Abstract
Alzheimer’s disease (AD), as a neurodegenerative disorder, is characterized by mass neuronal and synaptic loss and, currently, there are no successful curative therapies. Extracellular vesicles (EVs) are an emerging approach to intercellular communication via transferring cellular materials such as proteins, lipids, mRNAs, and miRNAs from parental cells to recipient cells, leading to the reprogramming of the molecular machinery. Numerous studies have suggested the therapeutic potential of EVs derived from mesenchymal stem cells (MSCs) in the treatment of AD, based on the neuroprotective, regenerative and immunomodulatory effects as effective as MSCs. In this review, we focus on the biology and function of EVs, the potential of MSC-derived EVs for AD therapy in preclinical and clinical studies, as well as the potent mechanisms of MSC-derived EVs actions. Finally, we highlight the modification strategies and diagnosis utilities in order to make advance in this field.
Keywords: Alzheimer’s disease, mesenchymal stem cells, extracellular vesicles, therapy
1. Introduction
Alzheimer’s disease (AD) is the world’s most common cause of dementia that will affect over 100 million people by 2050, and which will bring a significant physical, psychological, social and economic burden to patients, their families, caregivers and society [1]. As a neurodegenerative disease, the clinical symptoms of AD include severe cognitive impairments, irreversible memory loss and motor abnormalities, which are attributed to the loss of synapses and neurons in vulnerable regions [2]. AD is characterized by increased neuritic (senile) plaques composed of β-amyloid (Aβ) peptides [3]. Excess aggregated Aβ peptide is generally considered to initiate the pathogenic cascade, including propagation of microtubule-associated tau aggregation throughout the brain [4]. In the past decades, strategies targeting Aβs are mainstream approaches for the treatment and prevention of AD; most of the relevant clinical trials have been conducted at the early/pre-symptomatic stage of AD [5,6]. For instance, the initial trial of aducanumab, an Aβ-directed monoclonal antibody, has shown that it could significantly slow cognitive decline in patients with early stages of AD and reduce Aβ plaques in a dose-and time-dependent manner [7]. Additionally, aducanumab has been approved for medical use in the United States by the FDA in June 2021, but this decision is still controversial and follow-up study is required [8,9]. When it comes to Aβ-targeting drugs, most of them did not show positive outcomes in their phase III trials, e.g., semagacestat, verubecestat, solanezumab and gantenerumab [10,11,12]. Despite that there are five FDA-approved medications for clinical use in dementia, including three cholinesterase inhibitors (donepezil, rivastigmine, and galantamine), a N-methyl-d-aspartate (NMDA) receptor inhibitor (memantine), and a combination therapy with the cholinergic and glutamatergic inhibitors, the symptoms of AD may be improved but the disease progression fails to be halted [1]. It is apparent that a single remedy targeting Aβs is not sufficient to cure AD and the optimal therapeutic approach should tackle Aβ-induced AD pathology as well as prevent cognitive decline simultaneously.
In recent years, mesenchymal stem cells (MSCs) have been used as potential therapeutic cells in multiple diseases due to their immunomodulatory and tissue regenerative properties [13]. MSCs are adult multipotent stem cells that exist in multiple tissues, including bone marrow, adipose tissue, umbilical cord and peripheral blood. They are able to self-renew and differentiate into osteogenic, chondrogenic, adipogenic, myogenic, or stromal lineages. Under different culture conditions, MSCs are reported to differentiate into neuronal cells, hepatocytes, cardiomyocytes, alveolar and gut epithelial cells, making them a promising source in the regenerative medicine. Numerous reports have addressed the beneficial effects of MSCs in damaged tissue repair, including liver failure rescue [14,15], cardiovascular regeneration [16,17], treatment of stroke [18], spinal cord injury [19] and lung fibrosis [20]. Since the characteristics of AD include mass loss of synapses and neurons, MSC transplantation is a rational therapeutic strategy for regeneration of neuronal circuits [21]. Studies have indicated that MSCs are able to reduce Aβ deposition, enhance neurogenesis, alleviate spatial learning and memory deficits in both cellular models and animal models of AD [22,23,24]. Notably, these therapeutic effects in tissue protection and repair are attributed to the paracrine action of MSCs, and further emphasize the role of soluble factors including extracellular vesicles (EVs) secreted from MSCs [25,26].
Several published reviews have described the biogenesis and methodology of isolation of EVs in detail [27,28,29,30,31,32]. In the following paragraphs, we review the origins and characterization of isolated EVs, summarize the current applications of MSC-derived EVs in AD treatments and the molecular/cellular mechanisms of MSC derived EVs actions during therapy, and discuss the potential of drug delivery vehicles and diagnosis utilities for AD. The electronic searches were performed in PubMed, EMBASE, Google Scholar, Clinical Trials database, from 2002 to 2021. The following combinations were used in a search of titles and abstracts in September 2021: Alzheimer’s disease and mesenchymal stem cells; Alzheimer’s disease and mesenchymal stem cells and extracellular vesicles; Alzheimer’s disease and mesenchymal stem cells and exosomes; Alzheimer’s disease and mesenchymal stem cells and microvesicles. The abstracts of all the relevant articles were reviewed by the authors, who further ensured these relevant articles were included in the current review.
2. Origins, Classification and Nomenclature of EVs
In general, EVs can be divided into three classes depending on their size and origins, including exosomes, microvesicles (MVs) and apoptotic bodies (ABs) [33]. Exosomes are nanoscale vesicles (30~200 nm) secreted from most types of cells, and commonly found in plasma, tears, urine, breast milk and body fluids [34]. When molecules are transported through the cell membrane via endocytosis, the cargos are formed and then delivered to early endosomes. During the maturation of early endosomes, the cargos are sorted to form interluminal vesicles (ILVs) through the folding back of the endosomal-limiting membrane. ILVs are the origin of exosomes encapsulated by multivesicular bodies (MVBs); the release of ILVs in the form of exosomes is switched in the absence of recycling molecules, such as transferrin receptors or mannose 6-phosphate receptors [35,36].
Different from exosomes, MVs are heterogeneous vesicles with a broad range of size distribution (45–1000 nm), directly budding from the plasma membrane, then released into the extracellular space [37]. The biogenesis of MVs is dependent on the phospholipid asymmetry, lipid transporter activity and calcium signaling [38]. In contrast, the biogenesis of exosomes occurs via the endosomal sorting complex required for a transport (ESCRT)-dependent pathway that is required for the process of cargo ubiquitination in the pre-MVB/early endosomes. The cargos transferred to endosome are selected by the ESCRT-binding ubiquitinated proteins [39]. Despite that the biogenesis of MVs has been reported to be regulated by ESCRT independent pathways, the ESCRT-I subunit TSG101 is found to interact with arrestin domain-containing protein 1 (ARRDC1) to control the release of MVs. In other words, ESCRT proteins are involved in MVs biogenesis [40]. Unlike the canonical ESCRT pathway, a recent report has addressed that the biogenesis of exosomes can be modulated by active RAB31, a Ras-related protein, driving the formation of epidermal growth factor receptor (EGFR)-containing ILV, thereby decreasing GTPase Rab7 activity to prevent the fusion of MVBs with lysosomes and eventually promoting exosomes release [41]. There are various factors involved in biogenesis pathways and the process remains elusive. In addition, apoptotic bodies (ABs), one of EV subtypes, are released when cells undergo apoptosis. Once the apoptosis is induced, a series of events happen, including cell shrinking, chromatin condensation, organelles collapse, and membrane blebbing, leading to the formation of apoptotic bodies (ABs) [42,43]. ABs also carry various molecules, e.g., proteins, lipids, and RNAs, but the size (1–2 μm) is much larger than other EV subgroups [44]. Smaller ABs, termed apoptotic vesicles, have been identified [45]. In fact, ABs present phosphatidylserine (PS) on their surfaces, so they are cleared quickly. It elucidates that the more precise classification of EVs subtypes is needed.
Over the past decade, the number of publications about EVs research is increasing exponentially [46]. These studies include the basic research (biogenesis, secretion, uptake, and pharmacokinetic properties), biomarker identification (EVs, EV-carried proteins, EV-carried RNA, EV-carried DNA, EV-carried microRNA, and EV-carried lipids), pharmaceutical agents (native and engineered EVs), and biomaterial-based drug delivery (loading with protein, microRNA, or drugs) [47,48]. However, the nomenclature of EVs was not defined accurately. These irregular terms used to describe vesicles not only have led to misunderstanding for readers but also caused the findings hard to verify. In 2014, the International Society for Extracellular Vesicles (ISEV) promulgated guidelines called MISEV (minimal information for studies of extracellular vesicles) for the investigators who conduct the EVs studies [47], and now also updated to the latest version (MISEV 2018) [49]. According to these guidelines, “extracellular vesicle” is an expert consensus term and is used to describe the vesicle that cannot replicate and naturally be secreted from the cell and consists of lipid bilayers. Nevertheless, other terms are not prohibited. For instance, the term “exosomes” is generally used in industry, which might fascinate costumers to purchase the related products [50]. In general, the term “EV” is widely used in research and the use of other terms should be defined carefully and clearly.
3. Recommendations in Characterization of EVs
Based on MISEV 2018, the characterization of protein markers should be verified using at least three positive markers (one transmembrane/lipid-bound protein is included) and one negative marker. In terms of characterization of a single particle, one electron or atomic force microscopy and one single particle analyzer should be included to examine the size, distribution, and morphology of EVs. Regarding the characterization of protein markers, tetraspanins (e.g., CD9, CD63, CD81, CD82), MVB biogenesis-related protein (Alix, and TSG101), and heat-shock proteins (Hsp60, Hsp70, and Hsp90) are generally used as EVs’ markers [51]. In addition, the proteins specially expressed in cells need to be found in EVs (as cell-type fingerprint) [52]. For example, EVs secreted from T cells and B cells contain T cell receptor (TCR) and B cell receptor (BCR), respectively [53]. MSC-derived EVs bear the markers of CD29, CD44, CD73 and CD90; these markers are widely used in characterization of MSCs [54].
As a subtype of EVs, MVs also package the abundant proteins and nucleic acids that serve as biomarkers for identifying the disease types and the prognosis of disease state [55]. However, the specific markers of MV are still lacking; it is hard to differentiate the MVs from other subgroups of EVs by proteins markers. Since the results obtained from current studies have shown that MVs can be used as good biomarkers for diseases without excluding the existence of other vesicles, pure MVs seem not to be necessary in clinical analysis [56,57,58]. With the large size, ABs can be easily distinguished from smaller vesicles by transmission electron microscopy (TEM), dynamic light scattering (DLS) and nanoparticle tracking analysis (NTA). The specific proteins related to apoptotic process, such as tubulin β-1 and β-4, integrin β-3, Ras-related protein, Fructose-2-P-Aldolase and Glutathione-S-Transferase omega-1, are found in ABs [59]. However, increasing studies have indicated that ABs are not the only secreted vesicles during apoptosis, both apoptotic exosomes (ApoExos) and apoptotic microvesicles (ApoMVs) are also released from apoptotic cells but exhibit different origins, heterogeneities and physical characteristics. Thus, the terms “ApoEVs” are gradually used to describe the EVs released from dying cells rather than “ABs” [60,61]. Collectively, the work of characterizing EVs is under development, and investigators can follow the guidelines recommended by MISEV 2018 to characterize the vesicles they collect.
