Abstract
Background: young adults represent a critical target for mass-vaccination strategies of COVID-19 that aim to achieve herd immunity. Healthcare students, including dental students, are perceived as the upper echelon of health literacy; therefore, their health-related beliefs, attitudes and behaviors influence their peers and communities. The main aim of this study was to synthesize a data-driven model for the predictors of COVID-19 vaccine willingness among dental students. Methods: a secondary analysis of data extracted from a recently conducted multi-center and multi-national cross-sectional study of dental students’ attitudes towards COVID-19 vaccination in 22 countries was carried out utilizing decision tree and regression analyses. Based on previous literature, a proposed conceptual model was developed and tested through a machine learning approach to elicit factors related to dental students’ willingness to get the COVID-19 vaccine. Results: machine learning analysis suggested five important predictors of COVID-19 vaccination willingness among dental students globally, i.e., the economic level of the country where the student lives and studies, the individual’s trust of the pharmaceutical industry, the individual’s misconception of natural immunity, the individual’s belief of vaccines risk-benefit-ratio, and the individual’s attitudes toward novel vaccines. Conclusions: according to the socio-ecological theory, the country’s economic level was the only contextual predictor, while the rest were individual predictors. Future research is recommended to be designed in a longitudinal fashion to facilitate evaluating the proposed model. The interventions of controlling vaccine hesitancy among the youth population may benefit from improving their views of the risk-benefit ratio of COVID-19 vaccines. Moreover, healthcare students, including dental students, will likely benefit from increasing their awareness of immunization and infectious diseases through curricular amendments.
Keywords: COVID-19 vaccines, decision making, decision trees, dental education, international association of dental students, machine learning, mass vaccination, regression analysis
1. Introduction
The race towards achieving substantial levels of population immunity, commonly known as herd immunity, against the coronavirus disease (COVID-19) embraces a myriad of milestones that should be unlocked by the world’s governments by fall 2021 [1]. The immunization of young adults is one of these challenging milestones due to numerous reasons. First, the low risk of COVID-19 morbidity and mortality among the youth population can trigger reluctance and/or resistance to getting vaccinated against the severe acute respiratory syndrome coronavirus—2 (SARS-CoV-2) [2,3,4,5,6]. In a recent scoping review, Aw et al. 2021 found that the low self-perceived risk of contracting COVID-19 was an individual/group factor of COVID-19 vaccine hesitancy in high-income countries [7].
The COVID-19 mass vaccination strategies followed a priority approach that was suggested by the World Health Organization (WHO) and endorsed by all its member states; therefore, the older adults, healthcare personnel, essential workers, etc., were prioritized to receive COVID-19 vaccines at the expenses of the young adults who had to wait around six months until they were permitted to register for vaccination [8,9]. Mass media and social media play a key role in shaping youth views and attitudes towards health-related issues, including receiving vaccines [10,11,12,13,14,15]. The negative impacts of social media on vaccine acceptance levels were found in the Czech Republic, Palestine, the United Kingdom (UK), and the United States of America (US) [13,15,16,17].
University students are an interesting group for both public health research and interventions because they constitute a special subset of the general youth population that is supposed to retain the highest possible levels of health literacy [15,18,19,20]. Likewise, studying health-related subjects was found to be a pivotal promoter of health literacy; therefore, healthcare students represent the upper echelon of health literacy among the youth population [20]. The social role of healthcare students in health promotion is underscored by the hypothesis that those students are broadly perceived as opinion leaders within their local communities and social circles; therefore, the policies aiming to improve their health-related attitudes and behaviors can yield an indirect and long-term benefit for the public health literacy [21,22,23,24].
Dental students had been recruited in this study as representatives of healthcare students, even though they are challenged by additional strains during this pandemic that could have affected their willingness to accept the COVID-19 vaccine either positively or negatively [25,26,27,28,29]. The discontinuation of clinical training, the abrupt shift to online education, and the increased risk of contracting COVID-19 infection through aerosol-generating procedures were found to be affecting the dental students’ attitudes and behaviors amid the pandemic, which may promote their willingness to get vaccinated in order to overcome the pandemic restrictions [25,26,27,28,29]. Moreover, COVID-19 as a syndromic disease imposes further challenges to the dental practice through its puzzling oral manifestations, e.g., loss of taste (dysgeusia), oral ulcers, oral candidiasis, etc., that can complicate the timely and proper diagnosis of oral lesions [30,31,32,33,34,35,36,37]. Contrarily, dental students’ knowledge about the COVID-19 pandemic was barely adequate in some countries, especially the low-income ones, which might endanger their willingness to get vaccinated [38].
Prior to the COVID-19 pandemic, dental students were used to being vaccinated against various infections, including hepatitis B, tetanus, and influenza as part of their clinical training prerequisites [39]. In addition to high-income countries, the middle-income ones adopted intense policies during the last few years that yielded a significant increase in the percentage of immunized dentists [40,41]. Nonetheless, the attitudes of dental students toward novel vaccines, e.g., human papillomavirus (HPV) vaccine, were found to be unsatisfactory in the high and middle-income countries due to a lack of knowledge [42,43,44]. Recently, a growing number of studies had been designed to describe the attitudes of healthcare students towards the novel COVID-19 vaccines [11,13,15,45,46,47,48]. One of the major critiques of these studies is the lack of in-depth analysis of the promoters and barriers of vaccine willingness; therefore, it had been recommended to carry out a deep analysis utilizing machine learning-based approaches for evaluation of the predictors of COVID-19 vaccine-related attitudes [11].
Machine learning-based approaches had been widely utilized in understanding the epidemiology, clinical presentation, and outcomes of COVID-19, as well as its vaccine acceptance sentiments and vaccine side effects [49,50,51,52,53,54]. Artificial intelligence (AI) models could be as accurate as medical specialists in the diagnosis and prognosis of COVID-19; however, their current diagnostic accuracy needs to be improved through further integration of big datasets of radiographic and clinical information [49]. Discourse analyses of social media platforms, e.g., Twitter, Facebook, and YouTube, also utilized AI models to better understand COVID-19 vaccine misinformation and hesitancy [53,54,55]. Hussain et al. 2021 used AI to analyze Facebook and Twitter content in the UK and the US during March–November 2020, and their findings were highly correlated with the results of the concurrent national surveys in both countries [53]. Therefore, AI-enabled social media analysis was recommended for large-scale adoption by institutions and governments alongside survey-based techniques for real-time assessment of public sentiments of vaccination willingness [53].
The overall aim of this study was to synthesize a data-driven model for the predictors of COVID-19 vaccine willingness among dental students worldwide. The primary objective was to identify the important predictors of vaccination willingness from the pool of demographic and psychological independent variables, and the secondary objective was to articulate these predictors in a conceptual model following the socio-ecological theory.
2. Materials and Methods
2.1. Study Design
This analytical study is based on the data curated by an international cross-sectional survey carried out by the Standing Committee on Research and Education (SCORE) of the International Association of Dental Students (IADS) in February 2021 [56,57]. The survey aimed to evaluate the attitudes of dental students in twenty-two countries towards COVID-19 vaccination and to explore the potential drivers of their vaccine hesitancy stand [11]. A non-random sampling technique through snowballing recruitment (where the participants recruited other participants to fill in the questionnaire) was employed to collect data from the target population, and the digital form that curated data was coded and extended to the participating subjects using KoBoToolbox (Harvard Humanitarian Initiative, Cambridge, MA, USA, 2021) [58]. The national delegates of the IADS acted as liaison officers for data collection in their respective countries, and they used the communication platforms of their national students’ associations to promote the survey, e.g., mail lists, social media pages, and instant messaging groups [57].
The self-administered questionnaire (SAQ) used in this survey consisted of 20 multiple-choice items inquiring about a) demographic information (gender, age, academic level, and country), b) COVID-19-related experience (prior infection, caring for COVID-19 patients, or having a COVID-19 case or fatality within the social circle), c) willingness to receive COVID-19 vaccine (measured by a 5-point Likert scale), and d) the drivers of COVID-19 vaccine-related attitudes [11]. The SAQ was developed and validated through a panel of public health and medical education experts, then its test re-test reliability was established through a group of volunteer students that indicated that the English version of the used SAQ retained a perfect level of reliability. The whole validation process and psychometric properties of the SAQ had been described earlier somewhere [11].
The drivers of vaccine hesitancy evaluated in this study were adapted from the compendium of the Strategic Advisory Group of Experts on Immunization (SAGE) of the World Health Organization (WHO) [59]. Ten drivers were included, of which five were contextual (“influences arising due to historic, socio-cultural, environmental, health system/institutional, economic or political factors”), two were individual/group (“influences arising from personal perception of the vaccine or influences of the social/peer environment”), and three were vaccine-specific (“directly related to vaccine or vaccination”) drivers [60]. The impact of media and social media, celebrities and opinion leaders, trust in government, trust in the pharmaceutical industry, and cultural and religious values were deemed to be the contextual drivers in the SAQ, while the misconception of natural immunity and perceived knowledge were employed as the individual/group drivers. The vaccine-specific drivers were the risk/benefit ratio of COVID-19 vaccination, the attitudes towards new vaccines, and the local availability of the COVID-19 vaccine. (Table 1)
Table 1.
