, 2021. https://www.uclahealth.org/covid19-exposes-how-native-hawaiians-and-pacific-islanders-face-stark-health-care-disparities.
- 28.UCLA Center for Health Policy and Research, author. NHPI COVID-19 Datra Policy Lab Dashboard. Tableau Software. Accessed January 1, 2021. https://public.tableau.com/views/NHPI_CDPL_Dashboard_with_extract/NHPICDPLDashboard?:embed=y&:showVizHome=no&:host_url=https%3A%2F%2Fpublic.tableau.com%2F&:embed_code_version=3&:tabs=no&:toolbar=yes&:animate_transition=yes&:display_static_image=no&:display_spinner=no&:display_overlay=yes&:display_count=yes&:language=en&publish=yes&:loadOrderID=0.
- 29.Hawaii COVID-19 Data. Accessed January 4, 2021. https://health.hawaii.gov/coronavirusdisease2019/what-you-should-know/current-situation-in-hawaii/
- 30.Centers for Disease Control and Prevention, author. COVID-19 Racial and Ethnic Health Disparities. Centers for Disease Control and Prevention; Published February 11, 2020. Accessed January 4, 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/index.html. [Google Scholar]
- 31.National Institute on Minority Health and Health Disparities, author. Amplifying the voice of Native Hawaiian and Pacific Islander communities amid the COVID-19 crisis. NIMHD Insights Blog. Published November 30, 2020. Accessed January 8, 2021. https://nimhd.blogs.govdelivery.com/2020/11/30/amplifying-the-voice-of-native-hawaiian-and-pacific-islander-communities-amid-the-covid-19-crisis/
- 32.The Native Hawaiian Health Research Consortium, author. E Ola Mau: The Native Hawaiian Health Needs Study. Published online 2016. Accessed December 15, 2020. http://papaolalokahi.org/images/pdf-files/E-OLA-MAU-Native-Hawaiian-Health-Needs-Study-reprint-2016.pdf.
- 33.Kaholokula JK, Samoa RA, Miyamoto RES, Palafox N, Daniels S-A. COVID-19 special column: COVID-19 hits Native Hawaiian and Pacific Islander communities the hardest. Hawaii J Health Soc Welf. 2020;79((5)):144–146. [PMC free article] [PubMed] [Google Scholar]
- 34.Samoa R, Kaholokula J, Penaia C, et al. COVID-19 and the state of health of Pacific Islanders in the U.S. AAPI Nexus Policy Practice and Community. 2020;17 [Google Scholar]
- 35.Research Economic Analysis Division, author. Hawaii Population Characteristics 2019. Published online June 25, 2020. Accessed April 7, 2020. https://census.hawaii.gov/wp-content/uploads/2020/06/Hawaii-Population-Characteristics-2019.pdf.
- 36.Sorensen CA, Wood B, Prince EW. Race & ethnicity data. Californian Journal of Health Promotion. 2003;1((SI)):91–104. doi: 10.32398/cjhp.v1iSI.561. [DOI] [Google Scholar]
- 37.Grube N. Hawaii lags behind other states in release of COVID-19 data. Honolulu Civil Beat. Published April 15, 2020. Accessed January 2, 2021. https://www.civilbeat.org/2020/04/hawaii-lags-behind-other-states-in-release-of-covid-19-data/
- 38.Panapasa SV, Crabbe KM, Kaholokula JK. Efficacy of federal data: Revised Office of Management and Budget Standard for Native Hawaiian and Other Pacific Islanders examined. AAPI Nexus. 2011;9((1-2)):212–220. doi: 10.17953/appc.9.1-2.cp21x04488016643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization, author. Ten health issues WHO will tackle this year. Accessed January 6, 2021. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 40.Hennon TR, Penque MD, Abdul-Aziz R, et al. COVID-19 associated Multisystem Inflammatory Syndrome in Children (MIS-C) guidelines; a Western New York approach. Prog Pediatr Cardiol. doi: 10.1016/j.ppedcard.2020.101232. Published online May 23, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rando HM, Bennett TD, Byrd JB, et al. Challenges in defining Long COVID: Striking differences across literature, Electronic Health Records, and patient-reported information. medRxiv. Published online March 26, 2021. [DOI]