4. Application of MSC-Derived EVs in AD Treatment
EVs act as mediators of intercellular communication through transferring bioactive molecules such as proteins, lipids, mRNAs, microRNAs (miRNAs), genomic DNA and mitochondrial DNA. When recipient cells uptake these bioactive molecules, the molecular machinery of cells is altered in an epigenetic way [51,62,63]. Besides, EVs can serve as drug delivery vectors to transfer enhanced therapeutic agents through chemically or biologically engineering to treat diseases or halt disease progression. The beneficial effect of MSC-derived EVs has been demonstrated in animal models of multiple diseases, such as chronic kidney disease, ischemic stroke, pulmonary hypertension, indicating that MSC-derived EVs exert similar effects as MSCs [64,65,66,67,68]. Due to their high stability in the bloodstream and the capacity to penetrate blood-brain barrier (BBB), MSC-derived EVs have a great potential for the treatment of neurological and neurodegenerative diseases, which has been experimentally confirmed as EVs administration through both intravenous and intranasal routes [25,69,70,71,72]. Additionally, an inflammatory state in AD or Parkinson’s disease (PD) makes the BBB more vulnerable to facilitate EVs transport from the peripheral circulation to the brain [73,74,75]. Therefore, it could reasonably be expected that MSC-derived EVs manifest beneficial effects in AD treatments.
MSC-derived EVs have shown promise in improving the cognitive deficits induced by Aβ1–42 aggregates and promoting neurogenesis in the hippocampus and subventricular zone (SVZ), which are of great significance in the transition from short-term memory to long-term memory [70,76]. In vitro results have addressed that MSC-derived EVs protect neurons from oxidative stress and synapse damage induced by Aβ oligomers [77,78]. Wang et al. and our lab demonstrated the positive effect of using MSC-derived EVs (BM-MSCs and WJ-MSCs, respectively) both in vitro and in vivo [71,79]. BM-MSC-derived EVs significantly reduced Aβs induced inducible nitric oxide synthase (iNOS) expression in cultured primary neurons. Administration of BM-MSC-derived EVs intracerebroventricularly was shown to improve cognitive behavior, rescue synaptic transmission in hippocampal CA1 regions and long-term potentiation (LTP) in APP/PS1 transgenic mice. In our research, the human neuroblastoma cell line overexpressing FAD mutations and J20 transgenic mice were used to investigate the therapeutic effect of WJ-MSC-derived EVs. Reduced Aβ expression and restored expression of neuronal memory/synaptic plasticity-related genes were observed in the cell model. In vivo studies demonstrated improved cognitive function, restored glucose metabolism, and inhibited astrocytes/microglia activation in mice that were administrated with WJ-MSC-derived EVs through an intravenous injection [71]. Furthermore, an alternative delivery of MSC-derived EVs for therapeutic intervention in AD through the intranasal route has been used in recent studies owing to the safety, low invasive procedure and a higher amount of EVs reaching the brain [70,80,81]. Similarly, MSC-derived EVs exhibit neuroprotective and immunomodulatory potential, evidenced by increased dendritic spine density and decreased microglia activation in treated mice [80]. Another recent study has demonstrated that MSC-derived EVs can lower Aβ plaque burden and decrease the colocalization between Aβ plaque and glial fibrillary acidic protein (GFAP, a reactive astrocyte marker) in the brain [81]. The therapeutic effects of MSC-derived EVs obtained from the cell and animal models of AD are summarized in Table 1.
Table 1.
A summary of preclinical studies of MSC-derived EVs-based therapy both in vitro and in vivo models of AD.
| Model | Source of EVs | Protocol | Administration Route | Reported Effects | Ref. |
|---|---|---|---|---|---|
| In vitro models | |||||
| N2a cells | ADSCs | 500 µg/well, 24 h | Co-culture | Decreased extracellular and intracellular Aβs levels | [82] |
| SH-SY5Y-APPswe cells | UC-MSC | 2 μg/well for 24 h | Co-culture | Decreased extracellular and intracellular Aβs levels | [83] |
| SH-SY5Y-APP(S/L) cells | WJ-MSCs | 50 µg/well, twice a week for 1 week | Co-culture | Decreased Aβs expression and restored the expression of neuronal memory/synaptic plasticity-related genes | [71] |
| NSCs isolated from Tg2576 mice | ADSCs | 200 μg/mL for 24 or 48 h | Co-culture | Reduced Aβ levels and the Aβ 42/40 ratio, increased neurite growth and alleviated cell apoptosis | [84] |
| Cortical neuron culture from newborn APP/PS1 mice | BM-MSCs | 100 μg/mL for 12 h | Co-culture | Reduced Aβs induced iNOS expression | [79] |
| Hippocampal neuron culture from rat embryos (E18) | BM-MSCs isolated from Wistar rats | 2.4 × 108 particles for 22 h | Co-culture (Pretreatment with 500 nM of AβOs for 2 h) |
Protected neurons from AβOs-induced oxidative stress and synapse damage | [77] |
| Hippocampal neuron culture from rat embryos (E18) | WJ-MSCs | 6 × 108 particles for 22 h | Co-culture (With 500 nM of AβOs for 2 h) |
Protected neurons from AβOs-induced oxidative stress and synapse damage | [78] |
| Cortical neurons culture from C57BL/6 mice embryos (E13–15) | ADSCs | 0.05, 0.1, 1 μg/mL for 24 h | Co-culture (Pretreatment with 20 μM of AβOs) |
Alleviated AβOs-induced neuronal toxicity | [70] |
| In vivo models | |||||
| APP/PS1 mice | |||||
| No age indicate | BM-MSCs | 100 μg/5 μL, once per 2 days for 2 weeks |
i.c.v. | Improved cognitive behavior, rescued impairment of CA1 synaptic transmission and LTP | [79] |
| 7-month-old | UC-MSC | 30 μg/100 μL, every 2 weeks, four times |
i.v. | Reduced Aβ deposition, improved cognitive behavior; enhanced expression of IDE and NEP; modulated the activation of microglia | [85] |
| 7-month-old | PC-BM-MSCs | 150 μg/80 μL, biweekly for 4 months |
i.v. | Improved cognitive behavior, reduced Aβ deposition; decreased proinflammatory factors and increased anti-inflammatory factors | [86] |
| 7-month-old | RVG-BM-MSCs | 5 × 1011 particles/100 μL, monthly for 4 months |
i.v. | Improved cognitive behavior, reduced Aβ deposition, and restored the levels of inflammatory cytokines | [87] |
| 5-month-old | BM-MSCs | 22.4 μg/4 μL | i.c.v | Reduced Aβ deposition and the amount of dystrophic neurons in both the cortex and hippocampus | [88] |
| 9-month-old | UC-MSC | 2 mg/mL, continuously at 0.25 µL/h for 14 days | i.c.v. | Reduced Aβ deposition, improved cognitive behavior and inhibited the inflammatory and oxidative stress | [83] |
| 7-month-old | BM-MSCs | 50 μg/80 μL, every 2 weeks for 16 weeks | i.v. | Reduced Aβ deposition, promoted cognitive function recovery and increased NeuN expression | [89] |
| 4-month-old | miRNA-22-loaded mouse ADSCs | 100 μg/mL, every 7 days until 30 days | i.v. | Improved cognitive behavior, inhibited the inflammatory factors expression and reduced the nerve cell damage | [90] |
| 9-month-old | ADSCs | 1 mg/kg in 10 μL, every two days for 2 weeks | IN | Ameliorated neurologic damage in the whole brain areas, increased neurogenesis, reduced Aβ deposition and decreased microglia activation | [70] |
| J20 mice | |||||
| 9-month-old | WJ-MSCs | 50 µg/100 µL, once a week for 4 weeks |
i.v. | Restored the expression of neuronal memory/synaptic plasticity-related genes, improved brain glucose metabolism and cognitive function; inhibited astrocyte and microglia activation | [71] |
| 3 × Tg | |||||
| 7-month-old | Cytokine-preconditioned BM-MSCs |
30 μg/100 µL | IN | Decreased microglia activation and increased dendritic spine density | [80] |
| 5 × FAD | |||||
| 2-month-old | BM-MSCs | 20 × 108 particles in 5 µL every 4 days until 4 months of age | IN | Improved cognitive behavior, reduced Aβ deposition in the hippocampus and decreased colocalization between GFAP and Aβ plaques | [81] |
| 1.5–2.5-month-old 5.0–6.5-month-old |
hNSC | 2.25 × 107 particles in 50 μL hibernation buffer | i.v. via RO injection | Restored fear extinction memory consolidation and reduced anxiety related behaviors; reduced the dense core Aβ plaque number and microglial activation; restored synaptophysin in the AD brain and homeostatic levels of pro-inflammatory cytokines | [91] |
| Administration of Aβ peptides into the dentate gyrus of C57BL/6 mice 8-week-old | MSCs (No source indicated) |
10 µg/2 µL of PBS | i.c.v. into the dentate gyrus | Promoted neurogenesis in the SVZ and alleviated Aβ1–42-induced cognitive impairment | [76] |
| Administration of Aβ peptides into the lateral ventricle of SD rats (7-week-old) | BM-MSCs isolated from SD rats | 30 μg/100 µL, once a month for 2 months | i.c.v. into the lateral ventricle | Reduced Aβ deposition, reduced the levels of inflammatory cytokines, elevated NEP and IDE expressions, increased neuron viability and reduced apoptosis rate | [92] |
Abbreviation: ADSC, adipose tissue-derived mesenchymal stem cells; WJ-MSCs, Wharton’s jelly mesenchymal stem cells; UC-MSC, umbilical cord mesenchymal stem cells; BM-MSCs, bone marrow-derived mesenchymal stem cells; PC, hypoxia-preconditioned; NSCs, neuronal stem cells; SD rat, Sprague–Dawley rat; RVG, rabies viral glycoprotein; i.v., intravenous injection; i.c.v, intracerebroventricular injection; IN, intranasal; RO, retro-orbital sinus; AβOs, Aβ oligomers; LTP, long-term potentiation; SVZ, subventricular zone; GFAP, glial fibrillary acidic protein; NEP, neprilysin; IDE, insulin-degrading enzyme.