The drivers of dental students’ COVID-19 vaccine hesitancy, February 2021 (n = 6639).
| Item | Outcome |
|---|---|
| Contextual Drivers | |
| Do reports you hear/read in the media/on social media make you reconsider the choice to take the COVID-19 vaccine? | No |
| Not Sure | |
| Yes | |
| Do celebrities, religious or political leaders influence your decision about being vaccinated? | No |
| Not Sure | |
| Yes | |
| Do you trust that your government is making decisions in your best interest with respect to what vaccines are provided (e.g., your government purchases the highest quality vaccines available)? | No |
| Not Sure | |
| Yes | |
| Do you trust pharmaceutical companies to provide credible data on COVID-19 vaccine safety and the effectiveness of the vaccines? | No |
| Not Sure | |
| Yes | |
| Do you know anyone who will not take the vaccine because of religious or cultural values? | No |
| Not Sure | |
| Yes | |
| If “Yes”, do you agree with these people? | No |
| Not Sure | |
| Yes | |
| Individual/Group Drivers | |
| Do you think that there are better ways to prevent COVID-19 than using vaccines (e.g., developing immunity by becoming sick and recovering)? | No |
| Not Sure | |
| Yes | |
| Do you feel you have enough information about COVID-19 vaccines and their safety? | No |
| Not Sure | |
| Yes | |
| Vaccine-Specific Drivers | |
| Do you think that the benefits of COVID-19 vaccines outweigh their reported side effects/adverse reactions? | No |
| Not Sure | |
| Yes | |
| In general, when a new vaccine is introduced, are you inclined to consent to your vaccination? | No |
| Not Sure | |
| Yes | |
| Do you feel confident that the health center or doctor’s office will have the COVID-19 vaccines you need, when you need them? | No |
| Not Sure | |
| Yes |
2.2. Study Variables
The downstream analyses utilized a higher version of the dataset that converted all the study variables into numerical variables. The target variable was the willingness to receive the COVID-19 vaccine, and its possible outcomes ranged between “Totally Disagree” denoted by 1 and “Totally Agree” denoted by 5. Vaccine acceptance was defined as the willingness to receive the COVID-19 vaccine once it becomes accessible, and it was denoted by the 4th and 5th levels of the Likert scale. Vaccine hesitancy was defined as the “delay in acceptance or refusal of vaccines despite availability of vaccinations services”, and it was denoted by the 3rd level of the Likert scale. Vaccine resistance was defined as the rejection of receiving vaccines despite of their local accessibility, and it was denoted by the 1st and 2nd levels of the Likert scale [61].
The predictor (candidate) variables included both demographic variables, COVID-19-related experience variables, and vaccine hesitancy drivers’ variables. The economic level variable was graded from low-income economies, denoted by 1, to high-income economies, denoted by 4. Each of the vaccine hesitancy drivers had three possible outcomes, “Yes” denoted by 2, “Not Sure” denoted by 1, and “No” denoted by 0 (Table 2).
Table 2.
The enhanced dataset of dental students’ COVID-19 vaccine-related attitudes, February 2021 (n = 6639).
| Variable | Outcome | Cd | Variable | Outcome | Cd | Variable | Outcome | Cd |
|---|---|---|---|---|---|---|---|---|
| Gender | Female | 1 | Knowing Fatality |
No | 0 | Pharmaceuticals | Yes | 2 |
| Male | 2 | Yes | 1 | Cultural Values | No | 0 | ||
| Academic Level | 1st Year | 1 | Flu Vaccine | Never | 0 | Not Sure | 1 | |
| 2nd Year | 2 | Sometimes | 1 | Yes | 2 | |||
| 3rd Year | 3 | Always | 2 |
Agreement
with Values |
No | 0 | ||
| 4th Year | 4 | Mandatory | 3 | Not Sure | 1 | |||
| 5th Year | 5 | Willingness of Vaccination |
Totally Disagree | 1 | Yes | 2 | ||
| 6th Year | 6 | Disagree | 2 | Natural Immunity |
No | 0 | ||
| Internship | 7 | Not Sure | 3 | Not Sure | 1 | |||
| Fresh Graduate | 8 | Agree | 4 | Yes | 2 | |||
| Clinical Training |
Pre-clinical | 1 | Totally Agree | 5 | Perceived Knowledge |
No | 0 | |
| Clinical | 2 | Media/Social Media |
No | 0 | Not Sure | 1 | ||
| Economic Level |
Low income | 1 | Not Sure | 1 | Yes | 2 | ||
| Lower-middle income | 2 | Yes | 2 | Risk/Benefit Ratio |
No | 0 | ||
| Upper-middle income | 3 | Public Figures | No | 0 | Not Sure | 1 | ||
| High income | 4 | Not Sure | 1 | Yes | 2 | |||
| Prior Infection |
No | 0 | Yes | 2 | Novel Vaccines |
No | 0 | |
| Yes | 1 | Government | No | 0 | Not Sure | 1 | ||
| Providing Care |
No | 0 | Not Sure | 1 | Yes | 2 | ||
| Yes | 1 | Yes | 2 | Local Availability |
No | 0 | ||
| Knowing Patient |
No | 0 | Pharmaceuticals | No | 0 | Not Sure | 1 | |
| Yes | 1 | Not Sure | 1 | Yes | 2 |
Cd = numerical code.
2.3. Ethical Considerations
The study protocol was reviewed and approved by the Ethics Committee of the Faculty of Medicine, Masaryk University on 20 January 2021 under the Ref No. 4/2021. The cross-sectional survey was conducted in accordance with the Declaration of Helsinki for research involving human subjects, and it had been previously reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cross-sectional studies [11,62,63].
The study data was stored and processed in full compliance with the EU General Data Protection Regulation (GDPR); therefore, no identifying personal data was collected from the participants that might enable their retrospective identification [64]. Prior to participation in the survey, each participant had to give their informed consent digitally, and no information was saved if the participant quit the study at any stage before submitting their answers.
2.4. Data Mining
2.4.1. Data Analysis
Initially, a regression decision tree analysis was carried out as the data mining approach to confirm the variables associated with vaccination willingness. Regression tree is a non-parametric technique that can find out the potential significant predictors for the target outcomes. After selection of the strongest candidate variables, we adopted a multi-level regression model based on the socio-ecological theory to predict individuals’ vaccination willingness by the candidate variables.
2.4.2. Decision Tree Analysis
The R package of “rpart” was utilized to construct the regression decision tree by a machine learning manner. By using “sample function” in R, we divided the sample randomly into the training dataset, 70% of the whole sample and the testing dataset, 30% of the whole sample. For training the decision tree splits, we set the stopping rule of the minimum observed cases of a node at 30. Each split is sought to decrease the overall lack of fitness by a factor of 0.01 (cost complexity factor) before being attempted.
We examined the cross-validated errors, selected the complexity parameters associated with the minimum errors, and pruned them in order to avoid over fitting. Eventually, with the aim to estimate the validity of this trained decision tree, we computed the R2 of the linear regression relationship between observed values in the test dataset and predicted values by the trained decision tree.
2.4.3. Multi-Level Regression
In our dataset, except for the economic level that was a contextual variable, all the other demographic variables belonged to the individual level, e.g., gender, academic level, clinical training, etc. The vaccine hesitancy drivers suggested by the SAGE also belonged to the individual level, e.g., trust in the government, trust in the pharmaceutical industry, and misconception of natural immunity, etc.
According to the socio-ecological theory, intrapersonal factors are nested at the contextual level [65]. Thus, if the decision tree decided that economic level was a significant predictor, the multi-level regression model would place the variable in level 2, and other candidate variables in level 1. This linear multi-level model was slope-fixed, as the relationships between the contextual factor and individual factors were fixed. We performed this step using the R-based open software Jamovi [66].
3. Results
3.1. Descriptive Statistics
A total of 6639 respondents were included in the downstream analyses, of which 70.5% were females and 63.5% were 17–22 years old. The most represented academic year was the third year (21.4%), followed by the fourth year (19%), and the second year (18.5%). According to the latest ranking of the World Bank, 74.4% of the participants were from upper-middle- and high-income countries [67].
Regarding their COVID-19-related experience, 16.6% had been previously infected by SARS-CoV-2, and 27.2% provided care to COVID-19 patients. While 87.4% of the participants knew someone who was infected by SARS-CoV-2, 45.7% of them knew someone who died due to SARS-CoV-2.
On answering the question of willingness to receive a vaccine against COVID-19, only 63.5% were vaccine accepting, 22.5% were vaccine hesitant, and 13.9% were vaccine resistant. About one-third (33.4%) of the participants acknowledged that their decision regarding vaccination was influenced by the reports they heard/read in the media/on social media, and 16.2% acknowledged that their vaccination decision was influenced by celebrities or religious or political leaders.
Interestingly, only 35.1% indicated their trust in their governments’ capacity to make appropriate decisions regarding the best vaccines to be provided, and 47.4% indicated their trust in the pharmaceutical industry to provide credible data on COVID-19 vaccines’ safety and effectiveness.
Over one quarter (26.4%) had the misconception of the superior effectiveness of natural immunity over vaccination against SARS-CoV-2, and only 31.5% felt that they had sufficient knowledge about COVID-19 vaccines and their safety. Almost one half (50.7%) of the participants thought that the benefits of COVID-19 vaccines outweighed their reported side effects and adverse reactions, and 43.2% exhibited positive attitude towards receiving novel vaccines generally. Regarding the local availability, 40.7% of the participants felt confident that their local health centers would have the COVID-19 vaccines whenever they need them (Table 3).
Table 3.