5. Therapeutic Mechanisms of MSC-Derived EVs Actions in AD
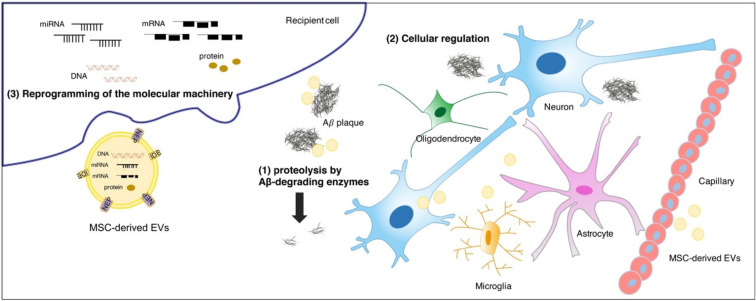
Accumulating studies have uncovered that the considerable therapeutic benefits of MSC-derived EVs can be attributed to the ability to degrade Aβs, modulate immunity and protect neurons in the brain (Figure 1). In this context, MSC-derived EVs are considered to be ideal potential therapeutics for AD.
Figure 1.
The illustration of potential mechanisms of MSC-derived EVs actions in AD. The therapeutic benefits of MSC-derived EVs are attributed to (1) the ability to degrade Aβs by membrane-bound Aβ-degrading enzymes, such as NEP and IDE; (2) the capability to regulate various cells in the brain including immunomodulation or neuroregeneration; (3) the reprogramming of the molecular machinery in recipient cells via proteins, mRNAs, and miRNAs transferred by EVs.
5.1. Aβ Degradation
The Aβ plaques are composed of Aβ peptides, a 40–42 amino acids proteolytic fragment of amyloid precursor protein (APP) [93]. These Aβ peptides undergo an aggregation process resulting in the formation of soluble oligomeric species and insoluble fibrillar species, eventually ending with the deposition of plaques [94]. Numerous reports have described that the excess accumulation might be of a result of a metabolic imbalance between the production and clearance of Aβs, thereby triggering synaptic deficits, neuronal alterations and neurodegeneration [95,96,97]. In clearance systems of the brain, Aβ related degradation clearance is contributed by different proteases, such as neprilysin (NEP), matrix metalloproteinases (MMPs), and glutamate carboxypeptidase II [98,99]. Among them, the critical role of NEP in AD has been intensively studied and thus regarded as a potential target for the treatment of AD [100,101]. Moreover, the expression and activity of NEP are significantly reduced in patients with AD [102]. Enzymatically active NEP expressed in AD-MSC-derived EVs was suggested to decrease both extracellular and intracellular Aβ levels in the N2a cells (a mouse neuroblastoma cell line) [82]. In our study, WJ-MSCs-derived EVs also expressed active NEP on their membranes by means of Western blot and NEP-specific activity assay [71]. Furthermore, MSCs-derived EVs-treated AD rodent models exhibited elevated NEP and IDE expressions along with decreased Aβ depositions [85,92]. Taken together, these reports have demonstrated the potential of MSCs-derived EVs in the treatment of AD and further reflect the feasibility to lower brain Aβ levels by delivering NEP or other Aβ-degrading enzymes.
5.2. Neuroprotection and Neuroregneration
Neuronal networks, astrocytes, microglia and oligodendrocytes contribute to a complex cellular phase of AD evolving over decades. In view of the critical role of neurons in CNS, dysfunction of the brain with AD is mediated by reduction in synaptic plasticity, changes in homeostatic scaling and disruption of neuronal connectivity, which characterize AD dementia [103]. The neuroprotection and neurogenesis contributed by MSC-derived EVs have been demonstrated in vitro and in vivo as addressed above; some of them have delineated the mechanisms of MSC-derived EVs actions. De Godoy et al. reported that the catalase contained in MSC-derived EVs was responsible for neuroprotection from AβOs-induced oxidative stress, and the capacity was checked by a membrane-permeant specific catalase inhibitor [77]. Our study addressed that one potential mechanism of the upregulation of neuronal memory/synaptic plasticity-related genes was in part due to the epigenetic regulation of a class IIa histone deacetylase [71]. On the other hand, EVs isolated from hypoxia preconditioned MSCs culture medium were found to increase the level of miR-21 in the brain of treated AD mice. The replenishment of miR-21 restored the cognitive deficits in AD mice, suggesting that miR-21a act as a regulator in this process [86]. Additionally, in a rat model of traumatic brain injury, MSC-derived EVs transferred miR-133b into astrocytes and neurons to enhance neurogenesis and improve functional recovery [104]. Thus, understanding the detailed mechanisms of MSC-derived EVs actions involved in neuroprotection and neuroregneration is beneficial to enhance the therapeutic potential in AD.
5.3. Immunomodulation
Increasing evidence suggests that AD pathogenesis is closely associated with the neuroinflammation, which might occur at early stage or mild cognitive impairment (MCI) even before Aβ plaque formation [105,106]. MSC-based therapy has been widely conducted in various disease treatments based on their ability to limit tissue inflammation microenvironments through the release of immunomodulatory factors such as prostaglandin E2 (PGE2), hepatic growth factor (HGF), transforming growth factor-β (TGF-β), indolamine 2,3-dioxygenase-1 (IDO-1), interleukin-10 (IL-10) and nitric oxide [65]. In terms of MSC-derived EVs, they acquire a lot of immunologically active molecules to regulate immune cells and thus exert similar therapeutic effects to their parental MSCs [107]. As evidenced by Harting and colleagues, MSCs exposed to TNF-α and IFN-γ generated EVs with a distinctly different profile, including the protein and nucleic acid composition. These EVs were found to partially alter the COX2/PGE2 pathway to enhance their anti-inflammatory properties [108]. In the recent research, cytokine-preconditioned MSC-derived EVs were intranasally administrated into AD mice and found to induce immunomodulatory and neuroprotective effects, evidenced by the inhibition of microglia activation and an increment in the dendritic spine density [80]. Given that EVs isolated from cytokine-pretreated MSCs exhibit more remarkable anti-inflammatory abilities than naïve EVs, it implies that preconditioned MSC-derived EVs might be a better option in the treatment of AD or other inflammatory diseases. It is necessary to compare the therapeutic effect on AD between cytokine-preconditioned MSC-derived EVs and naïve MSC-derived EVs.
MSC-derived EVs can regulate enzyme activity to suppress inflammatory response. Aβs-induce iNOS in glial cells and the subsequent release of high levels of nitric oxide (NO) inhibit integrated mitochondrial respiration, resulting in cell death [109]. Wang et al. demonstrated that BM-MSC-derived EVs not only reduced the expression of iNOS in cultured primary neurons but also significantly alleviated the deficits of CA1 synaptic transmission in APP/PS1 mice [79]. In a similar manner, BM-MSC-derived EVs were able to decrease iNOS expression in a model of osteoarthritis [110]. Additionally, levels of inflammatory cytokines, including IL-1β, IL-6 and TNF-α, were also decreased after MSC-derived EVs treatment [80,92].
Plenty of studies mainly focus on the status of microglia regulated by MSC-derived EVs. In line with other findings, our study also showed that MSC-derived EVs inhibited astrocytes and microglia activation in the brain of AD mice, indicating that these effects are attributed to immunomodulatory properties of EVs [70,71,81]. It should be noted that neuronal networks, astrocytes microglia, oligodendrocytes and the vascular system all contribute to a complex cellular phase of the disease. Once the cellular homeostasis is no longer maintained, the clinical phase of AD is initiated [111]. MSC-based therapy is considered to exert a dynamic homeostatic response that assists in tissue preservation, as well as function recovery, as do the MSC-derived EVs [108,112]. Thus, the effect of MSC-derived EVs on oligodendrocytes and vascular system involved in AD pathogenesis is worthy of further investigation.
6. Clinical Trials of MSC-Derived EVs in AD
The concept of using MSC-derived EVs as a regenerative medicine for neurological diseases or conditions is relatively new. Despite that the results obtained from cell and mouse models of AD have suggested that MSC-derived EVs therapies are promising, few clinical studies for AD currently registered in the National Institutes of Health clinical trials database (Table 2). To date, only one clinical trial has been approved to explore the safety and effectiveness of MSC-derived EVs in patients with mild to moderate dementia (NCT04388982). The researchers plan to give patients three doses of ADSC-derived EVs (5, 10 and 20 μg) via nasal drip, twice a week for 12 weeks. Besides the measurements of liver or kidney function and treatment-related adverse events for safety, the cognitive function tests, quality of life, MRI and PET neuroimaging, and Aβ levels in serum and CSF are further evaluated by schedule. As a good example, the clinical trial of MSC-derived EVs therapy for acute ischemic stroke is implemented based on the finding of EVs mediated delivery of miR-124 inducing neurogenesis after ischemia (NCT03384433) and this study will be completed in December 2021 [113]. Of note, emerging clinical trials using MSC-derived EVs in the treatment of COVID-19 or viral pneumonia are planned for the next two years (NCT04276987, NCT04491240, NCT04657458, NCT04493242), which emphasizes the role of immunomodulation and regeneration of MSC-derived EVs in various diseases.
Table 2.
Clinical trials using MSC-derived EVs in therapies.