Demographic characteristics, COVID-19-related experience, and COVID-19 vaccine willingness and its drivers among a global sample of dental students, February 2021 (n = 6639).
| Variable | Outcome | Frequency (n) | Percentage (%) | Cumulative Percentage (%) |
|---|---|---|---|---|
| Demographic Characterstics | ||||
| Gender | Female | 4682 | 70.5% | 70.5% |
| Male | 1836 | 27.7% | 98.2% | |
| Non-binary | 53 | 0.8% | 99% | |
| Prefer not to say | 68 | 1% | 100% | |
| Academic Level | First Year | 979 | 14.7% | 14.7% |
| Second Year | 1227 | 18.5% | 33.2% | |
| Third Year | 1422 | 21.4% | 54.6% | |
| Fourth Year | 1259 | 19% | 73.6% | |
| Fifth Year | 817 | 12.3% | 85.9% | |
| Sixth Year | 240 | 3.6% | 89.5% | |
| Internship/Fresh Graduate | 695 | 10.5% | 100% | |
| Clinical Training | Pre-clinical Stage | 2206 | 33.2% | 33.2% |
| Clinical Stage | 4433 | 66.8% | 100% | |
| Economic Level | Low-income Country | 467 | 7% | 7% |
| Lowe-middle-income Country | 1232 | 18.6% | 25.6% | |
| Upper-middle-income Country | 3035 | 45.7% | 71.3% | |
| High-income Country | 1905 | 28.7% | 100% | |
| COVID-19-Related Experience | ||||
| Prior Infection | Yes | 1105 | 16.6% | 16.6% |
| No | 5534 | 83.4% | 100% | |
| Providing Care | Yes | 1808 | 27.2% | 27.2% |
| No | 4831 | 72.8% | 100% | |
| Knowing Patient | Yes | 5801 | 87.4% | 87.4% |
| No | 838 | 12.6% | 100% | |
| Knowing Dead | Yes | 3031 | 45.7% | 45.7% |
| No | 3608 | 54.3% | 100% | |
| Attitudes Towards COVID-19 Vaccine | ||||
| I am willing to take the COVID-19 vaccine once it becomes available to me. | Totally Disagree | 491 | 7.4% | 7.4% |
| Disagree | 434 | 6.5% | 13.9% | |
| Not Sure | 1494 | 22.5% | 36.4% | |
| Agree | 1495 | 22.5% | 59% | |
| Totally Agree | 2725 | 41% | 100% | |
| Contextual Drivers | ||||
| Do reports you hear/read in the media/on social media make you re-consider the choice to take the COVID-19 vaccine? | No | 2903 | 43.7% | 43.7% |
| Not Sure | 1519 | 22.9% | 66.6% | |
| Yes | 2217 | 33.4% | 100% | |
| Do celebrities, religious or political leaders influence your decision about being vaccinated? | No | 4734 | 71.3% | 71.3% |
| Not Sure | 827 | 12.5% | 83.8% | |
| Yes | 1078 | 16.2% | 100% | |
| Do you trust that your government is making decisions in your best interest with respect to what vaccines are provided? | No | 2178 | 32.8% | 32.8% |
| Not Sure | 2130 | 32.1% | 64.9% | |
| Yes | 2331 | 35.1% | 100% | |
| Do you trust pharmaceutical companies to provide credible data on COVID-19 vaccine safety and the effectiveness of the vaccines? | No | 1448 | 21.8% | 21.8% |
| Not Sure | 2041 | 30.7% | 52.6% | |
| Yes | 3150 | 47.4% | 100% | |
| Do you know anyone who will not take the vaccine because of religious or cultural values? | No | 4286 | 64.6% | 64.6% |
| Not Sure | 830 | 12.5% | 77.1% | |
| Yes | 1523 | 22.9% | 100% | |
| If “Yes”, do you agree with these people? | No | 6260 | 94.3% | 94.3% |
| Not Sure | 192 | 2.9% | 97.2% | |
| Yes | 187 | 2.8% | 100% | |
| Individual/Group Drivers | ||||
| Do you think that there are better ways to prevent COVID-19 than using vaccines? | No | 2928 | 44.1% | 44.1% |
| Not Sure | 1955 | 29.4% | 73.6% | |
| Yes | 1756 | 26.4% | 100% | |
| Do you feel you have enough information about COVID-19 vaccines and their safety? | No | 2710 | 40.8% | 40.8% |
| Not Sure | 1838 | 27.7% | 68.5% | |
| Yes | 2091 | 31.5% | 100% | |
| Vaccine-Specific Drivers | ||||
| Do you think that the benefits of COVID-19 vaccines outweigh their reported side effects/adverse reactions? | No | 1188 | 17.9% | 17.9% |
| Not Sure | 2082 | 31.4% | 49.3% | |
| Yes | 3369 | 50.7% | 100% | |
| In general, when a new vaccine is introduced, are you inclined to consent to your vaccination? | No | 1606 | 24.2% | 24.2% |
| Not Sure | 2162 | 32.6% | 56.8% | |
| Yes | 2871 | 43.2% | 100% | |
| Do you feel confident that the health center or doctor’s office will have the COVID-19 vaccines you need, when you need them? | No | 1778 | 26.8% | 26.8% |
| Not Sure | 2158 | 32.5% | 59.3% | |
| Yes | 2703 | 40.7% | 100% | |
3.2. Decision Tree Analysis
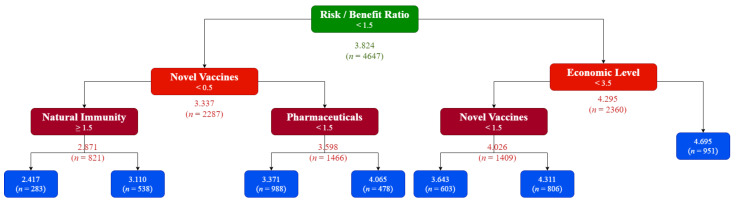
On comparing the predicted values and observed values for the vaccination willingness in the test dataset based on a linear regression model, the R2 was 0.27, which means that the model can explain 27% of the variance of the dependent variable. The generated model suggested that there were five important predictors towards individuals’ vaccination willingness, those are (1) economic level of the country, (2) individual’s level of trust in the pharmaceutical industry, (3) individual’s misconception of natural immunity, (4) individual’s attitudes toward novel vaccines in general, and (5) individual’s views for the risk-benefit-ratio of vaccines against COVID-19 (Figure 1).
Figure 1.
Decision tree for prediction of dental students’ willingness to receive COVID-19 vaccines, February 2021 (n = 6639). The values inside the colored blocks represent the cutoffs of the answers for each predictor when “No” = 0, “Not Sure” = 1, and “Yes” = 2. The values below the colored blocks represent the cutoff response to the COVID-19 vaccination willingness question when “Totally Disagree” = 1, “Disagree” = 2, “Not Sure” = 3, “Agree” = 4, and “Totally Agree” = 5.
To interpret the generated model, the students should be primarily classified according to their views for the risk-benefit-ratio of COVID-19 vaccines. If they agreed that the benefits of the vaccines outweighed their reported side effects and adverse reactions, then only those from high-income countries would be very likely to accept the vaccine, but if they were from upper-middle-, lower-middle-, or low-income countries, their vaccination decision would be highly dependent on their attitudes toward novel vaccines.
If the students were not sure or disagreed that benefits of the vaccines outweighed their reported side effects and adverse reactions, then their attitudes toward novel vaccines would be a determinant factor. Those students who did not reject novel vaccines were to be classified according to their level of trust of the pharmaceutical industry in order to predict their willingness towards receiving COVID-19 vaccines, while those students who rejected novel vaccines were to be classified according to their misconception of natural immunity in order to predict their willingness towards receiving COVID-19 vaccines.
3.3. Bivariate Correlation
On running bivariate correlation analysis using Pearson’s correlation coefficient (ρ), the vaccination willingness was found to be significantly (Sig. < 0.001) associated with the five important predictors (country’s economic level, individual’s trust of pharmaceuticals, misconception of natural immunity, belief of risk-benefit-ratio, and attitudes towards novel vaccines).
The misconception of natural immunity was inversely correlated with all other predictors, as well as the vaccination willingness. It was poorly correlated with the economic level (ρ = −0.222; Sig. < 0.001), the trust of pharmaceutical industry (ρ = −0.113; Sig. < 0.001), the belief of risk-benefit-ratio (ρ = −0.125; Sig. < 0.001), the attitudes toward novel vaccines generally (ρ = −0.085; Sig. < 0.001), and the vaccination willingness (ρ = −0.267; Sig. < 0.001).
On the other hand, the economic level was directly correlated with all other predictors except for the misconception of natural immunity. The economic level was poorly correlated with the trust of the pharmaceutical industry (ρ = 0.209; Sig. < 0.001), the belief of the risk-benefit-ratio (ρ = 0.199; Sig. < 0.001), the attitudes toward novel vaccines generally (ρ = 0.167; Sig. < 0.001), and the vaccination willingness (ρ = 0.236; Sig. < 0.001).
While the trust of the pharmaceutical industry was poorly correlated with the economic level (ρ = 0.209; Sig. < 0.001), it was fairly correlated with the belief of the risk-benefit-ratio (ρ = 0.389; Sig. < 0.001), the attitudes toward novel vaccines generally (ρ = 0.396; Sig. < 0.001), and the vaccination willingness (ρ = 0.401; Sig. < 0.001). Similarly, the belief of the risk-benefit-ratio was poorly correlated with the economic level (ρ = 0.199; Sig. < 0.001), even though it was fairly correlated with the trust of pharmaceutical industry (ρ = 0.389; Sig. < 0.001), the attitudes towards novel vaccines generally (ρ = 0.385; Sig. < 0.001), and vaccination willingness (ρ = 0.390; Sig. < 0.001).