| Disease/Condition | Clinical Trial Number | Title | Sponsor |
|---|---|---|---|
| “Exosome” used in title | |||
| Alzheimer’s disease | NCT04388982 | The Safety and the Efficacy Evaluation of Allogenic Adipose MSC-Exos in Patients with Alzheimer’s Disease (Adipose MSC-derived exosomes) | Ruijin Hospital |
| Cerebrovascular disorders | NCT03384433 | Allogenic Mesenchymal Stem Cell Derived Exosome in Patients with Acute Ischemic Stroke | Isfahan University of Medical Sciences |
| Acute respiratory distress syndrome (ARDS) |
NCT04602104 | A Clinical Study of Mesenchymal Stem Cell Exosomes Nebulizer for the Treatment of ARDS | Ruijin Hospital |
| Coronavirus | NCT04276987 | A Pilot Clinical Study on Inhalation of Mesenchymal Stem Cells Exosomes Treating Severe Novel Coronavirus Pneumonia | Ruijin Hospital |
| Healthy | NCT04313647 | A Tolerance Clinical Study on Aerosol Inhalation of Mesenchymal Stem Cells Exosomes in Healthy Volunteers | Ruijin Hospital |
| Macular holes | NCT03437759 | MSC-Exos Promote Healing of MHs | Tianjin Medical University |
| Multiple organ failure | NCT04356300 | Exosome of Mesenchymal Stem Cells for Multiple Organ Dysfuntion Syndrome After Surgical Repaire of Acute Type A Aortic Dissection | Fujian Medical University |
| Dry eye | NCT04213248 | Effect of UMSCs Derived Exosomes on Dry Eye in Patients With cGVHD (Umbilical MSCs derived exosomes) |
Zhongshan Ophthalmic Center, Sun Yat-sen University |
| Drug-resistant | NCT04544215 | A Clinical Study of Mesenchymal Progenitor Cell Exosomes Nebulizer for the Treatment of Pulmonary Infection | Ruijin Hospital |
| Sepsis Critical illness |
NCT04850469 | Study of MSC-Exo on the Therapy for Intensively Ill Children | Children’s Hospital of Fudan University |
| Periodontitis | NCT04270006 | Effect of Adipose Derived Stem Cells Exosomes as an Adjunctive Therapy to Scaling and Root Planning in the Treatment of Periodontitis: A Human Clinical Trial (Adipose derived stem cells exosomes) |
Beni-Suef University |
| COVID-19 SARS-CoV-2 Pneumonia |
NCT04491240 | Evaluation of Safety and Efficiency of Method of Exosome Inhalation in SARS-CoV-2 Associated Pneumonia | State-Financed Health Facility “Samara Regional Medical Center Dinasty” |
| “Extracellular vesicle” used in title | |||
| Bronchopulmonary Dysplasia | NCT03857841 | A Safety Study of IV Stem Cell derived Extracellular Vesicles (UNEX-42) in Preterm Neonates at High Risk for BPD | United Therapeutics |
| Dystrophic epidermolysis Bullosa |
NCT04173650 | MSC Evs in Dystrophic Epidermolysis Bullosa | Aegle Therapeutics |
| COVID-19 ARDS Hypoxia Cytokine storm |
NCT04657458 | Expanded Access Protocol on Bone Marrow Mesenchymal Stem Cell Derived Extracellular Vesicle Infusion Treatment for Patients With COVID-19 Associated ARDS (BM-MSC derived EVs) |
Direct Biologics, LLC |
| COVID-19 ARDS Pneumonia, Viral |
NCT04493242 | Extracellular Vesicle Infusion Treatment for COVID-19 Associated ARDS (BM-MSC derived EVs) |
Direct Biologics, LLC |
According to clinicaltrials.gov as of 30 August 2021.
Although using MSC-derived EVs as cell-free therapy is promising, several major issues should be addressed. The safety and doses for clinical use are certainly priorities; other issues include the establishment of the optimal cell culture conditions, the protocol for isolation, characterization and quantification of MSC-derived EVs, and therapeutic schedules [10,114].
7. Strategies for EV-Based Therapies
As nanoscale biomaterials, various molecules including proteins, RNAs, DNAs, hydrophilic and hydrophobic drugs have been successfully loaded into EVs [115]. The effect induced by these powerful agents in MSC-derived EVs are considered to reflect the “homing” ability of their parental cells, therefore, several studies have demonstrated that the lesions can attract MSC-derived EVs to their vicinity [116,117]. Generally, EVs tend to accumulate in organs that belong to mononuclear phagocyte system (MPS) such as liver and spleen, whereas the uptake by other organs is much lower and the clear-up is much faster [118,119,120]. In the brain, the accumulation of MSC-derived EVs is hardly found due to the BBB. Although MSC-derived EVs with the property of homing should pass through the tight junction in a pathological state expectedly, it is still necessary to enhance the efficacy by increasing the uptake and accumulation in the brain. Several approaches have been investigated to broaden or enhance their therapeutic properties through the modification of EVs and the route of administration applied (Table 3).
Table 3.
A summary of strategies that enhance the efficacy of EV-based therapy for brain diseases.
| Strategies | Cargo-Loaded Molecules | Source of EVs | Disease | Reported Effects | Ref. |
|---|---|---|---|---|---|
| Peptide-tagged | |||||
| Rabies viral glycoprotein (RVG) | Nucleic acid siRNAs specific to BACE1 |
Dendritic cells | AD | Significant knockdown of BACE1 in mRNA and protein levels | [69] |
| Naturally production | BM-MSCs | AD | Improved cognitive behavior, reduced Aβ deposition, and restored the levels of inflammatory cytokines | [87] | |
| miR-124 | Mouse BM-MSCs | Ischemic stroke | Promoted cortical neurogenesis | [113] | |
| siRNAs specific to α-synuclein | Dendritic cells | PD | Decreased α-synuclein aggregation and rescued the loss of dopaminergic neurons | [124] | |
| DNA aptamers that recognize the α-synuclein | HEK293T | PD | Reduced α-synuclein aggregation and improved motor impairments | [125] | |
| RGD peptides | Drug loaded Curcumin |
Mouse BM-MSCs | Ischemic stroke | Strong suppression of the inflammatory response and cellular apoptosis | [126] |
| T7 peptide | Antisense miRNA oligonucleotides against miR-21 (AMO-21) | HEK293T | Glioblastoma | Reduction of tumor sizes | [131] |
| NRP-1-targeted RGE peptide | Superparamagnetic iron oxide nanoparticles (SPIONs) and curcumin | Raw264.7 cells, a macrophage cell line | Glioma | Delayed tumor recurrence, extended the survival of tumor-bearing mice and had targeted-imaging ability | [127] |
| Low-density lipoprotein (LDL) | Drug loaded Methotrexate |
L929, a mouse fibroblastic cell line | Glioma | Prolonged the median survival period | [132] |
| Natural production | |||||
| LFA-1 expression | BDNF | Macrophage | PD | Enhanced delivery and accumulation in inflamed brain | [130] |
| Unidentified | Paclitaxel and doxorubicin | Brain endothelial cells | Brain cancer | Induction of cytotoxic effects against brain cancer | [133] |
| Administration route | |||||
| IN | Unmodified | ADSCs | AD | Decreased AβOs-induced neuronal toxicity | [70,81] |
| Cytokine-stimulated | BM-MSCs | AD | Increased dendritic spine density, reduced Aβ deposition and microglia activation | [80] | |
| Drug loaded Curcumin, JSI-124, a Stat3 inhibitor |
EL-4, a T cell line | Inflammation-mediated disease models, including LPS-induced brain inflammation model, EAE model and a GL26 brain tumor model | Selectively taken up by microglia and induced apoptosis | [134] | |
| Disruption of BBB by pFUS | Unmodified | Blood serum | Glioma | Suppressed glioma growth with no obvious side effects | [129] |
Abbreviation: IN, intranasal; NRP-1, Neuropilin-1; LFA-1, lymphocyte function-associated antigen 1; ICAM-1, intercellular adhesion molecule 1; pFUS, pulsed focused ultrasound; BACE 1, Beta-secretase 1; Stat3, signal transducer and activator of transcription 3; BDNF, brain-derived neurotrophic factor; LPS, lipopolysaccharide; EAE, experimental autoimmune encephalitis.
EVs can be chemically or biologically modified to insert membrane-binding species (e.g., peptides) into the membrane surface and package materials (e.g., drug, miRNA or small interfering RNA) into their vesicle interior [121,122,123]. To improve the brain targeting ability of MSC-derived EVs, Alvarez-Erviti et al. engineered dendritic cells to express Lamp2b, a membrane protein in EVs, fused to the neuron-specific rabies viral glycoprotein (RVG) peptide [69]. These RVG-tagged EVs were additionally loaded with exogenous siRNA specific to β-secretase 1 (BACE1), a key protease implicated in Aβ production. These modified EVs manifested therapeutic potential in AD therapy, demonstrated by the delivery of siRNA specifically to neurons, microglia, oligodendrocytes in the brain and the strong knockdown of BACE1. In a similar manner, this strategy has been applied for guiding MSC-derived EVs to the brain to alleviate AD pathology and deliver certain nucleic acids (DNA aptamer or shRNA specific to α-synuclein) to reduce the α-synuclein aggregates in the PD model [87,124,125]. The utilization of RGD peptides led the EVs to pass the BBB and target the ischemic lesion; meanwhile, the curcumin loaded in EVs was successfully delivered to repress the inflammatory response and cellular apoptosis [126]. Furthermore, EVs can be used as a theranostic agent, combining both targeted imaging and therapeutic effects. Jia et al. loaded superparamagnetic iron oxide nanoparticles (SPIONs) and curcumin into the EVs conjugated with neuropilin-1-targeted peptide and subsequently found the diagnostic and therapeutic effects on glioma were significantly enhanced [127].
To our knowledge, robust neurogenesis was observed after MSC-derived EVs treatment primarily via intracerebroventricular injection or intranasal route in comparison with that via systemic route, suggesting that the amount of MSC-derived EVs accumulated in brain reflects the therapeutic efficacy [70,76,80,81,128]. In addition to intranasal delivery, it is feasible to induce permeability by a temporary disruption of the BBB, such as pulsed focused ultrasound (pFUS). Bai et al. reported that pFUS increased the homing of blood serum-derived EVs to the brain by 4.45-fold and thus the glioma growth significantly was suppressed [129]. Noteworthy, the increased homing to the brain might be attributed to the use of different sources of EVs that certainly express different homing factors on the surface membrane. For example, macrophage-derived EVs were characterized to express the integrin lymphocyte function-associated antigen 1 (LFA-1) and thus was able to interact with intercellular adhesion molecule 1 (ICAM-1), upregulated in inflammation, to promote the uptake of EVs in the BBB cells [130].
Therefore, based on the achievements of abovementioned studies in brain diseases, MSC-derived EVs not only can be applied as active drug themselves but also can be used as a drug delivery vehicle after exogenously re-engineering and modification.
8. Conclusions and Prospects
Taken together, MSC-derived EVs have a lot of potential as therapeutics for AD. In addition to the therapeutic effects, similar to their parent cells, concomitantly they have a lower risk of teratoma formation and the capacity to cross BBB. Currently, the comprehensive works regarding nomenclature, classification and characterization of EVs and their subgroups should be urgently integrated to accelerate research on EVs. The safety, toxicity and doses also need to be further investigated to support the development from bench to bedside. For the EVs’ industry, the address of issues such as the robustness of manufacture, uniformity of production, and scale-up of processes are their priority. In addition, the strategies in accelerating EVs delivery and the action mechanisms should be further clarified. The underlying cellular and molecular mechanisms could stimulate studies about the understanding of pathogenesis and the employment of therapeutic strategies for AD. Especially, the importance of non-neuronal cells in the brain affected by AD is unneglectable. Despite that the utilization of MSC-derived EVs in the treatment of AD is promising, the clinical translation remains a huge challenge and further studies should be carried out to tackle the complicated pathology and promiscuous signaling pathway of AD.
Acknowledgments
The authors thank Tsuey-Ling Jan and the Molecular and Genetic Imaging Core/TMC of National Comprehensive Mouse Phenotyping and Drug Testing Center for assistance with manuscript preparation.
Author Contributions
Conceptualization, Y.-A.C. and R.-S.L.; Validation, Y.-A.C. and R.-S.L.; Investigation, Y.-A.C., C.-H.L. and C.-C.K.; Writing—Original Draft Preparation, Y.-A.C. and C.-H.L.; Writing—Review and Editing, R.-S.L.; Supervision, R.-S.L.; Project Administration, C.-C.K. and R.-S.L.; Funding Acquisition, R.-S.L.; All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the grants: MOST 110-2314-B-350-002 (Ministry of Science and Technology) and MOHW 110-TDU-B-211-144019 (Cancer research project, Ministry of Health and Welfare). The authors thank the technical support of the Molecular and Genetic Imaging Center, National Yang Ming Chiao Tung University and Taiwan Animal Consortium (MOST 110-2740-B-001-002).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tanaka M., Török N., Vécsei L. Novel Pharmaceutical Approaches in Dementia. NeuroPsychopharmacotherapy. 2021:1–18. doi: 10.1007/978-3-319-56015-1_444-1. [DOI] [Google Scholar]
- 2.Hodson R. Alzheimer’s disease. Nature. 2018;559:S1. doi: 10.1038/d41586-018-05717-6. [DOI] [PubMed] [Google Scholar]
- 3.Guo T., Zhang D., Zeng Y., Huang T.Y., Xu H., Zhao Y. Molecular and cellular mechanisms underlying the pathogenesis of Alzheimer’s disease. Mol. Neurodegener. 2020;15:1–37. doi: 10.1186/s13024-020-00391-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stancu I.-C., Vasconcelos B., Terwel D., Dewachter I. Models of β-amyloid induced Tau-pathology: The long and “folded” road to understand the mechanism. Mol. Neurodegener. 2014;9:51. doi: 10.1186/1750-1326-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Menting K.W., Claassen J.A.H.R. β-secretase inhibitor; a promising novel therapeutic drug in Alzheimer’s disease. Front. Aging Neurosci. 2014;6:165. doi: 10.3389/fnagi.2014.00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barve K.H., Kumar M.S. Recent Advancements in Pathogenesis, Diagnostics and Treatment of Alzheimer’s Disease. Curr. Neuropharmacol. 2020;18:1106–1125. doi: 10.2174/1570159x18666200528142429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sevigny J., Chiao P., Bussière T., Weinreb P., Williams L., Maier M., Dunstan R., Salloway S., Chen T., Ling Y., et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537:50–56. doi: 10.1038/nature19323. [DOI] [PubMed] [Google Scholar]
- 8.Rubin R. Recently Approved Alzheimer Drug Raises Questions That Might Never Be Answered. JAMA. 2021;326:469–472. doi: 10.1001/jama.2021.11558. [DOI] [PubMed] [Google Scholar]
- 9.Lalli G., Schott J.M., Hardy J., De Strooper B. Aducanumab: A new phase in therapeutic development for Alzheimer’s disease? EMBO Mol. Med. 2021;13:e14781. doi: 10.15252/emmm.202114781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang L.-K., Chao S.-P., Hu C.-J. Clinical trials of new drugs for Alzheimer disease. J. Biomed. Sci. 2020;27:18. doi: 10.1186/s12929-019-0609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herrup K. The case for rejecting the amyloid cascade hypothesis. Nat. Neurosci. 2015;18:794–799. doi: 10.1038/nn.4017. [DOI] [PubMed] [Google Scholar]
- 12.Van Dyck C.H. Anti-Amyloid-β Monoclonal Antibodies for Alzheimer’s Disease: Pitfalls and Promise. Biol. Psychiatry. 2017;83:311–319. doi: 10.1016/j.biopsych.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pittenger M.F., Discher D.E., Péault B.M., Phinney D.G., Hare J.M., Caplan A.I. Mesenchymal stem cell perspective: Cell biology to clinical progress. NPJ Regen. Med. 2019;4:22. doi: 10.1038/s41536-019-0083-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi M., Zhang Z., Xu R., Lin H., Fu J., Zou Z., Zhang A., Shi J., Chen L., Lv S., et al. Human Mesenchymal Stem Cell Transfusion Is Safe and Improves Liver Function in Acute-on-Chronic Liver Failure Patients. Stem Cells Transl. Med. 2012;1:725–731. doi: 10.5966/sctm.2012-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin B.-L., Chen J.-F., Qiu W.-H., Wang K.-W., Xie D.-Y., Chen X.-Y., Liu Q.-L., Peng L., Li J.-G., Mei Y.-Y., et al. Allogeneic bone marrow-derived mesenchymal stromal cells for hepatitis B virus-related acute-on-chronic liver failure: A randomized controlled trial. Hepatology. 2017;66:209–219. doi: 10.1002/hep.29189. [DOI] [PubMed] [Google Scholar]
- 16.Kim S.H., Cho J.H., Lee Y.H., Lee J.H., Kim S.S., Kim M.Y., Lee M.G., Kang W.Y., Lee K.S., Ahn Y.K., et al. Improvement in Left Ventricular Function with Intracoronary Mesenchymal Stem Cell Therapy in a Patient with Anterior Wall ST-Segment Elevation Myocardial Infarction. Cardiovasc. Drugs Ther. 2018;32:329–338. doi: 10.1007/s10557-018-6804-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karantalis V., DiFede D.L., Gerstenblith G., Pham S., Symes J., Zambrano J.P., Fishman J., Pattany P., McNiece I., Conte J., et al. Autologous Mesenchymal Stem Cells Produce Concordant Improvements in Regional Function, Tissue Perfusion, and Fibrotic Burden When Administered to Patients Undergoing Coronary Artery Bypass Grafting. Circ. Res. 2014;114:1302–1310. doi: 10.1161/CIRCRESAHA.114.303180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee J.S., Hong J.M., Moon G.J., Lee P.H., Ahn Y.H., Bang O.Y. A Long-Term Follow-Up Study of Intravenous Autologous Mesenchymal Stem Cell Transplantation in Patients With Ischemic Stroke. Stem Cells. 2010;28:1099–1106. doi: 10.1002/stem.430. [DOI] [PubMed] [Google Scholar]
- 19.Vaquero J., Zurita M., Rico M.A., Aguayo C., Bonilla C., Marin E., Tapiador N., Sevilla M., Vazquez D., Carballido J., et al. Intrathecal administration of autologous mesenchymal stromal cells for spinal cord injury: Safety and efficacy of the 100/3 guideline. Cytotherapy. 2018;20:806–819. doi: 10.1016/j.jcyt.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 20.Chu K.-A., Wang S.-Y., Yeh C.-C., Fu T.-W., Fu Y.-S., Ko T.-L., Chiu M.-M., Chen T.-H., Tsai P.-J. Reversal of bleomycin-induced rat pulmonary fibrosis by a xenograft of human umbilical mesenchymal stem cells from Wharton’s jelly. Theranostics. 2019;9:6646–6664. doi: 10.7150/thno.33741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sivandzade F., Cucullo L. Regenerative Stem Cell Therapy for Neurodegenerative Diseases: An Overview. Int. J. Mol. Sci. 2021;22:2153. doi: 10.3390/ijms22042153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teixeira F.G., Carvalho M.M., Neves-Carvalho A., Panchalingam K.M., Behie L.A., Pinto L., Sousa N., Salgado A.J. Secretome of Mesenchymal Progenitors from the Umbilical Cord Acts as Modulator of Neural/Glial Proliferation and Differentiation. Stem Cell Rev. Rep. 2014;11:288–297. doi: 10.1007/s12015-014-9576-2. [DOI] [PubMed] [Google Scholar]
- 23.Zilka N., Zilkova M., Kazmerova Z., Sarissky M., Cigankova V., Novak M. Mesenchymal stem cells rescue the Alzheimer’s disease cell model from cell death induced by misfolded truncated tau. Neuroscience. 2011;193:330–337. doi: 10.1016/j.neuroscience.2011.06.088. [DOI] [PubMed] [Google Scholar]
- 24.Oh S.H., Kim H.N., Park H.-J., Shin J.Y., Lee P.H. Mesenchymal Stem Cells Increase Hippocampal Neurogenesis and Neuronal Differentiation by Enhancing the Wnt Signaling Pathway in an Alzheimer’s Disease Model. Cell Transplant. 2015;24:1097–1109. doi: 10.3727/096368914X679237. [DOI] [PubMed] [Google Scholar]
- 25.Xin H., Li Y., Cui Y., Yang J.J., Zhang Z.G., Chopp M. Systemic Administration of Exosomes Released from Mesenchymal Stromal Cells Promote Functional Recovery and Neurovascular Plasticity After Stroke in Rats. Br. J. Pharmacol. 2013;33:1711–1715. doi: 10.1038/jcbfm.2013.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merimi M., El-Majzoub R., Lagneaux L., Agha D.M., Bouhtit F., Meuleman N., Fahmi H., Lewalle P., Fayyad-Kazan M., Najar M. The Therapeutic Potential of Mesenchymal Stromal Cells for Regenerative Medicine: Current Knowledge and Future Understandings. Front. Cell Dev. Biol. 2021;9 doi: 10.3389/fcell.2021.661532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo M., Yin Z., Chen F., Lei P. Mesenchymal stem cell-derived exosome: A promising alternative in the therapy of Alzheimer’s disease. Alzheimer’s Res. Ther. 2020;12:109. doi: 10.1186/s13195-020-00670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teng F., Fussenegger M. Shedding Light on Extracellular Vesicle Biogenesis and Bioengineering. Adv. Sci. 2020;8:2003505. doi: 10.1002/advs.202003505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dang X.T.T., Kavishka J.M., Zhang D.X., Pirisinu M., Le M.T.N. Extracellular Vesicles as an Efficient and Versatile System for Drug Delivery. Cells. 2020;9:2191. doi: 10.3390/cells9102191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sidhom K., Obi P., Saleem A. A Review of Exosomal Isolation Methods: Is Size Exclusion Chromatography the Best Option? Int. J. Mol. Sci. 2020;21:6466. doi: 10.3390/ijms21186466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Konoshenko M.Y., Lekchnov E.A., Vlassov A.V., Laktionov P.P. Isolation of Extracellular Vesicles: General Methodologies and Latest Trends. BioMed Res. Int. 2018;2018:8545347. doi: 10.1155/2018/8545347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liangsupree T., Multia E., Riekkola M.-L. Modern isolation and separation techniques for extracellular vesicles. J. Chromatogr. 2020;1636:461773. doi: 10.1016/j.chroma.2020.461773. [DOI] [PubMed] [Google Scholar]