The attitudes toward novel vaccines were poorly correlated with the economic level (ρ = 0.167; Sig. < 0.001), and they were fairly correlated with the trust of the pharmaceutical industry (ρ = 0.396; Sig. < 0.001), the belief of the risk-benefit-ratio (ρ = 0.385; Sig. < 0.001), and the vaccination willingness (ρ = 0.424; Sig. < 0.001) (Table 4).
Table 4.
Bivariate correlation among COVID-19 vaccine willingness and its suggested predictors, February 2021 (n = 6639).
| Economic Level |
Pharmaceutical Industry |
Natural Immunity |
Risk/Benefit Ratio |
Novel Vaccines |
Vaccination Willingness |
||
|---|---|---|---|---|---|---|---|
| Economic Level | ρ | 1.000 | |||||
| Sig. | N/A | ||||||
| Pharmaceutical Industry | ρ | 0.209 | 1.000 | ||||
| Sig. | <0.001 | N/A | |||||
| Natural Immunity | ρ | −0.222 | −0.113 | 1.000 | |||
| Sig. | <0.001 | <0.001 | N/A | ||||
| Risk/Benefit Ratio | ρ | 0.199 | 0.389 | −0.125 | 1.000 | ||
| Sig. | <0.001 | <0.001 | <0.001 | N/A | |||
| Novel Vaccines | ρ | 0.167 | 0.396 | −0.085 | 0.385 | 1.000 | |
| Sig. | <0.001 | <0.001 | <0.001 | <0.001 | N/A | ||
| Vaccination Willingness | ρ | 0.236 | 0.401 | −0.267 | 0.390 | 0.424 | 1.000 |
| Sig. | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | N/A |
Pearson bivariate correlation analysis was carried out with a significance level (Sig.) < 0.05, and the Pearson’s coefficient was rho (ρ).
3.4. Multi-Level Regression
On running multi-level regression analysis of the predictors, at level II where the slope was fixed, the variance of random intercepts of the economic level was 0.020, and the variance of the residuals was 1.039 Table 5.
Table 5.
Random components of the predictors of willingness to receive COVID-19 vaccines, February 2021 (n = 6639).
| Groups | Name | SD | Variance | ICC |
|---|---|---|---|---|
| Economic Level | (Intercept) | 0.142 | 0.0202 | 0.0191 |
| Residual | 1.019 | 1.0388 |
Multi-level linear regression analysis was carried out. ICC refers to the interclass correlation coefficient, which is used to describe the portion of explained variance by random effects.
At level I where the intercept was fixed, the trust of the pharmaceutical industry had a positive effect on vaccination willingness (β = 0.304; Sig. < 0.001). Likewise, the belief of the risk-benefit-ratio (β = 0.285; Sig. < 0.001) and the attitudes toward novel vaccines (β = 0.382; Sig. < 0.001) predicted the vaccination willingness positively and significantly. In contrast to the mentioned three variables at level I, the misconception of natural immunity in the same level showed a negative influence on vaccination willingness (β = −0.270; Sig. < 0.001) (Table 6).
Table 6.
Fixed effects parameters estimates of the predictors of willingness to receive COVID-19 vaccines, February 2021 (n = 6639).
| 95% Confidence Intervale | |||||||
|---|---|---|---|---|---|---|---|
| Predictor | Estimate | SE | Lower | Upper | df | t | Sig. |
| (Intercept) | 3.809 | 0.073 | 3.666 | 3.951 | 2.96 | 52.3 | <0.001 |
| Pharmaceutical Industry | 0.304 | 0.018 | 0.269 | 0.340 | 6633.72 | 16.8 | <0.001 |
| Natural Immunity | −0.270 | 0.016 | −0.301 | −0.239 | 6604.25 | −17.1 | <0.001 |
| Risk/Benefit Ratio | 0.285 | 0.019 | 0.248 | 0.322 | 6633.77 | 15.2 | <0.001 |
| Novel Vaccines | 0.382 | 0.018 | 0.347 | 0.417 | 6633.99 | 21.5 | <0.001 |
Multi-level linear regression analysis was carried out with a significance level (Sig.) < 0.05.
3.5. Socio-Ecological Model
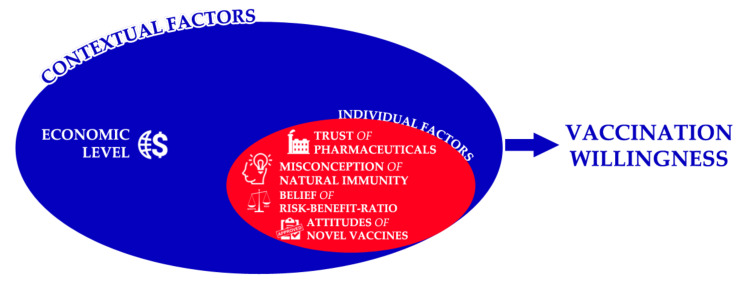
In accordance with the socio-ecological theory, the economic level of the country was controlled in level II as a contextual factor [68]. The correlation analysis results indicated that the higher the economic level where the students lived and studied predicted a higher propensity of vaccination willingness. The multi-level regression analysis suggested that in level I, the trust of the pharmaceutical industry, the belief that COVID-19 vaccine benefits outweighed their reported side effects and adverse reactions, and positive attitudes towards novel vaccines predicted vaccination willingness positively and significantly. The misconception of natural immunity decreased the vaccination willingness, and the regression model explained 30% of the variance (See Figure 2).
Figure 2.
Conceptual map of vaccination willingness predictors according to the socio-ecological theory, February 2021 (n = 6639).
4. Discussion
In our study, a conceptual model was tailored based on the data of 6639 dental students worldwide who participated in a cross-sectional survey exploring their demographic characteristics, COVID-19-related experience, and vaccination willingness and its drivers. The model had been utilizing a machine learning-based approach to test and verify its components that indicated that there were five important predictors of COVID-19 vaccination willingness among dental students globally, i.e., the economic level, the trust of the pharmaceutical industry, the misconception of natural immunity, the belief of vaccines risk-benefit-ratio, and the attitudes toward novel vaccines. The socio-ecological theory had been employed to place the five predictors at two levels, i.e., the individual factors at level I and the contextual factors at level II.
The sole contextual factor suggested by our model was the economic level of the country where the students lived and studied. In agreement with this finding, Carrieri et al. 2021 synthesized a machine-learning model for vaccine hesitancy among Italian municipalities’ inhabitants, which indicated that socioeconomic indicators, e.g., the proportion of waste recycling and the employment rate, were the most powerful predictors of vaccine hesitancy at an area-level [69]. The household income was found to be a significant determinant for COVID-19 vaccine hesitancy among South African, Italian, and Portuguese adult populations during the pre-vaccination stage and the early stages of mass vaccination [70,71,72]. In a recent cross-sectional study, the lack of financial resources needed for health insurance was a trigger for COVID-19 vaccine hesitancy among US adults, thus emphasizing the role of a functional universal health coverage system in each country in the world, regardless of its economic level, to enhance the public’s vaccination willingness [73]. Similarly, Bertoncello et al. 2020 found that perceived financial hardship was a significant driver of parental vaccine hesitancy in Italy [74].
Trust of the pharmaceutical industry was one of the four individual predictors of COVID-19 vaccine willingness in our model. The recent cross-sectional studies of vaccine hesitancy found that mistrust of the pharmaceutical industry was very common among individuals with anti-vaccination positions in Austria, France, Italy, Malaysia, and the US [75,76,77,78,79]. Karafillakis et al. 2016 conducted a qualitative study for European healthcare workers, which indicated that in spite of their trust of their health systems, the mistrust of the pharmaceutical industry was profound among the participants, and it was suggested to be one of the promoters of vaccine hesitancy [80]. The European healthcare workers believed that pharmaceutical companies had financial interest that may retain them from disclosing safety and efficacy data of their products openly and place additional pressures on healthcare workers [80].
In their recent scoping review, Biswas et al. 2021 found that insufficient knowledge about the vaccines was a predictor for COVID-19 vaccine hesitancy among healthcare workers globally [81]. The misconception of natural immunity, which reflects the lack of factual knowledge about immunization, was the second individual predictor of vaccination willingness in our model. This misconception had been profoundly reported among the anti-vaccination parents, and it was dependent on their belief that illness is natural in childhood and the vaccine-preventable diseases are not life-threatening [82]. Therefore, this misconception can also be attributed to the low perceived risk of COVID-19 infection among young adults [3,4,5,6,7]. The general knowledge about vaccines had been consistently reported as a predictor of COVID-19 vaccination willingness, especially in low-income countries, e.g., Bangladesh, Cameroon, Ghana, Nigeria, and Palestine [83,84,85,86,87].