- 33.Tan S.J.O., Floriano J.F., Nicastro L., Emanueli C., Catapano F. Novel Applications of Mesenchymal Stem Cell-Derived Exosomes for Myocardial Infarction Therapeutics. Biomolecules. 2020;10:707. doi: 10.3390/biom10050707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doyle L.M., Wang M.Z. Overview of Extracellular Vesicles, Their Origin, Composition, Purpose, and Methods for Exosome Isolation and Analysis. Cells. 2019;8:727. doi: 10.3390/cells8070727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Futter C., Pearse A., Hewlett L.J., Hopkins C.R. Multivesicular endosomes containing internalized EGF-EGF receptor complexes mature and then fuse directly with lysosomes. J. Cell Biol. 1996;132:1011–1023. doi: 10.1083/jcb.132.6.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palmulli R., Van Niel G. To be or not to be. secreted as exosomes, a balance finely tuned by the mechanisms of biogenesis. Essays Biochem. 2018;62:177–191. doi: 10.1042/ebc20170076. [DOI] [PubMed] [Google Scholar]
- 37.Clancy J.W., Schmidtmann M., D’Souza-Schorey C. The ins and outs of microvesicles. FASEB BioAdvances. 2021;3:399–406. doi: 10.1096/fba.2020-00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taylor J., Bebawy M. Proteins Regulating Microvesicle Biogenesis and Multidrug Resistance in Cancer. Proteomics. 2018;19:e1800165. doi: 10.1002/pmic.201800165. [DOI] [PubMed] [Google Scholar]
- 39.Song Y., Kim Y., Ha S., Sheller-Miller S., Yoo J., Choi C., Park C.H. The emerging role of exosomes as novel therapeutics: Biology, technologies, clinical applications, and the next. Am. J. Reprod. Immunol. 2020;85:e13329. doi: 10.1111/aji.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nabhan J.F., Hu R., Oh R.S., Cohen S.N., Lu Q. Formation and release of arrestin domain-containing protein 1-mediated microvesicles (ARMMs) at plasma membrane by recruitment of TSG101 protein. Proc. Natl. Acad. Sci. USA. 2012;109:4146–4151. doi: 10.1073/pnas.1200448109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wei D., Zhan W., Gao Y., Huang L., Gong R., Wang W., Zhang R., Wu Y., Gao S., Kang T. RAB31 marks and controls an ESCRT-independent exosome pathway. Cell Res. 2020;31:157–177. doi: 10.1038/s41422-020-00409-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akers J.C., Gonda D., Kim R., Carter B.S., Chen C.C. Biogenesis of extracellular vesicles (EV): Exosomes, microvesicles, retrovirus-like vesicles, and apoptotic bodies. J. Neuro-Oncology. 2013;113:1–11. doi: 10.1007/s11060-013-1084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abou-Ghali M., Stiban J. Regulation of ceramide channel formation and disassembly: Insights on the initiation of apoptosis. Saudi J. Biol. Sci. 2015;22:760–772. doi: 10.1016/j.sjbs.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ma Q., Liang M., Wu Y., Luo F., Ma Z., Dong S., Xu J., Dou C. Osteoclast-derived apoptotic bodies couple bone resorption and formation in bone remodeling. Bone Res. 2021;9:5. doi: 10.1038/s41413-020-00121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Balakrishnan A., Roy S., Fleming T., Leong H.S., Schuurmans C. The Emerging Role of Extracellular Vesicles in the Glioma Microenvironment: Biogenesis and Clinical Relevance. Cancers. 2020;12:1964. doi: 10.3390/cancers12071964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bazzan E., Tinè M., Casara A., Biondini D., Semenzato U., Cocconcelli E., Balestro E., Damin M., Radu C., Turato G., et al. Critical Review of the Evolution of Extracellular Vesicles’ Knowledge: From 1946 to Today. Int. J. Mol. Sci. 2021;22:6417. doi: 10.3390/ijms22126417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang B., Xing D., Zhu Y., Dong S., Zhao B. The State of Exosomes Research: A Global Visualized Analysis. BioMed Res. Int. 2019;2019:1–10. doi: 10.1155/2019/1495130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Palviainen M., Saraswat M., Varga Z., Kitka D., Neuvonen M., Puhka M., Joenväärä S., Renkonen R., Nieuwland R., Takatalo M., et al. Extracellular vesicles from human plasma and serum are carriers of extravesicular cargo—Implications for biomarker discovery. PLoS ONE. 2020;15:e0236439. doi: 10.1371/journal.pone.0236439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Théry C., Witwer K.W., Aikawa E., Alcaraz M.J., Anderson J.D., Andriantsitohaina R., Antoniou A., Arab T., Archer F., Atkin-Smith G.K., et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles. 2018;7:1535750. doi: 10.1080/20013078.2018.1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Witwer K.W., Théry C. Extracellular vesicles or exosomes? On primacy, precision, and popularity influencing a choice of nomenclature. J. Extracell. Vesicles. 2019;8:1648167. doi: 10.1080/20013078.2019.1648167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang Y., Liu Y., Liu H., Tang W.H. Exosomes: Biogenesis, biologic function and clinical potential. Cell Biosci. 2019;9:1–18. doi: 10.1186/s13578-019-0282-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lässer C., Eldh M., Lötvall J. Isolation and Characterization of RNA-Containing Exosomes. J. Vis. Exp. 2012;59:e3037. doi: 10.3791/3037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gutierrez-Vazquez C., Villarroya-Beltri C., Mittelbrunn M., Sánchez-Madrid F. Transfer of extracellular vesicles during immune cell-cell interactions. Immunol. Rev. 2012;251:125–142. doi: 10.1111/imr.12013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Qiu G., Zheng G., Ge M., Wang J., Huang R., Shu Q., Xu J. Functional proteins of mesenchymal stem cell-derived extracellular vesicles. Stem Cell Res. Ther. 2019;10:359. doi: 10.1186/s13287-019-1484-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Samanta S., Rajasingh S., Drosos N., Zhou Z., Dawn B., Rajasingh J. Exosomes: New molecular targets of diseases. Acta Pharmacol. Sin. 2017;39:501–513. doi: 10.1038/aps.2017.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Menck K., Sivaloganathan S., Bleckmann A., Binder C. Microvesicles in Cancer: Small Size, Large Potential. Int. J. Mol. Sci. 2020;21:5373. doi: 10.3390/ijms21155373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen Y., Li G., Liu M.-L. Microvesicles as Emerging Biomarkers and Therapeutic Targets in Cardiometabolic Diseases. Genom. Proteom. Bioinform. 2018;16:50–62. doi: 10.1016/j.gpb.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kaid C., Assoni A., Marçola M., Semedo-Kuriki P., Bortolin R.H., Carvalho V.M., Okamoto O.K. Proteome and miRNome profiling of microvesicles derived from medulloblastoma cell lines with stem-like properties reveals biomarkers of poor prognosis. Brain Res. 2020;1730:146646. doi: 10.1016/j.brainres.2020.146646. [DOI] [PubMed] [Google Scholar]
- 59.Serrano-Heras G., Díaz-Maroto I., Castro-Robles B., Carrión B., Perona-Moratalla A.B., Gracia J., Arteaga S., Hernández-Fernández F., García-García J., Ayo-Martín O., et al. Isolation and Quantification of Blood Apoptotic Bodies, a Non-invasive Tool to Evaluate Apoptosis in Patients with Ischemic Stroke and Neurodegenerative Diseases. Biol. Proced. Online. 2020;22:17. doi: 10.1186/s12575-020-00130-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kakarla R., Hur J., Kim Y.J., Kim J., Chwae Y.-J. Apoptotic cell-derived exosomes: Messages from dying cells. Exp. Mol. Med. 2020;52:1–6. doi: 10.1038/s12276-019-0362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Caruso S., Poon I.K.H., Caruso S., Poon I.K.H. Apoptotic Cell-Derived Extracellular Vesicles: More Than Just Debris. Front. Immunol. 2018;9:1486. doi: 10.3389/fimmu.2018.01486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pant S., Hilton H., Burczynski M.E. The multifaceted exosome: Biogenesis, role in normal and aberrant cellular function, and frontiers for pharmacological and biomarker opportunities. Biochem. Pharmacol. 2012;83:1484–1494. doi: 10.1016/j.bcp.2011.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gurung S., Perocheau D., Touramanidou L., Baruteau J. The exosome journey: From biogenesis to uptake and intracellular signalling. Cell Commun. Signal. 2021;19:47. doi: 10.1186/s12964-021-00730-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vizoso F.J., Eiro N., Cid S., Schneider J., Perez-Fernandez R. Mesenchymal Stem Cell Secretome: Toward Cell-Free Therapeutic Strategies in Regenerative Medicine. Int. J. Mol. Sci. 2017;18:1852. doi: 10.3390/ijms18091852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Phinney D.G., Pittenger M.F. Concise Review: MSC-Derived Exosomes for Cell-Free Therapy. Stem Cells. 2017;35:851–858. doi: 10.1002/stem.2575. [DOI] [PubMed] [Google Scholar]
- 66.Bang O.Y., Kim E.H. Mesenchymal Stem Cell-Derived Extracellular Vesicle Therapy for Stroke: Challenges and Progress. Front. Neurol. 2019;10:211. doi: 10.3389/fneur.2019.00211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Abreu S.C., Lopes-Pacheco M., Weiss D.J., Rocco P.R.M. Mesenchymal Stromal Cell-Derived Extracellular Vesicles in Lung Diseases: Current Status and Perspectives. Front. Cell Dev. Biol. 2021;9:97. doi: 10.3389/fcell.2021.600711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Eirin A., Lerman L.O. Mesenchymal Stem/Stromal Cell–Derived Extracellular Vesicles for Chronic Kidney Disease: Are We There Yet? Hypertension. 2021;78:261–269. doi: 10.1161/HYPERTENSIONAHA.121.14596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Alvarez-Erviti L., Seow Y., Yin H., Betts C., Lakhal S., Wood M.J.A. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat. Biotechnol. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 70.Ma X., Huang M., Zheng M., Dai C., Song Q., Zhang Q., Li Q., Gu X., Chen H., Jiang G., et al. ADSCs-derived extracellular vesicles alleviate neuronal damage, promote neurogenesis and rescue memory loss in mice with Alzheimer’s disease. J. Control. Release. 2020;327:688–702. doi: 10.1016/j.jconrel.2020.09.019. [DOI] [PubMed] [Google Scholar]