A nationwide survey of the French population indicated that the perceived risk–benefit balance (RBB) was a strong predictor for vaccination willingness among the surveyed parents [88]. The regression analysis confirmed that the perceived vaccine RBB was consistently unfavorable among the individuals with vaccine-hesitant and vaccine-resistant positions [88]. Another recent report had been jointly published by the WHO and the United Nations Children’s Fund (UNICEF) in 2017, and it revealed that the RBB was the most cited reason for vaccine hesitancy globally in the last few years [89]. In consistence with these results, our model depicted the RBB as the third individual predictor of COVID-19 vaccination willingness. The perceived vaccine RBB can be an emotional and intuitive process, rather than being based on logic and rationality, as the perceived risk of vaccination was commonly attributed to exaggerated feelings, e.g., the fear of potential adverse reactions, even the mildest ones [90]. Therefore, the independent (non-sponsored) research of post-vaccination side effects is believed to be a valid asset for delivering robust and non-biased evidence to hesitant individuals that can help them understand the nature of post-vaccination side effects [91,92,93,94,95,96,97,98,99]. The mild side effects, however non-life-threatening, can interfere with the daily routine of the vaccinated individuals and may require one or few days of absenteeism from work or school; therefore, they can be perceived as a vaccination barrier if the yielded benefit was not convincing [90].
The fourth individual predictor of vaccination willingness in our model was the general attitudes toward novel vaccines. The HPV vaccine is relatively novel, and the attitudes of dental students towards it were found to be unsatisfactory in the high- and middle-income countries due to the lack of knowledge [42,43,44]. The novel vaccines are usually associated with a unique set of concerns and fears, including the public apprehension over their safety and effectiveness; therefore, the WHO-SAGE issued guidelines in 2015 for controlling vaccine hesitancy, especially in the regions or the countries where new vaccines are introduced [100].
4.1. Strengths
Compared to the traditional studies, our research was innovatively based on the data mining technique, which is an efficient approach for analyzing big data, as there could be a mass of variables and interactions between each variable. Unlike most previous studies on the foundation of hypothesis-driven tests, the data mining-based method does not establish any initial assumptions. Traditional statistical methods aim to test the hypothesis extracted from previous evidences or theories by the criteria of type I error and type II error. In contrast, the data mining approach does not make any assumptions prior to analysis. The findings of this study are purely driven by data, while there were more than twenty COVID-19 vaccination drivers in our dataset. The machine learning-based methods can select the strongest predictors in one step, thus improving the analysis efficiency and simplifying the multi-level regression in the following step.
In addition, for a more robust explanation of results by data mining, we continued to build a multi-level regression model with the combination of the classical theory of socio-ecological framework, which helps researchers to understand the nested relationship of factors and avoid mixing all variables in one level simply. Moreover, the portion of explained variance by the multi-level regression (30%) had proven the accuracy of our decision tree model, which explained 27% of variance. Hence the more complicated multi-level regression that was based on the strong socio-ecological theory had an improved explanation of only 3%, which is much smaller when compared to the decision tree model (27%).
In a nutshell, our research not only adopted a data mining approach, which is an alternative way for multivariable analyses, especially for the complicated datasets, but also was rooted in a strong theory.
4.2. Limitations
The first limitation is that even though this study adopted a data mining strategy, we did not compare our results with other machine learning methods, e.g., network analysis. However, our decision tree model demonstrated high accuracy and validity with effective selection of significant predictors, even though other machine learning models have their unique advantages. For instance, the network analysis can visualize the strength of the associations of each candidate predictor and target variable. Our aim of using a machine learning-based approach was primarily to select the important predictors for the dependent variable, while we recommend further comparison of other varieties of machine learning-based approaches to interpret the dependent variables deeply based on pure data mining. The second limitation is that we could not perform longitudinal research to know participants’ real decision of COVID-19 vaccination in the future; it was impossible to compare our decision tree results with their final vaccination decision.
The third limitation is related to the non-random sampling technique that had been used to recruit the participants, as snowballing is prone to a number of biases that can affect the representativeness (external validity) of the recruited sample, e.g., self-selection bias. The fourth limitation is attributed to the social desirability bias, as the dental students may have tended to underreport their unfavorable attitudes/opinions of vaccination in order to look ideal and avoid criticism, even if they were assured that their answers will be completely anonymous.
4.3. Implications
This cross-sectional study-based model implies that longitudinal investigation of university students’ attitudes and decisions regarding COVID-19 vaccination is highly warranted to validate our proposed predictors. Based on the findings of our model, the interventions on the control of vaccine hesitancy among the youth population may benefit from improving their views of the risk-benefit ratio of COVID-19 vaccines through focusing on the societal benefits and being transparent about the potential side effects. Increasing the awareness of dental students, particularly, and healthcare students, generally, regarding vaccines will protect them from adopting misconceptions about immunization; such a target can be ideally achieved by amending the undergraduate dental curricula and giving more room for the infectious disease content.
5. Conclusions
In conclusion, the proposed conceptual model, which was based on the data of 6639 dental students worldwide, was developed through a machine learning-based approach to test and verify its components that indicated that there were five important predictors of COVID-19 vaccination willingness among dental students globally, i.e., the economic level of the country where the student lives and studies, the individual’s trust of the pharmaceutical industry, the individual’s misconception of natural immunity, the individual’s belief of vaccines risk-benefit-ratio, and the individual’s attitudes toward novel vaccines. According to the socio-ecological theory, the country’s economic level was the only contextual predictor, while the rest were individual predictors. Healthcare students, including dental students, will probably benefit from increasing their awareness of immunization and infectious diseases through curricular amendments.
Acknowledgments
This work is dedicated to the more than 3 million worldwide fatalities, including the frontline healthcare workers and their families who have fallen victim to COVID-19. The authors thank João Botelho and Vanessa Machado for their contribution to validate the questionnaire of this study.
Appendix A. Members of IADS-SCORE Consortium
Faculty of Dentistry, McGill University, Canada (Jacques Jaar); Schulich School of Medicine & Dentistry, Western University, Canada (Nima Lighvan); Faculty of Dentistry, University of British Columbia, Canada (Karen Lin);
Faculty of Dentistry, SEGi University, Malaysia (Sandy Tan Qing Wen); Faculty of Dentistry, University of Malaya, Malaysia (Tan Hian Wei);
School of Dentistry, Kathmandu University School of Medical Sciences, Nepal (Nitesh Singh);
Department of Oral and Maxillofacial Surgery, School of Dentistry, Zanjan University of Medical Sciences, Iran (Parsa Firoozi); Department of Oral and Maxillofacial Surgery, School of Dentistry, Islamic Azad University Isfahan, Iran (Mohammad Mostafa Aghamohseni; Samin Sirous);
Institute of Dentistry, CMH Lahore Medical College and Institute of Dentistry, Pakistan (Aneeqa Aslam; Maha Sohail); Dental College, Akhtar Saeed Medical and Dental College, Pakistan (Mehroz Ahmad Khan);
Faculty of Dentistry, Beirut Arab University, Lebanon (Julien Issa; Mirna Abou Ibrahim);
Faculty of Dental Medicine, Catholic University of Portugal, Portugal (António Coimbra Amaral);
Faculty of Dental Sciences, Aldent University, Albania (Ersid Domnori);
Faculty of Odontology, Universidad San Francisco De Quito, Ecuador (Jorge Ayala); Faculty of Odontology, Catholic University of Cuenca, Ecuador (Maria Sol Medina);
Faculty of Dentistry, Universitas Indonesia, Indonesia (Viandra Tjokroadiredjo; Farih Aminah)
Department of Dentistry, Al-rafidain University College, Iraq (Noor Sarmad); College of Dentistry, Uruk University, Iraq (Nabaa Abduladheem); Department of Dentistry, Al-rasheed University College, Iraq (Batool Mohammed);
Department of Neuroscience, Reproductive Sciences and Dentistry, University of Naples Federico II, Italy (Matteo Cafasso); Department of Biomedical, Surgical and Dental Sciences, School of Dentistry, University of Milan, Italy (Gregorio Tortora); Department of Medicine and Surgery, School of Dentistry, University of Insubria, Italy (Anita Homayuni);
Faculty of Dentistry, Riga Stradiņš University, Latvia (Kristīne Romanovska);
Faculty of Odontology, Medical Academy, Lithuanian University of Health Sciences, Lithuania (Kriste Trijonytė; Julius Mikonis);
Faculty of Dentistry, University of Khartoum, Sudan (Ahmed Abdalla); Faculty of Dentistry, Al Neelain University, Sudan (Zeinab Hassan); Faculty of Dentistry, University of Medical Sciences and Technology, Sudan (Aya Abdelrahim);
Faculty of Dental Medicine, Monastir University, Tunisia (Haythem Ben Hadj Belgacem; Maya Fedhila);
Faculty of Dentistry, Istanbul University, Turkey (İrem Erdoğdu); Faculty of Dentistry, Beykent University, Turkey (Berk Koparan); Faculty of Dentistry, Yeditepe University, Turkey (Ezgi Y eşiltan); Faculty of Dentistry, Marmara University, Turkey (Serap Beşiroğlu);
Faculty of Dentistry, Ural State Medical University, Russia (Tatiana Spitsyna);
Faculty of Dental Medicine, University of Rijeka, Croatia (Valentina Marasović; Elizabeta Vrkljan; Lovre Labura);
Institute of Dentistry, Faculty of Medicine, University of Tartu, Estonia (Estelle Saavaste);
College of Dentistry, University of Florida, United States of America (Natalie Atyeo); School of Dentistry, University of Michigan, United States of America (Alexandra Herzog);
Oral Health Research and Promotion Unit, Faculty of Dentistry, Al-Quds University, Palestine (Mayar Danadneh)
Author Contributions
Conceptualization, A.R., Y.H. and E.K.; methodology, A.R.; Y.H.; validation, H.A., S.D., M.M. and J.J.M.; formal analysis, A.R. and Y.H.; investigation I.-S.; data curation, I.-S.; writing—original draft preparation, A.R. and Y.H.; writing—review and editing, A.R., Y.H. and M.K. (Michal Koščík); supervision, E.K.; project administration, A.R.; funding acquisition, M.K. (Miloslav Klugar). All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by Masaryk University, grant numbers MUNI/IGA/1543/2020 and MUNI/A/1608/2020. The work of A.R. and M.K. (Miloslav Klugar) was supported by the INTER-EXCELLENCE grant number LTC20031—"Towards an International Network for Evidence-based Research in Clinical Health Research in the Czech Republic”.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Medicine, Masaryk University Ref. 4/2021 on 20 January 2021.
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.D’souza G., Dowdy D. What is Herd Immunity and How Can We Achieve It with COVID-19? [(accessed on 17 August 2021)]. Available online: https://www.jhsph.edu/covid-19/articles/achieving-herd-immunity-with-covid19.html.
- 2.Liao J., Fan S., Chen J., Wu J., Xu S., Guo Y., Li C., Zhang X., Wu C., Mou H., et al. Epidemiological and Clinical Characteristics of COVID-19 in Adolescents and Young Adults. Innov. 2020;1:100001. doi: 10.1016/j.xinn.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barber S.J., Kim H. COVID-19 Worries and Behavior Changes in Older and Younger Men and Women. J. Gerontol. 2021;76:e17–e23. doi: 10.1093/geronb/gbaa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ceccato I., Palumbo R., Di Crosta A., La Malva P., Marchetti D., Maiella R., Verrocchio M.C., Marin A., Mammarella N., Palumbo R., et al. Age-related differences in the perception of COVID-19 emergency during the Italian outbreak. Aging Ment. Health. 2020;25:1305–1313. doi: 10.1080/13607863.2020.1856781. [DOI] [PubMed] [Google Scholar]
- 5.Barari S., Caria S., Davola A., Falco P., Fetzer T., Fiorin S., Hensel L., Ivchenko A., Jachimowicz J., King G., et al. Evaluating COVID-19 Public Health Messaging in Italy: Self-Reported Compliance and Growing Mental Health Concerns. medRxiv. 2020 doi: 10.1101/2020.03.27.20042820. [DOI] [Google Scholar]
- 6.Guastafierro E., Toppo C., Magnani F.G., Romano R., Facchini C., Campioni R., Brambilla E., Leonardi M. Older Adults’ Risk Perception during the COVID-19 Pandemic in Lombardy Region of Italy: A Cross-sectional Survey. J. Gerontol. Soc. Work. 2021;64:585–598. doi: 10.1080/01634372.2020.1870606. [DOI] [PubMed] [Google Scholar]
- 7.Aw J., Seng J.J.B., Seah S.S.Y., Low L.L. COVID-19 Vaccine Hesitancy—A Scoping Review of Literature in High-Income Countries. Vaccines. 2021;9:900. doi: 10.3390/vaccines9080900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.PAHO . Introducing COVID-19 Vaccination: Guidance for Determining Priority Groups and Microplanning. Pan American Health Organization (PAHO); Washington, DC, USA: 2021. [Google Scholar]
- 9.Russo A.G., Decarli A., Valsecchi M.G. Strategy to identify priority groups for COVID-19 vaccination: A population based cohort study. Vaccine. 2021;39:2517–2525. doi: 10.1016/j.vaccine.2021.03.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benis A., Seidmann A., Ashkenazi S. Reasons for Taking the COVID-19 Vaccine by US Social Media Users. Vaccines. 2021;9:315. doi: 10.3390/vaccines9040315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riad A., Abdulqader H., Morgado M., Domnori S., Koščík M., Mendes J.J., Klugar M., Kateeb E. Global Prevalence and Drivers of Dental Students’ COVID-19 Vaccine Hesitancy. Vaccines. 2021;9:566. doi: 10.3390/vaccines9060566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puri N., Coomes E.A., Haghbayan H., Gunaratne K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020;16:2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kateeb E., Danadneh M., Pokorná A., Klugarová J., Abdulqader H., Klugar M., Riad A. Predictors of Willingness to Receive COVID-19 Vaccine: Cross-Sectional Study of Palestinian Dental Students. Vaccines. 2021;9:954. doi: 10.3390/vaccines9090954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Almaghaslah D., Alsayari A., Kandasamy G., Vasudevan R. COVID-19 Vaccine Hesitancy among Young Adults in Saudi Arabia: A Cross-Sectional Web-Based Study. Vaccines. 2021;9:330. doi: 10.3390/vaccines9040330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Riad A., Pokorná A., Antalová N., Krobot M., Zviadadze N., Serdiuk I., Koščík M., Klugar M. Prevalence and Drivers of COVID-19 Vaccine Hesitancy among Czech University Students: National Cross-Sectional Study. Vaccines. 2021;9:948. doi: 10.3390/vaccines9090948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Community Health. 2021;46:270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chadwick A., Kaiser J., Vaccari C., Freeman D., Lambe S., Loe B.S., Vanderslott S., Lewandowsky S., Conroy M., Ross A.R.N., et al. Online Social Endorsement and Covid-19 Vaccine Hesitancy in the United Kingdom. Soc. Media Soc. 2021;7 doi: 10.1177/20563051211008817. [DOI] [Google Scholar]
- 18.Juvinyà-Canal D., Suñer-Soler R., Porquet A.B., Vernay M., Blanchard H., Bertran-Noguer C. Health Literacy among Health and Social Care University Students. Int. J. Environ. Res. Public Health. 2020;17:2273. doi: 10.3390/ijerph17072273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vozikis A., Drivas K., Milioris K. Health literacy among university students in Greece: Determinants and association with self-perceived health, health behaviours and health risks. Arch. Public Heal. 2014;72:1–6. doi: 10.1186/2049-3258-72-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sukys S., Cesnaitiene V.J., Ossowsky Z.M. Is health education at university associated with students’ health literacy? evidence from cross-sectional study applying HLS-EU-Q. Biomed Res. Int. 2017;2017 doi: 10.1155/2017/8516843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Belingheri M., Facchetti R., Scordo F., Butturini F., Turato M., De Vito G., Cesana G., Riva M.A. Risk behaviors among Italian healthcare students: A cross-sectional study for health promotion of future healthcare workers. Med. Lav. 2019;110:155. doi: 10.23749/MDL.V110I2.7573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alba L.H., Badoui N., Gil F. Attitude toward preventive counseling and healthy practices among medical students at a Colombian university. Front. Med. 2015;9:251–259. doi: 10.1007/s11684-015-0393-z. [DOI] [PubMed] [Google Scholar]
- 23.Frank E., Carrera J.S., Elon L., Hertzberg V.S. Predictors of US medical students’ prevention counseling practices. Prev. Med. 2007;44:76–81. doi: 10.1016/j.ypmed.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 24.Lobelo F., Duperly J., Frank E. Physical activity habits of doctors and medical students influence their counselling practices. Br. J. Sports Med. 2009;43:89–92. doi: 10.1136/bjsm.2008.055426. [DOI] [PubMed] [Google Scholar]
- 25.Alawia R., Riad A., Kateeb E. Risk perception and readiness of dental students to treat patients amid COVID-19: Implication for dental education. Oral Dis. 2020 doi: 10.1111/odi.13593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alawia R., Riad A., Kateeb E. Knowledge and attitudes among dental students about COVID-19 and its precautionary measures: A cross-sectional study. J. Oral Med. Oral Surg. 2021;27:17. doi: 10.1051/mbcb/2020056. [DOI] [Google Scholar]
- 27.Wu D.T., Wu K.Y., Nguyen T.T., Tran S.D. The impact of COVID-19 on dental education in North America—Where do we go next? Eur. J. Dent. Educ. 2020;24:825–827. doi: 10.1111/eje.12561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iyer P., Aziz K., Ojcius D.M. Impact of COVID-19 on dental education in the United States. J. Dent. Educ. 2020;84:718–722. doi: 10.1002/jdd.12163. [DOI] [PubMed] [Google Scholar]
- 29.Machado R.A., Bonan P.R.F., Da Cruz Perez D.E., Martelli Júnior H. COVID-19 pandemic and the impact on dental education: Discussing current and future perspectives. Braz. Oral Res. 2020;34:e083. doi: 10.1590/1807-3107bor-2020.vol34.0083. [DOI] [PubMed] [Google Scholar]
- 30.dos Santos J.A., Normando A.G.C., da Silva R.L.C., Acevedo A.C., Canto G.D.L., Sugaya N., Santos-Silva A.R., Guerra E.N.S. Oral Manifestations in Patients with COVID-19: A 6-Month Update. J. Dent. Res. 2021 doi: 10.1177/00220345211029637. [DOI] [PubMed] [Google Scholar]