- 71.Chen Y.-A., Lu C.-H., Ke C.-C., Chiu S.-J., Jeng F.-S., Chang C.-W., Yang B.-H., Liu R.-S. Mesenchymal Stem Cell-Derived Exosomes Ameliorate Alzheimer’s Disease Pathology and Improve Cognitive Deficits. Biomedicines. 2021;9:594. doi: 10.3390/biomedicines9060594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gratpain V., Mwema A., Labrak Y., Muccioli G.G., van Pesch V., Rieux A.D. Extracellular vesicles for the treatment of central nervous system diseases. Adv. Drug Deliv. Rev. 2021;174:535–552. doi: 10.1016/j.addr.2021.05.006. [DOI] [PubMed] [Google Scholar]
- 73.Matsumoto J., Stewart T., Sheng L., Li N., Bullock K., Song N., Shi M., Banks W.A., Zhang J. Transmission of α-synuclein-containing erythrocyte-derived extracellular vesicles across the blood-brain barrier via adsorptive mediated transcytosis: Another mechanism for initiation and progression of Parkinson’s disease? Acta Neuropathol. Commun. 2017;5:71. doi: 10.1186/s40478-017-0470-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen C.C., Liu L., Ma F., Wong C.W., Guo X.E., Chacko J.V., Farhoodi H., Zhang S., Zimak J., Ségaliny A., et al. Elucidation of Exosome Migration Across the Blood–Brain Barrier Model In Vitro. Cell. Mol. Bioeng. 2016;9:509–529. doi: 10.1007/s12195-016-0458-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ridder K., Keller S., Dams M., Rupp A.-K., Schlaudraff J., Del Turco D., Starmann J., Macas J., Karpova D., Devraj K., et al. Extracellular Vesicle-Mediated Transfer of Genetic Information between the Hematopoietic System and the Brain in Response to Inflammation. PLoS Biol. 2014;12:e1001874. doi: 10.1371/journal.pbio.1001874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Reza-Zaldivar E.E., Hernández-Sapiéns M.A., Gutiérrez-Mercado Y.K., Sandoval-Ávila S., Gomez-Pinedo U., Márquez-Aguirre A.L., Vazquez-Mendez E., Padilla-Camberos E., Canales-Aguirre A.A. Mesenchymal stem cell-derived exosomes promote neurogenesis and cognitive function recovery in a mouse model of Alzheimer’s disease. Neural Regen. Res. 2019;14:1626–1634. doi: 10.4103/1673-5374.255978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.De Godoy M.A., Saraiva L.M., de Carvalho L.R., Vasconcelos-Dos-Santos A., Beiral H.J., Ramos A.B., Silva L.R.D.P., Leal R.B., Monteiro V.H.S., Braga C.V., et al. Mesenchymal stem cells and cell-derived extracellular vesicles protect hippocampal neurons from oxidative stress and synapse damage induced by amyloid-β oligomers. J. Biol. Chem. 2018;293:1957–1975. doi: 10.1074/jbc.M117.807180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bodart-Santos V., De Carvalho L.R.P., De Godoy M.A., Batista A.F., Saraiva L.M., Lima L.G., Abreu C.A., De Felice F.G., Galina A., Mendez-Otero R., et al. Extracellular vesicles derived from human Wharton’s jelly mesenchymal stem cells protect hippocampal neurons from oxidative stress and synapse damage induced by amyloid-β oligomers. Stem Cell Res. Ther. 2019;10:332. doi: 10.1186/s13287-019-1432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang S.-S., Jia J., Wang Z. Mesenchymal Stem Cell-Derived Extracellular Vesicles Suppresses iNOS Expression and Ameliorates Neural Impairment in Alzheimer’s Disease Mice. J. Alzheimer’s Dis. 2018;61:1005–1013. doi: 10.3233/JAD-170848. [DOI] [PubMed] [Google Scholar]
- 80.Losurdo M., Pedrazzoli M., D’Agostino C., Elia C.A., Massenzio F., Lonati E., Mauri M., Rizzi L., Molteni L., Bresciani E., et al. Intranasal delivery of mesenchymal stem cell-derived extracellular vesicles exerts immunomodulatory and neuroprotective effects in a 3xTg model of Alzheimer’s disease. Stem Cells Transl. Med. 2020;9:1068–1084. doi: 10.1002/sctm.19-0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cone A.S., Yuan X., Sun L., Duke L.C., Vreones M.P., Carrier A.N., Kenyon S.M., Carver S.R., Benthem S.D., Stimmell A.C., et al. Mesenchymal stem cell-derived extracellular vesicles ameliorate Alzheimer’s disease-like phenotypes in a preclinical mouse model. Theranostics. 2021;11:8129–8142. doi: 10.7150/thno.62069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Katsuda T., Tsuchiya R., Kosaka N., Yoshioka Y., Takagaki K., Oki K., Takeshita F., Sakai Y., Kuroda M., Ochiya T. Human adipose tissue-derived mesenchymal stem cells secrete functional neprilysin-bound exosomes. Sci. Rep. 2013;3:1–11. doi: 10.1038/srep01197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yang L., Zhai Y., Hao Y., Zhu Z., Cheng G. The Regulatory Functionality of Exosomes Derived from hUMSCs in 3D Culture for Alzheimer’s Disease Therapy. Small. 2019;16:e1906273. doi: 10.1002/smll.201906273. [DOI] [PubMed] [Google Scholar]
- 84.Lee M., Ban J.-J., Yang S., Im W., Kim M. The exosome of adipose-derived stem cells reduces β-amyloid pathology and apoptosis of neuronal cells derived from the transgenic mouse model of Alzheimer’s disease. Brain Res. 2018;1691:87–93. doi: 10.1016/j.brainres.2018.03.034. [DOI] [PubMed] [Google Scholar]
- 85.Ding M., Shen Y., Wang P., Xie Z., Xu S., Zhu Z., Wang Y., Lyu Y., Wang D., Xu L., et al. Exosomes Isolated From Human Umbilical Cord Mesenchymal Stem Cells Alleviate Neuroinflammation and Reduce Amyloid-Beta Deposition by Modulating Microglial Activation in Alzheimer’s Disease. Neurochem. Res. 2018;43:2165–2177. doi: 10.1007/s11064-018-2641-5. [DOI] [PubMed] [Google Scholar]
- 86.Cui G., Wu J., Mou F., Xie W., Wang F., Wang Q., Fang J., Xu Y., Dong Y., Liu J., et al. Exosomes derived from hypoxia-preconditioned mesenchymal stromal cells ameliorate cognitive decline by rescuing synaptic dysfunction and regulating inflammatory responses in APP/PS1 mice. FASEB J. 2018;32:654–668. doi: 10.1096/fj.201700600R. [DOI] [PubMed] [Google Scholar]
- 87.Cui G.-H., Guo H.-D., Li H., Zhai Y., Gong Z.-B., Wu J., Liu J.-S., Dong Y.-R., Hou S.-X. RVG-modified exosomes derived from mesenchymal stem cells rescue memory deficits by regulating inflammatory responses in a mouse model of Alzheimer’s disease. Immun. Ageing. 2019;16:1–12. doi: 10.1186/s12979-019-0150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Elia C.A., Tamborini M., Rasile M., Desiato G., Marchetti S., Swuec P., Mazzitelli S., Clemente F., Anselmo A., Matteoli M., et al. Intracerebral Injection of Extracellular Vesicles from Mesenchymal Stem Cells Exerts Reduced Aβ Plaque Burden in Early Stages of a Preclinical Model of Alzheimer’s Disease. Cells. 2019;8:1059. doi: 10.3390/cells8091059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang X., Yang G. Bone marrow mesenchymal stem cells-derived exosomes reduce Aβ deposition and improve cognitive function recovery in mice with Alzheimer’s disease by activating sphingosine kinase/sphingosine-1-phosphate signaling pathway. Cell Biol. Int. 2020;45:775–784. doi: 10.1002/cbin.11522. [DOI] [PubMed] [Google Scholar]
- 90.Zhai L., Shen H., Sheng Y., Guan Q. ADMSC Exo-MicroRNA-22 improve neurological function and neuroinflammation in mice with Alzheimer’s disease. J. Cell. Mol. Med. 2021;25:7513–7523. doi: 10.1111/jcmm.16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Apodaca L.A., Baddour A.A.D., Garcia C., Alikhani L., Giedzinski E., Ru N., Agrawal A., Acharya M.M., Baulch J.E. Human neural stem cell-derived extracellular vesicles mitigate hallmarks of Alzheimer’s disease. Alzheimer’s Res. Ther. 2021;13:57. doi: 10.1186/s13195-021-00791-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sha S., Shen X., Cao Y., Qu L. Mesenchymal stem cells-derived extracellular vesicles ameliorate Alzheimer’s disease in rat models via the microRNA-29c-3p/BACE1 axis and the Wnt/β-catenin pathway. Aging. 2021;13:15285–15306. doi: 10.18632/aging.203088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Van Es M.A., Berg L.H.V.D. Alzheimer’s disease beyond APOE. Nat. Genet. 2009;41:1047–1048. doi: 10.1038/ng1009-1047. [DOI] [PubMed] [Google Scholar]
- 94.Huang L., Su X., Federoff H.J. Single-Chain Fragment Variable Passive Immunotherapies for Neurodegenerative Diseases. Int. J. Mol. Sci. 2013;14:19109–19127. doi: 10.3390/ijms140919109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dahlgren K.N., Manelli A.M., Stine W.B., Baker L., Krafft G.A., LaDu M.J. Oligomeric and Fibrillar Species of Amyloid-β Peptides Differentially Affect Neuronal Viability. J. Biol. Chem. 2002;277:32046–32053. doi: 10.1074/jbc.M201750200. [DOI] [PubMed] [Google Scholar]
- 96.Haass C., Selkoe D.J. Soluble protein oligomers in neurodegeneration: Lessons from the Alzheimer’s amyloid β-peptide. Nat. Rev. Mol. Cell Biol. 2007;8:101–112. doi: 10.1038/nrm2101. [DOI] [PubMed] [Google Scholar]
- 97.Shankar G.M., Li S., Mehta T.H., Garcia-Munoz A., Shepardson N.E., Smith I., Brett F.M., Farrell M.A., Rowan M.J., Lemere C.A., et al. Amyloid-β protein dimers isolated directly from Alzheimer’s brains impair synaptic plasticity and memory. Nat. Med. 2008;14:837–842. doi: 10.1038/nm1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tarasoff-Conway J.M., Carare R.O., Osorio R., Glodzik L., Butler T., Fieremans E., Axel L., Rusinek H., Nicholson C., Zlokovic B.V., et al. Clearance systems in the brain—implications for Alzheimer disease. Nat. Rev. Neurol. 2015;11:457–470. doi: 10.1038/nrneurol.2015.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Erickson M., Banks W.A. Blood–Brain Barrier Dysfunction as a Cause and Consequence of Alzheimer’s Disease. Br. J. Pharmacol. 2013;33:1500–1513. doi: 10.1038/jcbfm.2013.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Iwata N., Tsubuki S., Takaki Y., Shirotani K., Lu B., Gerard N.P., Gerard C., Hama E., Lee H.-J., Saido T.C. Metabolic Regulation of Brain Aβ by Neprilysin. Science. 2001;292:1550–1552. doi: 10.1126/science.1059946. [DOI] [PubMed] [Google Scholar]