- 31.Riad A., Kassem I., Badrah M., Klugar M. Acute Parotitis as a Presentation of COVID-19? Oral Dis. 2020:odi.13571. doi: 10.1111/odi.13571. [DOI] [PubMed] [Google Scholar]
- 32.Riad A., Kassem I., Hockova B., Badrah M., Klugar M. Halitosis in COVID-19 patients. Spec. Care Dent. 2021;41:282–285. doi: 10.1111/scd.12547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riad A., Kassem I., Stanek J., Badrah M., Klugarova J., Klugar M. Aphthous Stomatitis in COVID-19 Patients: Case-series and Literature Review. Dermatol. Ther. 2021;34 doi: 10.1111/dth.14735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hocková B., Riad A., Valky J., Šulajová Z., Stebel A., Slávik R., Bečková Z., Pokorná A., Klugarová J., Klugar M. Oral Complications of ICU Patients with COVID-19: Case-Series and Review of Two Hundred Ten Cases. J. Clin. Med. 2021;10:581. doi: 10.3390/jcm10040581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Riad A., Gomaa E., Hockova B., Klugar M. Oral Candidiasis of COVID-19 Patients: Case Report and Review of Evidence. J. Cosmet. Dermatol. 2021;20:1580–1584. doi: 10.1111/jocd.14066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Riad A., Kassem I., Hockova B., Badrah M., Klugar M. Tongue ulcers associated with SARS--CoV-2 infection: A case series. Oral Dis. 2020:odi.13635. doi: 10.1111/odi.13635. [DOI] [PubMed] [Google Scholar]
- 37.Riad A., Boccuzzi M., Sagiroglu D., Klugar M., Krsek M. Pediatric multisystem inflammatory syndrome temporally associated with SARS-COV-2: Oral manifestations and implications. Int. J. Paediatr. Dent. 2020;31:ipd.12694. doi: 10.1111/ipd.12694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Umeizudike K.A., Isiekwe I.G., Fadeju A.D., Akinboboye B.O., Aladenika E.T. Nigerian undergraduate dental students’ knowledge, perception, and attitude to COVID-19 and infection control practices. J. Dent. Educ. 2021;85:187–196. doi: 10.1002/jdd.12423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davide S., Macarelli C., Lam A. Vaccination Recommendations for Oral Health Professionals. [(accessed on 15 April 2021)]. Available online: https://decisionsindentistry.com/article/vaccination-recommendations-for-oral-health-professionals/
- 40.Souza R.A., Namen F.M., Galan J., Jr., Vieira C., Sedano H.O. Infection Control Measures Among Senior Dental Students in Rio de Janeiro State, Brazil. J. Public Health Dent. 2006;66:282–284. doi: 10.1111/j.1752-7325.2006.tb04084.x. [DOI] [PubMed] [Google Scholar]
- 41.Singh A., Purohit B.M., Bhambal A., Saxena S., Singh A., Gupta A. Knowledge, Attitudes, and Practice Regarding Infection Control Measures among Dental Students in Central India. J. Dent. Educ. 2011;75:421–427. doi: 10.1002/j.0022-0337.2011.75.3.tb05055.x. [DOI] [PubMed] [Google Scholar]
- 42.Shetty S., Prabhu S., Shetty V., Shetty A.K. Knowledge, attitudes and factors associated with acceptability of human papillomavirus vaccination among undergraduate medical, dental and nursing students in South India. Hum. Vaccin. Immunother. 2019;15:1656–1665. doi: 10.1080/21645515.2019.1565260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rutkoski H., Tay D.L., Dixon B.L., Pinzon L.M., Mooney R., Winkler J.R., Kepka D. A Multi-state Evaluation of Oral Health Students’ Knowledge of Human Papillomavirus-Related Oropharyngeal Cancer and HPV Vaccination. J. Cancer Educ. 2020;35:1017–1025. doi: 10.1007/s13187-019-01561-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Farsi N.J., Al Sharif S., Al Qathmi M., Merdad M., Marzouki H., Merdad L. Knowledge of Human Papillomavirus (HPV) and Oropharyngeal Cancer and Acceptability of the HPV Vaccine among Dental Students. Asian Pac. J. Cancer Prev. 2020;21:3595–3603. doi: 10.31557/APJCP.2020.21.12.3595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Szmyd B., Karuga F.F., Bartoszek A., Staniecka K., Siwecka N., Bartoszek A., Błaszczyk M., Radek M. Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland. Vaccines. 2021;9:218. doi: 10.3390/vaccines9030218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lucia V.C., Kelekar A., Afonso N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health. 2020:1–5. doi: 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sovicova M., Zibolenova J., Svihrova V., Hudeckova H. Odds Ratio Estimation of Medical Students’ Attitudes towards COVID-19 Vaccination. Int. J. Environ. Res. Public Health. 2021;18:6815. doi: 10.3390/ijerph18136815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Olaimat A.N., Aolymat I., Shahbaz H.M., Holley R.A. Knowledge and Information Sources About COVID-19 among University Students in Jordan: A Cross-Sectional Study. Front. Public Health. 2020;8:254. doi: 10.3389/fpubh.2020.00254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huang S., Yang J., Fong S., Zhao Q. Artificial intelligence in the diagnosis of COVID-19: Challenges and perspectives. Int. J. Biol. Sci. 2021;17:1581. doi: 10.7150/ijbs.58855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gunasekeran D.V., Tseng R.M.W.W., Tham Y.-C., Wong T.Y. Applications of digital health for public health responses to COVID-19: A systematic scoping review of artificial intelligence, telehealth and related technologies. NPJ Digit. Med. 2021;4:1–6. doi: 10.1038/s41746-021-00412-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van der Schaar M., Alaa A.M., Floto A., Gimson A., Scholtes S., Wood A., McKinney E., Jarrett D., Lio P., Ercole A. How artificial intelligence and machine learning can help healthcare systems respond to COVID-19. Mach. Learn. 2020;110:1–14. doi: 10.1007/s10994-020-05928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mendels D.-A., Dortet L., Emeraud C., Oueslati S., Girlich D., Ronat J.-B., Bernabeu S., Bahi S., Atkinson G.J.H., Naas T. Using artificial intelligence to improve COVID-19 rapid diagnostic test result interpretation. Proc. Natl. Acad. Sci. USA. 2021;118:2021. doi: 10.1073/pnas.2019893118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hussain A., Tahir A., Hussain Z., Sheikh Z., Gogate M., Dashtipour K., Ali A., Sheikh A. Artificial Intelligence–Enabled Analysis of Public Attitudes on Facebook and Twitter Toward COVID-19 Vaccines in the United Kingdom and the United States: Observational Study. J. Med. Internet Res. 2021;23:e26627. doi: 10.2196/26627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hatmal M.M., Al-Hatamleh M.A.I., Olaimat A.N., Hatmal M., Alhaj-Qasem D.M., Olaimat T.M., Mohamud R. Side Effects and Perceptions Following COVID-19 Vaccination in Jordan: A Randomized, Cross-Sectional Study Implementing Machine Learning for Predicting Severity of Side Effects. Vaccines. 2021;9:556. doi: 10.3390/vaccines9060556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Griffith J., Marani H., Monkman H. COVID-19 vaccine hesitancy in Canada: A content analysis of Tweets using the Theoretical Domains Framework. J. Med. Internet Res. 2020;23:e26874. doi: 10.2196/26874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.International Association of Dental Students (IADS) Workforce. [(accessed on 14 March 2021)]. Available online: https://iads-web.org/governance/workforce/
- 57.International Association of Dental Students (IADS) Delegates List. [(accessed on 14 March 2021)]. Available online: https://iads-web.org/governance/delegates/
- 58.KoBoToolbox.org KoBoToolbox. [(accessed on 15 August 2020)]. Available online: https://support.kobotoolbox.org/welcome.html.
- 59.Larson H.J., Jarrett C., Schulz W.S., Chaudhuri M., Zhou Y., Dube E., Schuster M., MacDonald N.E., Wilson R., Eskola J., et al. Measuring vaccine hesitancy: The development of a survey tool. Vaccine. 2015;33:4165–4175. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 60.Strategic Advisory Group of Experts on Immunization (SAGE) Report of the Sage Working Group on Vaccine Hesitancy. World Health Organization; Geneva, Switzerland: 2014. [Google Scholar]
- 61.Dudley M.Z., Privor-Dumm L., Dubé È., MacDonald N.E. Words matter: Vaccine hesitancy, vaccine demand, vaccine confidence, herd immunity and mandatory vaccination. Vaccine. 2020;38:709–711. doi: 10.1016/j.vaccine.2019.11.056. [DOI] [PubMed] [Google Scholar]
- 62.World Medical Association World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA−J. Am. Med. Assoc. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 63.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. UroToday Int. J. 2009;2 doi: 10.1097/EDE.0b013e3181577654. [DOI] [PubMed] [Google Scholar]
- 64.Proton Technologies AG General Data Protection Regulation (GDPR) Compliance Guidelines. [(accessed on 1 May 2020)]. Available online: https://gdpr.eu/
- 65.Boerner F., Keelan J., Winton L., Jardine C., Driedger S.M. Understanding the interplay of factors informing vaccination behavior in three Canadian provinces. Hum. Vaccines Immunother. 2013;9:1477–1484. doi: 10.4161/hv.24427. [DOI] [PubMed] [Google Scholar]
- 66.jamovi (Version 1.6) The jamovi Project. [(accessed on 2 August 2021)]. Available online: https://www.jamovi.org/
- 67.World Bank World Bank Country and Lending Groups. [(accessed on 14 March 2021)]. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 68.Al-Jayyousi G.F., Sherbash M.A.M., Ali L.A.M., El-Heneidy A., Alhussaini N.W.Z., Elhassan M.E.A., Nazzal M.A. Factors Influencing Public Attitudes towards COVID-19 Vaccination: A Scoping Review Informed by the Socio-Ecological Model. Vaccines. 2021;9:548. doi: 10.3390/vaccines9060548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Carrieri V., Lagravinese R., Resce G. Predicting vaccine hesitancy from area-level indicators: A machine learning approach. medRxiv. 2021 doi: 10.1101/2021.03.08.21253109. [DOI] [PubMed] [Google Scholar]
- 70.Kollamparambil U., Oyenubi A., Nwosu C. COVID19 Vaccine Intentions in South Africa: Health Communication Strategy to Address Vaccine Hesitancy. Res. Sq. 2021 doi: 10.21203/RS.3.RS-533888/V1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Soares P., Rocha J.V., Moniz M., Gama A., Laires P.A., Pedro A.R., Dias S., Leite A., Nunes C. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines. 2021;9:300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Reno C., Maietti E., Fantini M.P., Savoia E., Manzoli L., Montalti M., Gori D. Enhancing COVID-19 Vaccines Acceptance: Results from a Survey on Vaccine Hesitancy in Northern Italy. Vaccines. 2021;9:378. doi: 10.3390/vaccines9040378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Callaghan T., Moghtaderi A., Lueck J.A., Hotez P.J., Strych U., Dor A., Franklin Fowler E., Motta M. Correlates and Disparities of COVID-19 Vaccine Hesitancy. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3667971. [DOI] [Google Scholar]
- 74.Bertoncello C., Ferro A., Fonzo M., Zanovello S., Napoletano G., Russo F., Baldo V., Cocchio S. Socioeconomic Determinants in Vaccine Hesitancy and Vaccine Refusal in Italy. Vaccines. 2020;8:276. doi: 10.3390/vaccines8020276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sandhofer M.J., Robak O., Frank H., Kulnig J., Sandhofer M.J., Frank H., Robak O., Kulnig J. Vaccine hesitancy in Austria A cross-sectional survey. Wien. Klin. Wochenschr. 2017;129:59–64. doi: 10.1007/s00508-016-1062-1. [DOI] [PubMed] [Google Scholar]
- 76.Raude J., Fressard L., Gautier A., Pulcini C., Peretti-Watel P., Verger P. Opening the ‘Vaccine Hesitancy’ black box: How trust in institutions affects French GPs’ vaccination practices. Expert Rev. Vaccines. 2016;15:937–948. doi: 10.1080/14760584.2016.1184092. [DOI] [PubMed] [Google Scholar]
- 77.Kalok A., Loh S.Y.E., Chew K.T., Abdul Aziz N.H., Shah S.A., Ahmad S., Mohamed Ismail N.A., Abdullah Mahdy Z. Vaccine hesitancy towards childhood immunisation amongst urban pregnant mothers in Malaysia. Vaccine. 2020;38:2183–2189. doi: 10.1016/j.vaccine.2020.01.043. [DOI] [PubMed] [Google Scholar]
- 78.Giambi C., Fabiani M., D’Ancona F., Ferrara L., Fiacchini D., Gallo T., Martinelli D., Pascucci M.G., Prato R., Filia A., et al. Parental vaccine hesitancy in Italy—Results from a national survey. Vaccine. 2018;36:779–787. doi: 10.1016/j.vaccine.2017.12.074. [DOI] [PubMed] [Google Scholar]
- 79.Rungkitwattanakul D., Yabusaki A., Singh D., Lawson P., Nwaogwugwu U., Iheagwara O.S., Mere C. COVID-19 vaccine hesitancy among African American hemodialysis patients: A single-center experience. Hemodial. Int. 2021 doi: 10.1111/hdi.12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Karafillakis E., Dinca I., Apfel F., Cecconi S., Wűrz A., Takacs J., Suk J., Celentano L.P., Kramarz P., Larson H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine. 2016;34:5013–5020. doi: 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 81.Biswas N., Mustapha T., Khubchandani J., Price J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health. 2021:1–8. doi: 10.1007/S10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Díaz Crescitelli M.E., Ghirotto L., Sisson H., Sarli L., Artioli G., Bassi M.C., Appicciutoli G., Hayter M. A Meta-Synthesis Study of the Key Elements Involved in Childhood Vaccine Hesitancy. Public Health. 2020;180:38–45. doi: 10.1016/j.puhe.2019.10.027. [DOI] [PubMed] [Google Scholar]
- 83.Islam M.S., Siddique A.B., Akter R., Tasnim R., Sujan M.S.H., Ward P.R., Sikder M.T. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: A cross-sectional community survey in Bangladesh. medRxiv. 2021 doi: 10.1101/2021.02.16.21251802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dinga J.N., Sinda L.K., Titanji V.P.K. Assessment of vaccine hesitancy to a covid-19 vaccine in cameroonian adults and its global implication. Vaccines. 2021;9:175. doi: 10.3390/vaccines9020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Acheampong T., Akorsikumah E.A., Osae-Kwapong J., Khalid M., Appiah A., Amuasi J.H. Examining Vaccine Hesitancy in Sub-Saharan Africa: A Survey of the Knowledge and Attitudes among Adults to Receive COVID-19 Vaccines in Ghana. Vaccines. 2021;9:814. doi: 10.3390/vaccines9080814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Afolabi A.A., Ilesanmi O.S. Dealing with vaccine hesitancy in Africa: The prospective COVID-19 vaccine context. Pan Afr. Med. J. 2021;38:1–7. doi: 10.11604/pamj.2021.38.3.27401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Maraqa B., Nazzal Z., Rabi R., Sarhan N., Al-Shakhrah K., Al-Kaila M. COVID-19 vaccine hesitancy among health care workers in Palestine: A call for action. Prev. Med. 2021;149:106618. doi: 10.1016/j.ypmed.2021.106618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rey D., Fressard L., Cortaredona S., Bocquier A., Gautier A., Peretti-Watel P., Verger P., On Behalf of the Baromètre Santé 2016 Group Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk–benefit balance. Eurosurveillance. 2018;23:17-00816. doi: 10.2807/1560-7917.ES.2018.23.17.17-00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lane S., MacDonald N.E., Marti M., Dumolard L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine. 2018;36:3861–3867. doi: 10.1016/j.vaccine.2018.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Miko D., Costache C., Colosi H.A., Neculicioiu V., Colosi I.A. Qualitative Assessment of Vaccine Hesitancy in Romania. Medicina. 2019;55:282. doi: 10.3390/medicina55060282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Riad A., Pokorná A., Attia S., Klugarová J., Koščík M., Klugar M. Prevalence of COVID-19 Vaccine Side Effects among Healthcare Workers in the Czech Republic. J. Clin. Med. 2021;10:1428. doi: 10.3390/jcm10071428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Menni C., Klaser K., May A., Polidori L., Capdevila J., Louca P., Sudre C.H., Nguyen L.H., Drew D.A., Merino J., et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: A prospective observational study. Lancet. Infect. Dis. 2021 doi: 10.1016/S1473-3099(21)00224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Riad A., Pokorná A., Mekhemar M., Conrad J., Klugarová J., Koščík M., Klugar M., Attia S. Safety of ChAdOx1 nCoV-19 Vaccine: Independent Evidence from Two EU States. Vaccines. 2021;9:673. doi: 10.3390/vaccines9060673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Alhazmi A., Alamer E., Daws D., Hakami M., Darraj M., Abdelwahab S., Maghfuri A., Algaissi A. Evaluation of Side Effects Associated with COVID-19 Vaccines in Saudi Arabia. Vaccines. 2021;9:674. doi: 10.3390/vaccines9060674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Klugar M., Riad A., Mekhemar M., Conrad J., Buchbender M., Howaldt H.-P., Attia S. Side Effects of mRNA-Based and Viral Vector-Based COVID-19 Vaccines among German Healthcare Workers. Biology. 2021;10:752. doi: 10.3390/biology10080752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Riad A., Schünemann H., Attia S., Peričić T.P., Žuljević M.F., Jürisson M., Kalda R., Lang K., Morankar S., Yesuf E.A., et al. COVID-19 Vaccines Safety Tracking (CoVaST): Protocol of a Multi-Center Prospective Cohort Study for Active Surveillance of COVID-19 Vaccines’ Side Effects. Int. J. Environ. Res. Public Health. 2021;18:7859. doi: 10.3390/ijerph18157859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jęśkowiak I., Wiatrak B., Grosman-Dziewiszek P., Szeląg A. The Incidence and Severity of Post-Vaccination Reactions after Vaccination against COVID-19. Vaccines. 2021;9:502. doi: 10.3390/vaccines9050502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Riad A., Sağıroğlu D., Üstün B., Pokorná A., Klugarová J., Attia S., Klugar M. Prevalence and Risk Factors of CoronaVac Side Effects: An Independent Cross-Sectional Study among Healthcare Workers in Turkey. J. Clin. Med. 2021;10:2629. doi: 10.3390/jcm10122629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Riad A., Hocková B., Kantorová L., Slávik R., Spurná L., Stebel A., Havriľak M., Klugar M. Side Effects of mRNA-Based COVID-19 Vaccine: Nationwide Phase IV Study among Healthcare Workers in Slovakia. Pharmaceuticals. 2021;14:873. doi: 10.3390/ph14090873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Eskola J., Duclos P., Schuster M., MacDonald N.E., Liang X., Chaudhuri M., Dube E., Gellin B., Goldstein S., Larson H., et al. How to deal with vaccine hesitancy? Vaccine. 2015;33:4215–4217. doi: 10.1016/j.vaccine.2015.04.043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.