- 101.Iwata N., Tsubuki S., Takaki Y., Watanabe K., Sekiguchi M., Hosoki E., Kawashima-Morishima M., Lee H.-J., Hama E., Sekine-Aizawa Y., et al. Identification of the major Aβ1–42-degrading catabolic pathway in brain parenchyma: Suppression leads to biochemical and pathological deposition. Nat. Med. 2000;6:143–150. doi: 10.1038/72237. [DOI] [PubMed] [Google Scholar]
- 102.Yasojima K., Akiyama H., McGeer E.G., McGeer P.L. Reduced neprilysin in high plaque areas of Alzheimer brain: A possible relationship to deficient degradation of β-amyloid peptide. Neurosci. Lett. 2001;297:97–100. doi: 10.1016/S0304-3940(00)01675-X. [DOI] [PubMed] [Google Scholar]
- 103.Mufson E., Mahady L., Waters D., Counts S., Perez S., DeKosky S., Ginsberg S., Ikonomovic M., Scheff S., Binder L. Hippocampal plasticity during the progression of Alzheimer’s disease. Neuroscience. 2015;309:51–67. doi: 10.1016/j.neuroscience.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Xin H., Li Y., Liu Z., Wang X., Shang X., Cui Y., Zhang Z.G., Chopp M. MiR-133b Promotes Neural Plasticity and Functional Recovery After Treatment of Stroke with Multipotent Mesenchymal Stromal Cells in Rats Via Transfer of Exosome-Enriched Extracellular Particles. Stem Cells. 2013;31:2737–2746. doi: 10.1002/stem.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Heneka M.T., Carson M.J., El Khoury J., Landreth G.E., Brosseron F., Feinstein D.L., Jacobs A.H., Wyss-Coray T., Vitorica J., Ransohoff R.M., et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015;14:388–405. doi: 10.1016/S1474-4422(15)70016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chasaide C.N., Lynch M.A. The role of the immune system in driving neuroinflammation. Brain Neurosci. Adv. 2020;4:2398212819901082. doi: 10.1177/2398212819901082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Xie M., Xiong W., She Z., Wen Z., Abdirahman A.S., Wan W., Wen C. Immunoregulatory Effects of Stem Cell-Derived Extracellular Vesicles on Immune Cells. Front. Immunol. 2020;11:13. doi: 10.3389/fimmu.2020.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Harting M.T., Srivastava A., Zhaorigetu S., Bair H., Prabhakara K.S., Furman N.E.T., Vykoukal J.V., Ruppert K.A., Cox C.S., Olson S.D. Inflammation-Stimulated Mesenchymal Stromal Cell-Derived Extracellular Vesicles Attenuate Inflammation. Stem Cells. 2017;36:79–90. doi: 10.1002/stem.2730. [DOI] [PubMed] [Google Scholar]
- 109.Togo T., Katsuse O., Iseki E. Nitric oxide pathways in Alzheimer’s disease and other neurodegenerative dementias. Neurol. Res. 2004;26:563–566. doi: 10.1179/016164104225016236. [DOI] [PubMed] [Google Scholar]
- 110.Cosenza S., Ruiz M., Toupet K., Jorgensen C., Noël D. Mesenchymal stem cells derived exosomes and microparticles protect cartilage and bone from degradation in osteoarthritis. Sci. Rep. 2017;7:1–12. doi: 10.1038/s41598-017-15376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.De Strooper B., Karran E. The Cellular Phase of Alzheimer’s Disease. Cell. 2016;164:603–615. doi: 10.1016/j.cell.2015.12.056. [DOI] [PubMed] [Google Scholar]
- 112.Vizoso F., Fernández-Francos S., Eiro N. Mesenchymal Stem/Stromal Cells and Their Derivates in Acute Diseases: Emergency in the Post-COVID-19 Times. Int. J. Mol. Sci. 2021;22:8395. doi: 10.3390/ijms22168395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yang J., Zhang X., Chen X., Wang L., Yang G. Exosome Mediated Delivery of miR-124 Promotes Neurogenesis after Ischemia. Mol. Ther. Nucleic Acids. 2017;7:278–287. doi: 10.1016/j.omtn.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mendt M., Rezvani K., Shpall E. Mesenchymal stem cell-derived exosomes for clinical use. Bone Marrow Transplant. 2019;54:789–792. doi: 10.1038/s41409-019-0616-z. [DOI] [PubMed] [Google Scholar]
- 115.Fu S., Wang Y., Xia X., Zheng J.C. Exosome engineering: Current progress in cargo loading and targeted delivery. NanoImpact. 2020;20:100261. doi: 10.1016/j.impact.2020.100261. [DOI] [Google Scholar]
- 116.Seo Y., Kim H.-S., Hong I.-S. Stem Cell-Derived Extracellular Vesicles as Immunomodulatory Therapeutics. Stem Cells Int. 2019;2019:5126156. doi: 10.1155/2019/5126156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Grange C., Tapparo M., Bruno S., Chatterjee D., Quesenberry P.J., Tetta C., Camussi G. Biodistribution of mesenchymal stem cell-derived extracellular vesicles in a model of acute kidney injury monitored by optical imaging. Int. J. Mol. Med. 2014;33:1055–1063. doi: 10.3892/ijmm.2014.1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Shao J., Zaro J., Shen Y. Advances in Exosome-Based Drug Delivery and Tumor Targeting: From Tissue Distribution to Intracellular Fate. Int. J. Nanomed. 2020;15:9355–9371. doi: 10.2147/IJN.S281890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lu C.-H., Chen Y.-A., Ke C.-C., Chiu S.-J., Chen C.-C., Hsieh Y.-J., Yang B.-H., Liu R.-S. Preclinical Characterization and In Vivo Imaging of 111In-Labeled Mesenchymal Stem Cell–Derived Extracellular Vesicles. Mol. Imaging Biol. 2020;23:361–371. doi: 10.1007/s11307-020-01562-0. [DOI] [PubMed] [Google Scholar]
- 120.Takahashi Y., Nishikawa M., Shinotsuka H., Matsui Y., Ohara S., Imai T., Takakura Y. Visualization and in vivo tracking of the exosomes of murine melanoma B16-BL6 cells in mice after intravenous injection. J. Biotechnol. 2013;165:77–84. doi: 10.1016/j.jbiotec.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 121.Armstrong J.P.K., Holme M., Stevens M.M. Re-Engineering Extracellular Vesicles as Smart Nanoscale Therapeutics. ACS Nano. 2017;11:69–83. doi: 10.1021/acsnano.6b07607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Piffoux M., Nicolás-Boluda A., Mulens-Arias V., Richard S., Rahmi G., Gazeau F., Wilhelm C., Silva A.K. Extracellular vesicles for personalized medicine: The input of physically triggered production, loading and theranostic properties. Adv. Drug Deliv. Rev. 2018;138:247–258. doi: 10.1016/j.addr.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 123.Jurgielewicz B., Stice S., Yao Y. Therapeutic Potential of Nucleic Acids when Combined with Extracellular Vesicles. Aging Dis. 2021;12:1476–1493. doi: 10.14336/AD.2021.0708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Izco M., Blesa J., Schleef M., Schmeer M., Porcari R., Al-Shawi R., Ellmerich S., De Toro M., Gardiner C., Seow Y., et al. Systemic Exosomal Delivery of shRNA Minicircles Prevents Parkinsonian Pathology. Mol. Ther. 2019;27:2111–2122. doi: 10.1016/j.ymthe.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ren X., Zhao Y., Xue F., Zheng Y., Huang H., Wang W., Chang Y., Yang H., Zhang J. Exosomal DNA Aptamer Targeting α-Synuclein Aggregates Reduced Neuropathological Deficits in a Mouse Parkinson’s Disease Model. Mol. Ther. Nucleic Acids. 2019;17:726–740. doi: 10.1016/j.omtn.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tian T., Zhang H.-X., He C.-P., Fan S., Zhu Y.-L., Qi C., Huang N.-P., Xiao Z.-D., Lu Z.-H., Tannous B.A., et al. Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials. 2017;150:137–149. doi: 10.1016/j.biomaterials.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 127.Jia G., Han Y., An Y., Ding Y., He C., Wang X., Tang Q. NRP-1 targeted and cargo-loaded exosomes facilitate simultaneous imaging and therapy of glioma in vitro and in vivo. Biomaterials. 2018;178:302–316. doi: 10.1016/j.biomaterials.2018.06.029. [DOI] [PubMed] [Google Scholar]
- 128.Wang Z., Xiong G., Tsang W.C., Schätzlein A.G., Uchegbu I.F. Nose-to-Brain Delivery. J. Pharmacol. Exp. Ther. 2019;370:593–601. doi: 10.1124/jpet.119.258152. [DOI] [PubMed] [Google Scholar]
- 129.Bai L., Liu Y., Guo K., Zhang K., Liu Q., Wang P., Wang X. Ultrasound Facilitates Naturally Equipped Exosomes Derived from Macrophages and Blood Serum for Orthotopic Glioma Treatment. ACS Appl. Mater. Interfaces. 2019;11:14576–14587. doi: 10.1021/acsami.9b00893. [DOI] [PubMed] [Google Scholar]
- 130.Yuan D., Zhao Y., Banks W.A., Bullock K.M., Haney M., Batrakova E., Kabanov A.V. Macrophage exosomes as natural nanocarriers for protein delivery to inflamed brain. Biomaterials. 2017;142:1–12. doi: 10.1016/j.biomaterials.2017.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kim G., Kim M., Lee Y., Byun J.W., Hwang D.W., Lee M. Systemic delivery of microRNA-21 antisense oligonucleotides to the brain using T7-peptide decorated exosomes. J. Control. Release. 2020;317:273–281. doi: 10.1016/j.jconrel.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 132.Ye Z., Zhang T., He W., Jin H., Liu C., Yang Z., Ren J. Methotrexate-Loaded Extracellular Vesicles Functionalized with Therapeutic and Targeted Peptides for the Treatment of Glioblastoma Multiforme. ACS Appl. Mater. Interfaces. 2018;10:12341–12350. doi: 10.1021/acsami.7b18135. [DOI] [PubMed] [Google Scholar]
- 133.Yang T., Martin P., Fogarty B., Brown A., Schurman K., Phipps R., Yin V.P., Lockman P., Bai S. Exosome Delivered Anticancer Drugs Across the Blood-Brain Barrier for Brain Cancer Therapy in Danio Rerio. Pharm. Res. 2015;32:2003–2014. doi: 10.1007/s11095-014-1593-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhuang X., Xiang X., Grizzle W., Sun D., Zhang S., Axtell R.C., Ju S., Mu J., Zhang L., Steinman L., et al. Treatment of Brain Inflammatory Diseases by Delivering Exosome Encapsulated Anti-inflammatory Drugs From the Nasal Region to the Brain. Mol. Ther. 2011;19:1769–1779. doi: 10.1038/mt.2011.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.